- 1Department of Human Physiology, College of Medicine and Health Science, School of Medicine, University of Gondar, Gondar, Ethiopia
- 2Department of Epidemiology and Biostatistics, College of Medicine and Health Science, Institute of Public Health, University of Gondar, Gondar, Ethiopia
- 3Department of Human Anatomy, College of Medicine and Health Science, School of Medicine, University of Gondar, Gondar, Ethiopia
- 4Department of Women and Family Health, College of Medicine and Health Science, School of Midwifery, University of Gondar, Gondar, Ethiopia
- 5Department of Pediatrics and Child Health, College of Medicine and Health Science, School of Medicine, University of Gondar, Gondar, Ethiopia
Background: Despite progress in reducing maternal and child mortality, many low- and middle-income countries (LMICs) still experience an unacceptably high level of the problem. The World Health Organization (WHO) recently recommended pregnant women should have at least eight antenatal care visits (ANC8+) with a trained healthcare provider as a key strategy to promote pregnant women's health. Antenatal care is an imperative factor for subsequent maternal healthcare utilization such as health facility delivery and early postnatal care (EPNC). This study aimed to examine the net impact of ANC8+ visits on health facility delivery and EPNC in LMICs using a propensity score matching analysis.
Methods: We used the recent Demographic and Health Survey (DHS) datasets from 19 LMICs. Women of reproductive age (15–49 years) who had given birth within 1 year preceding the survey were included. A propensity score matching analysis was employed to assess the net impact of eight or more antenatal care visits on health facility delivery and early postnatal care.
Result: After matching the covariates, women who attended ANC8+ visits had a 14% (ATT = 0.14) higher chance of having their delivery at health facilities compared with women who attended less than eight ANC visits. This study further revealed that women who had ANC8+ visits were associated with a 10% (ATT = 0.10) higher probability of early PNC compared with their counterparts.
Conclusion and recommendation: This study confirmed that ANC8+ visits significantly increased the likelihood of health facility-based delivery and early PNC utilization in LMICs. These findings call for public health programs to focus on pregnant women attending adequate ANC visits (according to revised WHO recommendation) as our study indicates that ANC8+ visits significantly improved the chances of subsequent care.
Background
Despite progress in reducing maternal and child mortality, many low- and middle-income countries (LMICs) still experience an unacceptably high level of the problem (1, 2). In 2017, 295,000 women died due to complications in pregnancy and childbirth globally. The vast majority of these deaths (86%) occurred in Sub-Saharan Africa and Southern Asia (3). All countries with the United Nations have agreed and adopted 17 Sustainable Development Goals so that they can change the world for the better (4, 5). Sustainable development goal 3 (SDG-3) aims to reduce the global maternal mortality ratio to 70 deaths per 100,000 live births by 2030 (6). To achieve this goal, timely and frequent care for pregnant women by healthcare providers has paramount significance (7, 8).
The World Health Organization (WHO) recently recommended pregnant women should have at least eight antenatal care (ANC8+) visits with a trained healthcare provider as a key strategy to promote pregnant women's health (9, 10). Timely and frequent ANC endorses existing disease treatments, vaccination, malaria prophylaxis, iron supplementation, nutrition counseling, HIV counseling and testing, urinary tract infection treatment, and other related services (11–13). Antenatal care is also an imperative factor for subsequent maternal healthcare utilization such as health facility delivery and early postnatal care (EPNC) (14, 15). As advocated by the WHO, health facility delivery with trained birth attendants and EPNC have principal importance in reducing maternal mortality (16–18).
The first ANC visit should start in the first trimester while postnatal care should be given to a woman within 48 h after the delivery of the placenta and continue for 42 days (19, 20). In LMICs, numerous studies have revealed empirical evidence concerning the impact of individual, household, and community-level factors on this continuum of care utilization in different settings (21–24). However, the relationship between ANC and the subsequent continuum of care in a cross-sectional study might not be robust because of the presence of selection bias and confounding (25). Despite country-specific studies that have tried to link the ANC4+ visits with institutional delivery and early PNC (14, 25, 26), there is no evidence of the net impact of ANC8+ visits on subsequent institutional delivery and early PNC in LMICs. Many women in developing countries do not adhere to the WHO recommendation of at least eight ANC visits during pregnancy (27). Subsequent care aspects such as having delivery at a health facility and attending early postnatal care also remain a significant problem in those nations. Exploring the impact of ANC8+ on subsequent care can help to inform better policy and practice (28, 29). Therefore, our study aimed to examine the net impact of ANC8+ visits on health facility delivery and EPNC in LMICs using PSM and employing sensitivity analyses to assure the robustness of our findings.
Materials and methods
Study design and setting
This study used secondary data from 19 LMICs that have a recent Demographic Health Survey (DHS) collected after the 2016 WHO ANC model (30). This model recommends a minimum of eight ANC contacts during pregnancy, with the first contact occurring in the first trimester of gestation followed by two and five contacts in the second and third trimesters, respectively (9).
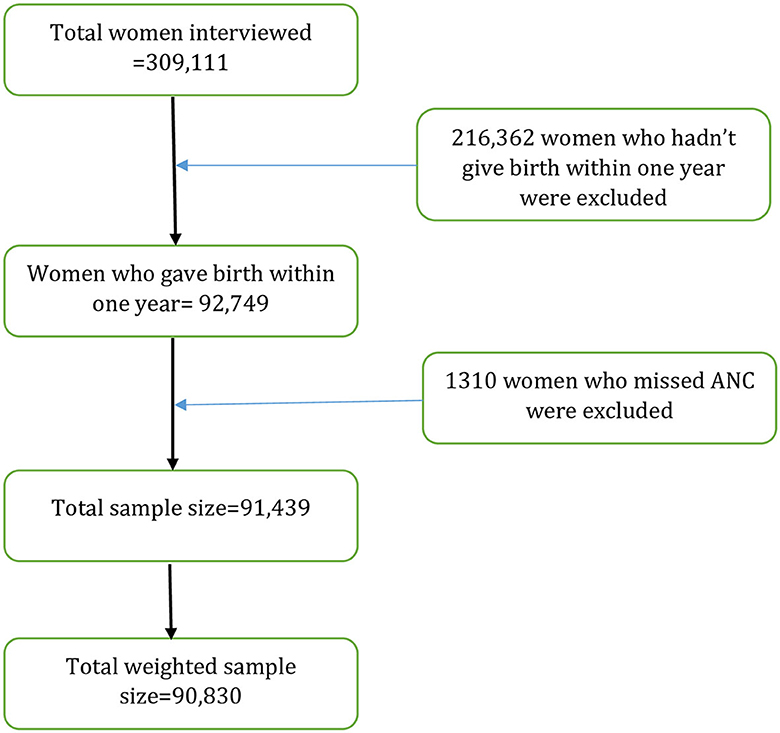
The DHS is a nationally representative survey that uses a cross-sectional design to collect data on women, men, and children. The surveys use the same standardized data collection procedures, sampling, questionnaires, and coding, making the results comparable across countries. A total of 309,111 reproductive ages (15–49 years) were interviewed in 19 LMICs. However, this study was limited to women aged 15–49 years who had live births within the year prior to the surveys. Finally, 90,830 women aged 15–49 years were included in the analysis (Figure 1). The list of those countries and the respective year of surveys is provided in Table 1.
Definition of variables
Outcome variable
The outcome variables of this study were health facility delivery and EPNC. Health facility delivery was a dichotomous variable where respondents were coded as having an institutional delivery if they delivered within a public, private, or non-governmental organization facility. Early PNC is a postnatal checkup from a skilled health provider within 2 days after childbirth. It was coded into a binary variable where women who had a postnatal checkup by a skilled provider within 2 days of delivery were coded 1 and otherwise 0.
Treatment variable
The treatment variable was an ANC visit of their most recent pregnancy that ended with a live birth. The number of ANC contacts of pregnant women was categorized as those who had at least eight ANC contacts and those who had fewer than eight ANC contacts, according to the 2016 WHO recommendation.
Matching variables
This study considered covariates on the basis of available literature that was related to both the treatment (ANC visits) and the outcome variables (health facility delivery and early PNC) (14, 25, 26). The lists of included variables were as follows: age, education level, household wealth status, marital status, wanted pregnancy, media exposure, birth order, residence, sex of household head, and accessing healthcare.
Statistical analyses
This study used PSM to draw causal inferences about the effect of eight or more ANC on health facility delivery, and early PNC. PSM is a statistical method that allows us to evaluate the treatment effects for observational data, in cases where randomized controlled trials are either infeasible, unethical, or when researchers need to evaluate treatment effects from survey data (31). It reduces bias due to observable individual characteristics by matching and helps create comparable balanced groups of respondents with respect to observed covariates (25).
STATA V.14.2 software was used to clean, recode, and analyze the data. Pscore Stata command was used to generate the propensity score including covariates associated with ANC visits (treatment variable) and both outcomes. The common support option was employed to limit testing of the balancing property to only treated mothers whose propensity scores for health facility delivery and EPNC were within the propensity score range. The average treatment effect on the treated (ATT) was estimated using the psmatch2 or teffects psmatch Stata command. To generate ATT, one-to-one nearest neighbor matching with replacement within a caliper range of ±0.01 was performed. Balancing tests were performed using the pstest stata command. For each covariate included in the propensity score estimation model, percentage (%) bias and % reduction bias were reported. Finally, a sensitivity analysis was undertaken to assess the assumption of the unconfoundedness of PSM using a Mantel–Haenszel bounds procedure.
Results
Background characteristics of study participants
A total of 90,830 women were included in the analysis. Of the total, 47.05% were aged 25–34 years and 43.27% had attained secondary education. In total, 95.43% of women were married and only 15.54% of them were head of the household. Almost half (49.07%) of the participants were from low-wealth quintile households (poorest and poorer). In total, 85.98% of women had a wanted pregnancy. In total, 58.72% of respondents watch television. Almost a third-fourth (73.08%) of participants were rural residents, and healthcare access was a big problem for more than half (51.45%) of them (Table 2).
Estimated propensity scores and model significance
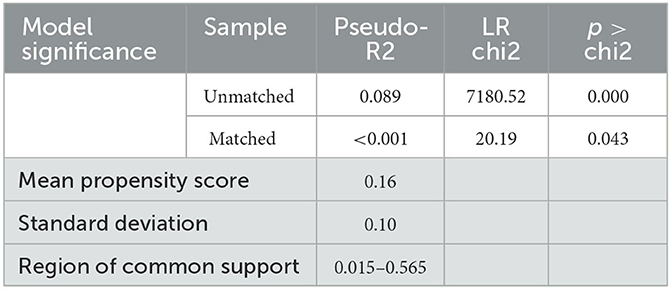
The mean propensity score was 0.16, with a standard deviation of 0.10 indicating the variability is little between the treatment and control groups. Regarding model significance, the pseudo-R2 before matching and after matching was 0.089 and < 0.001, respectively. Very low pseudo-R2 (< 0.001) indicates the distribution of covariates between both groups was similar (Table 3).
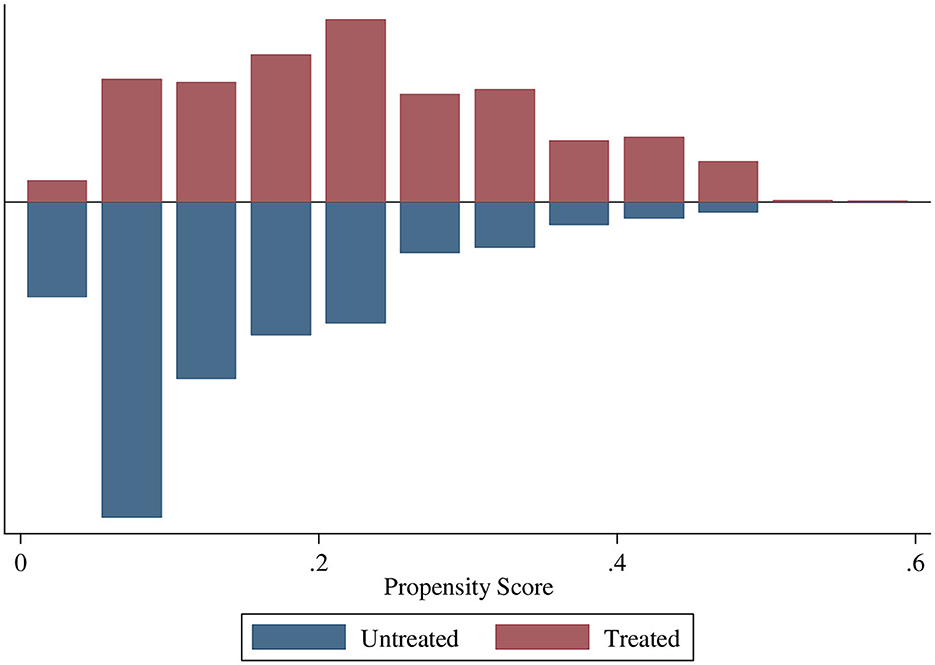
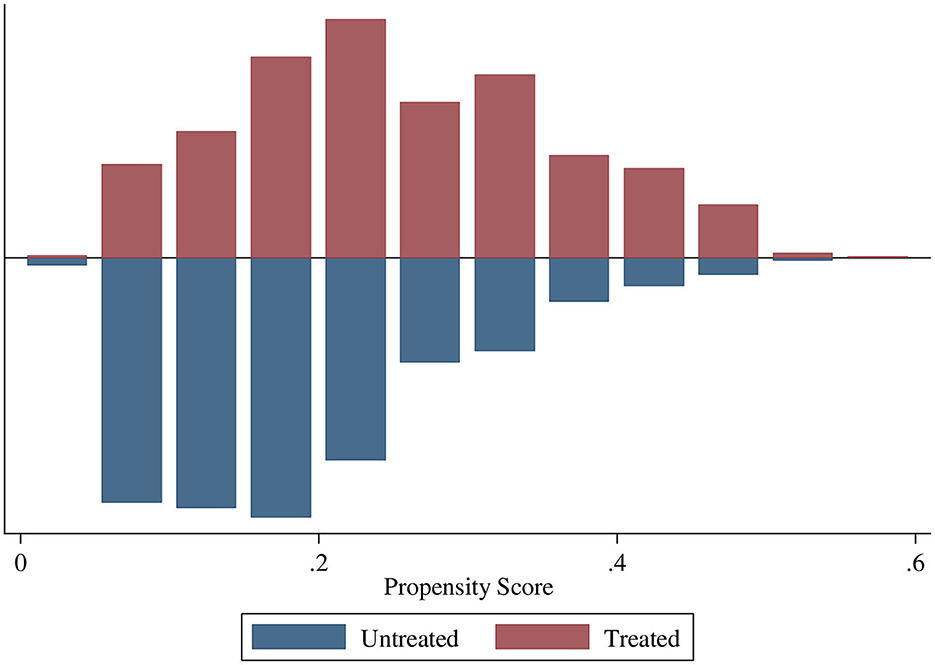
Common support
The region of common support ranges from 0.015 to 0.565. The common support improves the quality of matching by discarding individuals when there is no availability of a match. The treatment (ANC8 + visits) and control (<8 ANC visits) groups are matched and comparable as the quality of matching by health facility delivery and early PNC were balanced with no off support (Figures 2, 3).
Average treatment effect of ANC8+ on health facility delivery and EPNC
Our study showed that the average treatment effect on the treated (ATT) on facility delivery and early PNC was 0.14 and 0.10, respectively. This indicates that the probability of facility-based delivery was 14% higher among treated women (who have ANC8+ visits) compared with the control group. Meanwhile, women who had ANC 8+ have an increased chance of having early PNC by 10% compared with those who had not. The net difference of ANC4 between treated and control was higher on institutional delivery; however, the ANC8+ had more impact on the EPNC. Generally, the ATT of ANC8+ has more impact in the treated (94%), while in ANC4+ it is 86% (Table 4).
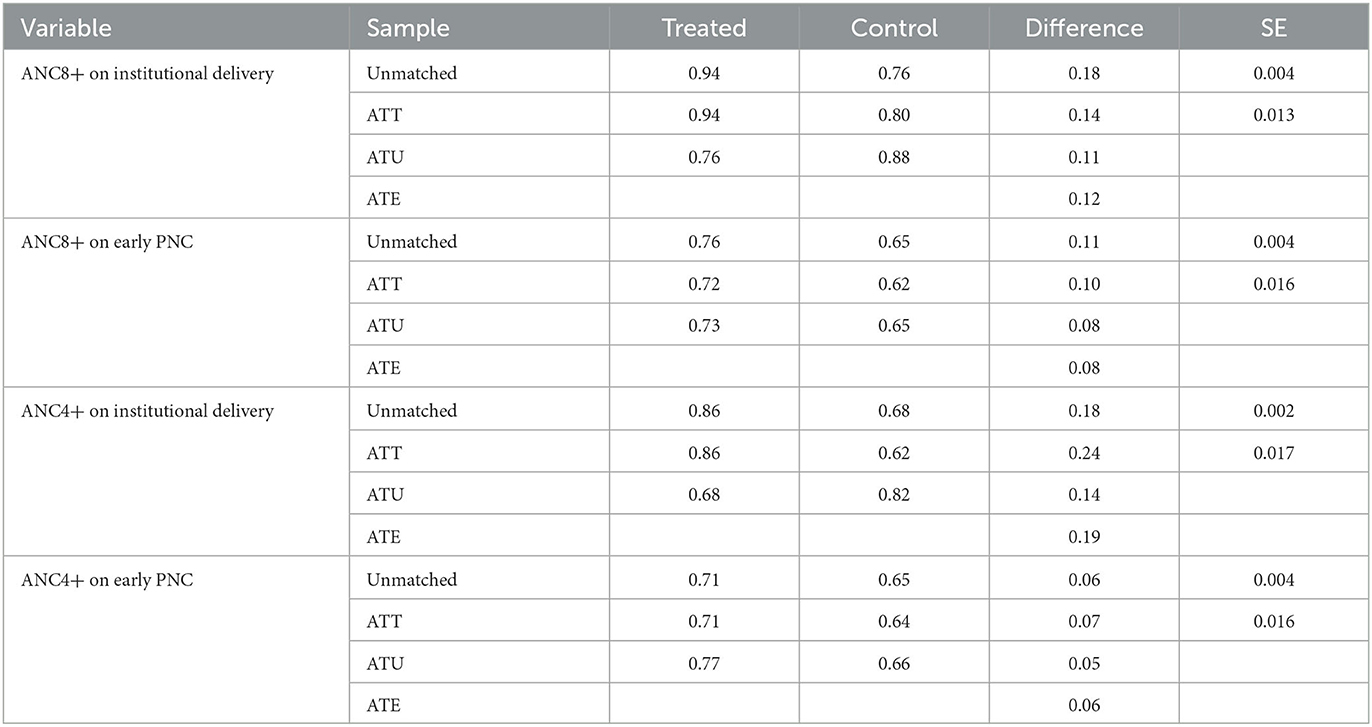
Table 4. Estimation of average treatment effect on the treated, average treatment effect on the untreated, and average treatment effect of 8+ ANCs on facility delivery and early PNC.
Balancing test
This study depicted before and after matching mean values and bias of each covariate in both groups. There is a percentage bias reduction for all matching covariates presented along with the t-test. The significance level of the t-test was also calculated, and it showed that the majority of covariates were balanced (Table 5).
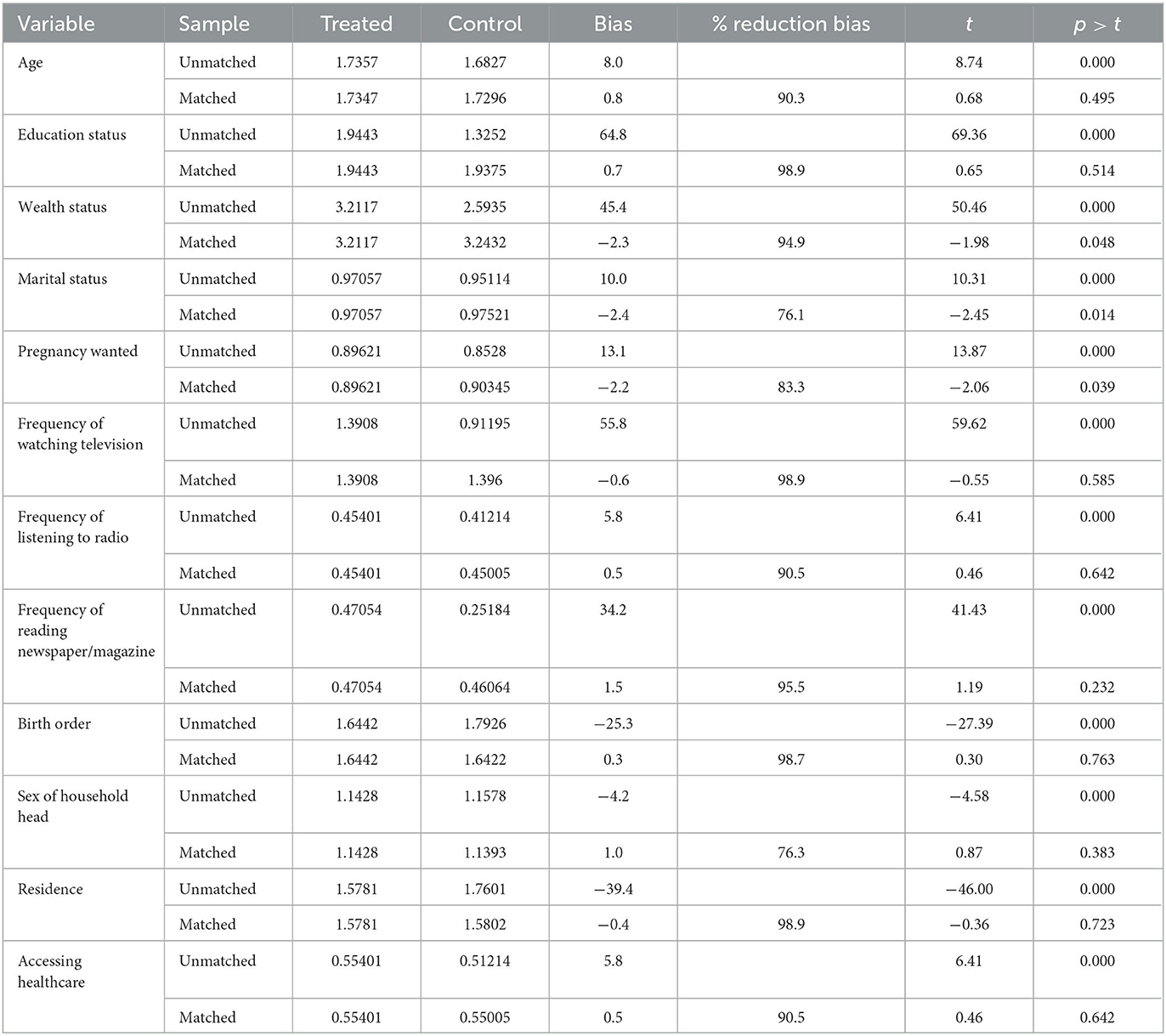
Table 5. Comparison of the standardized differences of baseline characteristics before and after matching.
Sensitivity analysis for hidden bias
The sensitivity analysis was performed using the Mantel–Haenszel statistic to estimate the extent of unobservable covariates biases on our inferences about the effects of 8+ ANC visits. The Q_mh+ statistic adjusts the MH statistic downward for positive unobserved selection bias, and as the estimated ANC visits effect is positively related to outcome variables, we focused on the positive bias. Based on this, a critical value >1.4 indicates that the result will be insensitive and the conclusion could be uncertain (Supplementary Table).
Discussion
Maternal and child mortality remain a substantial public health concern worldwide, especially in LMICs (2, 32, 33). Complications during pregnancy and childbirth are the leading causes of maternal and child deaths (34, 35). The WHO recommended ANC8+ visits as a key strategy to endorse pregnant women's health (9). In addition to ANC visits, health facility delivery and early PNC have been reported as major contributors to preserving women's and child's health (28, 36, 37). Previous studies showed that prenatal care is an imperative factor for subsequent healthcare utilization (38–40). This study revealed that ANC8+ visits have a significant and positive influence on health facility delivery as well as EPNC.
We used an innovative statistical method called the propensity score matching (PSM) to understand the net impact of ANC8+ visits on health facility delivery and EPNC. This method is useful to ensure that study participants in the control and treatment groups are similar based on measured characteristics. PSM reduces selection bias and offers an alternative for measuring treatment effects in cross-sectional/observational/non-experimental data when randomized clinical trials are not possible or unethical. Therefore, the groups are the same except for the treatment variable ensuring a less-biased estimate of treatment effects.
This study found that women who attended ANC8+ visits had a 14% higher chance of having their delivery at health facilities. Our finding was supported by previous studies conducted in the developing world (41–43). For example, a study from Uganda assessed the impact of ANC visits based on previous WHO recommendations (ANC4+ visits), and the result showed that the treated women were almost 12 and 10% higher to give birth at health facilities and have EPNC, respectively (26). This is likely due to the fact that women who attend adequate ANC receive maternal education and are often referred to health facilities for delivery. However, this result showed that ANC4+ contact has more impact (24%) on health facility delivery. Generally, we can conclude that adequate ANC contacts are critical for institutional delivery. Therefore, this health facility delivery in turn could advantageous for pregnant women to attend early PNC.
This study further showed that women who had ANC8+ visits were associated with a 10% higher probability of early PNC compared with their counterparts. ANC8+ contact showed a strong impact (10%) compared with ANC4+ contacts (7%) on EPNC. In LMICs, PNC is one of the most underutilized and weakest of all maternal and child health services. The result aligns with previous studies, which highlighted a positive association between ANC8+ visits and early PNC utilization (26, 44). This is probably because frequent contact with healthcare providers throughout the ANC period would create an understanding of the importance of attending early PNC.
Our study has strengths and weaknesses. Among the strengths, we used a large sample and conducted a propensity score matching to reduce selection bias between groups based on observable confounders. This gives better and unbiased estimates of the treatment effects of ANC8+ visits. Even though including women who had given birth within the year prior to the surveys is the strength of this study to reduce recall bias compared with previous studies that included women who had given birth within 5 years prior to the surveys, still recall bias could happen (ANC8+). Among the weaknesses, although PSM removes bias based on observable variables, bias due to unobservable confounders (hidden bias) is not accounted for and could lead to overestimated effects of the treatment on outcome variables. Moreover, important covariates which may directly affect the net impact such as women with a high risk of pregnancy were not included.
Conclusion and recommendation
Our study confirmed that ANC8+ visits significantly increased the likelihood of health facility-based delivery and early PNC utilization in LMICs. Health policymakers and healthcare providers should focus on and target pregnant women to attend adequate ANC visits (according to revised WHO recommendation) as our study indicates that ANC8+ visits significantly improved the chances of subsequent care, particularly the early PNC compared with the ANC4 visits.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: https://dhsprogram.com/data/dataset_admin/index.cfm.
Author contributions
DC: conceptualization. DC, FA, DB, MA, MM, AK, NT, and AA: study design, execution, acquisition of the data, analysis and interpretation, writing, and review and editing. All authors contributed to the article and approved the submitted version.
Acknowledgments
The authors acknowledge the Measure DHS for providing them with the datasets.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2023.1107008/full#supplementary-material
Abbreviations
AOR, adjusted odds ratio; ANC, antenatal care; ANC8+, eight or more antenatal care; DHSs, Demographic and Health Surveys; EPNC, early postnatal care; LMICs, low- and middle-income countries; SDG-3, sustainable development goal 3; WHO, World Health Organization.
References
1. Liu L, Oza S, Hogan D, Perin J, Rudan I, Lawn JE, et al. Global, regional, and national causes of child mortality in 2000–13, with projections to inform post-2015 priorities: an updated systematic analysis. Lancet. (2015) 385:430–40. doi: 10.1016/S0140-6736(14)61698-6
2. World Health Organization. Trends in Maternal Mortality 2000 to 2017: Estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. Geneva: World Health Organization (2019).
3. World Health Organization. Maternal Mortality: Evidence Brief. Geneva: World Health Organization (2019).
4. Fukuda-Parr S. From the millennium development goals to the sustainable development goals: shifts in purpose, concept, and politics of global goal setting for development. Gender Dev. (2016) 24:43–52. doi: 10.1080/13552074.2016.1145895
5. Halkos G, Gkampoura E-C. Where do we stand on the 17 sustainable development goals? An overview on progress. Econ Anal Policy. (2021) 70:94–122. doi: 10.1016/j.eap.2021.02.001
6. Callister LC, Edwards JE. Sustainable development goals and the ongoing process of reducing maternal mortality. J Obstetr Gynecol Neonat Nurs. (2017) 46:e56–64. doi: 10.1016/j.jogn.2016.10.009
7. Griggs D, Nilsson M, Stevance A, McCollum D. A Guide to SDG Interactions: From Science to Implementation. Paris: International Council for Science (2017).
8. Seidman G. Does SDG 3 have an adequate theory of change for improving health systems performance? J Global Health. (2017) 7. doi: 10.7189/jogh.07.010302
9. World Health Organization. WHO Recommendations on Antenatal Care for a Positive Pregnancy Experience. Geneva: World Health Organization (2016).
10. McCauley M, Brown A, Ofosu B, Van Den Broek N. “I just wish it becomes part of routine care”: healthcare providers' knowledge, attitudes and perceptions of screening for maternal mental health during and after pregnancy: a qualitative study. BMC Psychiatry. (2019) 19:1–8. doi: 10.1186/s12888-019-2261-x
11. Agaba P, Misinde C. Predictors of the timing and number of antenatal care visits among unmarried compared to married youth in Uganda between 1995 and 2011. (2020). doi: 10.21203/rs.3.rs-33567/v1
12. Konje ET, Magoma MTN, Hatfield J, Kuhn S, Sauve RS, Dewey DM. Missed opportunities in antenatal care for improving the health of pregnant women and newborns in Geita district, Northwest Tanzania. BMC Pregn Childb. (2018) 18:1–13. doi: 10.1186/s12884-018-2014-8
13. Tekelab T, Chojenta C, Smith R, Loxton D. Factors affecting utilization of antenatal care in Ethiopia: a systematic review and meta-analysis. PLoS ONE. (2019) 14:e0214848. doi: 10.1371/journal.pone.0214848
14. Dixit P, Dwivedi LK, Ram F. Estimating the impact of antenatal care visits on institutional delivery in India: a propensity score matching analysis. (2013). doi: 10.1371/journal.pone.0066175
15. Atuhaire R, Atuhaire LK, Wamala R, Nansubuga E. Interrelationships between early antenatal care, health facility delivery and early postnatal care among women in Uganda: a structural equation analysis. Glob Health Action. (2020) 13:1830463. doi: 10.1080/16549716.2020.1830463
16. World Health Organization. Standards for Improving Quality of Maternal and Newborn Care in Health Facilities. Geneva: WHO (2016).
17. Yoseph M, Abebe SM, Mekonnen FA, Sisay M, Gonete KA. Institutional delivery services utilization and its determinant factors among women who gave birth in the past 24 months in Southwest Ethiopia. BMC Health Serv Res. (2020) 20:1–10. doi: 10.1186/s12913-020-05121-9
18. Ndugga P, Namiyonga NK, Sebuwufu D. Determinants of early postnatal care attendance: analysis of the 2016 Uganda demographic and health survey. BMC Pregn Childb. (2020) 20:1–14. doi: 10.1186/s12884-020-02866-3
19. Kanté AM, Chung CE, Larsen AM, Exavery A, Tani K, Phillips JF. Factors associated with compliance with the recommended frequency of postnatal care services in three rural districts of Tanzania. BMC Pregn Childb. (2015) 15:1–10. doi: 10.1186/s12884-015-0769-8
20. World Health Organization. Trend in Maternal Mortality: 1990 to 2010: WHO, UNICEF, UNFPA and The World Bank Estimates. Geneva: World Health Organization (2012).
21. Gehendra M, Collins A, Kai C, Ali AM, Andrea S, Jill B, et al. Utilization of ANC and PNC services in Nepal: A multivariate analysis based on nepal demographic health survey 2001 and 2006. Am J Health Res. (2015) 3:318–27. doi: 10.11648/j.ajhr.20150306.11
22. Islam MM, Masud MS. Health care seeking behaviour during pregnancy, delivery and the postnatal period in Bangladesh: Assessing the compliance with WHO recommendations. Midwifery. (2018) 63:8–16. doi: 10.1016/j.midw.2018.04.021
23. Ejigu Tafere T, Afework MF, Yalew AW. Antenatal care service quality increases the odds of utilizing institutional delivery in Bahir Dar city administration, North Western Ethiopia: a prospective follow up study. PLoS ONE. (2018) 13:e0192428. doi: 10.1371/journal.pone.0192428
24. Serván-Mori E, Heredia-Pi I, García DC, Nigenda G, Sosa-Rubí SG, Seiglie JA, et al. Assessing the continuum of care for maternal health in Mexico, 1994–2018. Bull World Health Organ. (2021) 99:190. doi: 10.2471/BLT.20.252544
25. Ryan BL, Krishnan RJ, Terry A, Thind A. Do four or more antenatal care visits increase skilled birth attendant use and institutional delivery in Bangladesh? A propensity-score matched analysis. BMC Public Health. (2019) 19:1–6. doi: 10.1186/s12889-019-6945-4
26. Mwebesa E, Kagaayi J, Ssebagereka A, Nakafeero M, Ssenkusu JM, Guwatudde D, et al. Effect of four or more antenatal care visits on facility delivery and early postnatal care services utilization in Uganda: a propensity score matched analysis. BMC Pregn Childb. (2022) 22:1–9. doi: 10.1186/s12884-021-04354-8
27. Odusina EK, Ahinkorah BO, Ameyaw EK, Seidu A-A, Budu E, Zegeye B, et al. Noncompliance with the WHO's recommended eight antenatal care visits among pregnant women in sub-Saharan Africa: a multilevel analysis. Biomed Res Int. (2021) 2021:1–11. doi: 10.1155/2021/6696829
28. Doctor HV, Nkhana-Salimu S, Abdulsalam-Anibilowo M. Health facility delivery in sub-Saharan Africa: successes, challenges, and implications for the 2030 development agenda. BMC Public Health. (2018) 18:1–12. doi: 10.1186/s12889-018-5695-z
29. Tessema ZT, Yazachew L, Tesema GA, Teshale AB. Determinants of postnatal care utilization in sub-Saharan Africa: a meta and multilevel analysis of data from 36 sub-Saharan countries. Ital J Pediatr. (2020) 46:1–11. doi: 10.1186/s13052-020-00944-y
30. Mathers C. Global Strategy for Women's, Children's and Adolescents' Health (2016-2030). World Health Organization (2016). p. 4–103.
31. Guo S, Fraser MW. Propensity Score Analysis: Statistical Methods and Applications. SAGE Publications (2014).
32. Nwagbara UI, Osuala EC, Chireshe R, Babatunde GB, Okeke NO, Opara N, et al. Mapping evidence on factors contributing to maternal and child mortality in sub-Saharan Africa: A scoping review protocol. PLoS ONE. (2022) 17:e0272335. doi: 10.1371/journal.pone.0272335
33. Kalipeni E, Iwelunmor J, Grigsby-Toussaint D. Maternal and Child Health in Africa for Sustainable Development GOALS Beyond 2015. Taylor & Francis (2017). p. 643–7.
34. Tekelab T, Chojenta C, Smith R, Loxton D. The impact of antenatal care on neonatal mortality in sub-Saharan Africa: a systematic review and meta-analysis. PLoS ONE. (2019) 14:e0222566. doi: 10.1371/journal.pone.0222566
35. Nagata C, Yang L, Yamamoto-Hanada K, Mezawa H, Ayabe T, Ishizuka K, et al. Complications and adverse outcomes in pregnancy and childbirth among women who conceived by assisted reproductive technologies: a nationwide birth cohort study of Japan environment and children's study. BMC Pregn Childb. (2019) 19:1–11. doi: 10.1186/s12884-019-2213-y
36. Yoseph S, Dache A, Dona A. Prevalence of early postnatal-care service utilization and its associated factors among mothers in Hawassa Zuria district, Sidama regional State, Ethiopia: a cross-sectional study. Obstetr Gynecol Int. (2021) 2021. doi: 10.1155/2021/5596110
37. Huda TM, Chowdhury M, El Arifeen S, Dibley MJ. Individual and community level factors associated with health facility delivery: a cross sectional multilevel analysis in Bangladesh. PLoS ONE. (2019) 14:e0211113. doi: 10.1371/journal.pone.0211113
38. Geremew AB, Boke MM, Yismaw AE. The effect of antenatal care service utilization on postnatal care service utilization: a systematic review and meta-analysis study. J Pregn. (2020). doi: 10.1155/2020/7363242
39. Grenier L, Suhowatsky S, Kabue MM, Noguchi LM, Mohan D, Karnad SR, et al. Impact of group antenatal care (G-ANC) versus individual antenatal care (ANC) on quality of care, ANC attendance and facility-based delivery: a pragmatic cluster-randomized controlled trial in Kenya and Nigeria. PLoS ONE. (2019) 14:e0222177. doi: 10.1371/journal.pone.0222177
40. Suparmi MI, Lestari H. Health Insurance as a Solution for Barriers to Maternal Healthcare Access in Indonesia. Ethiop J Health Sci. (2019).
41. Pervin J, Moran A, Rahman M, Razzaque A, Sibley L, Streatfield PK, et al. Association of antenatal care with facility delivery and perinatal survival–a population-based study in Bangladesh. BMC Pregn Childb. (2012) 12:1–12. doi: 10.1186/1471-2393-12-111
42. Choe S-A, Kim J, Kim S, Park Y, Kullaya SM, Kim C-Y. Do antenatal care visits always contribute to facility-based delivery in Tanzania? A study of repeated cross-sectional data. Health Policy Plann. (2016) 31:277–84. doi: 10.1093/heapol/czv054
43. Berhan Y, Berhan A. Antenatal care as a means of increasing birth in the health facility and reducing maternal mortality: a systematic review. Ethiop J Health Sci. (2014) 24:93–104. doi: 10.4314/ejhs.v24i0.9S
Keywords: antenatal care, health facility delivery, early PNC, propensity score matching, low- and middle-income countries
Citation: Chilot D, Aragaw FM, Belay DG, Asratie MH, Merid MW, Kibret AA, Teshager NW and Alem AZ (2023) Effectiveness of eight or more antenatal contacts on health facility delivery and early postnatal care in low- and middle-income countries: a propensity score matching. Front. Med. 10:1107008. doi: 10.3389/fmed.2023.1107008
Received: 24 November 2022; Accepted: 30 June 2023;
Published: 21 July 2023.
Edited by:
Ranadip Chowdhury, Society for Applied Studies, IndiaCopyright © 2023 Chilot, Aragaw, Belay, Asratie, Merid, Kibret, Teshager and Alem. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dagmawi Chilot, ZGFnaW1jaGlsb3QyMUBnbWFpbC5jb20=
 Dagmawi Chilot
Dagmawi Chilot Fantu Mamo Aragaw
Fantu Mamo Aragaw Daniel Gashaneh Belay
Daniel Gashaneh Belay Melaku Hunie Asratie
Melaku Hunie Asratie Mehari Woldemariam Merid
Mehari Woldemariam Merid Anteneh Ayelign Kibret
Anteneh Ayelign Kibret Nahom Worku Teshager5
Nahom Worku Teshager5 Adugnaw Zeleke Alem
Adugnaw Zeleke Alem