- 1Department of Anesthesiology, First Affiliated Hospital of Dalian Medical University, Dalian, China
- 2Department of Graduate, Dalian Medical University, Dalian, China
- 3Department of Anesthesiology, Dalian Medical University, Dalian, China
Background: The rapid growth of online education has led to the extensive exploration of innovative teaching methods to improve learning outcomes in medical training. This study aimed to evaluate the effectiveness of online scenario-based simulation in an airway management course for undergraduate anesthesia students.
Methods: A total of 130 undergraduate students participated in an online airway management course. The primary objective was to assess the effectiveness of this teaching method by comparing post-class quiz scores. Secondary outcomes were evaluated based on technical and non-technical skills scores across four simulation scenarios. An anonymous questionnaire was also distributed to gather students’ perceptions and experiences.
Results: The simulation group exhibited a significant improvement in post-class quiz scores compared to the traditional group (p < 0.001). In the second simulation, students showed enhanced technical skills across all four scenarios (p = 0.030, p = 0.037, p = 0.028, p = 0.028, respectively), as well as improved non-technical skills, including task management, teamwork, communication, vigilance, crisis identification, decision-making, and self-confidence. Questionnaire responses indicated that students found the course both enjoyable and beneficial in improving their problem-solving abilities. Additionally, 97.3% of participants felt the course enhanced their self-learning and teamwork skills, while 97.22% reported it facilitated mastery of anesthesia techniques.
Conclusion: Online scenario-based simulation teaching has proven to be a highly effective and engaging educational tool for undergraduate anesthesia students. It significantly improves both technical and non-technical skills while promoting critical thinking and problem-solving development.
1 Background
The rapid advancement of mobile Internet technology has positioned online medical education as a pivotal approach in medical training, primarily due to its flexibility and accessibility, which overcome the traditional limitations of time and space (1). This integration of medical education with online platforms has led to the emergence of various innovative educational models (2, 3). During the COVID-19 pandemic, our institution, like many others globally, shifted to online teaching (4). However, this transition presented significant challenges, especially in courses focusing on clinical skills. The conventional online teaching model often struggles to foster active student participation and engagement in the learning process (5, 6). Traditional teaching methods typically rely on one-way knowledge transmission through lectures, theoretical instruction, and limited video demonstrations, providing few opportunities for students to actively engage or participate in hands-on practice (7, 8). These challenges are amplified in an online setting, where the absence of immediate interaction and feedback—typical in face-to-face communication—further reduces student engagement (9). Given the highly practical nature of anesthesiology and the limited existing research on web-based anesthesia education, it is essential to explore and develop effective online teaching strategies for professional skills training to enhance the quality of teaching and learning in this domain.
Simulation training, which involves creating realistic medical scenarios where students assume various roles, is a valuable teaching method (10). It not only organizes and integrates theoretical knowledge but also effectively bridges the gap between foundational knowledge and clinical practice (11). Furthermore, it helps students enhance their teamwork, critical thinking, and clinical decision-making skills (12). Given the limited clinical experience of undergraduate students, which often results in challenges in applying knowledge flexibly and difficulties in crisis management and diagnosis (13), online simulation-based teaching can effectively address these gaps. Additionally, it can stimulate students’ interest in learning and improve their clinical reasoning and communication abilities (14, 15).
Students’ limited clinical experience was found to hinder their performance during initial simulation exercises in previous simulation-based teaching activities (13). To enhance the effectiveness of simulation training, a question-and-answer session was incorporated prior to the simulation activities. This session was designed to help students consolidate theoretical knowledge and prepare for the practical scenarios they would encounter. Additionally, debriefing is commonly integrated into the teaching process to optimize the outcomes of simulation training (16). In this phase, instructors guide students to critically evaluate the simulation process and review their clinical performance, fostering systematic and reflective learning while addressing areas for improvement (16, 17). This approach is particularly crucial in medical education, as it emphasizes collaboration, situational learning, and the development of presentation and decision-making skills (12, 18). With this method, students are more engaged in the online course, while instructors maintain greater control over the learning process, ultimately enhancing teaching quality (19).
Airway management is a critical responsibility for anesthesiologists. The identification and management of difficult airways present significant challenges, as inadequate management can lead to severe complications (20). To tackle these challenges, this study focused on teaching content related specifically to difficult airway management. Initially, students consolidated their theoretical knowledge of difficult airways through a question-and-answer session. Following this, online simulation teaching was implemented, incorporating effective debriefing techniques. In summary, this study aims to evaluate the efficacy of scenario-based simulation teaching in an online airway management course.
2 Materials and methods
2.1 Ethical approval and informed consent
The entire training process was conducted online via Tencent Meeting, with the simulation teaching facilitated through vital signs simulation software. No patients were involved or harmed during this study. The study was covered under the ethics review of the First Affiliated Hospital of Dalian Medical University and received approval from the teaching management of Dalian Medical University. The curriculum followed the teaching standards of Dalian Medical University. This study adhered to the Declaration of Helsinki and the ethical review guidelines of the First Affiliated Hospital of Dalian Medical University. All procedures were conducted in compliance with relevant guidelines and regulations, including but not limited to the use of online teaching platforms, confidentiality of student data, and privacy protection. Formal consent was obtained from all participants.
2.2 Sample and sample size
The sample size was calculated based on the primary outcome variable, measured by post-class quiz scores. According to our pilot study, the mean post-class quiz score in the traditional group was 29.03 with a standard deviation of 6.27. This study hypothesized a five-point difference in post-class quiz scores between the traditional group and the simulation group. Thus, a sample size of 84 students was required, assuming α = 0.05 and β = 0.05. To account for potential data loss, 130 participants were enrolled. All students were in their fourth year of university, with 65 participants in the simulation teaching group and 65 in the traditional teaching group. The sample size calculation was performed using PASS version 15.0.
2.3 Preparation phase
A total of 130 students participated in the study. All participants had previously completed the theoretical course in anesthesia and relevant training in tracheal intubation. Before the course, students were provided with study materials, including the latest airway management guidelines (20), in both Chinese and English. Each student was required to review these materials alongside the textbook before attending the class.
2.4 Pre-class quiz
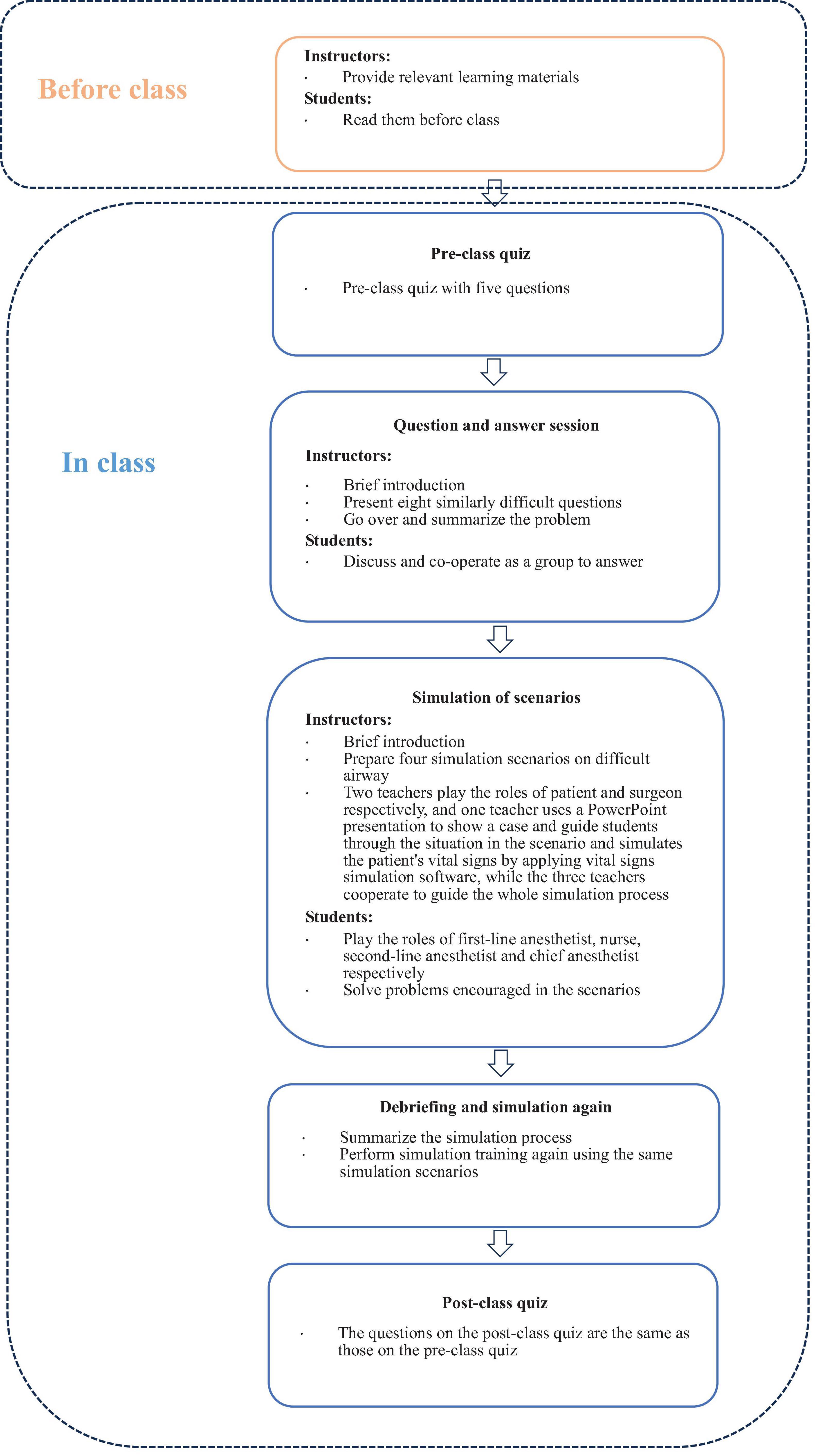
The detailed process of the web-based anesthesia teaching study is outlined in Figure 1. All students first completed a 20 min quiz assessing their knowledge of airway management. The quiz covered topics including: (1) how to perform airway assessments in patients with head and neck trauma; (2) preparation for tracheal intubation and extubation precautions in patients with pharyngeal tumors; (3) causes of hypoxia after anesthesia induction in patients with normal preoperative airway assessment; (4) measures to take after multiple failed intubations during general anesthesia induction. The instructor did not provide answers during the quiz, and the results were kept concealed. The same topics were retested at the end of the class to evaluate changes in students’ proficiency in professional knowledge.
2.5 Question and answer session
To enhance the effectiveness of simulation training, a question-and-answer session was introduced prior to the simulation exercises, aimed at reinforcing students’ theoretical knowledge and preparing them for the practical scenarios they would face. Students were randomly assigned to eight groups, each consisting of four members. Eight questions of comparable difficulty were prepared, with each group assigned one question to answer, and their responses were scored. Once a group completed its answer, other groups were invited to provide supplementary responses and earn points for correct answers. Following the session, detailed explanations were provided for each question. Topics covered included: (1) risk factors for difficult mask ventilation; (2) risk factors for difficult tracheal intubation; (3) methods for awake tracheal intubation; (4) strategies for managing anticipated difficult tracheal intubation; (5) grading of laryngoscopic exposure; (6) treatments for bronchospasm; (7) techniques for establishing an invasive airway; and (8) considerations for extubating patients with difficult tracheal intubation.
2.6 Scenario simulation training process
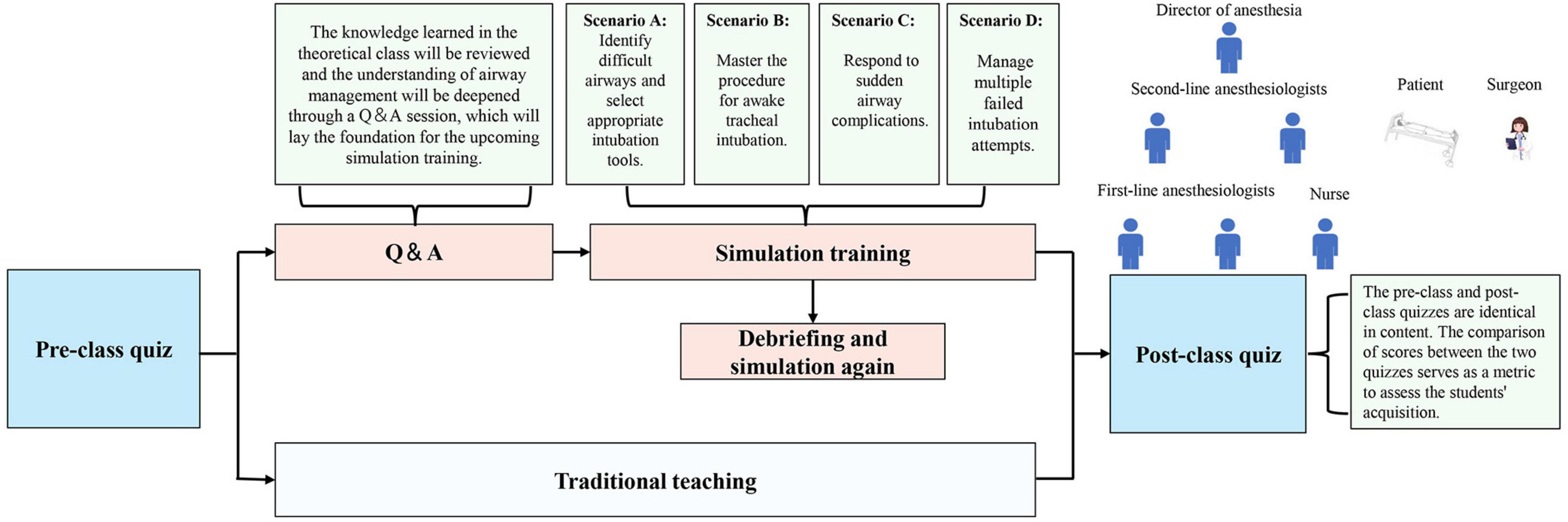
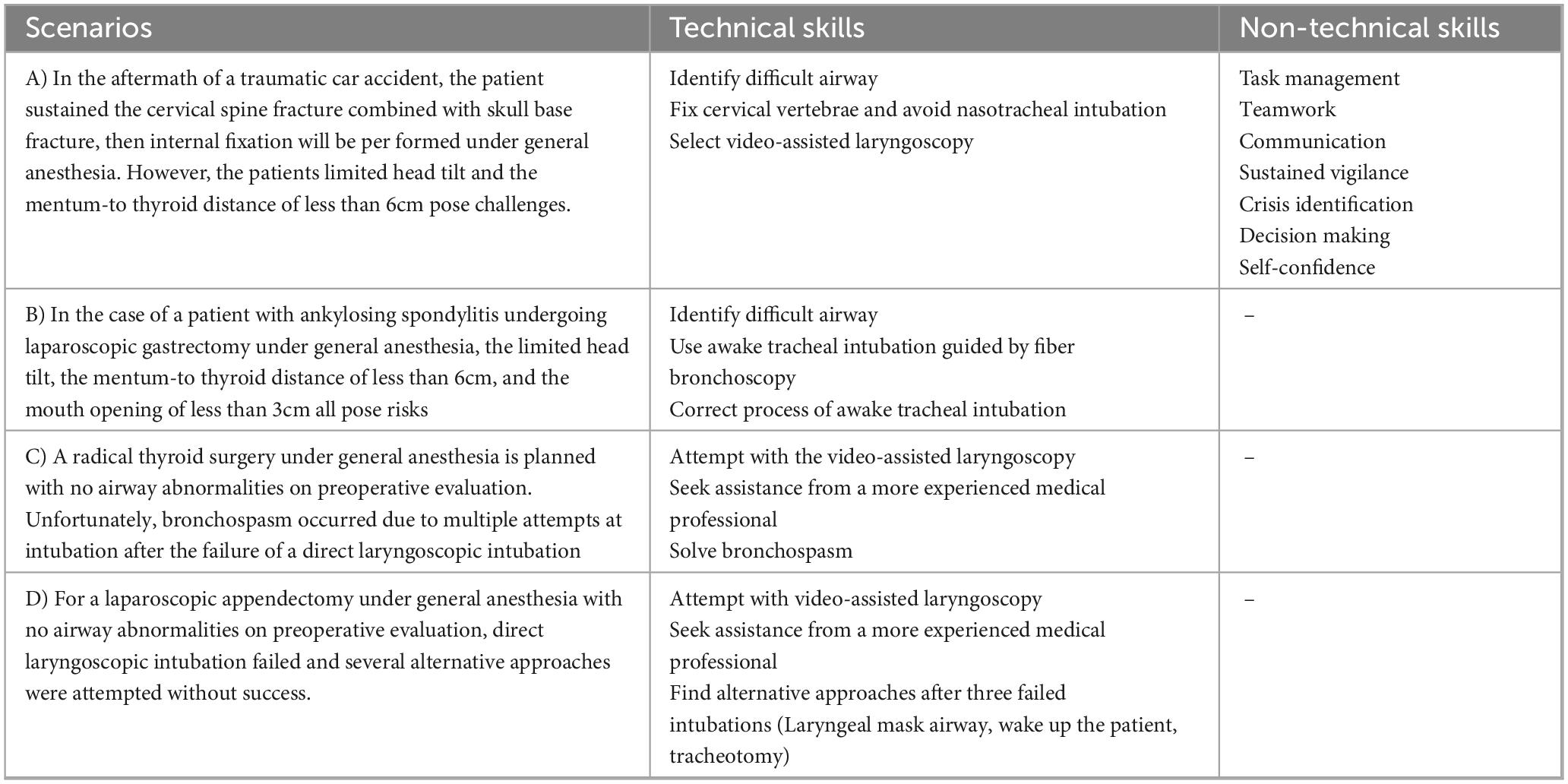
Prior to the training, roles were assigned to participants: two first-line anesthesiologists, two second-line anesthesiologists, an anesthesia director, and a nurse. To support the simulation, two instructors took on the roles of patient and surgeon, respectively (the structure and scenarios of the online simulation are illustrated in Figure 2). The instructor provided a thorough briefing on the simulation process, outlining the method and the responsibilities of each role. The simulation was designed to closely replicate the clinical workflow, including a preoperative patient visit and scenarios where first-line anesthesiologists sought assistance from second-line anesthesiologists or the director when encountering challenges. Four simulation scenarios were prepared: two for anticipated difficult airways and two for unanticipated difficult airways (Table 1). Virtual props, such as laryngoscopes, laryngeal masks, light sticks, fiberoptic bronchoscopes, and other relevant tools, as well as drugs used in simulations, were provided to the students. One instructor utilized a PowerPoint presentation to present case details (patient history, past medical history, relevant examinations, type of surgery, etc.) and a simulated training scenario in the operating room. Vital signs simulation software was employed to simulate the patient’s real-time vital signs, adjusting them based on the students’ actions. The other instructor played the role of the patient, simulating stress responses (e.g., choking, nausea, dyspnea) in reaction to the students’ interventions. The instructor guided the students through appropriate responses, utilizing PowerPoint to present emergency scenarios during the simulation (a demonstration of specific parts of the simulation is available in Supplementary Material 1). Students had the opportunity to communicate with both the patient and the surgeon at any point to gather information on the patient’s medical history and the surgical procedure. Each scenario lasted 20 min, followed by a teacher-led debriefing that addressed both technical and non-technical aspects of the simulation. Afterward, the same students participated in a second simulation. The instructor assessed and scored their performance across both simulations. Upon completion of each case, the instructor provided a comprehensive summary, including an analysis of any adverse patient effects and an evaluation of whether appropriate actions and precautions were taken.
2.7 Evaluation of scenario simulation training
The instructor evaluated the entire simulation process using both technical and non-technical criteria. Technical points were awarded according to the following scoring system: two points for each completed exercise, two points for completing all exercises, one point for completing more than 50% of the exercises, and 0.5 points for completing less than 50%. Non-technical points were assessed based on the criteria established by the Stanford Anesthesia Cognitive Aid Group (21), covering aspects such as task management (e.g., task allocation, equipment preparation), teamwork, communication, sustained vigilance, crisis identification, decision-making, and self-confidence (non-technical criteria detailed in Supplementary Material 2). Each fully completed item earned 1 point, partially completed items were awarded 0.5 points, and incomplete items received 0 points. The detailed scoring scale for scenario simulation teaching is provided in Table 1.
2.8 Post-class quiz
A post-class quiz was administered at the end of the course, using the same questions as the pre-class quiz, to assess the effectiveness of the teaching modality by comparing pre- and post-class quiz scores.
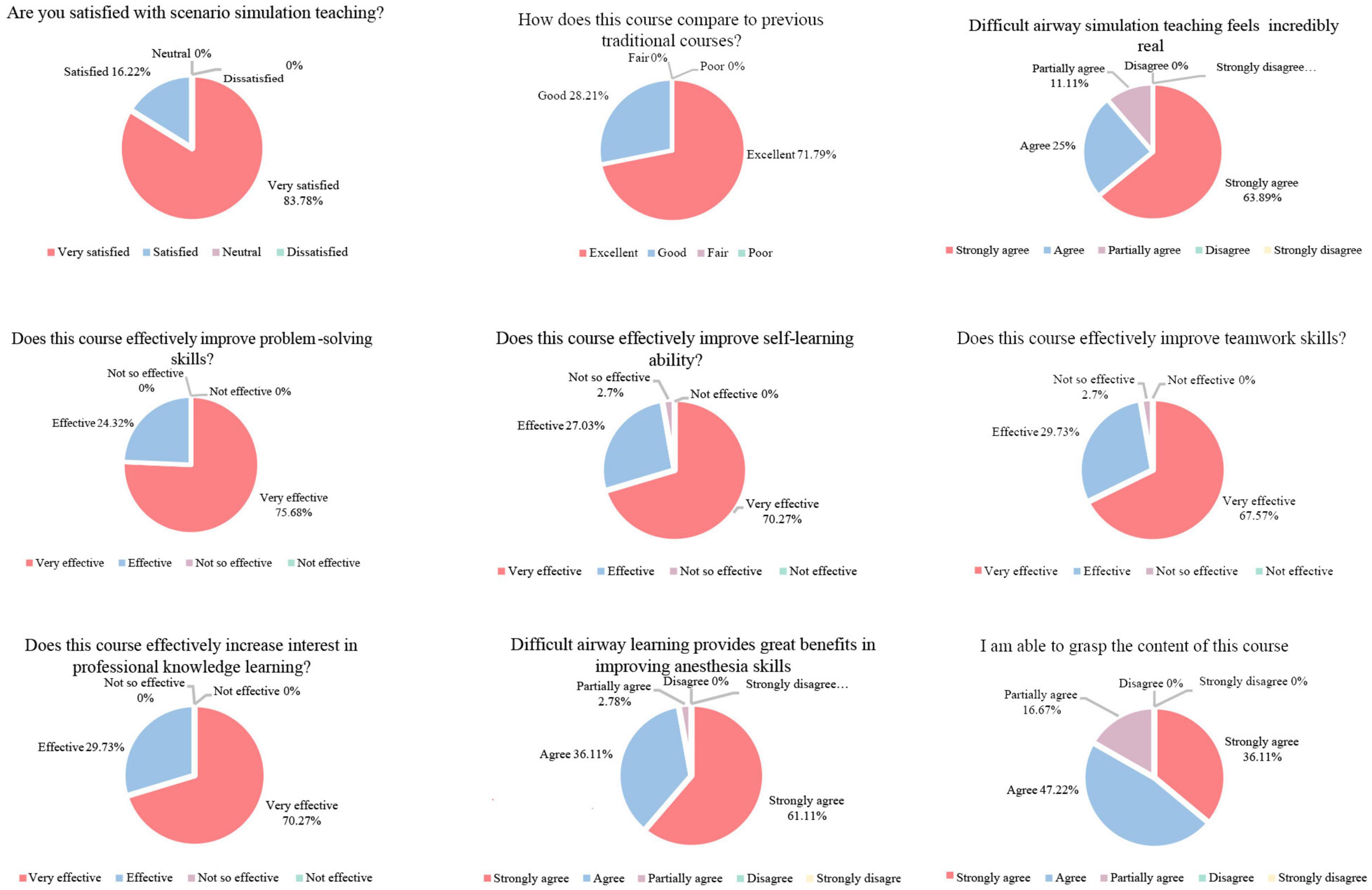
2.9 Questionnaire
An anonymous online questionnaire was distributed to gather student feedback. The questionnaire included the following questions: (1) Are you satisfied with scenario simulation teaching? (2) How does this course compare to previous traditional courses? (3) Difficult airway simulation teaching feels incredibly real. (4) Does this course effectively improve problem-solving skills? (5) Does this course effectively improve self-learning ability? (6) Does this course effectively improve teamwork skills? (7) Does this course effectively increase interest in professional knowledge learning? (8) Difficult airway learning provides great benefits in improving anesthesia skills? (9) I am able to grasp the content of this course.
2.10 Statistical analysis
This study was a controlled trial, with students assigned to either the simulation or traditional teaching groups to evaluate the effectiveness of the online simulation. The primary objective was to assess the impact of the teaching modality by comparing post-class quiz scores. Secondary outcomes were evaluated based on technical and non-technical skills scores across two simulation scenarios. Data were presented as mean ± standard deviation. Post-class quiz scores were compared using a t-test. Both technical and non-technical skills in each of the four scenarios were analyzed using a paired t-test. Descriptive statistics were employed to summarize the questionnaire data, with frequency distributions and percentages used to illustrate the proportions within each category. A significance level of α = 0.05 was applied, with p < 0.05 considered statistically significant.
3 Results
3.1 Student basic information
Table 2 provides a comprehensive overview of participant information. All students had successfully completed theoretical coursework and practical exams; however, they had not undergone clinical practice.
3.2 Web-based anesthesia simulation teaching enhanced students’ understanding of airway management
Figure 3 illustrates the quiz scores of 130 students, showing a significant increase in post-class scores for the simulation group compared to the traditional group (p < 0.001). There were no significant differences in pre-class scores.

Figure 3. Comparison of post-class quiz scores between traditional group and simulation group. Post-class quiz scores are presented as means ± SD. Significantly different from the simulation group at ***P < 0.001.
3.3 Web-based anesthesia simulation teaching demonstrated high effectiveness
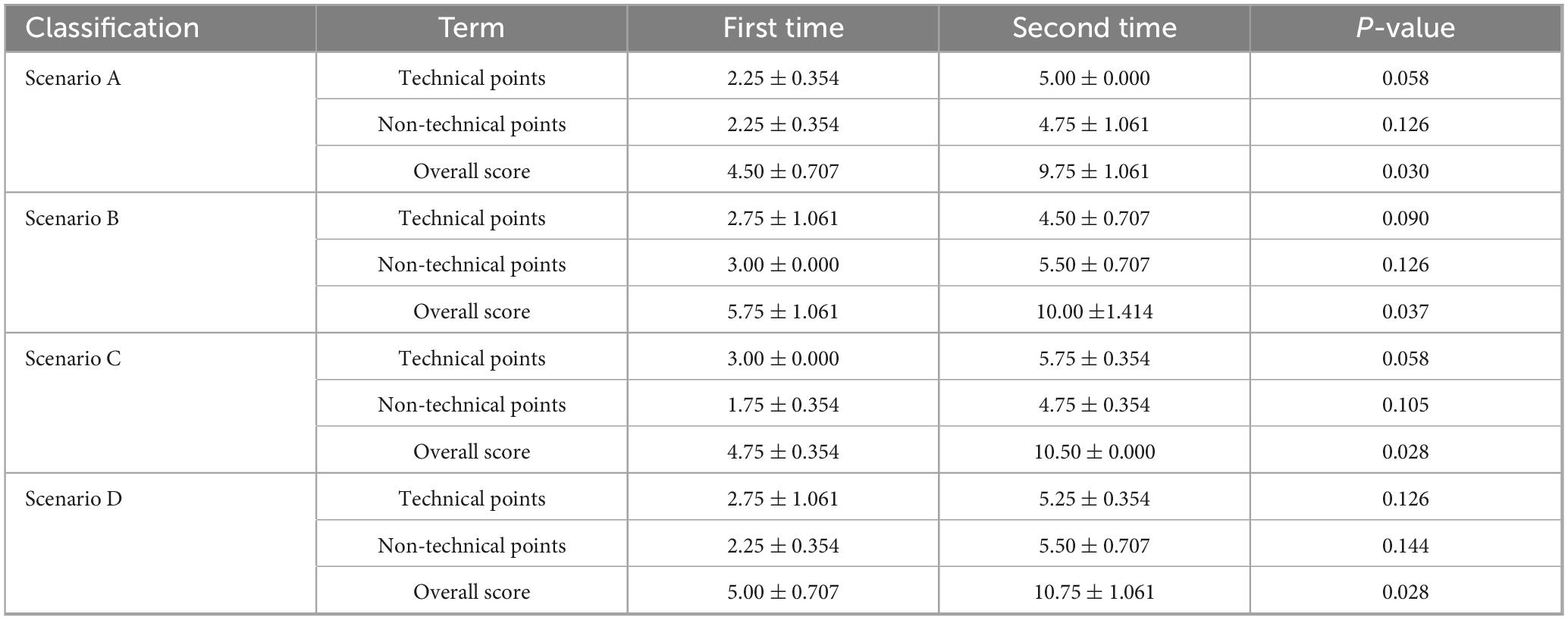
Table 3 presents the evaluation of technical and non-technical points across four scenarios: two anticipated difficult airway scenarios and two unanticipated difficult airway scenarios. While no significant differences were observed in technical and non-technical points across the scenarios, the total scores (technical + non-technical) for all four scenarios demonstrated a statistically significant improvement during the second attempt compared to the first (p < 0.05).
3.4 Course feedback and satisfaction survey results
The survey results (Figure 4) revealed that all students expressed a preference for scenario simulation teaching, finding it superior and more engaging than their previous learning methods. The students highly valued this teaching approach. Specifically, 88.89% of participants found the simulation scenarios in the airway management course to be realistic. Additionally, 97.3% of students reported that the course enhanced their self-learning and teamwork skills, while 97.22% indicated that it improved their abilities in difficult airway management. A majority of students (83.33%) felt confident in their mastery of the course content. Overall, the survey responses unanimously indicated that the course effectively fostered independent exploration and problem-solving skills, with students subjectively reporting that this teaching method positively impacted their learning outcomes.
4 Discussion
The COVID-19 pandemic has profoundly reshaped the landscape of medical education, accelerating the widespread adoption of online teaching methods (22). While traditional online approaches offer increased accessibility, they often struggle to engage students effectively and fail to foster clinical reasoning (23), particularly in hands-on fields like anesthesia. Online scenario simulation teaching presents a promising solution to these limitations (23).
Simulation-based learning, long valued for its ability to replicate realistic clinical scenarios, allows students to apply theoretical knowledge in a controlled, risk-free environment (12). By integrating online platforms with simulation training, the flexibility and accessibility of the Internet can be combined with the interactive and immersive nature of simulation exercises (24). This hybrid approach not only enhances students’ technical competencies but also promotes the development of essential non-technical skills, such as teamwork, communication, and crisis management (12, 18, 25). Online simulation training offers students the opportunity to encounter and manage a variety of airway scenarios, including both anticipated and unanticipated difficult airways, without the risks associated with real clinical settings (26). For undergraduate students preparing to enter clinical practice, this simulation course equips them with the confidence needed to navigate complex clinical situations in their future careers (27). Moreover, the online format eliminates the need for physical presence in a simulation center, increasing accessibility for a larger number of students while reducing costs and enhancing convenience compared to traditional simulation training (24).
To maximize the effectiveness of simulation training, we facilitated students’ consolidation of knowledge related to difficult airways by posing a series of open-ended questions prior to the simulation exercises. This method not only fostered critical thinking but also maintained high levels of student engagement and motivation throughout the training (28, 29).
Our findings indicated that web-based anesthesia simulations significantly enhanced students’ understanding of airway management, facilitated the translation of theoretical knowledge into practical skills, and improved performance in subsequent simulations. Additionally, non-technical skills—such as task management, teamwork, communication, sustained vigilance, crisis identification, decision-making, and self-confidence—also showed marked improvement. The benefits of this simulation training included increased confidence, reduced anxiety, and improved proficiency (30). In the present study, post-class quiz scores from the simulation group significantly outperformed those from the traditional group, confirming the effectiveness of scenario simulation training.
Questionnaire results revealed that all students found the approach beneficial, enhancing their learning efficiency and interest in systematic professional development. Specifically, 97.3% of students reported improvements in self-learning and teamwork skills, while 97.22% felt the course enhanced their difficult airway management capabilities and believed the teaching method positively impacted their learning outcomes. Through the integration of online teaching and scenario simulation, undergraduate anesthesia students developed essential crisis management skills, crucial for addressing practical clinical challenges.
Overall, our findings indicate that online scenario simulation training is both highly effective and engaging for anesthesia education. These results align with studies in nursing and pharmacy education, which have shown that online simulation teaching improves students’ learning outcomes and offers a positive educational experience (31, 32). Furthermore, students have demonstrated enhanced execution and leadership skills in crisis situations (33). Another study found that students involved in online simulation-based teaching exhibited significant improvements in knowledge acquisition, with the interactive nature of simulation-based learning proving particularly effective in fostering enthusiasm for the subject matter (34).
In online simulation teaching, active student engagement is essential. However, instructors often face challenges in closely monitoring student involvement and accurately assessing participation rates in an online environment (35). This lack of control can directly affect the quality of instruction and hinder the achievement of desired learning outcomes (18). Direct debriefing effectively addresses these challenges by extending teaching sessions, motivating students, and enhancing instructors’ control over the online classroom (36). Based on the learning outcomes observed during the direct debriefing phase, instructors can guide students back into simulation scenarios, help them identify areas of weakness, supplement their knowledge, and integrate it into a coherent framework (37). Additionally, debriefing encourages students to articulate their thoughts and emotions, promoting reflection on both individual and collective experiences (38).
Despite these promising results, several limitations exist in this study. First, the absence of blinding led to potential bias in the analysis of subjective observations. Second, the study did not include follow-up assessments to evaluate the long-term impact of online simulation training on students’ clinical practice. Future work will involve tracking these students’ progress over the long term to assess the continued influence of this teaching method. Additionally, multicenter, randomized controlled trials with larger sample sizes will be conducted to further investigate the effectiveness of this approach.
5 Conclusion
In conclusion, online scenario simulation training has proven to be a highly effective and engaging educational tool for undergraduate anesthesia students. Incorporating this training into the curriculum not only enhances students’ technical and non-technical skills but also fosters the development of critical thinking and problem-solving abilities.
Data availability statement
The datasets analyzed in this study are available from the corresponding authors on a reasonable request.
Ethics statement
The studies involving humans were approved by First Affiliated Hospital of Dalian Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
YL: Writing – original draft, Writing – review and editing, Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization. T-tW: Writing – original draft, Writing – review and editing. Y-yH: Investigation, Software, Supervision, Validation, Visualization, Writing – review and editing. X-yL: Conceptualization, Project administration, Writing – review and editing. L-jG: Software, Writing – review and editing. SH: Writing – review and editing. PG: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review and editing. Q-pW: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review and editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by Liaoning Teaching Science Researching Program, China (Grant No. JG21DB154).
Acknowledgments
We would like to thank the students who participated in this study. We would also like to thank Yi-tong Zhang for her efforts and performance during this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2025.1563540/full#supplementary-material
References
1. Chandran V, Balakrishnan A, Rashid M, Pai Kulyadi G, Khan S, Devi E, et al. Mobile applications in medical education: A systematic review and meta-analysis. PLoS One. (2022) 17:e0265927. doi: 10.1371/journal.pone.0265927
2. Almutawa J, Nicolaou C. Medical students’ view on enhancing engagement in online teaching. Med Teach. (2022) 44:697. doi: 10.1080/0142159X.2021.1970733
3. Chang M, Liao M, Lue J, Yeh C. The impact of asynchronous online anatomy teaching and smaller learning groups in the anatomy laboratory on medical students’ performance during the Covid-19 pandemic. Anat Sci Educ. (2022) 15:476–92. doi: 10.1002/ase.2179
4. Chan E, Khong M, Torda A, Tanner J, Velan G, Wong G. Medical teachers’ experience of emergency remote teaching during the COVID-19 pandemic: A cross-institutional study. BMC Med Educ. (2022) 22:303. doi: 10.1186/s12909-022-03367-x
5. Kaup S, Jain R, Shivalli S, Pandey S, Kaup S. Sustaining academics during COVID-19 pandemic: The role of online teaching-learning. Indian J Ophthalmol. (2020) 68:1220–1. doi: 10.4103/ijo.IJO_1241_20
6. Longhurst G, Stone D, Dulohery K, Scully D, Campbell T, Smith C. Strength, weakness, opportunity, threat (SWOT) analysis of the adaptations to anatomical education in the United Kingdom and republic of ireland in response to the covid-19 Pandemic. Anat Sci Educ. (2020) 13:301–11. doi: 10.1002/ase.1967
7. Michael J. Where’s the evidence that active learning works? Adv Physiol Educ. (2006) 30:159–67. doi: 10.1152/advan.00053.2006
8. Rossi I, de Lima J, Sabatke B, Nunes M, Ramirez G, Ramirez M. Active learning tools improve the learning outcomes, scientific attitude, and critical thinking in higher education: Experiences in an online course during the COVID-19 pandemic. Biochem Mol Biol Educ. (2021) 49:888–903. doi: 10.1002/bmb.21574
9. Wilcha R. Effectiveness of virtual medical teaching during the COVID-19 crisis: Systematic review. JMIR Med Educ. (2020) 6:e20963. doi: 10.2196/20963
10. Gong T, Wang Y, Pu H, Yin L, Zhou M. Study on the application value of PBL combined with situational simulation teaching method in clinical practice teaching of radiology department. Comput Math Methods Med. (2022) 2022:6808648. doi: 10.1155/2022/6808648
11. Koukourikos K, Tsaloglidou A, Kourkouta L, Papathanasiou I, Iliadis C, Fratzana A, et al. Simulation in clinical nursing education. Acta Inform Med. (2021) 29:15–20. doi: 10.5455/aim.2021.29.15-20
12. Seam N, Lee A, Vennero M, Emlet L. Simulation training in the ICU. Chest. (2019) 156:1223–33. doi: 10.1016/j.chest.2019.07.011
13. Gao P, Wang C, Liu S, Tran K, Wen Q. Simulation of operating room crisis management - hypotension training for pre-clinical students. BMC Med Educ. (2021) 21:60. doi: 10.1186/s12909-020-02477-8
14. Hofmann H, Harding C, Youm J, Wiechmann W. Virtual bedside teaching rounds with patients with COVID-19. Med Educ. (2020) 54:959–60. doi: 10.1111/medu.14223
15. Chandra S, Laoteppitaks C, Mingioni N, Papanagnou D. Zooming-out COVID-19: Virtual clinical experiences in an emergency medicine clerkship. Med Educ. (2020) 54:1182–3. doi: 10.1111/medu.14266
16. Meny L, de Voest M, Salvati L. Assessment of student pharmacist learning within an interprofessional simulation: A comparison of small group vs. large group debriefing. Curr Pharm Teach Learn. (2019) 11:533–7. doi: 10.1016/j.cptl.2019.02.007
17. Eppich W, Hunt E, Duval-Arnould J, Siddall V, Cheng A. Structuring feedback and debriefing to achieve mastery learning goals. Acad Med. (2015) 90:1501–8. doi: 10.1097/ACM.0000000000000934
18. Khan R, Atta K, Sajjad M, Jawaid M. Twelve tips to enhance student engagement in synchronous online teaching and learning. Med Teach. (2022) 44:601–6. doi: 10.1080/0142159X.2021.1912310
19. Lee J, Lee H, Kim S, Choi M, Ko I, Bae J, et al. Debriefing methods and learning outcomes in simulation nursing education: A systematic review and meta-analysis. Nurse Educ Today. (2020) 87:104345. doi: 10.1016/j.nedt.2020.104345
20. Apfelbaum J, Hagberg C, Connis R, Abdelmalak B, Agarkar M, Dutton R, et al. 2022 American society of anesthesiologists practice guidelines for management of the difficult airway. Anesthesiology. (2022) 136:31–81. doi: 10.1097/ALN.0000000000004002
21. Cumin D, Weller J, Henderson K, Merry A. Standards for simulation in anaesthesia: Creating confidence in the tools. Br J Anaesth. (2010) 105:45–51. doi: 10.1093/bja/aeq095
22. Mian A, Khan S. Medical education during pandemics: A UK perspective. BMC Med. (2020) 18:100. doi: 10.1186/s12916-020-01577-y
23. Murdock H, Penner J, Le S, Nematollahi S. Virtual morning report during COVID-19: A novel model for case-based teaching conferences. Med Educ. (2020) 54:851–2. doi: 10.1111/medu.14226
24. Su B, Zhang T, Yan L, Huang C, Cheng X, Cai C, et al. Online medical teaching in china during the Covid-19 pandemic: Tools, modalities, and challenges. Front Public Health. (2021) 9:797694. doi: 10.3389/fpubh.2021.797694
25. Sung T, Hsu H. Improving critical care teamwork: Simulation-based interprofessional training for enhanced communication and safety. J Multidiscip Healthc. (2025) 18:355–67. doi: 10.2147/JMDH.S500890
26. McDonald E, Boulton J, Davis JL. E-learning and nursing assessment skills and knowledge - An integrative review. Nurse Educ Today. (2018) 66:166–74. doi: 10.1016/j.nedt.2018.03.011
27. Rochlen L, Housey M, Gannon I, Mitchell S, Rooney D, Tait A, et al. Assessing anesthesiology residents’ out-of-the-operating-room (OOOR) emergent airway management. BMC Anesthesiol. (2017) 17:96. doi: 10.1186/s12871-017-0387-2
28. Nuampa S, Ratinthorn A, Tangsuksan P, Chalermpichai T, Kuesakul K, Ruchob R, et al. Factors influencing critical thinking in simulation-based maternal-child nursing education among undergraduate nursing students: A mixed methods study. BMC Nurs. (2025) 24:389. doi: 10.1186/s12912-025-03016-w
29. Klasen J, Meienberg A, Bogie B. Medical student engagement during COVID-19: Lessons learned and areas for improvement. Med Educ. (2021) 55:115–8. doi: 10.1111/medu.14405
30. Cass G, Crofts J, Draycott T. The use of simulation to teach clinical skills in obstetrics. Semin Perinatol. (2011) 35:68–73. doi: 10.1053/j.semperi.2011.01.005
31. Cant R, Cooper S. Simulation in the Internet age: The place of web-based simulation in nursing education. An integrative review. Nurse Educ Today. (2014) 34:1435–42. doi: 10.1016/j.nedt.2014.08.001
32. Selcuk A, Ozturk N, Onal N, Bozkir A, Aksoy N. Online simulation versus traditional classroom learnings in clinical pharmacy education: Effect on students’ knowledge, satisfaction and self-confidence. BMC Med Educ. (2025) 25:437. doi: 10.1186/s12909-025-07028-7
33. Webster D. Using standardized patients to teach therapeutic communication in psychiatric nursing. Clin Simulat Nurs. (2014) 10:e81–6. doi: 10.1016/j.ecns.2013.08.005
34. Bindoff I, Ling T, Bereznicki L, Westbury J, Chalmers L, Peterson G, et al. A computer simulation of community pharmacy practice for educational use. Am J Pharm Educ. (2014) 78:168. doi: 10.5688/ajpe789168
35. Adsız M, Dinçer S. The analysis of classroom management challenges faced by teachers in online classrooms. TechTrends. (2025) 69:345–61. doi: 10.1007/s11528-025-01042-8
36. Woda A, Johnson B, Hansen J, Chen K, Dreifuerst K. The importance of feedback with an asynchronous online training program when learning debriefing for meaningful learning. Clin Simulat Nurs. (2025) 101:101709. doi: 10.1016/j.ecns.2025.101709
37. Decker S, Sapp A, Bibin L, Brown M, Crawford S, Jabeen Fayyaz J, et al. The impact of the simulation debriefing process on learning outcomes – an umbrella review protocol. Clin Simulat Nurs. (2024) 89:101505. doi: 10.1016/j.ecns.2023.101505
Keywords: online teaching, scenario simulation teaching, anesthesia, airway management, undergraduate students
Citation: Lin Y, Wang T-t, Hou Y-y, Lu X-y, Gao L-j, Hersi SA, Gao P and Wen Q-p (2025) Online scenario simulation teaching in airway management for undergraduate anesthesia students. Front. Med. 12:1563540. doi: 10.3389/fmed.2025.1563540
Received: 20 January 2025; Accepted: 20 May 2025;
Published: 10 June 2025.
Edited by:
Nourhan F. Wasfy, Suez Canal University, EgyptReviewed by:
Chenguang Zhang, Sanofi Genzyme, United StatesHend Abo Elatta, Mansoura University, Egypt
Copyright © 2025 Lin, Wang, Hou, Lu, Gao, Hersi, Gao and Wen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qing-ping Wen, ZG11d3FwQDE2My5jb20=; Peng Gao, ZGFsaWFucGVvcGxlQDE2My5jb20=
†These authors share first authorship
 Yun Lin
Yun Lin Ting-ting Wang1†
Ting-ting Wang1† Salad Abdirahman Hersi
Salad Abdirahman Hersi Peng Gao
Peng Gao