- 1Healthcare Professions Department, Fondazione IRCCS Ca' Granda Ospedale Maggiore Policlinico, Milan, Italy
- 2Thoracic Surgery and Lung Transplant Unit, Fondazione IRCCS Ca' Granda Ospedale Maggiore Policlinico, Milan, Italy
- 3Internal Medicine Department, Respiratory Unit and Adult Cystic Fibrosis Center, Fondazione IRCCS Ca' Granda Ospedale Maggiore Policlinico, Milan, Italy
- 4Respiratory Physiotherapy Equipe, ASST Grande Ospedale Metropolitano Niguarda, Milan, Italy
- 5Intensive Care Respiratory Physiotherapy, Rehabilitation and Functional Education, San Martino Policlinico Hospital, IRCCS for Oncology and Neurosciences, Genoa, Italy
- 6Rehabilitation Department, Santa Chiara Hospital, APSS di Trento, Trento, Italy
- 7Anesthesia and Intensive Care, San Martino Policlinico Hospital, IRCCS for Oncology and Neurosciences, Genoa, Italy
- 8Department of Medicine, University of Barcelona, Barcelona, Spain
- 9Department of Anaesthesiology, Intensive Care and Emergency, Fondazione IRCCS Ca' Granda Ospedale Maggiore Policlinico, Milan, Italy
- 10Department of Anesthesia and Intensive Care Medicine, ASST Grande Ospedale Metropolitano Niguarda, Milan, Italy
- 11Department of Surgical Sciences and Integrated Diagnostics, University of Genoa, Genoa, Italy
- 12Department of Pathophysiology and Transplantation, University of Milan, Milan, Italy
Background: Respiratory physiotherapy is reported as safe and feasible in mechanically ventilated patients with severe Coronavirus Disease (COVID-19) admitted to Intensive Care Unit (ICU), but the short-term benefits remain unclear.
Methods: We performed a retrospective observational study in four ICUs in Northern Italy. All patients with COVID-19 admitted to ICU and under invasive mechanical ventilation (MV) between March 1st and May 30th, 2020, were enrolled into the study. Overlap weighting based on the propensity score was used to adjust for confounding in the comparison of patients who had or had not been treated by physiotherapists. The primary outcome was the number of days alive and ventilator-free (VFDs). The secondary outcomes were arterial partial pressure of oxygen (PaO2)/fraction of inspired oxygen (FiO2) ratio (P/F) at ICU discharge, ICU length of stay, ICU and hospital mortality, and survival at 90 days. The trial protocol was registered on clinicaltrials.gov (NCT 05067907).
Results: A total of 317 patients were included in the analysis. The median VFDs was 18 days [interquartile range (IQR) 10; 24] in patients performing physiotherapy and 21 days (IQR 0; 26) in the group without physiotherapy [incidence rate ratio (IRR) 0.86, 95% confidence interval (CI): 0.78; 0.95]. The chance of 0 VFDs was lower for patients treated by physiotherapists compared to those who were not [odds ratio (OR) = 0.36, 95% CI: 0.18–0.71]. Survival at 90 days was 96.0% in the physiotherapy group and 70.6% in patients not performing physiotherapy [hazard ratio (HR) = 0.14, 95% CI: 0.03–0.71]. Number of VFDs was not associated with body mass index (BMI), sex, or P/F at ICU admission for individuals with at least 1 day off the ventilator.
Conclusion: In patients with COVID-19 admitted to ICU during the first pandemic wave and treated by physiotherapists, the number of days alive and free from MV was lower compared to patients who did not perform respiratory physiotherapy. Survival at 90 days in the physiotherapy group was greater compared to no physiotherapy. These findings may be the starting point for further investigation in this setting.
Introduction
Early physical and occupational therapy is safe and well-tolerated in mechanically ventilated critically ill patients, and results in better functional outcomes at hospital discharge (1). Early mobilization in the Intensive Care Unit (ICU) was shown to decrease the duration of mechanical ventilation (MV) and shortening the length of ICU stay (2). In patients with acute respiratory distress syndrome (ARDS), early rehabilitation is associated with a reduction of the functional impairment due to the prolonged duration of ventilatory support and ICU stay (3). However, conflicting results were reported on the impact of active mobilization and rehabilitation in ICU on survival (4).
Physiotherapy and rehabilitation interventions have been recommended to minimize the functional sequelae of Coronavirus Disease (COVID-19) in mechanically ventilated patients admitted to ICU (5–8). Notably, critically ill patients with COVID-19 associated ARDS (CARDS) may require longer rehabilitation time than patients with non-COVID ARDS (9, 10). Respiratory physiotherapy combines early mobilization and other techniques optimizing secretion clearance, gas exchange, lung recruitment, and aiding with weaning from MV. Recent evidence suggests that respiratory physiotherapy in mechanically ventilated patients with CARDS is safe and feasible, although the benefits of early rehabilitation in these patients remain unclear (11, 12).
The aim of the present study was to assess whether the number of ventilator-free days (VFDs) and alive at day 28 was different in mechanically ventilated patients with severe COVID-19 and admitted to ICU, who performed or not respiratory physiotherapy.
Methods
Study design
We planned a retrospective, pragmatic, observational study of consecutive mechanically ventilated patients with COVID-19 admitted to the ICU of four Italian referral centers. A pragmatic design allowed for relaxed inclusion criteria thus contributing to our understanding of the real-life implementation of respiratory physiotherapy in ICU (13). The study was approved by the Ethics Committee of the Fondazione IRCCS Ca' Granda Ospedale Maggiore Policlinico (Comitato Etico Milano Area 2, approval n. 966_2020bis) and subsequently by the local Ethics Committees of the participating sites. Informed consent was waived due to the retrospective nature of the study. Baseline characteristics, comorbidities, pharmacological therapies, and clinical outcomes of all patients were extracted from electronic health records, collected, and managed using an electronic database (REDCap) (14) hosted at the coordinating center in Milano. The trial protocol and outcomes measures were published before study initiation (NCT 05067907). This observational study is presented in accordance with the STROBE guidelines (15).
Study population
Patients admitted to an ICU from March 1st, 2020 to May 30th, 2020 at four centers [Fondazione IRCCS Ca' Granda Ospedale Maggiore Policlinico (Milano), ASST Grande Ospedale Metropolitano Niguarda (Milano), Ospedale Policlinico San Martino (Genova), and APSS Provincia Autonoma di Trento Ospedale Santa Chiara (Trento)] were included in the study. Centers were selected among the hospitals of the northern regions of Italy, which were mainly hit by the first pandemic wave, according to the following criteria: (1) the presence of a dedicated COVID-19 ICU; and (2) an established physiotherapy team with experience in the cardio-respiratory field and in the care of critically ill patients. Patients were eligible once neuromuscular blocking agents (NMBAs) were withdrawn. At this time, each ICU team could assign patients to respiratory physiotherapy pragmatically, consistent with the clinical practice of each ICU team (16). Thus, it was possible to evaluate a control group of patients who did not receive physiotherapy. We analyzed patients aged ≥18 and <80 years, with a confirmed severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, who developed ARDS (17) and required invasive MV. Previous cognitive impairment (i.e., mini-mental state examination <20) was considered an exclusion criterion.
Standard of care procedures
All the clinical interventions, such as use of antibiotics, ventilatory strategy, laboratory testing, and hemodynamic management were left at the discretion of each ICU team and in accordance with the most updated guidelines at the time of the study (18).
Respiratory physiotherapy intervention
In Italy, physiotherapists oversee both musculoskeletal and respiratory rehabilitation. Each study center was encouraged to follow the best practice guidelines (19–21) and their institutional protocols for the care of individuals with COVID-19. Respiratory physiotherapy treatments were administered 7 days per week. Interventions included early mobilization and respiratory care, as previously described (11, 12). All patients that received respiratory physiotherapy treatments were assessed by physiotherapists once free from NMBAs. The respiratory physiotherapy protocol included different levels of activities; when patients were partially sedated, intubated, and mechanically ventilated, the treatment mainly focused on respiratory and peripheral muscles training, reaching, and maintaining lateral, sitting, and vertical positions, passive and active mobilization in bed and activity of daily life (ADL) training to promote independence and bed mobility (1). If necessary, modification of MV settings during mobilization/exercise were adopted according to the respiratory need of the patient. Moreover, airway clearance strategies were proposed as well as lung expansion techniques (i.e., deep breathing exercises) (22). When patients were completely awake and started weaning from MV, physiotherapists assessed their ability to perform bed mobility activities and to reach and maintain sitting and vertical position while receiving minimal or no ventilator support. In this phase, physiotherapists assisted MV weaning, eventually supporting patient with non-invasive ventilation after extubation. Active and strengthening exercises, ADL training, and endurance training were performed. In patients with tracheostomy, physiotherapists evaluated cough efficacy, swallowing, and humidification need and the treatment included spontaneous breathing trials, tracheal suctioning as well as promoting early speech recovery.
Outcomes
The primary outcome was VFDs, defined as the number of days alive and ventilator-free for at least 24 consecutive hours, and calculated as follows: VFDs = 0 if patients died within 28 days or if patients were still ventilated within or after 28 days; VFDs = 28 – x if patients were liberated from ventilation x days after withdrawal of NMBAs. Pre-specified secondary outcomes were the following: ICU length of stay, arterial partial pressure of oxygen (PaO2)/fraction of inspired oxygen (FiO2) (P/F) ratio at ICU discharge, ICU and hospital survival, and survival at 90-days after NMBAs withdrawal.
Statistical analysis
Due to overwhelming workload during the pandemic, the original sample size of 340 patients based on a difference of two VFDs between groups decreased to 244 (two-sided alpha level of 0.01 and power 90%) because one center declined to participate after protocol approval. All descriptive statistics were reported as counts (percentage), median [interquartile range (IQR)], or mean [Standard Deviation (SD)]. Data analysis was conducted following recommended methodological standards (23, 24). To estimate an association between VFDs and respiratory physiotherapy that is unbiased by pretreatment group differences on other observed variables, we included the following covariates in a propensity score from a multivariable logistic regression model of respiratory physiotherapy: age, body mass index (BMI), hospital center, sex, number of days under NMBAs, occurrence of reintubation and pronation, and presence of tracheostomy. In the propensity score calculation, variables associated with the intervention and outcome were chosen for inclusion according to Brookhart et al. (25). The overlap propensity score weighting (OPSW) method was then applied, in which each patient's weight is the probability of that patient being assigned to the opposite intervention group (26). The OPSW mimics the characteristics of highly inclusive trial, and it is proven to optimize precision of the estimates (27). Balance was demonstrated by reporting the standardized difference in means (or percentage) between the group that received physiotherapy intervention and the group that did not receive physiotherapy intervention. A zero-inflated negative binomial model (ZINB) (28) was used to estimate the association of respiratory physiotherapy with the primary outcome, combining a negative binomial and a logit model. The effect size was estimated as incidence rate ratio (IRR) and odds ratio (OR), respectively, with their 95% confidence interval (CI), obtained using robust standard errors. The count part of the model (i.e., the negative binomial) was adjusted with age, BMI, sex, and P/F ratio at ICU admission whereas the inflation part (i.e., the logit model) used presence of tracheostomy and exposure to pronation as adjusting covariates. We further adjusted the count component with hospital centers interacting with physiotherapy. To estimate secondary outcomes, mean difference was used to describe P/F ratio at ICU discharge between groups. We used adjusted Cox proportional hazard regression models for survival endpoints: to increase statistical efficiency, analyses were further adjusted for age, sex, and P/F ratio at ICU admission, with physiotherapy interacting with hospital center strata; hazard ratios (HRs) were then calculated. Crude and weighted estimates are presented before and after OPSW along with 95% CI. All analyses were performed using the R software version 4.0.3 (29), with packages cobalt (30) and pscl (31) added.
Results
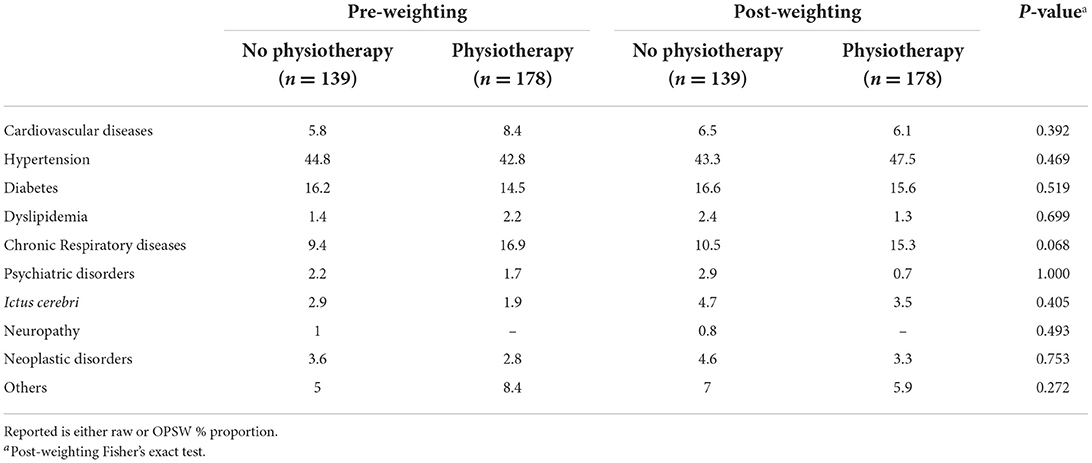
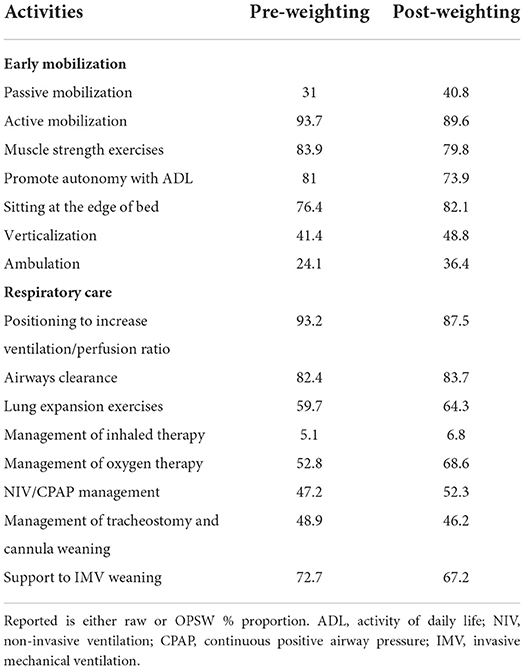
From March 1st to May 30th, 2020, 317 consecutive patients [mean (SD) age 60.5(11.5) years and 73(25%) women] were enrolled (Figure 1). Once NMBAs were withdrawn, 178 individuals received respiratory physiotherapy and 139 did not. Characteristics of included patients are summarized in Table 1. Pharmacological treatments are reported in Supplementary Table 1. Patients had a substantial prevalence of hypertension, without any remarkable difference between patients treated or not by physiotherapists (Table 2). Respiratory physiotherapy interventions are reported in Table 3. The most common respiratory physiotherapy maneuvers were active mobilization (89.6% of patients), reaching sitting at the edge of bed position (82.1% of patients) and muscle strength exercises (79.8% of patients); respiratory care was performed as well in 83.7% of patients with airways clearance techniques to decrease airways resistance and 87.5% of patients with prone or lateral positioning to improve gas exchange.
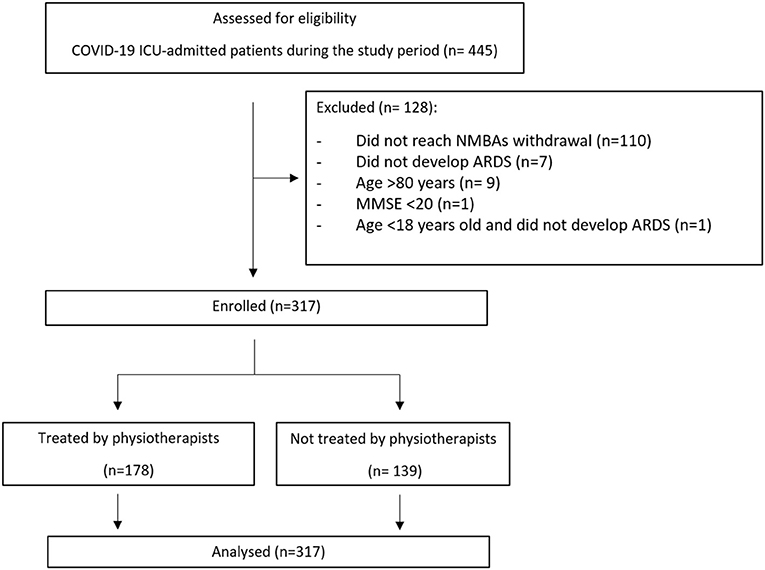
Figure 1. STROBE flow diagram.
COVID-19, Coronavirus Disease 2019; ICU, Intensive Care Unit; NMBAs, neuromuscular blocking agents; ARDS, acute respiratory distress syndrome; MMSE, mini-mental state examination.
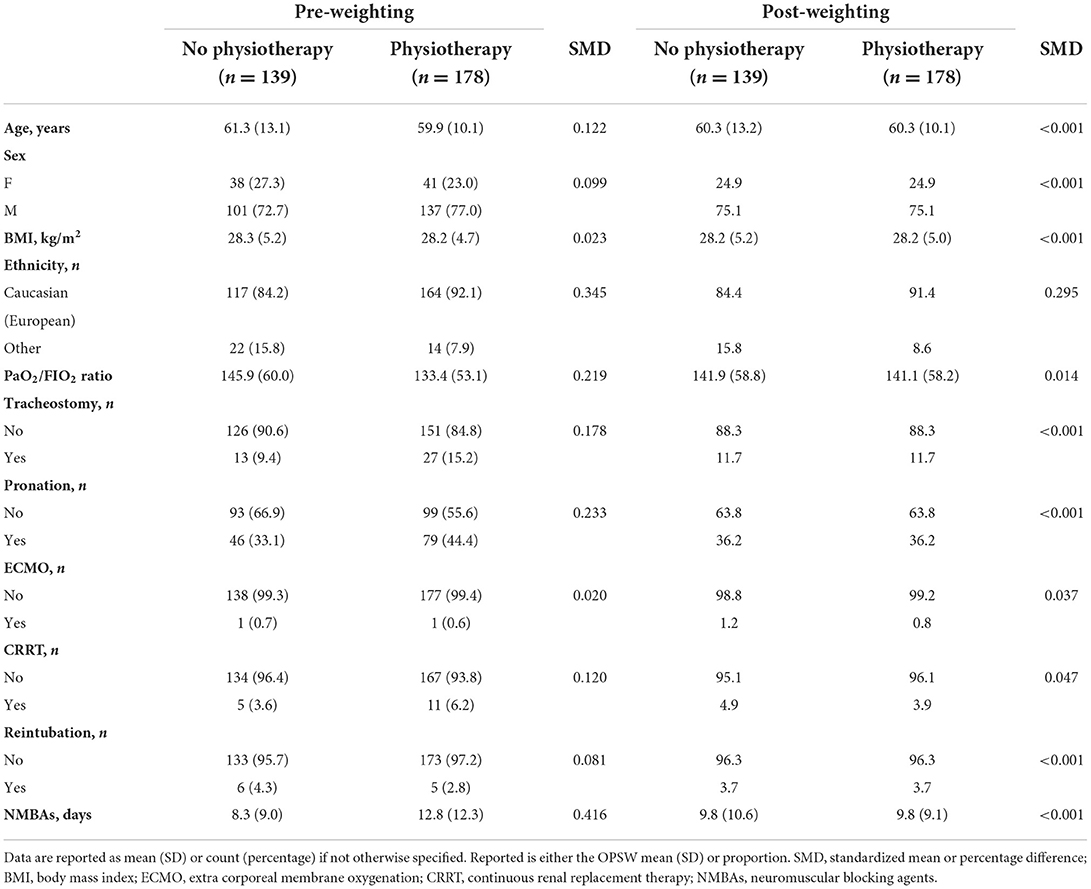
Table 1. Baseline characteristics of patients with COVID-19 before and after overlap propensity score-weighting.
Primary outcome
At day 28, 178 patients performing respiratory physiotherapy had a median of 18 ventilator-free days (IQR, 10; 24), and 139 patients not followed by physiotherapists had a median of 21 VFDs (IQR, 0; 26). Distribution of VFDs is depicted in Figure 2. Patients referred to respiratory physiotherapy were less likely to have 0 VFDs compared to those not treated (OR 0.36, 95%CI: 0.18; 0.71). The ZINB estimates are reported in Supplementary Table 2. From the inflation part, presence of tracheostomy increased the odds of having 0 VFDs by 2.1, but with a high uncertainty (95%CI: 0.92; 4.89). Patients treated with prone position were more likely to have 0 VFDs (OR 2.1, 95%CI: 1.09; 4.23). The count part shows that average number of VFDs was lower in the respiratory physiotherapy group compared to the other group (IRR 0.86, 95%CI: 0.78; 0.95). Older patients have slightly fewer VFDs (IRR 0.99, 95%CI: 0.99; 1.0). No evidence of statistical association was found between VFDs and BMI (IRR 1.0; 95%CI: 0.99; 1.01), sex (IRR 0.97, 95%CI: 0.89; 1.05), and P/F ratio at ICU admission (IRR 1.0, 95%CI: 1.0; 1.0). The number of VFDs was not different across centers whether patients received or not physiotherapy (P = 0.962); however, hospital centers did account for statistically significant differences in the VFDs (P < 0.001) (Table S2).
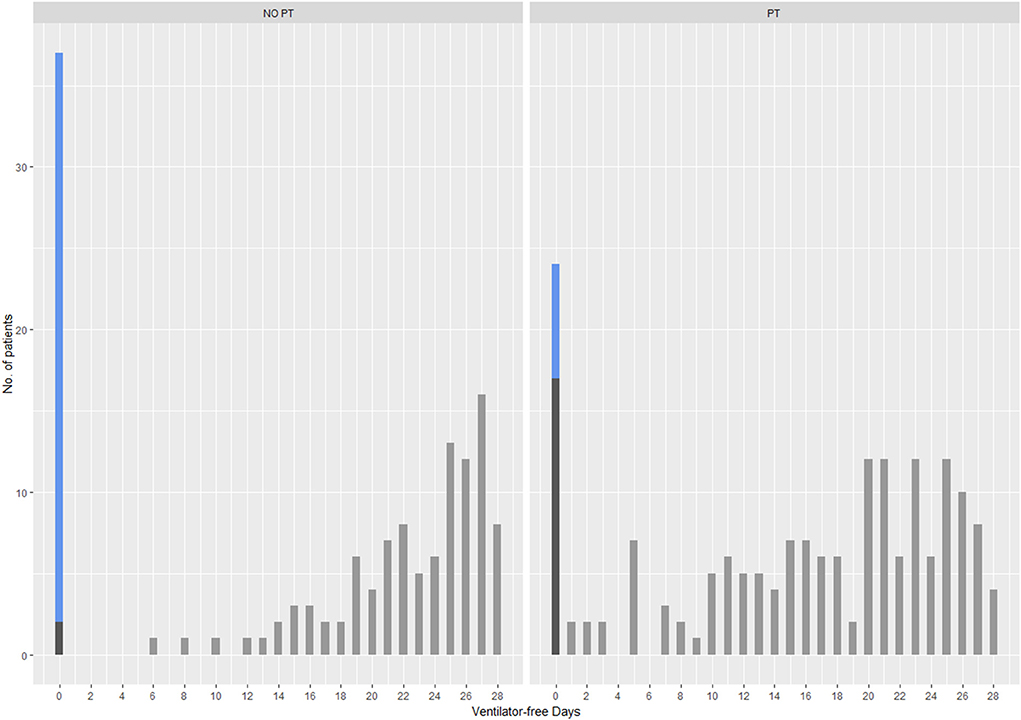
Figure 2. Distributions of VFDs between patients treated (PT) or not (NO-PT) by physiotherapists at 28 days. Blue bars denote patients who died (VFD = 0), dark gray bars denote patients alive with VFD = 0 and light gray bars identify patients alive with VFDs > 0.
Secondary outcomes
The mean P/F ratio at ICU discharge was 35.4 points higher in patients receiving respiratory physiotherapy than those who did not perform respiratory physiotherapy (95%CI: 12.6; 58.3 points). Patients receiving respiratory physiotherapy had 8.2 days longer mean ICU stay than those who did not perform respiratory physiotherapy (95%CI: 5; 11.4 days), indicating a narrow range of plausible true length of stay (Table 4). Among patients treated by physiotherapists, 96% (vs. 70.6% in the group not performing respiratory physiotherapy) survived up to 90 days (HR 0.14; 95%CI: 0.03; 0.71). No interaction was found between respiratory physiotherapy and centers in 90-day survival (P = 0.7018) as well as no evidence of association between respiratory physiotherapy and ICU survival (HR: 0.22; 95%CI: 0.04; 1.20). Overall, 96% of patients treated by physiotherapists, compared to 70% of patients in the group without physiotherapy was discharged alive from hospital (P < 0.001).
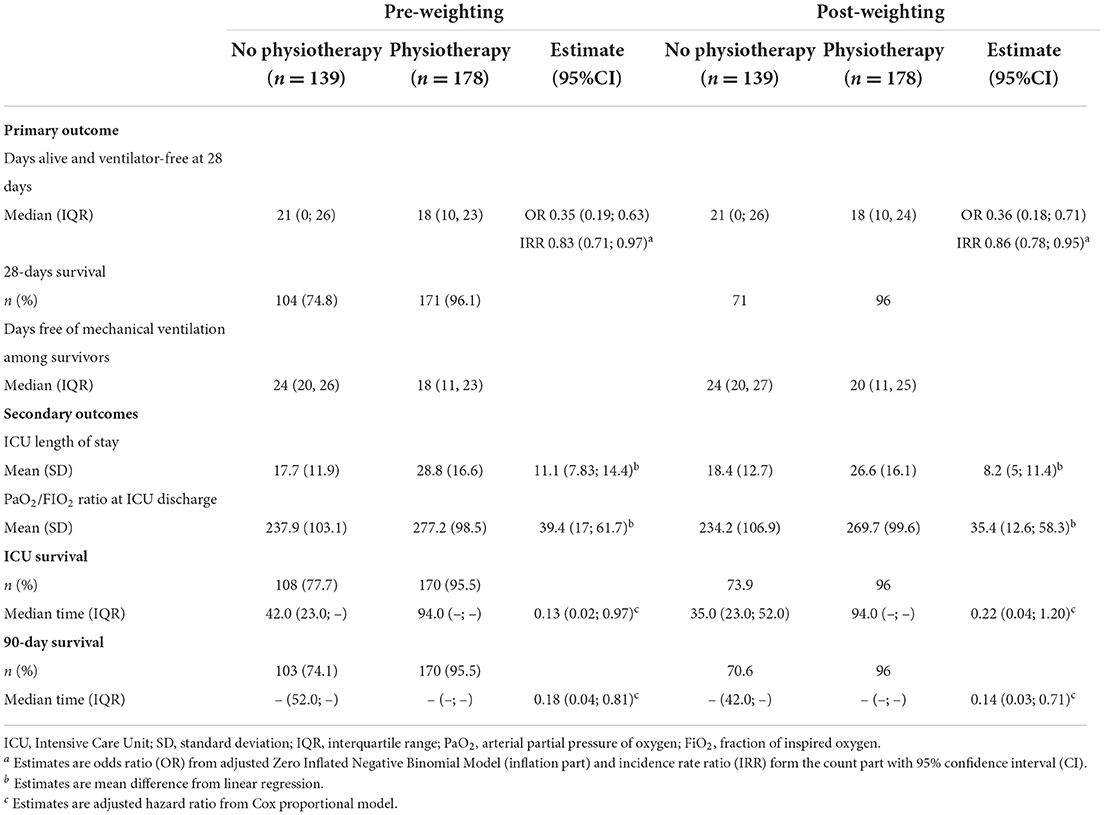
Table 4. Outcomes in patients hospitalized with COVID-19 before and after overlap propensity score-weighting.
Discussion
In this pragmatic, observational study of critically ill patients with COVID-19, we found that respiratory physiotherapy after NMBAs withdrawal was associated with less VFDs compared to no physiotherapy. In addition, patients receiving respiratory physiotherapy showed increased P/F ratio at ICU discharge, prolonged ICU stay duration; most of the patients were discharged alive from hospital. Probability of zero VFDs was lower in patients receiving respiratory physiotherapy. There was no evidence of association between VFDs and BMI, sex, or P/F ratio at ICU admission.
In the present study we included many patients treated by physiotherapists in four different ICUs, making our findings rather generalizable. The multi-modal intervention of physiotherapists in ICU during the first wave of COVID-19 pandemic, represents a pragmatic scenario of the current clinical practice (13). The primary outcome was VFDs because it is a clinically relevant measure in ICU, likely affected by both early mobilization (32) and respiratory care. In contrast to our original hypothesis, we observed that patients who received respiratory physiotherapy had less VFDs than patients who did not. Several factors may explain this result. Liberation from MV was defined for a period ≥24 h, implying that interval disconnections were not considered (this is especially true for patients with tracheostomy in whom count of VFDs started after the last successful disconnection from the ventilator). Different features could have possibly influenced the respiratory physiotherapy pathway. Firstly, delirium can affect patients' cooperation and their ability to reach functional goals (33); secondly, illness severity and comorbidities, identified by severity scores at ICU admission, may be responsible for difficult weaning, thus requiring more frequent and demanding interventions (33, 34). Thirdly, respiratory physiotherapy uses different methods or techniques of treatment (35), that allow to personalize each intervention, tuning frequency, timing, and dosage according to patient's needs and available evidence. The heterogeneity of ICU-related respiratory physiotherapy interventions described in the literature makes it difficult to measure the effectiveness of a specific treatment (36). To date, no solid short-term outcomes exist to support one respiratory physiotherapy technique over another in the ICU setting, especially if we consider the unprecedented pandemic scenario in which all healthcare professions worked with limited evidence-based guidance. We might speculate that VFDs may not be an appropriate endpoint to evaluate respiratory physiotherapy in mechanically ventilated patients. A recent systematic review (32) reports only two studies over six with a net effect of early mobilization on VFDs with high heterogeneity, thus suggesting the small responsiveness of VFDs to respiratory physiotherapy interventions. The fundamental question remains if respiratory physiotherapy has a combined and consistent effect on both mortality and on MV duration, and if this can be captured by the composite VFDs outcome. Thus, the use of time to extubation may be more appropriate since it is associated with both ICU- and post-discharge morbidity and mortality in critically ill adults, representing a patient-centered outcome measure (37). Other outcome measures might include re-intubation rate, which is potentially associated with acquisition of ventilatory acquired pneumonia (22).
The number of VFDs differed among centers likely due to regional disparities in the spread of COVID-19 with hospitals facing an extreme burden and very challenging work conditions. We hypothesize that the decision to address patients to physiotherapists varied among centers. However, there was no association between respiratory physiotherapy among centers and VFDs, which indirectly means that different physiotherapists used similar clinical approaches. This is further supported by the lack of interaction of physiotherapy with center in the survival model.
Patients treated by physiotherapists showed a longer duration of MV and ICU stay but better oxygenation at ICU discharge and 90-day survival. The improvement in oxygenation after respiratory physiotherapy has been previously reported (38). Survival rate is not in line with previous studies (39) since those patients who did not reach the NMBAs withdrawal and therefore died in ICU were not eligible. The COVID-19 pandemic forced the medical team to allocate treatments in resource-limited circumstances (40), including respiratory physiotherapy (41). In our study, each ICU medical team decided autonomously if patients needed or not respiratory physiotherapy and this might have introduced a selection bias. As a matter of fact, indications for respiratory physiotherapy initiation are currently missing. We addressed this issue in the study design by enrolling only patients who achieved the NMBAs withdrawal, which is the moment when respiratory physiotherapy can potentially start. To account for the selection bias, we used the OPSW. Therefore, presented estimates are measures of association between respiratory physiotherapy/no-respiratory physiotherapy and VFDs, with respect to a population of patients at equipoise either to receive treatment or not (27). Nevertheless, we cannot exclude that a further bias may had occurred in the group of individuals deemed more likely to survive, resulting in respiratory physiotherapy requested for individuals who were experiencing difficult weaning, leaving others exposed to natural disease recovery. All these implicit decisions could be plausibly responsible for the survival benefit as seen in the respiratory physiotherapy group but could also account for the longer MV duration and ICU stay. Considering that respiratory physiotherapy interventions in ICU are not limited to early mobilization but also to respiratory care (42), especially in patients with respiratory diseases, yet it remains crucial to understand how intensivists decide which patient needs or not these treatments. Where physiotherapists are not part of the ICU staff or not involved in the routine assessment of individuals hospitalized in ICU (16, 43, 44), goal-oriented allocation criteria shared between physiotherapists and intensivists are needed. Under this perspective, we convene that respiratory physiotherapy initiation in ICU is not a random process. Decisional rules should be further explored and validated in terms of disease-oriented and patient-important outcomes. Patient assessment and proactive respiratory physiotherapy remain crucial to optimize treatments and ICU staff utilization.
Limitations
Several limitations must be acknowledged. First, this is an observational retrospective study which can be susceptible to selection bias. Second, unmeasured confounders might have been overlooked since different ventilatory strategies among centers could have played a role in the MV duration. Third, despite respiratory physiotherapy treatments were individualized, the dose, intensity, and frequency of each intervention were not evaluated. Finally, we cannot exclude that our results could be further biased by regional differences in COVID-19 management and hospital staff workload; however, we used center as adjusting factor (37).
Conclusion
In mechanically ventilated COVID-19 patients admitted to ICU, respiratory physiotherapy intervention, including early mobilization and respiratory care, was associated with a lower number of VFDs compared to patients who were not treated by physiotherapists. Future studies on respiratory physiotherapy in ICU should be designed considering responsive outcomes to both early mobilization and respiratory care, given that physiotherapy is an ensemble of methods and techniques with different rationales.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Ethics Committee of the Fondazione IRCCS Ca' Granda Ospedale Maggiore Policlinico (Comitato Etico Milano Area 2, approval n. 966_2020bis). Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
EP: conceptualization, resources, methodology, supervision, and project administration. SG: methodology, formal analysis, visualization, data curation, writing original draft, writing review, and editing. VR and FB: conceptualization, methodology, investigation, data curation, writing review, and editing. MS: conceptualization, methodology, data curation, investigation, data curation, writing original draft, writing review, and editing. DT and SC: investigation and data curation. VT and CC: investigation, resources, writing review, and editing. DB: investigation, writing review, and editing. MP: conceptualization, methodology, writing original draft, writing review, and editing. RF and PP: resources, writing review, and editing. GG: resources, supervision, writing review, and editing.
Funding
This study was (partially) funded by Italian Ministry of Health—Current research IRCCS.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2022.994900/full#supplementary-material
References
1. Schweickert WD, Pohlman MC, Pohlman AS, Nigos C, Pawlik AJ, Esbrook CL, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet. (2009) 373:1874–82. doi: 10.1016/S0140-6736(09)60658-9
2. Zhang G, Zhang K, Cui W, Hong Y, Zhang Z. The effect of early mobilization for critical ill patients requiring mechanical ventilation: a systematic review and meta-analysis. J Emerg Crit Care Med. (2018) 2:9–9. doi: 10.21037/jeccm.2018.01.04
3. Kim RY, Murphy TE, Doyle M, Pulaski C, Singh M, Tsang S, et al. Factors associated with discharge home among medical icu patients in an early mobilization program. Crit Care Explor. (2019) 1:e0060. doi: 10.1097/CCE.0000000000000060
4. Tipping CJ, Harrold M, Holland A, Romero L, Nisbet T, Hodgson CL. The effects of active mobilisation and rehabilitation in ICU on mortality and function: a systematic review. Intens Care Med. (2017) 43:171–83. doi: 10.1007/s00134-016-4612-0
5. Halpin SJ, McIvor C, Whyatt G, Adams A, Harvey O, McLean L, et al. Postdischarge symptoms and rehabilitation needs in survivors of COVID-19 infection: a cross-sectional evaluation. J Med Virol. (2022) 93:1013–22. doi: 10.1002/jmv.26368
6. Boutou AK, Asimakos A, Kortianou E, Vogiatzis I, Tzouvelekis A. Long COVID-19 pulmonary sequelae and management considerations. J Pers Med. (2021) 11:838. doi: 10.3390/jpm11090838
7. Paneroni M, Simonelli C, Saleri M, Bertacchini L, Venturelli M, Troosters T, et al. Muscle strength and physical performance in patients without previous disabilities recovering from COVID-19 pneumonia. Am J Phys Med Rehabil. (2021) 100:105–9. doi: 10.1097/PHM.0000000000001641
8. Huang C, Huang L, Wang Y, Li X, Ren L, Gu X, et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet. (2021) 397:220–32. doi: 10.1016/S0140-6736(20)32656-8
9. McWilliams D, Weblin J, Hodson J, Veenith T, Whitehouse T, Snelson C. Rehabilitation levels in patients with COVID-19 admitted to intensive care requiring invasive ventilation an observational study. Ann Am Thorac Soc. (2021) 18:122–9. doi: 10.1513/AnnalsATS.202005-560OC
10. Rossi V, Del Monaco C, Gambazza S, Santambrogio M, Binda F, Retucci M, et al. Time to active sitting position: one-year findings from a temporary COVID-19 Intensive Care Unit. Respir Med. (2022) 194:106773. doi: 10.1016/j.rmed.2022.106773
11. Battaglini D, Robba C, Caiffa S, Ball L, Brunetti I, Loconte M, et al. Chest physiotherapy: an important adjuvant in critically ill mechanically ventilated patients with COVID-19. Respir Physiol Neurobiol. (2020) 282:103529. doi: 10.1016/j.resp.2020.103529
12. Rossi V, Santambrogio M, del Monaco C, Retucci M, Tammaro S, Ceruti C, et al. Safety and feasibility of physiotherapy in ICU-admitted severe COVID-19 patients: an observational study. Monaldi Arch Chest Dis. (2022). doi: 10.4081/monaldi.2022.2087. [Epub ahead of print].
13. Barnish M, Turner S. The value of pragmatic and observational studies in health care and public health. Pragm Observ Res. (2017) 8:49–55. doi: 10.2147/POR.S137701
14. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. (2009) 42:377–81. doi: 10.1016/j.jbi.2008.08.010
15. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. (2008) 61:344–9. doi: 10.1016/j.jclinepi.2007.11.008
16. Salvitti S, Repossini E. Perception, experience and knowledge of early physiotherapy in Intensive Care Units of Rome: a survey. Monaldi Arch Chest Dis. (2020) 90:742–50. doi: 10.4081/monaldi.2020.1412
17. ARDS Definition Task Force, Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, et al. Acute respiratory distress syndrome: the Berlin definition. JAMA. (2012) 307:2526–33. doi: 10.1001/jama.2012.5669
18. Alhazzani W, Evans L, Alshamsi F, Møller MH, Ostermann M, Prescott HC, et al. Surviving sepsis campaign guidelines on the management of adults with Coronavirus Disease 2019 (COVID-19) in the ICU: first update. Crit Care Med. (2021) 49:E219–34. doi: 10.1097/CCM.0000000000004899
19. Lazzeri M, Lanza A, Bellini R, Bellofiore A, Cecchetto S, Colombo A, et al. Respiratory physiotherapy in patients with COVID-19 infection in acute setting: a position paper of the Italian Association of Respiratory Physiotherapists (ARIR). Monaldi Arch Chest Dis. (2020) 90:163–8. doi: 10.4081/monaldi.2020.1285
20. Thomas P, Baldwin C, Bissett B, Boden I, Gosselink R, Granger CL, et al. Physiotherapy management for COVID-19 in the acute hospital setting: clinical practice recommendations. J Physiother. (2020) 66:73–82. doi: 10.1016/j.jphys.2020.03.011
21. Zhao HM, Xie YX, Wang C, Chinese Chinese Association of Rehabilitation Medicine; Respiratory Rehabilitation Committee of Chinese Association of Rehabilitation Medicine; Cardiopulmonary Rehabilitation Group of Chinese Society of Physical Medicine and Rehabilitation. Recommendations for respiratory rehabilitation in adults with Coronavirus Disease 2019. Chin Med J (Engl). (2020) 133:1595–602. doi: 10.1097/CM9.0000000000000848
22. Tronstad O, Martí JD, Ntoumenopoulos G, Gosselink R. An update on cardiorespiratory physiotherapy during mechanical ventilation. Semin Respir Crit Care Med. (2022). 43:390–404. doi: 10.1055/s-0042-1744307
23. Chen JW, Maldonado DR, Kowalski BL, Miecznikowski KB, Kyin C, Gornbein JA, et al. Best practice guidelines for propensity score methods in medical research: consideration on theory, implementation, and reporting. A review. Arthroscopy. (2022) 38:632–42. doi: 10.1016/j.arthro.2021.06.037
24. Webster-Clark M, Stürmer T, Wang T, Man K, Marinac-Dabic D, Rothman KJ, et al. Using propensity scores to estimate effects of treatment initiation decisions: state of the science. Stat Med. (2021) 40:1718–35. doi: 10.1002/sim.8866
25. Brookhart MA, Schneeweiss S, Rothman KJ, Glynn RJ, Avorn J, Stürmer T. Variable selection for propensity score models. Am J Epidemiol. (2006) 163:1149–56. doi: 10.1093/aje/kwj149
26. Desai RJ, Franklin JM. Alternative approaches for confounding adjustment in observational studies using weighting based on the propensity score: a primer for practitioners. BMJ. (2019) 367:l5657. doi: 10.1136/bmj.l5657
27. Li F, Morgan KL, Zaslavsky AM. Balancing covariates via propensity score weighting. J Am Stat Assoc. (2018) 113:390–400. doi: 10.1080/01621459.2016.1260466
28. Zeileis A, Kleiber C, Jackman S. Regression models for count data in R. J Stat Softw. (2008) 27:1–25. doi: 10.18637/jss.v027.i08
29. R Core Team. R: A Language and Environment for Statistical Computing. Vienna: R Foundation for Statistical Computing. (2019).
31. Jackman S. pscl: Classes and Methods for R Developed in the Political Science Computational Laboratory. United States Studies Centre, University of Sydney, Sydney, NSW, Australia (2020).
32. Zhang L, Hu W, Cai Z, Liu J, Wu J, Deng Y, et al. Early mobilization of critically ill patients in the Intensive Care Unit: a systematic review and meta-analysis. PLoS ONE. (2019) 14:e0223185. doi: 10.1371/journal.pone.0223185
33. Parry SM, Knight LD, Connolly B, Baldwin C, Puthucheary Z, Morris P, et al. Factors influencing physical activity and rehabilitation in survivors of critical illness: a systematic review of quantitative and qualitative studies. Intens Care Med. (2017) 43:531–42. doi: 10.1007/s00134-017-4685-4
34. Harrold ME, Salisbury LG, Webb SA, Allison GT. Early mobilisation in Intensive Care Units in Australia and Scotland: a prospective, observational cohort study examining mobilisation practises and barriers. Crit Care. (2015). 19:336. doi: 10.1186/s13054-015-1033-3
35. Jull G, Moore AP. Physiotherapy is not a treatment technique. Musculoskelet Sci Pract. (2021) 56:102480. doi: 10.1016/j.msksp.2021.102480
36. van der Lee L, Hill AM, Patman S. A survey of clinicians regarding respiratory physiotherapy intervention for intubated and mechanically ventilated patients with community-acquired pneumonia. What is current practice in Australian ICUs? J Eval Clin Pract. (2017) 23:812–20. doi: 10.1111/jep.12722
37. Yehya N, Harhay MO, Curley MAQ, Schoenfeld DA, Reeder RW. Reappraisal of ventilator-free days in critical care research. Amer J Respir Crit Care Med. (2019) 200:828–36. doi: 10.1164/rccm.201810-2050CP
38. Battaglini D, Caiffa S, Gasti G, Ciaravolo E, Robba C, Herrmann J, et al. An experimental pre-post study on the efficacy of respiratory physiotherapy in severe critically III COVID-19 patients. J Clin Med. (2021) 10:2139. doi: 10.3390/jcm10102139
39. Grasselli G, Greco M, Zanella A, Albano G, Antonelli M, Bellani G, et al. Risk factors associated with mortality among patients with COVID-19 in Intensive Care Units in Lombardy, Italy. JAMA Intern Med. (2020) 180:1345–55. doi: 10.1001/jamainternmed.2020.3539
40. Vergano M, Bertolini G, Giannini A, Gristina GR, Livigni S, Mistraletti G, et al. Clinical ethics recommendations for the allocation of intensive care treatments in exceptional, resource-limited circumstances: the Italian perspective during the COVID-19 epidemic. Crit Care. (2020) 24:165. doi: 10.1186/s13054-020-02891-w
41. Gambazza S, Bargeri S, Campanini I, Meroni R, Turolla A, Castellini G, et al. Prevalence and associated factors of COVID-19 across Italian regions: a secondary analysis from a national survey on physiotherapists. Arch Physiother. (2021) 11:30. doi: 10.1186/s40945-021-00125-y
42. Black C, Klapaukh R, Gordon A, Scott F, Holden N. Unanticipated demand of physiotherapist-deployed airway clearance during the COVID-19 surge 2020 a single centre report. Physiotherapy. (2021) 113:138–40. doi: 10.1016/j.physio.2021.03.010
43. Bakhru RN, Wiebe DJ, McWilliams DJ, Spuhler VJ, Schweickert WD. An environmental scan for early mobilization practices in U.S. ICUs. Crit Care Med. (2015) 43:2360–9. doi: 10.1097/CCM.0000000000001262
Keywords: respiratory physiotherapy, Intensive Care Unit, ventilator-free days, COVID-19, critical illness
Citation: Privitera E, Gambazza S, Rossi V, Santambrogio M, Binda F, Tarello D, Caiffa S, Turrin V, Casagrande C, Battaglini D, Panigada M, Fumagalli R, Pelosi P and Grasselli G (2022) Association of ventilator-free days with respiratory physiotherapy in critically ill patients with Coronavirus Disease 2019 (COVID-19) during the first pandemic wave. A propensity score-weighted analysis. Front. Med. 9:994900. doi: 10.3389/fmed.2022.994900
Received: 15 July 2022; Accepted: 25 August 2022;
Published: 12 September 2022.
Edited by:
Abele Donati, Marche Polytechnic University, ItalyReviewed by:
Andrea Carsetti, Marche Polytechnic University, ItalyLucía Presa Fernández, Hospital Clínico Universitario de Valencia, Spain
Copyright © 2022 Privitera, Gambazza, Rossi, Santambrogio, Binda, Tarello, Caiffa, Turrin, Casagrande, Battaglini, Panigada, Fumagalli, Pelosi and Grasselli. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Martina Santambrogio, bXNhbnRhbWJyb2dpb0BnbWFpbC5jb20=
 Emilia Privitera
Emilia Privitera Simone Gambazza
Simone Gambazza Veronica Rossi
Veronica Rossi Martina Santambrogio
Martina Santambrogio Filippo Binda
Filippo Binda Davide Tarello4
Davide Tarello4 Salvatore Caiffa
Salvatore Caiffa Denise Battaglini
Denise Battaglini Mauro Panigada
Mauro Panigada Paolo Pelosi
Paolo Pelosi Giacomo Grasselli
Giacomo Grasselli