- Department of Orthopedics, Dandong Central Hospital, China Medical University, Dandong, China
Background: Urinary tract infection (UTI) is a prevalent and consequential complication in hip fracture patients, leading to significant disability and heightened healthcare expenditures. Consequently, there is a critical need for a comprehensive systematic review to identify risk factors and establish early and effective preventive measures.
Methods: A comprehensive search was performed across the PubMed, Cochrane, Embase, Web of Science, and Scopus databases (up to August 31, 2023). Article screening, data extraction, and quality assessment were independently completed by two reviewers.
Results: Forty-four studies were eligible for inclusion, yielding an overall incidence rate of 11% (95% CI: 8%−14%). Our pooled analysis revealed 18 significant risk factors, including being female (OR = 2.23, 95% CI: 1.89–2.63), advanced age (MD = 1.35, 95% CI: 0.04–2.66), obesity (OR = 1.21, 95% CI: 1.11–1.31), catheterization (OR = 3.8, 95% CI: 2.29–6.32), blood transfusion (OR = 1.39, 95% CI: 1.21–1.58), American Society of Anesthesiologists ≥III (OR = 1.28, 95% CI: 1.18–1.40), general anesthesia (OR = 1.26, 95% CI: 1.11–1.43), intertrochanteric fracture (OR = 1.25, 95% CI: 1.01–1.54), hemiarthroplasty (OR = 1.43, 95% CI: 1.19–1.69), prolonged length of hospital stay (MD = 1.44, 95% CI: 0.66–2.23), delirium (OR = 2.66, 95% CI: 2.05–3.47), dementia (OR = 1.82, 95% CI: 1.62–2.06), Parkinson's disease (OR = 1.53, 95% CI: 1.46–1.61), diabetes (OR = 1.27, 95% CI: 1.13–1.43), hypertension (OR = 1.14, 95% CI: 1.03–1.26), congestive heart failure (OR = 1.35, 95% CI: 1.10–1.66), history of sepsis (OR = 7.13, 95% CI: 5.51–9.22), and chronic steroid use (OR = 1.29, 95% CI: 1.06–1.57).
Conclusion: Our study identifies numerous risk factors strongly associated with UTI, offering compelling evidence and actionable strategies for improving clinical prediction, enabling early intervention, and facilitating targeted UTI management.
Systematic review registration: identifier [CRD42023459600], https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=459600.
Introduction
Hip fracture, the prevailing type of fracture in the geriatric populace, has garnered substantial attention globally. Reports indicate an alarming annual global incidence of approximately 1.6 million cases, accompanied by an exorbitant sum surpassing 10 billion US dollars in medical expenses (1–3). Moreover, owing to the progressive aging of populations, it is anticipated that hip fracture occurrences will experience a rapid annual increase ranging from 1% to 3% (4). This trend forecasts a staggering projection of approximately 6.1 million global hip fracture cases by the year 2050. Unfortunately, the elderly population afflicted with hip fractures is plagued by a multitude of pre-existing conditions, physical deterioration, and prolonged immobilization, thus yielding a complication rate ranging from 7% to 40% (5). Among these complications, UTI stands out as a prominent affliction afflicting hip fracture patients, with occurrence rates ranging from 4% to 32% (6, 7). The grave implications of UTIs are correlated with elevated mortality rates, profound disabilities, and escalated healthcare expenditures, ultimately dealing an irrevocable blow to the already vulnerable elderly hip fracture population.
To date, numerous systematic reviews have reported on other associated complications of hip fractures, such as pneumonia (3, 8), delirium (9), and deep vein thrombosis (10). However, no systematic review has been conducted to identify potential risk factors for UTI in hip fracture patients. Therefore, identifying the risk factors for UTI in hip fracture patients is crucial for clinical physicians to identify high-risk patients, guide targeted early interventions, and predict patient outcomes. This systematic review aims to address two crucial questions: (1) What is the incidence rate of UTI in hip fracture patients? (2) What are the related risk factors for UTI in hip fracture patients?
Methods
This study has been registered on PROSPERO (CRD42023459600) and conducted according to the guidelines of Meta-analysis Of Observational Studies in Epidemiology (MOOSE).
Search strategy
A comprehensive search was performed on the PubMed, Cochrane, Embase, Web of Science, and Scopus databases from their inception to August 31, 2023, to identify all relevant studies. To mitigate the inclusion of irrelevant articles, Keywords and relevant terms, such as “hip fracture,” “urinary tract infection,” and “risk factors,” were concatenated using the Boolean operator “AND.” The search was conducted without language or country restrictions. Furthermore, to prevent the omission of relevant primary studies, we manually reviewed the references cited in the primary studies and reviews.
Study selection
The inclusion criteria for studies are as follows: (1) cohort or case-control studies; (2) restricted to patients with hip fractures, but excluding cases caused by multiple traumas; (3) The studies should report risk factors associated with UTI in patients with hip fractures that have been documented at least twice; (4) The diagnostic criteria for UTI are well-defined, and the occurrence of UTI is observed during the patient's hospitalization. The following will be excluded: (1) letters, comments, case reports, conference records, and animal studies; (2) inability to obtain full text, data duplication, or inability to calculate odds ratios (OR), mean difference (MD), and 95% confidence intervals (CI). The review will be excluded after manually reviewing the references.
A summary of all relevant studies retrieved, excluding duplicate records, was conducted for screening. To ensure the objectivity of the review results, the titles and abstracts of all articles were independently examined by two reviewers (WW and WY). Studies that met the criteria underwent an independent full-text review by the same reviewers, resulting in the final inclusion of studies. After each round of screening, the results were compared, and any discrepancies were thoroughly discussed to reach a consensus. In cases where consensus could not be reached, a third-party reviewer (WBD) was consulted for resolution.
Data extraction
A standardized electronic form was utilized to extract the following data from the included studies: author, year of publication, country, study type, sample size, number of UTI patients, UTI diagnostic criteria, and relevant risk factors. The entire process was independently completed by two reviewers (WW and WY) who compared the extracted data. Comprehensive discussion was used to resolve any discrepancies, and in cases where a consensus could not be reached, a third-party reviewer (WBD) was consulted for resolution.
Quality assessment
The quality of the included studies was independently assessed by two reviewers (WW and WY) using the Newcastle-Ottawa Quality Assessment Scale (NOS). The NOS is a tool used for systematically evaluating the quality of non-randomized controlled studies. It consists of 3 dimensions (selection, comparability, and outcome or exposure) and 8 items. One point is awarded for each fulfilled requirement, with a total score ranging from 0 to 9 (11). Only studies that meet the majority of the requirements (≥6 points) are considered to be of high quality. Any disagreements in scoring were resolved through discussion or consultation with a third-party reviewer (WBD).
Statistical analysis
To obtain the pooled incidence rate, a meta-analysis was performed using the inverse variance method and random effects model in STATA 15.0 (STATA Corporation, College Station, TX, USA). Heterogeneity was assessed by I2 and chi-squared tests. If heterogeneity was present (I2 > 50% or P < 0.1), a meta-regression was used to explore the sources of heterogeneity.
When more than two studies reported the same risk factor, a meta-analysis was conducted using RevMan 5.4 (The Cochrane Collaboration, Oxford, UK). A random effects model was pre-specified, and the inverse variance or Mantel-Haenszel methods were used to estimate the pooled OR or MD depending on the data type of the risk factor (continuous or dichotomous). The effect model was adjusted according to the heterogeneity of the results. When significant heterogeneity was observed among studies (I2 > 50% or P < 0.1), a random effects model was used; otherwise, a fixed effects model was applied.
Sensitivity analyses were conducted to test the reliability and stability of the results by repeatedly excluding individual studies and examining changes in the pooled effect. Publication bias was assessed using funnel plots, Begg's test, and Egger's test. If publication bias was detected, the trim-and-fill method was used to adjust for it. These parts of analyses were conducted in STATA 15.0.
A two-tailed P value < 0.05 was considered statistically significant. There were no unavailable effect sizes or 95% CIs in our study.
Results
Study selection and quality assessment
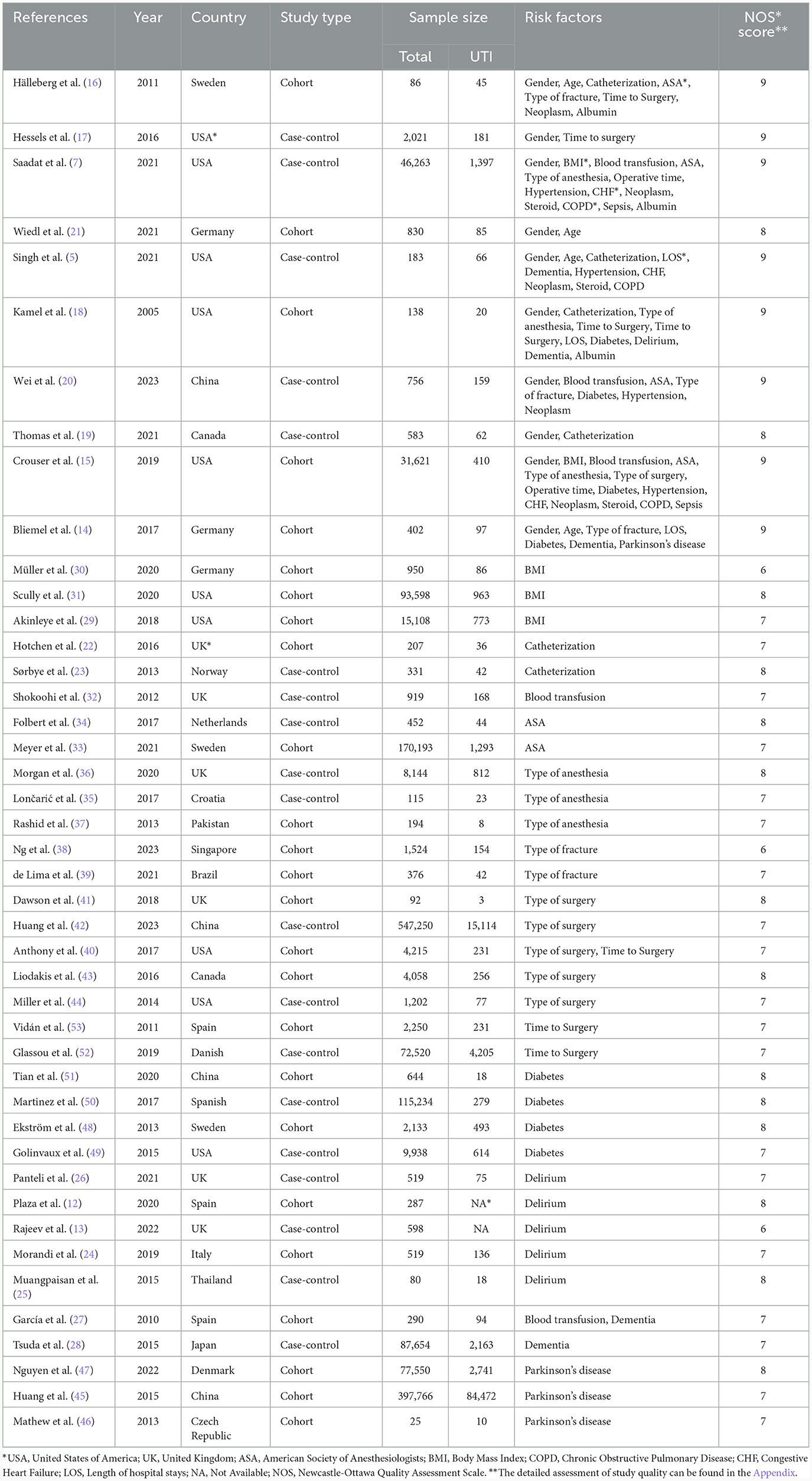
A total of 1,116 articles were initially collected through searching five databases (all articles obtained from manual review of reference lists were included in the articles retrieved from the database search). After excluding duplicates and reviews, the titles and abstracts of 646 articles were screened, resulting in the removal of 455 articles that did not align with our research topic. Full-text review was performed on the remaining 191 articles. Ultimately, 44 studies that met our inclusion criteria were included in this meta-analysis. All included studies were English articles, primarily sourced from Europe, the Americas, and Asia. A detailed flowchart of study selection process is presented in Figure 1.
The quality of non-randomized controlled studies included in this meta-analysis was assessed using the NOS. The quality scores of all included studies in the analysis were ≥6 (9 points for 8 studies, 8 points for 14 studies, 7 points for 19 studies, and 6 points for the remaining 3 studies), meeting the requirements for conducting a meta-analysis. Detailed scoring criteria can be found in Supplementary Table 1.
Incidence rate
The incidence of UTI in patients with hip fractures was reported in 42 included studies [2 articles (12, 13) only reported risk factors and did not provide incidence data]. The pooled incidence of UTI in hip fracture patients was 11% (95% CI: 0.08–0.14) (Supplementary Figure 1). We observed significant heterogeneity among the studies (I2 = 99.97%, P < 0.01). To explore the source of heterogeneity, a meta-regression was conducted. The meta-regression results indicated that the percentage of female patients (P < 0.001), year of publication (P < 0.02), and region (P = 0.018) were significantly associated with heterogeneity. However, sample size (P = 0.213), and study type (P = 0.593) were not identified as the sources of heterogeneity. The details can be found in Supplementary Table 2.
Potential risk factors
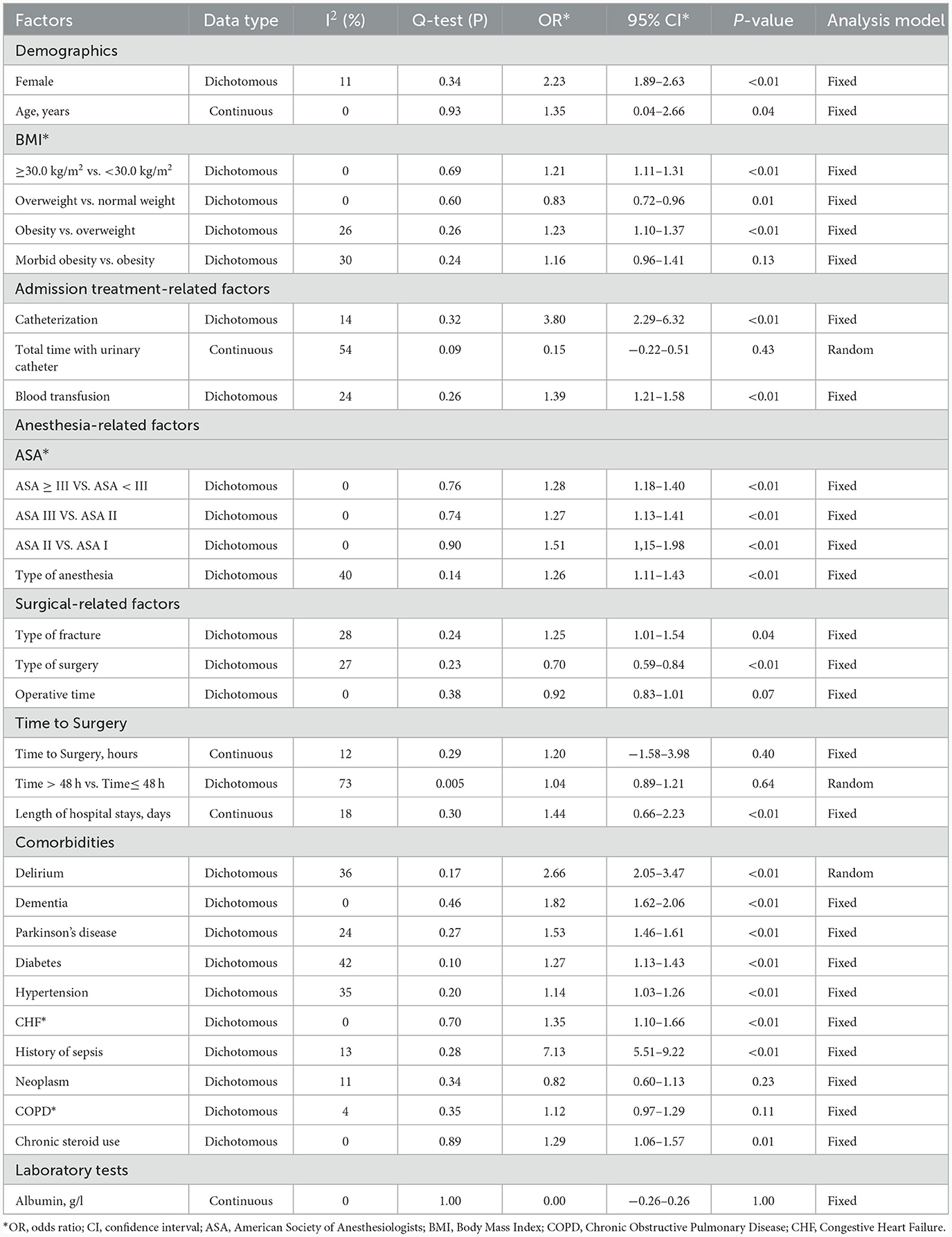
Table 1 details the main characteristics of the 44 items included in the study, while Table 2 presents the specific results of the meta-analysis. The following risk factors are crucial for clinical doctors to identify and intervene in the occurrence of UTI: female [9 studies (5, 14–21), OR = 2.23, 95% CI: 1.89–2.63, Figure 2A]; urinary catheterization [4 studies (18, 19, 22, 23), OR = 3.8, 95% CI: 2.29–6.32, Figure 3A]; delirium [6 studies (12, 13, 18, 24–26), OR = 2.66, 95% CI: 2.05–3.47, Figure 5A]; dementia [5 articles (5, 14, 18, 27, 28), OR = 1.82, 95% CI: 1.62–2.06, Figure 5B]; history of sepsis [2 articles (7, 15), OR = 7.13, 95% CI: 5.51–9.22, Figure 6A].
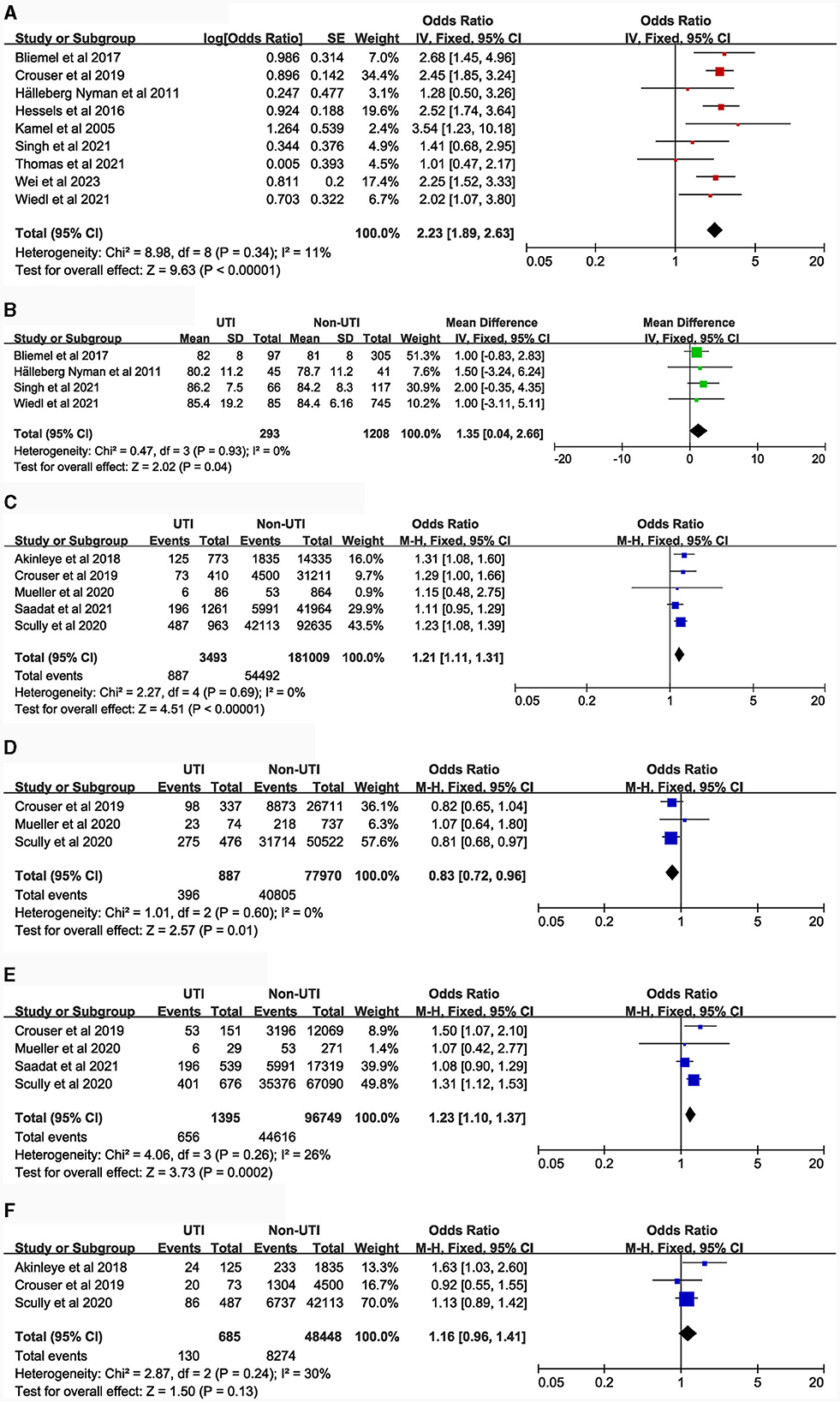
Figure 2. Forest plot for Demographics. (A), Gender; (B), Age (continuous data); (C), BMI (≥30.0 kg/m2 vs. <30.0 kg/m2); (D), BMI (Overweight VS. Normal weight); (E), Body Mass Index (Obesity VS. Overweight); (F), BMI (Morbid obesity vs. Obesity). CI, Confidence Interval; df, Degrees of Freedom; M-H, Mantel-Haenszel.
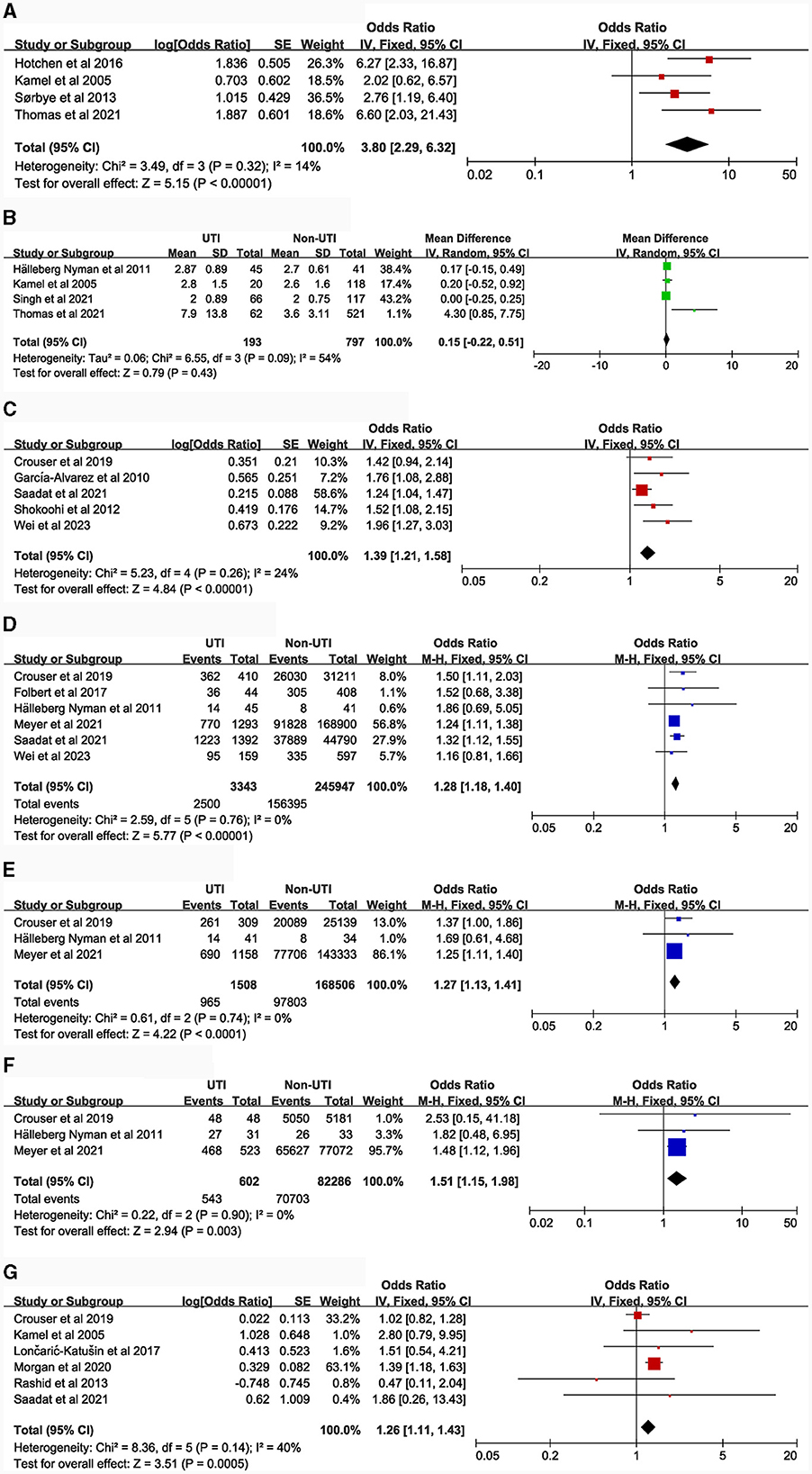
Figure 3. Forest plots for Admission treatment and Anesthesia-related factors. (A), Catheterization; (B), Total time with urinary catheter; (C), Blood transfusion; (D), American Society of Anesthesiologists (≥III vs. <III); (E), ASA (III vs. II); (F), ASA (II vs. I); (G), Type of anesthesia (General anesthesia vs. Spinal anesthesia).
The following risk factors hold moderate clinical significance and warrant attention in clinical practice: advanced age [4 studies (5, 14, 16, 21), MD = 1.35, 95% CI: 0.04–2.66, Figure 2B]; Body Mass Index ≥ 30.0 kg/m2 [5 studies (7, 15, 29–31), OR = 1.21, 95% CI: 1.11–1.31, Figure 2C]; blood transfusion [5 studies (7, 15, 20, 27, 32), OR = 1.39, 95% CI: 1.21–1.58, Figure 3C]; American Society of Anesthesiologists classification ≥ III [6 articles (7, 15, 16, 20, 33, 34), OR = 1.28, 95% CI: 1.18–1.40, Figure 3D]; general anesthesia [6 studies (7, 15, 18, 35–37), OR = 1.26, 95% CI: 1.11–1.43, Figure 3G]; intertrochanteric fractures [compared to femoral neck fractures, 5 articles (14, 16, 20, 38, 39), OR = 1.25, 95% CI: 1.01–1.54, Figure 4A]; hemiarthroplasty [compared to total hip replacement, 6 studies (15, 40–44), OR = 1.43, 95% CI: 1.19–1.69, Figure 4B]; length of hospital stay [3 articles (5, 14, 18), MD = 1.44, 95% CI: 0.66–2.23, Figure 4F]; Parkinson's disease [4 articles (14, 45–47), OR = 1.53, 95% CI: 1.46–1.61, Figure 5C]; diabetes [8 articles (14, 15, 18, 20, 48–51), OR = 1.27, 95% CI: 1.13–1.43, Figure 5D]; hypertension [4 articles (5, 7, 15, 20), OR = 1.14, 95% CI: 1.03–1.26, Figure 5E]; congestive heart failure [3 articles (5, 7, 15), OR = 1.35, 95% CI: 1.10–1.66, Figure 5F]; and long-term steroid use [3 studies (5, 7, 15), OR = 1.29, 95% CI: 1.06–1.57, Figure 6D]. Additionally, we conducted a more detailed analysis by categorizing high BMI (Body Mass Index) into different groups according to guidelines: Normal weight (BMI: 18.5–24.9 kg/m2), Overweight (BMI: 25–29.9 kg/m2), Obesity (BMI: 30–39.9 kg/m2), and Morbid Obesity (BMI ≥ 40 kg/m2). The comparison between groups revealed that obese patients with hip fractures had an increased risk of UTI compared to overweight patients (OR = 1.23, 95% CI: 1.10–1.37, Figure 2E). No significant difference was observed between morbid obesity and obesity groups (P > 0.05, Figure 2F). Surprisingly, overweight patients had lower UTI risk than normal-weight patients (OR = 0.83, 95% CI: 0.72–0.96, Figure 2D). Similarly, our findings indicate a direct association between the incremental rise in ASA (American Society of Anesthesiologists) classification and the heightened risk of UTI occurrence (P < 0.05, Figures 3E, F).
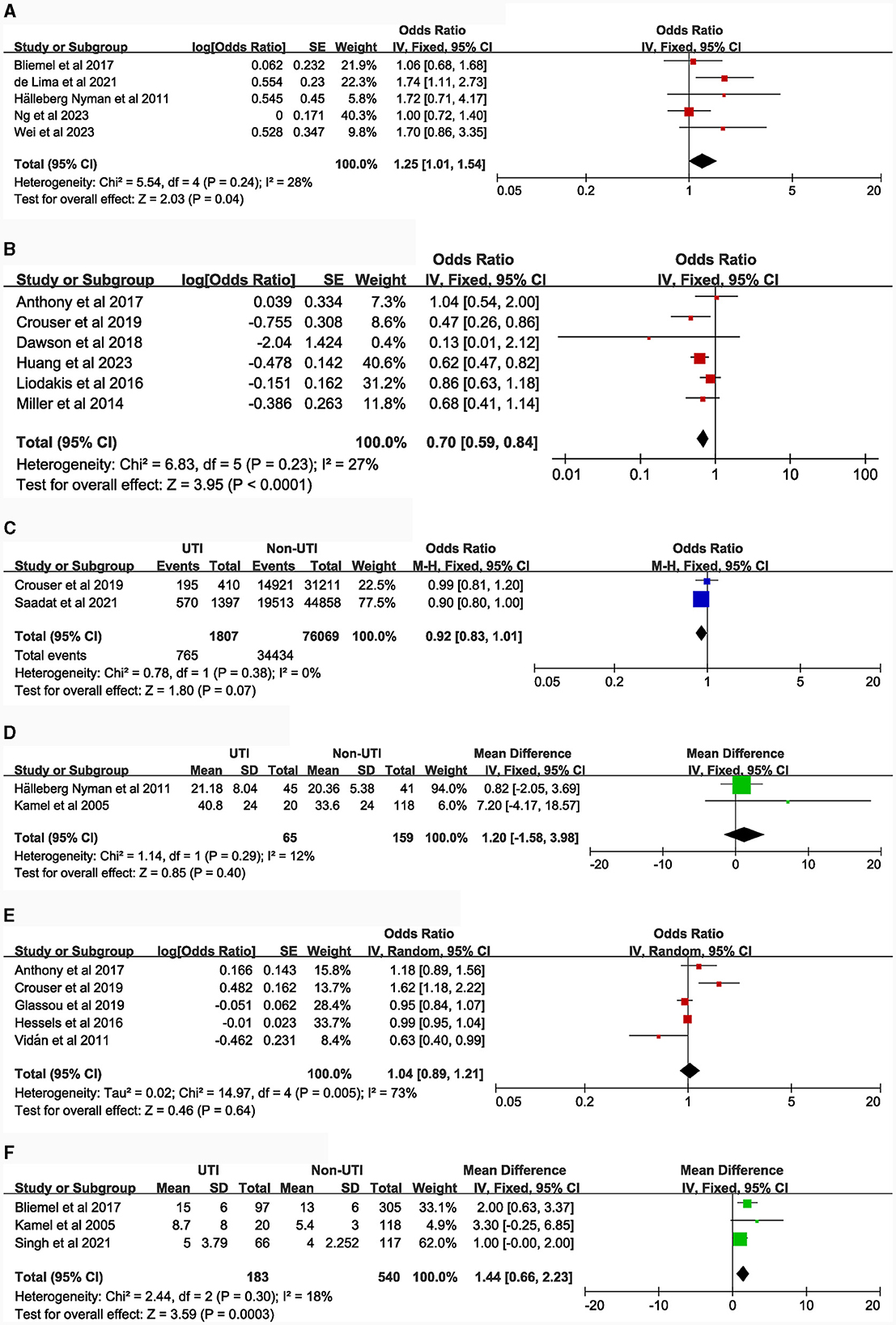
Figure 4. Forest plots for surgical-related factors. (A), Type of fracture (intertrochanteric fracture vs. femoral neck fracture); (B), type of surgery (total hip replacement vs. hemiarthroplasty); (C), Operative time (>1 h vs. ≤ 1 h); (D), Time to Surgery (continuous data); (E), Time to Surgery (>48 h vs. ≤ 48 h); (F), Length of hospital stays (continuous data).
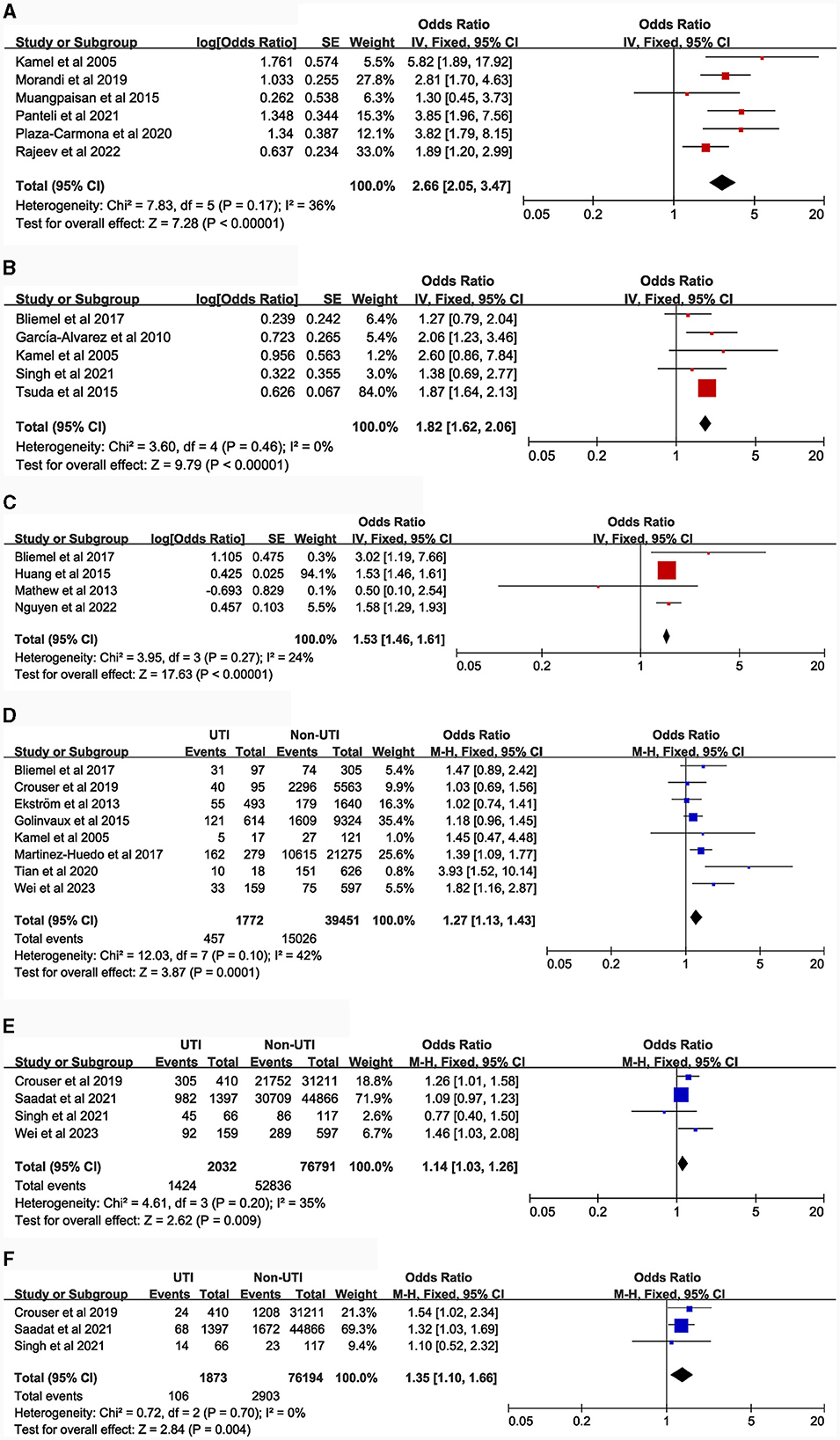
Figure 5. Forest plots for comorbidities. (A), delirium; (B), dementia; (C), Parkinson's disease; (D), diabetes; (E), hypertension; (F), congestive heart failure.
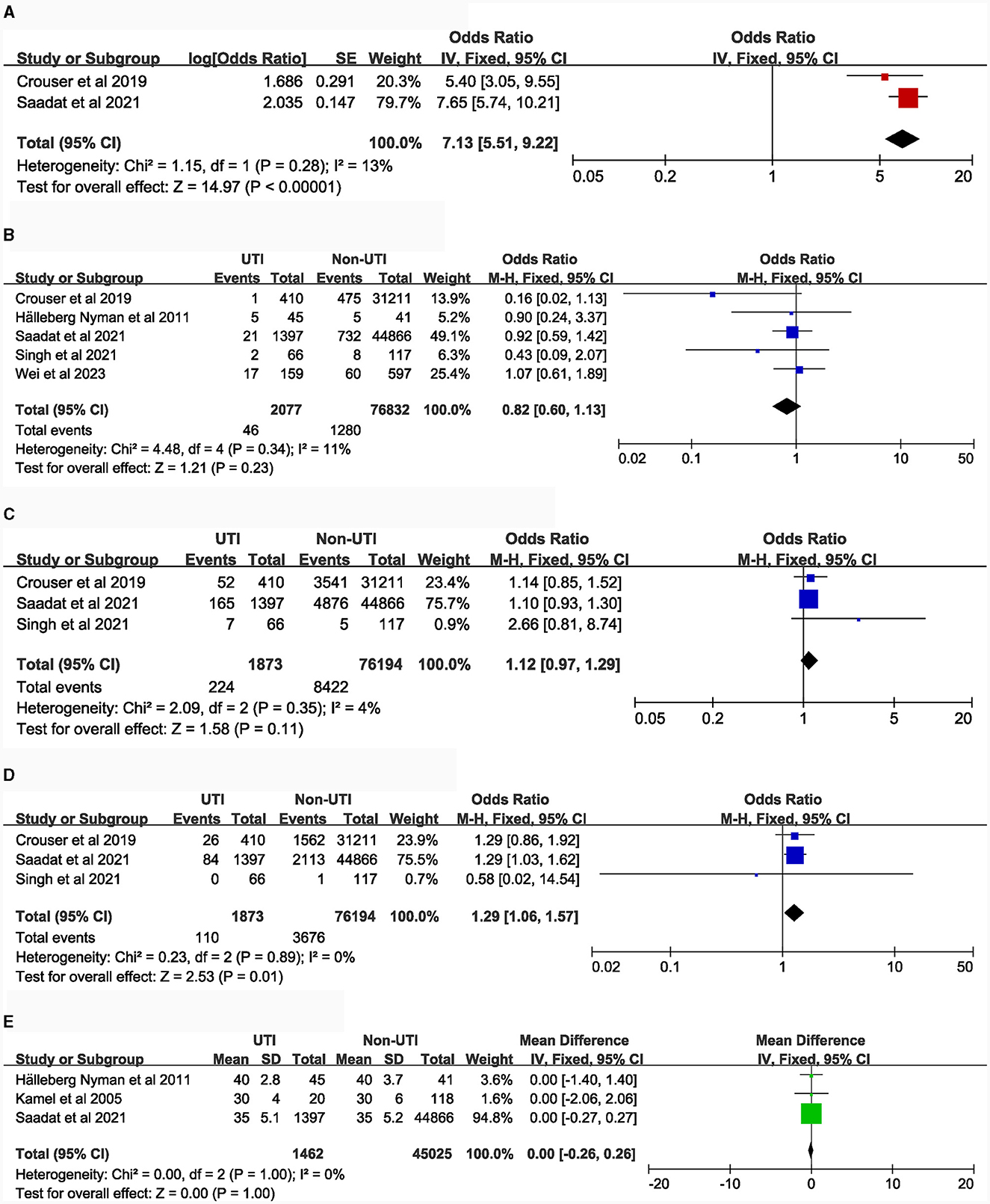
Figure 6. Forest plots for comorbidities and laboratory tests. (A), history of sepsis; (B), neoplasm; (C), chronic obstructive pulmonary disease; (D), chronic steroid use; (E), preoperative albumin.
There was no observed correlation between the following risk factors and UTI in patients with hip fractures: duration of catheterization [4 studies (5, 16, 18, 19), Figure 3B]; surgical duration longer than 1 h [2 articles (7, 15), Figure 4C]; time to surgery [dichotomous and continuous variables, 7 articles (15–18, 40, 52, 53), Figures 4D, E]; neoplasm [5 articles (5, 7, 15, 16, 20), Figure 6B]; chronic obstructive pulmonary disease [3 studies (5, 7, 15), Figure 6C]; preoperative albumin levels [3 articles (7, 16, 18), Figure 6E].
Sensitivity analyses
It was observed that the effect size of the gender risk factor lacked robustness (Supplementary Figure 3a). Consequently, the study (7) conducted by Saadat et al. was excluded from the investigation concerning the relationship between gender and UTI in patients with hip fractures. However, the effect sizes of the remaining risk factors demonstrated consistent stability during sensitivity tests. Supplementary Figures 3, 4 provide the detailed results of these sensitivity tests.
Publication bias
A funnel plot was examined for visual inspection, and quantitative assessments using Begg's test and Egger's test were conducted. The results indicated no evidence of publication bias among the included studies (Supplementary Figures 5, 6).
Discussion
As the sole systematic review investigating the risk factors for UTIs in hip fracture patients, this study synthesizes findings from forty-four articles concerning UTI incidence and associated risk factors in this patient population. The primary results are as follows: UTI emerges as a prevalent complication following hip fracture, with an incidence rate reaching up to 11% (95% CI: 8%−14%), consistent with findings reported across multiple studies (54, 55), and influenced by the proportion of female patients in the sample, year of publication, and regional variations. We explore a total of twenty-four potential risk factors, eighteen of which demonstrate significance. While some risk factors may warrant further investigation, our review represents the most current and inclusive assessment available at present.
The majority of studies (14, 15, 17, 20, 21) have identified females as a potential independent risk factor for UTI in hip fracture patients, a finding consistent with the final conclusion of this study. The susceptibility of females to UTI is primarily attributed to the anatomical structure of their short urethra, which is located close to the anus, thereby increasing the risk of bacterial colonization. This unique physiological structure predisposes women to UTI, which is further exacerbated by the decline in estrogen levels after menopause. Recent studies have demonstrated that specific estrogen receptors are expressed on urethral epithelial cells, and the reduction of postmenopausal estrogen alters the immune status of the urethral mucosa, leading to an increased risk of UTI. Hormone replacement therapy is therefore recommended for the prevention and treatment of UTIs in postmenopausal women (56).
This systematic review suggests that elderly hip fracture patients should be cautious about the occurrence of UTI. With the decline of physical function, immune system, bladder urine retention (due to prostate hyperplasia and relaxation of the bladder detrusor muscle), the risk of UTI increases significantly in the elderly population (57). Furthermore, hip fracture patients who have lost their ability to stand and perform self-care may experience a decrease in urinary flow rate and an increase in residual urine, thereby increasing the risk of UTI (58).
Most studies (15, 29, 31) have reported a potential correlation between high body mass index (BMI ≥ 30.0 kg/m2) and UTI in hip fracture patients, suggesting that obese individuals are more susceptible to UTIs. However, the specific mechanisms underlying this association remain unclear. Some articles have proposed that the link between obesity and UTI susceptibility may be attributed to reduced immune response (59, 60). In subgroup analysis, we observed that overweight hip fracture patients did not exhibit a higher risk of UTI compared to patients with normal weight. This finding aligns with the conclusion of Alhabeeb's systematic review (59) on the relationship between BMI and UTI. However, obese hip fracture patients were not as fortunate, as their risk of UTI was 1.23 times higher than that of overweight patients. Moreover, the risk of UTI did not further increase in the morbidly obese hip fracture population.
The question of whether catheterized patients are more prone to UTIs has long been of interest. Kamel's study (18) indicated that the use of catheters may not be associated with an increased risk of UTI, as catheters can alleviate urinary retention and reduce residual urine volume. Conversely, Thomas's study (19) suggested that catheterization could elevate the risk of UTI in hip fracture patients and recommended prompt removal or reevaluation of catheter benefits within 24 h after surgery. Our study provides stronger evidence supporting the occurrence of UTIs in hip fracture patients due to catheterization. This can be explained by the mucosal damage caused by catheter insertion, which provides an opportunity for bacterial colonization due to insufficient urine flushing. Our study emphasizes the importance of thoroughly assessing the individual benefits and risks of catheterization for patients, rather than routine preoperative or postoperative catheterization. Additionally, the lack of differentiation between indwelling and intermittent catheterization in the included studies, as well as the limited number of studies, may have contributed to the absence of significant differences in conclusions regarding the total duration of catheterization. Several studies (7, 20, 27, 32) unanimously suggest a potential relationship between receiving allogeneic red blood cell transfusion during hospitalization and UTIs in hip fracture patients. However, the underlying mechanism linking transfusion and UTI remains unclear, although current research indicates that the host's immune defense undergoes changes after transfusion.
The ASA identifies high-risk patients by assessing comorbidities and other health issues (34). Saadat (7, 34) observed that patients with hip fractures and an ASA score ≥III are more likely to develop UTIs than those with an ASA score of I-II. This finding is consistent with our overall conclusion, suggesting that patients with higher ASA scores may be more susceptible to UTIs. A higher ASA score signifies poorer physical function, debilitation leading to longer bedridden periods, and reduced self-care ability, which may contribute to the increased risk of UTIs.
The impact of anesthesia type on postoperative UTI in hip fracture patients remains controversial. While Morgan's study (36) suggested a possible correlation between general anesthesia and postoperative UTI, Rashid (37) did not support this conclusion. Some scholars even argue that spinal anesthesia may be more likely to lead to postoperative UTI. Our summary results indicate that hip fracture patients who undergo general anesthesia may have a higher risk of developing postoperative UTIs.
Surgical risk factors highlight the need to identify and intervene in high-risk patients for UTI before and during surgery. de Lima (39) reported an increased risk of UTI in patients with intertrochanteric fractures compared to those with femoral neck fractures, although Bliemel's research (14) did not find a corresponding difference. Regarding surgical type, patients undergoing hemiarthroplasty (HHA) appeared significantly older, resulting in a higher incidence of UTI in such patients. This challenges the fixed mindset that total hip replacement surgery carries a higher risk of complications due to its larger trauma and longer postoperative recovery time. The summarized results suggest that we should pay more attention to elderly patients receiving hemiarthroplasty. UTI risk was not significantly affected at the 1-h surgical time point, and it was not found that early surgery recommended in guidelines could reduce complications, possibly due to limited inclusion studies. Finally, our results suggest that hip fracture patients with longer hospital stays may have a higher risk of developing UTIs, which is consistent with the concept of early discharge and recovery.
With advancing research, an expanding body of literature has established a strong correlation between pre-existing comorbidities and postoperative UTIs in hip fracture patients. Recent studies have specifically focused on the association between delirium, dementia, Parkinson's disease, and UTIs. In hip fracture patients, these conditions are characterized by cognitive impairment or acute confusional states, leading to a loss of self-care ability that significantly increases the risk of postoperative UTIs. The influence of diabetes on UTIs after hip fracture is explained by the role of hyperglycemia in compromising the immune system and facilitating bacterial invasion, although the exact underlying mechanism requires further exploration (20). Patients with a medical history of sepsis or prolonged steroid use who are currently suffering from hip fractures may be at an increased risk of developing postoperative UTIs due to immunodeficiency. However, conflicting evidence exists regarding the impact of hypertension and congestive heart failure on UTI susceptibility in hip fracture patients. Therefore, the association between cardiovascular disease and UTI warrants further investigation to elucidate potential mechanisms. Additionally, no significant correlation was found between UTIs and hip fracture patients with COPD or tumors. Serum albumin levels reflect patients' nutritional and immune statuses. However, this study did not establish a conclusive link between preoperative albumin levels and UTI risk.
This study provides recommendations and management strategies to reduce the occurrence of UTIs in patients with hip fractures, based on a systematic review. Firstly, patients admitted due to hip fractures should undergo an assessment of the risk factors for UTIs. For high-risk patients, such as females, older age, obesity, and those with current comorbidities of mental disorders (such as delirium, dementia, Parkinson's) or previous sepsis, it is recommended to enhance urethral care and urine testing during the hospitalization. Additionally, prophylactic use of antibiotics may be considered if necessary. For non-high-risk patients, promoting early mobilization and minimizing hospital stay duration are encouraged in clinical practice to reduce the occurrence of UTIs. Regarding the use of urinary catheters in clinical settings, it is suggested that their removal within a short period or individualized evaluation of their necessity can be beneficial. Special attention should be given to patients undergoing general anesthesia or blood transfusion to prevent UTIs.
Limitation
This study has several limitations, including the lack of robust evidence from randomized controlled trials and mechanistic studies to definitively identify risk factors. Causal relationships cannot be determined, and all associations should be interpreted as such. Furthermore, the assessment of risk factors relied on limited or contradictory non-randomized controlled trials. Future research should aim to include a more extensive range of studies. Finally, our search was confined to mainstream databases, potentially limiting the breadth of information retrieved.
Conclusions
This systematic review and meta-analysis demonstrate that UTI is indeed one of the most common complications in hip fracture patients worldwide, with varying incidence rates depending on geographical regions, year of publication and gender distributions. By focusing on the high-risk populations identified in this study, the aim is to achieve clinical prediction, guide early intervention, and implement targeted management.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
WW: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Writing – original draft, Writing – review & editing. WY: Investigation, Methodology, Software, Validation, Writing – review & editing. WT: Formal analysis, Investigation, Methodology, Software, Writing – review & editing. YL: Formal analysis, Investigation, Methodology, Writing – review & editing. HS: Conceptualization, Investigation, Methodology, Project administration, Writing – review & editing. WD: Conceptualization, Investigation, Project administration, Software, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2024.1360058/full#supplementary-material
Abbreviations
UTI, Urinary tract infection; OR, odds ratio; CI, Confidence Interval; MOOSE, Observational Studies in Epidemiology; ASA, American Society of Anesthesiologists; BMI, Body Mass Index; COPD, Chronic Obstructive Pulmonary Disease; CHF, Congestive Heart Failure; NOS, Newcastle-Ottawa Quality Assessment Scale.
References
1. Socci AR, Casemyr NE, Leslie MP, Baumgaertner MR. Implant options for the treatment of intertrochanteric fractures of the hip: rationale, evidence, and recommendations. Bone Joint J. (2017) 99:128–133. doi: 10.1302/0301-620X.99B1.BJJ-2016-0134.R1
2. Li L, Bennett-Brown K, Morgan C, Dattani R. Hip fractures. Br J Hosp Med. (2020) 81:1–10. doi: 10.12968/hmed.2020.0215
3. Han SB, Kim SB, Shin KH. Risk factors for postoperative pneumonia in patients undergoing hip fracture surgery: a systematic review and meta-analysis. BMC Musculoskeletal Disor. (2022) 23:553. doi: 10.1186/s12891-022-05497-1
4. Gullberg B, Johnell O, Kanis JA. World-wide projections for hip fracture. Osteopor Int. (1997) 7:407–13. doi: 10.1007/PL00004148
5. Singh S, Angus LDG, Munnangi S, Shaikh D, Digiacomo JC, Angara VC, et al. Reducing catheter-associated urinary tract infection: the impact of routine screening in the geriatric hip fracture population. J Trauma Nurs. (2021) 28:290–7. doi: 10.1097/JTN.0000000000000603
6. Goh EL, Lerner RG, Achten J, Parsons N, Griffin XL, Costa PML. Complications following hip fracture: results from the World Hip Trauma Evaluation cohort study. Injury. (2020) 51:1331–6. doi: 10.1016/j.injury.2020.03.031
7. Saadat GH, Alsoof D, Ahmad B, Butler BA, Messer TA, Bokhari F. Incidence, risk factors and clinical implications of postoperative urinary tract infection in geriatric hip fractures. Injury. (2022) 53:2158–62. doi: 10.1016/j.injury.2022.03.012
8. Lee SH, Kim KU. Risk factors for postoperative pneumonia in the elderly following hip fracture surgery: a systematic review and meta-analysis. Geriatr Orthop Surg Rehabil. (2022) 13:21514593221083825. doi: 10.1177/21514593221083825
9. Qi YM Li YJ, Zou JH, Qiu XD, Sun J, Rui YF. Risk factors for postoperative delirium in geriatric patients with hip fracture: a systematic review and meta-analysis. Front Aging Neurosci. (2022) 14:960364. doi: 10.3389/fnagi.2022.960364
10. Wang T, Guo J, Long Y, Yin Y, Hou Z. Risk factors for preoperative deep venous thrombosis in hip fracture patients: a meta-analysis. J Orthopaedics Traumatol. (2022) 23:19–6. doi: 10.1186/s10195-022-00639-6
11. Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. Ottawa: Ottawa Hospital Research Institute (2011) 1–12.
12. Plaza-Carmona M, Requena-Hernández C, Jiménez-Mola S. (2020). Predictors of delirium in octogenarian patients hospitalized for a hip fracture. Int J Environ Res Public Health. 17:7467. doi: 10.3390/ijerph17207467
13. Rajeev A, Railton C, Devalia K. The crucial factors influencing the development and outcomes of postoperative delirium in proximal femur fractures. Aging Med. (2022) 5:94–100. doi: 10.1002/agm2.12206
14. Bliemel C, Buecking B, Hack J, Aigner R, Eschbach DA, Ruchholtz S, et al. Urinary tract infection in patients with hip fracture: an underestimated event? Geriatr Gerontol Int. (2017) 17:2369–75. doi: 10.1111/ggi.13077
15. Crouser N, Malik AT, Phieffer LS, Ly TV, Khan SN, Quatman CE. Urinary tract infection (UTI) at time of geriatric hip fracture surgery increases the risk of experiencing adverse 30-day outcomes. J Clin Orthopaed Trauma. (2019) 10:774–778. doi: 10.1016/j.jcot.2018.07.014
16. Hälleberg Nyman M, Johansson JE, Persson K, Gustafsson M. A prospective study of nosocomial urinary tract infection in hip fracture patients. J Clin Nurs. (2011) 20:2531–9. doi: 10.1111/j.1365-2702.2011.03769.x
17. Hessels AJ, Agarwal M, Liu J, Larson EL. Incidence and risk factors for health-care associated infections after hip operation. Surg Infect. (2016) 17:761–5. doi: 10.1089/sur.2016.062
18. Kamel HK. The frequency and factors linked to a urinary tract infection coding in patients undergoing hip fracture surgery. J Am Med Dir Assoc. (2005) 6:316–20. doi: 10.1097/00130535-200509000-00004
19. Thomas S, Harris N, Dobransky J, Grammatopoulos G, Gartke K, Liew A, et al. Urinary catheter use in patients with hip fracture: Are current guidelines appropriate? A retrospective review. Canadian J Surg. (2021) 64:E630–e635. doi: 10.1503/cjs.014620
20. Yao W, Tang W, Wang W, Lv Q, Ding W. The relationship between admission hyperglycaemia and urinary tract infections in geriatric patients with hip fractures. Int Orthop. (2023) 47:2591–600. doi: 10.1007/s00264-023-05882-y
21. Wiedl A, Förch S, Fenwick A, Mayr E. Incidence, risk-factors and associated mortality of complications in orthogeriatric co-managed inpatients. Geriatr Orthop Surg Rehabil. (2021) 12:2151459321998314. doi: 10.1177/2151459321998314
22. Hotchen AJ, Vonberg FW, Ironside EC, Ross-Thriepland S, Avery N, Pearce OJ. Predictors of infective outcomes following hip fracture: a cohort study. Gerontol Geriatr Med. (2016) 2:2333721416649488. doi: 10.1177/2333721416649488
23. Sørbye LW, Grue EV. Hip fracture and urinary incontinence–use of indwelling catheter postsurgery. Scand J Caring Sci. (2013) 27:632–42. doi: 10.1111/j.1471-6712.2012.01075.x
24. Morandi A, Mazzone A, Bernardini B, Suardi T, Prina R, Pozzi C, et al. Association between delirium, adverse clinical events and functional outcomes in older patients admitted to rehabilitation settings after a hip fracture: A multicenter retrospective cohort study. Geriatr Gerontol Int. (2019) 19:404–8. doi: 10.1111/ggi.13628
25. Muangpaisan W, Wongprikron A, Srinonprasert V, Suwanpatoomlerd S, Sutipornpalangkul W, Assantchai P. Incidence and risk factors of acute delirium in older patients with hip fracture in Siriraj Hospital. J Med Assoc Thailand. (2015) 98:423–430.
26. Panteli M, Giannoudi MP, Lodge CJ, West RM, Pountos I, Giannoudis PV. Mortality and medical complications of subtrochanteric fracture fixation. J Clin Med. (2021) 10:540. doi: 10.3390/jcm10030540
27. García-Alvarez F, Al-Ghanem R, García-Alvarez I, López-Baisson A, Bernal M. Risk factors for postoperative infections in patients with hip fracture treated by means of Thompson arthroplasty. Arch Gerontol Geriatr. (2010) 50:51–5. doi: 10.1016/j.archger.2009.01.009
28. Tsuda Y, Yasunaga H, Horiguchi H, Ogawa S, Kawano H, Tanaka S. Association between dementia and postoperative complications after hip fracture surgery in the elderly: analysis of 87,654 patients using a national administrative database. Arch Orthop Trauma Surg. (2015) 135:1511–7. doi: 10.1007/s00402-015-2321-8
29. Akinleye SD, Garofolo G, Culbertson MD, Homel P, Erez O. The role of BMI in hip fracture surgery. Geriatr Orthop Surg Rehabil. (2018) 9:2151458517747414. doi: 10.1177/2151458517747414
30. Müller M, Gutwerk A, Greve F, Völker L, Zyskowski M, Kirchhoff C, et al. The association between high body mass index and early clinical outcomes in patients with proximal femur fractures. J Clin Med. 9:2076. doi: 10.3390/jcm9072076
31. Scully W, Piuzzi NS, Sodhi N, Sultan AA, George J, Khlopas A, et al. The effect of body mass index on 30-day complications after total hip arthroplasty. Hip Int. (2020) 30:125–34. doi: 10.1177/1120700019826482
32. Shokoohi A, Stanworth S, Mistry D, Lamb S, Staves J, Murphy MF. The risks of red cell transfusion for hip fracture surgery in the elderly. Vox Sang. (2012) 103:223–30. doi: 10.1111/j.1423-0410.2012.01606.x
33. Meyer AC, Eklund H, Hedström M, Modig K. The ASA score predicts infections, cardiovascular complications, and hospital readmissions after hip fracture - a nationwide cohort study. Osteoporosis Int. (2021) 32:2185–92. doi: 10.1007/s00198-021-05956-w
34. Folbert EC, Hegeman JH, Gierveld R, van Netten JJ, Velde DV, Ten Duis HJ, et al. Complications during hospitalization and risk factors in elderly patients with hip fracture following integrated orthogeriatric treatment. Arch Orthop Trauma Surg. (2017) 137:507–15. doi: 10.1007/s00402-017-2646-6
35. Lončarić-Katušin M, Mišković P, Lavrnja-Skolan V, Katušin J, Bakota B, Žunić J. General versus spinal anaesthesia in proximal femoral fracture surgery - treatment outcomes. Injury. (2017) 48 Suppl 5:S51–s55. doi: 10.1016/S0020-1383(17)30740-4
36. Morgan L, McKeever TM, Nightingale J, Deakin DE, Moppett IK. Spinal or general anaesthesia for surgical repair of hip fracture and subsequent risk of mortality and morbidity: a database analysis using propensity score-matching. Anaesthesia. (2020) 75:1173–9. doi: 10.1111/anae.15042
37. Rashid RH, Shah AA, Shakoor A, Noordin S. Hip fracture surgery: does type of anesthesia matter? Biomed Res Int. (2013) 2013:252356. doi: 10.1155/2013/252356
38. Ng JPH, Tan TL, Pillai A, Ho SWL. Outcomes of ultra-old vs old patients after hip fracture surgery: a matched cohort analysis of 1524 patients. Arch Orthop Trauma Surg. (2023) 143:3145–54. doi: 10.1007/s00402-022-04550-x
39. Lima BR, Nunes BKG, Guimarães L, Almeida LF, Pagotto V. Incidence of delirium following hospitalization of elderly people with fractures: risk factors and mortality. Rev Esc Enferm USP. (2021) 55:e20200467. doi: 10.1590/1980-220x-reeusp-2020-0467
40. Anthony CA, Duchman KR, Bedard NA, Gholson JJ, Gao Y, Pugely AJ, et al. Hip fractures: appropriate timing to operative intervention. J Arthroplasty. (2017) 32:3314–8. doi: 10.1016/j.arth.2017.07.023
41. Dawson D, Milligan D, Callachand F, Cusick L. Hip hemi-arthroplasty vs total hip replacement for displaced intra-capsular hip fractures: retrospective age and sex matched cohort study. Ulster Med J. (2018) 87:17–21.
42. Huang Y, Yang Q, Wang Z, Pan Z, Zhang Y, Shi Z, et al. Comparisons of in-hospital complications between total hip arthroplasty and hip resurfacing arthroplasty. BMC Musculoskeletal Disor. (2023) 24:375. doi: 10.1186/s12891-023-06487-7
43. Liodakis E, Antoniou J, Zukor DJ, Huk OL, Epure LM, Bergeron SG. Major complications and transfusion rates after hemiarthroplasty and total hip arthroplasty for femoral neck fractures. J Arthroplasty. (2016) 31:2008–12. doi: 10.1016/j.arth.2016.02.019
44. Miller CP, Buerba RA, Leslie MP. Preoperative factors and early complications associated with hemiarthroplasty and total hip arthroplasty for displaced femoral neck fractures. Geriatr Orthop Surg Rehabil. (2014) 5:73–81. doi: 10.1177/2151458514528951
45. Huang YF, Cherng YG, Hsu SP, Yeh CC, Chou YC, Wu CH, et al. Risk and adverse outcomes of fractures in patients with Parkinson's disease: two nationwide studies. Osteoporosis Int. (2015) 26:1723–32. doi: 10.1007/s00198-015-3052-y
46. Mathew PG, Sponer P, Kucera T, Grinac M, Knízek J. Total HIP arthroplasty in patients with Parkinson's disease. Acta Med. (2013) 56:110–6. doi: 10.14712/18059694.2014.18
47. Nguyen PV, Hjelholt TJ, Heide-Jørgensen U, Pedersen AB. Postoperative complications, mortality, and quality of in-hospital care among hip fracture patients with Parkinson's disease. Injury. (2022) 53:2150–7. doi: 10.1016/j.injury.2022.03.015
48. Ekström W, Al-Ani AN, Sääf M, Cederholm T, Ponzer S, Hedström M. Health related quality of life, reoperation rate and function in patients with diabetes mellitus and hip fracture–a 2 year follow-up study. Injury. (2013) 44:769–75. doi: 10.1016/j.injury.2012.10.003
49. Golinvaux NS, Bohl DD, Basques BA, Baumgaertner MR, Grauer JN. Diabetes confers little to no increased risk of postoperative complications after hip fracture surgery in geriatric patients. Clin Orthop Relat Res. (2015) 473:1043–51. doi: 10.1007/s11999-014-3945-7
50. Martínez-Huedo MA, Jiménez-García R, Jiménez-Trujillo I, Hernández-Barrera V, Del Rio Lopez B, López-de-Andrés A. Effect of type 2 diabetes on in-hospital postoperative complications and mortality after primary total hip and knee arthroplasty. J Arthroplasty. (2017) 32:3729–3734.e3722. doi: 10.1016/j.arth.2017.06.038
51. Tian W, Wu J, Tong T, Zhang L, Zhou A, Hu N, et al. Diabetes and risk of post-fragility hip fracture outcomes in elderly patients. Int J Endocrinol. (2020) 2020:8146196. doi: 10.1155/2020/8146196
52. Glassou EN, Kjørholt KK, Hansen TB, Pedersen AB. Delay in surgery, risk of hospital-treated infections and the prognostic impact of comorbidity in hip fracture patients. A Danish nationwide cohort study, 2005–2016. Clin Epidemiol. (2019) 11:383–395. doi: 10.2147/CLEP.S200454
53. Vidán MT, Sánchez E, Gracia Y, Marañón E, Vaquero J, Serra JA. Causes and effects of surgical delay in patients with hip fracture: a cohort study. Ann Intern Med. (2011) 155:226–33. doi: 10.7326/0003-4819-155-4-201108160-00006
54. Rosencher N, Vielpeau C, Emmerich J, Fagnani F, Samama CM. Venous thromboembolism and mortality after hip fracture surgery: the ESCORTE study. J Thromb Haemost. (2005) 3:2006–14. doi: 10.1111/j.1538-7836.2005.01545.x
55. Prieto-Alhambra D, Reyes C, Sainz MS, González-Macías J, Delgado LG, Bouzón CA, et al. In-hospital care, complications, and 4-month mortality following a hip or proximal femur fracture: the Spanish registry of osteoporotic femur fractures prospective cohort study. Arch. Osteopor. (2018) 13:96. doi: 10.1007/s11657-018-0515-8
56. Perrotta C, Aznar M, Mejia R, Albert X, Ng CW. Oestrogens for preventing recurrent urinary tract infection in postmenopausal women. Cochr Datab System Rev. (2008) 2008:CD005131. doi: 10.1002/14651858.CD005131.pub2
57. Foxman B. Urinary tract infection syndromes: occurrence, recurrence, bacteriology, risk factors, and disease burden. Infect Dis Clin North Am. (2014) 28:1–13. doi: 10.1016/j.idc.2013.09.003
58. Rønfeldt I, Larsen LK, Pedersen PU. Urinary tract infection in patients with hip fracture. Int J Orthopaed Trauma Nurs. (2021) 41:100851. doi: 10.1016/j.ijotn.2021.100851
59. Alhabeeb H, Baradwan S, Kord-Varkaneh H, Tan SC, Low TY, Alomar O, et al. Association between body mass index and urinary tract infection: a systematic review and meta-analysis of observational cohort studies. Eating Weight Disor. (2021) 26:2117–25. doi: 10.1007/s40519-020-01101-4
Keywords: urinary tract infection, UTI, hip fracture, risk factors, meta-analysis
Citation: Wang W, Yao W, Tang W, Li Y, Sun H and Ding W (2024) Risk factors for urinary tract infection in geriatric hip fracture patients: a systematic review and meta-analysis. Front. Med. 11:1360058. doi: 10.3389/fmed.2024.1360058
Received: 22 December 2023; Accepted: 29 January 2024;
Published: 09 February 2024.
Edited by:
Vered Hermush, Technion Israel Institute of Technology, IsraelCopyright © 2024 Wang, Yao, Tang, Li, Sun and Ding. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wenbo Ding, ZHdiOTgwMDMwMDdAMTYzLmNvbQ==; Hongbo Sun, c2hiMTk5NzEwQDE2My5jb20=
 Wei Wang
Wei Wang Wanyun Tang
Wanyun Tang Wenbo Ding
Wenbo Ding