- 1Department of Infectious Diseases, Jiangshan People’s Hospital, Quzhou, China
- 2Department of Infectious Diseases, Sir Run Run Shaw Hospital, Zhejiang University School of Medicine, Hangzhou, China
- 3Key Laboratory of Microbial Technology and Bioinformatics of Zhejiang Province, Hangzhou, China
- 4Regional Medical Center for National Institute of Respiratory Diseases, Sir Run Run Shaw Hospital, Zhejiang University School of Medicine, Hangzhou, China
- 5Taizhou Hospital, Zhejiang University, Taizhou, China
- 6Department of Critical Care Medicine, Sir Run Run Shaw Hospital, Zhejiang University School of Medicine, Hangzhou, China
- 7Pilot Gene Technologies (Hangzhou) Co., Ltd., Hangzhou, China
- 8Department of Infectious Diseases, Shangyu People’s Hospital of Shaoxing, Shaoxing University, Shaoxing, Zhejiang, China
- 9Department of Respiratory and Critical Care Medicine, The First Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou, China
Background: Plasma droplet digital polymerase chain reaction (ddPCR) has been used for pathogen detection and has shown good diagnostic value, but no studies have yet demonstrated its application in focal infections. Herein a pilot study using plasma ddPCR to diagnose focal infection is discussed.
Methods: Eight patients with a diagnosed focal infection who underwent plasma ddPCR for bacterial detection between 2021 and 2022 in Sir Run Run Shaw hospital were enrolled in this retrospective single-center pilot study. Results of ddPCR and focal cultures were compared as well as the turnaround time of two methods and other clinical data.
Results: In 7/8 cases, plasma ddPCR results were consistent with focal culture results. The turnaround time for ddPCR was 2.5 h, significantly lower than the average time for focal cultures of 2.63 days.
Conclusion: This pilot study indicates the promising value of the plasma ddPCR method in the rapid diagnosis of focal infection. If larger studies support the findings here, this method can help improve diagnostic accuracy and guide treatment decisions in suspected focal infections.
Introduction
A focal infection occurs when an infection is localized in a specific organ or part of an organ such as brain, liver and kidneys. The pathogenic spectrum of focal infection varies from organ to organ, including bacteria, fungi, viruses, parasites, etc. Bacteria as common causative pathogens for most foci are usually detected by culture while this gold standard method reported insufficient sensitivity (1).
The droplet digital polymerase chain reaction (ddPCR) is an improved technique of conventional PCR with higher sensitivity, better accuracy and more stable amplification of rare target DNA sequences (2, 3). This technology achieves absolute quantification by quantifying nucleic acid molecules at the single-molecule level, and thus can accurately measure when testing low-abundance targets. For example, SARS-CoV-2 can be detected at as low as 0.688 or 1.1 cDNA copies (4). It has been proved to be a potential method for the detection of specific bacteria in the study of bloodstream infections (BSI) (5, 6), demonstrating its diagnostic value for infectious diseases.
From our experience of utilizing plasma ddPCR in clinical settings, we found that bacteria concordant with focal cultures could be detected in the blood samples of some patients who were later confirmed to have focal infection. We therefore performed this retrospective study to assess the possibility of using plasma ddPCR for microbial diagnosis of focal infections caused by bacteria.
Methods
Study design
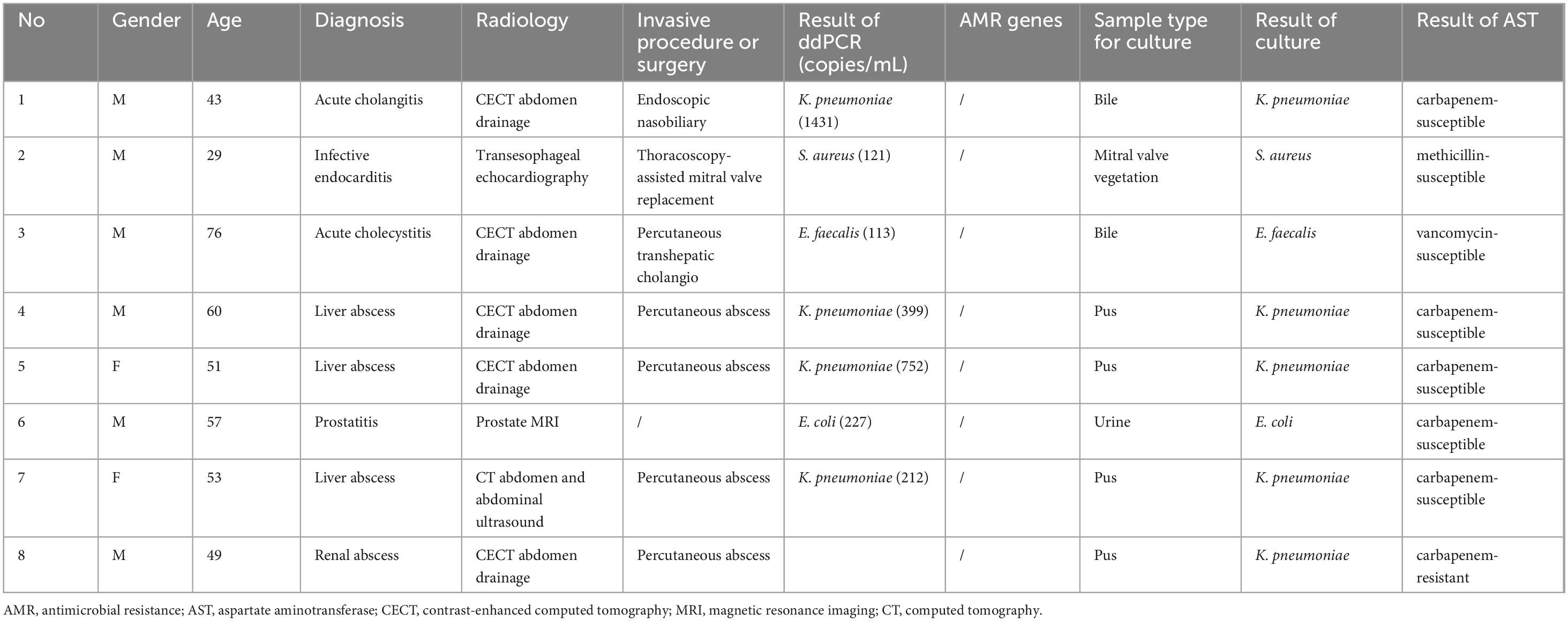
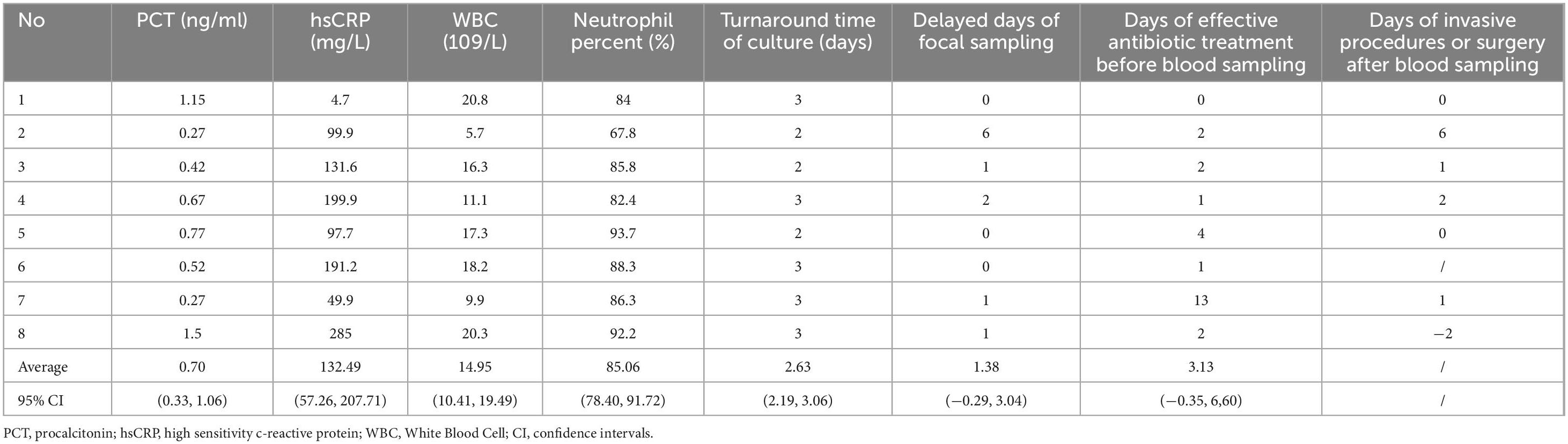
This retrospective review was conducted in Sir Run Run Shaw hospital (a tertiary hospital in Zhejiang province, China) from January 2021 to December 2022. For an accurate assessment, we restricted inclusion criteria to exclude the presence of BSI. Patients were enrolled who met the following criteria concurrently: (1) diagnosed with culture-proven focal infection; (2) paired blood culture (BC) and plasma ddPCR conducted synchronously; (3) blood culture-negative. The demographic data and clinical data of the patients were recorded (Tables 1, 2). Due to the pilot nature of the study and the small number of patients enrolled, clinical data were descriptive only.
Sample collection and plasma DNA extraction
Peripheral venous blood (4 ml) was drawn from each patient into an ethylenediaminetetraacetate (EDTA)-containing tube after two sets of blood cultures (both aerobic and anaerobic bottles, 10 mL per bottle) were taken from the same catheter or venipuncture. Plasma was immediately isolated after centrifugation at 1,600 × g, and 22°C for 15 min. Plasma DNA extraction was completed within 1 h from 2 ml of plasma using a Magnetic Serum/Plasma DNA Kit (TIANGEN Biotech, Beijing, China) and the Auto-Pure20B Nucleic Acid Purification System (Hangzhou Allsheng Instruments Company, Hangzhou, China) following the manufacturer’s protocol. DNA was eluted in 50 μl of elution buffer and isolated DNA was quantified with a UV-Vis spectrophotometer (Thermo Fisher, Massachusetts, US). Each sample was measured three times and the average value was taken. The sample concentration ranged from 12 to 22 ng/uL. Regardless of the DNA concentration, 5 uL of the eluted DNA sample was taken for the next step of ddPCR testing for each test.
Droplet digital PCR
The multiplex ddPCR testing allowed for the detection of eight common bacteria (Enterococcus faecium, Enterococcus faecalis, Staphylococcus aureus, Streptococcus pneumoniae, Klebsiella pneumoniae, Pseudomonas aeruginosa, Acinetobacter baumannii, Escherichia coli) and three antimicrobial resistance (AMR) genes (blaKPC, blaNDM, mecA) in amounts as small as 50 copies/mL (Pilot Gene Technologies. Hangzhou, China). The whole procedure was performed as previously described (6) with minor modifications. The ddPCR test was performed using the Droplet Digital PCR System (Pilot Gene Technology, Hangzhou, China), according to the manufacturer’s instructions. Briefly, 5 μl of extracted DNA sample was added to 10 μl of the ddPCR premix which includes primers, probes, dNTP mixture, Taq polymerase and other necessary components for PCR amplification. The 15 μl mixture was added into a microfluidic chip and loaded into a DG32 droplet generator for droplet generation. Chips were then amplified in a thermal cycler TC1 with the thermal cycling parameters: 95°C for 5 min, followed by 40 cycles of 95°C for 15 s and 60°C for 30 s. Next, chips were transferred to a chip scanner CS5 for fluorescence signal reading and data analysis using GenePMS software (v2.0.01.20011). Synthesized DNA fragment was used as positive control, and DNase- free water or blood samples from three healthy subjects were used as negative controls.
Results
Ultimately, eight cases with definite diagnosis of focal infection were enrolled in this retrospective pilot study (Tables 1, 2, and Supplementary Figure 1). All patients had fever but no drop in blood pressure when samples were drawn. All blood cultures came back negative even though 7 of them were drawn two sets (both aerobic and anaerobic bottles). Three patients were diagnosed with liver abscess. The other five patients were diagnosed with acute cholangitis, acute cholecystitis, infective endocarditis, prostatitis and renal abscess, respectively, based on radiology and focal culture results. Except for case No. 6, all patients underwent invasive procedures or surgery for treatment and specimen collection. All cultured bacteria from bile, pus, urine and mitral valve vegetation were included in the ddPCR panel, including K. pneumoniae (n = 5), E. coli (n = 1), S. aureus (n = 1) and E. faecalis (n = 1). The ddPCR test reported concordantly positive results with focal culture in 7 cases while failed to detect the causative bacterium (K. pneumoniae) in the remaining 1 case (No. 8). The concentration of bacterial DNA copies detected ranged from 113 to 1431 copies/mL (Table 2).
Antimicrobial resistance genes including blaKPC, blaNDM, and mecA were not detected, consistent with the results of 7 cases in antimicrobial susceptibility testing (AST). In case No. 8, carbapenem-resistant K. pneumoniae strain was detected by culture and AST but missed in ddPCR and no blaKPC or blaNDM genes were detected. This negative result may be due to the fact that this case was the only one in which drainage was performed 2 days prior to blood collection (Table 2).
Procalcitonin, high-sensitivity C-reactive protein (hs-CRP) as well as blood routine tests were performed in all patients at the time of BC and ddPCR. PCT and hs-CRP were elevated to varying degrees in all patients. The PCT levels of all 8 patients were lower than 2 ng/mL at the time of sampling, suggesting that they were at a moderate risk of sepsis. Among them, the PCT levels of patients No. 2, 3, and 7 were lower than 0.5 ng/mL, indicating a state of localized infection rather than systemic bacterial infection (7). White blood cell counts and neutrophil percentages were elevated in all patients except patient No. 2 who was diagnosed with infective endocarditis.
The turnaround time of focal culture ranged from 2 to 3 days regardless of sample type, with an average time of 2.63 ± 0.62 days, which was significantly higher than that 2.5 h per sample of ddPCR test (Mann-Whitney U test, P < 0.0001). All focal samples were obtained no earlier than blood samples, with a maximum interval of 6 days later (No. 2). Late sampling of focal specimens, combined with longer turnaround times of culture, resulted in focal culture results being available an average of 3 days later than ddPCR results.
Prior to the blood draw, all patients received effective antibiotic treatment except patient No. 1. Case No. 8 with negative ddPCR result received effective treatment for 2 days, while 4 of the positive cases exceeded this time, the longest of which even lasted 13 days (No. 7). This suggested that the duration of effective treatment may not affect the results of ddPCR in our study.
Discussion
Focal infections can cause intermittent bacteremia, which is difficult to detect by blood cultures (8, 9). In this case, however, ddPCR may have an increased capability of pathogen detection because of its ability to identify bacterial DNA, which might have persisted in a patient’s bloodstream after a period of intermittent bacteremia (10). In this pilot study, we reviewed in detail 8 patients with definite diagnosis of focal infection, in an effort to evaluate the robustness of plasma ddPCR results, in the context of a concurrent negative BC. In 7 out of 8 (87.5%) cases we included, causative DNA fragments were detected in peripheral blood samples, i.e., plasma ddPCR results were consistent with focal culture results. This result suggested that it may be a common phenomenon that ddPCR can detect causative bacteria of focal infection in peripheral blood.
This approach, if successfully applied, would bring many advantages in clinical practice. Traditionally, the diagnosis of focal infection has relied on radiology examination and focal cultures. However, when focal infection is in its early stage, radiological methods may fail to detect the foci due to the lack of substantial anatomical changes (11), making localization and sampling of the infection difficult. Furthermore, sampling of deep site infection is often difficult and traumatic. When surgery is required for sampling, it might be delayed according to clinical condition. As in our study, focal sampling was no earlier than blood collections in all cases and it took 6 days in case No. 2 after the blood draw to get vegetations for culture by mitral valve surgery. Plasma ddPCR, however, could be performed rapidly and less invasively. Compared to culture, ddPCR method could reduce turnaround time from days to hours. Timely sampling along with a short turnaround time enables this method to achieve rapid etiological diagnosis and thus antibiotic de-escalation or treatment adjustment.
Our novel findings provide the first step evidence that plasma ddPCR has the potential to act like liquid biopsy for diagnosing and monitoring remote foci in a non-invasive manner as shown with the Karius test in pneumonia, bone and joint infections and central nervous system infections (12–14). However, there were still many issues to be further explored. First, due to the limitation of retrospective design, this study had potential selection bias and reporting bias. Second, due to the small sample size of our study, we were not yet able to evaluate the efficacy of plasma ddPCR in the diagnosis of focal infection as well as to identify factors that affecting ddPCR results. Previous study (6) has reported a presumptive false positive rate of 7.5% using similar PCR panels for the diagnosis of BSI. The possible reasons of false-positive results might be explained by the presence of possible contamination or DNAemia which presents circulating cell-free DNA from dead bacteria in the absence of infection (15). Similar cases may arise when the application of plasma ddPCR is expanded to focal infection. ddPCR testing of focal fluid or pus samples can be used to verify focal culture-negative cases. In addition, using two or more sets of primers and probes to detect the same pathogen by plasma ddPCR may reduce the false positive rate, but this idea also needs to be verified by further research.
In conclusion, our study demonstrates the etiological diagnostic value of plasma ddPCR in different types of focal infections. This method is not only highly sensitive, but also less invasive and has a shorter turnaround time than sample collection from infected organs, so its early application may help improve patient outcomes and reduce healthcare burden. To promote this method in the clinic, further investigations with larger sample sizes are required to evaluate the diagnostic efficiency, clinical efficacy, cost-effectiveness, and optimal timing of the assay.
Conclusion
The ultra-high sensitivity of plasma ddPCR detection technology for cell-free DNA in peripheral blood samples provides the possibility of etiological diagnosis of even focal infection. If studies with larger sample size support the findings here, it will be of great help to judge whether patients are infected with common pathogens in clinical practice.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The study was approved by the Ethics Committee of Sir Run Run Shaw hospital (20200818-7) and informed consent was obtained from all participants. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
YZ: Data curation, Writing – review and editing, Writing – original draft. SW: Writing – review and editing, Writing – original draft, Conceptualization, Data curation. XM: Writing – original draft, Writing – review and editing, Data curation, Conceptualization. LL: Conceptualization, Writing – review and editing, Data curation, Writing – original draft. YC: Writing – review and editing, Conceptualization, Writing – original draft, Data curation. BF: Data curation, Writing – original draft, Conceptualization, Writing – review and editing. JX: Writing – review and editing, Conceptualization, Data curation. JY: Writing – review and editing, Data curation, Supervision. HZ: Writing – review and editing, Writing – original draft, Supervision. YY: Supervision, Writing – review and editing. DZ: Supervision, Funding acquisition, Data curation, Writing – review and editing, Writing – original draft.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by the Key R&D Plan of the Ministry of Science and Technology of China (Grant number 2022YFC2504502), and the Key Research Program of the Science Technology Department of Zhejiang Province (Grant number 2021C03055).
Acknowledgments
We acknowledge the professionalism and compassion demonstrated by all the healthcare workers involved in the care of patients.
Conflict of interest
JX was employed by Pilot Gene Technologies (Hangzhou) Co., Ltd.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Generative AI statement
The authors declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2025.1613077/full#supplementary-material
Supplementary Figure 1 | Timeline diagram.
References
1. Zhang H, Ai J, Cui P, Zhu Y, Hong-Long W, Li Y, et al. Incremental value of metagenomic next generation sequencing for the diagnosis of suspected focal infection in adults. J Infect. (2019) 79:419–25. doi: 10.1016/j.jinf.2019.08.012
2. Chen B, Jiang Y, Cao X, Liu C, Zhang N, Shi D. Droplet digital Pcr as an emerging tool in detecting pathogens nucleic acids in infectious diseases. Clin Chim Acta Int J Clin Chem. (2021) 517:156–61. doi: 10.1016/j.cca.2021.02.008
3. Wouters Y, Dalloyaux D, Christenhusz A, Roelofs H, Wertheim H, Bleeker-Rovers C, et al. Droplet digital polymerase chain reaction for rapid broad-spectrum detection of bloodstream infections. Microbial Biotechnol. (2020) 13:657–68. doi: 10.1111/1751-7915.13491
4. Truyols-Vives J, Stiliyanov-Atanasov K, Sala-Llinàs E, Toledo-Pons N, Baldoví H, Mercader-Barceló J. Efficiency and sensitivity optimization of a protocol to quantify indoor airborne SARS-CoV-2 levels. J Hosp Infect. (2022) 130:44–51. doi: 10.1016/j.jhin.2022.08.011
5. Hu B, Tao Y, Shao Z, Zheng Y, Zhang R, Yang X, et al. A comparison of blood pathogen detection among droplet digital Pcr, metagenomic next-generation sequencing, and blood culture in critically Ill patients with suspected bloodstream infections. Front Microbiol. (2021) 12:641202. doi: 10.3389/fmicb.2021.641202
6. Wu J, Tang B, Qiu Y, Tan R, Liu J, Xia J, et al. Clinical validation of a multiplex droplet digital Pcr for diagnosing suspected bloodstream infections in Icu practice: a promising diagnostic tool. Crit Care. (2022) 26:243. doi: 10.1186/s13054-022-04116-8
7. Morgenthaler N, Struck J, Fischer-Schulz C, Seidel-Mueller E, Beier W, Bergmann A. Detection of Procalcitonin (Pct) in healthy controls and patients with local infection by a sensitive Ilma. Clin Lab. (2002) 48:263–70.
8. Reimer L, Wilson M, Weinstein M. Update on detection of bacteremia and fungemia. Clin Microbiol Rev. (1997) 10:444–65. doi: 10.1128/cmr.10.3.444
9. Kalligeros M, Zacharioudakis I, Tansarli G, Tori K, Shehadeh F, Mylonakis E. In-depth analysis of T2Bacteria positive results in patients with concurrent negative blood culture: a case series. BMC Infect Dis. (2020) 20:326. doi: 10.1186/s12879-020-05049-9
10. Nguyen M, Clancy C, Pasculle A, Pappas P, Alangaden G, Pankey G, et al. Performance of the T2bacteria panel for diagnosing bloodstream infections: a diagnostic accuracy study. Ann Internal Med. (2019) 170:845–52. doi: 10.7326/m18-2772
11. Bleeker-Rovers C, de Kleijn E, Corstens F, van der Meer J, Oyen W. Clinical value of Fdg pet in patients with fever of unknown origin and patients suspected of focal infection or inflammation. Eur J Nuclear Med Mol Imaging. (2004) 31:29–37. doi: 10.1007/s00259-003-1338-3
12. Bergin S, Chemaly R, Dadwal S, Hill J, Lee Y, Haidar G, et al. Plasma microbial cell-free DNA sequencing in immunocompromised patients with pneumonia: a prospective observational study. Clin Infect Dis. (2024) 78:775–84. doi: 10.1093/cid/ciad599
13. Echeverria A, Cohn I, Danko D, Shanaj S, Blair L, Hollemon D, et al. Sequencing of circulating microbial cell-free DNA can identify pathogens in periprosthetic joint infections. J Bone Joint Surg Am. (2021) 103:1705–12. doi: 10.2106/jbjs.20.02229
14. Shishido A, Noe M, Saharia K, Luethy P. Clinical impact of a metagenomic microbial plasma cell-free DNA next-generation sequencing assay on treatment decisions: a single-center retrospective study. BMC Infect Dis. (2022) 22:372. doi: 10.1186/s12879-022-07357-8
Keywords: focal infection, droplet digital PCR, molecular diagnosis, blood samples, focal culture
Citation: Zhang Y, Weng S, Ma X, Lin L, Chen Y, Feng B, Xia J, Ye J, Zhou H, Yu Y and Zhao D (2025) Plasma ddPCR for etiological diagnosis of focal bacterial infections. Front. Med. 12:1613077. doi: 10.3389/fmed.2025.1613077
Received: 16 April 2025; Accepted: 08 July 2025;
Published: 24 July 2025.
Edited by:
Mohammad Tahir Siddiqui, Indian Institute of Technology Delhi, IndiaReviewed by:
Selvaraj Anthonymuthu, University of California, Irvine, United StatesJosep Mercader-Barceló, University of the Balearic Islands, Spain
Copyright © 2025 Zhang, Weng, Ma, Lin, Chen, Feng, Xia, Ye, Zhou, Yu and Zhao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dongdong Zhao, MzMxMzAwNEB6anUuZWR1LmNu; Hua Zhou, emhvdWh1YTFAemp1LmVkdS5jbg==; Yunsong Yu, eXZ5czExOUB6anUuZWR1LmNu
 Yongfeng Zhang
Yongfeng Zhang ShanShan Weng2,3,4
ShanShan Weng2,3,4 Jiayuan Ye
Jiayuan Ye Hua Zhou
Hua Zhou Yunsong Yu
Yunsong Yu Dongdong Zhao
Dongdong Zhao