- 1Royal College of Surgeons Ireland, Bahrain RCSI–Medical University of Bahrain (MUB), Busaiteen, Bahrain
- 2University of Sharjah, Sharjah, United Arab Emirates
Introduction: A compassionate and patient-centered care leads to improved clinical outcomes. Promoting empathy and compassion of medical students is a forerunner of their well-being, emotional stability, and a patient-centered care. However, there is slender evidence about best educational interventions that can inculcate empathy and compassion skills. Our objective was to conduct a systematic review of research evaluating the associations between spectrum, effectiveness, frequency of teaching modalities and their outcomes on compassion and empathy to highlight best practices.
Methods: We searched the Web of Science, PubMed, Scopus, and EBSCO Host on 22nd July 2020. We adapted our search strategy from a previously published systematic review on education for compassion and empathy. Selected studies were required to have used unique educational interventions for promoting empathy and compassion of medical students. The research questions were based on Participants (medical students), Intervention (empathy and/or compassion related teaching), Comparison, and Outcome.
Results: We analyzed 24 articles from the initial yield of 2,861. Twenty-two were quantitative studies with a mean of 12.8 on MERSQI. Twelve were randomized controlled trials while 5 measured outcomes with single group pre- and post-tests. There was no association found between duration, frequency and complexity of an educational intervention and its effectiveness. Twenty used multimodality curricula, and of those 18 reported statistically significant positive improvement in empathy, while 3 of 4 single modality were effective. Only three studies looked for long-term effects of educational interventions. Fourteen studies evaluated Kirkpatrick's level one (self-reported knowledge), 2 level three (behavior), and 6 level four (patient outcomes). We identified six major educational constructs of teaching empathy and compassion; communication, mindfulness, early clinical exposure, technology-enhanced learning, comics and arts and culture.
Discussion: Our review couldn't identify a standard teaching construct in place and highlighted that different teaching tools carry similar impact in promoting compassion and empathy and a sustainable program rather than a single training activity is essential.
Introduction
The quality of the interaction between physicians and patients influences patient outcomes in clinical settings (1, 2). A fundamental pillar of the healthcare mission is based upon compassionate care that forecasts greater patient trust and satisfaction, superior patient-physician connections, and better patient outcomes (2, 3). Within healthcare organizations, compassionate care entails diverse responsibilities of healthcare professionals in explaining their roles, establishing rapport, and in spending time on attentively listening to the patients' concerns (4). Compassionate healthcare—a key competency is characterized by reflections of others' concerns, respect for persons, and contextualized understanding of the patient as a key player of healthcare systems (5).
The two leading elements of patient centered care include empathy and compassion. Empathy refers to “a capacity to understand but without joining the feeling of the patient” (6) while compassion refers to “the feeling that arises in witnessing another's suffering and that motivates a subsequent desire to help” (7). In the medical field, empathy pertains to a multifaceted strand with moral, cognitive and behavioral enlightenment (8). When applied with objective reasoning, empathy promotes the impact of medical care and facilitates physician-patient communication (9). Empathy, being a multi-construct concept, includes, but not limited to, physician-patient interactions, interprofessional practice, self-compassion, empathy for others' pain, professional identity formation, stress awareness, and self-reflection and communication. Empathetic communication in patient-physicians interactions fosters information exchange and the impact of understanding and adherence to management plans, which lead to an early return to work, pain relief, mood elevation, and improved functional status of patients (10). Both empathy and compassion are generally considered to be interchangeable terms. However, empathy (understanding of patient feelings) is necessary to trigger compassion (emotional response including actions to alleviate patient sufferings) (11).
There is a compelling evidence in literature that treating patients without compassion can lead to deleterious outcomes (12). An absence of compassionate care results in poor quality of care and higher risk of complications through medical errors (13). Unfortunately, despite an explicit emphasis on the vital role of compassionate patient care, healthcare professionals often miss opportunities to be compassionate, rather they pay attention to biomedical data and management plans. From another perspective, sustaining compassion in medicine is hard as “compassion fatigue” prevails in ~20–70% of healthcare professionals (14). Compassion fatigue refers to loss of compassion in healthcare providers due to work related stress (15). Compassion fatigue certainly impairs the ability of healthcare providers in providing compassionate care which is a fundamental pillar inpatient-centered service (16). Educators have argued that a great majority of medical students enter health care with a strong set of espoused ideals for providing high-quality, patient-centered care (17). Unfortunately, during their training, medical students witness dissonance between the personal and professional conducts of their faculty and clinical teachers, students become more frustrated, less empathetic and more distanced from patients (18).
By and large, the ethos of most health care professional curricula uses typical biomedical models that primarily focus on teaching, training, and practice of clinical medicine with less emphasis on patients' psycho-social well-being (19). In the absence of a rigorous integration of biomedical knowledge with the understanding of human behaviors will potentially further detach medical and health sciences students and healthcare professionals from the patient's emotions and contextualized perspectives (20). Likewise, empathy plays a vital role in interprofessional practice where physicians from various disciplines work together toward the safe and effective patient-related clinical outcomes by shared decision-making and by regular consultations among healthcare teams and patients (21). This interprofessional practice alleviates patients' anxiety, stress, and uncertainty. From another perspective, self-awareness and self-regulation with empathy facilitates patient-doctor therapeutic interactions by evolving physicians' self-discovery (22). Among the practicing physicians, the phenomenon of self-discovery is an ingredient to professional identity formation (23). An empathetic professional identity formation is considered to be an effective tool for therapeutic actions in the healthcare system (24). In summary, empathy embodies a constellation of inter-related and interchangeable attributes that collectively lead to improved positive patient-related outcomes and the quality of care.
In clinical practice, a compassionate care has shown a strong association between improved clinical outcomes, quality of life and well-being (25). Among health professionals, empathetic, and compassionate care helps in mitigating the risk of burnouts (26). From the neuroscience perspective, a study on the functional magnetic resonance imaging has shown that empathy activates distinct pain centers of the brain; whereas focusing on compassion activates the reward pathways (27). These findings propound that a synchronous teaching and practice of empathy and compassion enhance patient and clinician well-being. Such outcomes may be accomplished with great success if educators can inculcate structured training programs for empathy and compassion in undergraduate and residency programs. However, there is a compelling evidence of empathy decline during the course of educational and training programs (28) and there is an urgent need for developing evidence-based curricula that can secure a sustained change in attitudes and behaviors (29).
A wealth of teaching pedagogies has been used to develop empathy, compassion and respect for patients in medical students (30–33) These include, but not limited to, patients' narratives and creative arts, drama workshops, communication skills, reflective writing, video-based learning and experiential learning (34–37). Lastly, the impact of role modeling and hidden curriculum in teaching compassion and empathy is well-established (38–40). There is little evidence about how the learning contexts, including the structure and delivery of medical curricula, influence the understanding of medical students about empathy and compassion (41). However, some patient-reported studies about compassion and empathy have shown the influence of educational interventions on medical students in enhancing their approach toward patients and their families (42).
The analysis of existing body of literature emphasizes a need to introduce a standard teaching modalities within medical curricula that can enrich traits of empathy and compassion in undergraduate medical students. Currently, there is scarce evidence of horizontal or vertical integration of teaching programs of empathy and compassion in undergraduate medical curricula (43, 44). Furthermore, there is little evidence about the effectiveness and quality of teaching programs for empathy and compassion. We conducted this systematic review of the literature to summarize and report the published work on educational interventions for empathy and/or compassion curricula in undergraduate medical students. This review also aims to highlight best practices to implement an evidence-based empathy and/or compassion curriculum in undergraduate medical training.
Materials and Methods
In our study, we used the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (45). The PRISMA tool provides an evidence-based minimum set of data for a standard reporting in systematic reviews and meta-analyses.
Research Objectives
Our research questions were based on Population, Intervention, Comparison, and Outcome (PICO) (46) as shown in Box 1.
Box 1. The checklist used for screening abstracts to determine the eligibility of studies for their full-text analysis.
Population
*Does this study look at medical students? YES/NO
If NO exclude
Intervention
Does this study use compassion/empathy/caring training? YES/NO
If NO exclude
Does this study train medical students to compassionate or empathetic strategies? YES/NO
If NO exclude
Does this study include information regarding the content of the compassion or empathy or caring training? YES/NO
If NO exclude
Comparison
Present? YES/NO
Absent? YES/NO
Outcome
Does this study include outcome measures related to the compassion/empathy/caring training? YES/NO
If NO exclude
Does this study isolate the outcomes for medical students? YES/NO
If NO exclude
We conducted this systematic review with two major objectives.
1. To describe and summarize the published literature about empathy and/or compassion curriculum in undergraduate medical education.
2. To summarize and highlight the best practices to implement an evidence-based empathy and/or compassion curriculum in undergraduate medical education.
Literature Search Strategy
We searched four major electronic databases of Web of Science, PubMed, Scopus and EBSCO Host for the English-language articles, published during 2015–2020. Our search strategy was adapted from a previously published systematic review on education for compassion and empathy (47, 48). We tweaked this work further to explicitly focus on medical students. The final search was performed on July 22nd, 2020 and a detailed search strategy is attached as Appendix 1. We looked into three core concepts and their associated Medical Subject Headings (MeSH) terms and keywords: Compassion and empathy, medical students, and educational interventions (Compassion OR Empathy OR Caring AND Medical students AND Education OR Training OR Workshop OR Simulation). A hand search of reference lists of the relevant articles yielded some more studies which were included in the final list of selected articles.
Data Collection, Eligibility Criteria, and Selection of Articles
We included original research studies that (i) carried out research on undergraduate medical students; and (ii) showed a clear educational intervention for empathy and/or compassion; and (iii) measured educational outcomes about compassion and/or empathy. These articles showed educational outcomes after training interventions to improve empathy (the understanding component) and compassion (i.e., the action component). The original studies included controlled trials, randomized controlled trials, pre- /post-test and post-test only designs. Review and editorial articles, commentaries, experts' opinion, short communications, and letter to the editor were excluded from our search. PM and SSG reviewed the titles and abstract independently and separately using PICO criteria. Any discrepancies were resolved by SG.
Data Extraction and Data Synthesis
Two researchers (PM and SSG) thoroughly scanned the full text of articles that met inclusion criteria and then using a standard data extraction form charted the required information. The researcher SG independently reviewed the entire process and filled gaps in data mining, data extraction and synthesis. We considered the following components during data extraction; types and designs of studies, primary objectives of studies, quality of studies, invitees' study level, response rate, self-reported or objective measurements in each study, and type, duration, frequency, skills taught and modality of educational interventions. We also recorded the outcomes according to the following four levels of the Kirkpatrick's model (49);
1. Self-reported changes in knowledge, skills, and attitude
2. Changes in knowledge
3. Changes in behavior
4. Patient-reported outcomes
We identified and classified the primary outcomes of the selected studies according to Kirkpatrick's level. A number of studies assessed multiple competencies such as empathy and compassion and self-compassion, and the highest-level outcome was considered as the primary outcome. While, in the studies where the primary outcomes did not relate to compassion or empathy, we used the highest-level empathy-specific variable as the primary outcome (Boxes 1, 2).
Box 2. The data mining rubric used in our study to record characteristics of each study (n = 24).
First Author
Title
Year of Publication
Country
Study Design
• Pre-post curriculum evaluation
• Randomized controlled trial
• Controlled trial
• Other
Population
• Number of students
• Year of students
Curriculum Hours
Number of sessions
Pedagogical approach
• Didactics
• Small group discussions
• Written/verbal reflections
• Simulation
• Standardized patient practice
• Apprenticeship/mentoring/service learning
• Video/Demonstration
• Other (Virtual hangouts, blogs, hot spotting etc.)
Compassion/empathy related Outcomes
• Self-reported changes in knowledge, skills, and attitudes
• Knowledge
• Behaviors
• Patient outcomes
Effectiveness of Educational Interventions
To identify best educational practices for teaching compassion and/or empathy, we determined the effectiveness of interventions in the selected studies, where effective was defined as a statistically significant improvement in primary educational outcomes as measured by p-value or effect size, where applicable. A p < 0.05 and an effect size >0.25 was considered significant. This rule was applicable only for quantitative studies with a control group design or a single group pre and post-test design.
Quality Assessment
We used Medical Education Research Study Quality Instrument (MERSQI), a tool designed for evaluation of quantitative educational research studies (50). The MERSQI checklist has 10 items in 6 domains: study design, sampling, type of data, validity evidence, data analysis, and type of outcomes with a maximum score of 3 in each domain. A study can have a maximum MERSQI score of 18 (highest quality). PM and SSG individually scored each study and in case of score discrepancies, SG assessed the scoring and discussed and made the final decision.
Quality Assurance
All researchers (PM, SSG and SG) objectively reviewed the workflow of selection of studies. In case of discrepancies, the researchers reached consensus by comparing the studies with inclusion criteria and key words. The discrepancies, inconsistencies and controversies were resolved with consensus until all the concerns were resolved.
Results
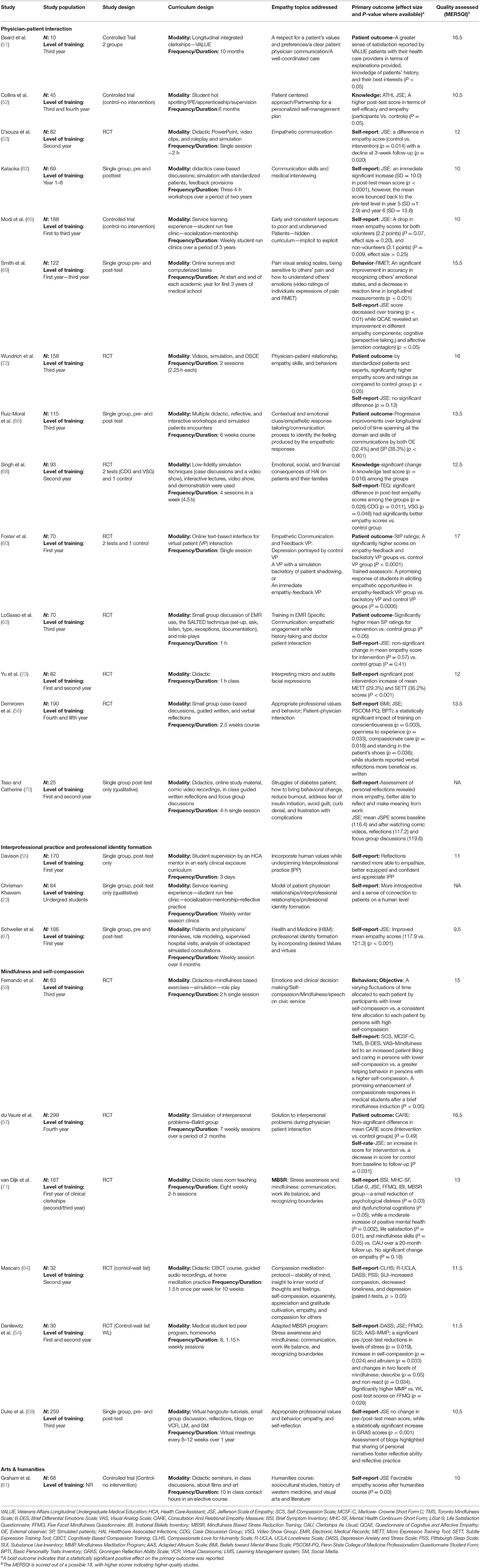
Figure 1 outlines the workflow and algorithm of studies selection in this study. Our initial search yielded 2,861 studies. After removing duplicates, we screened 754 titles and abstracts. This led to the identification of 244 articles using PICO for a detailed full-text review. This helped us to exclude another 227 articles whose content did not meet the inclusion criteria. We reviewed reference lists of the included articles to identify additional studies for potential inclusion, used electronic citation tracking, and consulted the librarian. This hand search yielded 15 review articles with 7 additional articles for inclusion. Finally, authors agreed on a list of 24 articles (23, 51–73), that had used 24 unique educational interventions either de novo, validated or adapted from previous publications and explicitly met inclusion criteria of our research. The summarized and comprehensive information about each article is presented in Table 1.
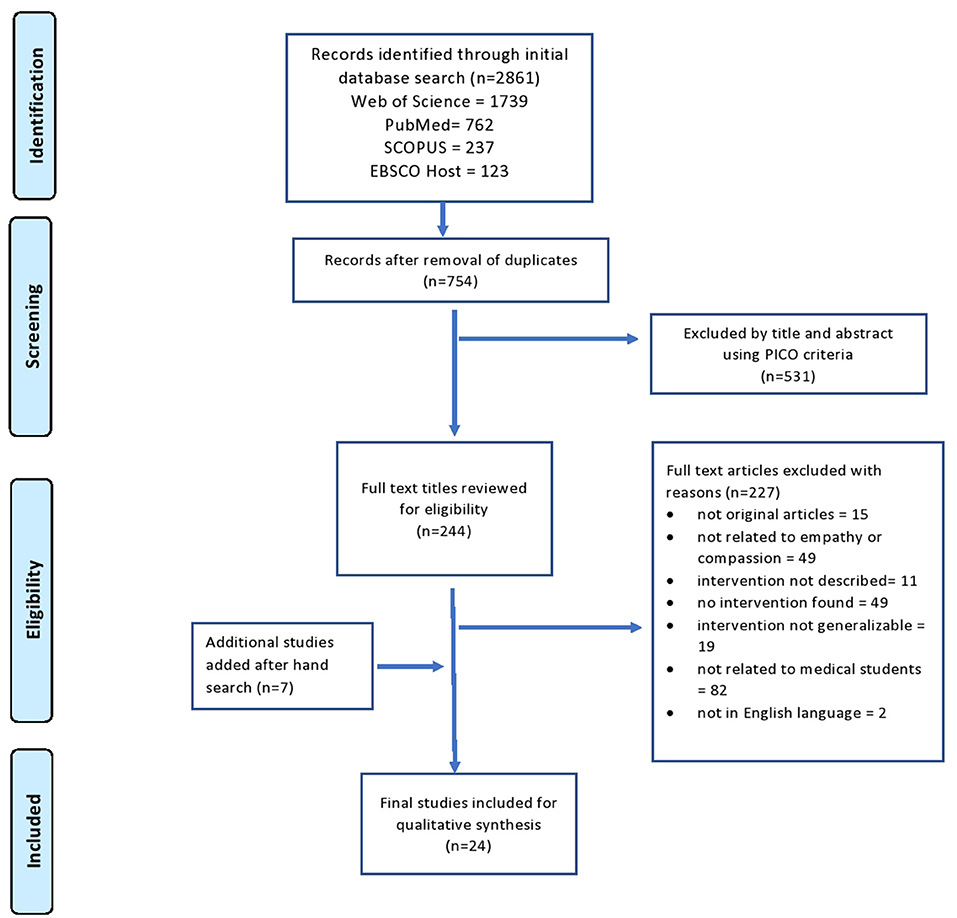
Figure 1. Flow diagram of the preferred reporting items for systematic reviews and meta-analysis (PRISMA) guidelines for the selection of articles in this study.
A maximum number of 9/24 (37.5%) articles were published in 2017, while 11/24 (45.8 %) studies originated from the USA. The sample size varied greatly across the selected studies, ranging from 10 to 299 participants. Our research included a total of 2,657 respondents with a mean of 110. Table 2 outlines the range of study designs that were used in the selected 24 studies. Most studies (21/24; 87.5%) were single-center, 11 (50%) were randomized controlled trials (54, 56, 57, 59, 60, 63, 64, 68, 71, 72), 4 (16.6%) controlled trials. (51, 52, 61, 65) Five (20.8%) studies measured outcomes with single group pre- and post-tests. (58, 62, 66, 67, 69) Our research identified 22/24 studies with their reported quantitative data that allowed us to calculate their MERSQI scores as shown in Table 3. All studies used statistical means to evaluate effectiveness. Collectively all studies have a total MERSQI score of 283 with a mean of 12.8. The study by Foster et al. (60) secured the highest MERSQI score of 17 from a maximum of 18. Finally, 10/22 (45.5%) studies scored ≥13 on MERSQI checklist.
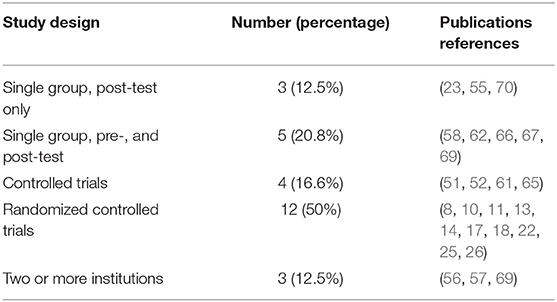
Table 2. The range of study designs used in the selected studies about empathy and compassion in medical students (n = 24).
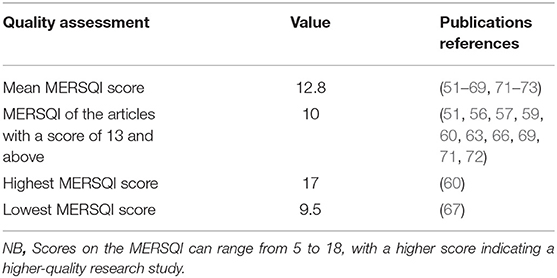
Table 3. The quality of the 22 quantitative studies as measured by the medical education research study quality instrument (MERSQI).
Most curricula (20/24, 83.3%) used multiple educational modalities and 90% of studies turned out to be effective in achieving their primary outcomes (Table 4). A variety of teaching modalities were employed; didactics (53, 59, 61, 62, 64, 66, 70, 71, 73), small-group discussions (56–58, 61, 63, 66–68), reflection exercises (23, 56, 58, 66, 70) and simulations. (53, 57, 59, 62, 66, 68, 72) Likewise, virtual hangouts and technology-enhanced interventions (52, 58, 60, 69) were also significantly effective. A great majority of studies were conducted in multiple sessions within one academic year.
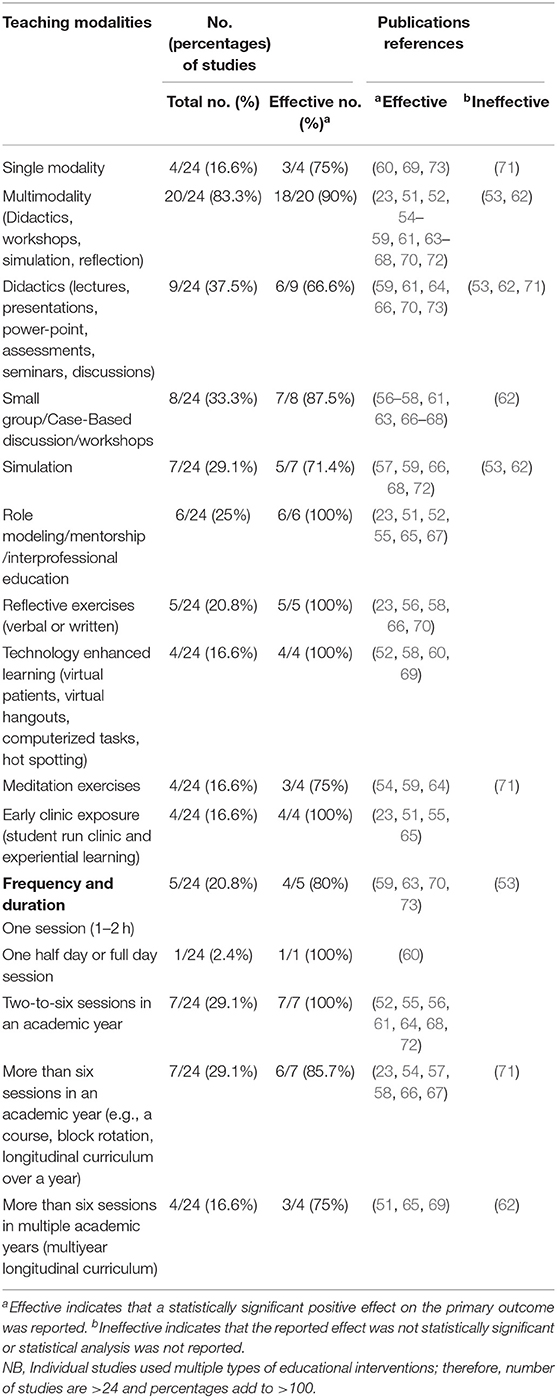
Table 4. Educational interventions with frequency and duration used in the selected studies (n = 24).
Only one study instituted the Balint training groups (57), while four studies (54, 59, 64, 71) used adapted mindfulness based curricular tools (75% effective ratio) developed by Kabat-Zinn (74). We did not observe any clear association between duration, frequency and complexity of an educational intervention and its effectiveness. For example, 75% (3/4) of single modality curricula were effective while multimodality curricula turned out to be effective in 90% (18/20) of the selected studies. Our data showed that single cross-sectional curricula (4/5) were as effective as longitudinal curricula (3/4) as shown in Table 4.
According to the four-level outcome-based Kirkpatrick model, 14/24 (58.3%) studies had a primary outcome pitching on level one; self-reported changes in attitudes and behavior (23, 53–56, 58, 61, 62, 64, 65, 67, 70, 71, 73). Two (4.8%) studies evaluated level three outcome (behavior), while six (25%) studies evaluated level four (patient outcomes) either by standardized or simulated patients or by a third party observation (51, 57, 60, 63, 66, 72). The leading constructs used in education interventions that showed positive impact on empathy and compassion of medical students in our study include communication skills, mindfulness, early clinical exposure, technology-enhanced learning, and humanities. A maximum of 10 studies used communication skills (53, 54, 56, 57, 60, 62, 63, 66, 71, 72), followed by mindfulness by 5 studies (54, 59, 64, 71), early clinical exposure by four (23, 51, 55, 65), technology-enhanced learning by virtual patient hangouts, computerized tasks, hot spotting by another four (52, 58, 60, 69), and comics (70), and arts and culture (61). Table 5 outlines an inventory of the validated instruments for outcome assessments used in the selected studies. The most commonly used self-assessment outcome tool was the Jefferson's Scale of Empathy by 15/24 (62.5%) studies (52–54, 56–58, 61–63, 65, 67, 69–72) that recruited 1,973 students. Conversely, 6/24 (25%) studies (54, 56, 59, 64, 69, 71) used a combination of tools to probe the impact of their interventions on behaviors and attitudes of medical students toward empathy and/or compassion and to determine the impact of self-compassion on behavior change. (59) Only three studies looked for the long-term effects of educational interventions (53, 62, 71).
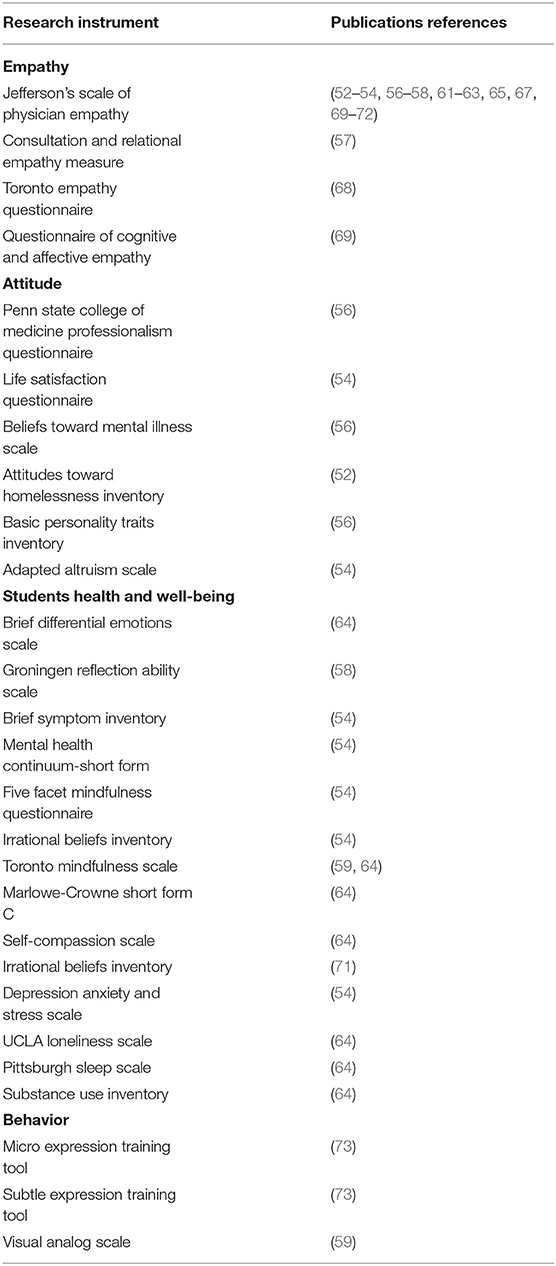
Table 5. An inventory of the validated instruments for outcome assessments used in the selected studies (n = 24).
Discussion
Our study elucidates major findings of 24 studies that have collected data from 2,657 medical students using educational interventions on empathy and compassion. Overall, there is a positive impact of teaching empathy and compassion on medical students using a wide range of teaching pedagogies. The body of evidence from our research has deduced that effective communication skills, mindfulness, early clinical experience, comics, arts and culture, and technology-enhanced learning by virtual patients, hangouts and hot spotting had a positive impact on empathy and compassion of medical students.
The overarching findings in our study underpin a need to teach empathy using the concepts of physician-patient interactions, interprofessional practice with professional identity formation, stress awareness, and self-reflection and communication. In our study, a substantial body of evidence has stressed on empathetic communication for better patient outcomes (51, 57, 60, 63, 66, 72). Communication is the foremost determinant of a safe clinical practice and ensures satisfaction of both patients and healthcare providers (75). The outright benefits of timely and professional communication in the medical field are far ranging; greater patient understanding and compliance, superior clinical outcomes, improved patient safety and alleviation of patient stress (76). Kelley and Kelley have argued that verbal communication between a healthcare professional and a patient enacts an empathetic connection to the patient that carries a powerful transformative and healing power (77). Pity, sympathy, fellow-feeling, comfort, commiseration, assuagement, and reflexive encouragement constitute effective strands of practicing empathy and compassion (78). The identification of compassionate opportunities, conformation, and appreciation with pursuit provide a practice of compassionate and empathetic care (79). In the study by Beard et al. the researchers measured patients' satisfaction about clear communication by medical students comparing the Veterans Affairs Longitudinal Undergraduate (VALUE) program with a control group of patients matched with disease severity (51). The results of this longitudinal study on students' involvement using VALUE program (patient education, communication, and collaboration) and a control group without the VALUE program. The VALUE students showed significant improvement in care coordination among their patients and physicians. Educators should provide regular and sustainable opportunities to medical students to develop and validate their interpersonal communication skills that can potentially improve empathetic communication. The study by du Vaure et al. (57) used the Consultation And Relational Empathy Measure (CARE) scale in a two-site randomized controlled trial on medical students in a weekly Balint group forum for 2 months. Results of this group were compared with the group of routine education. There was an insignificant difference in mean CARE score (Intervention vs. control groups) however an increase in Jefferson Scale of Empathy (JSE) score for intervention and decrease in score for control from baseline to follow-up was recorded. LoSasso et al. have studied the impact of SALTED (Set-up, Ask, Listen, Type, Exceptions, Documentation) technique and role-plays in a case controlled trial on medical students using little educational time of 1 h only (63). At the start and end of clerkships, both groups completed the JSE. While faculty and standardized patients examined and graded students' history-taking and communication skills as well as their empathic behaviors using the Jefferson Scale of Patient Perceptions of Physician Empathy (JSPPPE) at the end of clerkships. The mean scores of JSE of both groups increased from pre-test to post-test. Historically, the Balint groups have been used to facilitate physicians and students in promoting and sustaining their empathy skills (12) This analysis reflects how the patient-related outcomes can be improved by using a wide range of educational tools and techniques (VALUE, CARE, and SALTED) for incorporating, measuring, and enhancing empathy and compassion in medical students.
In our research, a great majority of studies have measured self-reported changes in knowledge and skills of participants and only two studies could tap into behavioral changes after an intervention (59, 69). Sustained training sessions are essential for achieving such paradigm change in behaviors. Although literature has shown some controlled trials on empathy, a precursor for compassion, but there is scarce information on compassion training of medical students or healthcare professionals (80). One such compassion enhancing training exercise is provided by mindfulness, “a continuous awareness of present moment experience in a calm and non-judgmental manner” (81). Mindfulness is a multi-factorial construct that contains a host of correlates such as healthy lifestyle, health education, wellness, empathy, compassion, good quality of life, regular exercise, sleep and hygiene, yoga, and guided imagery (82). Training for enhancement of mindfulness can potentially enhance compassionate care in clinical practice (83), close physician-patient relationship and can help alleviate physician burnout (84). Mindful meditation, attention to breathing, didactic learning, reflection, mindful walking, journalism, and sitting meditation are some of the most popular mindfulness training exercises that have shown to enhance empathy and compassion in medical students and healthcare workers (59). In the study by van Dijik et al. (71), the authors incorporated a stress reduction training curriculum based on mindfulness strategies to improve the mental health of medical students during clinical clerkships. This intervention led to an insignificant betterment of mental health of students which was followed up longitudinally over a 20 month period. However, the researchers could not detect a difference in JSE at 12 months in the studied cohort of students. Such findings necessitate the incorporation of a sustained empathy training program, particularly empathetic communication, for undergraduate medical students.
Technology-enhanced learning has gained popularity in several branches of medical education. Likewise, virtual patients (VPs) and standardized patients (StPs) are used as attractive alternatives to real patients with promising results (58). Unfortunately, research has shown an empathy decline in medical students', particularly in the third year of medical school (85). At this stage, medical students enter clinical clerkships that witness their encounters with patients and their relatives. A suitable ramification to sustain empathy and compassion is the use of VPs and StPs that can provide a constant source for medical students' experiential learning and behavioral development without endangering patient safety. Experiential learning such as patient shadowing or wellness programs can potentially enhance cognitive and behavioral dimensions of empathy. The long-lasting impact of experiential learning is further endorsed by a study conducted by Modi et al. which showed that volunteering students had better empathy than the non-volunteered medial students (65), who showed a decline in empathy over time.
The intelligent use of arts, culture, and humanities in medical education is an emerging and promising approach that can revitalize the declining empathy in medical students (70). Comics “the combined use of images and text, sequentially, to tell a story, where the images complement and/or enhance the text” (86) is a powerful means of portraying complexities of medical knowledge. Graphical illustration with juxtaposed texts, depicts stories in a tangible manner which help to amalgamate the pictorial and textual cues highlighting an innovative use of technology enhanced learning and comics. Our research has shown some evidence that comics may serve as a distinct tool to promote empathy in medical education (87). Finally, interprofessional education and practice carries great potential to promote empathy and compassion by alleviating anxiety, stress and burnout associated with medical education (21, 88).
Our results highlight the fact that the educational interventions pitched at improving the knowledge outcomes can be significantly effective, followed by behaviors and finally, patient outcomes. This is understandable for some reasons; medical students are attuned to work hard to acquire knowledge which can be easily measured as an educational outcome. Behavioral change in students and improvement in patient outcomes demand a sustained interplay of generic and acquired traits and, therefore, it's hard to achieve. Another interesting finding of our research springs from the fact that frequency, duration and teaching modalities didn't have any bearing on the effectiveness of the educational intervention. Even single session interventions were as effective as longitudinal curricula and such curricula did not have a sustained and long-lasting impact. However, experiential learning drills lead to emotional and behavioral remodeling that can result in durable personality developments.
Study Limitations
There are number of limitations of this review. The first relates to the comprehensiveness of the search and included articles. We searched four databases quite rigorously, but there remains a chance that certain pertinent studies are not captured by our search of databases, time and language restrictions. Second, though we aimed at highlighting the best practices in teaching empathy and/or compassion, this turned out to be difficult due to profound heterogeneity in the educational interventions and measurement tools used and the types of accomplished outcomes. Third, we planned to find a common curriculum for teaching and assessing empathy and compassion in medical education, its diverse and heterogeneous nature did not allow us to achieve our goal.
Conclusion
In our systematic review, the identified 24 studies evaluated the empathy and/or compassion curricula for undergraduate medical students. There was a great diversity of teaching pedagogies, curriculum design, and duration of teaching that did not let us secure a single best-evidence teaching modality for empathy and/or compassion. Keeping the multidimensional construct nature in mind, a blend of teaching pedagogies is needed. However, major educational constructs of communication, mindfulness, self-care, self-regulation, reflective practice, early clinical exposure, technology-enhanced learning, comics and arts and culture should be targeted for teaching empathy and compassion. We found that even short standalone curriculum was as effective as longitudinal curriculum. In order to mitigate the risk of decline of empathy and compassion, a sustainable program rather than a single training activity is essential.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author Contributions
PM and SSG contributed substantially to conceiving the idea, created, reviewed, and validated the search strategy, hand searched and screened the titles and abstract, extracted, analyzed and interpreted the data and came up with the initial draft of manuscript. Later SYG individually evaluated the search strategy, tweaked the data mining process, revised and improved the intellectual content of the initial draft. PM, SYG, and SSG agreed to take responsibility for the final draft. All authors contributed to the article and approved the submitted version.
Funding
This research was funded by the School of Postgraduate Studies and Research of the Royal College of Surgeons Ireland—Medical University Bahrain.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We are highly obliged to Dr. Bindhu Nair, AHIP Deputy and Research Support Librarian at RCSI-MUB for providing the technical support for library services.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2021.758377/full#supplementary-material
References
1. Lelorain S, Brédart A, Dolbeault S, Sultan S. A systematic review of the associations between empathy measures and patient outcomes in cancer care. Psycho Oncol. (2012) 21:1255–64. doi: 10.1002/pon.2115
2. Hojat M. Empathy and patient outcomes. In: Empathy in Health Professions Education and Patient Care. Springer (2016). p. 189–201. doi: 10.1007/978-3-319-27625-0_11
3. Duarte J, Pinto-Gouveia J. Empathy and feelings of guilt experienced by nurses: a cross-sectional study of their role in burnout and compassion fatigue symptoms. Appl Nurs Res. (2017) 35:42–7. doi: 10.1016/j.apnr.2017.02.006
4. Tehranineshat B, Rakhshan M, Torabizadeh C, Fararouei M. Compassionate care in healthcare systems: a systematic review. J Natl Med Assoc. (2019) 111:546–54. doi: 10.1016/j.jnma.2019.04.002
5. Sinclair S, McClement S, Raffin-Bouchal S, Hack TF, Hagen NA, McConnell S, et al. Compassion in health care: an empirical model. J Pain Sympt Manage. (2016) 51:193–203. doi: 10.1016/j.jpainsymman.2015.10.009
6. Hojat M, Gonnella JS, Mangione S, Nasca TJ, Magee M editors. Physician empathy in medical education and practice: experience with the jefferson scale of physician empathy. Semi Integrat Med. (2003) 1:25–41. doi: 10.1016/S1543-1150(03)00002-4
7. Goetz JL, Keltner D, Simon-Thomas E. Compassion: an evolutionary analysis and empirical review. Psychol Bull. (2010) 136:351–74. doi: 10.1037/a0018807
8. Williams J, Stickley T. Empathy and nurse education. Nurse Educ Today. (2010) 30:752–5. doi: 10.1016/j.nedt.2010.01.018
9. Sinclair S, Norris JM, McConnell SJ, Chochinov HM, Hack TF, Hagen NA, et al. Compassion: a scoping review of the healthcare literature. BMC Palliat Care. (2016) 15:6. doi: 10.1186/s12904-016-0080-0
10. Dasinger LK, Krause N, Thompson PJ, Brand RJ, Rudolph L. Doctor proactive communication, return-to-work recommendation, and duration of disability after a workers' compensation low back injury. J Occupat Environ Med. (2001) 43:515–25. doi: 10.1097/00043764-200106000-00001
11. Engelen E-M, Röttger-Rössler B. Current disciplinary and interdisciplinary debates on empathy. Emot Rev. (2012) 4:3–8. doi: 10.1177/1754073911422287
12. Wear D, Zarconi J. Can compassion be taught? Let's ask our students. J Gen Intern Med. (2008) 23:948–53. doi: 10.1007/s11606-007-0501-0
13. Neumann M, Bensing J, Mercer S, Ernstmann N, Ommen O, Pfaff H. Analyzing the “nature” and “specific effectiveness” of clinical empathy: a theoretical overview and contribution towards a theory-based research agenda. Pat Educ Couns. (2009) 74:339–46. doi: 10.1016/j.pec.2008.11.013
14. Markwell AL, Wainer Z. The health and wellbeing of junior doctors: insights from a national survey. Med J Austra. (2009) 191:441–4. doi: 10.5694/j.1326-5377.2009.tb02880.x
15. Sinclair S, Raffin-Bouchal S, Venturato L, Mijovic-Kondejewski J, Smith-MacDonald L. Compassion fatigue: a meta-narrative review of the healthcare literature. Int J Nurs Stud. (2017) 69:9–24. doi: 10.1016/j.ijnurstu.2017.01.003
16. Lee M, Laurenson M, Whitfield C. Can compassion be taught to lessen the effects of compassion fatigue? J Care Serv Manag. (2012) 6:121–30. doi: 10.1179/1750168713Y.0000000016
17. Shield RR, Tong I, Tomas M, Besdine RW. Teaching communication and compassionate care skills: an innovative curriculum for pre-clerkship medical students. Med Teach. (2011) 33:e408–16. doi: 10.3109/0142159X.2011.586748
19. Draper C, Louw G. What is medicine and what is a doctor? Medical students' perceptions and expectations of their academic and professional career. Med Teach. (2007) 29:e100–7. doi: 10.1080/01421590701481359
20. Díaz-Narváez VP, Alonso-Palacio LM, Caro SE, Silva M, Arboledacastillo J, Bilbao J, et al. Compassionate care“ component of the construct empathy in medical students in colombia and dominican republic. Acta Medica Cordoba. (2017) 33:101. doi: 10.19193/0393-6384_2017_1_018
21. Al-Qahtani MF, Guraya SY. Measuring the attitudes of healthcare faculty members towards interprofessional education in KSA. J Taibah Univer Med Sci. (2016) 11:586–93. doi: 10.1016/j.jtumed.2016.10.001
22. Ayed A, Malak MZ, Al-amer RM, Batran A, Salameh B. Effect of high fidelity simulation on perceptions of self-awareness, empathy, and patient-centered care among university pediatric nursing classes. Clin Simul Nurs. (2021) 56:84–90. doi: 10.1016/j.ecns.2021.04.005
23. Chrisman-Khawam LM, Manzi JA. Empathy in medicinecultivating an empathetic professional identity in osteopathic medical students through service learning: a qualitative analysis of reflective essays. J Osteop Med. (2020) 120:263–72. doi: 10.7556/jaoa.2020.043
24. Brazeau CM, Schroeder R, Rovi S, Boyd L. Relationships between medical student burnout, empathy, and professionalism climate. Acad Med. (2010) 85:S33–6. doi: 10.1097/ACM.0b013e3181ed4c47
25. Trzeciak S, Roberts BW, Mazzarelli AJ. Compassionomics: hypothesis and experimental approach. Med Hypotheses. (2017) 107:92–7. doi: 10.1016/j.mehy.2017.08.015
26. Thomas MR, Dyrbye LN, Huntington JL, Lawson KL, Novotny PJ, Sloan JA, et al. How do distress and well-being relate to medical student empathy? A multicenter study. J Gen Intern Med. (2007) 22:177–83. doi: 10.1007/s11606-006-0039-6
27. Lamm C, Decety J, Singer T. Meta-analytic evidence for common and distinct neural networks associated with directly experienced pain and empathy for pain. Neuroimage. (2011) 54:2492–502. doi: 10.1016/j.neuroimage.2010.10.014
28. Roff S. Reconsidering the “decline” of medical student empathy as reported in studies using the jefferson scale of physician empathy-student version (JSPE-S). Med Teach. (2015) 37:783–6. doi: 10.3109/0142159X.2015.1009022
29. Guraya SY, Norman RI, Roff S. Exploring the climates of undergraduate professionalism in a Saudi and a UK medical school. Med Teach. (2016) 38:630–2. doi: 10.3109/0142159X.2016.1150987
30. Holmgren L. Empathic communications and narrative competence in contemporary medical education. Enthymema. (2016) 90–104. doi: 10.13130/2037-2426/7662
31. de Leeuw S, Larstone R, Fell B, Cross N, Greenwood M, Auerbach K, et al. Educating medical students'“hearts and minds”: a humanities-informed cultural immersion program in indigenous experiential community learning. Int J Indigen Health. (2021) 16:87–107. doi: 10.32799/ijih.v16i1.33078
32. White CB, Perlman RL, Fantone JC, Kumagai AK. The interpretive project: a creative educational approach to fostering medical students' reflections and advancing humanistic medicine. Reflect Pract. (2010) 11:517–27. doi: 10.1080/14623943.2010.505718
33. Gorny-Wegrzyn E, Perry B. Nurse educators should use pedagogies of kindness and hope to teach nursing students' compassion. Arch Nurs Healthc. (2021) 1:1–2. doi: 10.46439/nursing.1.001
34. Dev V, Fernando AT, Consedine NS. Self-compassion as a stress moderator: a cross-sectional study of 1700 doctors, nurses, and medical students. Mindfulness. (2020) 9:1–12. doi: 10.1007/s12671-020-01325-6
35. Daryazadeh S, Adibi P, Yamani N, Mollabashi R. Impact of a narrative medicine program on reflective capacity and empathy of medical students in Iran. J Educ Eval Health Prof. (2020) 17:3. doi: 10.3352/jeehp.2020.17.3
36. Rajput V, Rosenberger R. Developing self-empathy in medical students and physicians to improve patient outcomes. MedEdPublish. (2017) 6:151. doi: 10.15694/mep.2017.000151
37. Markhamjr F, Westlake E, Desantis J. The effect of reflection rounds on Medical Students' Empathy. Med Res Arch. (2021) 9. doi: 10.18103/mra.v9i7.2506
38. Dulay MCB, Domingo JEA, Domingo KFR, Domondon HOF, Dumangon L, Duran R. An exploratory study of factors influencing student nurses' empathy. J Health Educ Res Dev. (2018) 6:2–7. doi: 10.4172/2380-5439.1000259
39. Khan R, Martimianakis MA. Empathy, burnout, and the hidden curriculum in medical training. In: Foster A, Yaseen Z, editors. Teaching Empathy in Healthcare. Cham: Springer (2019). doi: 10.1007/978-3-030-29876-0_15
40. L Holmes C, Miller H, Regehr G. (Almost) forgetting to care: an unanticipated source of empathy loss in clerkship. Med Educ. (2017) 51:732–9. doi: 10.1111/medu.13344
41. Ferreira-Valente A, Monteiro JS, Barbosa RM, Salgueira A, Costa P, Costa MJ. Clarifying changes in student empathy throughout medical school: a scoping review. Adv Health Sci Educ. (2017) 22:1293–313. doi: 10.1007/s10459-016-9704-7
42. Gholamzadeh S, Khastavaneh M, Khademian Z, Ghadakpour S. The effects of empathy skills training on nursing students' empathy and attitudes toward elderly people. BMC Med Educ. (2018) 18:196. doi: 10.1186/s12909-018-1297-9
43. Pedersen R. Empathy development in medical education–a critical review. Med Teach. (2010) 32:593–600. doi: 10.3109/01421590903544702
44. Chen DC, Kirshenbaum DS, Yan J, Kirshenbaum E, Aseltine RH. Characterizing changes in student empathy throughout medical school. Med Teach. (2012) 34:305–11. doi: 10.3109/0142159X.2012.644600
45. Guraya SY, Chen S. The impact and effectiveness of faculty development program in fostering the faculty's knowledge, skills, and professional competence: a systematic review and meta-analysis. Saudi J Biol Sci. (2019) 26:688–97. doi: 10.1016/j.sjbs.2017.10.024
46. Methley AM, Campbell S, Chew-Graham C, McNally R, Cheraghi-Sohi S. PICO, PICOS and SPIDER: a comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv Res. (2014) 14:579. doi: 10.1186/s12913-014-0579-0
47. Patel S, Pelletier-Bui A, Smith S, Roberts MB, Kilgannon HJ, Trzeciak S, et al. Curricula and methods for physician compassion training: protocol for a systematic review. BMJ Open. (2018) 8:e024320. doi: 10.1136/bmjopen-2018-024320
48. Patel S, Pelletier-Bui A, Smith S, Roberts MB, Kilgannon H, Trzeciak S, et al. Curricula for empathy and compassion training in medical education: a systematic review. PLoS ONE. (2019) 14:e0221412. doi: 10.1371/journal.pone.0221412
49. Smidt A, Balandin S, Sigafoos J, Reed VA. The kirkpatrick model: a useful tool for evaluating training outcomes. J Intellect Dev Disabil. (2009) 34:266–74. doi: 10.1080/13668250903093125
50. Reed DA, Cook DA, Beckman TJ, Levine RB, Kern DE, Wright SM. Association between funding and quality of published medical education research. JAMA. (2007) 298:1002–9. doi: 10.1001/jama.298.9.1002
51. Beard AS, Candy AE, Anderson TJ, Derrico NP, Ishani KA, Gravely AA, et al. Patient satisfaction with medical student participation in a longitudinal integrated clerkship: a controlled trial. Acad Med. (2020) 95:417–24. doi: 10.1097/ACM.0000000000003021
52. Collins L, Sicks S, Hass RW, Vause-Earland T, Ward J, Newsome C, et al. Self-efficacy and empathy development through interprofessional student hotspotting. J Interprof Care. (2020) 35:320–3. doi: 10.1080/13561820.2020.1712337
53. D'souza PC, Rasquinha SL, D'souza TL, Jain A, Kulkarni V, Pai K. Effect of a single-session communication skills training on empathy in medical students. Accad Psychiatry. (2019) 44:289–94. doi: 10.1007/s40596-019-01158-z
54. Danilewitz M, Bradwejn J, Koszycki D. A pilot feasibility study of a peer-led mindfulness program for medical students. Can Med Educ J. (2016) 7:e31. doi: 10.36834/cmej.36643
55. Davison E, Lindqvist S. Medical students working as health care assistants: an evaluation. Clin Teach. (2020) 17:382-8. doi: 10.1111/tct.13108
56. Demirören M, Saka MC, Senol Y, Sentürk V, Baysal Ö, Öztuna D. The impact of reflective practices on medical students' attitudes towards mental illness. Anatol J Psychiatry. (2016) 17:466–75. doi: 10.5455/apd.214188
57. du Vaure CB, Lemogne C, Bunge L, Catu-Pinault A, Hoertel N, Ghasarossian C, et al. Promoting empathy among medical students: a two-site randomized controlled study. J Psychosom Res. (2017) 103:102–7. doi: 10.1016/j.jpsychores.2017.10.008
58. Duke P, Grosseman S, Novack DH, Rosenzweig S. Preserving third year medical students' empathy and enhancing self-reflection using small group “virtual hangout” technology. Med Teach. (2015) 37:566–71. doi: 10.3109/0142159X.2014.956057
59. Fernando AT, Skinner K, Consedine NS. Increasing compassion in medical decision-making: can a brief mindfulness intervention help? Mindfulness. (2017) 8:276–85. doi: 10.1007/s12671-016-0598-5
60. Foster A, Chaudhary N, Kim T, Waller JL, Wong J, Borish M, et al. Using virtual patients to teach empathy: a randomized controlled study to enhance medical students' empathic communication. Simulat Healthc. (2016) 11:181–9. doi: 10.1097/SIH.0000000000000142
61. Graham J, Benson LM, Swanson J, Potyk D, Daratha K, Roberts K. Medical humanities coursework is associated with greater measured empathy in medical students. Am J Med. (2016) 129:1334–7. doi: 10.1016/j.amjmed.2016.08.005
62. Kataoka H, Iwase T, Ogawa H, Mahmood S, Sato M, DeSantis J, et al. Can communication skills training improve empathy? A six-year longitudinal study of medical students in Japan. Med Teach. (2019) 41:195–200. doi: 10.1080/0142159X.2018.1460657
63. LoSasso AA, Lamberton CE, Sammon M, Berg KT, Caruso JW, Cass J, et al. Enhancing student empathetic engagement, history-taking, and communication skills during electronic medical record use in patient care. Acad Med. (2017) 92:1022–7. doi: 10.1097/ACM.0000000000001476
64. Mascaro JS, Kelley S, Darcher A, Negi LT, Worthman C, Miller A, et al. Meditation buffers medical student compassion from the deleterious effects of depression. J Posit Psychol. (2018) 13:133–42. doi: 10.1080/17439760.2016.1233348
65. Modi A, Fascelli M, Daitch Z, Hojat M. Evaluating the relationship between participation in student-run free clinics and changes in empathy in medical students. J Prim Care Community Health. (2017) 8:122–6. doi: 10.1177/2150131916685199
66. Ruiz-Moral R, de Torres LP, Monge D, Leonardo CG, Caballero F. Teaching medical students to express empathy by exploring patient emotions and experiences in standardized medical encounters. Patient Educ Couns. (2017) 100:1694–700. doi: 10.1016/j.pec.2017.04.018
67. Schweller M, Ribeiro DL, Celeri EV, de Carvalho-Filho MA. Nurturing virtues of the medical profession: does it enhance medical students' empathy? Int J Med Educ. (2017) 8:262. doi: 10.5116/ijme.5951.6044
68. Singh SP, Modi CM, Patel CP, Pathak AG. Low-fidelity simulation to enhance understanding of infection control among undergraduate medical students. Natl Med J India. (2017) 30:215–8. doi: 10.4103/0970-258X.218677
69. Smith KE, Norman GJ, Decety J. The complexity of empathy during medical school training: evidence for positive changes. Med Educ. (2017) 51:1146–59. doi: 10.1111/medu.13398
70. Tsao P, Catherine HY. “There's no billing code for empathy”-animated comics remind medical students of empathy: a qualitative study. BMC Med Educ. (2016). 16:204. doi: 10.1186/s12909-016-0724-z
71. van Dijk I, Lucassen PL, Akkermans RP, Van Engelen BG, van Weel C, Speckens AE. Effects of mindfulness-based stress reduction on the mental health of clinical clerkship students: a cluster-randomized controlled trial. Acad Med. (2017) 92:1012–21. doi: 10.1097/ACM.0000000000001546
72. Wündrich M, Schwartz C, Feige B, Lemper D, Nissen C, Voderholzer U. Empathy training in medical students–a randomized controlled trial. Med Teach. (2017) 39:1096–8. doi: 10.1080/0142159X.2017.1355451
73. Yu EH, Choi EJ, Lee SY, Im SJ, Yune SJ, Baek SY. Effects of micro-and subtle-expression reading skill training in medical students: a randomized trial. Pat Educ Couns. (2016) 99:1670–5. doi: 10.1016/j.pec.2016.04.013
74. Kabat-Zinn J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary results. Gen Hosp Psychiatry. (1982) 4:33–47. doi: 10.1016/0163-8343(82)90026-3
75. Dean S, Zaslawski C, Roche M, Adams J. ”Talk to them": teaching communication skills to students of traditional chinese medicine. J Nurs Educ Pract. (2016) 6:49–56. doi: 10.5430/jnep.v6n12p49
76. Bensing J, Rimondini M, Visser A. What patients want. Pat Educ Couns. (2013) 90:287–90. doi: 10.1016/j.pec.2013.01.005
77. Kelley KJ, Kelley MF. Teaching empathy and other compassion-based communication skills. J Nurses Prof Dev. (2013) 29:321–4. doi: 10.1097/01.NND.0000436794.24434.90
78. Sinclair S, Beamer K, Hack TF, McClement S, Raffin Bouchal S, Chochinov HM, et al. Sympathy, empathy, and compassion: a grounded theory study of palliative care patients' understandings, experiences, and preferences. Palliat Med. (2017) 31:437–47. doi: 10.1177/0269216316663499
79. Babaei S, Taleghani F. Compassionate care challenges and barriers in clinical nurses: a qualitative study. Iran J Nurs Midwifery Res. (2019) 24:213–9. doi: 10.4103/ijnmr.IJNMR_100_18
80. Riess H, Kelley JM, Bailey RW, Dunn EJ, Phillips M. Empathy training for resident physicians: a randomized controlled trial of a neuroscience-informed curriculum. J Gen Intern Med. (2012) 27:1280–6. doi: 10.1007/s11606-012-2063-z
81. Fernando A, Consedine N, Hill AG. Mindfulness for surgeons. ANZ J Surg. (2014) 84:722–4. doi: 10.1111/ans.12695
82. Van der Riet P, Rossiter R, Kirby D, Dluzewska T, Harmon C. Piloting a stress management and mindfulness program for undergraduate nursing students: student feedback and lessons learned. Nurse Educ Today. (2015) 35:44–9. doi: 10.1016/j.nedt.2014.05.003
83. Weng HY, Fox AS, Shackman AJ, Stodola DE, Caldwell JZ, Olson MC, et al. Compassion training alters altruism and neural responses to suffering. Psychol Sci. (2013) 24:1171–80. doi: 10.1177/0956797612469537
84. Krasner MS, Epstein RM, Beckman H, Suchman AL, Chapman B, Mooney CJ, et al. Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA. (2009) 302:1284–93. doi: 10.1001/jama.2009.1384
85. Hojat M, Vergare MJ, Maxwell K, Brainard G, Herrine SK, Isenberg GA, et al. The devil is in the third year: a longitudinal study of erosion of empathy in medical school. Acad Med. (2009) 84:1182–91. doi: 10.1097/ACM.0b013e3181b17e55
86. Green MJ, Myers KR. Graphic medicine: use of comics in medical education and patient care. BMJ. (2010) 340:c863. doi: 10.1136/bmj.c863
87. Williams IC. Graphic medicine: comics as medical narrative. Med Humanit. (2012) 38:21–7. doi: 10.1136/medhum-2011-010093
Keywords: compassion, empathy, medical students, communication skills, mindfulness, technology-enhanced learning
Citation: Menezes P, Guraya SY and Guraya SS (2021) A Systematic Review of Educational Interventions and Their Impact on Empathy and Compassion of Undergraduate Medical Students. Front. Med. 8:758377. doi: 10.3389/fmed.2021.758377
Received: 13 August 2021; Accepted: 14 October 2021;
Published: 08 November 2021.
Edited by:
Orit Karnieli-Miller, Tel Aviv University, IsraelReviewed by:
Diantha Soemantri, University of Indonesia, IndonesiaJoana Duarte, Royal Holloway, University of London, United Kingdom
Copyright © 2021 Menezes, Guraya and Guraya. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shaista Salman Guraya, c3NhbG1hbkByY3NpLmNvbQ==
†ORCID: Salman Y. Guraya orcid.org/0000-0001-5183-023X
Shaista Salman Guraya orcid.org/0000-0003-2903-8697
 Prianna Menezes
Prianna Menezes Salman Y. Guraya
Salman Y. Guraya Shaista Salman Guraya
Shaista Salman Guraya