Abstract
Introduction:
Chronic kidney disease (CKD) is mostly asymptomatic until reaching an advanced stage. Although conditions such as hypertension and diabetes can cause it, CKD can itself lead to secondary hypertension and cardiovascular disease (CVD). Understanding the types and prevalence of associated chronic conditions among CKD patient could help improve screening for early detection and case management.
Methods:
A cross sectional study of 252 CKD patients in Cuttack, Odisha (from the last 4 years CKD data base) was telephonically carried out using a validated Multimorbidity Assessment Questionnaire for Primary Care (MAQ-PC) tool with the help of an android Open Data Kit (ODK). Univariate descriptive analysis was done to determine the socio-demographic distribution of CKD patients. A Cramer’s heat map was generated for showing Cramer’s coefficient value of association of each diseases.
Results:
The mean age of participants was 54.11 (±11.5) years and 83.7% were male. Among the participants, 92.9% had chronic conditions (24.2% with one, 26.2% with two and 42.5% with three or more chronic conditions). Most prevalent chronic conditions were hypertension (48.4%), peptic ulcer disease (29.4%), osteoarthritis (27.8%) and diabetes (13.1%). Hypertension and osteoarthritis were found to be most commonly associated (Cramer’s V coefficient = 0.3).
Conclusion:
Increased vulnerability to chronic conditions among CKD patients make them at higher risk for mortality and compromised quality of life. Regular screening of CKD patient for other chronic conditions (hypertension, diabetes, peptic ulcer disease, osteoarthritis and heart diseases) would help in detecting them early and undertake prompt management. The existing national program could be leveraged to achieve this.
Introduction
Chronic kidney disease (CKD) is defined as a decrease in Glomerular Filtration Rate (GFR) to less than 60 mL/min/1.73m2 for at least 3 months, irrespective of cause (1, 2). It was estimated, around 13% of the world’s population has CKD. Additionally, prevalence estimates imply the problem is 15% greater in low- and middle-income nations compared to high-income ones (3). CKD is mostly asymptomatic until its stage is advanced (4) and so, the documented cases presenting to hospitals represent the tip of the iceberg. As the disease stage progresses, it leads to many complications that include CVD (myocardial infarction, ischemic stroke, peripheral vascular disease, valvular disease and arrhythmias), anemia, bone mineral disease, volume overload and electrolyte imbalances (5). On the other hand, diseases such as hypertension and diabetes mellitus are known risk factors for CKD (6, 7). Hence, CKD is often linked to multimorbidity (3). Multimorbidity is defined as presence of two or more chronic conditions in the same individual at a point in time (8). Research study among older age group (>60 years) has shown multimorbidity to be prevalent in 73.9% of general participants and 86% among participants having CKD (any stage) (9). The presence of multimorbidity especially among CKD patients increases the risk of complications and influences the prognosis greatly leading to longer hospital stays, greater health-care expenses, mortality, polypharmacy and low quality of life (4, 10). Early detection of associated morbidities through detailed evaluation in the community and their prompt management will undoubtedly aid in preventing the potential consequences (10). As in other lower middle income countries (LMICs), multimorbidity has become the norm among Indian adults. Data on the prevalence and pattern of multimorbidity among CKD patients in India, particularly in a rural setting, are nonetheless lacking. Decision-making about the degree of multimorbidity in CKD patients in India is therefore hindered by contradicting clinical guidelines, particularly in a rural setting (11, 12). Because of this, contemporary health care programs urgently need guidance concerning the pattern and prevalence of multimorbidity.
In India, many states have hotspot regions for CKD including Odisha, an Eastern state (13). Badamba and Narasinghpur blocks of Cuttack district, Odisha, are in the limelight for CKD burden for last more than a decade and have brought the attention of researchers, program implementers and policy makers to prevent and control it (14). With this backdrop, a research study was carried out to determine prevalence of multimorbidity among CKD patients and explore the pattern of chronic conditions among CKD population of the said areas. This will primarily aid policy makers in identifying which other disease areas’ recommendations should be taken into account when incorporating renal disease recommendations. This study was done through Model Rural Health Research Unit (MRHRU) established in the catchment area of this CKD hotspot.
Materials and methods
A cross-sectional study was conducted among the diagnosed CKD patient in the catchment area of MRHRU at Tigiria, a block of Cuttack district, Odisha. Under the study, a total of 674 CKD patients diagnosed between (January 2017–January 2021) were line listed after collecting data from the healthcare management information system (HMIS) database of community health centers of both the study blocks. Among all the patients, 97 were deceased, 99 were bed ridden and 221 could not be contacted (incorrect phone number). Finally, among the 257 CKD patients contacted for the study, 5 declined to participate, and a total of 252 interested participants who verbally consented for the study were enrolled, with a non-response rate of 1.95%.
Data collection tool
A standardized structured schedule ‘Multimorbidity Assessment Questionnaire for Primary Care (MAQ-PC)’ was used for data collection. This is a validated tool for community based assessment of multimorbidity (15). Additionally, socio-demographic information was collected using a standardized tool. Considering the COVID-19 pandemic related restrictions during the study period, data were collected telephonically by the trained field investigators using an android based Open Data Kit (ODK) platform.
Statistical analysis
Univariate descriptive analysis was done to determine the socio-demographic distribution of CKD patients tabulated by n (%) and confidence interval. To assess the distribution of associated disease with number of chronic conditions, a bivariate descriptive table was presented with n (%). A Cramer’s heat map was generated by estimating Cramer’s V coefficient value by using R studio 2021.09.1 to assess the association between diseases among participants having two or more chronic conditions other than CKD.
Results
The mean age of the study participants was 54.11 (±11.57) years, ranging from20 to 86 years. While 52.4% were in the (40–59) age group, 37.7% were 60 or above and 9.9% were in the 20-39 age group. The majority (83.7%) were male, 97.6% of participants were Hindus and 91.5% were married. While most of the participants (88.2%) were from rural villages, 84.9% of participants were literate,69.1% of participants belonged to below poverty line (BPL) and 44.1% had monthly family income less than 6,000 Indian rupees. The detailed socio-demographic distribution of study participants is presented in Table 1.
Table 1
| Socio-demographic characteristics | Participant (N = 252) n (%) |
95% Confidence interval |
|---|---|---|
| Age group | ||
| 20–39 | 25 (9.92%) | (6.52–14.29%) |
| 40–59 | 132 (52.38%) | (46.01–58.68%) |
| 60 above | 95 (37.70%) | (31.69–43.99%) |
| Gender | ||
| Male | 211 (83.73%) | (23.25–78.58%) |
| Female | 40 (15.94%) | (11.58–20.98%) |
| Religion | ||
| Hindu | 245 (97.61%) | (94.36–98.87%) |
| Islam | 6 (2.39%) | (0.87–5.11%) |
| Marital status | ||
| Currently married | 226 (91.50%) | (87.29–94.66%) |
| Never married | 11 (4.45%) | (2.24–7.82%) |
| Widow/Widower | 10 (4.05%) | (1.95–7.31%) |
| Ethnicity | ||
| General | 76 (30.77%) | (25.07–36.93%) |
| OBC | 111 (44.94%) | (38.62–51.37%) |
| Other | 60 (24.29%) | (19.07–30.13%) |
| Residence | ||
| Urban | 29 (11.84%) | (8.07–16.55%) |
| Rural | 216 (88.16%) | (83.44–91.92%) |
| Education | ||
| Illiterate | 36 (15.13%) | (10.82–20.32%) |
| Literate | 202 (84.87%) | (79.67–89.17%) |
| House type | ||
| Kutcha | 58 (24.37%) | (19.05–30.33%) |
| Pucca | 94 (39.50%) | (33.24–46.01%) |
| Semi pucca | 86 (36.13%) | (30.02–42.59%) |
| Monthly family income | ||
| Below 6,000 | 101 (44.10%) | (37.56–50.79%) |
| Above 6,000 | 128 (55.90%) | (49.20–62.43%) |
| Poverty status | ||
| Above poverty line (APL) | 73 (30.93%) | (25.09–37.25%) |
| Below poverty line (BPL) | 163 (69.07%) | (62.74–74.90%) |
Distribution of participants according to socio-demographic characteristics.
Among 252 study participants, 234 (92.9%) had other chronic conditions apart from CKD (multimorbidity). Upon analyzing for the number of chronic conditions associated at the individual level, 18 (7.1%) had no other chronic condition, 61 (24.2%) had one additional chronic condition, 66 (26.2%) had two additional chronic conditions and 107 (42.5%) had three or more additional chronic conditions among CKD patients. The distribution of number of associated chronic conditions is presented in Figure 1.
Figure 1
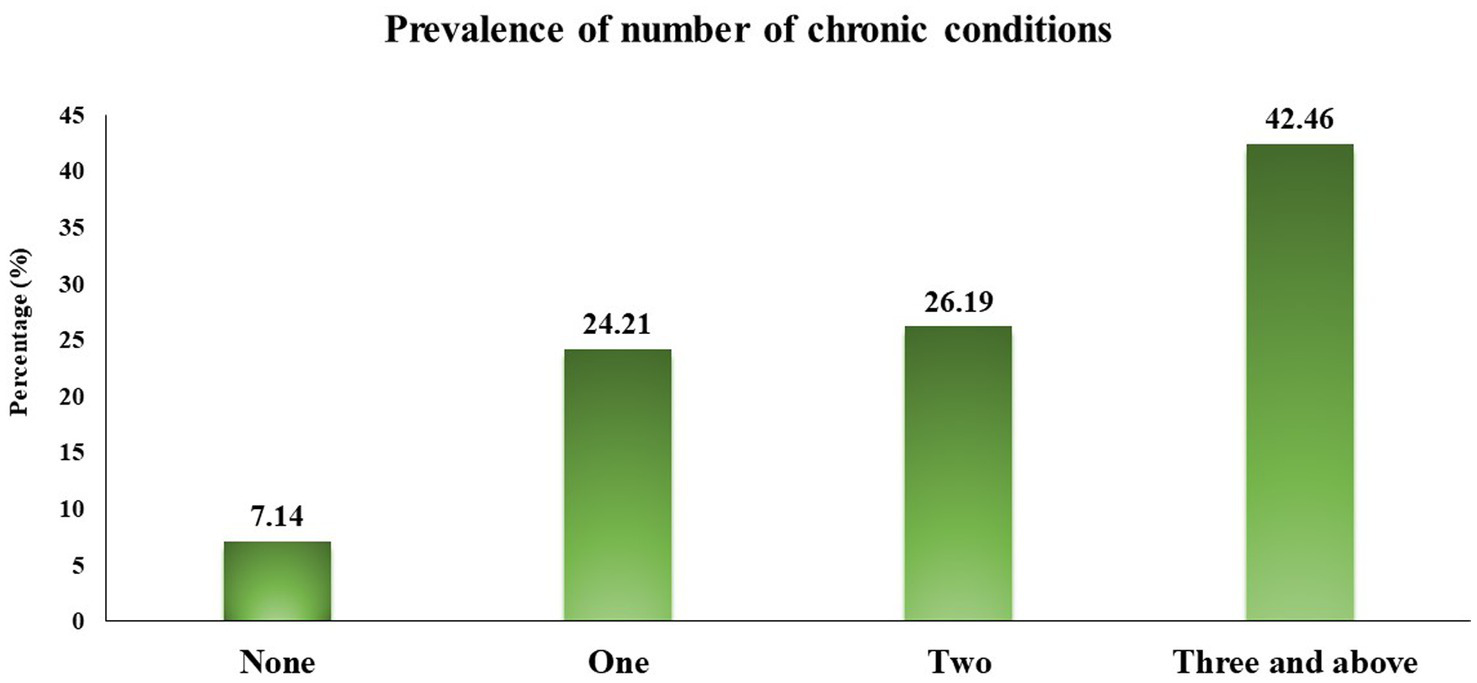
Distribution of number of other chronic conditions among participants.
Among the participants with multimorbidity, the major associated disease conditions included hypertension (48.41%), peptic ulcer disease (29.4%), osteoarthritis (27.8%) and diabetes mellitus (13.1%). The prevalence of different chronic conditions among CKD patients is depicted in Figure 2.
Figure 2
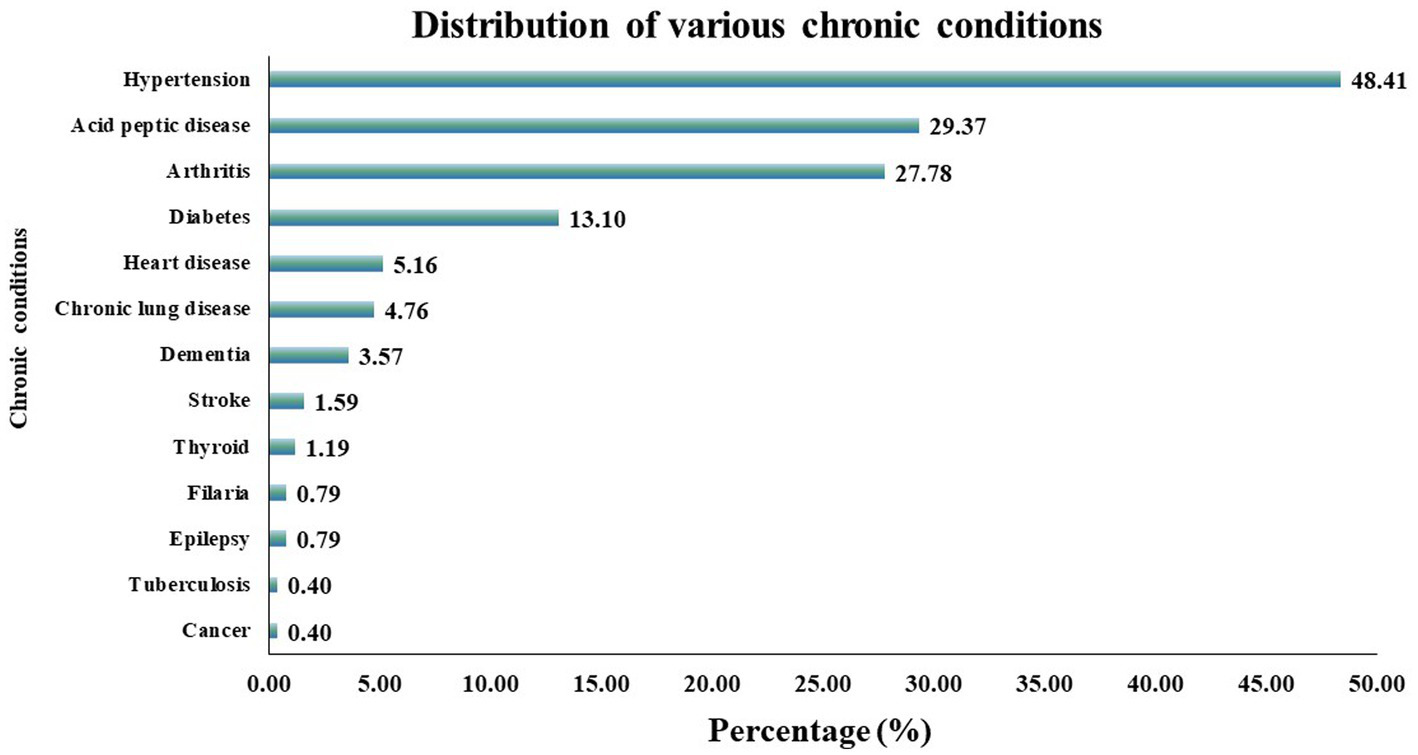
Prevalence of various chronic conditions among CKD participants with Multimorbidity.
Upon further analysis of the associated morbidities according to number of chronic conditions among the participants with multimorbidity, a total of 346 co-morbid conditions were identified. Out of those, 15 (4.3%) were among participants having one additional chronic condition, 68 (19.6%) were among participants having two additional chronic conditions and 263 (76%) were among participants having three or more additional chronic conditions.
Among participants having one associated chronic condition, hypertension and peptic ulcer disease were the major associated conditions. Among participants with two associated morbidities, hypertension, osteoarthritis and peptic ulcer disease were the major conditions. Among participants with three or more additional comorbidities, hypertension, peptic ulcer disease, osteoarthritis and diabetes mellitus were the major associated conditions. The detailed distribution of chronic conditions is presented in Table 2.
Table 2
| Chronic conditions | None or One comorbidity | Two comorbidities | Three and above comorbidities |
|---|---|---|---|
| Hypertension | 7 (46.7%) | 28 (41.2%) | 87 (33.1%) |
| Acid peptic | 4 (26.7%) | 11 (16.2%) | 59 (22.4%) |
| Osteoarthritis | 1 (6.7%) | 21 (30.9%) | 48 (18.2%) |
| Diabetes mellitus | 2 (13.3%) | 3 (4.4%) | 28 (10.6%) |
| Heart disease | 1 (6.7%) | 1 (1.5%) | 11 (4.2%) |
| Chronic lung disease | 0 | 2 (2.9%) | 10 (3.8%) |
| Dementia | 0 | 0 | 9 (3.4%) |
| Stroke | 0 | 0 | 4 (1.5%) |
| Thyroid | 0 | 0 | 3 (1.1%) |
| Filaria | 0 | 0 | 2 (0.8%) |
| Epilepsy | 0 | 0 | 2 (0.8%) |
| Tuberculosis | 0 | 1 (1.5%) | 0 |
| Cancer | 0 | 1 (1.5%) | 0 |
| Total | 15 (4.3%) | 68 (19.7%) | 263 (76%) |
Distributions of number of associated disease conditions according to presence of number of chronic conditions.
We further analyzed the co-occurrence of different diseases among the study participants having two and more additional chronic conditions. To find out this association between diseases, the eight most prevalent chronic conditions were considered to run a Cramer heat map (refer to Figure 2; Table 2). Cramer’s V coefficient lies between 0 and 1, where 0 indicates no association between diseases and 1 indicates a perfect strong association between the diseases. The highest crammer’s V coefficient value (0.3) was between hypertension and osteoarthritis. Crammer’s V coefficient value of 0.2 was observed between diabetes mellitus and peptic ulcer disease, chronic backache and osteoarthritis, osteoarthritis and peptic ulcer disease, and diabetes mellitus and dementia. Among other diseases, the Crammer’s V coefficient value was either 0.1 or 0. The association between morbidities is depicted in Figure 3 below.
Figure 3
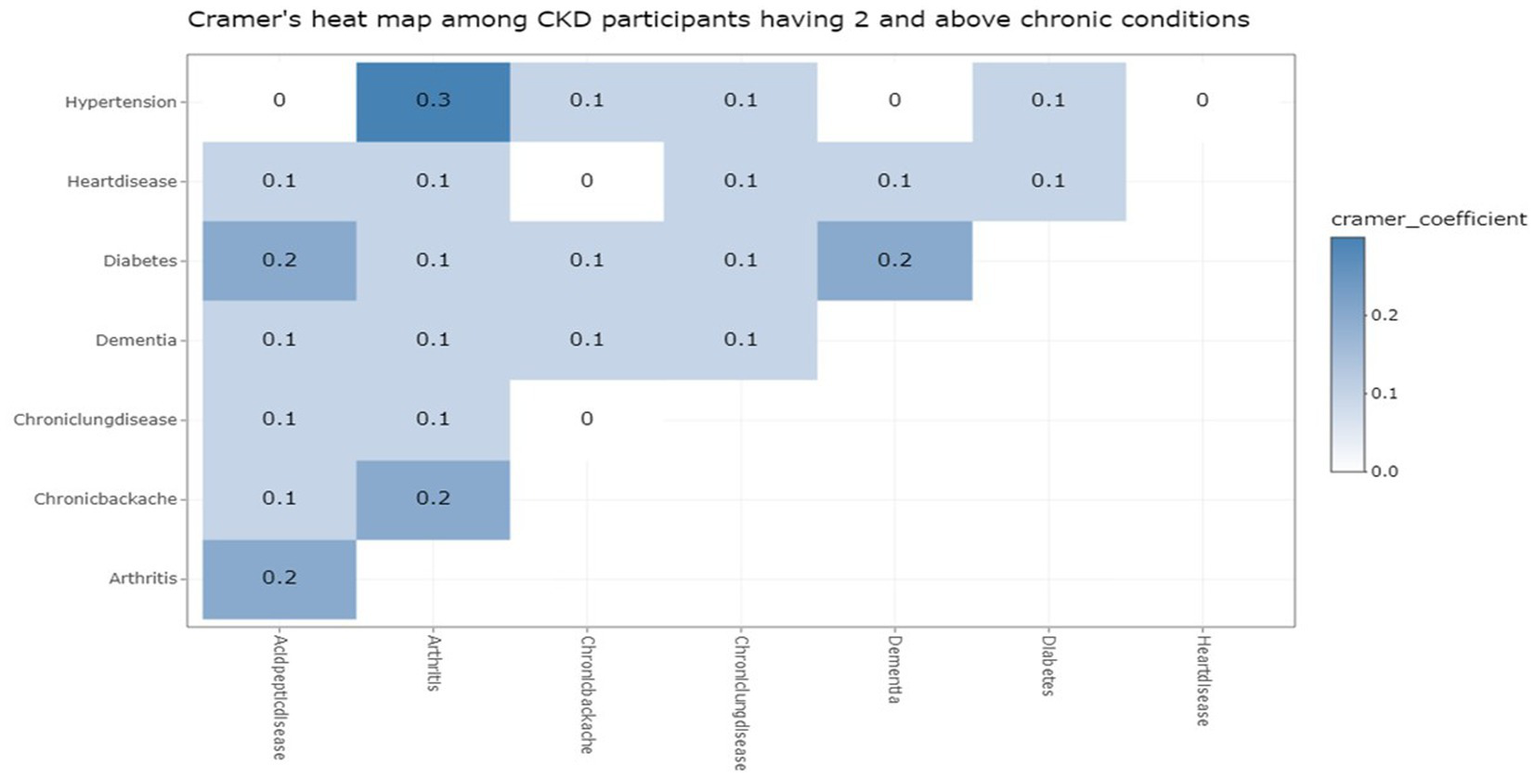
Crammer’s heat map showing the association between chronic conditions.
Discussion
With improved life expectancy, aging people are also at increased risk for chronic illnesses such as hypertension, diabetes mellitus, cancer, chronic kidney disease and mental health problems (16). In addition to aging, unhealthy lifestyles and unplanned exposure to urban environments attribute to the occurrence of non-communicable diseases (17). Due to limited research studies on multimorbidity among CKD patients, the present study has explored the prevalence of other chronic conditions among CKD patients in the hotspot area of Odisha, Eastern India. Additionally, we assessed the pattern of other chronic conditions among CKD patients.
CKD patients have a high prevalence of multimorbidity because CKD is a systemic disorder. In our study, we found that the majority of participants had two or more other chronic conditions in addition to CKD. This finding is supported by a study conducted in the UK with 1741 participants, which revealed that the majority of participants had two or more chronic conditions in addition to CKD (18). Our study also showed that about one-fifth of the participants had one or more other chronic conditions in addition to CKD, which is supported by a study among primary care patients that found 26 and 29% of all participants had one and two other chronic conditions, respectively, in addition to CKD (18). As the kidneys are responsible for filtering waste products, electrolyte balance, and important endocrine system functions, progression of CKD can cause toxin accumulation, electrolyte imbalances, and certain endocrine dysfunctions. As a result, CKD progression can cause disruptions to numerous metabolic pathways. While the sodium dysregulation, increased sympathetic nervous system, and alterations in the renin-angiotensin aldosterone system caused by CKD have primarily been associated with hypertension (19), these pathologic conditions could lead to the occurrence of other chronic diseases.
The presence of additional chronic conditions leads to an increased risk of mortality and a poor quality of life (18). The most prevalent associated disease conditions that we found were hypertension followed by peptic ulcer disease, osteoarthritis and diabetes mellitus. This finding was also reflected by a community based study from North Kerala which found the chronic conditions among CKD patient include hypertension (61.4%), diabetes (47.3%), cardiovascular disease (30.6%), chronic obstructive pulmonary disease (10%), malignancies (2.6%), and retinopathy (28%) (20). Both Studies found that hypertension is the most common co-morbid condition, and this correlates with the pathophysiology of CKD-associated hypertension where renin-angiotensin-aldosterone system (RAAS) over expression accompanied by eGFR reduction results in sodium and water retention (19).
Whereas CKD is an attributing factor for many other non-communicable diseases such as cardiovascular diseases, hypertension, anemia, bone mineral, volume overload and electrolyte imbalances (5), diseases such as hypertension and diabetes mellitus are risk factors for CKD (8). In addition, studies have shown that consumption of NSAIDs is another important CKD risk factor (21). Patients suffering from osteoarthritis often take pain medicines such as non-steroidal anti-inflammatory drugs (NSAIDs). Also, these drugs cause peptic ulcer diseases (22, 23). In this context, we also observed a higher association between hypertension and osteoarthritis, diabetes and peptic ulcer disease, and osteoarthritis and peptic ulcer disease. This clearly indicates that CKD patients are more vulnerable for having multimorbidity because of the risk factors involved, nature and complications of the disease, and the medications prescribed and consumed.
Conclusion
In view of increased vulnerability for different chronic conditions among CKD patients leading to their higher risk of mortality and morbidity, it is critically important to regularly screen the CKD patient for hypertension, diabetes, peptic ulcer disease, osteoarthritis and heart diseases especially in CKD hotspot areas. Early detection of these chronic conditions and their prompt management could help in improving their quality of life and mortality. The current national program for prevention and control of cancer, diabetes mellitus, CVD and stroke (NPCDCS) through established health and wellness centers could be leveraged for this purpose.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Statements
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by ICMR-Regional Medical Research Centre, Institutional Human Ethics Committee. Written informed consent to participate in this study was provided by the participants'.
Author contributions
SKP, SP, DS, SN, and SRN: conceptualization, design of the study, acquisition, and writing original draft. SRN, DS, SN, AM, and AS: data collection, data curation, statistical analysis, and writing original draft. SKP, DS, PD, and SP: intellectual content, study supervision, critical review, and draft editing. SKP, SRN, DS, SN, AM, AS, PD, and SP: integrity of any part of the work are appropriately investigated and resolved. All authors approved the final draft.
Acknowledgments
The authors are thankful to all staffs of Model Rural Health Research Unit for all supports.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1.
Glynn LG Buckley B Reddan D Newell J Hinde J Dinneen SF et al . Multimorbidity and risk among patients with established cardiovascular disease: a cohort study. Br J Gen Pract. (2008) 58:488–94. doi: 10.3399/bjgp08X319459
2.
Hirst JA Ordóñez Mena JM O’Callaghan CA Ogburn E Taylor CJ Yang Y et al . Prevalence and factors associated with multimorbidity among primary care patients with decreased renal function. PLoS One. (2021) 16:e0245131. doi: 10.1371/journal.pone.0245131
3.
Coresh J . Update on the burden of CKD. J Am Soc Nephrol JASN. (2017) 28:1020–2. doi: 10.1681/ASN.2016121374
4.
Zeba Z Fatema K Sumit AF Zinnat R Ali L . Early screening of chronic kidney disease patients among the asymptomatic adult population in Bangladesh. J Prev Epidemiol. (2020) 5:e10. doi: 10.34172/jpe.2020.10
5.
Go AS Chertow GM Fan D McCulloch CE Hsu C . Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. (2004) 41:177–305. doi: 10.1016/j.jvs.2004.10.020
6.
Hannan M Ansari S Meza N Anderson AH Srivastava A Waikar S et al . Risk factors for CKD progression: overview of findings from the CRIC study. Clin J Am Soc Nephrol CJASN. (2021) 16:648–59. doi: 10.2215/CJN.07830520
7.
Wang F He K Wang J Zhao M-H Li Y Zhang L et al . Prevalence and risk factors for CKD: a comparison between the adult populations in China and the United States. Kidney Int Rep. (2018) 3:1135–43. doi: 10.1016/j.ekir.2018.05.011
8.
Ene-Iordache B Perico N Bikbov B Carminati S Remuzzi A Perna A et al . Chronic kidney disease and cardiovascular risk in six regions of the world (ISN-KDDC): a cross-sectional study. Lancet Glob Health. (2016) 4:e307–19. doi: 10.1016/S2214-109X(16)00071-1
9.
ShariffGhazali S Seman Z Zainuddin NH Omar MA Sooryanarayana R Ariaratnam S et al . Prevalence and factors associated with multimorbidity among older adults in Malaysia: a population-based cross-sectional study. BMJ Open. (2021) 11:e052126. doi: 10.1136/bmjopen-2021-052126
10.
Sullivan MK Rankin AJ Jani BD Mair FS Mark PB . Associations between multimorbidity and adverse clinical outcomes in patients with chronic kidney disease: a systematic review and meta-analysis. BMJ Open. (2020) 10:e038401. doi: 10.1136/bmjopen-2020-038401
11.
Kernick D Chew-Graham CA O'Flynn N . Clinical assessment and management of multimorbidity: NICE guideline. Br J Gen Pract. (2017) 67:235–6. doi: 10.3399/bjgp17x690857
12.
Grover S . Multimorbidity in the elderly: are we prepared for it!J Geriatric Mental Health. (2019) 6:35. doi: 10.4103/jgmh.jgmh_1_20
13.
Mohanty NK Sahoo KC Pati S Sahu AK Mohanty R . Prevalence of chronic kidney disease in Cuttack District of Odisha, India. Int J Environ Res Public Health. (2020) 17:E456. doi: 10.3390/ijerph17020456
14.
CKD . Establishing a Chronic Kidney Disease (CKD) Surveillance in Cuttack District, Odisha, India. Indian J Public Health Res Dev. (2021). Available at: http://medicopublication.com/index.php/ijphrd/article/view/16563 (Accessed March 24, 2022)
15.
Pati S Swain S Metsemakers J Knottnerus JA van den Akker M . Pattern and severity of multimorbidity among patients attending primary care settings in Odisha, India. PloS One. (2017) 12:e0183966. doi: 10.1371/journal.pone.0183966
16.
The Academy of Medical Sciences . (2018). Multimorbidity: A priority for global health research. UK Academy of Medical Sciences. Available at: https://acmedsci.ac.uk/file-download/82222577 (Accessed April 20, 2022).
17.
Kanungo S Bhowmik K Mahapatra T Mahapatra S Bhadra UK Sarkar K . Perceived morbidity, healthcare-seeking behavior and their determinants in a poor-resource setting: observation from India. PLoS ONE. (2015) 10:e0125865. doi: 10.1371/journal.pone.0125865
18.
Fraser SDS Roderick PJ May CR McIntyre N McIntyre C Fluck RJ et al . The burden of comorbidity in people with chronic kidney disease stage 3: a cohort study. BMC Nephrol. (2015) 16:193. doi: 10.1186/s12882-015-0189-z
19.
Hamrahian SM Falkner B . Hypertension in chronic kidney disease. Adv Exp Med Biol. (2017) 956:307–25. doi: 10.1007/5584_2016_84
20.
Jacob SR Raveendran R Kannan S . Causes, comorbidities and current status of chronic kidney disease: a community perspective from North Kerala. J Fam Med Prim Care. (2019) 8:2859–63. doi: 10.4103/jfmpc.jfmpc_478_19
21.
Gooch K Culleton BF Manns BJ Zhang J Alfonso H Tonelli M et al . NSAID use and progression of chronic kidney disease. Am J Med. (2007) 120:280.e1–7. doi: 10.1016/j.amjmed.2006.02.015
22.
Drini M . Peptic ulcer disease and non-steroidal anti-inflammatory drugs. Aust Prescr. (2017) 40:37. doi: 10.18773/austprescr.2017.037
23.
Matsui H Shimokawa O Kaneko T Nagano Y Rai K Hyodo I . The pathophysiology of non-steroidal anti-inflammatory drug (NSAID)-induced mucosal injuries in stomach and small intestine. J Clin Bio Chem Nutr. (2011) 48:107–11. doi: 10.3164/jcbn.10-79
Summary
Keywords
CKD, multimorbidity, GFR, chronic conditions, Cramer’s coefficient
Citation
Palo SK, Nayak SR, Sahoo D, Nayak S, Mohapatra AK, Sahoo A, Dash P and Pati S (2023) Prevalence and pattern of multimorbidity among chronic kidney disease patients: a community study in chronic kidney disease hotspot area of Eastern India. Front. Med. 10:1131900. doi: 10.3389/fmed.2023.1131900
Received
26 December 2022
Accepted
27 April 2023
Published
12 May 2023
Volume
10 - 2023
Edited by
Frank A. Orlando, University of Florida, United States
Reviewed by
Rohan Mehta, University of Florida, United States; Nivedita Kamath, St. John’s Medical College Hospital, India
Updates
Copyright
© 2023 Palo, Nayak, Sahoo, Nayak, Mohapatra, Sahoo, Dash and Pati.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Subrata Kumar Palo, drpalsubrat@gmail.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.