- 1Korean Medicine Science Research Division, Korea Institute of Oriental Medicine, Daejeon, Republic of Korea
- 2Global Cooperation Center, Korea Institute of Oriental Medicine, Daejeon, Republic of Korea
- 3Digital Health Research Division, Korea Institute of Oriental Medicine, Daejeon, Republic of Korea
- 4Korean Medicine Convergence Research Division, Korea Institute of Oriental Medicine, Daejeon, Republic of Korea
Background: Musculoskeletal pain is a leading cause of disability and reduced quality of life worldwide. Given the growing interest in complementary and alternative therapies, acupuncture has been widely explored as a potential treatment for alleviating musculoskeletal pain. This evidence map aimed to identify, describe, and summarize the current available evidence about acupuncture interventions on musculoskeletal pain.
Methods: For this map, searches were conducted in PubMed, Embase, Cochrane Library, Allied and Complementary Medicine Database (AMED), Web of Science, and Epistemonikos to identify systematic reviews (SRs) with meta-analysis published up to 23 August 2024. Included SRs were independently assessed for eligibility in pairs. The data from the eligible SRs were extracted and evaluated for methodological quality using AMSTAR 2. The findings were tabulated and mapped using bubble plots.
Results: A total of 111 SRs fulfilled the eligibility criteria and were included in this evidence map. All of the SRs included manual acupuncture or electroacupuncture. Comparators included in SRs involved active comparators, inactive comparators, sham acupuncture, and no intervention. The included 111 SRs were categorized into 35 musculoskeletal pain conditions. The short-term effects of acupuncture showed a positive effect across most comparators in major musculoskeletal pain. All included SRs were rated low or critically low in terms of methodological quality.
Conclusion: This evidence map demonstrated that acupuncture has favorable effects on major musculoskeletal disorders. Further improvements in the quality of evidence should be prioritized and more clinical trials on the acupuncture for treating musculoskeletal pain are needed.
1 Introduction
Musculoskeletal pain is the most common symptom associated with musculoskeletal disorders affecting the bones, muscles, joints, ligaments, and tendons. This type of pain can be acute and chronic and may be localized to one area or widespread throughout the body (1). According to the Global Burden of Disease (GBD) analysis, approximately 1.71 billion individuals worldwide are living with musculoskeletal conditions (2). Musculoskeletal pain can arise from various causes, including injuries, degenerative conditions, and poor posture. Diagnosing musculoskeletal pain can be complicated and requires a thorough examination which involves reviewing medical history and performing physical examinations. Additional radiology tests such as X-rays, CT scans, and MRI may also be needed to identify the specific cause of pain (3). At present, musculoskeletal pain is treated with both pharmaceutical and non-pharmacological approaches, depending on the underlying cause. Most guidelines for the management of musculoskeletal pain mainly focus on medications, physical therapy, manual therapies, as well as lifestyle modifications (4).
Acupuncture is a form of traditional medicine involving the insertion of needles into specific points of the body to relieve various symptoms and stimulate holistic healing. Acupuncture therapy, whether used alone or in combination with other therapies like physiotherapy, has gained widespread use for treating musculoskeletal pain in many countries around the world (3). The number of published studies on this topic has been steadily increasing over the past two decades, indicating growing interest and research in this field (5, 6). A comprehensive review of alternative therapies, including acupuncture, for chronic pain management highlighted that acupuncture is a promising method for reducing chronic musculoskeletal pain (7).
An evidence map is a form of review that evaluates a broad subject to identify the current state of the evidence, knowledge gaps, and areas in need of future research, and that visualizes the findings in an easily comprehensible format (8, 9). As new evidence continues to accumulate, evidence of the effectiveness of acupuncture on musculoskeletal pain should be further explored and analyzed. Therefore, this evidence map is to identify, describe, and summarize the current available evidence about acupuncture interventions on musculoskeletal pain.
2 Methods
This evidence map was performed based on the methodology proposed by the Global Evidence Mapping (GEM) (10) and was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses–Scoping Review extension (PRISMA-ScR) (11) and Preferred Reporting Items for Overviews of Reviews including harms checklist (PRIO-harms) (12). An evidence map aims to identify, classify, and describe patterns, trends, or gaps to facilitate a more in-depth thematic understanding of prior research on a given topic (8, 9).
2.1 Literature search
Six databases were searched from inception to 18 April 2024, including PubMed, Embase, Cochrane Library, Allied and Complementary Medicine Database (AMED), Web of Science, and Epistemonikos. Searches for all databases were rerun and updated until 23 August 2024, before data synthesis to ensure we included newly published records. The search terms of keywords, subject headings, and index terms describing acupuncture and musculoskeletal pain, such as “acupuncture,” “electroacupuncture,” “musculoskeletal pain,” “carpal tunnel syndrome,” “fibromyalgia,” “low back pain,” and “osteoarthritis” among others, were included. The detailed search strategy for the PubMed database is presented in Supplementary Table 1.
2.2 Study selection
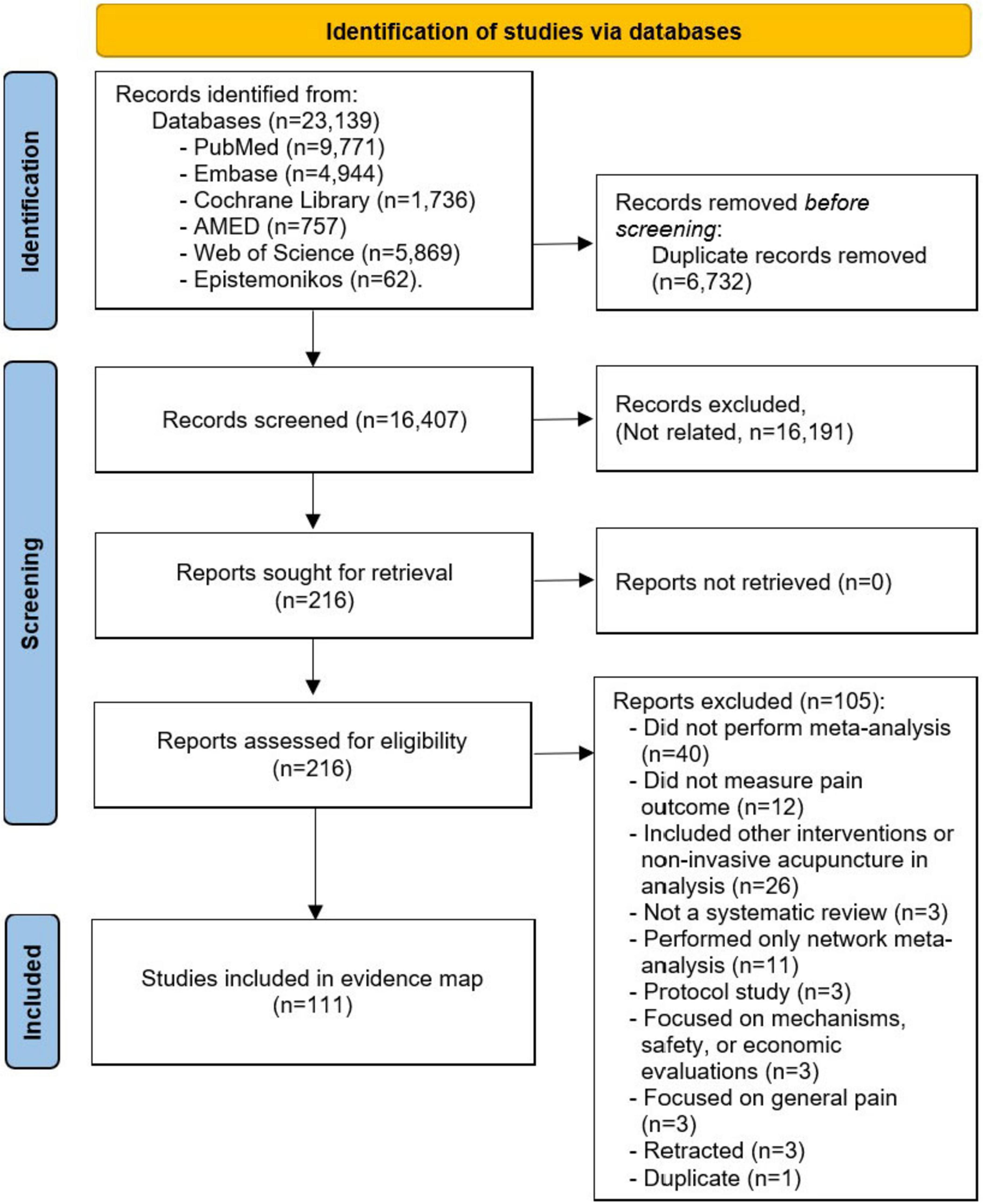
Following the search, all the identified records were uploaded to Endnote reference management software, and duplicates were removed. Two reviewers (LA and ES) independently screened the title and abstract for relevance. Full texts of the potential included systematic reviews (SRs) were then reviewed in duplicate, with any discrepancies resolved by the other reviewers (T-YC and JJ).
Studies were included if they met the following criteria: (a) participants with any musculoskeletal pain; (b) included invasive acupuncture as intervention (manual acupuncture, electro-acupuncture, and warm acupuncture); (c) where acupuncture intervention was compared with controls such as sham or placebo acupuncture, no treatment, or another intervention (pharmacological and non-pharmacological); (d) assessed at least one pain outcome measured by validated scales such as visual analog scale (VAS) or numeric rating scale (NRS); and (e) published SRs with meta-analysis. Systematic reviews that covered other interventions were still considered if results for acupuncture were reported separately. Network meta-analysis reviews were also eligible if results for meta-analysis of pain outcomes were reported separately.
Exclusion criteria for this map included (a) studies focused on general chronic or acute pain; (b) only healthy participants; (c) studies involving non-invasive acupuncture as one of the interventions (acupressure, laser acupuncture, or auriculotherapy), dry needling – acupuncture at a local point instead of standard acupoints, or additional elements such as bee venom, pharmacopuncture; (d) studies involving non-acupuncture-related interventions (cupping, herbal medicine, etc.); (e) studies that did not measure pain outcome; (f) SRs without meta-analysis; and (g) preprints and conference abstracts. Reasons for the exclusion of potential included SRs were recorded and reported, with any discrepancies resolved by additional reviewers (T-YC and JJ).
2.3 Data collection
Data extraction was performed by two independent reviewers in pairs (T-YC and JJ). All data extracted were further checked by another reviewer (ES). Data extracted included intervention characteristics, type of musculoskeletal disorders, comparators types, number of articles in a review, and impact of intervention. For acupuncture interventions, the acupuncture types were extracted based on the original authors’ report. When SRs that included specific acupuncture such as manual acupuncture, electro-acupuncture, and warm acupuncture, we report the type of acupuncture as reported by the authors. When the SRs are reported simply as acupuncture as they included several types of acupunctures, we did not reclassify and referred to them as acupuncture as well. The impact of the intervention is reported in accordance with the findings of the meta-analysis.
2.4 Quality assessment
The quality of the included SRs was evaluated by two independent reviewers (LA and BL) using the AMSTAR 2 tool (13), with any discrepancies resolved by the other reviewer (ML). AMSTAR 2 contains 16 items with 7 key items. The overall quality of SRs is divided into four levels: high – no or one non-key item unavailable; moderate – more than one non-key item unavailable; low – one key item unavailable; and critically low – more than one key item unavailable.
2.5 Data synthesis
The identified SRs were grouped into five major musculoskeletal conditions and the residual musculoskeletal conditions were categorized as other conditions. Musculoskeletal conditions were only eligible for comparative effectiveness analysis if at least three SRs were available for the musculoskeletal conditions. Based on post-intervention time measurements of pain outcome, the impact of acupuncture is categorized as short-term when the outcome is measured within 3 months post-intervention and long-term when the outcome is measured after 3 months post-intervention. Extracted data were tabulated and summarized in the form of an evidence map.
2.6 Evidence mapping
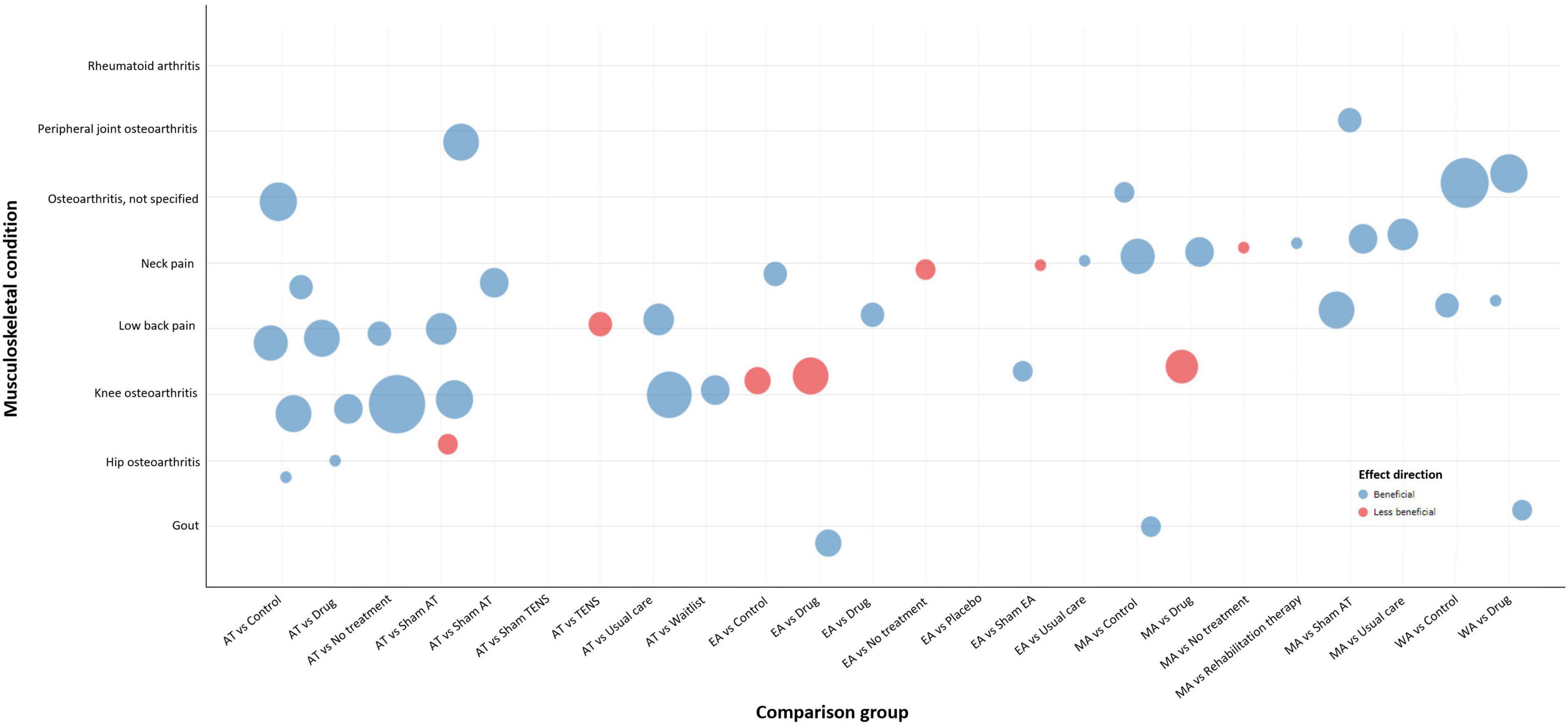
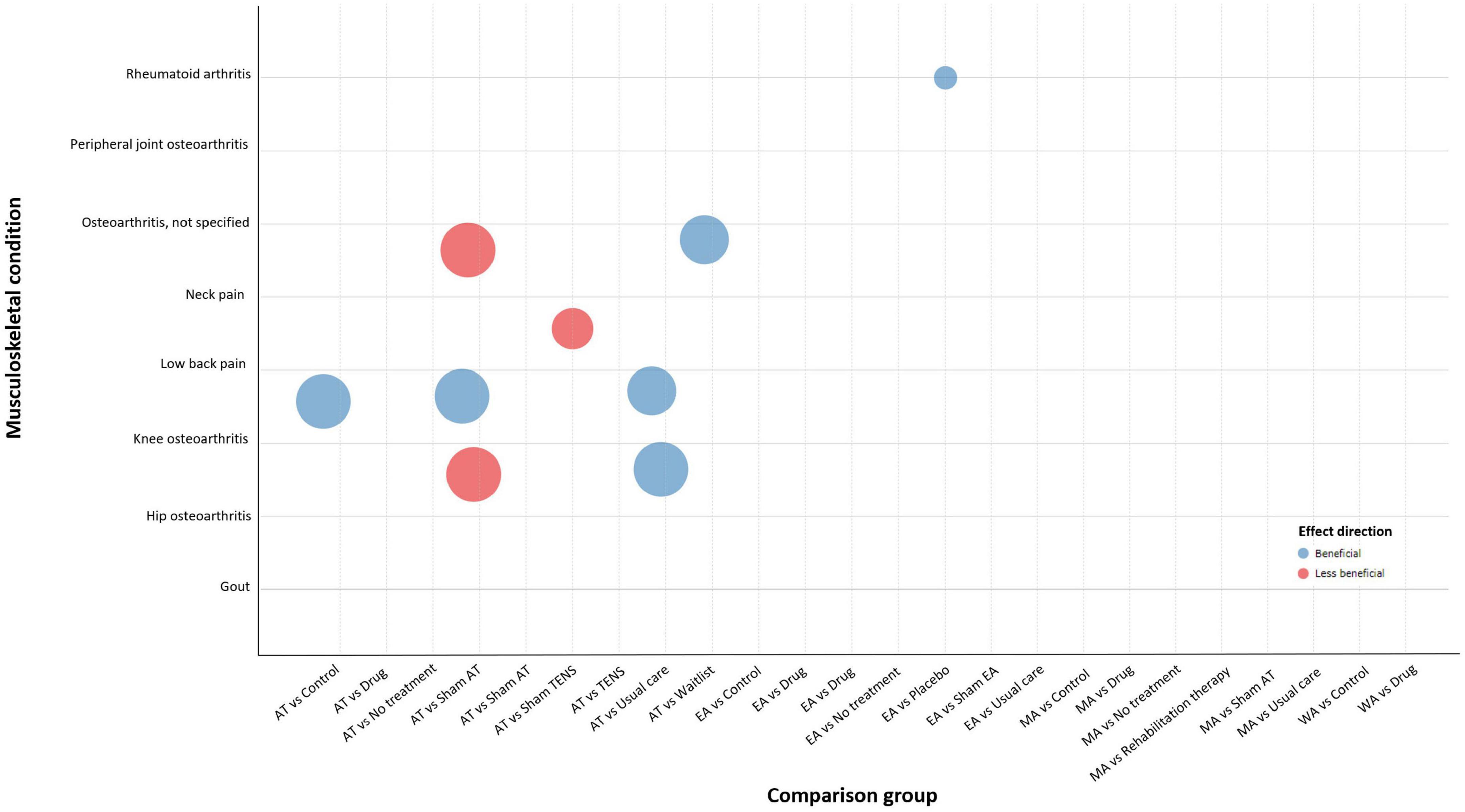
Bubble plots were used to depict multidimensional information including:
(a) X-axis – acupuncture relative to comparison treatment. The x-axis shows the different types of comparison treatments for major musculoskeletal conditions.
(b) Y-axis – major musculoskeletal conditions. The y-axis shows the specific topic of the major musculoskeletal conditions when available.
(c) Bubble color – effect of acupuncture. Each musculoskeletal condition is plotted in either beneficial or less beneficial for the effect of acupuncture based on meta-analysis findings.
(d) Bubble size – number of included SRs. Each bubble size is proportional to the number of SRs evaluating the pain outcomes associated with acupuncture intervention.
Each condition (y-axis) is presented in the form of color (effect of intervention) and size (research volume) across different comparators (x-axis).
3 Results
3.1 Study screening
The search identified 16,407 records after duplicates were removed. After reviewing the titles and abstracts, 216 full-text articles were further reviewed for potential inclusion. A total of 111 SRs fulfilled the eligibility criteria and were included in this evidence map. The list of the 105 excluded studies and reasons for exclusion are available in Supplementary Table 2. A flowchart outlining the process of the study selection is detailed in Figure 1.
3.2 Study characteristics
Systematic reviews included in this evidence map were published from 1998 to 2024, with the majority published within the last 4 years (64/111, 57.66%). The highest number of SRs originated from China (72/111, 64.9%), followed by South Korea (15/111, 13.5%). Other countries included United States (5/111, 4.5%), United Kingdom (5/111, 4.5%), Canada (4/111, 3.6%), Spain (3/111, 2.7%), Taiwan (3/111, 2.7%), Australia (2/111, 1.8%), Germany (1/111, 0.9%), and Netherlands (1/111, 0.9%).
The number of primary studies included in the SRs ranged from 2 to 77, with a total of 1,776 studies. Twenty-six SRs included less than 10 studies, 64 SRs included 10–20 studies, 9 SRs included 20–30 studies, 8 SRs included 30–40 studies, and 4 SRs included 50 or more studies. The sample size ranged from 84 to 9,650. All of the SRs included RCTs except for one SR which included case-controlled trials. Most of the SRs were non-Cochrane reviews and 8 of the SRs were Cochrane reviews.
All of the SRs included manual acupuncture or electroacupuncture. Seventy-five SRs included more than one type of acupuncture, 16 SRs included all types of acupuncture, 7 SRs included only electroacupuncture, and 13 SRs included only manual acupuncture. Comparators included in SRs involved active comparators, inactive comparators, sham acupuncture, and no intervention. Only 15 SRs reported on the diagnostic criteria for the musculoskeletal conditions included. All SRs employed VAS or NRI as pain outcome measurement. In addition, 69 SRs (62.2%) assessed adverse events and no major adverse events were reported. Forty-two SRs (37.8%) did not report adverse events or relevant data.
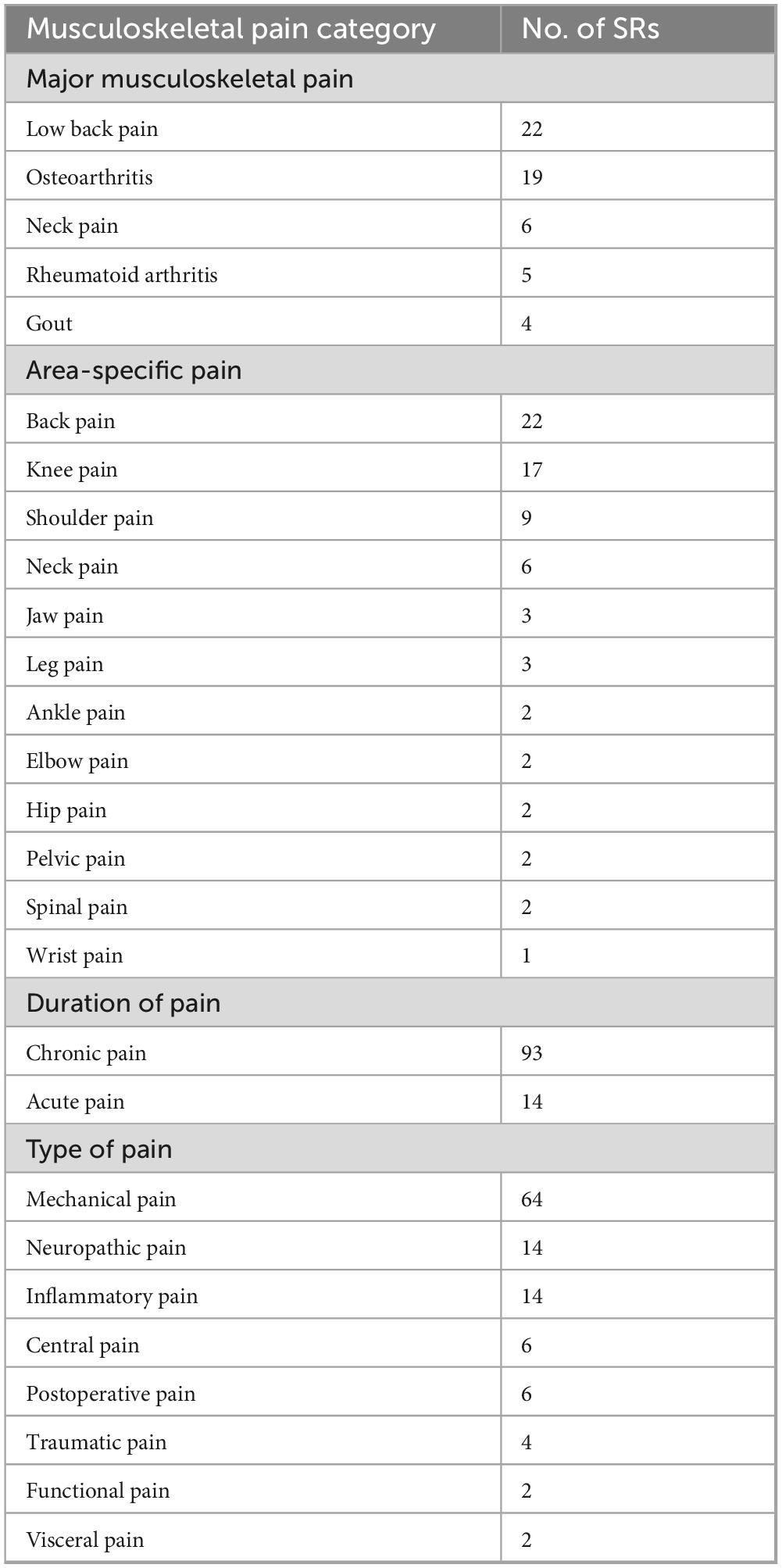
The included 111 SRs were categorized into 35 musculoskeletal pain conditions which were further categorized into major musculoskeletal disorders (56/111, 50.5%) and other musculoskeletal disorders (55/111, 49.5%). Major musculoskeletal disorders are categorized according to the Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) (14) which includes low back pain (n = 22), osteoarthritis (n = 19), neck pain (n = 6), rheumatoid arthritis (n = 5), and gout (n = 4) (Table 1).
Aside from five specific musculoskeletal condition categories, the residual musculoskeletal disorders of a wide range of acute and chronic conditions are categorized as the sixth category of other musculoskeletal disorders (14). Other musculoskeletal pain in this evidence map includes fibromyalgia (n = 6), chemotherapy-induced peripheral neuropathy (n = 3), osteoporosis (n = 3), postoperative knee arthroplasty (n = 3), sciatica (n = 3), temporomandibular disorders (n = 3), aromatase inhibitor-related arthralgia (n = 2), chronic knee pain (n = 2), chronic pelvic pain (n = 2), chronic spinal pain (n = 2), frozen shoulder (n = 2), lateral epicondylalgia (n = 2), injury-related pain (n = 2), postoperative acute orthopedic pain (n = 2), post-stroke shoulder pain (n = 2), post-stroke shoulder-hand syndrome (n = 2), acute ankle sprains (n = 1), carpal tunnel syndrome (n = 1), chronic ankle instability (n = 1), delayed-onset muscle soreness (n = 1), diabetic neuropathic pain (n = 1), fracture-related pain (n = 1), hip pain (n = 1), myofascial pain syndrome (n = 1), neuropathic pain (n = 1), diabetic peripheral neuropathy (n = 1), postoperative pain of lumbar disc herniation (n = 1), rotator cuff diseases (n = 1), shoulder adhesive capsulitis (n = 1), and shoulder pain (n = 1).
The included musculoskeletal pain conditions were further categorized into area-specific pains: back pain (22/111, 19.8%), knee pain (17/111, 15.3%), shoulder pain (9/111, 8.1%), neck pain (6/111, 5.4%), jaw pain (3/111, 2.7%), leg pain (3/111, 2.7%), ankle pain (2/111, 1.8%), elbow pain (2/111, 1.8%), hip pain (2/111, 1.8%), pelvic pain (2/111, 1.8%), spinal pain (2/111, 1.8%), and wrist pain (1/111, 0.9%).
In terms of pain duration, chronic pain was predominant (70/111, 63.1%), while acute pain was less common (41/111, 36.9%). The most prevalent pain type was mechanical (51/111, 45.7%), followed by neuropathic and inflammatory pain (11/111, 10.2% each), postoperative pain (5/111, 4.5%), traumatic pain (3/111, 2.7%), functional pain (2/111, 1.8%), visceral pain (2/111, 1.8%), and central pain (5/111, 4.5%). Details of the musculoskeletal conditions’ categorization are provided in Supplementary Tables 3, 4.
3.3 Impact of acupuncture intervention
The short- and long-term effects of acupuncture on pain outcomes were evaluated across the five major musculoskeletal conditions. Effect directions of each comparison group for acupuncture were reported when available to provide an overall picture of the intervention effects across available evidence. In Table 2, the effect of acupuncture for each major musculoskeletal is listed as either beneficial or less beneficial based on meta-analysis findings. The effect of acupuncture for all included musculoskeletal is listed in Supplementary Table 5.
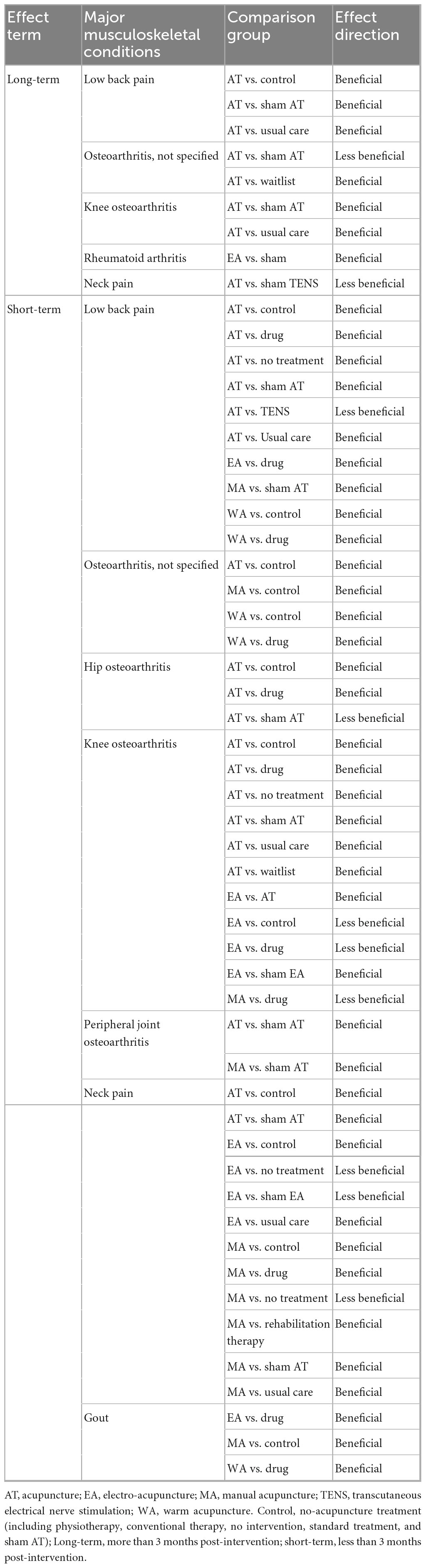
Table 2. Effectiveness of acupuncture for major musculoskeletal conditions across comparison groups.
3.3.1 Short-term effects of acupuncture
As shown in Table 2, the effects of acupuncture show a positive effect across most comparators in major musculoskeletal pain. For low back pain, the included SRs showed a positive effect of acupuncture compared to sham, usual care, drug, and no treatment, but showed an equivalent effect compared to transcutaneous electrical nerve stimulation (TENS) intervention. For osteoarthritis, the comparative effectiveness of acupuncture with no-acupuncture controls showed positive effects in the overall analysis. Yet, it is noted that acupuncture compared to sham for hip osteoarthritis, and electro-acupuncture or manual acupuncture compared to drug for knee osteoarthritis, showed statistically non-significant results. For neck pain, the included SRs reported that acupuncture was more effective than most no-acupuncture controls, but electro-acupuncture was no more effective than no treatment or sham, and similar findings for manual acupuncture compared to no treatment. In the treatment of gouty arthritis, included SRs showed that acupuncture was superior to no-acupuncture controls.
3.3.2 Long-term effects of acupuncture
Based on the findings of meta-analysis, the included SRs showed a positive effect of acupuncture for the treatment of low back pain. For osteoarthritis, it is noted that acupuncture compared to sham showed no better effect but showed a positive effect as compared to other no-acupuncture controls. In the treatment of neck pain, acupuncture compared to sham TENS tended toward an equivalent effect.
3.4 Evidence maps
The bubble plot summarizes the results for distinct major musculoskeletal conditions relevant to the pain outcome. The bubble plot depicts the treatment effect of acupuncture compared to various active and inactive controls and the estimated research volume based on the number of published SRs. Figure 2 shows the results of short-term acupuncture effect on musculoskeletal pain, and Figure 3 shows the results of long-term acupuncture effect on musculoskeletal pain. Two bubble plots with four depicted dimensions provide a broad visual overview of the evidence.
3.5 Methodological quality of SRs
According to AMSTAR 2, 23 SRs were rated “low,” and 88 SRs were rated “critically low.” The least often met criteria were Items 2, 7, and 10. None of the studies (0.0%) fully met the criteria for Item 4. The main reason for the downgrading in Item 4 was the inclusion of content experts in the field for the search strategy used, which was not reported by any of the included SRs. Yet, 81.1% of the included SRs managed to partially meet the criteria Item 2. 93.7% of SRs did not report on the sources of funding in primary studies (Item 10) and 87.4% of SRs did not report the list of excluded studies with reasons for exclusion (Item 7). The details of the AMSTAR 2 scoring were listed in Supplementary Table 6.
4 Discussion
4.1 Overview of findings
This evidence map included 111 SRs across 2 major musculoskeletal disorder categories and 35 musculoskeletal pain conditions. The most frequently studied musculoskeletal pain was low back pain followed by osteoarthritis. Most meta-analysis findings for major musculoskeletal disorders have shown that acupuncture treatments are beneficial for pain conditions and there was no adverse event evidence showing that acupuncture was least safe. Despite the promising effect, the methodological quality of the included SRs was modest and required further research.
4.2 Area of major gaps in findings
The available evidence compiled in this map shows that acupuncture has short-term benefits in relieving pain for musculoskeletal conditions. However, there was a lack of evidence for the long-term effectiveness of acupuncture in treating musculoskeletal pain. Acupuncture treatment periods are generally 4, 8, and 12 weeks (15), and many trials do not have follow-ups to evaluate the long-term effects. Therefore, the evidence is insufficient to support the use of acupuncture for improving pain symptoms for musculoskeletal conditions in the long-term.
Another gap identified was the research volume for other musculoskeletal conditions. Besides the major musculoskeletal conditions identified as the GBD (14), there are relatively less evidence to demonstrate the benefits of acupuncture on other musculoskeletal pain such as carpal tunnel syndrome, shoulder pain and hip pain among others.
4.3 Implications for practice and research
Despite the available evidence on acupuncture in treating musculoskeletal pain, most SRs conclude that the evidence is uncertain and warrant more researches to be conducted. Therefore, researchers should prioritize the quality of trials and investigate on topic areas where evidence is still limited. There is a need for more high-quality evidence for health professionals to utilize and recommend the use of acupuncture, and for patients to have confidence in the benefit of acupuncture for their musculoskeletal conditions.
Also, the researchers should avoid producing similar SRs to prevent research waste. In recent years, the number of SRs has increased overwhelmingly (16). There are as many SRs as clinical trials since conducting a clinical trial involves many barriers, such as funding, time-consuming, human capacity, patient recruitment, and ethical issues (17–19). Yet, evidence from SRs are highly dependent on the included primary studies (20–22). Therefore, the research focus should be on increasing the SR evidence quality by improving the quality of clinical trials to address the insufficient high-quality evidence.
In addition, this evidence map highlights the geographic concentration of acupuncture research in Asia, limiting the generalizability of findings. While acupuncture is a global modality, the preponderance of studies from this region reflects local practices. Future research should prioritize geographic diversity to enhance the global applicability of acupuncture and support evidence-based practice.
4.4 Limitations
This study has limitations. The first limitation of the evidence map is that we may not have identified all available evidence due to the limited database search. The second limitation is that we did not evaluate the quality or overlapping of primary studies in the included SRs. In this evidence map, we took the meta-analysis findings of the authors of SRs as it is in determining the effect direction of acupuncture. The third limitation is that the definition of control varies from studies to studies. Some SRs did not define control and this somehow limits us to compare the benefits of acupuncture over certain control.
5 Conclusion
This evidence map showed that acupuncture has beneficial effects on musculoskeletal pain, especially for major musculoskeletal disorders. The quality of evidence was concerning and future researches should focus on increasing the quality of clinical trials.
Authors contributions
LA: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Writing – original draft, Writing – review and editing. ES: Conceptualization, Formal Analysis, Investigation, Methodology, Writing – original draft, Writing – review and editing. T-YC: Investigation, Methodology, Writing – review and editing. JJ: Investigation, Methodology, Writing – review and editing. BL: Investigation, Methodology, Writing – review and editing. MY: Data curation, Formal Analysis, Visualization, Writing – review and editing. HL: Methodology, Resources, Writing – review and editing. ML: Conceptualization, Funding acquisition, Methodology, Resources, Supervision, Writing – review and editing.
Data availability statement
The original contributions presented in this study are included in this article/Supplementary material, further inquiries can be directed to the corresponding author.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by Korea Institute of Oriental Medicine (KSN20234114 and KSN2122211).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2025.1575226/full#supplementary-material
References
1. El-Tallawy S, Nalamasu R, Salem G, LeQuang J, Pergolizzi J, Christo P. Management of musculoskeletal pain: an update with emphasis on chronic musculoskeletal pain. Pain Ther. (2021) 10:181–209. doi: 10.1007/s40122-021-00235-2
2. Cieza A, Causey K, Kamenov K, Hanson S, Chatterji S, Vos T. Global estimates of the need for rehabilitation based on the global burden of disease Study 2019: a systematic analysis for the global burden of disease study 2019. Lancet. (2021) 396:2006–17. doi: 10.1016/s0140-6736(20)32340-0
3. de Sire A, Ferraro E, Leigheb M. Advance in the diagnostics and management of musculoskeletal diseases. Diagnostics. (2022) 12:1588. doi: 10.3390/diagnostics12071588
4. Ernstzen D, Louw Q, Hillier S. Clinical practice guidelines for the management of chronic musculoskeletal pain in primary healthcare: a systematic review. Implement Sci. (2017) 12:1. doi: 10.1186/s13012-016-0533-0
5. Mao Q, Huang B, Zhu D, Wang Y, Xu S, Wu D, et al. A bibliometric analysis of acupuncture therapy in the treatment of musculoskeletal pain from 2003 to 2022. J Pain Res. (2023) 16:3853–70. doi: 10.2147/jpr.S431689
6. Ang L, Song E, Jong M, Alræk T, Wider B, Choi T, et al. An evidence map on traditional medicine across health outcomes. Integr Med Res. (2024) 13:101070. doi: 10.1016/j.imr.2024.101070
7. Urits I, Schwartz R, Orhurhu V, Maganty N, Reilly B, Patel P, et al. A comprehensive review of alternative therapies for the management of chronic pain patients: acupuncture, tai chi, osteopathic manipulative medicine, and chiropractic care. Adv Ther. (2021) 38:76–89. doi: 10.1007/s12325-020-01554-0
8. Miake-Lye I, Hempel S, Shanman R, Shekelle P. What is an evidence map? A systematic review of published evidence maps and their definitions, methods, and products. Syst Rev. (2016) 5:28. doi: 10.1186/s13643-016-0204-x
9. Schuller-Martínez B, Meza N, Pérez-Bracchiglione J, Franco J, Loezar C, Madrid E. Graphical representation of the body of the evidence: the essentials for understanding the evidence gap map approach. Medwave. (2021) 21:e8164. doi: 10.5867/medwave.2021.03.8164
10. Bragge P, Clavisi O, Turner T, Tavender E, Collie A, Gruen R. The global evidence mapping initiative: scoping research in broad topic areas. BMC Med Res Methodol. (2011) 11:92. doi: 10.1186/1471-2288-11-92
11. Tricco A, Lillie E, Zarin W, O’Brien K, Colquhoun H, Levac D, et al. Prisma extension for scoping reviews (Prisma-Scr): checklist and explanation. Ann Intern Med. (2018) 169:467–73. doi: 10.7326/m18-0850
12. Bougioukas K, Liakos A, Tsapas A, Ntzani E, Haidich A. Preferred reporting items for overviews of systematic reviews including harms checklist: a pilot tool to be used for balanced reporting of benefits and harms. J Clin Epidemiol. (2018) 93:9–24. doi: 10.1016/j.jclinepi.2017.10.002
13. Shea B, Reeves B, Wells G, Thuku M, Hamel C, Moran J, et al. Amstar 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. (2017) 358:j4008. doi: 10.1136/bmj.j4008
14. GBD 2021 Other Musculoskeletal Disorders Collaborators. Global, regional, and national burden of other musculoskeletal disorders, 1990–2020, and projections to 2050: a systematic analysis of the global burden of disease study 2021. Lancet Rheumatol. (2023) 5:e670–82. doi: 10.1016/s2665-9913(23)00232-1
15. Ma S. Establishing an adequate dose of acupuncture is essential for clinical trial studies. Clin Res Trials. (2020) 6:1000295. doi: 10.15761/crt.1000295
16. Bastian H, Glasziou P, Chalmers I. Seventy-five trials and eleven systematic reviews a day: how will we ever keep up? PLoS Med. (2010) 7:e1000326. doi: 10.1371/journal.pmed.1000326
17. Djurisic S, Rath A, Gaber S, Garattini S, Bertele V, Ngwabyt S, et al. Barriers to the conduct of randomised clinical trials within all disease areas. Trials. (2017) 18:360. doi: 10.1186/s13063-017-2099-9
18. Alemayehu C, Mitchell G, Nikles J. Barriers for conducting clinical trials in developing countries- a systematic review. Int J Equity Health. (2018) 17:37. doi: 10.1186/s12939-018-0748-6
19. Ebrahimi H, Megally S, Plotkin E, Shivakumar L, Salgia N, Zengin Z, et al. Barriers to clinical trial implementation among community care centers. JAMA Netw Open. (2024) 7:e248739. doi: 10.1001/jamanetworkopen.2024.8739
20. Khan K, Daya S, Jadad A. The importance of quality of primary studies in producing unbiased systematic reviews. Arch Intern Med. (1996) 156:661–6. doi: 10.1001/archinte.1996.00440060089011
21. Hopewell S, Boutron I, Altman D, Ravaud P. Incorporation of assessments of risk of bias of primary studies in systematic reviews of randomised trials: a cross-sectional study. BMJ Open. (2013) 3:e003342. doi: 10.1136/bmjopen-2013-003342
Keywords: evidence map, systematic review, overview, acupuncture, musculoskeletal pain
Citation: Ang L, Song E, Choi T-Y, Jun JH, Lee B, Yim MH, Lee HW and Lee MS (2025) Effects of acupuncture on musculoskeletal pain: an evidence map. Front. Med. 12:1575226. doi: 10.3389/fmed.2025.1575226
Received: 12 February 2025; Accepted: 23 July 2025;
Published: 11 August 2025.
Edited by:
Pathirage Kamal Perera, University of Colombo, Sri LankaReviewed by:
Lamine Mahi, Axelys Santé, FranceRiccardo Rustichelli, Center for Studies on Natural and Physical Therapies (CSTNF), Italy
Copyright © 2025 Ang, Song, Choi, Jun, Lee, Yim, Lee and Lee. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Myeong Soo Lee, ZHJtc2xlZUBnbWFpbC5jb20=
 Lin Ang
Lin Ang Eunhye Song
Eunhye Song Tae-Young Choi
Tae-Young Choi Ji Hee Jun
Ji Hee Jun Boram Lee
Boram Lee Mi Hong Yim
Mi Hong Yim Hye Won Lee
Hye Won Lee Myeong Soo Lee
Myeong Soo Lee