- 1School of Nursing, Hunan Normal University & Affiliated Hengyang Central Hospital, Changsha, Hunan, China
- 2School of Nursing, Kiang Wu Nursing College of Macao, Cotai, Macao SAR, China
Objectives: This study aims to integrate the data on the effects of a pre-established medical care program on hospitalized older adults with chronic heart failure (CHF).
Method: A comprehensive systematic review incorporating mixed research methodologies was undertaken. Quality assessment was conducted using the Critical Appraisal Tool developed by Joanna Briggs Institute, adhering to the PRISMA guidelines for studies. Where appropriate, data were synthesized and aggregated for meta-analysis or meta-aggregation.
Results: A total of 2,825 articles were found, of which 11 met the inclusion criteria. Meta-analysis showed that the implementation of advance care planning (ACP) can significantly increase the willingness and proportion of patients with CHF to choose and receive hospice services during their end-of-life phase. Meta-aggregation showed that the ACP intervention has a positive impact on participants, promotes their knowledge and understanding, and makes them share their decision-making with their families.
Conclusion: ACP is a promising and feasible intervention that can help older adults with CHF accurately understand ACP and express their wishes timely. This study provides insights and empirical evidence to improve ACP, and valuable guidance and reference for future clinical practice.
Systematic review registration: https://www.crd.york.ac.uk/PROSPERO/, PROSPERO, identifier: CRD42024580814.
1 Introduction
As the population ages and the incidence of chronic diseases increases, medical and social healthcare systems are facing an increasingly heavy burden (1). Chronic diseases are illnesses that persist for a long time and are rarely cured, which generally need long-term treatment and monitoring, and hospitalization is always possible (2, 3). Previous studies have shown that heart failure (HF) is a significant contributor to hospital admissions and that HF patients usually have a high comorbidity rate, which can lead to a significant disease burden (4, 5). Estimates suggest that total healthcare costs due to HF in the USA will reach $69.8 billion by 2030, which equates to a cost of approximately $244 per US adult (6). Although the lifespan of HF patients has increased of late, their quality of life has not significantly improved (7, 8). Consequently, HF imposes economic and life burden on the family, which makes it a significant worldwide health burden (9, 10).
Chronic heart failure (CHF) is rapidly becoming a major threat to human health (11) and is one of the primary causes of hospitalization in the older adults (10). Clinical manifestations of CHF usually include dyspnea, edema, fluid retention, and fatigue. Patients with CHF are more likely to develop other comorbidities (12). Cardiogenic shock (CS) is an extremely serious clinical condition, and studies have shown that more than half of CS cases may be closely associated with CHF (13). In addition, patients with CHF often suffer from complications due to psychological disorders, which not only further severely impair their quality of life but also significantly increase the mortality rate, perhaps even doubling it (14). Furthermore, CHF patients have high rates of rehospitalization within 2 years and in-hospital mortality, so approaches to alleviating unnecessary burdens need to be developed (15).
Advance care planning (ACP) is a comprehensive and ongoing process in which the individual is actively involved in making decisions about their future healthcare, with a special emphasis on ensuring that they receive care in accordance with their preferences, values, and philosophy of life, especially in the face of a serious illness or at the end of life (EOL). This approach enables the individual to express their wishes and preferences regarding their healthcare, thereby safeguarding their autonomy even when they may lose the capacity to do so directly (16). Previous studies have shown that ACP interventions can improve outcomes in older patients, including making specific decisions together with relatives, identifying wishes and values, and reducing unnecessary treatment and hospitalization (17–19). However, promoting ACP remains challenging, especially among CHF patients who have conscious disturbances due to the changes in their illness (e.g., CS), which makes it impossible for the patients to accurately convey their wishes (20). Therefore, timely ACP interventions are necessary for patients with CHF (21).
Several systematic assessments have been conducted to evaluate the efficacy of ACP programs in different groups of older patients (22–25). However, none of these assessments have focused on ACP for older adults with CHF. Therefore, this mixed-methods systematic review (MMSR) aims to bring together relevant evidence from both quantitative and qualitative studies using a holistic approach, taking into account the importance of validity and practical experience (26). In an MMSR, the quantitative component incorporates a wide range of research design options, whereas the qualitative component explores the meaning and understanding of interventions. In this study, a definitive synthesis study combining quantitative and qualitative evidence was designed to provide strategic guidance for the design and implementation of ACP for older populations with CHF.
2 Method
This review followed the MMSR methodological framework developed by Joanna Briggs Institute (JBI) and Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) and aimed to accurately address the established review questions and systematically synthesize and integrate the data (27, 28). This review was registered on PROSPERO (CRD42022329615).
2.1 Search strategy
Seven databases were used in the search, namely PubMed, CINAHL, MEDLINE, Web of Science, CNKI, Embase, and Cochrane Library, which was carried out from the date of initiation of the database to 29 October 2024. The search keywords encompassed relevant subject headings and universal symbols related to “advance care planning,” “end of life discuss,” “heart failure,” and “aged.” The gray literature database and clinical trial registries were searched for relevant unpublished studies. Reference lists of the included studies and relevant review articles were manually searched to identify eligible studies that may have been overlooked during the initial search. A detailed search plan was developed and documented prior to the beginning of the search to ensure that the search was comprehensive and reproducible. To mitigate the risk of publication bias, searches were not restricted by publication status.
2.2 Study selection
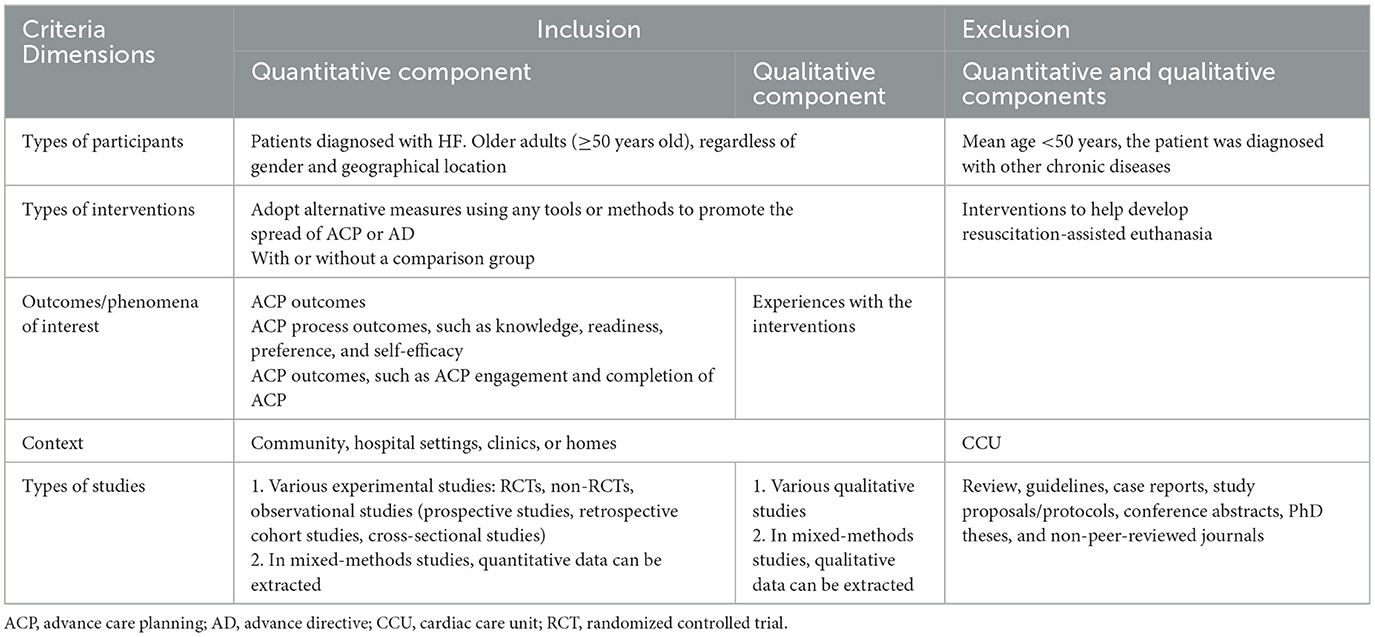
The inclusion criteria were developed based on participants, interventions, outcomes/associated phenomena, context, and type of study. Interventions that focused on the development of resuscitation-assisted euthanasia were excluded, but interventions that focused on ACP or advance directive (AD) forms were included. ACP is an ongoing process and should therefore report its relevant process outcomes (including various outcomes in the progress of the ACP as well as the final outcome) (22, 29). Coronary care unit (CCU) patients were excluded because they could not make clear decisions (30). Average age was set as 50 years to cater to a sufficient number of included studies and to improve the reliability of the results (Table 1). Two reviewers independently screened the title and abstract of the studies to exclude those that were not relevant to the present study, and potentially compatible studies were retained for further evaluation. One reviewer first meticulously browsed and reviewed the full text of an initially included study according to the eligibility criteria, followed by an independent review by another reviewer. In case of any disagreement, an in-depth discussion was held to reach consensus and make a decision.
2.3 Data extraction
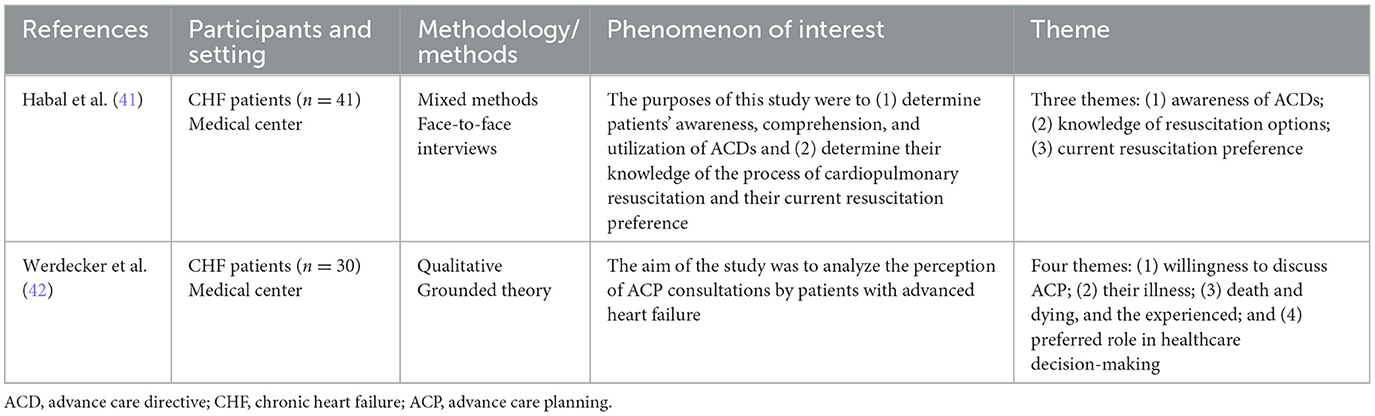
Using standardized JBI data extraction methods, one reviewer extracted quantitative and qualitative data separately and discussed the methods and findings with the other reviewer (31). The quantitative data extracted included information on authors, published year, participants, environmental context, study design, interventions, findings, and effectiveness (Table 2). The qualitative data extracted included information on the phenomenon of interest related to the research objectives, study population, research methodology, contextual environment, cultural information, and data analyses (Table 3). In addition, an interpretation of the results of qualitative data analysis was obtained from the authors, which encompassed the primary theme of cultural literacy and its subthemes. Two reviewers independently assessed the “confidence” (defined as clarity, reliability, and unsupported) of the study information based on the established descriptions (specifically, direct quotations from participants' original statements, field observation records, or other raw data) (31).
2.4 Quality appraisal
The two independent reviewers applied the JBI Critical Appraisal Tool to evaluate eligible studies (31), which included assessment checklists for randomized controlled trials (RCTs), quasi-experimental studies (non-randomized experimental studies), and qualitative studies. Assessment checklists provided answers to all questions in the form of “Yes,” “No,” or “Unclear.” An all-“Yes” response represented high quality of the study; one or two “Unclear” or “No” responses represented medium quality; and more than two “Unclear” or “No” responses represented low quality. All the included studies were categorized into low, moderate, and high quality using this method. Any disagreements that arose during the data extraction and quality assessment process were discussed in depth until a consensus was reached.
2.5 Data synthesis and integration
As this review aimed to explore the different dimensions of a phenomenon of interest, a convergent segmentation method was used to synthesize and integrate quantitative and qualitative data (27, 31). Where available, statistical meta-analyses of the quantitative data were conducted, and Review Manager V.5.4 of Cochrane Collaboration was used to obtain combined effect estimates. In addition, I2 statistic and χ2 test were used to assess heterogeneity. When statistical aggregation was not feasible, a narrative approach was followed to summarize the results. For the results of the qualitative study, the JBI methodology was adopted and meta-aggregation methods were used for integration (31). The findings obtained from the included studies (level 1) were compiled into coherent statements. Subsequently, similarities in meaning among these findings were collected to establish categorization (level 2). Finally, by synthesizing these categories (level 3), a comprehensive collection of the synthesized findings was produced for use in evidence-based practice (31).
3 Results
3.1 Study selection
A total of 2,825 articles were retrieved in our search. After removing 517 duplicates, the title and abstract of the remaining 2,308 papers were examined, which resulted in the selection of 61 studies. Then, the full text of these 61 studies was checked. Finally, 11 articles were included (32–42) (Figure 1).

Figure 1. Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram of the study selection process.
3.2 Methodological quality
Among the quantitative studies included (n = 9), six studies were rated as medium quality, one as high quality, and two as low quality. There were five RCTs, two of which had missing information regarding the blinding of participants (32, 40) and four lacked information on the blinding of treatment assignment (32, 35, 37, 40). The remaining three studies were classified as quasi-experimental studies and one as mixed study. Four studies lacked a control group (33, 34, 38, 39). Two studies did not provide information on whether participants received comparable treatment or care in addition to the specific exposure or intervention being investigated (38, 39). One study lacked information regarding multiple outcome measurements (39). All included qualitative studies (n = 2) were rated as moderate quality because the authors did not clearly articulate their theoretical frameworks, cultural orientations, and the potential impact of these factors (41, 42).
3.3 Characteristics of the included studies
The core characteristics of the included studies were summarized and presented. A total of 11 articles, whose publication year spanned from 2011 to 2024, were included in this review. Study designs encompassed five two-arm RCTs (n = 5) (32, 35–37, 40), one mixed-method design combining a one-arm pretest–posttest approach with a qualitative component (38), two one-arm pretest–posttest design (33, 34), one one-arm posttest design (39), and two qualitative studies (41, 42). A total of 2,809 participants were recruited in these studies. The sample size varied between 20 and 1,894 participants, all of whom were sourced from medical centers. Study samples had an average age of 53–83 years, and all the samples were from hospital settings.
3.4 Synthesis of quantitative evidence
A meta-analysis can be conducted to examine the impact of interventions on EOL care preferences as it allows for the analysis of consistent data across studies (32, 35). Other outcomes, including ACP completion, satisfaction, readiness, attitude, knowledge, ACP engagement, ACP self-efficacy, dynamics for EOL preferences, congruence, and EOL care preferences. These results could not be statistically summarized and were therefore represented through narrative integration.
3.4.1 ACP-related completion
Three studies showed ACP-related completion after ACP intervention (32–34). In one study, a significant proportion of participants (94.3%) who finished the disease-specific advance care planning (DS-ACP) had a health directive in place, whereas only 24.8% of those who did not complete the DS-ACP process had a health directive (32). Another study demonstrated that after the intervention, 62% of patients had completed either an AD or physician orders for life-sustaining treatment (POLST) form within a 6-month period, as opposed to 51% who did that before the intervention. Furthermore, there was an increase in the number of patients completing a POLST form within 6 months of the intervention, from 13 patients (35%) to 19 patients (51%) (34). One showed an increase in the number of participants completing ADs (28% vs. 47%) (33).
3.4.2 Satisfaction
Only one study reported satisfaction regarding ACP interventions (39). The results indicated a high level of satisfaction by patients, with 80% of patients expressing either satisfaction or very high satisfaction and stating that they would recommend the intervention to other patients.
3.4.3 Readiness
A statistically significant increase was observed in patient readiness to engage in ACP from before the intervention to after the intervention, with a change score of +0.53 (p < 0.01) (38). However, at the 1-month follow-up, it decreased almost back to the level before the panel visit (change score of 0.52; p < 0.01) (38).
3.4.4 Attitude
One study used a revised version of the Advance Directive Attitude Survey (ADAS) to evaluate patients' attitudes toward ACP interventions. The findings revealed a notable increase in ADAS mean scores, from 57% at baseline to 80% after 3 months (33). A statistically significant enhancement was observed in patients' readiness to engage in ACP from before the intervention to after the intervention, with a change score of +0.53 (p < 0.01) (36).
3.4.5 Knowledge
One study used ACP Knowledge Questionnaire to evaluate ACP knowledge and found that participants in the intervention arm had higher mean knowledge scores compared with control participants (4.1 ± 1.4 vs. 3.0 ± 1.5; p < 0.001) (35).
3.4.6 ACP engagement
Only one study addressed ACP engagement, not through specific data points but rather by noting that participants in the intervention group were more inclined to report having conversations about goals of care (GOC) with their healthcare providers (35).
3.4.7 Dynamics for end-of-life preferences
One study used a self-efficacy questionnaire to assess patients' self-efficacy levels and found that those with higher self-efficacy were more likely to choose aggressive EOL care (37). Conversely, it reported a progressive increase in the percentage of patients who changed their EOL care preferences compared with the baseline figures (37). In addition, the same study found that EOL preferences are influenced by other factors, suggesting that older patients have a lower level of interest in preferences for aggressive EOL care as their preferences are more influenced by factors such as financial constraints, proper knowledge of prognosis, and conflicts in decision-making (37).
3.4.8 AD-related outcomes
A study that used the self-efficacy questionnaire as an assessment tool showed that there was no statistically significant overall change in patient self-efficacy (with a change score of +0.29; p = 0.11). Notably, 1 month after the group intervention, a decline in self-efficacy was observed, with levels falling below those recorded before the group intervention (change score −0.40; p < 0.05) (38).
3.4.9 Congruence
Two studies examined the consistency in preferences by patients and their families/doctors. One study revealed that the intervention group showed a higher degree of alignment with respect to GOC. Specifically, individuals in the intervention group were approximately nine times more likely to achieve congruence in GOC compared with those in the control group. However, the difference observed between the two groups did not reach statistical significance (p = 0.064) (36). Another study reported that the agreement between clinicians' and patients' ACP preferences was higher in the intervention group than in the control group (35).
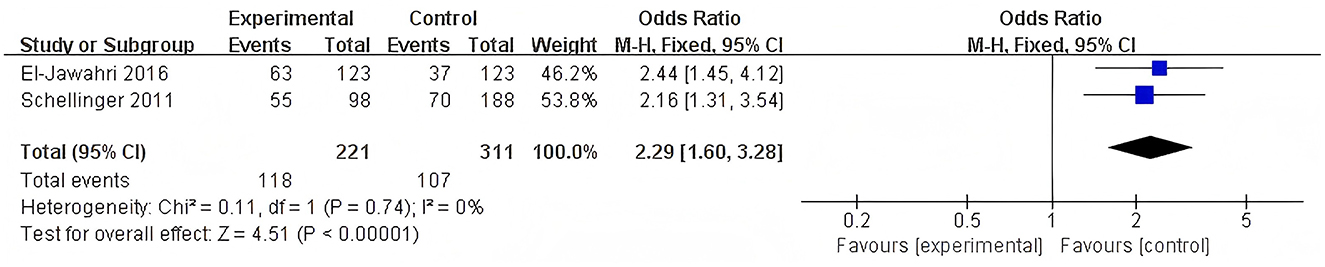
3.4.10 Preference of EOL care
A combined analysis of two studies showed a significant impact of the intervention on the selection of EOL care preferences (Figure 2). Specifically, the mean difference in EOL care preference was 2.29, with a 95% confidence interval (CI) ranging from 1.60 to 3.28. However, it should be noted that the p-value was 0.75, indicating no statistical significance, and the I2 statistic was 0%, suggesting no heterogeneity between the two studies (32, 35).
3.5 Synthesis of qualitative evidence
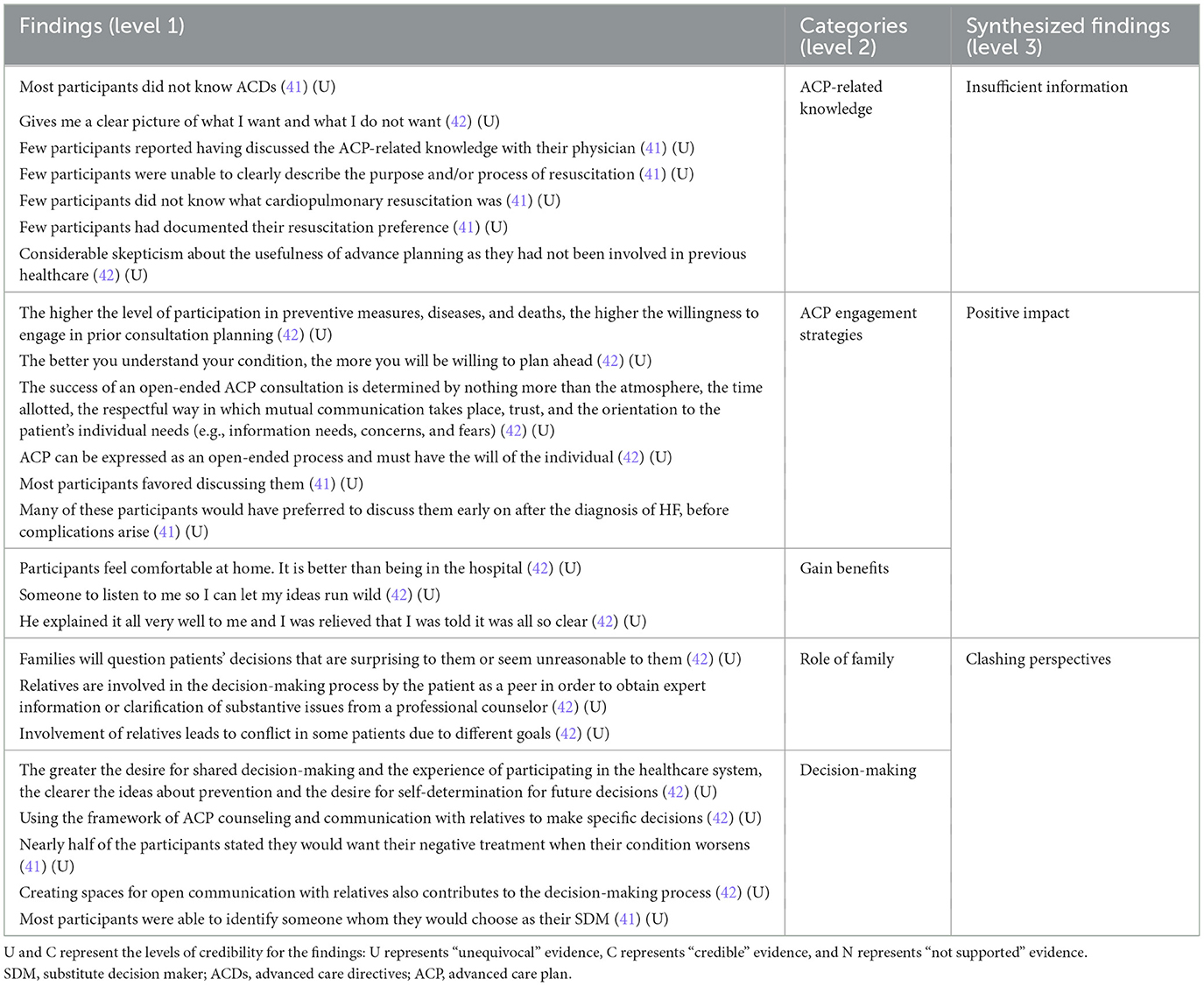
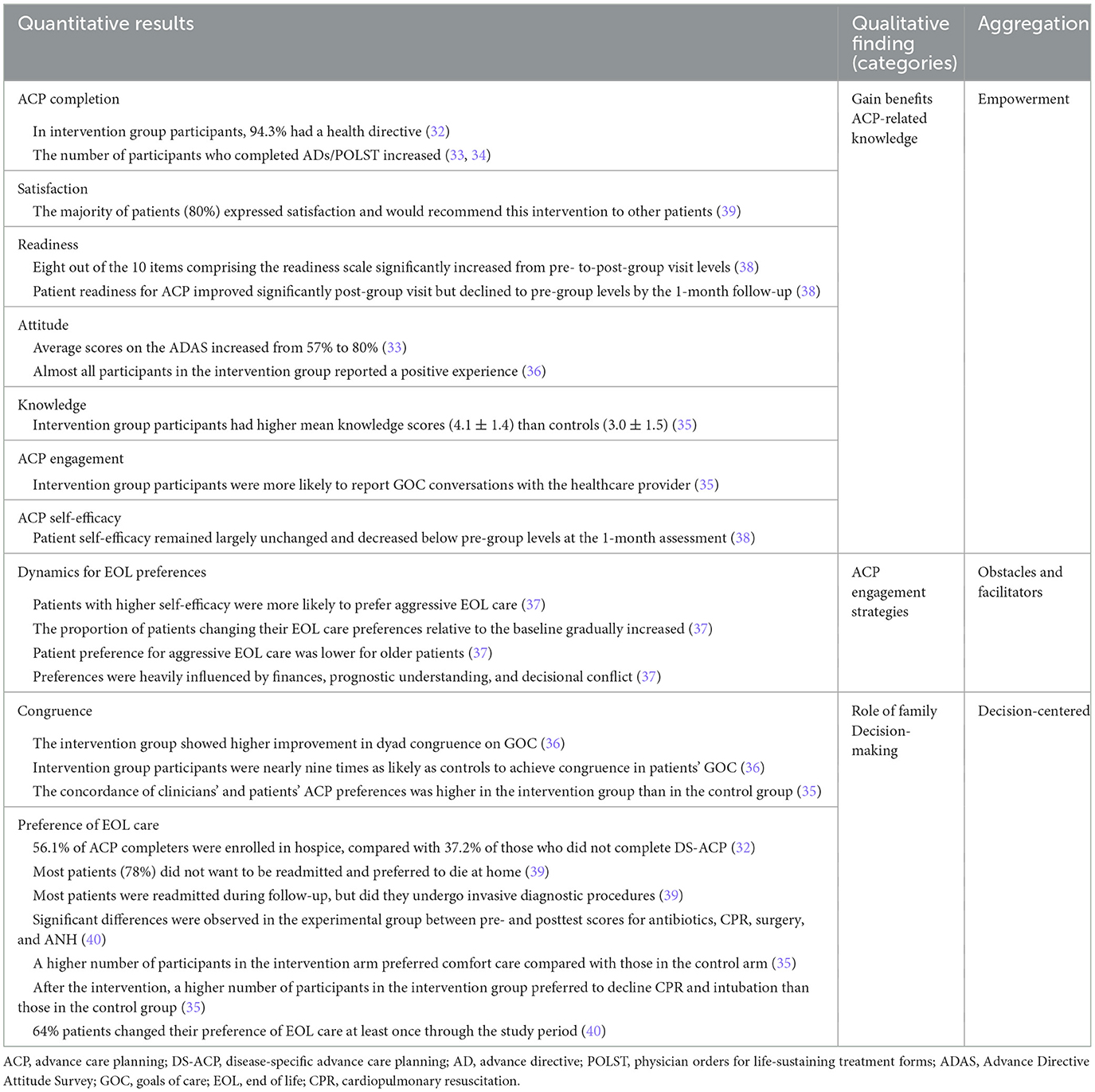
Using a meta-aggregation process of the qualitative evidence, three key themes were identified: insufficient information, positive impact, and clashing perspectives. ACP-related knowledge was categorized under the insufficient information theme. ACP engagement strategies and gain benefits were two subthemes identified in the positive impact theme. Role of family and decision-making are two subthemes identified within the clashing perspectives theme (Table 4).
3.5.1 ACP-related knowledge
The majority of participants did not know ACP and were even rather skeptical about the usefulness of ACP (41, 42). Some participants thought that an ACP intervention gives them a clear idea of what they want and do not want (42).
3.5.2 ACP engagement strategies
The majority of participants expressed a willingness to engage in ACP discussions and believed that they obtained higher levels of knowledge about the disease after the discussion than earlier and showed a strong willingness of patients to participate in the ACP (41, 42). In addition, the success of an ACP discussion was found to be influenced by various factors, such as the atmosphere, time allotted, way of communication, trust, and orientation to the patient's individual needs (42).
3.5.3 Gain benefits
A number of participants reported that the medical staff explained the ACP clearly and made them feel comfortable and at ease (42). Some participants expressed that medical staff need to listen to them so that they can express their wild ideas (42).
3.5.4 Role of family
Besides participants, their families were also involved in ACP decision-making to obtain expert information or clarification of significant issues from professional advisers and to make unanimous decisions (42). However, when a participant makes a decision that surprises their family or seems unreasonable to them, the family questions the decision and potentially creates conflict (42).
3.5.5 Decision-making
Participants felt that creating spaces for open communication with relatives regarding ACP counseling helped their decision-making process (41, 42). The stronger the desire for co-decision-making, the stronger the desire for self-determination over future decision-making. After ACP intervention, participants expressed that they were able to identify someone whom they would choose as their substitute decision maker (41).
3.6 Integration of quantitative and qualitative evidence
The combined results of the quantitative and qualitative evidence were generally consistent, and the results of the three-part summary are presented in detail in Table 5. The positive perceptions of participants toward the ACP intervention, as reflected in the qualitative evidence, provided insights into the significant enhancements observed in various ACP outcomes reported in the quantitative evidence.
3.6.1 Empowerment
Quantitative and qualitative studies have consistently stated that ACP interventions are beneficial in promoting patients' understanding of ACP-related knowledge. In this study, quantitative data showed that ACP interventions significantly increase participants' completion (32–34) while also improving their engagement in ACP (35). In addition, quantitative data also suggested that the ACP intervention increases patient satisfaction and a sense of good experience during the intervention process, which depends largely on the professionalism of the ACP intervention. Besides, qualitative data suggested that ACP enables people to have a clear understanding of what they want and to be comfortable discussing it with medical staff/families to achieve the most satisfactory outcome (41, 42).
3.6.2 Obstacles and facilitators
Both quantitative and qualitative studies highlighted facilitators and obstacles to ACP preferences (37, 41, 42). Quantitative data showed that patients with higher self-efficacy are more likely to prefer aggressive EOL care and that age, economic status, knowledge of the disease, and decision-making conflicts are likely to influence patients' EOL preferences (37). However, participants' EOL preferences are not static; rather, they are more likely to change over time (37). Quantitative data also showed other subjective factors such as environment, timing, and way of communication style, but the most fundamental factor was the individual's willingness (42).
3.6.3 Decision-centered
Quantitative and qualitative studies emphasized decision-centered preference selection among clinicians, participants, and families. Quantitative data showed that after participants received ACP intervention, decision-making consistency between participants and both physicians and family members was found to be significantly higher than in the control group, and the majority of participants were more inclined to receive comfort care after the ACP intervention, reducing the invasive quality of care and enhancing patient quality of life (35, 36, 39, 40). Qualitative and quantitative evidence complemented each other, with quantitative data directly reflecting outcomes in this integration and qualitative data reflecting the complexity of the decision-making process, such as the conflict and mutual questioning of decision-making between patients and families, and the difficulty for patients in choosing an agent (42).
4 Discussion
4.1 Major findings
In this study, JBI's MMSR framework was used to synthesize both quantitative and qualitative evidence. This approach facilitated to achieve a comprehensive understanding of the effectiveness of ACP and the experiences of the participants (27). There were differences in the quality of quantitative studies as all prospective studies did not have a control group. The quality of qualitative studies was rated as moderate as these two studies lacked a theoretical framework and also due to the researcher's reflective and self-critical nature of the study.
The overall results showed that the integration of quantitative and qualitative research is both supplementary and consistent, with quantitative research as an etic perspective providing an objective outcome and qualitative research as an emic perspective providing process understanding. This helps demonstrate that the ACP intervention is a practical and effective approach to promoting ACP empowerment (including knowledge and attitudes) and decision-making for participants. Quantitative results in this study showed a significant increase in the number of ACP/AD completions and ACP knowledge scores in the intervention group (32, 35). This finding suggests that ACP intervention is effective in increasing patient understanding and engagement with the pre-established healthcare plan. This is consistent with the findings of the existing research. For example, Liu et al. (43) have found that a gamified ACP intervention significantly improves patients' ACP knowledge and completion rates. Qualitative results in this study add process to this finding and show that the medical staff provided clear explanations about ACP during the intervention, thus enhancing the patients' understanding of the ACP (42). Previous studies (44) have agreed that community populations show a low level of ACP participation. Therefore, based on the results of this review, promotion and explanation of ACP should be carried out at all levels of healthcare as the professional guidance of medical staff can have a positive effect on different populations. Participants in a qualitative study emphasized the importance of a respectful atmosphere and open communication (42), which may be one of the reasons for the high satisfaction rate reported in quantitative results (39). High-quality conversations are not possible without a good communication climate, and several cross-sectional studies (45, 46) now point to cursory, brief, and unprofessional communication as a significant impediment to achieving high patient satisfaction. Therefore, the quality of ACP interventions by medical staff relies not only on the content of communication but also on communication style and patient experience. Medical staff should be trained in communication skills to facilitate participation in ACP discussions. Quantitative results indicated a high rate of family involvement in decision-making and a significant increase in goal agreements between patients and families after ACP intervention (35, 36). However, one qualitative study also revealed the potential for conflict resulting from family involvement (42). Families may prefer aggressive treatment, whereas patients prefer comfort care. This inconsistency in decision-making may stem from emotional factors, differences in information about the condition, and cultural and social pressures. Therefore, healthcare professionals should train family members in communication skills and hospice knowledge to help them better understand the patient's wishes and values, to reduce emotional and practical pressures, to make clear that the role of the family is that of a supporter rather than a decision-maker, and to ensure that the patient's decision-making is autonomous and that the patient has the right to die with dignity, with the least amount of pain and suffering possible (47). In this study, we found that patients' ACP self-efficacy and readiness increased significantly after the intervention, but decreased to pre-intervention levels after 1 month (38). In contrast, previous studies have reported a significant increase in patients' self-efficacy and readiness after ACP intervention, but without returning to pre-intervention levels after a specific time period (43, 48, 49). Qualitative studies have further revealed patients' skepticism about the long-term usefulness of ACP (42). Therefore, it is possible that the long-term effectiveness of ACP intervention was affected by the skepticism and lack of knowledge of some of the participants.
Qualitative research and quantitative research complement each other, with the former revealing the mechanisms of action and contextual factors of interventions through in-depth analyses of participants' experiences and perspectives and the latter assessing the effectiveness of interventions through statistical analyses. However, in this study, qualitative research was not directly tested using quantitative research in some aspects, which provides a potential direction for future research. Regarding the timing of ACP discussions, qualitative findings suggested that many participants like to discuss ACP during the early stage of the disease (41), whereas quantitative studies did not explicitly test this. This finding is highly consistent with clinical practice recommendations that discussing ACP during the early stage of the disease significantly improves patient engagement and quality of decision-making. Ideal implementation of ACP should be an ongoing and dynamically adapted process that emphasizes a prospective and systematic approach rather than an acute and ad hoc one. For patients with CHF, the best practice is to initiate ACP at an early, stable stage of the disease, rather than waiting until the disease worsens. This early intervention helps build a therapeutic relationship based on care, trust, and long-term cooperation and creates favorable conditions for adequate communication and continuous adjustment of the patient's treatment preferences (50). In addition, qualitative findings revealed important insights into patients' preferences for EOL care, such as the desire to avoid hospital readmission and dying at home, and the dynamic nature of preferences (35). However, quantitative results, including a non-significant p-value for EOL care preferences (p = 0.75) and wide confidence intervals (1.60–3.28), suggest a significant uncertainty about the effect of the intervention, and these results should be interpreted with caution. Future studies should employ larger sample sizes and standardized intervention protocols to clarify the effect of interventions on hospice preferences.
Meta-analysis revealed that the ACP intervention for older adult individuals with CHF significantly enhances participants' satisfaction with ACP, readiness for ACP, knowledge related to ACP, engagement in ACP behaviors, and ultimately a higher completion rate of ACP. Meta-aggregation showed that participants generally lack ACP-related knowledge but have a positive attitude, and participants believe that ACP intervention provides a suitable opportunity to facilitate shared decision-making in the family and explain the relevant variables affecting ACP. These observations were consistent with the primary sources of the theory of planned behavior where attitude (i.e., evaluation of behavior and affective tendencies), subject norms (i.e., expectations and perceptions of others about particular behaviors), and perceived behavioral control (i.e., individuals' perceptions of their ability to successfully perform particular behaviors) shape an individual' s behavioral intentions (i.e., intention or desire to perform an act) and behavioral outcomes (i.e., behavior that is actually exhibited by an individual in a given situation) (51). The results of the present study are consistent with this theoretical model, which emphasizes that ACP participation is a dynamic process rather than a static event that fluctuates in response to changes in internal and external factors, such as self-efficacy maintenance and complexity of family involvement. These findings provide an important basis for optimizing ACP interventions and highlight the directions for future research. Future research should focus on the long-term effects of ACP interventions. Furthermore, intervention strategies targeting family engagement need to be developed to reduce conflict and increase consistency in decision-making.
4.2 Strengths and limitations
The advantage of this study lies in the comprehensive and thorough analysis of quantitative and qualitative data using the MMRS to elucidate the impact of ACP intervention on CHF participants and their experiences. Because of the limited number of studies on this subject, all identified studies were included in the literature, including one qualitative study in German. A consensus was established on the integration of quantitative and qualitative evidence, which subsequently enhanced the credibility of the findings regarding the effectiveness of ACP and engagement levels associated with it.
However, this review has some limitations. First, an in-depth search of the available literature was conducted, but relevant studies might have been overlooked due to the inclusion criterion limiting the study language to English and German. Second, the strength of the evidence was weakened as all prospective studies used a single-group design. In addition, the limited number of qualitative studies and the absence of a theoretical framework guiding the included qualitative evidence further compromised the level of evidence. Third, participants in the included studies were recruited exclusively from hospital settings. Thus, it is uncertain whether the findings of this study are applicable to older adult patients with CHF at home or in the community. Furthermore, the primary limitations of conducting a meta-analysis were the small number of included studies and the inability to formally assess publication bias (e.g., funnel plots or Egger's test) due to insufficient statistical power. This may affect the robustness and generalizability of our findings. Therefore, future studies should include a higher number of studies to address this limitation.
5 Conclusion
Comprehensive evidence from studies with quantitative and qualitative data suggests that ACP intervention is an effective method to make participants aware of healthcare values and goals, thereby improving their outcomes. Since older patients with CHF lack ACP-related knowledge and an opportunity to start ACP discussions with clinicians or families, they miss a valuable chance to have a serious and complete discussion about ACP. Therefore, broader and more rigorous studies, especially prospective studies, are required to analyze the effects of ACP on older patients with CHF using rigorous study designs and in different cultures. In addition, future studies need to extend the follow-up period to explore the possibility of and reasons for changes in the variables of ACP-related outcomes over time.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
LC: Writing – original draft. YC: Conceptualization, Formal analysis, Writing – original draft. JQ: Funding acquisition, Writing – review & editing. ZW: Funding acquisition, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by the Natural Science Foundation of Hunan Province in 2025 (Grant No: 2025JJ80594), the Scientific Research Project of Hunan Nursing Association (Grant No: HNKYP202413), Young Talent Project of Hunan Nursing Association (Grant No: Q20241204020), and the Hengyang Science and Technology Innovation Project (Grant No: 202205018).
Acknowledgments
All researchers would like to express their gratitude to all the participants for taking their precious time to participate in this study and also thank the hospital managers and nursing administrators for their firm support in conducting this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2025.1566977/full#supplementary-material
References
1. Bishop NJ, Haas SA, Quiñones AR. Cohort trends in the burden of multiple chronic conditions among aging us. Adults J Gerontol B Psychol Sci Soc Sci. (2022) 77:1867–79. doi: 10.1093/geronb/gbac070
2. Facchinetti G, D'Angelo D, Piredda M, Petitti T, Matarese M, Oliveti A, et al. Continuity of care interventions for preventing hospital readmission of older people with chronic diseases: a meta-analysis. Int J Nurs Stud. (2020) 101:103396. doi: 10.1016/j.ijnurstu.2019.103396
3. Riegel B, Westland H, Iovino P, Barelds I, Bruins SJ, Stawnychy MA, et al. Characteristics of self-care interventions for patients with a chronic condition: a scoping review. Int J Nurs Stud. (2021) 116:103713. doi: 10.1016/j.ijnurstu.2020.103713
4. Tisminetzky M, Gurwitz JH, Fan D, Reynolds K, Smith DH, Magid DJ, et al. Multimorbidity burden and adverse outcomes in a community-based cohort of adults with heart failure. J Am Geriatr Soc. (2018) 66:2305–13. doi: 10.1111/jgs.15590
5. Pratley R, Guan X, Moro RJ, Do LR. Chapter 1: the burden of heart failure. Am J Med. (2024) 137:S3–8. doi: 10.1016/j.amjmed.2023.04.018
6. Virani SS, Alonso A, Aparicio HJ, Benjamin EJ, Bittencourt MS, Callaway CW, et al. Heart disease and stroke statistics-2021 update: a report from the American Heart Association. Circulation. (2021) 143:e254–743. doi: 10.1161/CIR.0000000000000950
7. Ventoulis I, Kamperidis V, Abraham MR, Abraham T, Boultadakis A, Tsioukras E, et al. Differences in health-related quality of life among patients with heart failure. Medicina. (2024) 60:109. doi: 10.3390/medicina60010109
8. Kim S, Perry LM, Mossman B, Dunn A, Hoerger M. Financial burden and physical and emotional quality of life in copd, heart failure, and kidney failure. PLoS ONE. (2024) 19:e306620. doi: 10.1371/journal.pone.0306620
9. Savarese G, Becher PM, Lund LH, Seferovic P, Rosano G, Coats A. Global burden of heart failure: a comprehensive and updated review of epidemiology. Cardiovasc Res. (2023) 118:3272–87. doi: 10.1093/cvr/cvac013
10. Wammes J, Auener S, van der Wees PJ, Tanke M, Bellersen L, Westert GP, et al. Characteristics and health care utilization among patients with chronic heart failure: a longitudinal claim database analysis. ESC Heart Fail. (2019) 6:1243–51. doi: 10.1002/ehf2.12512
11. Khan MS, Shahid I, Bennis A, Rakisheva A, Metra M, Butler J. Global epidemiology of heart failure. Nat Rev Cardiol. (2024) 21:717–34. doi: 10.1038/s41569-024-01046-6
12. Aimo A, Vergaro G, Barison A, Maffei S, Borrelli C, Morrone D, et al. Sex-related differences in chronic heart failure. Int J Cardiol. (2018) 255:145–51. doi: 10.1016/j.ijcard.2017.10.068
13. Sundermeyer J, Kellner C, Beer BN, Besch L, Dettling A, Bertoldi LF, et al. Clinical presentation, shock severity and mortality in patients with de novo vs. acute-on-chronic heart failure-related cardiogenic shock. Eur J Heart Fail. (2024) 26:432–44. doi: 10.1002/ejhf.3082
14. Veskovic J, Cvetkovic M, Tahirovic E, Zdravkovic M, Apostolovic S, Kosevic D, et al. Depression, anxiety, and quality of life as predictors of rehospitalization in patients with chronic heart failure. BMC Cardiovasc Disord. (2023) 23:525. doi: 10.1186/s12872-023-03500-8
15. Crea F. Epidemiology and treatment of acute and chronic heart failure. Eur Heart J. (2023) 44:329–32. doi: 10.1093/eurheartj/ehad022
16. Komesaroff PA. Does advance care planning have a future? Intern Med J. (2023) 53:462–4. doi: 10.1111/imj.16060
17. Jimenez G, Tan WS, Virk AK, Low CK, Car J, Ho A. Overview of systematic reviews of advance care planning: summary of evidence and global lessons. J Pain Symptom Manage. (2018) 56:436–59. doi: 10.1016/j.jpainsymman.2018.05.016
18. Chan C, Chen YF, Chan H. Advance care planning in hong kong. Z Evid Fortbild Qual Gesundhwes. (2023) 180:90–3. doi: 10.1016/j.zefq.2023.05.015
19. Hickman SE, Unroe KT, Ersek M, Stump TE, Tu W, Ott M, et al. Systematic advance care planning and potentially avoidable hospitalizations of nursing facility residents. J Am Geriatr Soc. (2019) 67:1649–55. doi: 10.1111/jgs.15927
20. Denniss DL, Denniss AR. Advance care planning in cardiology. Heart Lung Circ. (2017) 26:643–4. doi: 10.1016/j.hlc.2017.05.111
21. Smith AK. Should we still believe in advance care planning? J Am Geriatr Soc. (2022) 70:1358–60. doi: 10.1111/jgs.17727
22. Wang X, Huang XL, Wang WJ, Liao L. Advance care planning for frail elderly: are we missing a golden opportunity? A mixed-method systematic review and meta-analysis. BMJ Open. (2023) 13:e68130. doi: 10.1136/bmjopen-2022-068130
23. Huynh L, Moore J. Palliative and end-of-life care for the older adult with cancer. Curr Opin Support Palliat Care. (2021) 15:23–8. doi: 10.1097/SPC.0000000000000541
24. O'Caoimh R, Cornally N, O'Sullivan R, Hally R, Weathers E, Lavan AH, et al. Advance care planning within survivorship care plans for older cancer survivors: a systematic review. Maturitas. (2017) 105:52–7. doi: 10.1016/j.maturitas.2017.06.027
25. Wang J, Zhou A, Peng H, Zhu N, Yang L, Zheng X, et al. Effects of advance care planning on end-of-life decisions among community-dwelling elderly people and their relatives: a systematic review and meta-analysis. Ann Palliat Med. (2023) 12:571–83. doi: 10.21037/apm-23-367
26. Pearson A, White H, Bath-Hextall F, Salmond S, Apostolo J, Kirkpatrick P, et al. mixed-methods approach to systematic reviews. Int J Evid Based Healthc. (2015) 13:121–31. doi: 10.1097/XEB.0000000000000052
27. Stern C, Lizarondo L, Carrier J, Godfrey C, Rieger K, Salmond S, et al. Methodological guidance for the conduct of mixed methods systematic reviews. JBI Evid Implement. (2021) 19:120–9. doi: 10.1097/XEB.0000000000000282
28. Lizarondo L, Stern C, Apostolo J, Carrier J, de Borges K, Godfrey C, et al. Five common pitfalls in mixed methods systematic reviews: lessons learned. J Clin Epidemiol. (2022) 148:178–83. doi: 10.1016/j.jclinepi.2022.03.014
29. Anderson BK, Mihilli S, Kumaresh M, Kumaresh A, Mirza RM, Klinger CA. Advance care planning for seniors diagnosed with dementia: a scoping review of the Canadian literature. Can J Aging. (2022) 41:377–403. doi: 10.1017/S0714980821000283
30. Yamamoto K, Hayama J, Nakayama K, Yonekura Y, Ota E. Intervention and efficacy of advance care planning for patients in intensive care units and their families: a scoping review protocol. Nurs Open. (2021) 8:997–1001. doi: 10.1002/nop2.722
31. Institute JB. The JBI Manual for Evidence Synthesis (2020). Available online at: https://wiki.jbi.global/display/MANUAL/JBI+Manual+for+Evidence+Synthesis (accessed March 17, 2025).
32. Schellinger S, Sidebottom A, Briggs L. Disease specific advance care planning for heart failure patients: implementation in a large health system. J Palliat Med. (2011) 14:1224–30. doi: 10.1089/jpm.2011.0105
33. Evangelista LS, Motie M, Lombardo D, Ballard-Hernandez J, Malik S, Liao S. Does preparedness planning improve attitudes and completion of advance directives in patients with symptomatic heart failure? J Palliat Med. (2012) 15:1316–20. doi: 10.1089/jpm.2012.0228
34. Sadeghi B, Walling AM, Romano PS, Ahluwalia SC, Ong MK, A. hospital-based advance care planning intervention for patients with heart failure: a feasibility study. J Palliat Med. (2016) 19:451–5. doi: 10.1089/jpm.2015.0269
35. El-Jawahri A, Paasche-Orlow MK, Matlock D, Stevenson LW, Lewis EF, Stewart G, et al. Randomized, controlled trial of an advance care planning video decision support tool for patients with advanced heart failure. Circulation. (2016) 134:52–60. doi: 10.1161/CIRCULATIONAHA.116.021937
36. Metzger M, Song M, Ward S, Chang PP, Hanson LC, Lin F, et al. randomized controlled pilot trial to improve advance care planning for lvad patients and their surrogates. Heart Lung J Crit Care. (2016) 45:186–92. doi: 10.1016/j.hrtlng.2016.01.005
37. Malhotra C, Hu MB, Malhotra R, Sim D, Jaufeerally FR, Bundoc FG, et al. Instability in end-of-life care preference among heart failure patients: secondary analysis of a randomized controlled trial in Singapore. J Gen Intern Med. (2020) 35:2010–6. doi: 10.1007/s11606-020-05740-2
38. Ahluwalia SC, Bandini JI, Coulourides Kogan A, Bekelman DB, Olsen B, Phillips J, et al. Impact of group visits for older patients with heart failure on advance care planning outcomes: preliminary data. J Am Geriatr Soc. (2021) 69:2908–15. doi: 10.1111/jgs.17283
39. Coster JE. ter Maat GH, Pentinga ML, Reyners A, van Veldhuisen DJ, de Graeff P. A pilot study on the effect of advance care planning implementation on healthcare utilisation and satisfaction in patients with advanced heart failure. Neth Heart J. (2022) 30:436–41. doi: 10.1007/s12471-022-01705-8
40. Cheng H-C, Wu S-FV, Chen Y-H, Tsan Y-H, Sung S-H, Ke L-S. Advance care planning affects end-of-life treatment preferences among patients with heart failure: a randomized controlled trial. J Hosp Palliat Nurs. (2024) 26:E13–9. doi: 10.1097/NJH.0000000000000988
41. Habal MV, Micevski V, Greenwood S, Delgado DH, Ross HJ. How aware of advanced care directives are heart failure patients, and are they using them? Can J Cardiol. (2011) 27:376–81. doi: 10.1016/j.cjca.2010.12.067
42. Werdecker L, Kujawa M, Schneider N, Neitzke G. [Advance care planning: a qualitative investigation on patients' perspectives with advanced heart failure]. Z Gerontol Geriatr. (2019) 52:157–63. doi: 10.1007/s00391-018-1385-9
43. Liu L, Zhao Y, Yang C, Chan HY. Gamification for promoting advance care planning: a mixed-method systematic review and meta-analysis. Palliat Med. (2021) 35:1005–19. doi: 10.1177/02692163211005343
44. Yorke J, Yobo-Addo E, Singh K, Muzzam A, Khan I, Shokur N, et al. Baseline knowledge attitudes satisfaction and aspirations with advance care planning: a cross-sectional study. Am J Hosp Palliat Care. (2022) 39:448–55. doi: 10.1177/10499091211030447
45. Dias LM, Bezerra MR, Barra WF, Carvalho AEV, Castro L, Rego F. Advance care planning and goals of care discussion: the perspectives of brazilian oncologists. BMC Palliat Care. (2022) 21:165. doi: 10.1186/s12904-022-01052-w
46. Gelfman LP, Barnes DE, Goldstein N, Volow AM, Shi Y, Li B, et al. Quality and satisfaction with advance care planning conversations among English- and Spanish-speaking older adults. J Palliat Med. (2023) 26:1380–5. doi: 10.1089/jpm.2022.0565
47. Ribeiro C, Pamplona P, Simonds AK. Advance care planning in patients with respiratory failure. Eur Respir Rev. (2024) 33:240120. doi: 10.1183/16000617.0120-2024
48. Yeung CC, Ho KH, Chan HY. A dyadic advance care planning intervention for people with early-stage dementia and their family caregivers in a community care setting: a feasibility trial. BMC Geriatr. (2023) 23:115. doi: 10.1186/s12877-023-03815-3
49. Tan M, Tang S, Feder S, Xiao J, Huang C, Cook A, et al. Interventions to promote readiness for advance care planning: a systematic review and meta-analysis. Int J Nurs Stud. (2024) 156:104778. doi: 10.1016/j.ijnurstu.2024.104778
50. Clayton JM, Butow PN, Tattersall MHN. When and how to initiate discussion about prognosis and end-of-life issues with terminally ill patients. J Pain Symptom Manage. (2005) 30:132–44. doi: 10.1016/j.jpainsymman.2005.02.014
Keywords: advance care planning, heart failure, meta-analysis, systematic review, older adults
Citation: Chen L, Cheng Y, Qu J and Wang Z (2025) Implementation and effectiveness of advance care planning in hospitalized older adults with chronic heart failure: a mixed-methods systematic review and meta-analysis. Front. Med. 12:1566977. doi: 10.3389/fmed.2025.1566977
Received: 26 January 2025; Accepted: 15 April 2025;
Published: 29 April 2025.
Edited by:
Marios Kyriazis, National Gerontology Centre, CyprusReviewed by:
Xueying Ding, Weifang University of Science and Technology, ChinaNader Alnomasy, University of Hail, Saudi Arabia
Copyright © 2025 Chen, Cheng, Qu and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhangyi Wang, MjgzNTM3NTQ4QHFxLmNvbQ==; Jun Qu, NTIzMzk3NjhAcXEuY29t
 Li Chen
Li Chen Yuqiu Cheng1,2
Yuqiu Cheng1,2 Zhangyi Wang
Zhangyi Wang