- 1School of Public Health, Lanzhou University, Lanzhou, Gansu, China
- 2Department of Public Health and Hospital Infection Management, Hospital of Northwest Minzu University (Second People’s Hospital of Gansu Province), Lanzhou, Gansu, China
- 3School of Public Health, Gansu University of Chinese Medicine, Lanzhou, Gansu, China
Introduction: Ventilator-associated pneumonia (VAP) is a common and life-threatening complication in ICU patients, with its occurrence closely related to ICU nurses’ knowledge, attitudes, and practices. This study aimed to investigate the current status and influencing factors of ICU nurses’ knowledge, attitudes, and practices regarding VAP prevention in Gansu Province, and to provide a basis for improving the effectiveness of VAP prevention.
Methods: A stratified random sampling method was used to select 600 ICU nurses from 24 hospitals in Gansu Province as study participants. Data related to VAP prevention among the nurses were collected through a questionnaire survey and statistically analyzed using SPSS 26.0.
Results: The overall score of nurses on VAP prevention was 113.92 ± 8.472, with the lowest score in the knowledge dimension (7.66 ± 1.200) and higher scores in the attitude (28.67 ± 3.528) and practice (77.59 ± 5.839) dimensions. Factors such as region, ICU type, number of training sessions, and years of work experience significantly affected VAP prevention knowledge, attitudes, and practices. The knowledge scores of nurses in the Lanzhou and Zhangye regions were significantly higher than those in other regions, and nurses in comprehensive ICUs had higher VAP knowledge scores. Additionally, nurses who participated in four or more VAP prevention training sessions had significantly higher scores in all dimensions compared to those with fewer training sessions. A significant positive correlation was found between knowledge, attitudes, and practices related to VAP prevention.
Conclusion: ICU nurses in Gansu Province performed better in the attitudes and practices of VAP prevention, but there is still room for improvement in their knowledge. Regional differences, ICU type, and the number of training sessions are important factors influencing VAP prevention and control abilities. The study suggests that enhanced training in VAP prevention and control knowledge can help improve nurses’ attitudes and practical skills. To improve the effectiveness of VAP prevention, hospitals should focus on strengthening training in areas with weaker knowledge and increasing the frequency of training sessions.
1 Introduction
Ventilator-associated pneumonia (VAP) is a type of pneumonia that occurs in patients with tracheal intubation or tracheotomy after receiving mechanical ventilation for more than 48 h (1). VAP is a common complication in intensive care unit (ICU) patients, leading not only to prolonged hospital stays and increased treatment costs, but, more importantly, it can worsen the patient’s condition and even become life-threatening (2–5).
In recent years, with the increasing number of patients in intensive care units (ICUs) and the widespread use of ventilators, ventilator-associated pneumonia (VAP) has become an urgent challenge facing the global medical community. The incidence of VAP varies by region, with significantly higher rates in middle- and low-income countries compared to high-income countries (6, 7). For example, in resource-limited regions such as Southeast Asia and developing countries, the incidence rate of adult VAP ranges from 10‰ to 41.7‰ (8). In contrast, U.S. data from 2013 showed that the incidence of VAP in ICUs was only 0.8–2.2‰ (9), while the incidence in North American hospitals was 1–2.5‰ (10). However, some regions in Europe have higher incidence rates, with the EU VAP/CAP study reporting an incidence rate of 18.3‰ (11). This disparity in data highlights the close association between healthcare standards and VAP incidence rates.
The occurrence of VAP is closely associated with multiple factors, among which the knowledge, attitudes, and practices (KAP) of healthcare workers play a crucial role in VAP prevention. International studies indicate that nurses’ performance in VAP prevention is closely related to their professional knowledge level and adherence to guidelines (12). A study in Tanzania found that nurses with higher education levels demonstrated significantly better VAP prevention practices than those with lower education levels, with primary barriers including insufficient skills, staff shortages, and lack of knowledge (13). A study in Saudi Arabia further confirmed that nurses’ educational background, work experience, and gender significantly influence the implementation of VAP prevention measures (14). Australian research has pointed out that although nurses report high compliance, there is still a significant lack of awareness of evidence-based guidelines (15).
In the clinical practice of ICUs in China, the prevention and control of VAP face a unique dilemma of “discrepancy between knowledge and action.” First, the allocation of nursing resources and operational standards have a decisive impact on the effectiveness of prevention and control. A multicenter study of 32 tertiary hospitals in Hebei Province showed that the incidence of VAP was significantly associated with nurse staffing levels and operational standards (16). Second, the issue of knowledge translation barriers is prominent (17). A cross-sectional survey in Hunan Province revealed that while nurses scored high on VAP knowledge tests, their compliance rates in clinical practice were low (18). Additionally, systemic constraints are significant. A qualitative study in China identified structural factors such as physical space limitations, inadequate technical equipment, and lack of standardized training (19), which prevent nurses from implementing standardized procedures even when they possess theoretical knowledge. Finally, the sustainability of intervention measures faces challenges (20). Furthermore, existing evidence is mostly from developed regions in the east, and there is a lack of adaptive solutions for resource-constrained regions.
This study is the first to conduct a Knowledge, Attitude, and Practice (KAP) survey on VAP among ICU nurses in Gansu Province, northwest China, aiming to assess the current status of VAP prevention KAP, identify influencing factors, and propose improvement strategies based on local medical resources. Compared to existing studies, the innovative aspects of this research include: it is the first systematic investigation of VAP prevention in underdeveloped regions of western China, and it provides targeted recommendations tailored to the characteristics of medical resources in economically underdeveloped regions, thereby providing empirical evidence for the development of regionally differentiated prevention and control strategies.
2 Materials and methods
2.1 Study population
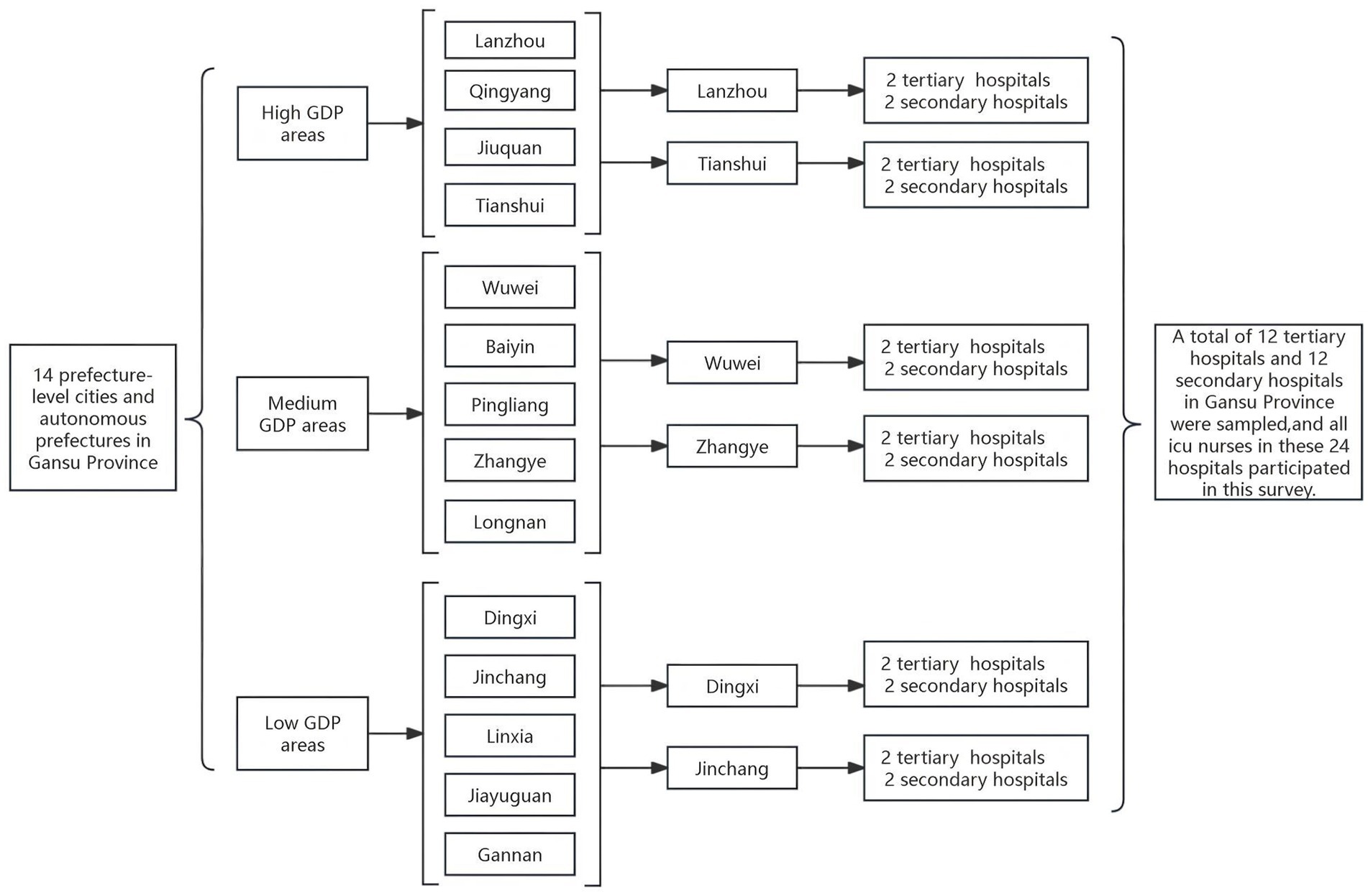
Using a combination of stratified random sampling and multi-stage sampling, a total of 14 prefecture-level administrative areas in Gansu Province, including 12 prefecture-level cities and 2 autonomous prefectures, were categorized into three groups based on the 2023 regional gross domestic product (GDP): high GDP, medium GDP, and low GDP. Two cities (or prefectures) were randomly selected from each group. In each of the six selected cities (or prefectures), two tertiary hospitals and two secondary hospitals were chosen, resulting in a total of 24 hospitals. A total of 600 ICU nurses from all 24 hospitals, sampled between January and December 2023, were selected as the study population (Figure 1).
2.2 Data collection tools
2.2.1 Questionnaire design
In this study, we referred to relevant literature and guidelines on VAP prevention both domestically and internationally, particularly the Chinese Guidelines for the Diagnosis and Treatment of Hospital-Acquired Pneumonia and Ventilator-Associated Pneumonia in Adults (2018 edition), developed by the Critical Care Medicine Branch of the Chinese Medical Association, as well as the VAP prevention guidelines issued by the Centers for Disease Control and Prevention. Based on this, we extensively reviewed relevant research materials and literature from both domestic and international sources to gain an in-depth understanding of the latest advancements and practical experience in VAP prevention. At the same time, we considered the local characteristics and realities of Gansu Province, while also taking into account China’s national conditions. To ensure the scientific validity and rationality of the questionnaire, we consulted experts in the fields of ICU nursing, infection control, nursing, and statistics, incorporating their valuable insights. Through this series of research and discussions, the questionnaire for this study was ultimately developed.
2.2.2 Composition of the questionnaire
The questionnaire for this study consisted of two parts: the first part was a general information survey of nurses, and the second part was the Knowledge, Attitude, and Practice (KAP) Questionnaire for ICU nurses to prevent VAP. The KAP Questionnaire was divided into three dimensions: knowledge, attitude, and practice, with a total of 44 items. The score range for the KAP Questionnaire was 22–120 points. The knowledge dimension contained 10 items, the attitude dimension had 6 items, and the practice dimension had 16 items. The knowledge dimension consisted of multiple-choice questions, with a score of 1 for a correct answer and 0 for an incorrect answer, giving a score range of 0–10 points. The attitude dimension was scored using a Likert 5-point scale, with the options “strongly agree,” “neutral,” “relatively agree,” “disagree,” and “strongly disagree” in descending order. The corresponding scores were 5, 4, 3, 2, and 1, respectively, resulting in a score range of 6–30 points. The practice dimension was also scored on a Likert 5-point scale, with the options “very compliant,” “basic compliant,” “basic noncompliant,” “noncompliant,” and “very noncompliant,” with scores of 5, 4, 3, 2, and 1, respectively. This dimension had a score range from 16 to 80 points.
2.2.3 Questionnaire pre-survey
This study employed a random sampling method to select 60 ICU nurses for a preliminary survey, systematically evaluating the reliability and validity indicators of the questionnaire. The reliability analysis results showed that the Cronbach’s α coefficients for the belief scale and behavior scale were 0.869 and 0.808, respectively, while the Cronbach’s α coefficient for the total scale was 0.792. All indicators exceeded the industry-recognized standard of 0.70, confirming that the questionnaire has ideal internal consistency. Validity testing results showed that the overall content validity index (CVI) of the questionnaire reached 0.91, significantly exceeding the critical requirement of 0.80; exploratory factor analysis (EFA) revealed a KMO value of 0.950, and Bartlett’s sphericity test results were significant (p < 0.05), The two extracted common factors collectively explained 75.1% of the variance, with all items having factor loadings exceeding 0.5 and no cross-factor loadings observed. Based on these measurement indicators, the questionnaire developed in this study exhibits good reliability and validity characteristics, meeting measurement requirements.
2.3 Data collection
This study was conducted in close coordination with all participating hospitals and received approval and support from hospital management. The study employed a questionnaire distribution method, targeting ICU nurses across all participating hospitals. Prior to data collection, researchers conducted departmental briefings to provide participants with detailed explanations of the study’s objectives, methods, and precautions. Each participant was given a verbal explanation, clearly informing them of the voluntary participation principle, data anonymization procedures, and the right to withdraw at any time without reason. The questionnaire survey commenced only after obtaining verbal informed consent. No personal identification information was recorded during questionnaire completion; only basic information such as department and years of service was retained. All questionnaires used an independent coding system (questionnaire IDs were completely separated from personal information) to ensure data anonymity. After collection, the questionnaires were immediately verified by researchers on-site and centrally stored. After electronic data entry, the original paper records were promptly destroyed. This study is a low-risk observational study that does not interfere with clinical diagnostic and treatment processes. The survey content solely pertains to healthcare professionals’ work practices and does not include patient privacy or sensitive information.
2.4 Statistical methods
This study utilized SPSS 26.0 software for data processing and analysis, with p < 0.05 indicating statistical significance. First, the Kolmogorov–Smirnov test was used to assess the normality of the data, with results showing p < 0.05. Given the large sample size (N = 600) and the fact that the absolute values of skewness for all variables were less than 2, the absolute values of kurtosis were less than 7, and no extreme outliers were detected, the basic conditions for parametric tests were still met. Descriptive statistical methods were used to analyze demographic characteristics, knowledge, belief, and behavior variables, calculating frequencies, proportions, means, and standard deviations. After testing, the data met the requirements for linear relationships and homogeneity of variance, so Pearson correlation analysis was used to explore the correlations between knowledge, beliefs, and behaviors related to VAP prevention among ICU nurses. Independent samples t-tests or one-way analysis of variance were used to compare differences in scores across knowledge, belief, and behavior dimensions among nurses with different demographic characteristics (e.g., age, years of experience, educational level, etc.). Finally, multiple linear regression analysis was employed to identify the primary factors influencing ICU nurses’ knowledge, beliefs, and behaviors regarding VAP prevention.
3 Results
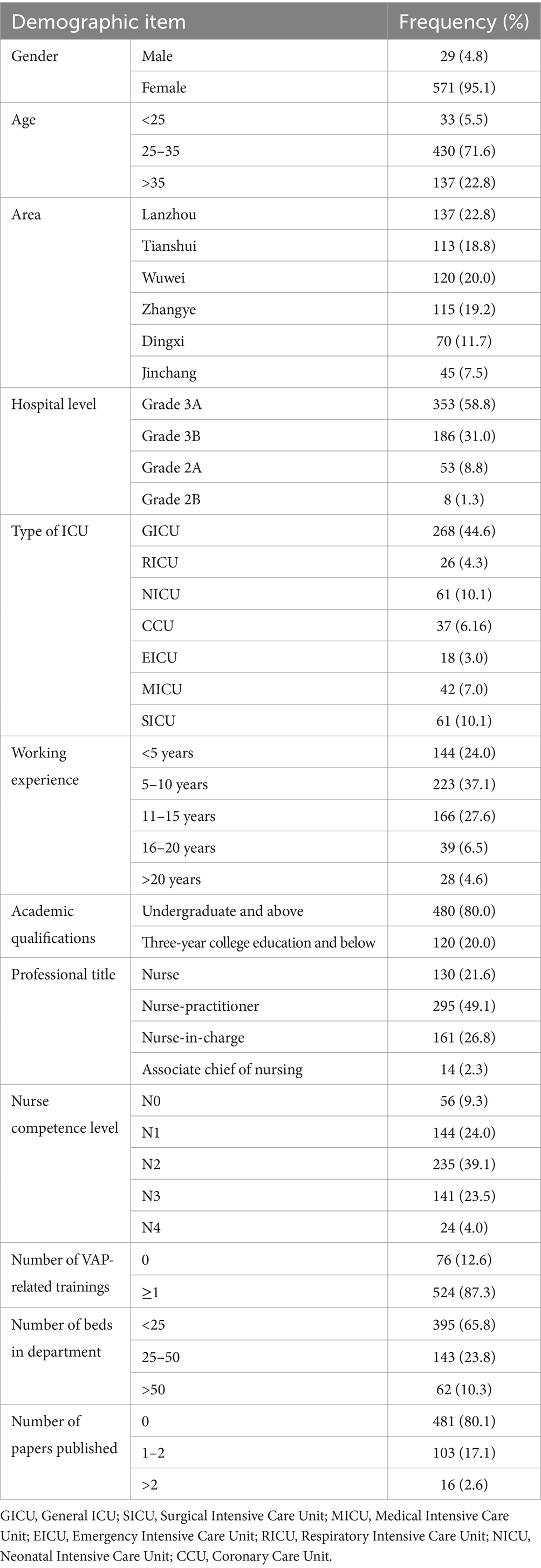
All ICU nurses in 24 hospitals agreed to participate in this study, and a total of 600 nurses completed the questionnaire. Among the participants, females accounted for the majority, 95.1%, while males accounted for only 4.8%. In terms of age distribution, 71.6% of the nurses were between 25 and 35 years old. In terms of geographical distribution, the largest number of nurses were from Lanzhou, accounting for 22.8%, while the smallest number of nurses were from Jinchang, accounting for 7.5%. In terms of hospital type, 89.8% of the nurses worked in tertiary hospitals. The most common clinical unit was general ICU, accounting for 44.6, and 76% of the nurses had more than 5 years of work experience. In terms of education, 80% of the nurses had a bachelor’s degree or higher. In addition, 87.3% of the nurses had attended at least one trainings related to VAP prevention in the past 2 years, while 80.1% of the nurses had not published any academic papers in the past 5 years. The detailed results are shown in Table 1.
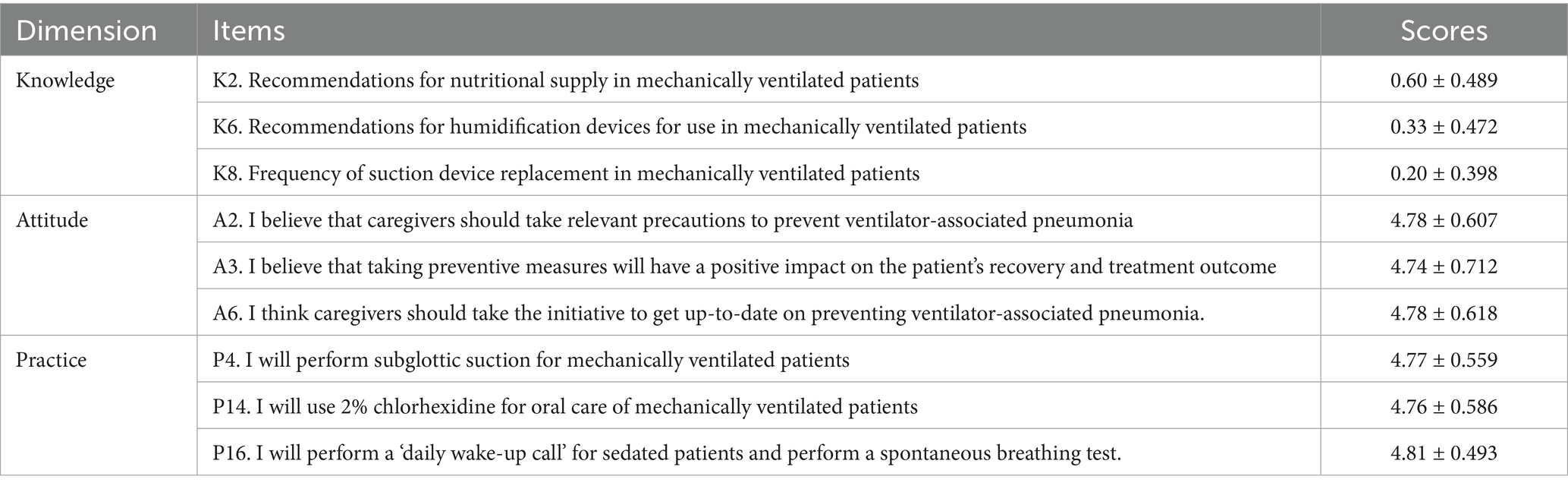
The ICU nurses’ KAP questionnaire score for preventing VAP was 113.92 ± 8.472, of which the knowledge dimension score was 7.66 ± 1.200, the attitude dimension score was 28.67 ± 3.528, and the practice dimension score was 77.59 ± 5.839. The bottom three entries of knowledge, attitude and practice dimension scores are shown in Table 2.
The results of one-way ANOVA showed (Table 3) that there was a significant relationship between knowledge level and region (p = 0.026). According to the LSD test, there were significant differences in VAP (ventilator-associated pneumonia) knowledge scores among nurses in Lanzhou, Tianshui, Wuwei, Zhangye, Dingxi, and Jinchang regions. Specifically, ICU nurses in Lanzhou had significantly higher VAP knowledge than nurses in the Wuwei (p = 0.1013) and Dingxi (p = 0.033) regions; and nurses in Zhangye had significantly higher VAP knowledge than nurses in the Wuwei (p = 0.005) and Dingxi (p = 0.016) regions. In addition, there were significant differences in the knowledge of VAP prevention among nurses in different types of ICUs (p < 0.001). According to the results of the LSD test, nurses in comprehensive ICUs had significantly higher knowledge of VAP prevention than those in RICUs (Respiratory Intensive Care Unit) (p < 0.001), NICUs (Neonatal Intensive Care Unit) (p < 0.001), CCUs (Coronary Care Unit) (p < 0.001), and EICUs (Emergency Intensive Care Unit) (p = 0.038); nurses in RICUs had significantly higher knowledge of VAP prevention than those in MICUs (Medical Intensive Care Unit) (p = 0.009) and SICUs (Surgical Intensive Care Unit) (p = 0.016); nurses in the NICU had significantly higher knowledge of VAP prophylaxis than those in the MICU (p < 0.001) and SICU (p < 0.001); and nurses in the CCU had significantly higher knowledge of VAP prophylaxis than those in the MICU (p = 0.003) and SICU (p = 0.005). Additionally, the results of the independent t-test (Table 1) showed that there was a significant difference between nurses’ mastery of VAP knowledge and the number of training sessions they had attended (p < 0.001). Nurses who had attended one VAP prevention-related training session in the past 2 years demonstrated significantly higher mastery of VAP knowledge than those who had attended zero training sessions. Finally, there was also a significant CHAYI1 between nurses’ knowledge acquisition and the number of beds in the department (p < 0.001). According to the results of the LSD test, ICU nurses with fewer than 25 beds in the unit had significantly higher knowledge of VAP prevention than nurses with 25–50 beds (p < 0.001) and those with more than 50 beds (p < 0.001).
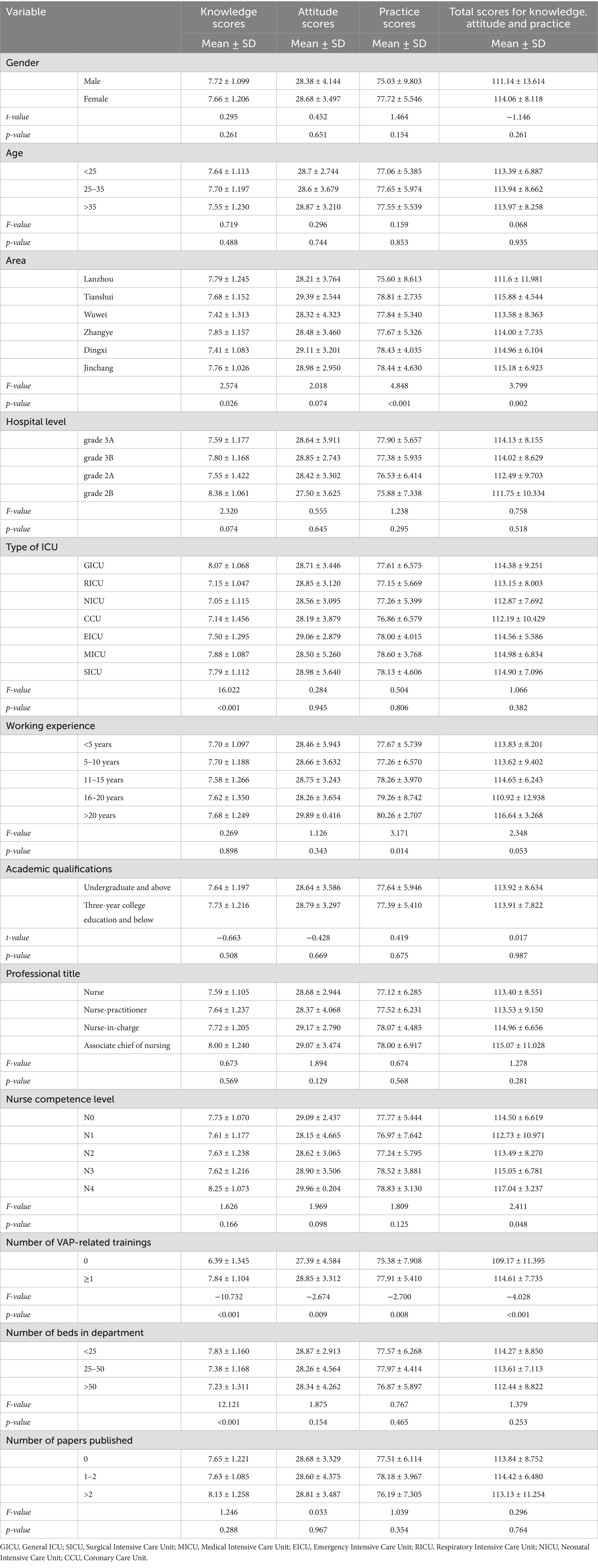
Table 3. Demographic characteristics correlation with knowledge, attitude, and practice in the area of VAP prevention (N = 600).
According to the results of the independent t-test (Table 1), there was a statistically significant difference in the beliefs of nurses with different training frequencies (p = 0.009). ICU nurses who had participated in VAP-related training more than once in the past 2 years had significantly stronger beliefs in VAP prevention than nurses who had participated zero times.
According to one-way ANOVA (Table 3), there was a significant difference in practice scores of VAP prevention among ICU nurses in different regions (p < 0.001). The practice scores of ICU nurses in VAP prevention were significantly higher in Lanzhou than in other regions. There was a significant difference in the practice scores of ICU nurses with different years of experience (p = 0.014), and the practice scores of nurses with 16–20 years of experience were all significantly lower than those of nurses with <5 years of experience (p = 0.013), 5–10 years of experience (p = 0.029), 11–15 (p = 0.002) years of experience, and >20 years of experience (p = 0.005).
The results of the independent samples t-test (Table 1) showed that the difference between the number of training sessions and the practice scores was also statistically significant (p = 0.008). ICU nurses who received one or more training sessions had significantly higher practice scores than nurses who did not receive any training.
One-way ANOVA showed (Table 3) that there was a significant difference in the total score of the questionnaire of knowing and believing in different regions (p = 0.002), with ICU nurses in Lanzhou having a significantly higher total score of the questionnaire of knowing and believing in ICU nurses than those in other regions, and the questionnaire of Tianshui having a significantly higher total score than those in Wuwei (p = 0.036). The differences between the questionnaires of nurses with different levels of competence were also statistically significant, with nurses with competence levels N3 (p = 0.021) and N4 (p = 0.021) having significantly higher total KAP questionnaire scores than nurses with competence level N1. The results of the independent t-test (Table 1) showed that there were also significant differences in the total scores of the knowledge, belief, and behavior questionnaire between nurses with different training frequencies (p < 0.001). Nurses who had received training one or more times had higher total scores than nurses who had not participated in training.
The results of the correlation between knowledge, attitude and practices related to VAP among ICU nurses are shown in Table 4. There was a significant positive correlation between knowledge and attitude (r = 0.100, p < 0.015). By increasing the knowledge scores, the attitude scores were also increased. Also, there was a significant positive correlation between knowledge and practice (r = 0.104, p < 0.011), with higher knowledge scores resulting in higher practice scores. There was also a significant positive correlation between attitude and practices (r = 0.522, p < 0.001), with higher attitude scores leading to higher practice scores.
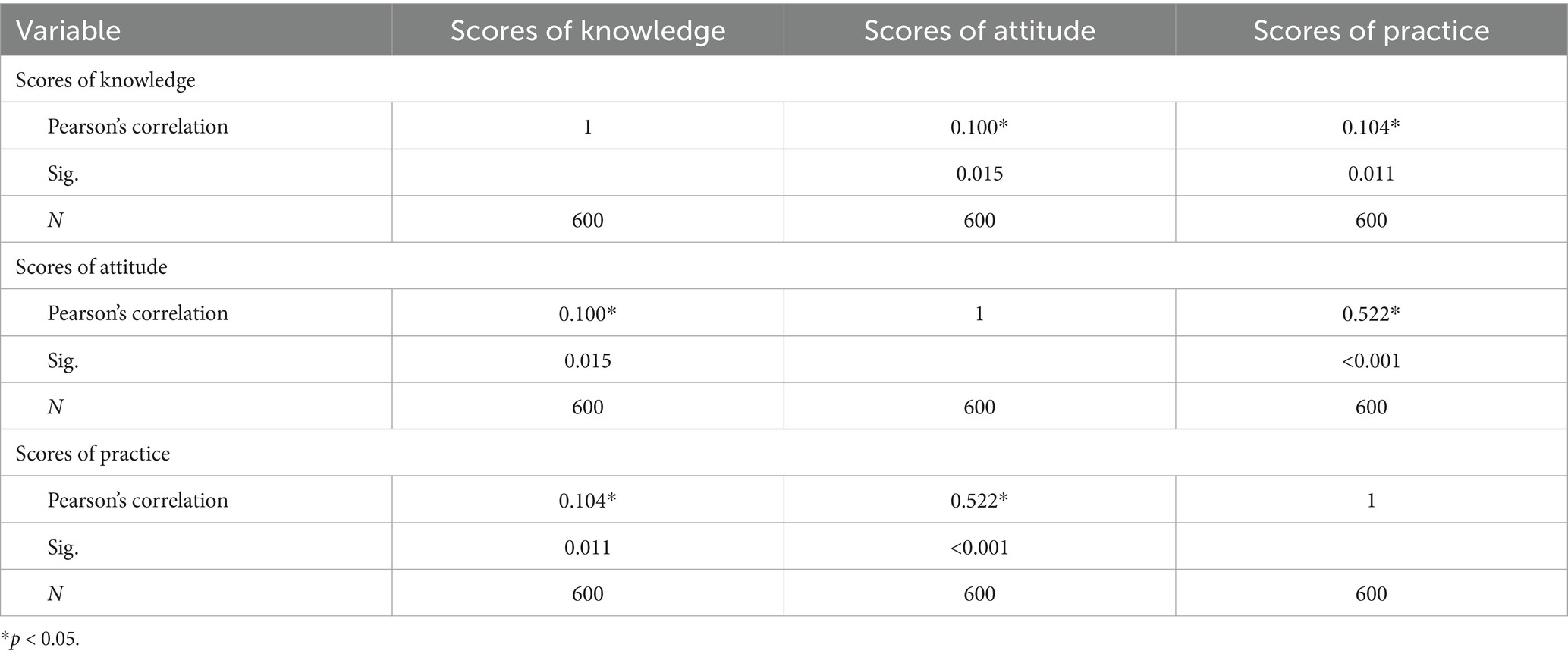
Table 4. Correlation of knowledge, attitude, and practice related to prevention VAP of nurses in ICU.
The results showed that the number of trainings and region were the influencing factors of ICU nurses’ knowledge and practice in this study. The number of trainings was also an influential factor in the total score of nurses’ attitude and KAP questionnaire (Table 5).
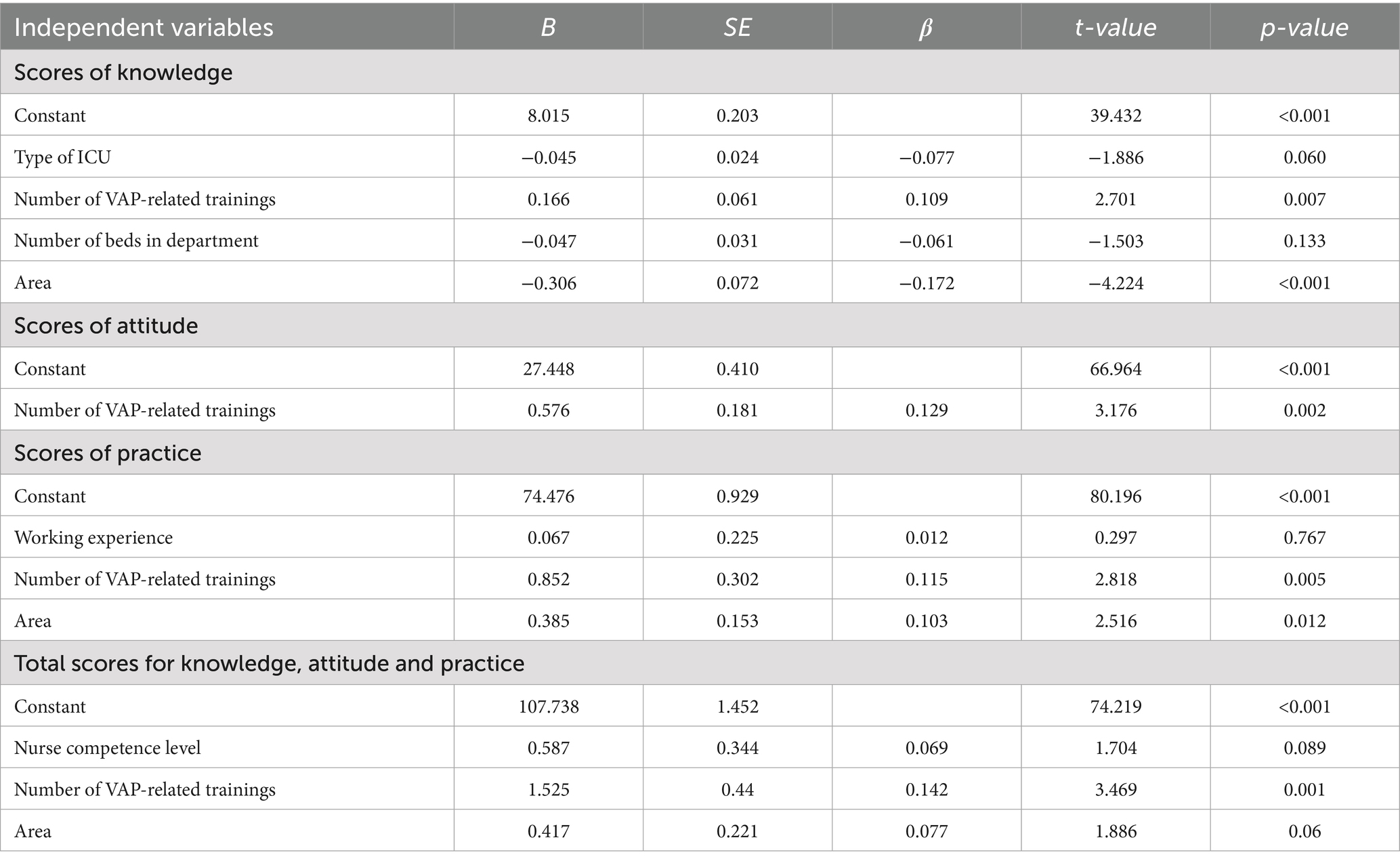
Table 5. Multiple linear regression analysis of ICU nurses’ total scores on nursing knowledge, attitude, practices, and knowledge, attitude and practices regarding VAP prevention (N = 600).
4 Discussion
According to the results of this study, ICU nurses demonstrated relatively insufficient knowledge regarding the prevention of VAP. Specifically, the nurses’ knowledge dimension score (7.66 ± 1.200) was low, indicating that there is still significant room for improvement in their understanding of VAP prevention-related knowledge. These findings are consistent with those of other domestic and international studies (21, 22). However, some studies have found that ICU nurses have a good understanding of knowledge related to VAP prevention (18). In this study, ICU nurses from different regions demonstrated varying levels of mastery of VAP prevention knowledge, particularly those from Lanzhou and Zhangye, whose knowledge scores were significantly higher than those from other regions. This may be attributed to differences in medical resource allocation, hospital management systems, and training opportunities available to nurses in these regions. In contrast, some regions may invest less in VAP prevention training, leading to deficiencies in nurses’ learning and mastery of related knowledge. In this study, nurses who had received VAP training demonstrated significantly better mastery of VAP knowledge than those who had not, a finding consistent with the results of several other scholars’ studies (18, 21, 23). Jordanian scholars conducted an observational study of 428 nurses working in intensive care units (24), finding that after receiving relevant training and education, nurses’ understanding of VAP prevention knowledge improved. Secondly, the type of ICU is also an important factor influencing nurses’ knowledge of VAP prevention. Nurses in general ICUs demonstrated significantly higher levels of VAP prevention knowledge compared to nurses in other types of ICUs. This is closely related to the clinical characteristics of ICUs, as general ICUs typically admit more complex cases, presenting nurses with greater clinical challenges. Additionally, numerous domestic and international studies have found that factors such as nurses’ educational background (21), years of ICU work experience, hospital level, and age (18) also influence ICU nurses’ VAP knowledge levels. However, these factors were not significant in this study.
According to the results of this study, ICU nurses generally have a positive attitude toward VAP prevention (mean attitude score: 28.67 ± 3.528), which is consistent with the findings of Li Suwen et al. in their study of 291 ICU nurses in Ganzhou City (17). Notably, nurses who had undergone specialized VAP training scored significantly higher than those who had not (p < 0.05). This finding holds important practical implications for healthcare settings with limited resources.
The results of this study indicate that ICU nurses demonstrate generally adequate performance in VAP prevention practices (mean score: 77.59 ± 5.839). This finding differs from the conclusions of a study conducted in Ethiopia (25), and such discrepancies may stem from systemic factors such as the allocation of medical resources and the sophistication of training systems. Notably, nurses who had received VAP training in the past 2 years demonstrated significantly better practice performance than those who had not received training. This result aligns with findings from a study at a tertiary care center in western India (26), further confirming the critical role of training interventions in improving clinical practice. The study also found significant differences in practice levels among ICU nurses across different regions, which may be related to variations in healthcare resource allocation, the completeness of training systems, and standardized quality control frameworks in these regions.
Based on the research findings, it is recommended to establish a tiered training system in resource-limited ICU settings. For junior nurses, foundational training should be conducted using the “1 + X” model, while senior nurses should receive advanced training such as updates on evidence-based guidelines. These efforts should be complemented by low-cost interventions such as daily knowledge point push notifications, peer micro-training, and visual checklists. At the management level, VAP prevention should be incorporated into performance evaluations, with priority given to ensuring adequate basic equipment configuration, and regional demonstration centers should be established to promote resource sharing. Future research should focus on comparing the effectiveness of different training models, analyzing practical barriers, and evaluating the long-term effects of intervention measures to continuously optimize VAP prevention strategies.
5 Conclusion
Most ICU nurses in Gansu Province performed well in terms of their attitude toward and practice of VAP prevention and were able to implement preventive and control measures effectively. However, there were deficiencies in their knowledge acquisition related to VAP prevention. Factors such as regional differences, ICU type, and the number of training sessions significantly impacted nurses’ VAP prevention and control abilities. In particular, the frequency of training sessions and regional resource allocation played a key role in nurses’ professional competence. A significant positive correlation was found between knowledge, attitude, and practice of VAP prevention, suggesting that enhanced knowledge training could improve nurses’ attitudes and practices. Therefore, hospitals should focus on providing regular training, especially in areas with limited knowledge and fewer training opportunities, to improve nurses’ comprehensive prevention and control competence.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by Medical Ethics Committee of Gansu Second People’s Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
XL: Data curation, Investigation, Methodology, Software, Writing – original draft, Writing – review & editing. XZ: Data curation, Investigation, Writing – review & editing. YF: Investigation, Writing – review & editing. ZY: Investigation, Writing – review & editing. YS: Investigation, Writing – review & editing. LZ: Investigation, Writing – review & editing. HZ: Supervision, Writing – review & editing. JW: Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by the National Natural Science Foundation of China under Grant (72064002), and the Special Fund for Basic Research Operating Costs of Central Universities (31920240079).
Acknowledgments
The authors thank all the ICU nurses who participated in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2025.1591582/full#supplementary-material
References
1. Osman, S, Al Talhi, YM, AlDabbagh, M, Baksh, M, Osman, M, and Azzam, M. The incidence of ventilator-associated pneumonia (VAP) in a tertiary-care center: comparison between pre- and post-VAP prevention bundle. J Infect Public Health. (2020) 13:552–7. doi: 10.1016/j.jiph.2019.09.015
2. Klompas, M, Branson, R, Eichenwald, EC, Greene, LR, Howell, MD, Lee, G, et al. Strategies to prevent ventilator-associated pneumonia in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol. (2014) 35:915–36. doi: 10.1086/677144
3. Sousa, AS, Ferrito, C, and Paiva, JA. Application of a ventilator associated pneumonia prevention guideline and outcomes: a quasi-experimental study. Intensive Crit Care Nurs. (2019) 51:50–6. doi: 10.1016/j.iccn.2018.10.001
4. Parisi, M, Gerovasili, V, Dimopoulos, S, Kampisiouli, E, Goga, C, Perivolioti, E, et al. Use of ventilator bundle and staff education to decrease ventilator-associated pneumonia in intensive care patients. Crit Care Nurse. (2016) 36:e1–7. doi: 10.4037/ccn2016520
5. Pileggi, C, Mascaro, V, Bianco, A, Nobile, CGA, and Pavia, M. Ventilator bundle and its effects on mortality among ICU patients: a meta-analysis. Crit Care Med. (2018) 46:1167–74. doi: 10.1097/CCM.0000000000003136
6. Bonell, A, Azarrafiy, R, Huong, VTL, Viet, TL, Phu, VD, Dat, VQ, et al. A systematic review and meta-analysis of ventilator-associated pneumonia in adults in Asia: an analysis of national income level on incidence and etiology. Clin Infect Dis. (2019) 68:511–8. doi: 10.1093/cid/ciy543
7. Rosenthal, VD, Jin, Z, Memish, ZA, Rodrigues, C, Myatra, SN, Kharbanda, M, et al. Multinational prospective cohort study of rates and risk factors for ventilator-associated pneumonia over 24 years in 42 countries of Asia, Africa, Eastern Europe, Latin America, and the Middle East: findings of the international nosocomial infection control consortium (INICC). Antimicrob Steward Healthc Epidemiol. (2023) 3:e6. doi: 10.1017/ash.2022.339
8. Luyt, CE, Sahnoun, T, Gautier, M, Vidal, P, Burrel, S, Pineton de Chambrun, M, et al. Ventilator-associated pneumonia in patients with SARS-CoV-2-associated acute respiratory distress syndrome requiring ECMO: a retrospective cohort study. Ann Intensive Care. (2020) 10:158. doi: 10.1186/s13613-020-00775-4
9. Dudeck, MA, Weiner, LM, Allen-Bridson, K, Malpiedi, PJ, Peterson, KD, Pollock, DA, et al. National healthcare safety network (NHSN) report, data summary for 2012, device-associated module. Am J Infect Control. (2013) 41:1148–66. doi: 10.1016/j.ajic.2013.09.002
10. Dudeck, MA, Horan, TC, Peterson, KD, Allen-Bridson, K, Morrell, G, Anttila, A, et al. National healthcare safety network report, data summary for 2011, device-associated module. Am J Infect Control. (2013) 41:286–300. doi: 10.1016/j.ajic.2013.01.002
11. Koulenti, D, Tsigou, E, and Rello, J. Nosocomial pneumonia in 27 ICUs in Europe: perspectives from the EU-VAP/CAP study. Eur J Clin Microbiol Infect Dis. (2017) 36:1999–2006. doi: 10.1007/s10096-016-2703-z
12. Al-Mugheed, K, Bani-Issa, W, Rababa, M, Hayajneh, AA, Syouf, AA, Al-Bsheish, M, et al. Knowledge, practice, compliance, and barriers toward ventilator-associated pneumonia among critical care nurses in eastern Mediterranean region: a systematic review. Healthcare (Basel). (2022) 10:1852. doi: 10.3390/healthcare10101852
13. Bankanie, V, Outwater, AH, Wan, L, and Yinglan, L. Assessment of knowledge and compliance to evidence-based guidelines for VAP prevention among ICU nurses in Tanzania. BMC Nurs. (2021) 20:209. doi: 10.1186/s12912-021-00735-8
14. Alanazi, S, and Alonazi, WB. Enhancing critical care practitioners’ knowledge and adherence to ventilator-associated events bundle: a comprehensive analysis. Front Med (Lausanne). (2024) 11:1365742. doi: 10.3389/fmed.2024.1365742
15. Madhuvu, A, Endacott, R, Plummer, V, and Morphet, J. Nurses’ knowledge, experience and self-reported adherence to evidence-based guidelines for prevention of ventilator-associated events: a national online survey. Intensive Crit Care Nurs. (2020) 59:102827. doi: 10.1016/j.iccn.2020.102827
16. Yin, Y, Sun, M, Li, Z, Bu, J, Chen, Y, Zhang, K, et al. Exploring the nursing factors related to ventilator-associated pneumonia in the intensive care unit. Front Public Health. (2022) 10:715566. doi: 10.3389/fpubh.2022.715566
17. SuWen, L, YuYang, H, and Fengzhen, W. Random forest analysis of ICU nurses’ knowledge, attitudes and practices in oral care for ventilator-associated pneumonia prevention. Nurs Crit Care. (2025) 30:e13289. doi: 10.1111/nicc.13289
18. Yao, N, Xu, B, Xu, R, Gong, Z, Ma, G, Peng, S, et al. Adult intensive care unit nurses’ knowledge of and compliance barriers to evidence-based guidelines for prevention of ventilator-associated pneumonia: a cross-sectional survey. Nurs Crit Care. (2024) 29:1591–1600. doi: 10.1111/nicc.13162
19. SuWen, L, YuYang, H, and Wei, B. Understanding oral care in the intensive care unit: a qualitative study of nurse experiences and practices with mechanically ventilated patients. Nurs Crit Care. (2025) 30:e13296. doi: 10.1111/nicc.13296
20. Wang, Y, Lan, Y, Jia, T, Ma, M, Liu, C, and Tang, H. Construction and application of a training program for ICU nurses to manage artificial airway gasbags to prevent ventilator-associated pneumonia. J Multidiscip Healthc. (2023) 16:3737–48. doi: 10.2147/JMDH.S438316
21. Getahun, AB, Belsti, Y, Getnet, M, Bitew, DA, Gela, YY, Belay, DG, et al. Knowledge of intensive care nurses’ towards prevention of ventilator-associated pneumonia in North West Ethiopia referral hospitals, 2021: a multicenter, cross-sectional study. Ann Med Surg (Lond). (2022) 78:103895. doi: 10.1016/j.amsu.2022.103895
22. El-Kass, SM, Alruwili, HA, Alrowily, MA, Ellayan, OM, El-Kass, LM, Hijo, EE, et al. Critical care nurses’ knowledge on prevention of ventilator-associated pneumonia: a cross-sectional study. Indian J Crit Care Med. (2024) 28:1122–9. doi: 10.5005/jp-journals-10071-24854
23. Rafiei, H, Rahimi, S, Shafaei, M, and Ommatmohammadi, M. Emergency nurses’ knowledge about ventilator-associated pneumonia. Int Emerg Nurs. (2020) 48:100783. doi: 10.1016/j.ienj.2019.06.006
24. Hassan, ZM, and Wahsheh, MA. Knowledge level of nurses in Jordan on ventilator-associated pneumonia and preventive measures. Nurs Crit Care. (2017) 22:125–32. doi: 10.1111/nicc.12273
25. Debas, SA, Zeleke, ME, Mersha, AT, Melesse, DY, Admassie, BM, Workie, MM, et al. Evaluation of ventilator-associated pneumonia care practice in the intensive care units of a comprehensive specialized hospital in Northwest Ethiopia: a 1.5-year prospective observational study. BMC Anesthesiol. (2024) 24:361. doi: 10.1186/s12871-024-02753-w
26. Paliwal, N, Bihani, P, Mohammed, S, Rao, S, Jaju, R, and Janweja, S. Assessment of knowledge, barrier in implementation, and compliance to ventilator bundle among resident doctors and nurses working in intensive care units of a tertiary care center of western India: a cross-sectional survey. Indian J Crit Care Med. (2023) 27:270–6. doi: 10.5005/jp-journals-10071-24434
Keywords: ventilator-associated pneumonia, ICU, knowledge, attitude, practice
Citation: Li X, Zhang X, Feng Y, Yao Z, Sun Y, Zhang L, Zhang H and Wang J (2025) Knowledge, attitude, and practice of nurses in ICU on preventing ventilator-associated pneumonia: a cross-sectional study in Gansu Province, China. Front. Med. 12:1591582. doi: 10.3389/fmed.2025.1591582
Edited by:
Jian-cang Zhou, Zhejiang University, ChinaReviewed by:
Sahbanathul Missiriya Jalal, King Faisal University, Saudi ArabiaXiangping Chen, Zhejiang University School of Medicine, China
Copyright © 2025 Li, Zhang, Feng, Yao, Sun, Zhang, Zhang and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Haojun Zhang, aGFvemlfNTIzQDE2My5jb20=; Junling Wang, d2FuZ2psQGx6dS5lZHUuY24=
 Xiarong Li
Xiarong Li Xiaoliang Zhang2
Xiaoliang Zhang2 Junling Wang
Junling Wang