- 1Department of Endocrinology and Metabolism, West China Hospital, Sichuan University, Chengdu, Sichuan, China
- 2General Practice Ward/International Medical Center Ward, General Practice Medical Center, National Clinical Research Center for Geriatrics, Multimorbidity Laboratory, West China Hospital, Sichuan University, Chengdu, Sichuan, China
- 3West China School of Public Health and West China Fourth Hospital, Sichuan University, Chengdu, Sichuan, China
- 4Department of General Practice, People’s Hospital of Lhasa, Lhasa, Tibet, China
Objectives: This study aimed to assess the knowledge and awareness of nicotine, nicotine replacement therapy (NRT), and electronic cigarettes (e-cigarettes) among general practitioners with a special interest (GPwSIs) in respiratory medicine.
Methods: A cross-sectional study was conducted from October 2021 to February 2022. Knowledge and awareness were compared among smokers and non-smokers, as well as different age and gender groups.
Results: The study consisted of 102 GPwSIs from 21 cities in Sichuan Province, China. Most respondents would recommend NRT for long-term use. Only a few believed that e-cigarettes are an effective means of smoking cessation and 71.6% would not recommend e-cigarettes as a substitute for cigarettes to their patients. Additionally, the majority did not regularly provide extensive help to assist patients in quitting smoking and needed smoking cessation counseling training.
Conclusion: GPwSIs in respiratory medicine in China could have a relatively low level of knowledge and awareness regarding nicotine, NRT, and e-cigarettes. The study highlights the need for smoking cessation training among GPwSIs to improve their knowledge and provide better assistance to patients who want to quit smoking.
Introduction
Tobacco use poses a significant threat to public health worldwide, with smoking causing over 8 million deaths annually, surpassing the combined deaths caused by diseases such as HIV, tuberculosis, and malaria (1). Numerous studies have shown that smoking is strongly linked to chronic diseases such as cardiovascular and respiratory diseases, as well as cancer (2–5). China, a significant contributor to global tobacco production and consumption, is a critical focal point in addressing this health crisis (6). In 2018, the Chinese Center for Disease Control and Prevention conducted a large-scale survey that revealed a smoking prevalence rate of 26.6% among individuals aged 15 and above, which was only slightly lower than the rate of 28.3% reported in 2010 (6). Despite the government’s efforts to promote smoking control policies over the last decade, these figures indicate that a significant number of people in China still engage in smoking (6, 7).
Quitting smoking is considered one of the most effective interventions for promoting health (8). In response to the addictive mechanism of nicotine, various strategies for treating tobacco dependence have been continuously developed and applied, divided into pharmacological interventions and non-pharmacological interventions based on whether drugs are used for withdrawal (9). Nicotine replacement therapy (NRT) is the most widely used pharmacological intervention include nicotine patches, gum, lozenges, inhalers, and nasal sprays (10). The effectiveness of NRT has been validated through multiple clinical trials, which show that NRT can enhance the success rates of smoking cessation. In addition, some drugs are also applied for smoking cessation, such as varenicline, bupropion and cytisine, whose mechanisms of action are similar to NRT (11). Research on e-cigarettes as a tool for reducing nicotine addiction is ongoing, but there is emerging evidence suggesting that they help aid smoking cessation (12, 13). Notably, a study comparing e-cigarettes with NRT found a higher 1-year abstinence rate in the e-cigarette group (18.0%) compared to the nicotine-replacement group (9.9%) (14).
General practitioners (GPs) are of essence in providing appropriate advice and guidance to smokers. The existing evidence indicates that GPs’ knowledge and beliefs about smoking and nicotine may not always be accurate or grounded in scientific evidence (15). Compared to smoking, many GPs overestimate the adverse effects of smokeless tobacco (snus) (16) and NRT (17). For example, a study of GPs in the UK and Sweden found that around 40 per cent of the participants mistakenly believed that nicotine was the primary or second most significant contributor to smoking-related illnesses (18). This misconception can affect the management of smokers, preventing them from using nicotine-based products or other alternatives that are less harmful than smoking.
GPs with a Special Interest (GPwSI) are GPs who have acquired additional training and expertise in a specific clinical area, allowing them to take referrals for specialized cases or provide enhanced services for certain conditions or patient groups (19). The prerequisite for GPwSI to effectively counsel smokers relies on appropriate education and understanding about the impact of smoking on health, as well as all available methods and products that help reduce or quit smoking (20). To our knowledge, there is no study reported from China on this subject. This study aims to assess the knowledge and awareness of GPwSI in respiratory medicine regarding nicotine, NRT, and e-cigarettes.
Methods
Population and sample
This cross-sectional study was conducted between October 2021 and February 2022. The population of GPwSI in respiratory medicine is relatively small and obtaining a random sample is difficult in China (21). Therefore, a convenient sampling technique was used to recruit GPwSIs in respiratory medicine for an online survey, through the Western General Practice Network, which includes GPs from primary healthcare settings across Sichuan Province. The sample size was calculated using the online sample size calculator RaoSoft ®. The minimum effective sample for this study was n = 97 with a 5% margin error, a confidence interval of 90%, response rate 10% and the total number of general practitioners in Sichuan was 10,394.
Eligible participants for this study were GPs who (1) currently practiced in the registered healthcare facilities at all levels located in Sichuan, China; (2) completed one of the following training programs: a specialty training program in respiratory medicine, academic education in respiratory medicine, or continuing education in respiratory medicine; (3) independently practiced in general practice outpatient clinics; (4) consented to the survey. Excluded practitioners were those who held part-time positions in pharmaceutical companies related to the sales of cessation medications agents.
Questionnaire design
The questionnaire was designed based on the previous literature (12, 20, 22, 23). In order to enhance the questionnaire’s design and readability, three healthcare professionals were recruited for modification, including two respiratory physicians, a general practitioner. Before the survey, we conducted a small-scale pilot survey, and a total of 20 pilot survey questionnaires were distributed. Feedback from the pilot questionnaire was used to refine the questionnaire for the survey. The researchers created a questionnaire and uploaded it to an online survey tool.1 The questionnaire consisted of five main sections, including: (1) demographic and professional characteristics of the participants, such as age, gender, professional title, highest education level, and hospital type; (2) a health risks score for smoking products measured through ‘Unfamiliar’ responses and Likert-type scales, ranging from 1 (low risk) to 5 (high risk); (3) knowledge and attitudes toward nicotine replacement therapy and electronic cigarettes; (4) awareness of the effects of nicotine on smoking-related diseases measured through ‘Unfamiliar’ responses and Likert-type scales, ranging from 1 (low risk) to 5 (high risk); and (5) confidence in providing smoking cessation services, as well as smoking cessation training needs.
With regard to nicotine, the main objective of the questionnaire was to assess its perceived contribution to smoking-related lung cancer and other organ tumors. For NRT, the questions mainly focused on the dosage selection, willingness to recommend long-term use as a smoking substitute, safety compared to tobacco cigarettes and e-cigarettes, and addictiveness compared to e-cigarettes. As e-cigarettes involved novel products, our goal was to assess whether GPwSIs would recommend e-cigarettes as a smoking cessation aid for those who could not or were unwilling to use other methods, as well as evaluate e-cigarettes addictiveness and safety. Finally, participants were asked to report their confidence in their own smoking cessation service capabilities. The survey questionnaire can be found in the Supplementary material (Additional file 1).
Quality control
To ensure the data credibility, quality control measures were implemented. Participants were only allowed to submit their responses once and were unable to make any changes after submitting. All survey items were required to be completed upon submission. Survey data containing logical errors were checked.
Ethics statement
This study was approved by the ethical committee, West China Hospital of Sichuan University, Chengdu, China (No. 2021–1745). All participants were informed about the study’s purpose, and they were assured that their data would remain anonymous and confidential.
Statistical analysis
Descriptive analysis was utilized to characterize the data. Categorical variables were presented as numerical values (%). Differences between categorical variables were assessed using chi-square (χ2) or Fisher’s exact tests. All statistical tests were two-tailed, and differences were deemed statistically significant when p ≤ 0.05. All analyses were performed in SPSS (SPSS version 22, SPSS, Inc., Chicago).
Results
Descriptive analysis of the study sample
The descriptive analysis results of the entire study sample are shown in Table 1. A total of 102 GPwSIs in respiratory medicine from 21 cities in Sichuan Province participated in this study. Approximately half were female (49.0%), and the majority aged between 40 and 49 years old (54.9%). The participants had either a bachelor degree (60.8%) or an associate degree (39.2%), with no master or above degree, and most held intermediate professional titles (68.6%). Seventy-eight point 4% of the participants were from tertiary hospitals. Eighteen participants were current smokers, eight past smokers, and seventy-six non-smokers. About half of the GPwSIs reported that they often asked patients about their smoking status, but most did not regularly provide extensive help to assist patients in quitting smoking. Only a small number of participants helped patients quit smoking by means of oral smoking cessation medication (6.9%) or NRT (20.6%). Five point 9% of the participants believed they were fully prepared to provide smoking cessation counseling, while 94.1% believed they needed to receive smoking cessation counseling training.
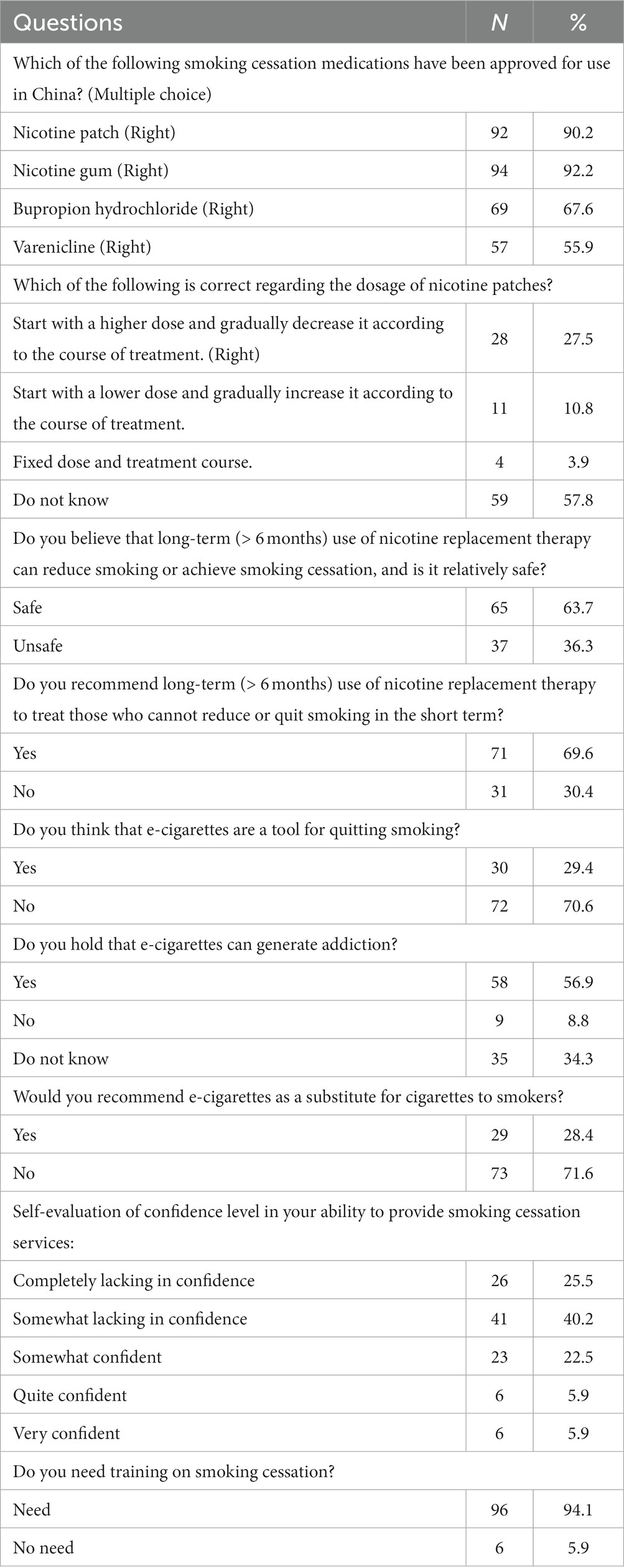
Beliefs and attitudes toward nicotine, NRT and e-cigarettes
The responses of GPwSIs to nicotine, NRT and e-cigarettes are shown in Table 2. When asked about the smoking cessation drugs approved for use in China, the majority knew about nicotine patch (90.2%) and nicotine gum (92.2%). Regarding the dosage and usage of nicotine patches, only 27.5% of the respondents knew that a higher dose should be used initially and gradually reduced according to the course of treatment. More than half of the respondents believed that long-term (more than 6 months) use of NRT to reduce or quit smoking was safe. Over half of the participants would recommend long-term (more than 6 months) use of NRT to treat those who could not reduce or quit smoking in the short term. The correct dosage of nicotine patches typically starts with the highest dose patch that a smoker can use based on their daily smoking volume. The dosage is then gradually reduced over a period of 8 to 12 weeks, to wean the smoker off nicotine dependence. Significant differences in knowledge regarding the correct dosage and usage of nicotine patches were found between smokers (current and past) and non-smokers (p < 0.05) (Supplementary Tables S1).
Regarding e-cigarette, 29.4% of the respondents believed that they were an effective tool for quitting smoking. More than half (56.9%) agreed that e-cigarettes could lead to addiction, and 34.3% were not aware of the addiction of e-cigarettes. A significant proportion of respondents (71.6%) stated that they would not recommend e-cigarettes as a substitute for cigarettes to their patients. Most lacked confidence in their counseling ability associated with smoking cessation service.
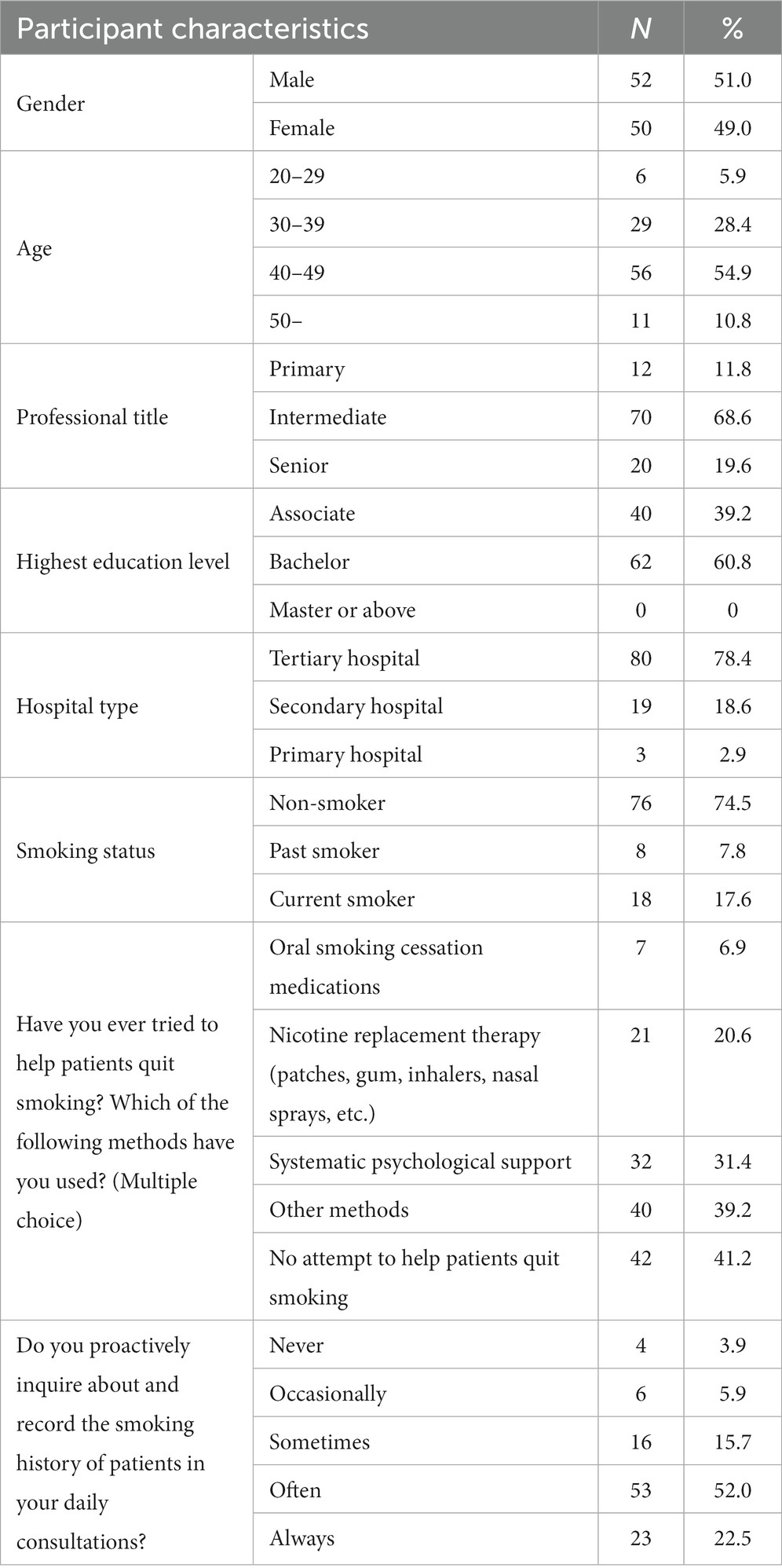
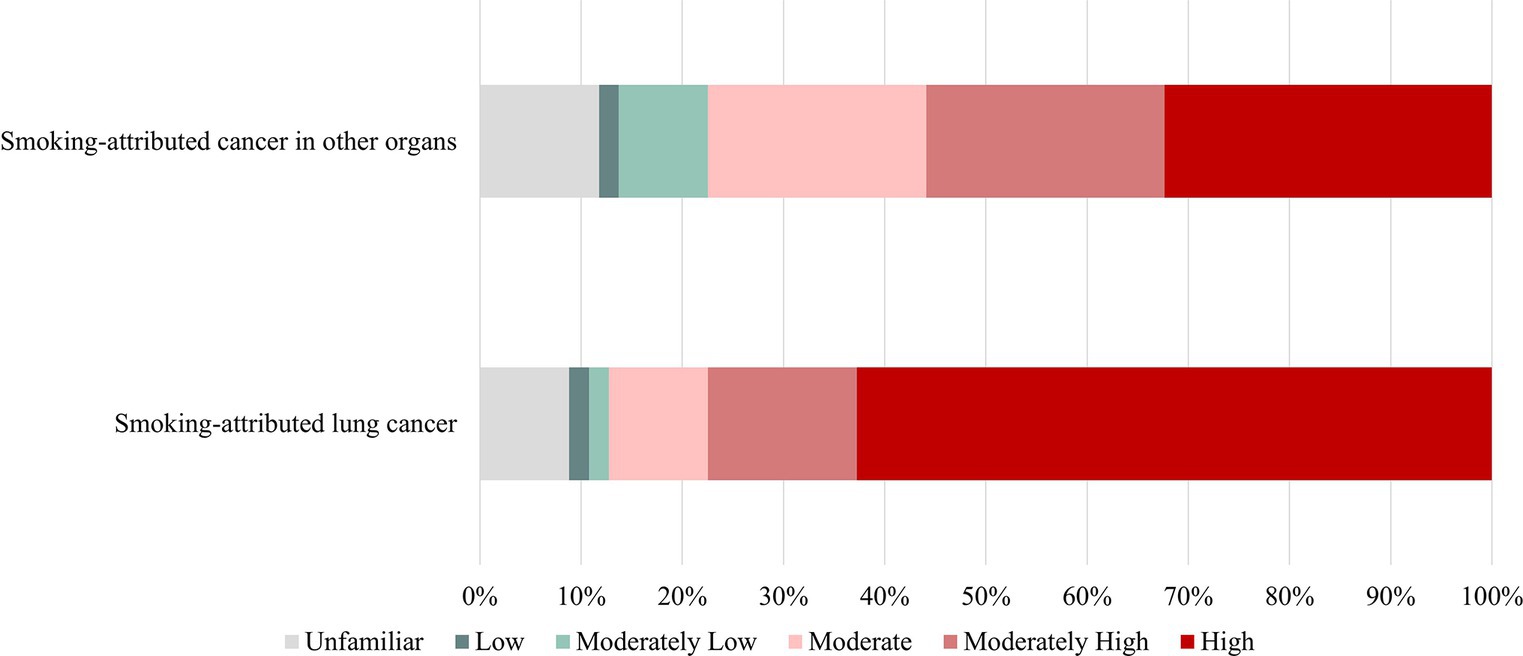
The participants were requested to assess the level of risk associated with tobacco cigarettes and various substitute products, which included e-cigarettes, NRT such as nicotine patches and gum, as well as oral cessation medications like bupropion and varenicline. According to the survey, 54.9% of the respondents considered tobacco cigarettes to pose a moderately high or high health risk, while the figures for e-cigarettes, NRT, and oral cessation medications were 32.4, 7.8, and 8.8%, respectively. On the other hand, 21.6% lack awareness of the health risks associated with cigarettes, while 25.5% are unaware of the harm that e-cigarettes can pose to health. Additionally, 35.3% of people do not have knowledge about the health risks of NRT, and 34.3% are not aware of the potential health risks associated with oral smoking cessation medications. Five individuals believed that smoking had a low health risk. Regarding e-cigarettes, respondents’ ratings were evenly distributed with 13.7, 11.8, 16.7, 17.6, and 14.7% rating them as low, moderately low, moderate, moderately high, and high risk, respectively. Furthermore, 25.5% of participants reported being unfamiliar with e-cigarettes (Figure 1).
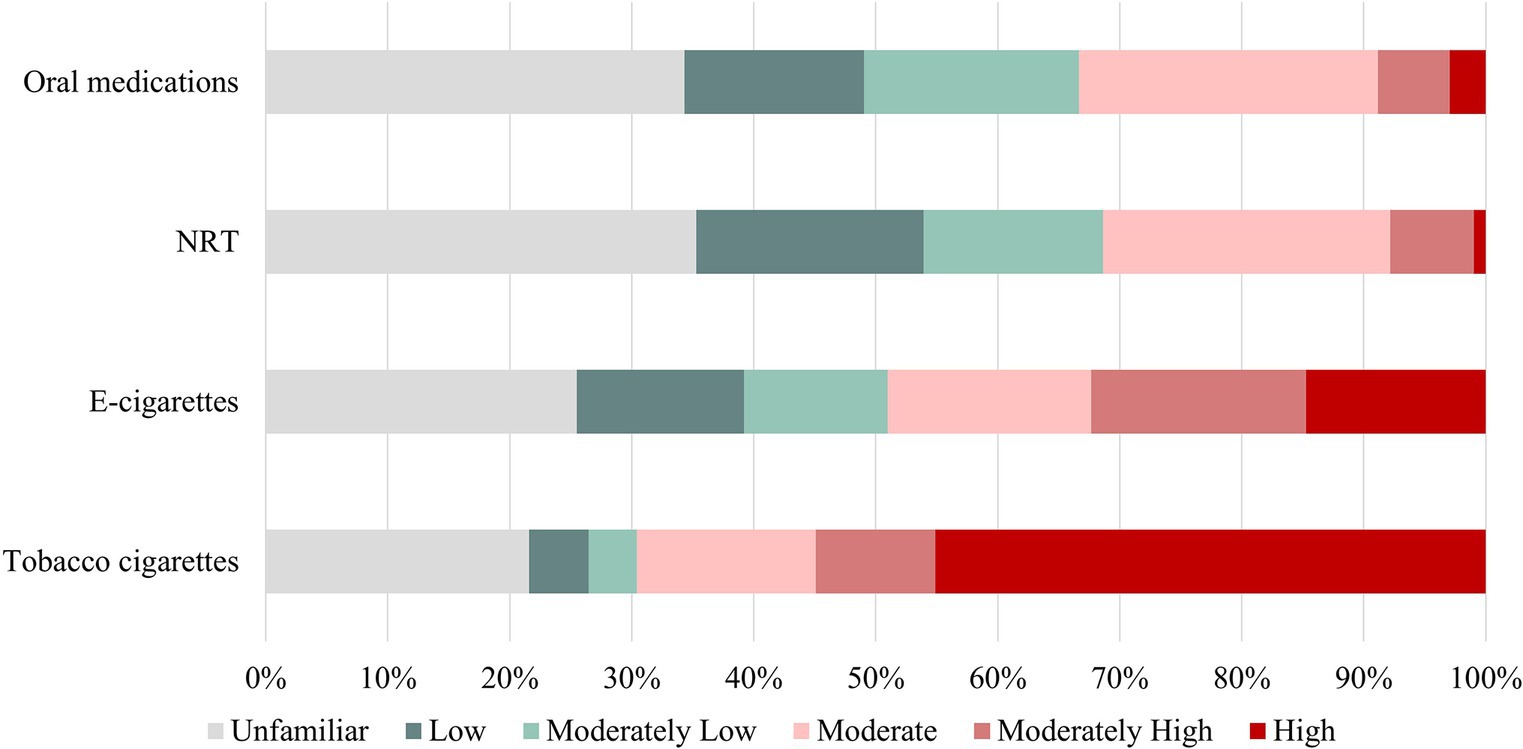
Figure 1. Health risks of smoking products. E-cigarettes, Electronic cigarettes; NRT, Nicotine replacement therapy.
Participants were also asked to report their perception of nicotine’s impact on specific diseases. Results showed that 77.5% (high and moderately high) believed that nicotine played an active role in the development of smoking-related lung cancer. Additionally, approximately 55.9% of participants believed that nicotine had an active role in the development of cancers in organs outside of the lungs, such as the bladder, pancreas, and gastrointestinal tract (Figure 2). Furthermore, 28 believed that e-cigarettes were less addictive (compared to cigarettes).
In subgroup analyses, we observed noteworthy differences in knowledge and perceptions between smokers and non-smokers among the GPwSIs in Supplementary Table S1. Regarding the health risks associated with tobacco cigarettes, a higher percentage of smokers (57.7%) rated these risks as high compared to non-smokers (40.8%) (p = 0.20). Similarly, for e-cigarettes, while 17.1% of non-smokers considered them to have a high health risk, only 7.7% of smokers shared this view (p = 0.55). Interestingly, smokers demonstrated a better understanding of the correct dosage and usage of nicotine patches, with 50% answering correctly, compared to only 19.7% of non-smokers (p = 0.01). However, both groups showed similar levels of confidence in the safety of long-term (>6 months) NRT use, with no significant difference in their responses (p = 0.46). The analysis revealed that respondents’ age impacted their attitudes toward NRT. Those aged 20–39 were more likely to have a positive attitude toward the long-term use of NRT for smoking cessation compared to their older counterparts (p < 0.05) (Supplementary Tables S3).
Discussion
This study aimed to assess the knowledge and awareness of GPwSIs in respiratory medicine regarding nicotine, NRT, and e-cigarettes. The study found that GPwSIs showed insufficient familiarity with the harms of smoking, NRT, oral smoking cessation medications, and e-cigarettes. This lack of familiarity was attributed to the possible absence of clinical guidelines for primary care and insufficient training on smoking cessation.
In this study, some GPwSIs were found to overestimate the risks of nicotine, despite its classification as a non-carcinogen (20). Misconceptions about the harmful effects of nicotine on human health are common among healthcare workers, which can be attributed to the belief that publicly downplaying the potential risks of nicotine may lead to an underestimation of smoking-related health problems (22). This viewpoint may create a bias against the use of NRT and oral smoking cessation medications, even though health organizations’ guidelines suggest that the risks of long-term nicotine use are far less than continued smoking (20). Consequently, there is a widespread stereotype of nicotine that leads some GPwSIs to discourage the long-term use of NRT for smokers.
Findings demonstrate that among GPwSIs, perceptions of harm and addictiveness of e-cigarettes is relatively diverse, possibly due to the inconsistent evaluation of e-cigarettes and the lack of unified guidelines (23). Current literature is insufficient to conclusively establish the effectiveness of e-cigarettes as a smoking cessation tool (24–26). However, a randomized controlled trial comparing e-cigarettes to NRT among adults who sought to quit smoking showed that the former had an advantage in achieving one-year abstinence rates (25). Although some health and medicine groups warn against e-cigarette use, others, including those in the United Kingdom and the United States, believe that e-cigarettes could be helpful in reducing the harm caused by smoking (12).
Smoking physicians are unlikely to advocate for smoking cessation to their patients (27). Over 25% of participants were current or former smokers, highlighting the persistent issue of smoking among GPwSIs. A meta-analysis on smoking rates among physicians revealed that family physicians and medical students had the highest proportion of smokers, and smoking rates among physicians in Europe and Asia were 40% higher than those in Oceania (27). Similarly, a meta-analysis on smoking among medical students in mainland China showed an overall smoking prevalence of 10.93% (range = 0.81 to 50.37%) in 65 studies involving 68,253 medical students, with a significantly higher prevalence among male medical students (28). As physicians serve as role models for patients and society, their smoking habits undermine their potential to persuade smoking patients to quit.
GPwSIs exhibited varying levels of knowledge and confidence in smoking cessation practices, including the use of NRT. This variation can be partly attributed to the diverse educational backgrounds of these practitioners. Typically, it appears that training in smoking cessation techniques and NRT is not consistently emphasized or standardized across programs (28). This education gap may contribute to the observed discrepancies in their approach to smoking cessation.
Implementation
Assessing the knowledge of healthcare trainees holds key to customize educational plans based on actual training needs. Additionally, although GPwSIs are aware of their importance in the anti-tobacco movement, they lack optimal confidence in tobacco control strategies. Our study calls for revising the education combination for GPs in public health and preventive medicine.
Limitations
The shortcomings of this study may have the following points. The first and foremost is that the study only included GPwSIs in respiratory medicine and may not accurately represent the views and knowledge of all Chinese GPs. Secondly, the study only focused on GPwSIs in respiratory medicine, who have relatively short practice experience in China and may have received different training and education, which could limit the generalizability of the findings. Thirdly, we did not explore the potential differences between GPwSIs in respiratory medicine and other GPs or respiratory specialists in terms of their knowledge and beliefs regarding smoking. More qualitative studies should be considered in future research. Nevertheless, our study succeeded in achieving its objectives by providing new insights into the perspectives of GPwSIs regarding e-cigarettes and NRT, and emphasizing the need for more research to enhance the knowledge of GPs in this field.
Conclusion
The study highlights serious knowledge gaps among GPwSIs in respiratory medicine regarding nicotine, NRT, and e-cigarettes, which could hinder their ability to provide accurate and reliable advice to smokers. Therefore, it is imperative that GPwSIs receive appropriate training in tobacco cessation counseling to enable them to better assist tobacco users with quitting and integrate smoking cessation services into their routine care.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
This study was approved by the Ethics Committee of West China Hospital, Sichuan University, Chengdu, China (No. 2021-1745). All the methods and protocols were performed in accordance with relevant guidelines and regulations and informed consent was obtained from all subjects. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their informed consent to participate in this study.
Author contributions
QZ and ZA conceived this study. QMZ, DY, ZW, and HZ designed the questionnaire. KA and LZ collected the data. QZ and HL analyzed the data. SL and CL illustrated the plots. QZ, KA, and ZA drafted the paper. All authors contributed to drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work.
Funding
This study was supported by National Clinical Research Center for Geriatrics, West China Hospital, Sichuan University (Grant number Z2021JC005) and Sichuan Science and Technology Program (Grant number 2021YFH0168).
Acknowledgments
The study team is grateful to all colleagues participating in practices at Fang-cao Community Health Service Center (Chengdu, Sichuan, China) who supported this work.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2023.1236453/full#supplementary-material
Abbreviations
E-cigarettes, Electronic cigarettes; GPwSIs, General practitioners with a special interest; NRT, Nicotine replacement therapy; GPs, General practitioners.
Footnotes
References
1. Au, WW, Su, D, and Yuan, J. Cigarette smoking in China: public health, science, and policy. Rev Environ Health. (2012) 27:43–9. doi: 10.1515/reveh-2012-0003
2. Ghebreyesus, TA. Progress in beating the tobacco epidemic. Lancet. (2019) 394:548–9. doi: 10.1016/s0140-6736(19)31730-1
3. Ambrose, JA, and Barua, RS. The pathophysiology of cigarette smoking and cardiovascular disease: an update. J Am Coll Cardiol. (2004) 43:1731–7. doi: 10.1016/j.jacc.2003.12.047
4. Lugg, ST, Scott, A, Parekh, D, Naidu, B, and Thickett, DR. Cigarette smoke exposure and alveolar macrophages: mechanisms for lung disease. Thorax. (2022) 77:94–101. doi: 10.1136/thoraxjnl-2020-216296
5. Sasco, AJ, Secretan, MB, and Straif, K. Tobacco smoking and cancer: a brief review of recent epidemiological evidence. Lung Cancer. (2004) 45:S3–9. doi: 10.1016/j.lungcan.2004.07.998
6. Yuan, L, Zhao, Z, Wang, J, Du, M, Xiao, Y, Liu, L, et al. Decomposition and comparative analysis of the prevalence of and factors associated with smoking between the rural and urban elderly population in China: a national cross-sectional study. Front Public Health. (2022) 10:824587. doi: 10.3389/fpubh.2022.824587
7. Li, N, Wu, P, Wang, Z, Shen, Y, Zhang, L, Xue, F, et al. Smoking-related cancer death among men and women in an ageing society (China 2020-2040): a population-based modelling study. Tob Control. (2023) 32:163–9. doi: 10.1136/tobaccocontrol-2020-056444
8. Caini, S, Del Riccio, M, Vettori, V, Scotti, V, Martinoli, C, Raimondi, S, et al. Quitting smoking at or around diagnosis improves the overall survival of lung cancer patients: a systematic review and meta-analysis. J Thorac Oncol. (2022) 17:623–36. doi: 10.1016/j.jtho.2021.12.005
9. Chen, H, Yang, Y, Miyai, H, Yi, C, and Oliver, BG. The effects of exercise with nicotine replacement therapy for smoking cessation in adults: a systematic review. Front Psych. (2022) 13:1053937. doi: 10.3389/fpsyt.2022.1053937
10. Li, J, Hui, X, Fu, J, Ahmed, MM, Yao, L, and Yang, K. Electronic cigarettes versus nicotine-replacement therapy for smoking cessation: a systematic review and meta-analysis of randomized controlled trials. Tob Induc Dis. (2022) 20:1–13. doi: 10.18332/tid/154075
11. Tindle, HA, Freiberg, MS, Cheng, DM, Gnatienko, N, Blokhina, E, Yaroslavtseva, T, et al. Effectiveness of varenicline and cytisine for alcohol use reduction among people with HIV and substance use: a randomized clinical trial. JAMA Netw Open. (2022) 5:e2225129. doi: 10.1001/jamanetworkopen.2022.25129
12. Shin, DW, Kim, YI, Kim, SJ, Kim, JS, Chong, S, Park, YS, et al. Lung cancer specialist physicians' attitudes towards e-cigarettes: a nationwide survey. PLoS One. (2017) 12:e0172568. doi: 10.1371/journal.pone.0172568
13. Etter, JF, and Bullen, C. Electronic cigarette: users profile, utilization, satisfaction and perceived efficacy. Addiction. (2011) 106:2017–28. doi: 10.1111/j.1360-0443.2011.03505.x
14. Hajek, P, Phillips-Waller, A, Przulj, D, Pesola, F, Myers Smith, K, Bisal, N, et al. A randomized trial of E-cigarettes versus nicotine-replacement therapy. N Engl J Med. (2019) 380:629–37. doi: 10.1056/NEJMoa1808779
15. Selamoglu, M, Erbas, B, Kasiviswanathan, K, and Barton, C. General practitioners' knowledge, attitudes, beliefs and practices surrounding the prescription of e-cigarettes for smoking cessation: a mixed-methods systematic review. BMC Public Health. (2022) 22:2415. doi: 10.1186/s12889-022-14696-3
16. Lund, I, and Scheffels, J. Perceptions of the relative harmfulness of snus among Norwegian general practitioners and their effect on the tendency to recommend snus in smoking cessation. Nicotine Tob Res. (2012) 14:169–75. doi: 10.1093/ntr/ntr159
17. Wikmans, T, and Ramström, L. Harm perception among Swedish daily smokers regarding nicotine, NRT-products and Swedish Snus. Tob Induc Dis. (2010) 8:9. doi: 10.1186/1617-9625-8-9
18. Ramesh Patwardhan, S, Klein, A, and Murphy, MA. Survey of GPs’ understanding of tobacco and nicotine products. Drugs Alcohol Today. (2013) 13:119–50. doi: 10.1108/dat-02-2013-0010
19. Malik, S. GPs with special interests. BMJ. (2006) 332:gp133–4. doi: 10.1136/bmj.332.7545.sgp133-a
20. Moysidou, A, Farsalinos, KE, Voudris, V, Merakou, K, Kourea, K, and Barbouni, A. Knowledge and perceptions about nicotine, nicotine replacement therapies and electronic cigarettes among healthcare professionals in Greece. Int J Environ Res Public Health. (2016) 13:514. doi: 10.3390/ijerph13050514
21. An, K, Zhang, L, Mao, TR, Liu, F, Cheng, CY, Yang, Y, et al. Exploration and practice of specialty training program in general practice. Sichuan Da Xue Xue Bao Yi Xue Ban. (2022) 53:431–6. doi: 10.12182/20220560303
22. Ferrara, P, Shantikumar, S, Cabral Verissimo, V, Ruiz-Montero, R, Masuet-Aumatell, C, Ramon-Torrell, JM, et al. Knowledge about E-cigarettes and tobacco harm reduction among public health residents in Europe. Int J Environ Res Public Health. (2019) 16:2071. doi: 10.3390/ijerph16122071
23. Nickels, AS, Warner, DO, Jenkins, SM, Tilburt, J, and Hays, JT. Beliefs, practices, and self-efficacy of US physicians regarding smoking cessation and electronic cigarettes: a national survey. Nicotine Tob Res. (2017) 19:197–207. doi: 10.1093/ntr/ntw194
24. Zhu, SH, Zhuang, YL, Wong, S, Cummins, SE, and Tedeschi, GJ. E-cigarette use and associated changes in population smoking cessation: evidence from US current population surveys. BMJ. (2017) 358:j3262. doi: 10.1136/bmj.j3262
25. Cao, DJ, Aldy, K, Hsu, S, McGetrick, M, Verbeck, G, De Silva, I, et al. Review of health consequences of electronic cigarettes and the outbreak of electronic cigarette, or vaping, product use-associated lung injury. J Med Toxicol. (2020) 16:295–310. doi: 10.1007/s13181-020-00772-w
26. Marques, P, Piqueras, L, and Sanz, MJ. An updated overview of e-cigarette impact on human health. Respir Res. (2021) 22:151. doi: 10.1186/s12931-021-01737-5
27. Besson, A, Tarpin, A, Flaudias, V, Brousse, G, Laporte, C, Benson, A, et al. Smoking prevalence among physicians: a systematic review and meta-analysis. Int J Environ Res Public Health. (2021) 18:13328. doi: 10.3390/ijerph182413328
Keywords: electronic cigarettes, nicotine, general practitioners with a special interest, knowledge, awareness
Citation: Zhong Q, An K, Wu Z, Zhang H, Li S, Zhang L, Li C, Li H, Zhuo Ga QM, Yang Zong DJ and An Z (2024) Knowledge and awareness of nicotine, nicotine replacement therapy, and electronic cigarettes among general practitioners with a special interest in respiratory medicine in China. Front. Med. 10:1236453. doi: 10.3389/fmed.2023.1236453
Edited by:
Arquimedes Gasparotto Junior, Federal University of Grande Dourados, BrazilReviewed by:
Hyunchan Lee, National Eye Institute (NIH), United StatesNihit Gupta, Dayton Children's Hospital, United States
Copyright © 2024 Zhong, An, Wu, Zhang, Li, Zhang, Li, Li, Zhuo Ga, Yang Zong and An. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhenmei An, YXptaHhuZm1AMTYzLmNvbQ==
†These authors have contributed equally to this work
 Qian Zhong
Qian Zhong Kang An
Kang An Zengxiang Wu
Zengxiang Wu Haijun Zhang2
Haijun Zhang2 Shengxi Li
Shengxi Li Lin Zhang
Lin Zhang Caizheng Li
Caizheng Li Zhenmei An
Zhenmei An