- 1Faculty of Physical Education, Gdansk University of Physical Education and Sport, Gdańsk, Poland
- 2Department of Rheumatology and Orthopedics, Sichuan Province Orthopedic Hospital, Chengdu, China
- 3Faculty of Social and Humanities, WSB Merito University Gdansk, Gdańsk, Poland
Background: Mild cognitive impairment (MCI) is characterized by a progressive decline in memory and other cognitive functions, falling between normal cognition and dementia. Traditional Chinese Exercises (TCEs) have been proven effective for managing MCI. A dose–response meta-analysis was conducted to evaluate the correlation between exercise temporal parameters and their effectiveness in older adults with MCI.
Methods: Randomized controlled trials (RCTs) on TCEs for MCI were searched across eight databases from their inception to September 2024. Literature was screened based on inclusion and exclusion criteria. Data from the selected studies were extracted, and the risk of bias was assessed using the RoB2 tool. The quality of the included studies was evaluated using the PEDro scale. The visualizations were conducted using the “robvis” package in R 4.3.3 software, while Stata 15.0 software was used to analyze the dose–response relations.
Result: Out of 2,216 records,17 RCTs were included in the meta-analysis. Although significant heterogeneity was present among the studies, sensitivity analysis demonstrated good robustness. The results revealed significant improvements in cognitive function among older adults with MCI in the TCEs group: Montreal Cognitive Assessment (MoCA) (SMD = 1.04, 95% CI: 0.71–1.38) and Mini-Mental State Examination (MMSE) (SMD = 0.82, 95% CI: 0.41–1.42). The relations between exercise cycle, frequency, and overall cognitive function (MoCA and MMSE) followed a “Λ”-shaped curve. For MoCA, the relations with exercise duration also exhibited a “Λ”-shaped curve, while the relations between duration and MMSE was nonlinear. The peak improvements in MoCA and MMSE were observed at 12 weeks (25.59, 95% CI: 25.07–26.10) and 13 weeks (26.24, 95% CI: 25.38–27.09). Improvement was positively correlated with the number of cycles up to a peak, after which it declined, following a “Λ”-shaped pattern.
Conclusion: This study demonstrates a nonlinear dose–response relations between exercise temporal parameters and therapeutic effects on cognitive function in older adults with MCI. Regarding exercise cycle, MoCA and MMES yield the optimal outcomes at 12 and 13 weeks. For exercise frequency, MoCA and MMES optimize results at three times per week. Concerning exercise duration, MoCA achieves optimal results at 45 min; MMES shows gradual improvement after 30 min.
Systematic review registration: The study protocol was registered with PROSPER on May 29, 2024, under the registration number CRD42024510378, https://www.crd.york.ac.uk/PROSPERO/view/CRD42024510378
1 Introduction
More than 55 million people worldwide are currently living with dementia, a condition that is growing at an alarming rate. The number is projected to reach 78 million by 2030 and 115.4 million by 2050 (1, 2). Alzheimer’s disease (AD) is the most common cause of dementia, accounting for 60–80% of all cases (3, 4). Mild cognitive impairment (MCI) is often considered a transitional stage between normal cognitive function and clinically probable AD (5–7). While some older adults with MCI remain stable or even return to normal cognitive function over time, more than 50% progress to AD within 5 years (8). Active interventions during the MCI stage may effectively prevent or slow the progression to AD (9, 10). Engaging in regular physical exercise has been shown to alleviate the continuous decline in cognitive function and serves as a protective factor against the progression from MCI to dementia (11–13). Additionally, physical exercise has been proven to reduce the risk of cognitive impairment in older adults (14).
Traditional Chinese Exercises (TCEs) are comprehensive mind–body exercise approaches that involve the regulation of breathing, body movements, and consciousness as core components. The specific items included in TCEs, such as Tai Chi, Baduanjin, Wuqinxi, Yijinjing, and Liuzijue, etc. TCEs have been shown to improve cognitive function and provide long-term clinical benefits (15–17). Tai Chi exercise as well as Qigong enhances cognitive function and reduces the risk of falls (18). Baduanjin exercise improves cognitive function and attention (19, 20). Wuqinxi exercise may slow the deterioration of working memory (21), while Liuzijue exercise enhances memory and has a positive impact on brain health (22). These studies collectively demonstrate that TCEs are effective and viable methods for enhancing cognitive function. In clinical practice, therapeutic outcomes may vary depending on the frequency, duration, and cycles of TCEs. Some researchers recommend at least 12 weeks of practice, with sessions three times per week, lasting 30–60 min each (23). Others suggest sessions of 30–90 min, performed 3–6 times per week, over a total cycle of 8–36 weeks (24). Additionally, certain scholars propose a regimen of 3 months, with three sessions per week, each lasting 40 min (25). The aforementioned meta-analysis highlights significant differences in the recommended exercise parameters for TCEs. However, evidence-based practice has not conclusively demonstrated additional benefits from increasing the frequency or duration of exercise. Establishing dose–response relationships is crucial for enhancing the quality of evidence, as these relationships ensure the association between dose and response through objective methods, thereby facilitating the formulation of scientifically effective intervention.
Therefore, this study aimed to utilize a robust error meta-regression model (REMR) to explore the dose–response relations between exercise temporal parameters (including cycle, frequency, and duration) and cognitive function improvements in older adults with MCI. By drawing on high-quality evidence, the study seeks to provide optimal timing protocols for the treatment of MCI.
2 Methods
This study adheres to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses of the Effects of TCEs on the Cognitive Function of Older Adults with MCI (PRISMA-A) guidelines (Supplementary material) (26). The study protocol was registered with PROSPERO 1 on May 29, 2024, under the registration number CRD42024510378.
2.1 Literature search strategy
Two researchers independently conducted a systematic search across multiple databases, including PubMed, Embase, The Cochrane Library, Web of Science, China Biology Medicine, China National Knowledge Infrastructure (CNKI), Wanfang Database, and the VIP Chinese Science and Technology Periodicals Database. From the establishment of the database to September 2024. References from review articles and included publications were manually screened to supplement the relevant literature. The search strategy combined subject terms and free-text keywords in both Chinese and English, using the following terms: (“MCI” OR “Mild Cognitive Impairment” OR “Mild Cognitive Impairment Disease” OR “Cognitive Impairment” OR “Cognitive Function”) AND (“Chinese Traditional Exercises” OR “Exercises” OR “Health Qigong” OR “Baduanjin” OR “Tai Chi” OR “Tai Chi Chuan” OR “Wuqinxi” OR “Yijinjing” OR “Liuzijue”). No restrictions were applied regarding region, language, or publication type.
2.2 Inclusion and exclusion criteria
2.2.1 Inclusion criteria
This study follows the PICOS framework and only RCTs were included based on the following criteria:
1. Subjects were required to meet the diagnostic criteria for MCI, or refer to the diagnostic criteria established by Petersen et al. (27, 28);
2. Participants were aged ≥ 60 years;
3. The intervention group underwent a planned and organized TCEs therapy;
4. The control group received health education, engaged in other forms of exercise different from the intervention group, or maintained their original lifestyle;
5. The outcome measure was the overall cognitive function score, including the Montreal Cognitive Assessment (MoCA) and Mini-Mental State Examination (MMSE) scores (29, 30).
2.2.2 Exclusion criteria
Studies with the following characteristics were excluded:
1. Studies with unclear age descriptions for the subjects;
2. Studies where the subjects’ lifestyle included regular exercise;
3. Studies that excluded MCI caused by stroke, vascular diseases, or other diseases;
4. Studies with incomplete outcome data that could not be extracted;
5. Duplicate publications, clinical protocols, case reports, review articles, and non-randomized controlled trials;
6. Studies not published in Chinese or English.
2.3 Data extraction
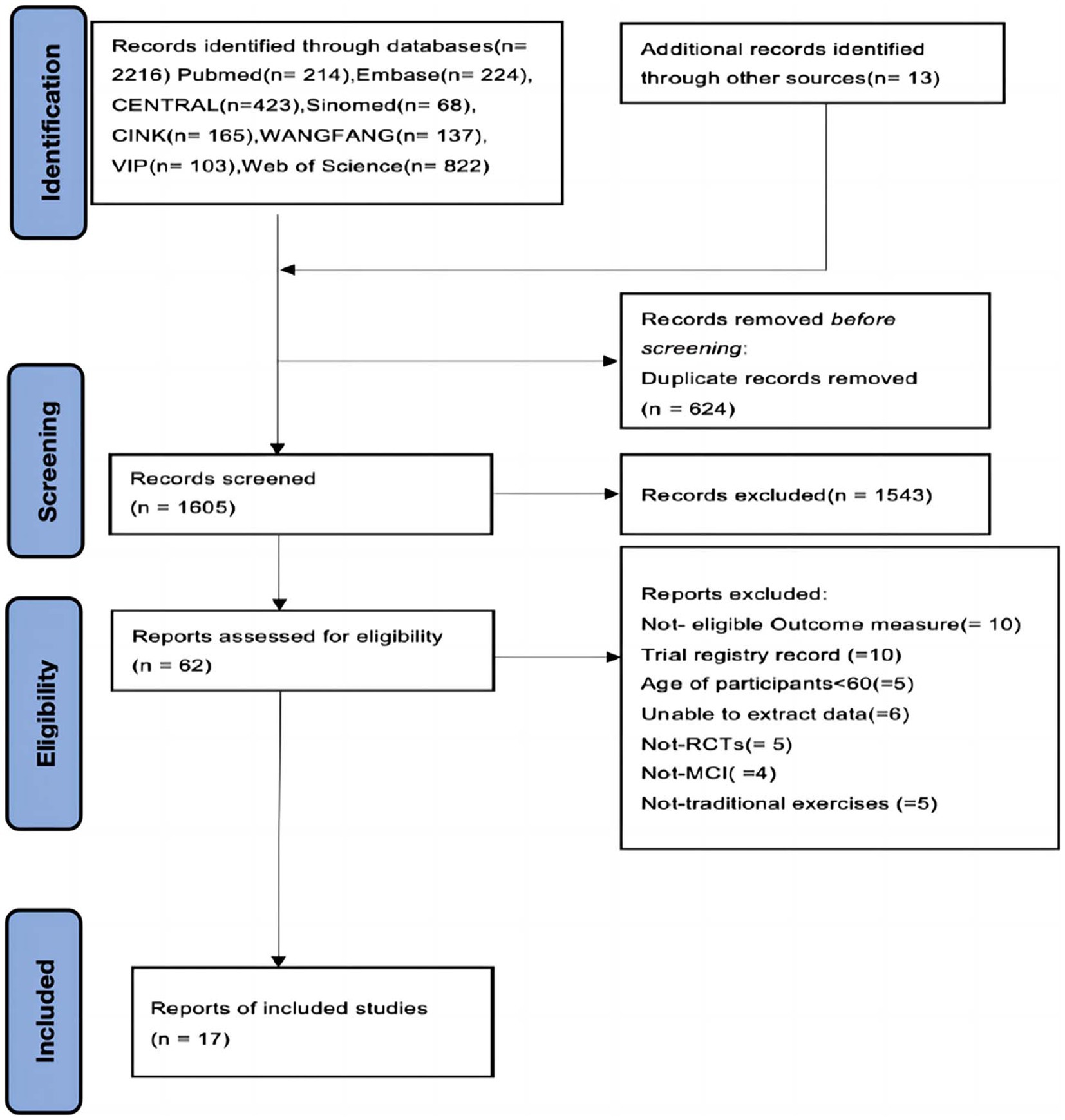
Duplicate literature was eliminated using EndNote 20 software. The titles and abstracts of the references were initially screened by two researchers (YL and LL), followed by a full-text review based on the inclusion and exclusion criteria. In cases of uncertainty, a third party (QL) was consulted to arbitrate. The PRISMA flowchart for literature screening is presented in Figure 1. Two researchers (QW and LL) independently extracted relevant information from the included studies. They reviewed and resolved any inconsistencies through discussion and negotiation, completing data merging and conversion (31). If any relevant information was unavailable, the corresponding authors were contacted for clarification. Data extraction was conducted using a predefined Excel sheet with the following categories: A. General Information: Literature ID, author details, year of publication, country, and participant characteristics (e.g., age, gender, sample size, and TCEs duration); B. Risk of Bias indicators: Randomization methods, blinding, and allocation concealment; C. TCEs Interventions: Details on interventions such as Baduanjin, Tai Chi, Wuqinxi, and Liuzijue, including exercise cycle, frequency, and duration; D. Outcomes: Mean and standard deviation of each post-test outcome.
2.4 Unification of data and dealing with missing data
Before conducting the statistical analysis, all extracted data were verified by one researcher (LL) to ensure accuracy. Corresponding authors were contacted to obtain any missing data. If the missing data could not be accurately retrieved, the study was excluded from the analysis.
2.5 Statistical analysis
We used R4.3.3 software, “robvis” package to assess bias risk and draw plots, and the “PEDro scale” to assess the quality of literature. The “Meta” package was used for meta-analysis, using the random-effects model (DerSimonian-Laird method), and I2 to measure heterogeneity quantitatively. Sensitivity analysis was performed when significant heterogeneity (I2 ≥ 50%) was present. The “forestplot” package was used to generate forest plots. We used Stata 15.0 software (Stata Corp., College Station, TX, United States) to analyze the dose–response relationship between TCEs exercise time parameters (cycle, frequency, and duration) and MoCA and MMSE improvements using robust error-meta regression (REMR). The effect size was estimated by the Standard Mean Difference (SMD) and 95% Confidence Interval (CI).
3 Results
3.1 Results of the literature search
A total of 2,216 records were obtained from eight databases (English and Chinese) and other meta literature, with 624 records remaining after deduplication. 1,543 literature entries were excluded after screening by titles and abstracts. After screening the full text of the remaining 62 studies, Not-eligible Outcome measure (=10), Frial registry record (=10), Age of participants<60 (=5), Unable to extract data (=6), Not-RCTs (= 5), Not-MCI (=4), Not-traditional exercises (=5). Finally, 17 eligible RCTs were included in this study, involving a total of 2,227older adults with MCI.
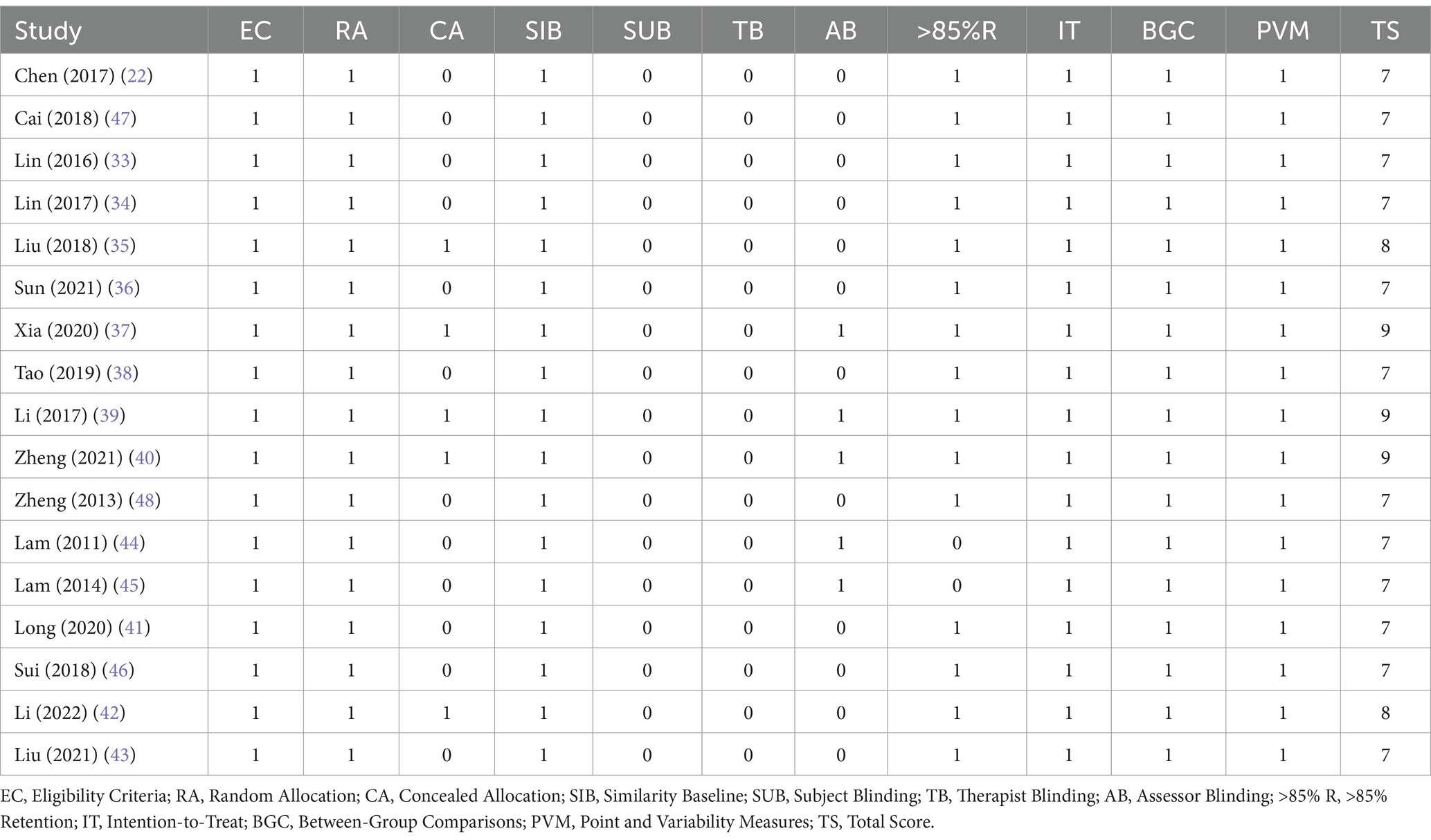
The articles were published between 2011 and 2023, with all 17 studies conducted in China. Seven articles were in English, and 10 were in Chinese. The study sample sizes ranged from 40 to 389, with an average of 118, and the mean age of participants was over 60 years. Table 1 summarizes the basic characteristics of the 17 studies included in the meta-analysis. None of the participants had prior experience with Traditional Chinese Exercises (TCEs) or regular exercise habits. In terms of exercise frequency, two studies did not report the number of sessions per week (22, 33), and one study did not report the duration exercise (34). The remaining studies provided complete details. Regarding outcomes, Thirteen studies included MoCA and MMSE assessments: 10 studies used MoCA outcome (19, 35–43), three studies used MMSE outcome (22, 44–46), and four studies used both MoCA and MMSE outcomes (33, 34, 47, 48).
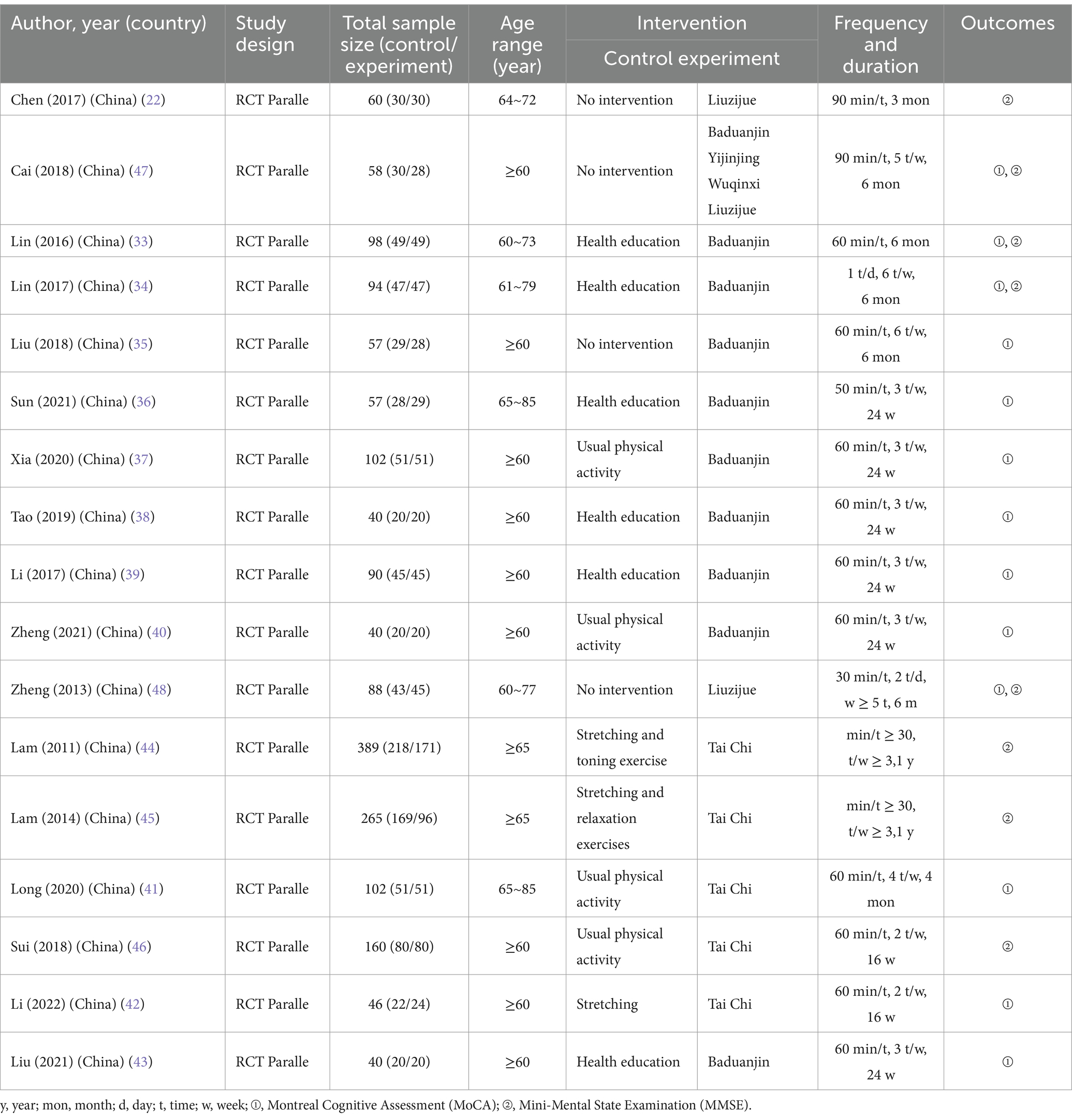
3.2 Risk of bias assessment
Figure 2 presents the results of the risk of bias assessment for RCTs indicating that their quality was relatively reliable. The high risk of bias was primarily due to deviations from intended interventions and the measurement of the outcome. Some concerns regarding bias were mainly due to deficiencies in the randomization process, missing outcome data, and selection of the reported result. High risk of bias was noted in four studies (22, 44–46), while seven studies demonstrated a low risk of bias (37, 38, 40–43, 47). The remaining studies all had some concerns regarding bias (19, 33–36, 39, 48).
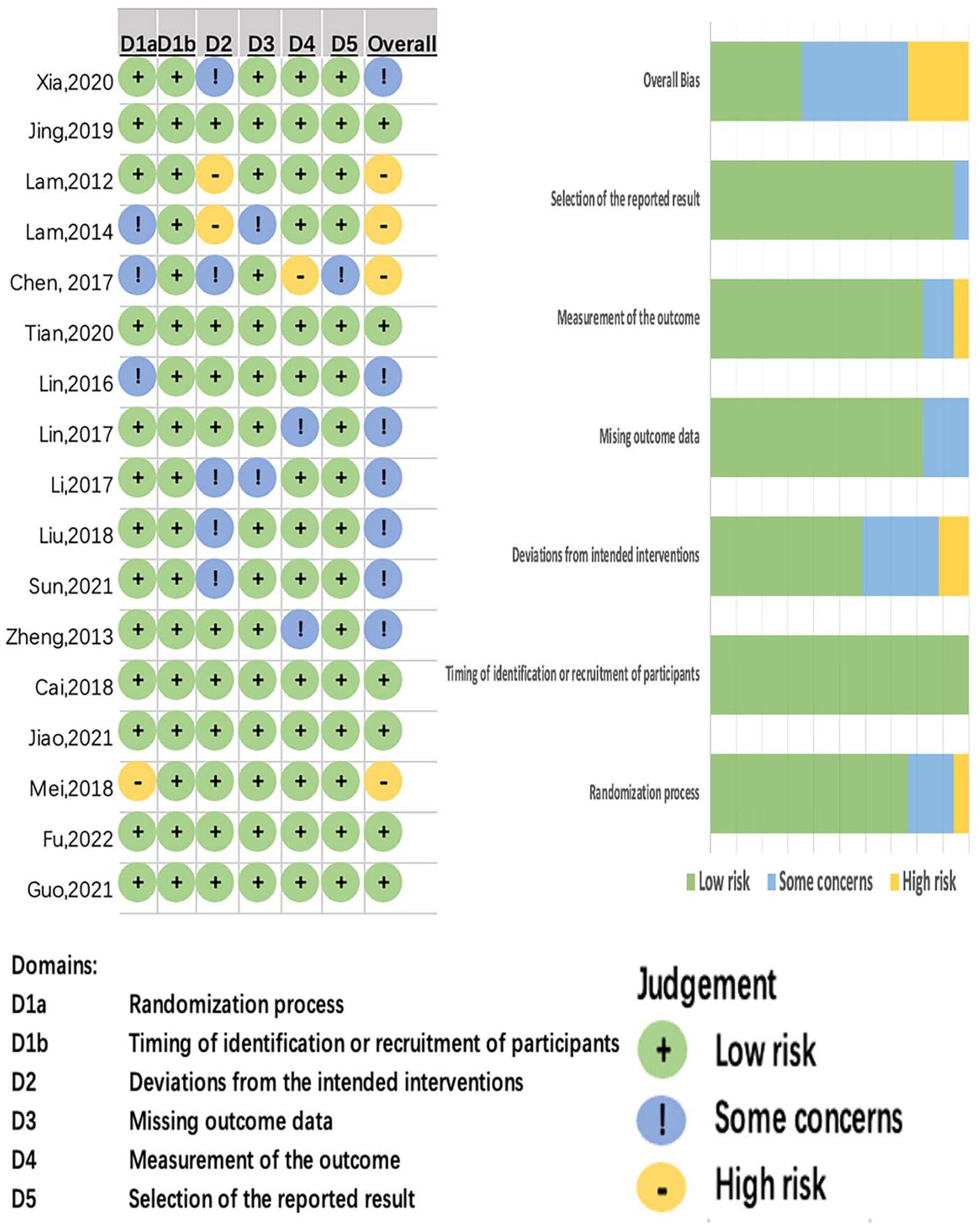
3.3 Quality assessment
Table 2 describes the completeness of the details of CTEs interventions reported in accordance with the Physiotherapy Evidence Database (PEDro) guidelines. No RCTs fulfilled all reporting items. Five items were consistently reported, earning a score of 5 points: random allocation, baseline similarity, intention-to-treat analysis, between-group comparisons, and point and variability measures. Due to the nature of exercise therapy, blinding of subjects and therapists was not possible, resulting in scores of 0 points for these two items. Additionally, five studies adopted allocation concealment in their experimental design, and five studies implemented single-blind protocols for assessor blinding. A study scoring 9 or 10 points was considered of very good quality, scores of 6–8 points reflected good quality, scores of 4–5 points indicated moderate quality, and scores of 0–3 points denoted poor quality (49). The results showed that all 17 studies scored between 7 and 9 points (Table 1), indicating the included studies were of good quality.
3.4 Intervention characteristics
Table 1 provides detailed information on TCE interventions for older adults with MCI. All included studies were RCTs with sample sizes ranging from 40 to 389, with the smallest sample size being 40 and the largest 389. In the control group, four studies had no intervention (22, 35, 47, 48), four studies focused on daily exercise (37, 40, 41, 46), six studies involved health education (33, 34, 36, 38, 39, 43), and three studies included stretching exercises (42, 44, 45). In the experimental group, nine studies examined Baduanjin (33–40, 43), five studies explored Tai Chi (41, 42, 44–46), two studies investigated Liuzijue (22, 40), and one study examined a combination of TCEs (Baduanjin, Tai Chi, Wuqinxi, Liuzijue) (47).
3.5 Meta-analysis
3.5.1 Meta-analysis of outcomes
3.5.1.1 Influence on the MOCA outcome
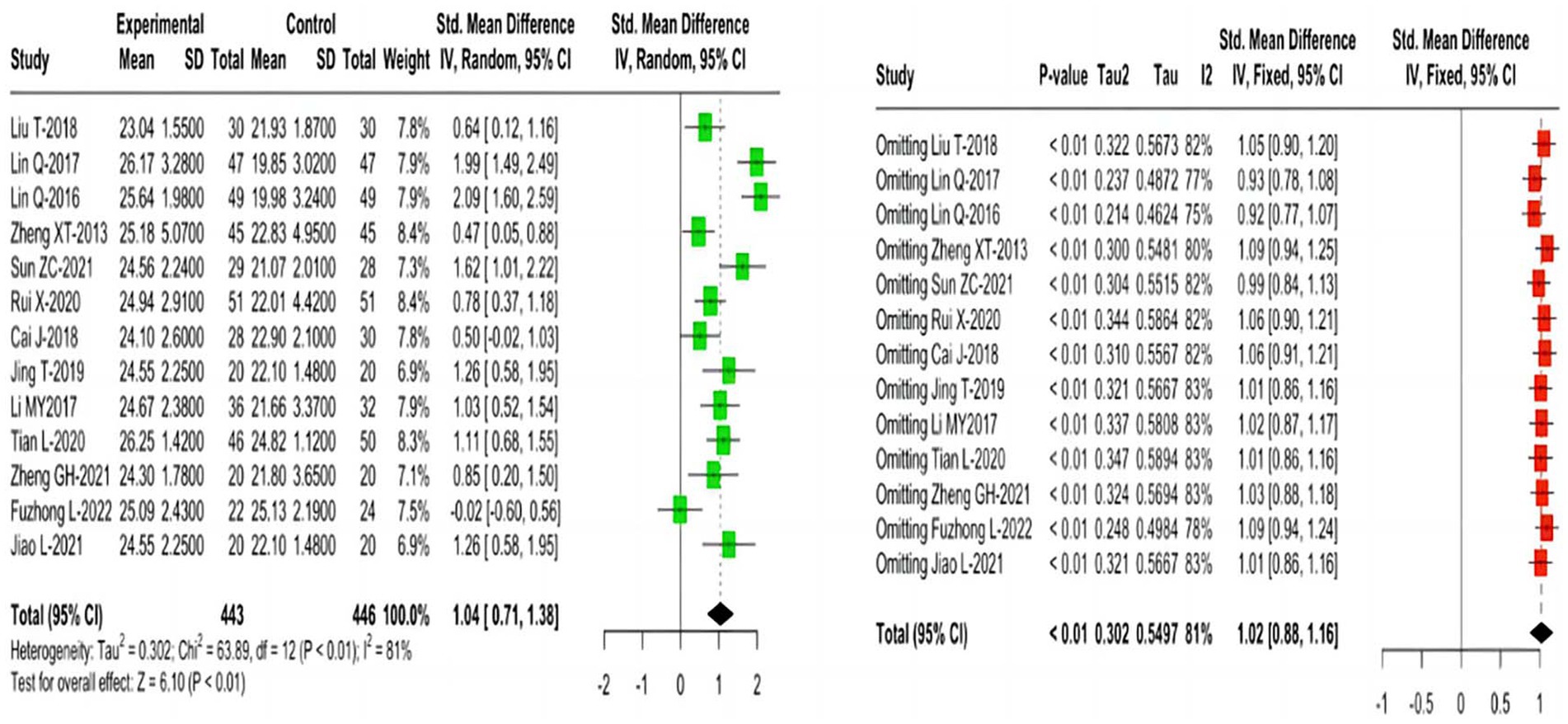
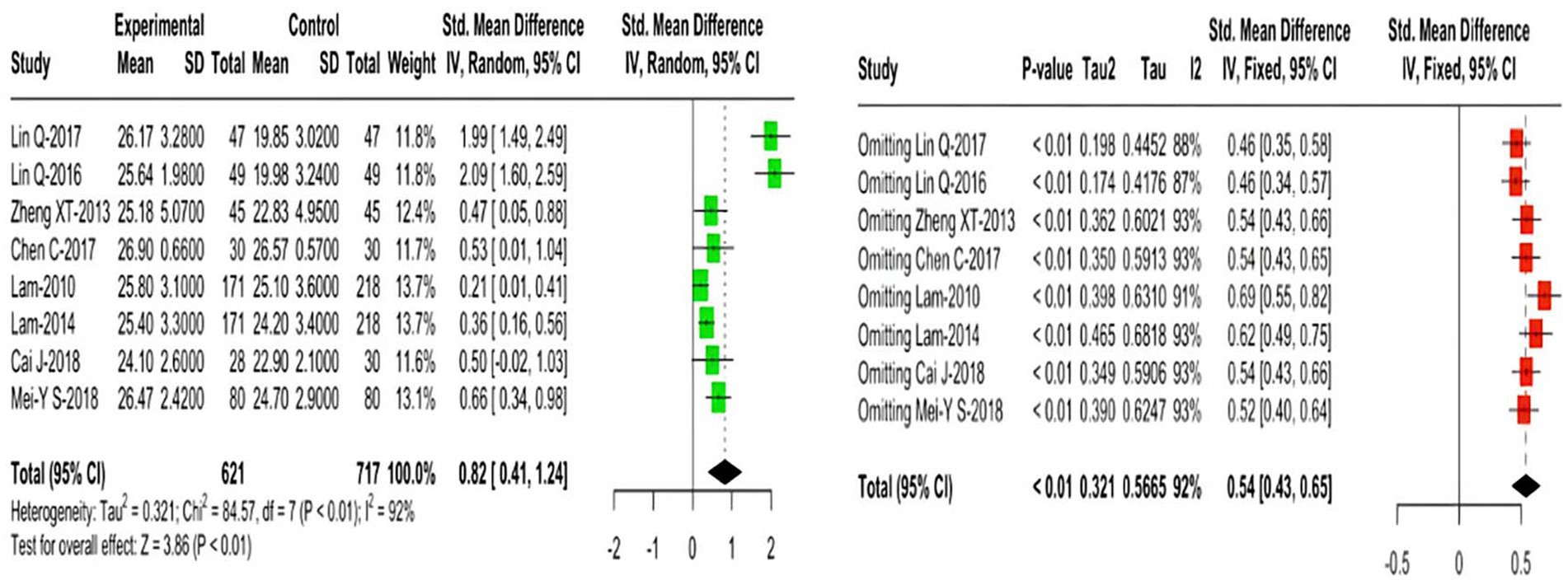
Thirteen studies reporting MoCA outcomes indicated that, compared with the control group, TCEs significantly improved cognitive function in older adults with MCI, using a random effects model (SMD = 1.04; 95% CI = 0.71 1.38; I2 = 81%). Sensitivity analysis demonstrated the good robustness of the result (Figure 3).
3.5.1.2 Impact on the MMSE outcome
Eight studies reporting MMSE outcomes indicated that, compared with the control group, TCEs significantly improved cognitive function in older adults with MCI, using a random-effects model (SMD = 0.82; 95% CI = 0.41 1.24; I2 = 92%). Further sensitivity analysis demonstrated the robustness (Figure 4).
3.5.2 Subgroup meta-analysis
Subgroup analyses used studies with MoCA and MMSE outcomes were conducted to investigate potential associations between efficacy and covariates (cycle, frequency, duration, and control type) (Table 3). TCEs demonstrated an overall enhancement in cognitive function. The MoCA results showed that the SMD for the experimental group was 1.28 (95% CI: 0.91–1.65) for Baduanjin, 0.57 (95% CI: −0.54–1.67) for Tai Chi, and 0.47 (95% CI: 0.05–0.88) for Liuzijue. The MMSE results revealed that the SMD for the experimental group was 2.04 (95% CI: 1.69–2.39) for Baduanjin, 0.38 (95% CI: 0.14–0.62) for Tai Chi, and 0.49 (95% CI: 0.17–0.82) for Liuzijue. For MoCA outcomes, the SMD for duration was 1.62 (95% CI: 1.01–2.22) for a practice duration of 50 min and 0.50 (95% CI: −0.02–1.03) for 90 min. For MMSE outcomes, the SMD for duration was 0.28 (95% CI: 0.13–0.43) for 30 min and 1.02 (95% CI: 0.20–1.85) for 60 min. Furthermore, the MoCA results demonstrated that the SMD for frequency ranged from −0.02 (95% CI: −0.60– 0.56) to 2.09 (95% CI: 1.60–2.59). Similarly, the MMSE results showed an SMD for frequency ranging from 0.28 (95% CI: 0.13–0.43) to 2.09 (95% CI: 1.60–2.59). The MoCA results indicated no significant statistical the experimental group (Tai Chi) (p = 0.32). However, variations in cycle, frequency, duration, experimental group, and control type were significantly associated with improvements in both MoCA and MMSE outcomes (p < 0.01).
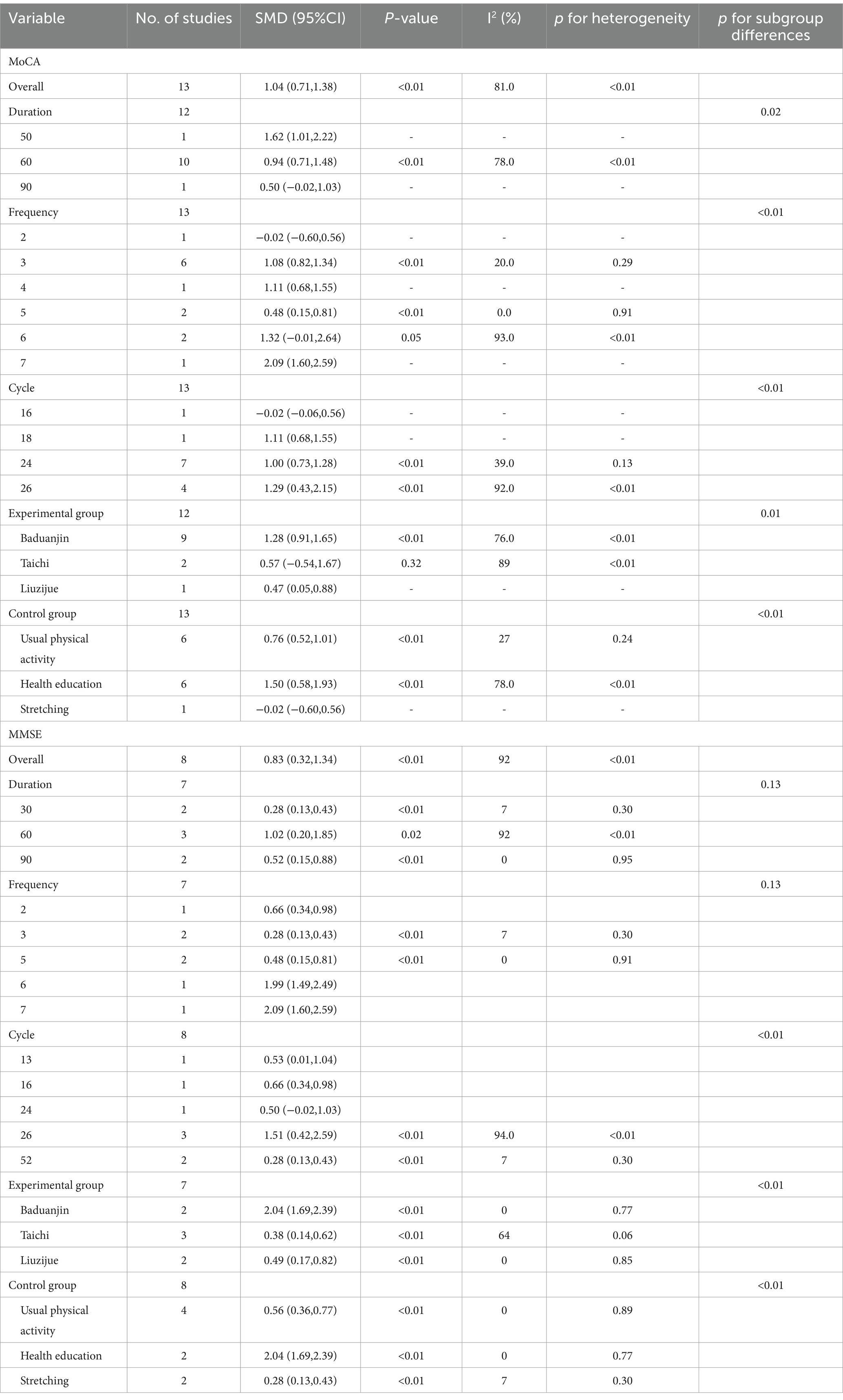
Table 3. Subgroup analysis results regarding the effects of Traditional Chinese Exercises on cognition function.
3.5.3 Dose–response meta-analysis
REMR methods were used to determine the non-linear, quantity-effectiveness relation between exercise temporal parameters (cycle, frequency, and duration) and the efficacy of overall cognitive function in MCI (improvements in MoCA and MMSE).
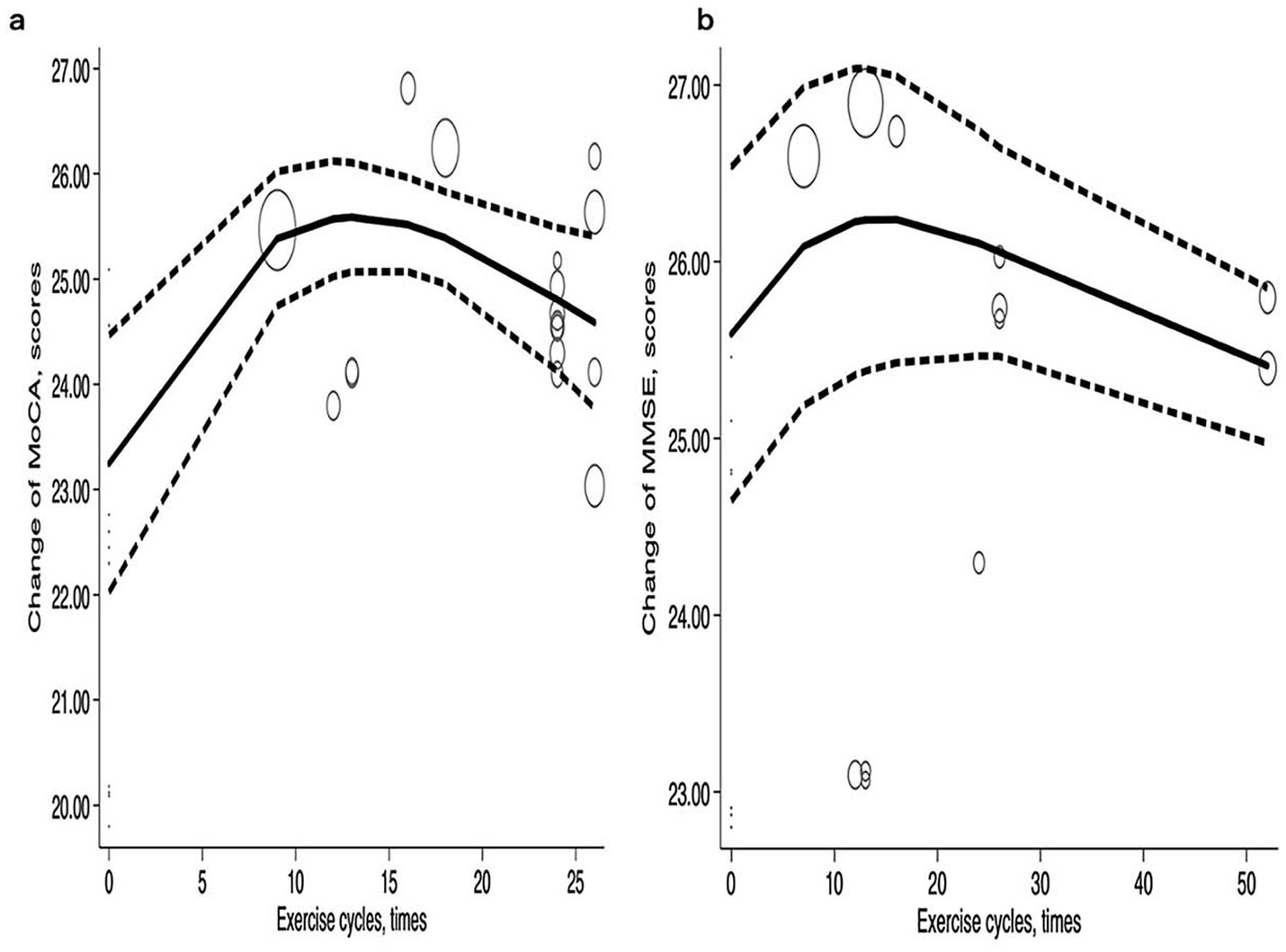
3.5.3.1 Exercise cycle
The exercise cycle refers to the process of facilitating physiological adaptation in the human body through systematic and periodic adjustments of load. In this study, a one-week timeframe was established as one exercise cycle. Within a certain range, the exercise cycle was positively correlated with improvements in MoCA and MMSE, but the effect began to decline after reaching a peak, showing a ‘Λ’ shape. Reaching the peak may result from the cumulative enhancement of the exercise cycle and overall cognitive ability, which promotes neuroplasticity in the brain and thereby assists patients in gradually recovering their cognitive functions. After nine exercise cycles, MoCA increased to 25.38 (95% CI: 24.74–26.02), and after 12 cycles, it peaked at 25.57 (95% CI: 25.02–26.12) before beginning to decline. MoCA improvements remained stable at 25.51 (95% CI: 25.07–25.96) after 16 cycles but decreased to 24.81 (95% CI: 24.13–25.49) after 24 cycles and further to 24.59 (95% CI: 23.77–25.41). For MMSE, the score increased to 26.23 (95% CI: 25.36–27.09) after 12 cycles, peaked at 26.24 (95% CI: 25.38–27.09) after 12 cycles, and stabilized at 26.24 (95% CI: 25.43–27.05) after 16 cycles. After 24 exercise cycles, the improvement slightly decreased to 26.10 (95% CI: 25.47–26.74) (Figure 5).
3.5.3.2 Exercise frequency
Figure 6 illustrates that with increased exercise frequency, improvements in MoCA and MMSE follow a ‘Λ’ pattern. Exercise frequency three times per week in a scientifically structured and appropriately tailored manner may represent a reasonable frequency for facilitating the recovery and enhancement of cognitive function in patients. The curves are similar, and the inflection points and peak values are consistent. The most significant improvements in MoCA and MMSE were observed at an exercise frequency of three times per week. Subsequently, MoCA stabilizes in a steady state, while MMSE exhibits a relatively rapid decline during the later phase. At an exercise frequency of two times per week, MoCA improved to 24.97 (95% CI: 24.15–25.79) and MMSE increased to 25.78 (95% CI: 24.66–26.61). With an exercise frequency of 3 times per week, MoCA peaked at 25.64 (95% CI: 24.62–25.89) and MMSE increased to 25.68 (95% CI: 24.84–26.52). When exercise frequency was maintained at four times per week, MoCA remained elevated at 25.26 (95% CI: 24.78–25.73), but it decreased to 24.5 (95% CI: 23.03–25.96) when exercise frequency increased to seven times per week. Additionally, the MMSE score began to decline after peaking at three times per week. An exercise frequency of seven times per week resulted in a significant decrease in the MMSE score, yielding a value of 24.25 (95% CI: 22.40–26.09).
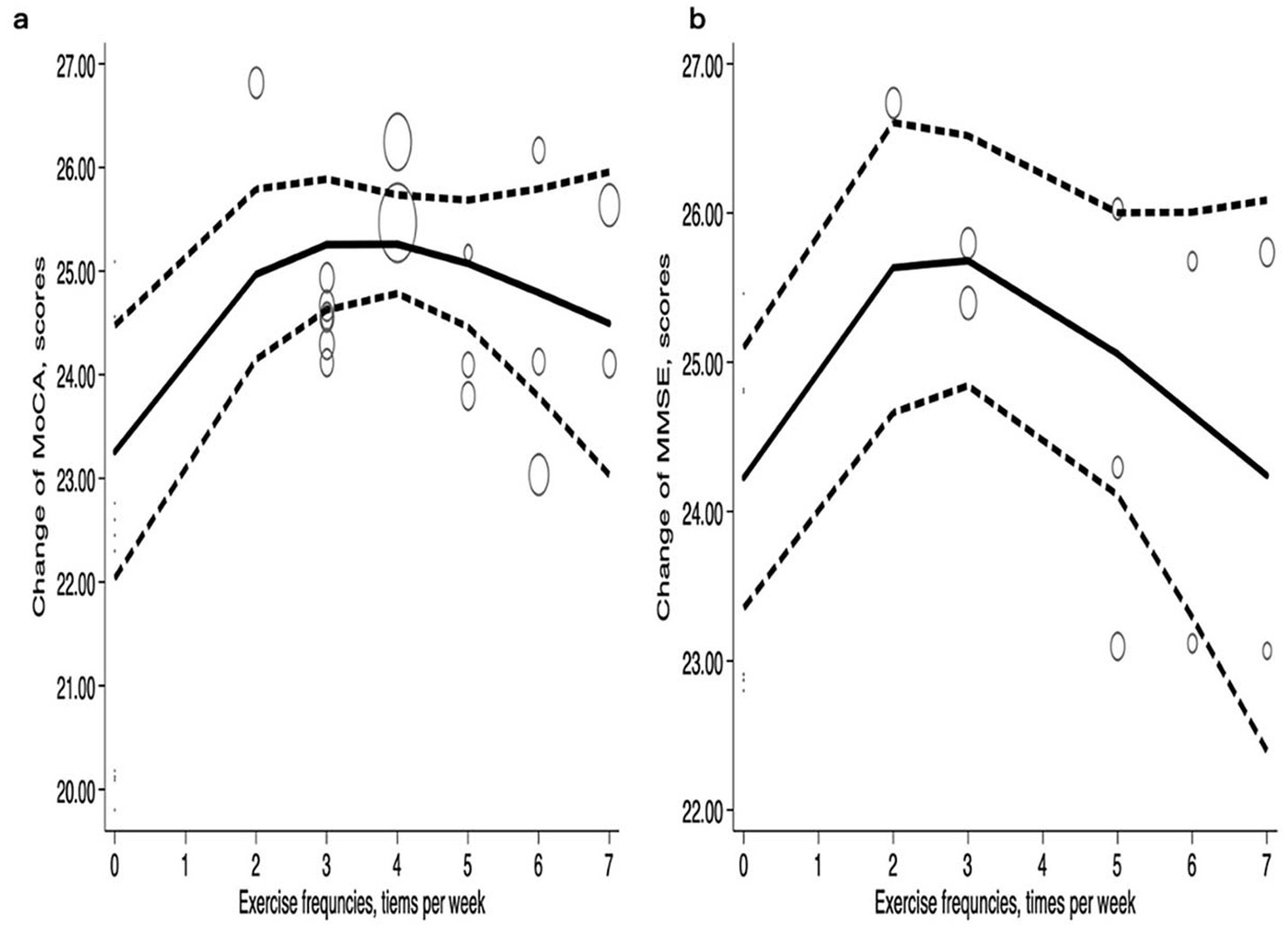
Figure 6. Dose–response relations between exercise frequencies and changes of (a) MoCA and (b) MMSE.
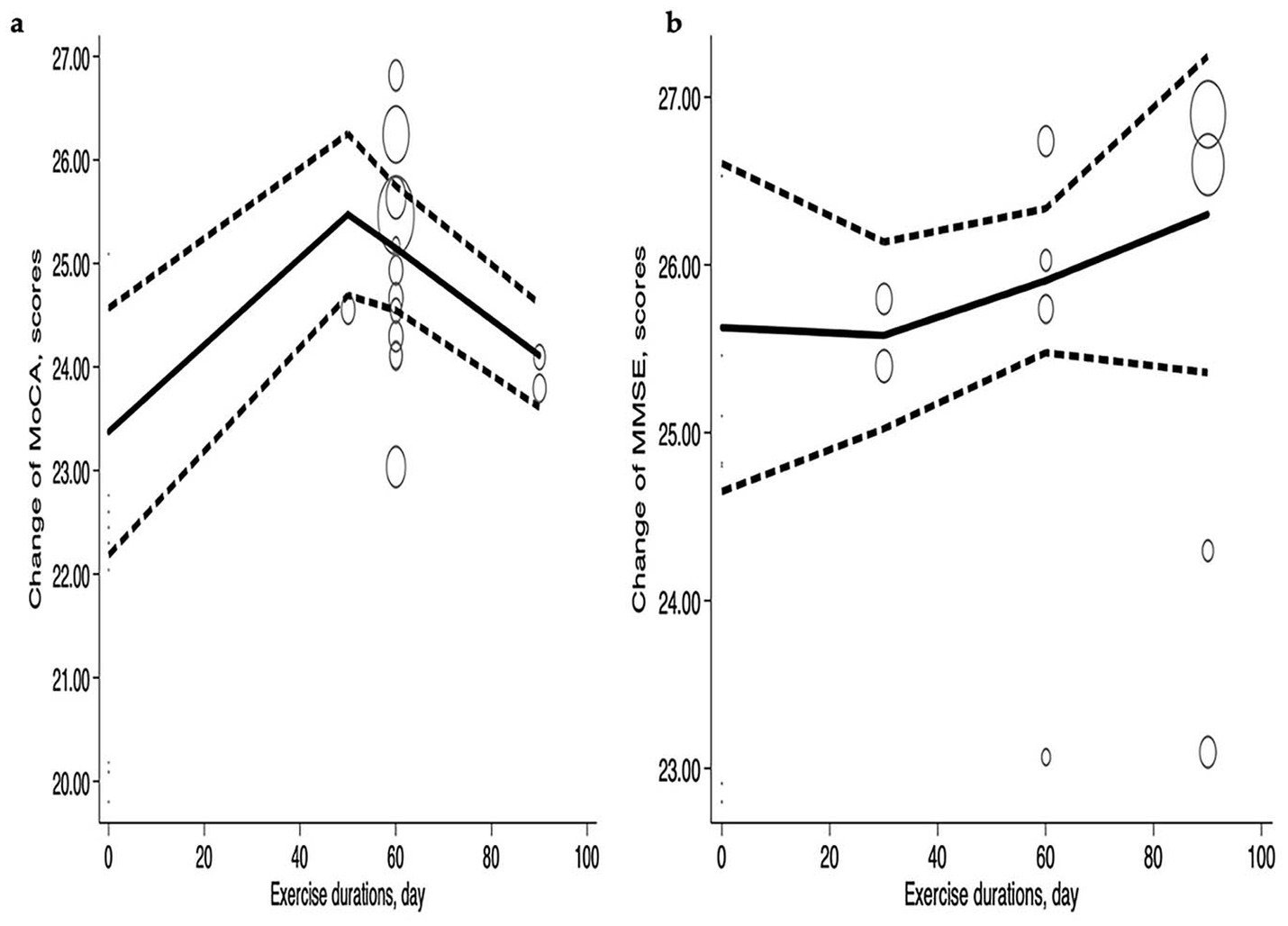
3.5.3.3 Exercise duration
Figure 7 illustrates the improvement in MoCA and MMSE scores as exercise duration increases. MoCA reached its peak value of 25.47 (95% CI: 24.69–26.25) at an exercise duration of 50 min, exhibiting a ‘Λ’ pattern. At 30 min, MMSE showed a slight decrease before improving over time. MoCA declined slightly to 25.15 (95% CI: 24.55–25.75) at 60 min and further decreased to 24.11 (95% CI: 23.61–24.61) at 90 min. In contrast, MMSE scores increased with longer exercise durations. There was a slight improvement at 30 min, reaching 25.58 (95% CI: 25.02–26.14), and the most significant improvement occurred at 90 min, with a value of 26.3 (95% CI: 25.36–27.24). The MoCA and MMSE scores reaching the peak may result from exercise duration may ensure an adequate level of physical activity, thereby promoting the restoration of cognitive functions.
4 Discussion
This study exclusively conducted a dose–response meta-analysis for overall cognitive function (MoCA and MMSE), with a comprehensive analysis of the novelty associated with three temporal parameters (cycle, frequency, and duration). This approach contrasts sharply with previous studies that predominantly focused on a single parameter. Furthermore, prior meta-analyses encompassed overall cognitive function as well as specific domains such as long-term memory, short-term memory, language abilities, and conversion. On the one hand, this study failed to include indicators of exercise intensity, which may limit its comprehensiveness. On the other hand, the accuracy of the REMR effect may be influenced by the use of SMD. Furthermore, only 1–2 indicators were typically selected in exercise dose–response meta-analysis studies. Generally, at least 10 samples are required for meta-regression analysis (50). MoCA and MMSE were chosen for this study due to their robust data support in assessing older adults with MCI and their widespread application in research.
TCEs significantly enhance cognitive function in older adults, particularly in terms of overall cognition, and exhibit a significant correlation with improvements in MCI. The included studies have indicated an uneven distribution of exercise temporal parameters. The exercise cycle predominantly focused on 16 weeks and 24 weeks, with the shortest cycle being 12 weeks and the longest extending to 1 year. Exercise frequency were primarily centered around 3 times per week, ranging from a minimum of 2 to a maximum of 7 times per week. Exercise duration typically emphasized 60 min per session, with durations spanning from a minimum of 30 min to a maximum of 90 min. Furthermore, TCEs demonstrate substantial effects in older adults with MCI. The data support a strong correlation between these factors, which is largely influenced by the exercise temporal parameters. A previous meta-analysis indicated that Baduanjin exercises yield optimal results when performed for 3 months, at a frequency of 3 times per week, with each session lasting 60 min (25). However, variability in exercise temporal parameters leads to discrepancies in efficacy, complicating the effective evaluation of optimal outcomes.
The study demonstrated a nonlinear dose–response relationship between exercise temporal parameters and cognitive function outcomes in older adults with MCI. The most pronounced improvement in cognitive function, as assessed by MoCA and MMSE, was observed after 12 weeks of exercise. Furthermore, both MoCA and MMSE exhibited a positive correlation with exercise frequency, with significant enhancement observed at a frequency of three sessions per week. Although significant heterogeneity was present in the study, sensitivity analysis demonstrated strong robustness. Subgroup analyses explored the potential impact of cycle, frequency, duration, experimental type, and control type. The results indicated significant associations between these factors and the efficacy of TCEs. Previous studies have also demonstrated that TCEs significantly improve MCI. TCEs have beneficial effects on overall cognition and memory, with Baduanjin showing more pronounced effects on overall cognition compared to other TCEs (51). TCEs possess the potential to enhance both global cognitive function and various domains of cognitive function (52, 53). In the network meta-analysis, the MMSE results ranked Baduanjin exercise (78%) as the best intervention, with Tai Chi (36%) ranking second. The MoCA results ranked Baduanjin exercise (62%) as the best intervention (54). Certain scholars contend that Tai Chi is effective in enhancing cognitive function among older adults and mitigating the onset of cognitive impairment (55). As research has progressed, an increasing number of scholars have focused on the influence of temporal parameters on cognitive function. A prior meta-analysis revealed that Tai Chi exercise interventions should be last for 12 weeks, with three times per week, each lasting between 30 and 60 min (23). Others believe that Tai Chi and Qigong may improve cognitive function and increase αβ1-42 protein levels while reducing Tau protein levels in older adults with mild to moderate cognitive impairment. They recommend exercises lasting 30–90 min per session, with a frequency of 3–6 times per week, over a total cycle of 8–36 weeks (23, 24). Additionally, some scholars argue that greater benefits may be achieved through more frequent participation in group classes and home practice, ideally at least 5 times per week (56). TCEs have been shown to enhance cognitive function in older adults with MCI, with recommendations suggesting an exercise cycle of at least 3 months, a frequency of 3 times per week, and a duration of 40 min per session (25). However, there remains a lack of standardized therapeutic guidelines. Our study identified nonlinear relationships among exercise cycle, frequency, and duration, as well as their effects on outcomes. This phenomenon may be attributed to the use of different analytical models. In clinical practice, the efficacy of exercise is closely related to the accumulation of “Exercise Temporal Parameters,” and the dose–response relationship does not follow a simple linear pattern. Therefore, nonlinear models may provide a more suitable framework for understanding this relationship.
Although a previous study found a significant correlation between exercise frequency and MCI outcomes (25), our study is the first to investigate the dose–response relationships between exercise temporal parameters and MCI outcomes. Moreover, it is unique in its comprehensive evaluation of the “Exercise Temporal Parameters,” specifically cycle, frequency, and duration. Based on the previous studies, it has been observed that cognitive function outcomes fluctuate among older adults with MCI (23–25, 56). Consequently, this study employs both MoCA and MMSE to objectively evaluate and validate the robustness of the dose–response relationship. Previous research has indicated that the optimal stimulation frequency for both MoCA and MMSE is moderate, specifically three times per week. This may be due to the observation that while MoCA scores gradually decline, the decline is not entirely irreversible. Adverse reactions associated with TCEs were documented in the included studies. Nevertheless, TCEs appear to be a safe and effective intervention for enhancing cognitive function in older adults. Furthermore, TCEs have been shown to improve overall cognitive function in older adults with MCI.
5 Limitations and strengths
This study has several limitations. Firstly, the regional bias introduced by the fact that all studies were conducted in China may limit the generalizability of the findings to other populations. Secondly, there is significant heterogeneity among the included studies, potentially influenced by temporal factors, variations in exercise types, and individual characteristics. Therefore, caution is warranted when interpreting the aggregated results. Thirdly, the REMR analysis did not consider other aspects of cognitive function, such as long-term memory, short-term memory, language abilities, and cognitive transfer. Moreover, most of the included studies primarily reported baseline and outcome data only, which could affect the robustness of both the model and its conclusions. Finally, while our findings focus on MoCA and MMSE scores, dose–response relationships for other therapeutic outcomes may differ and warrant further investigation.
6 Conclusion
In summary, our study reveals a non-linear dose–response relationship between exercise duration and the enhancement of cognitive function in older adults with MCI. The most significant improvements in MoCA and MMSE scores were observed after a 12 weeks and 13 weeks intervention period. Furthermore, both MoCA and MMSE exhibit a positive correlation with exercise frequency, with an optimal regimen of 3 times per week identified as the most effective approach. In terms of exercise duration, MoCA shows the most significant improvement at 45 min, while MMSE demonstrates a gradual upward trend after 30 min. Nevertheless, additional large-scale and rigorously designed randomized controlled trials are necessary to validate these findings. Future research should also explore the underlying structural mechanisms contributing to the differential effects associated with varying exercise duration and frequency parameters.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
QW: Formal analysis, Methodology, Software, Writing – original draft, Writing – review & editing. QL: Methodology, Software, Writing – review & editing. YL: Data curation, Writing – review & editing. LL: Data curation, Writing – review & editing. MB: Supervision, Writing – review & editing. DW: Supervision, Visualization, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2025.1568835/full#supplementary-material
Footnotes
References
1. University Asdim. World Alzheimer report (2021) Available online at: https://www.alzint.org/resource/world-alzheimer-report-2021/. (Accessed 15 April 2024).
2. Baazaoui, N, and Iqbal, K. A novel therapeutic approach to treat Alzheimer's disease by neurotrophic support during the period of synaptic compensation. J Alzheimers Dis. (2018) 62:1211–8. doi: 10.3233/JAD-170839
3. Winblad, B, Palmer, K, Kivipelto, M, Jelic, V, Fratiglioni, L, Wahlund, LO, et al. Mild cognitive impairment—beyond controversies, towards a consensus: report of the international working group on mild cognitive impairment. J Intern Med. (2004) 256:240–6. doi: 10.1111/j.1365-2796.2004.01380.x
4. Rostagno, AA. Pathogenesis of Alzheimer's disease. Int J Mol Sci. (2022) 24:10107. doi: 10.3390/ijms24010107
5. Gauthier, S, Reisberg, B, Zaudig, M, Petersen, RC, Ritchie, K, Broich, K, et al. Mild cognitive impairment. Lancet. (2006) 367:1262–70. doi: 10.1016/S0140-6736(06)68542-5
6. Petersen, RC. Mild cognitive impairment. Continuum. (2016) 22:404–18. doi: 10.1212/CON.0000000000000313
7. Domínguez-Chávez, CJ, Murrock, CJ, and Salazar-González, BC. Mild cognitive impairment: a concept analysis. Nurs Forum. (2019) 54:68–76. doi: 10.1111/nuf.12299
8. Wang, L, and Zhao, Y. Early recognition of mild cognitive impairment and research progress of relevant theoretical models. Chin J Nurs. (2018) 53:661–664. Available from: https://kns.cnki.net/kcms/detail/detail.aspx?dbcode=CJFD&filename=ZHHL201806002
9. Petersen, RC, Lopez, O, Armstrong, MJ, Getchius, TSD, Ganguli, M, Gloss, D, et al. Practice guideline update summary: mild cognitive impairment. Neurology. (2018) 90:126–35. doi: 10.1212/WNL.0000000000004826
10. Langa, KM, and Levine, DA. The diagnosis and management of mild cognitive impairment: a clinical review. JAMA. (2014) 312:2551–61. doi: 10.1001/jama.2014.13806
11. Zhou, Y, Zhou, X, Wang, J, and Wang, L. Risk factors and protective factors for the progression of mild cognitive impairment towards dementia. Chin General Pract. (2018) 21:4149–56. Available from: https://kns.cnki.net/kcms/detail/detail.aspx?dbcode=CJFD&filename=QKYX201833006
12. Sanders, LMJ, Hortobágyi, T, Karssemeijer, EGA, Van der Zee, EA, Scherder, EJA, and van Heuvelen, MJG. Effects of low- and high-intensity physical exercise on physical and cognitive function in older persons with dementia: a randomized controlled trial. Alzheimers Res Ther. (2020) 12:28. doi: 10.1186/s13195-020-00597-3
13. Nuzum, H, Stickel, A, Corona, M, Zeller, M, Melrose, RJ, and Wilkins, SS. Potential benefits of physical activity in MCI and dementia. Behav Neurol. (2020) 2020:1–10. doi: 10.1155/2020/7807856
14. Ahlskog, JE, Geda, YE, Graff-Radford, NR, and Petersen, RC. Physical exercise as a preventive or disease-modifying treatment of dementia and brain aging. Mayo Clin Proc. (2011) 86:876–84. doi: 10.4065/mcp.2011.0252
15. Zheng, G, Huang, M, Li, S, Li, M, Xia, R, Zhou, W, et al. Effect of Baduanjin exercise on cognitive function in older adults with mild cognitive impairment: study protocol for a randomised controlled trial. BMJ Open. (2016) 6:e010602. doi: 10.1136/bmjopen-2015-010602
16. Yu, AP, Chin, EC, Yu, DJ, Fong, DY, Cheng, CP, Hu, X, et al. Tai chi versus conventional exercise for improving cognitive function in older adults: a pilot randomized controlled trial. Sci Rep. (2022) 12:8868. doi: 10.1038/s41598-022-12526-5
17. Wang, Q, and Sheng, Y. Effect of tai Ji Quan on cognitive function in old adults with mild cognitive impairment. Chin J Rehabil Theory Pract. (2016) 22:645–9. Available from: https://kns.cnki.net/kcms/detail/detail.aspx?dbcode=CJFD&filename=ZKLS201606015
18. Sungkarat, S, Boripuntakul, S, Chattipakorn, N, Watcharasaksilp, K, and Lord, SR. Effects of tai chi on cognition and fall risk in older adults with mild cognitive impairment: a randomized controlled trial. J Am Geriatr Soc. (2017) 65:721–7. doi: 10.1111/jgs.14594
19. Xia, R, Wan, M, Lin, H, Ye, Y, Chen, S, and Zheng, G. Effects of mind-body exercise Baduanjin on cognition in community-dwelling older people with mild cognitive impairment: a randomized controlled trial. Neuropsychol Rehabil. (2023) 33:1368–83. doi: 10.1080/09602011.2022.2099909
20. Li, K, Yu, H, Kortas, JA, Lin, X, and Lipowski, M. The effect of 12 weeks of Baduanjin exercise on cognitive function, lower limb balance and quality of life of the elderly with mild cognitive impairment: a randomized controlled trial. Gazzetta Med Ital Arch Per LE Sci Med. (2022) 181:811–23. doi: 10.23736/S0393-3660.22.04802-1
21. Luo, SSCL, Wang, GB, Wang, YG, and Su, XY. Effects of long-term Wuqinxi exercise on working memory in older adults with mild cognitive impairment. Eur Geriatr Med. (2022) 13:1327–33. doi: 10.1007/s41999-022-00709-2
22. Chen, C, Luan, L, Zhang, Y, Zhang, Y, and Zhao, D. Clinical study on effects of six-word common health qigong on electroencephalogram in patients with mild cognitive impairment. Shanghai J Tradition Chin Med. (2017) 51:54–7. Available from: https://kns.cnki.net/kcms/detail/detail.aspx?dbcode=CJFD&filename=SHZC201706017
23. Wei, L, Chai, Q, Chen, J, Wang, Q, Bao, Y, Xu, W, et al. The impact of tai chi on cognitive rehabilitation of elder adults with mild cognitive impairment: a systematic review and meta-analysis. Disabil Rehabil. (2022) 44:2197–206. doi: 10.1080/09638288.2020.1830311
24. Cai, H, Zhang, K, Wang, M, Li, X, Ran, F, and Han, Y. Effects of mind-body exercise on cognitive performance in middle-aged and older adults with mild cognitive impairment: a meta-analysis study. Medicine. (2023) 102:e34905. doi: 10.1097/MD.0000000000034905
25. Zhao, Z. A Meta-analysis of the effect of traditional aerobic rehabilitation exercise on cognitive function in the elderly with mild cognitive impairment. Guiding J Tradition Chin Med Pharmacy. (2020) 26:92–95. Available from: https://kns.cnki.net/kcms/detail/detail.aspx?dbcode=CJFD&filename=ZYYZ202001021
26. Moher, D, Liberati, A, Tetzlaff, J, and Altman, DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6:e1000097. doi: 10.1371/journal.pmed.1000097
27. Petersen, RC, Smith, GE, Waring, SC, Ivnik, RJ, Tangalos, EG, and Kokmen, E. Mild cognitive impairment: clinical characterization and outcome. Arch Neurol. (1999) 56:303–8.
28. The Neurology Group of the Geriatrics Branch of the Chinese Medical Association. The expert consensus working group on diagnosis and treatment of cognitive impairment in older adults. Expert recommendations for the diagnostic and therapeutic procedures for cognitive impairment in Chinese older adults. Chin J Geriatr. (2014) 33:817–25. Available from: https://kns.cnki.net/kcms/detail/detail.aspx?dbcode=CJFD&filename=ZLXZ201409001
29. Nasreddine, ZS, Phillips, NA, Bédirian, V, Charbonneau, S, Whitehead, V, Collin, I, et al. The Montreal cognitive assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. (2005) 53:695–9. doi: 10.1111/j.1532-5415.2005.53221.x
30. Folstein, MF, Folstein, SE, and McHugh, PR. "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. (1975) 12:189–98.
31. Higgins, JP, Thompson, SG, Deeks, JJ, and Altman, DG. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
32. Sterne, JAC, Savović, J, Page, MJ, Elbers, RG, Blencowe, NS, Boutron, I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. (2019) 366:l4898. doi: 10.1136/bmj.l4898
33. Lin, Q. The effect of Baduanjin exercise intervention on cognitive function in patients with mild cognitive Impairmen. Shandong Med J. (2016) 56:113–114. Available from: https://kns.cnki.net/kcms/detail/detail.aspx?dbcode=CJFD&filename=SDYX201636031
34. Lin, Q. The application effect of Baduanjin exercise and improvement of cognitive function in elderly patients with mild cognitive impairment. Chin J Gerontol. (2017) 37:3558–3560. Available from: https://kns.cnki.net/kcms/detail/detail.aspx?dbcode=CJFD&filename=ZLXZ201714021
35. Liu, T, Guo, S, and Bai, S. Effect of Baduanjin on cognition in patients with mild cognitive impairment. Chinese J Rehabil Theory Pract. (2018) 24:854–9. Available from: https://kns.cnki.net/kcms/detail/detail.aspx?dbcode=CJFD&filename=ZKLS201807020
36. Sun, Z, Ma, J, Gu, X, Ouyang, G, Zhang, N, Chen, X, et al. Baduanjin training based on virtual reality can relieve mild cognitive impairment in the elderly. Chin J Phys Med Rehabil. (2021) 43:322–326. doi: 10.3760/cma.j.issn.0254-1424.2021.04.007
37. Xia, R. Neural mechanism of Baduanjin intervention forCognitive frailty based on triple brain network model [Thesis]: Fujian University of Traditional Chinese Medicine; (2020).
38. Tao, J, Liu, J, Chen, X, Xia, R, Li, M, Huang, M, et al. Mind-body exercise improves cognitive function and modulates the function and structure of the hippocampus and anterior cingulate cortex in patients with mild cognitive impairment. Neuroimage Clin. (2019) 23:101834. doi: 10.1016/j.nicl.2019.101834
39. Li, M. The effect of Baduanjin exercise on mild cognitive impairment: A functional imaging study based on the default mode network [Thesis]: Fujian University of Traditional Chinese Medicine; (2017).
40. Zheng, G, Ye, B, Xia, R, Qiu, P, Li, M, Zheng, Y, et al. Traditional Chinese mind-body exercise Baduanjin modulates gray matter and cognitive function in older adults with mild cognitive impairment: a brain imaging study. Brain Plast. (2021) 7:131–42. doi: 10.3233/BPL-210121
41. Long, T. The effect of Taijiquan on cognitive function and executive function in MCI elderly people. J Chengde Med Coll. (2020) 37:44–46. Available from: https://kns.cnki.net/kcms/detail/detail.aspx?dbcode=CJFD&filename=CDYX202001027
42. Li, F, Harmer, P, Fitzgerald, K, and Winters-Stone, K. A cognitively enhanced online tai Ji Quan training intervention for community-dwelling older adults with mild cognitive impairment: a feasibility trial. BMC Geriatr. (2022) 22:76. doi: 10.1186/s12877-021-02747-0
43. Liu, J, Tao, J, Xia, R, Li, M, Huang, M, Li, S, et al. Mind-body exercise modulates locus Coeruleus and ventral tegmental area functional connectivity in individuals with mild cognitive impairment. Front Aging Neurosci. (2021) 13:646807. doi: 10.3389/fnagi.2021.646807
44. Lam, LC, Chau, RC, Wong, BM, Fung, AW, Lui, VW, Tam, CC, et al. Interim follow-up of a randomized controlled trial comparing Chinese style mind body (tai chi) and stretching exercises on cognitive function in subjects at risk of progressive cognitive decline. Int J Geriatr Psychiatry. (2011) 26:733–40. doi: 10.1002/gps.2602
45. Lam, LCW, Chan, WM, Kwok, TCY, and Chiu, HFK. Effectiveness of tai chi in maintenance of cognitive and functional abilities in mild cognitive impairment: a randomised controlled trial. Hong Kong Med J. (2014) 20:S20–3. Available from: https://www.hkmj.org/abstracts/v20n7s2/20.htm
46. Siu, MY, and Lee, DTF. Effects of tai chi on cognition and instrumental activities of daily living in community dwelling older people with mild cognitive impairment. BMC Geriatr. (2018) 18:37. doi: 10.1186/s12877-018-0720-8
47. Cai, J, and Zhang, Z. The effect of continuous fitness qigong exercise on mild cognitive impairment in the elderly. J Baicheng Normal Univ. (2018) 32:59–63. Available from: https://kns.cnki.net/kcms/detail/detail.aspx?dbcode=CJFD&filename=BCSD201803015
48. Zheng, X, Yu, J, Tu, R, Sun, S, Sun, H, and Wang, X. Rehabilitation of "six healing sounds" on MCI of the old-aged persons. Int J Tradition Chin Med. (2013) 35:968–72. Available from: https://kns.cnki.net/kcms/detail/detail.aspx?dbcode=CJFD&filename=ZGZY201307032
49. Higgins, JPT, Li, T, and Deeks, JJ. Choosing effect measures and computing estimates of effect In: JPT Higgins, J Thomas, J Chandler, M Cumpston, T Li, and MJ Page, et al., eds. Cochrane Handbook for Systematic Reviews of Interventions 2nd ed. Chichester, UK: John Wiley & Sons; (2019) 143–176.
50. Fazel, S, Bains, P, and Doll, H. Substance abuse and dependence in prisoners: a systematic review. Addiction. (Abingdon, England). (2006) 101:181–91. doi: 10.1111/j.1360-0443.2006.01316.x
51. Song, D, Yu, D, Zhou, J, Zeng, L, and Fan, T. Effects of traditional Chinese medicine-based exercises on cognitive function in older people with mild cognitive impairment: a systematic review and meta-analysis. Geriatr Nurs. (2022) 46:98–104. doi: 10.1016/j.gerinurse.2022.05.005
52. Zheng, G, Xia, R, Zhou, W, Tao, J, and Chen, L. Aerobic exercise ameliorates cognitive function in older adults with mild cognitive impairment: a systematic review and meta-analysis of randomised controlled trials. Br J Sports Med. (2016) 50:1443–50. doi: 10.1136/bjsports-2015-095699
53. Li, L, Li, W, and Fan, T. Baduanjin exercise improves cognitive function in older adults with mild cognitive impairment: a systematic review and Meta-analysis. J Nerv Ment Dis. (2024) 212:500–6. doi: 10.1097/NMD.0000000000001796
54. Su, K, Yuan, J, Liu, H, Luo, M, Li, Q, Liu, S, et al. The comparative effectiveness of traditional Chinese medicine exercise therapies in elderly people with mild cognitive impairment: a systematic review and network Meta-analysis. Front Neurol. (2022) 13:775190. doi: 10.3389/fneur.2022.775190
55. Rampengan, DD, Gunawan, FA, Rampengan, JA, Ramadhan, RN, Iqhrammullah, M, and Yufika, A. Effectiveness of tai chi as a non-invasive intervention for mild cognitive impairment in the elderly: a comprehensive review and meta-analysis. Narra J. (2024) 4:e724. doi: 10.52225/narra.v4i1.724
Keywords: exercise therapy, cognitive functions, exercise parameters, mild cognitive impairment, Traditional Chinese Exercises
Citation: Wen Q, Luo Q, Liu Y, Li L, Białas M and Wilczyńska D (2025) Optimal exercise temporal parameters of Traditional Chinese Exercises for cognitive function of older adults with mild cognitive impairment: a systematic review and dose–response meta-analysis of randomized controlled trials. Front. Med. 12:1568835. doi: 10.3389/fmed.2025.1568835
Edited by:
Marios Kyriazis, National Gerontology Centre, CyprusReviewed by:
Yuxin Yuan, Beijing Sport University, ChinaCiobîcă Andrei, Grigore T. Popa University of Medicine and Pharmacy, Romania
Phaksachiphon Khanthong, Ubon Ratchathani Rajabhat University, Thailand
Copyright © 2025 Wen, Luo, Liu, Li, Białas and Wilczyńska. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qingpan Wen, cWluZ3Bhbi53ZW5AYXdmLmdkYS5wbA==
 Qingpan Wen
Qingpan Wen Qin Luo2
Qin Luo2 Marcin Białas
Marcin Białas Dominika Wilczyńska
Dominika Wilczyńska