- 1Department of Rheumatology and Clinical Immunology, Chinese Academy of Medical Sciences and Peking Union Medical College, National Clinical Research Center for Dermatologic and Immunologic Diseases (NCRC-DID), Ministry of Science and Technology, State Key Laboratory of Complex Severe and Rare Diseases, Peking Union Medical College Hospital (PUMCH), Key Laboratory of Rheumatology and Clinical Immunology, Ministry of Education, Beijing, China
- 2CAS Key Laboratory of Mental Health, Institute of Psychology, Beijing, China
- 3University of Chinese Academy of Sciences, Beijing, China
- 4Department of Epidemiology and Biostatistics, School of Basic Medicine Peking Union Medical College, Institute of Basic Medical Sciences Chinese Academy of Medical Sciences, Beijing, China
- 5Department of International Education, The Experimental High School Attached to Beijing Normal University, Beijing, China
- 6Department of Rheumatology, The People’s Hospital of Xinjiang Autonomous, Urumqi, China
- 7Department of Rheumatology, First Affiliated Hospital of Guangxi Medical University, Nanning, China
- 8Department of Clinical Immunology and Rheumatology, Xijing Hospital Affiliated with The Fourth Military Medical University, Xi’an, China
- 9Department of Rheumatology, The Second Affiliated Hospital of Nanchang University, Nanchang, China
- 10Department of Rheumatology, First Affiliated Hospital of Kunming Medical University, Kunming, China
- 11Department of Rheumatology, Hainan Provincial People’s Hospital, Haikou, China
- 12Department of Rheumatology, Nanfang Hospital, Southern Medical University, Guangzhou, China
- 13Department of Rheumatology, First Affiliated Hospital of Zhengzhou University, Zhengzhou, China
- 14Department of Rheumatology, The First People’s Hospital of Yunnan Province, Kunming, China
Background: Systemic lupus erythematosus (SLE) can significantly influence patients’ quality of life and subjective well-being (SWB), but the relationships between clinical characteristics, SWB, and related psychological factors have been little studied.
Objective: To measure SWB in patients with SLE and examine how major clinical determinants, emotional variables, and related positive factors affect SWB.
Methods: Overall, 1,110 patients with SLE from the Chinese SLE Treatment and Research Group (CSTAR) and 198 age and gender-matched individuals from the general population without self-reported SLE were invited to complete questionnaires of SWB evaluated by the satisfaction with life scale (SWLS), emotional variables assessed by the patient health questionnaire-9 (PHQ-9), and general anxiety disorder-7 (GAD-7) and related positive factors assessed by the self-esteem scale (SES), general self-efficacy scale (GESE), and Connor-Davidson resilience scale (CD-RISC). The multivariate linear regression was used to examine the relationship between clinical manifestations and SWB.
Results: Life satisfaction was significantly lower (p < 0.001) in patients with SLE than in the general population. Active skin involvement (OR = 0.923, 95% CI = 0.868–0.981, p < 0.05) was negatively associated with life satisfaction scores, and age at enrollment (OR = 1.160, 95% CI = 1.092–1.230, p < 0.001) were positively associated with life satisfaction scores in the multivariate regression model. The cumulative organ damage was significantly associated with depression (OR = 1.085, 95% CI = 1.022–1.153, p < 0.01) and the loss of self-esteem (OR = 1.067, 95% CI = 1.004–1.133, p < 0.05).
Conclusion: SWB provides useful insight into the impact of SLE on psychological health and opportunities to improve quality of life and clinical care.
Introduction
Systemic lupus erythematosus (SLE) is a chronic, progressive, autoimmune disease with complex clinical presentations ranging from mild arthralgia and skin rash to multiple organ involvement (1). In recent decades, survival among patients with SLE has improved and the treatment focus has shifted toward improving health-related quality of life (HRQoL) and long-term morbidity (2). Some disease-specific HRQoL instruments including Lupus Patient-Reported Outcome (LupusPRO), Lupus Quality of Life (LupusQoL), and Systemic Lupus Erythematosus-Specific Quality of Life Questionnaire (SLEQOL) are widely administered in clinical practice and clinical studies to better capture symptoms or issues that are specific to SLE than generic instruments (3, 4). HRQOL and subjective symptoms, including anxiety, fatigue, low self-esteem, and cognitive impairment are central to perspectives of adults living with SLE and have been found to be associated with subsequently greater cumulative organ damage (5, 6). Recently, subjective well-being (SWB) has gained increasing attention for mental health-related evaluation and has been referred to as an indicator of psychological adjustment (7, 8).
Life satisfaction is one of the major components of SWB. Life satisfaction is defined as a cognitive judgment process of personal life evaluation and is generally measured by the satisfaction with life scale (SWLS) (9). Studies have suggested that life satisfaction correlates with HRQoL in patients with SLE (10). Furthermore, SWB is affected by emotional variables including depression and anxiety (11), and related positive factors, such as self-esteem, self-efficacy, and resilience (12). These emotional variables and related positive factors can perform a mediating role in the relationship between disease burden and SWB (13, 14). However, no previous study has examined the association between SWB and these psychological factors in patients with SLE.
Poor self-reported mental health and life dissatisfaction have been reported to be associated with increased mortality and serve as general health risk indicators (15). The experience of patients with SLE related to disease activity and organ damage may predict a worse HRQoL, especially in the components of mental health, physical capability, and planning (16). However, the influence of disease activity and accumulated damage on SWB is still unknown. In 2016, an international expert panel (the definition of Remission in SLE, DORIS project) proposed that remission or the lupus low disease activity state (LDAS) could be potential treating target for patients with SLE; but if such cannot be reached, the lupus low disease activity state (LDAS) could be another potential treat to target goal (17). Despite growing evidence that being in remission or LDAS is associated with a better HRQoL in SLE (16, 18), few studies have evaluated the relationship between remission/LDAS and psychological well-being. This study aimed to evaluate SWB and related psychological factors of patients with SLE and to study their main clinical determinants and the impact on life satisfaction as an indicator of SWB.
Materials and methods
Samples and procedures
A total of 1,110 patients with SLE were enrolled in the Chinese SLE Treatment and Research Group (CSTAR) online registry covering 21 rheumatologic clinical centers in 15 provinces in China from 8 March 2011 to 7 June 2019. All the patients fulfilled the Systemic Lupus International Collaborating Clinics (SLICC) (19) classification criteria for SLE and had at least two clinical visits. Data were collected through the CSTAR online registry, including demographic characteristics, clinical features, laboratory examinations, disease activity evaluated by the SLE disease activity index 2000 (SLEDAI-2K) (20), and systemic lupus international collaborating clinics/ACR damage index (SLICC/SDI) and treatments. The LLDAS was defined as follows: (1) SLEDAI-2K ≤ 4 with no scores for the renal, central nervous system, cardiopulmonary, vasculitis, fever, hemolytic anemia, or gastrointestinal activity; (2) No increase in any SLEDAI-2K component since the previous visit; (3) Physician global assessment (PGA) ≤ 1; and (4) stable immunosuppressants or biological immunomodulators and less than 7.5 mg/day prednisone (or equivalent) (21). The definition of remission is as follows: (1) clinical SLEDAI-2K = 0; (2) PGA < 0.5; (3) stable immunosuppressants or biological immunomodulators and less than 5 mg/day prednisone (or equivalent)(17). We recruited 198 age- and gender-matched controls through the Wenjuanxing platform among the general social group who self-declared that they were not suffering from SLE or other diseases.
Psychological measures
SWB was assessed by life satisfaction scores and related psychological factors including self-esteem, self-efficacy, resilience, depression, and anxiety. Life satisfaction was evaluated by the SWLS (9) containing five items rated on a 7-point Likert scale (1 = strongly disagree; 7 = strongly agree). Higher scores reflect higher life satisfaction. Emotional variables including depression and anxiety were assessed by the patient health questionnaire-9 (PHQ-9) and general anxiety disorder-7 (GAD-7) scales. Related positive factors, including self-esteem, self-efficacy, and resilience were assessed by the self-esteem scale (SES), general self-efficacy scale (GESE), and Connor-Davidson resilience scale (CD-RISC), respectively. The SES includes 10 items (e.g., “I feel that I am a person of worth, at least on an equal plane with others”) on a 4-point scale (22). Higher scores reflect lower self-esteem. The GESE is a widely internationally used scale containing 10 items, for example, “I am confident that I can deal with anything unexpected” (23). This scale has a scoring system ranging from 0 to 3. Higher scores reflect higher self-efficacy. Resilience was measured by the 25-item CD-RISC, which has been well validated in the Chinese population (24). This scale is a 5-point Likert scale (0 = not true at all, 4 = true nearly all of the time), with a higher score indicating greater resilience. The reliability of all psychological measurements used in our research has been validated among Chinese general population.
Statistical analysis
The Shapiro–Wilk test was used to test for a normal distribution of continuous variables. The continuous variables were summarized as the means and standard deviation (SD) if normally distributed, or as the median and interquartile range (IQR) if they had a skewed distribution. The t-tests and χ2-tests were conducted for univariate analysis. The Pearson and Spearman tests were used for linear correlation between psychological measures. A linear regression model was used for multivariate analysis, with SWB and related psychological factors as dependent variables and age, sex, LDAS, and the variables which were significantly associated within univariate analysis as independent variables. Statistical analyses were performed using R version 3.6 (R Core Team, Vienna, Austria) and SPSS 25.0 (IBM, Armonk, NY, USA).
Ethics statement
Informed consent was obtained from all participants. This study was approved by the Medical Ethics Committee of Peking Union Medical College Hospital, Chinese Academy of Medical Sciences.
Results
Participants’ clinical and psychological characteristics are shown in Table 1. A total of 1,062 (95.7%) were females and lupus duration at recruitment was 6.00 (IQR 2.00–10.00) years. The compliance with the Systemic Lupus International Collaborating Clinics (SLICC) 2012 classification criteria is shown in Supplementary Table 1. The SLEDAI indices were analyzed: musculoskeletal involvement (4.9%), renal involvement (11.7%), skin involvement (9.1%), etc. In total, 105 (9.5%) patients achieved remission, and 283 (25.5%) patients achieved LDAS. Additional data on treatments are shown in Supplementary Table 2. Life satisfaction was 21.13 ± 6.75 among patients with SLE and 23.76 ± 5.41 in the general population (p < 0.001). Depression of patients with SLE was 7.47 ± 5.31, in contrast to 5.20 ± 3.90 in the general population (p < 0.001). The SWB and related psychological factors questionnaires all demonstrated good reliability (Cronbach’s α = 0.857–0.931).
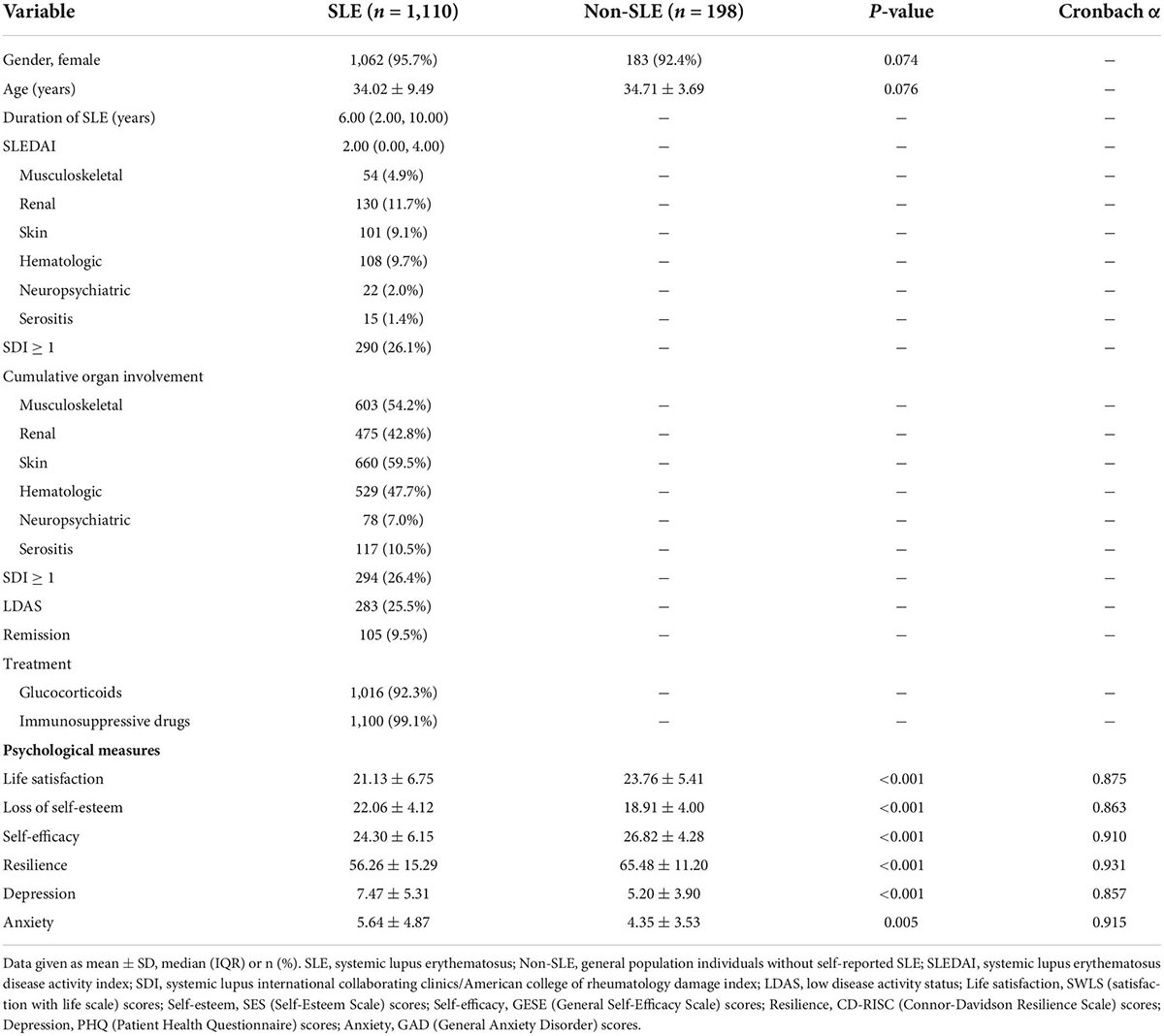
Table 1. Comparison of clinical and psychological characteristics of 1,110 patients with SLE and 198 individuals from the general population without self-reported SLE.
As shown in Figure 1, we observed significant correlations between the life satisfaction scores and the scores of all the related psychological factors (loss of self-esteem, depression, self-efficacy, anxiety, and resilience). Depression (r = −0.468, p < 0.001) and the loss of self-esteem (r = −0.544, p < 0.001) appeared to be negatively correlated with life satisfaction scores.
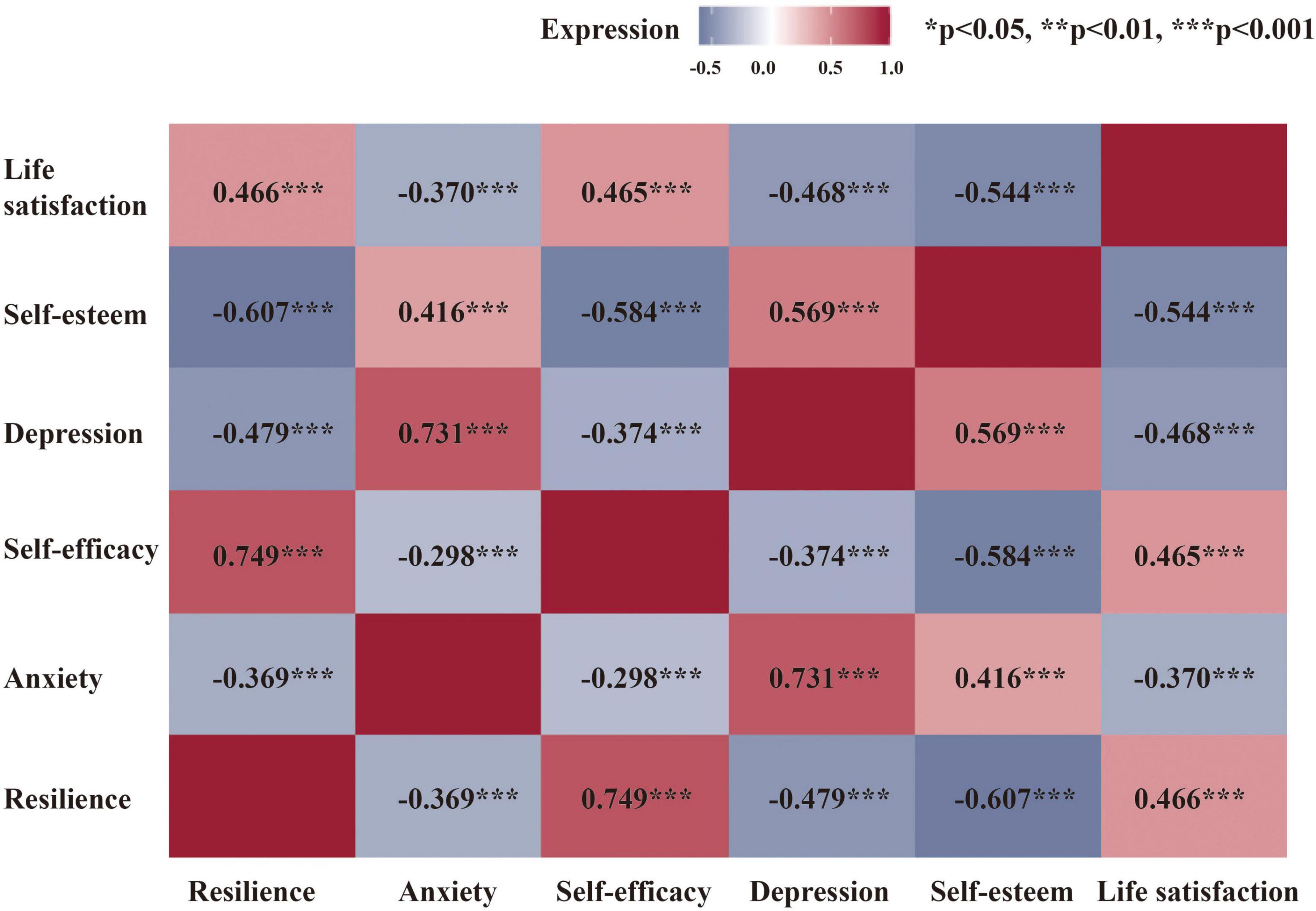
Figure 1. Correlation between subjective well-being and related psychological factors. For abbreviations, see the previous table.
The clinical determinants of SWB and related psychological factors in the multivariate linear regression model are depicted in Table 2. Active skin involvement (OR = 0.923, 95% CI = 0.868–0.981, p < 0.05) had negative predictive effects on life satisfaction scores. Otherwise, age at enrollment (OR = 1.160, 95% CI = 1.092–1.230, p < 0.001) had positive predictive effects on life satisfaction scores. Higher damage index predicted higher depression scores (OR = 1.085, 95% CI = 1.022–1.153, p < 0.01) and the loss of self-esteem (OR = 1.067, 95%CI = 1.004–1.133, p < 0.05). Moreover, age at enrollment was strong predictors of less self-esteem loss (OR = 0.914, 95% CI = 0.861–0.971, p < 0.01) and lower depression scores (OR = 0.922, 95% CI = 0.868–0.979, p < 0.01).
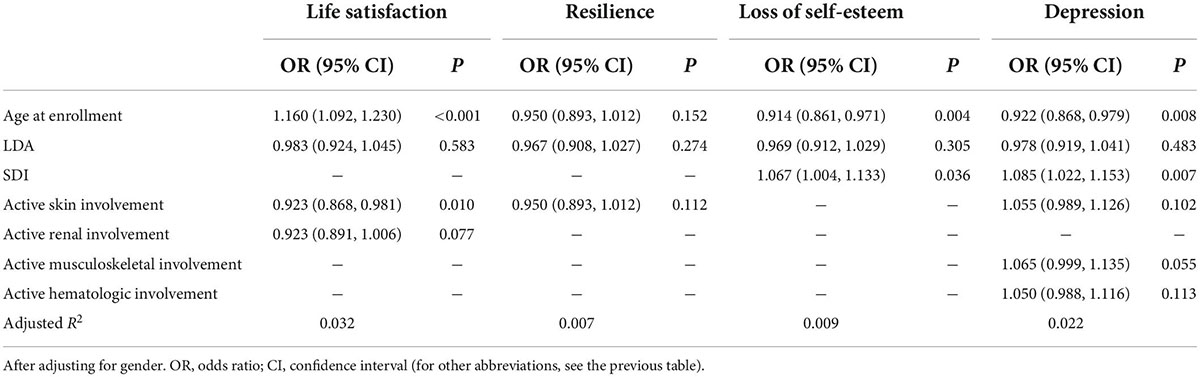
Table 2. Multivariate linear analysis of the major determinants of subjective well-being and related psychological factors.
Discussion
This is the first study reporting SWB and its related psychological factors among Chinese patients with SLE and identifying its relationship with active disease manifestations and damage index. Our results show that life satisfaction is significantly impaired in patients with SLE compared with the general population. Active skin involvement and age are significantly associated with life satisfaction in the linear regression model.
Low life satisfaction scores obtained by investigated patients, in a significant way, confirm how serious is the psychological problem in SLE. Similar life satisfaction results were presented in patients with cancer (7). Although many studies addressed the high prevalence of depression and anxiety in patients with SLE (25), little attention has been paid to the patient’s positive attitude which seems to be a crucial determinant of therapeutic adherence (26, 27). People may experience very low levels of SWB even in the absence of overt depression or anxiety. Moreover, SWB and related psychological factors contribute substantially to low HRQoL in patients with SLE (10, 28). Some disease-specific HRQoL instruments may also help recognize major mental health disorders promptly (29). However, the relationship between SWB and these disease-specific HRQoL in patients with SLE needs to be further evaluated. In routine care visits or mental health studies of patients with SLE, SWB should be considered as a supplementary assessment of health status to achieve a more holistic assessment of patients’ lives and optimize lupus care.
Skin injury is the second most common manifestation of patients with SLE after renal impairment (30). Patients with skin injury tend to have a higher risk for mental comorbidities and experience lower levels of happiness (31). The rashes and lesions on the skin of patients with SLE could cause severe physical changes in appearance. Individuals with body image concerns reported more psychosocial issues, including impaired psychosocial functioning (32). SWB in patients with skin diseases is found to be linked to better health outcomes, thus integrating SWB into the treatment of the diseases seems a promising approach (31, 33). Moreover, some scholars stated that emotional stress seems to upregulate inflammation and could aggravate some chronic inflammatory diseases (34). Although the most serious problems of SLE are often attributable to internal organ damage, patients with skin involvement deserve more attention in mental health evaluation and require a new type of treatment strategy integrating wellbeing improvement into the target.
Decades of psychological research revealed that external factors such as demographic characteristics including marital status, income, and educational level only had a modest impact on SWB (35). Thus, a lot of work has focused on the significant role of internal personality on SWB. Personality dispositions such as self-esteem were significantly associated with life satisfaction (36), which was consistent with our finding in SLE. Loss of self-esteem was reported to be prevalent in patients with SLE (6) and associated with greater cumulative organ damage (5). Physician-measured damage score is the focus in routine clinical practice as a poor prognostic sign and a predictor of mortality (37). Accumulated damage was associated with quality of life due to activity limitation in patients with SLE with skin and joint involvement (38). In our study, SDI was associated with depression and the loss of self-esteem. Thus, for patients with SLE with a greater physician-measured organ damage index, qualitative research can provide a comprehensive assessment of experiences and beliefs of SLE from the patient’s perspective. Moreover, psychotherapy (39) and some lupus self-management programs (40) have already been studied as interventions in clinical trials, which showed improvement in patients’ health outcomes. Therefore, future research should consider a combination of medication and psychological interventions as a whole, especially for patients with more organ damage.
In the wake of the principle of treating-to-target (T2T) in rheumatoid arthritis, remission and LDAS have been proposed as desirable therapeutic goals for patients with SLE (2, 21, 41). Emerging studies have demonstrated that the attainment of remission/LDAS was associated with improved outcomes in SLE, including lower damage accrual, lower probability of flares, and a better HRQoL (42). Regarding HRQoL, being on remission/LDAS was reported to predict higher scores in the components of physical health, but not in the components of mental health (16, 18, 42). The data from our study also indicated a lack of associations between remission/LDAS and SWB, probably because the mental domains are influenced by more complicated factors such as demographic characteristics, personality, and culture except for SLE-related factors involved in the definition of remission/LDAS at present. Thus, mental health evaluation and adjustment should be considered to incorporate into the treatment target of SLE. However, Heijke et al. reported that disease duration might affect patient-reported outcome measures (43). The results of the relationship between clinical determinants and SWB in patients with SLE duration of 1 year or less are shown in Supplementary Table 3. In patients with recent-onset SLE, LDAS appears to be associated with the related psychological factors of SWB. The interplay between remission/LDAS and patient-reported outcome measures might be influenced by SLE disease duration. This suggests that the mental health evaluation of patients with recent-onset SLE needs more attention.
The limitation of our study is the absence of quality-of-life assessments. The relationship between HRQoL and SWB in patients with SLE needs to be further evaluated. Second, many confounding factors such as socioeconomic status and education level may affect SWB, which could cause biases in our results. Third, patients with more active disease or specific active organ involvement should be considered in future research on the relationship between disease activity and SWB. Fourth, we recruited controls through the Wenjuanxing platform among the general population without self-reported SLE, which might have caused biases. Moreover, the effect of steroids, antimalarials, and immunosuppressants including the dosage and mode of administration on SWB warrant further investigation. SLE is quite heterogeneous, so including patients with different clinical manifestations in different percentages might cause more heterogeneity in the results when compared to the general population.
Conclusion
In conclusion, SLE is a multisystem disorder associated with poor SWB status. Active skin involvement and higher organ damage index are the major clinical determinants of SWB and its related psychological factors in patients with SLE. SWB may be a potential psychological outcome in clinical trials and should be considered when developing therapeutic targets for SLE management.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: The dataset used and/or analyzed during the current study are available from the corresponding author on reasonable request. Requests to access these datasets should be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of Peking Union Medical College Hospital. All participants gave informed consent to participate in the study before taking part. The patients/participants provided their written informed consent to participate in this study.
Author contributions
XL and QW were the guarantor and took responsibility for the integrity of the work. XL, QW, XT, and XZ conceived and designed the study. YS, DB, and YW performed the data analysis and drafted the manuscript. All authors critically revised the manuscript and approved the final manuscript, contributed to the acquisition, and interpretation of the data.
Funding
This work was supported by the Chinese National Key Technology R&D Program, Ministry of Science and Technology (2021YFC2501301-5 and 2017YFC0907601-3), Beijing Municipal Science and Technology Commission (No. Z201100005520022, 23, and 25–27), and CAMS Innovation Fund for Medical Sciences (CIFMS) (2021-I2M-1-005).
Acknowledgments
We thank all investigators, study coordinators, and patients for participating in the CSTAR cohort.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2022.984183/full#supplementary-material
References
1. Gurevitz S, Snyder J, Wessel E, Frey J, Williamson B. Systemic lupus erythematosus: a review of the disease and treatment options. Consult Pharm. (2013) 28:110–21.
2. Van Vollenhoven RF, Mosca M, Bertsias G, Kuhn A, Lerstrøm K, Aringer M, et al. Treat-to-target in systemic lupus erythematosus: recommendations from an international task force. Ann Rheum Dis. (2014) 73:958–67.
3. Yazdany J. Health-related quality of life measurement in adult systemic lupus erythematosus: lupus quality of life (LupusQoL), Systemic lupus erythematosus-specific quality of life questionnaire (SLEQOL), and systemic lupus erythematosus quality of life questionnaire (L-QoL). Arth Care Res. (2011) 63:S413–9. doi: 10.1002/acr.20636
4. Shi Y, Li M, Liu L, Wang Z, Wang Y, Zhao J, et al. Relationship between disease activity, organ damage and health-related quality of life in patients with systemic lupus erythematosus: a systemic review and meta-analysis. Autoimmun Rev. (2021) 20:102691. doi: 10.1016/j.autrev.2020.102691
5. Ward MM, Lotstein DS, Bush TM, Lambert RE, van Vollenhoven R, Neuwelt CM. Psychosocial correlates of morbidity in women with systemic lupus erythematosus. J Rheumatol. (1999) 26:2153–8.
6. Sutanto B, Singh-Grewal D, McNeil HP, O’Neill S, Craig JC, Jones J, et al. Experiences and perspectives of adults living with systemic lupus erythematosus: thematic synthesis of qualitative studies. Arth Care Res. (2013) 65:1752–65. doi: 10.1002/acr.22032
7. Lorenzo-Seva U, Calderon C, Ferrando PJ, Del Mar Muñoz M, Beato C, Ghanem I, et al. Psychometric properties and factorial analysis of invariance of the Satisfaction with life scale (SWLS) in cancer patients. Quality Res Int J Quality Life Aspects Treat Care Rehabili. (2019) 28:1255–64. doi: 10.1007/s11136-019-02106-y
8. Dolan P, Metcalfe R. Measuring subjective wellbeing: recommendations on measures for use by national governments. J Soc Policy. (2012) 41:409–27.
9. Diener E, Emmons RA, Larsem RJ, Griffin S. The satisfaction with life scale. J Personali Assess. (1985) 49:71–5. doi: 10.1207/s15327752jpa4901_13
10. Kulczycka L, Sysa-Jedrzejowska A, Robak E. Life satisfaction together with positive and negative aspects in polish patients with systemic lupus erythematosus. J Eur Acad Dermatol Venereol JEADV. (2009) 23:251–5. doi: 10.1111/j.1468-3083.2008.03044.x
11. Malone C, Wachholtz A. The relationship of anxiety and depression to subjective well-being in a mainland chinese sample. J Relig Health. (2018) 57:266–78. doi: 10.1007/s10943-017-0447-4
12. Hajek A, Konig HH. The role of optimism, self-esteem, and self-efficacy in moderating the relation between health comparisons and subjective well-being: results of a nationally representative longitudinal study among older adults. Br J Health Psychol. (2019) 24:547–70. doi: 10.1111/bjhp.12367
13. Cho I-K, Lee J, Kim K, Lee J, Lee S, Yoo S, et al. Schoolteachers’ resilience does but self-efficacy does not mediate the influence of stress and anxiety due to the COVID-19 pandemic on depression and subjective well-being. Front Psychiatry. (2021) 12:756195–756195. doi: 10.3389/fpsyt.2021.756195
14. Steca P, Greco A, Monzani D, Politi A, Gestra R, Ferrari G, et al. How does illness severity influence depression, health satisfaction and life satisfaction in patients with cardiovascular disease? The mediating role of illness perception and self-efficacy beliefs. Psychol Health. (2013) 28:765–83.
15. Koivumaa-Honkanen H, Honkanen R, Viinamäki H, Heikkilä K, Kaprio J, Koskenvuo M. Self-reported life satisfaction and 20-year mortality in healthy finnish adults. Am J Epidemiol. (2000) 152:983–91. doi: 10.1093/aje/152.10.983
16. Ugarte-Gil MF, Gamboa-Cardenas RV, Reategui-Sokolova C, Medina-Chinchón M, Zevallos F, Elera-Fitzcarrald C, et al. Low disease activity state/remission predicts a better health-related quality of life in systemic lupus erythematosus patients. Arthr Care Res. (2019) 72:1159–62. doi: 10.1002/acr.24009
17. van Vollenhoven R, Voskuyl A, Bertsias G, Aranow C, Aringer M, Arnaud L, et al. A framework for remission in SLE: consensus findings from a large international task force on definitions of remission in SLE (DORIS). Ann Rheum Dis. (2017) 76:554–61. doi: 10.1136/annrheumdis-2016-209519
18. Tsang AS, Bultink IEM, Heslinga M, van Tuyl LH, van Vollenhoven RF, Voskuyl AE. The relationship between remission and health-related quality of life in a cohort of SLE patients. Rheumatology. (2019) 58:628–35. doi: 10.1093/rheumatology/key349
19. Petri M, Orbai AM, Alarcón GS, Gordon C, Merrill JT, Fortin PR, et al. Derivation and validation of the Systemic Lupus International Collaborating Clinics classification criteria for systemic lupus erythematosus. Arthritis Rheum. (2012) 64:2677–86. doi: 10.1002/art.34473
20. Bombardier C, Gladman DD, Urowitz MB, Caron D, Chang CH. Derivation of the sledai. A disease activity index for lupus patients. Arthr Rheumat. (1992) 35:630–40.
21. Franklyn K, Lau CS, Navarra SV, Louthrenoo W, Lateef A, Hamijoyo L, et al. Definition and initial validation of a lupus low disease activity state (LLDAS). Ann Rheum Dis. (2016) 75:1615–21. doi: 10.1136/annrheumdis-2015-207726
22. Rosenberg M. Society and the Adolescent Self-Image. Princeton, NJ: Princeton university press (2015).
23. Schwarzer R. Optimistic self-beliefs: assessment of general perceived self-efficacy in thirteen cultures. World Psychol. (1997) 3:177–90.
24. Wu L, Tan Y, Liu Y. Factor structure and psychometric evaluation of the connor-davidson resilience scale in a new employee population of China. BMC Psychiatry. (2017) 17:49. doi: 10.1186/s12888-017-1219-0
25. Moustafa AT, Moazzami M, Engel L, Bangert E, Hassanein M, Marzouk S, et al. Prevalence and metric of depression and anxiety in systemic lupus erythematosus: a systematic review and meta-analysis. Semin Arthr Rheum. (2020) 50:84–94. doi: 10.1016/j.semarthrit.2019.06.017
26. Rodrigues JR, Faria DS, Neves JS, Neves JS, Peixoto D, Alcino S, et al. Positive affect as a predictor of adherence in patients with rheumatoid arthritis. Acta Reumatol Portug. (2019) 44:132–7.
27. Du X, Chen H, Zhuang Y, Zhao Q, Shen B. Medication adherence in Chinese patients with systemic lupus erythematosus. J Clin Rheumatol. (2020) 26:94–8. doi: 10.1097/rhu.0000000000000952
28. Jones JT, Cunningham N, Kashikar-Zuck S, Brunner HI. Pain, fatigue, and psychological impact on health-related quality of life in childhood-onset lupus. Arthr Care Res. (2016) 68:73–80. doi: 10.1002/acr.22650
29. Parperis K, Psarelis S, Chatzittofis A, Michaelides M, Nikiforou D, Antoniade E, et al. Association of clinical characteristics, disease activity and health-related quality of life in SLE patients with major depressive disorder. Rheumatology. (2021) 60:5369–78. doi: 10.1093/rheumatology/keab123
30. Deng GM, Tsokos GC. Pathogenesis and targeted treatment of skin injury in SLE. Nat Rev Rheumatol. (2015) 11:663–9. doi: 10.1038/nrrheum.2015.106
31. Schuster B, Ziehfreund S, Albrecht H. Happiness in dermatology: a holistic evaluation of the mental burden of skin diseases. J Eur Acad Dermatol Venereol JEADV. (2020) 34:1331–9. doi: 10.1111/jdv.16146
32. Monaghan SM, Sharpe L, Denton F, Levy J, Schrieber L, Sensky T. Relationship between appearance and psychological distress in rheumatic diseases. Arthr Rheum. (2007) 57:303–9. doi: 10.1002/art.22553
33. Jafferany M, Franca K. Psychodermatology: basics concepts. Acta Derm Venereol. (2016) 96:35–7. doi: 10.2340/00015555-2378
34. DeWeerdt S. Psychodermatology: an emotional response. Nature. (2012) 492:S62–3. doi: 10.1038/492S62a
35. Diener E, Oishi S, Lucas RE. Personality, culture, and subjective well-being: emotional and cognitive evaluations of life. Annu Rev Psychol. (2003) 54:403–25. doi: 10.1146/annurev.psych.54.101601.145056
36. Diener E, Diener M. Cross-cultural correlates of life satisfaction and self-esteem. J Pers Soc Psychol. (1995) 68:653–63. doi: 10.1037//0022-3514.68.4.653
37. Romero-Diaz J, Isenberg D, Ramsey-Goldman R. Measures of adult systemic lupus erythematosus: updated version of british isles lupus assessment group (BILAG 2004), european consensus lupus activity measurements (ECLAM), systemic lupus activity measure, revised (SLAM-R), systemic lupus activity questionnaire for population studies (SLAQ), systemic lupus erythematosus disease activity index 2000 (SLEDAI-2K), and systemic lupus international collaborating clinics/american college of rheumatology damage index (SDI). Arthr Care Res. (2011) 63:S37–46. doi: 10.1002/acr.20572
38. Björk M, Dahlström Ö, Wetterö J, Sjöwall C. Quality of life and acquired organ damage are intimately related to activity limitations in patients with systemic lupus erythematosus. BMC Muscul Dis. (2015) 16:188. doi: 10.1186/s12891-015-0621-3
39. Conceicao CTM, Meinao IM, Bombana JA, Sato EI. Psychoanalytic psychotherapy improves quality of life, depression, anxiety and coping in patients with systemic lupus erythematosus: a controlled randomized clinical trial. Adv Rheumatol. (2019) 59:4. doi: 10.1186/s42358-019-0047-y
40. Williams EM, Dismuke CL, Faith TD, Smalls BL, Brown E, Oates JC, et al. Cost-effectiveness of a peer mentoring intervention to improve disease self-management practices and self-efficacy among African American women with systemic lupus erythematosus: analysis of the peer approaches to lupus self-management (PALS) pilot study. Lupus. (2019) 28:937–44. doi: 10.1177/0961203319851559
41. Gatto M, Zen M, Iaccarino L, Doria A. New therapeutic strategies in systemic lupus erythematosus management. Nat Rev Rheumatol. (2019) 15:30–48. doi: 10.1038/s41584-018-0133-2
42. Ugarte-Gil MF, Mendoza-Pinto C, Reátegui-Sokolova C, Pons-Estel GJ, van Vollenhoven RF, Bertsias G, et al. Achieving remission or low disease activity is associated with better outcomes in patients with systemic lupus erythematosus: a systematic literature review. Lupus Sci Med. (2021) 8:e000542. doi: 10.1136/lupus-2021-000542
Keywords: systemic lupus erythematosus, subjective well-being, life satisfaction, skin involvement, organ damage, quality of life
Citation: Shi Y, Bi D, Wang Y, Li R, Wu L, Zhao C, Wu Z, Duan X, Xu J, Zhan F, Yang M, Liu S, Li Q, Zhang S, Liu L, Zhao J, Tian X, Li X, Wang Q and Zeng X (2022) Chinese SLE Treatment and Research Group Registry (CSTAR) XIV: the subjective well-being of patients with systemic lupus erythematosus. Front. Med. 9:984183. doi: 10.3389/fmed.2022.984183
Received: 01 July 2022; Accepted: 25 August 2022;
Published: 20 September 2022.
Edited by:
Chris Wincup, King’s College Hospital NHS Foundation Trust, United KingdomReviewed by:
Christopher Sjöwall, Linköping University, SwedenMassimo Radin, University of Turin, Italy
Filipa Farinha, University College London, United Kingdom
Copyright © 2022 Shi, Bi, Wang, Li, Wu, Zhao, Wu, Duan, Xu, Zhan, Yang, Liu, Li, Zhang, Liu, Zhao, Tian, Li, Wang and Zeng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xinying Li, bGl4eUBwc3ljaC5hYy5jbg==; Qian Wang, d2FuZ3FpYW5fcHVtY2hAMTI2LmNvbQ==
†These authors have contributed equally to this work
 Yue Shi
Yue Shi Dandan Bi2,3†
Dandan Bi2,3† Yanhong Wang
Yanhong Wang Lijun Wu
Lijun Wu Min Yang
Min Yang Shuo Zhang
Shuo Zhang Lingshan Liu
Lingshan Liu Jiuliang Zhao
Jiuliang Zhao Xinping Tian
Xinping Tian Xinying Li
Xinying Li Qian Wang
Qian Wang Xiaofeng Zeng
Xiaofeng Zeng