- 1Department of Gynecology and Obstetrics, Chengdu Women’s and Children’s Central Hospital, School of Medicine, University of Electronic Science and Technology of China, Chengdu, China
- 2Bazhong Maternal and Child Health Hospital, Bazhong, China
- 3Department of Obstetrics and Gynecology, Women and Children’s Hospital of Chongqing Medical University, Chongqing, China
- 4NHC Key Laboratory of Birth Defects and Reproductive Health, Chongqing, China
- 5Key Laboratory of Birth Defects and Related Diseases of Women and Children, Ministry of Education, West China Second Hospital, Sichuan University, Chengdu, China
Objective: This study aimed to compare the perioperative outcomes of single-incision laparoscopic surgery (SILS) and dual-port laparoscopic myomectomy in patients with solitary uterine fibroids.
Methods: This retrospective observational study included 162 patients who underwent laparoscopic myomectomy for solitary fibroids from January 2022 to December 2023 at a single tertiary center. Patients were divided into a SILS group (n = 77) and a dual-port group (n = 85). Perioperative outcomes—including operative time, intraoperative blood loss, analgesic use, hospital stay, and cosmetic results—were compared between the groups. Multivariate linear and logistic regression analyses were conducted to identify factors associated with surgical complexity and recovery.
Results: The dual-port group had significantly lower intraoperative blood loss (41.71 ± 65.37 mL vs. 89.55 ± 93.70 mL, p < 0.001), lower rates of postoperative analgesic use (24.7% vs. 40.3%, p = 0.034), and shorter hospital stays (1.07 ± 0.30 vs. 1.30 ± 0.65 days, p = 0.005) compared to the SILS group. Fibroid size and procedure time were independent predictors of increased bleeding. Posterior wall fibroids were significantly associated with postoperative analgesic use. Delayed discharge was more common in patients with larger fibroids and those requiring postoperative analgesia. Cosmetic outcomes in the dual-port group remained favorable despite the auxiliary incision.
Conclusion: Dual-port laparoscopic myomectomy is a feasible and potentially more effective alternative to single-incision surgery, offering better ergonomic access, improved perioperative outcomes, and excellent cosmetic results. This approach may be especially advantageous when addressing large or posteriorly located fibroids. Individualized surgical planning remains essential to optimize outcomes in minimally invasive myomectomy.
Background
Uterine fibroids (leiomyomas) are the most prevalent benign tumors among women of reproductive age, affecting up to 70% of this population (1, 2). While many cases are asymptomatic, a substantial proportion of women experience clinical symptoms such as heavy menstrual bleeding, pelvic pain, urinary frequency, and infertility (3, 4). For women who wish to preserve fertility or retain the uterus for other reasons, myomectomy remains the preferred surgical intervention. The evolution of minimally invasive surgical techniques has led to laparoscopic myomectomy becoming the gold standard, offering advantages including less postoperative pain, faster recovery, lower complication rates, and better cosmetic outcomes compared to open surgery (5–7).
In recent years, single-incision laparoscopic surgery (SILS) has gained traction due to its superior aesthetic results and potential to further reduce postoperative discomfort (8). However, despite its cosmetic appeal, SILS presents notable technical challenges. These include restricted instrument triangulation, limited maneuverability, and a higher likelihood of external and internal instrument collisions (9, 10). Such constraints may increase operative time, intraoperative blood loss, and surgeon fatigue, especially in procedures requiring complex dissection or suturing, such as myomectomy for larger or deeply embedded fibroids (11, 12).
To overcome these limitations, dual-port laparoscopic surgery has emerged as a modified minimally invasive approach (13). By introducing a small auxiliary port—typically only 5 mm in diameter—this technique preserves much of the cosmetic advantage of SILS while enhancing surgical ergonomics and precision. The additional port enables the formation of a triangular working space, improving instrument mobility and facilitating more efficient dissection and suturing (14, 15). Thus, dual-port laparoscopy is proposed as a balanced alternative, potentially optimizing both operative efficiency and patient satisfaction.
Despite the theoretical advantages, comparative data on dual-port vs. single-incision laparoscopic myomectomy remain limited, especially in cases involving solitary fibroids. Furthermore, the extent to which operative variables—such as fibroid size, location, and pelvic adhesions—impact outcomes across surgical techniques is poorly defined. A better understanding of these factors is essential to guide surgical planning and tailor treatment approaches according to patient-specific anatomical and clinical characteristics.
In this context, the present study aimed to compare the perioperative outcomes of single-incision and dual-port laparoscopic myomectomy in patients with solitary uterine fibroids. The analysis focused on surgical efficiency (operative time and blood loss), recovery-related indicators (pain management, gastrointestinal function, and hospital stay), and cosmetic considerations. By identifying key factors influencing surgical outcomes in each approach, this study seeks to provide practical insights into optimizing myomectomy strategies and enhancing individualized care in minimally invasive gynecologic surgery.
Methods
Study design and patient selection
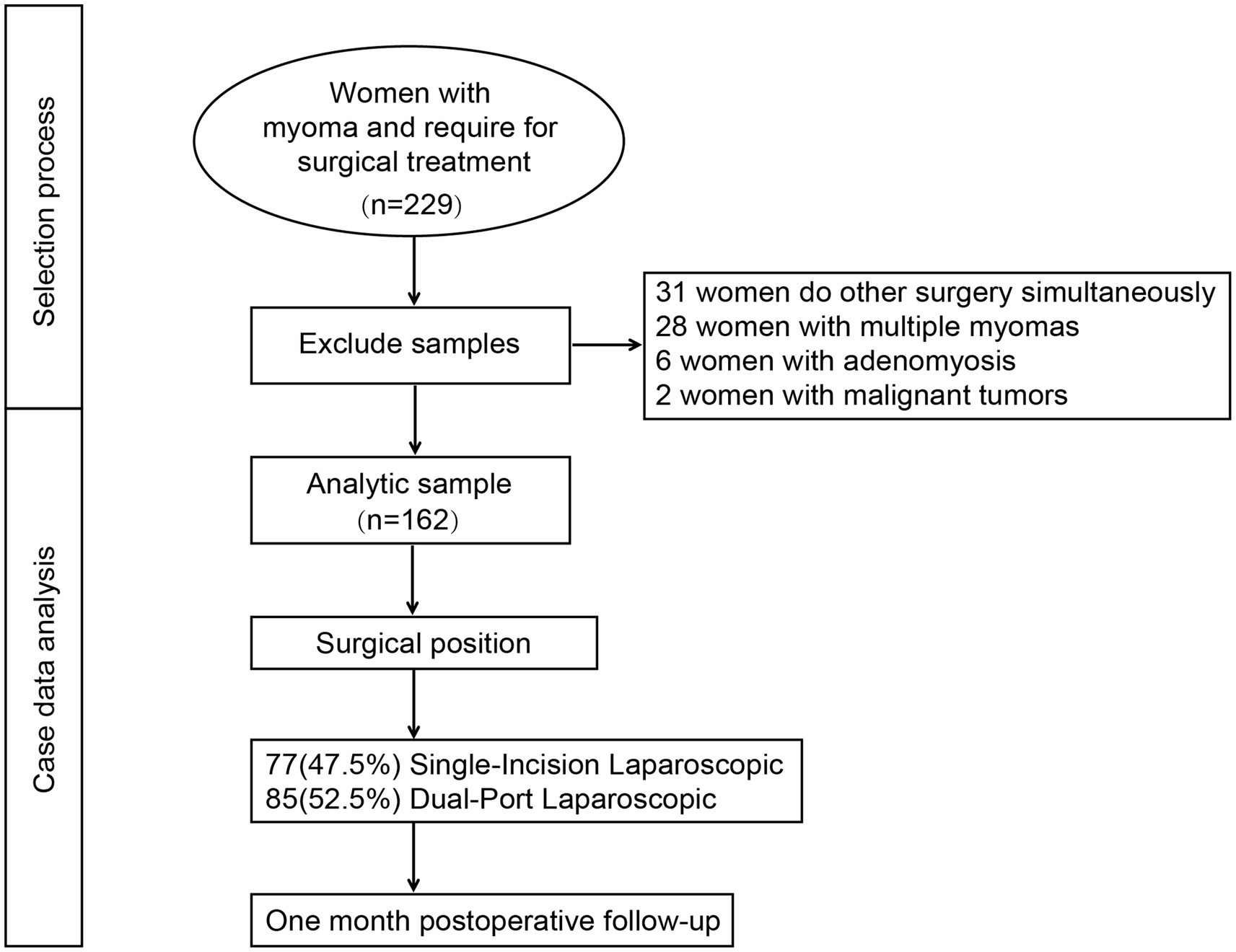
This was a single-center, retrospective observational study conducted at Chengdu Women’s and Children’s Central Hospital, a tertiary referral center specializing in minimally invasive gynecologic surgery. The study period extended from January 2022 to December 2023. The protocol was approved by the institutional Ethics Committee of Chengdu Women’s and Children’s Central Hospital (No. 2022207), and informed consent was obtained from all participants prior to surgery. A total of 229 patients diagnosed with uterine fibroids and scheduled to undergo laparoscopic myomectomy were initially screened. The inclusion criteria were: (1) age between 18 and 50 years, (2) presence of a solitary uterine fibroid confirmed by preoperative ultrasound or MRI, and (3) planned laparoscopic myomectomy via either a single-incision or dual-port technique. Exclusion criteria included: (1) intraoperative concurrent procedures (e.g., ovarian cystectomy and hysteroscopic surgery), (2) multiple fibroids requiring extensive uterine reconstruction, (3) postoperative histopathological confirmation of adenomyosis or uterine malignancy, and (4) incomplete perioperative data. After applying the exclusion criteria, a total of 162 patients were included in the final analysis.
Surgical procedures
All surgeries were performed by experienced gynecologic laparoscopists with more than 10 years of operative experience. Surgeons were categorized according to operative experience as either having ≥10 years or ≥20 years of independent laparoscopic surgical practice, and this variable was included in multivariate models to adjust for potential allocation bias. The choice of surgical approach—single-incision laparoscopy or dual-port laparoscopy—was based on surgeon preference and intraoperative feasibility.
Single-incision laparoscopic myomectomy (SILS group)
A 2–2.5 cm longitudinal incision was made in the umbilicus to insert a multichannel single-port device. A standard 10-mm laparoscope and conventional straight laparoscopic instruments were used for dissection, fibroid enucleation, and myometrial repair. Due to limited triangulation, instrument crossing and rotation were frequently required.
Dual-port laparoscopic myomectomy (dual-port group)
A 10-mm umbilical port was placed on the laparoscope, and an additional 5-mm auxiliary port was inserted in the lower left or right abdominal quadrant under direct visualization. This configuration enabled triangular instrument alignment, facilitating more ergonomic tissue manipulation and suturing. The remainder of the procedure followed the same steps as in the SILS group.
Data collection and variables
Clinical and perioperative data were collected from electronic medical records. Baseline variables included age, body mass index (BMI), gravidity, parity, history of pelvic surgery, fibroid size and location (anterior vs. posterior wall), and the presence of pelvic adhesions (graded intraoperatively by the operating surgeon). Surgical outcomes included operative time (from skin incision to closure), intraoperative blood loss (estimated by suction volume minus irrigation fluid), conversion to multi-port or laparotomy, request for postoperative analgesics within 24 h, postoperative recovery indicators (time to first flatus, time to first oral intake, time to first ambulation, and time to first voiding), length of hospital stay, delayed discharge (defined as length of stay exceeding the institutional median by >1 day), and postoperative complications (including fever, infection, hematoma, or need for reoperation).
Complications were defined as adverse events occurring after surgery, including but not limited to wound infection, hemorrhage, thromboembolic episodes, and urinary tract-related issues. The severity of each complication was classified according to the modified Clavien–Dindo system, following the version adopted by our institution (Supplementary Table 1) (16).
Pain and analgesia assessment
Postoperative pain was assessed using the Visual Analog Scale (VAS) at 3 and 6 h after surgery. Patients were offered non-steroidal anti-inflammatory drugs (NSAIDs) or opioids based on the severity of pain and their analgesic request. Analgesic use (yes/no) was recorded as a dichotomous variable. Photographic documentation of the abdominal wall was performed 1 week after surgery. Surgeons evaluated incision healing and size, with emphasis on the auxiliary port site in the dual-port group.
Statistical analysis
All statistical analyses were performed using SPSS software (version XX.0, IBM Corp., Armonk, NY, United States). Continuous variables were expressed as mean ± standard deviation (SD) and compared using independent t-tests or Mann–Whitney U-tests, depending on their normality. Categorical variables were presented as counts and percentages and analyzed using chi-squared or Fisher’s exact tests as appropriate. Multivariate linear regression analyses were conducted to identify predictors of operative time and intraoperative blood loss. Multivariate logistic regression models were used to assess factors independently associated with postoperative analgesic use and delayed hospital discharge. Variables with a p-value of <0.10 in univariate analysis were entered into the multivariate models. Odds ratios (ORs) and beta coefficients (β) with 95% confidence intervals (CIs) were reported. A p-value of <0.05 was considered statistically significant.
Results
A total of 229 patients with uterine fibroids were initially enrolled in this study (Figure 1). After excluding cases involving concurrent surgeries, multiple fibroids, postoperative pathological confirmation of adenomyosis, and malignant tumors, 162 patients were included in the final analysis. Among them, 77 patients (47.5%) underwent single-incision laparoscopic myomectomy, while 85 patients (52.5%) received dual-port laparoscopic myomectomy. The baseline demographic and clinical characteristics of the patients are summarized in Table 1. The mean age was 38.21 ± 7.26 years, and the mean BMI was 22.64 ± 3.08 kg/m2. A total of 76 patients (46.9%) had a history of pelvic surgery, including 62 (38.3%) with a prior cesarean section. No statistically significant differences were found between the two groups in terms of age, BMI, gestational history, or history of pelvic surgery (all p > 0.05).
Intraoperative parameters showed that the mean procedure time was comparable between the single-incision and dual-port groups (p = 0.278), whereas intraoperative bleeding volume was significantly higher in the single-incision group (p < 0.001). Additionally, the posterior wall fibroid location was more common in the dual-port group (p = 0.008), while the incidence of pelvic adhesions and surgical conversion rates did not differ significantly. In terms of postoperative recovery, the request for analgesics was significantly more frequent in the single-incision group (p = 0.034). Furthermore, the length of hospital stay was longer (p = 0.005), and the rate of delayed discharge was higher in the single-incision group (p = 0.003). No significant differences were observed between the two groups in terms of gastrointestinal recovery indicators, infection, or reoperation.
In the multivariate linear regression analysis (Figure 2A), larger fibroid size (β = 4.70, 95% CI: 1.91 to 7.49, p < 0.001), higher body mass index (BMI) (β = 1.65, 95% CI: 0.11 to 3.18, p = 0.036), and the presence of pelvic adhesions (β = 7.47, 95% CI: 0.67 to 14.27, p = 0.031) were significantly associated with prolonged operative time. Conversely, surgeries performed by more senior surgeons were associated with shorter operative durations (β = −14.26, 95% CI: −24.62 to −3.90, p = 0.007). Specifically, each 1 kg/m2 increase in BMI was associated with an approximately 1.7-min increase in procedure time; each level of severity of pelvic adhesions prolonged surgery by approximately 7.5 min; and each 1 cm increase in maximum fibroid diameter extended operative time by approximately 4.7 min. Other factors, including patient age, history of pelvic surgery, fibroid location (posterior wall), and surgical approach (single- vs. dual-port laparoscopy), were not independently associated with procedure duration.
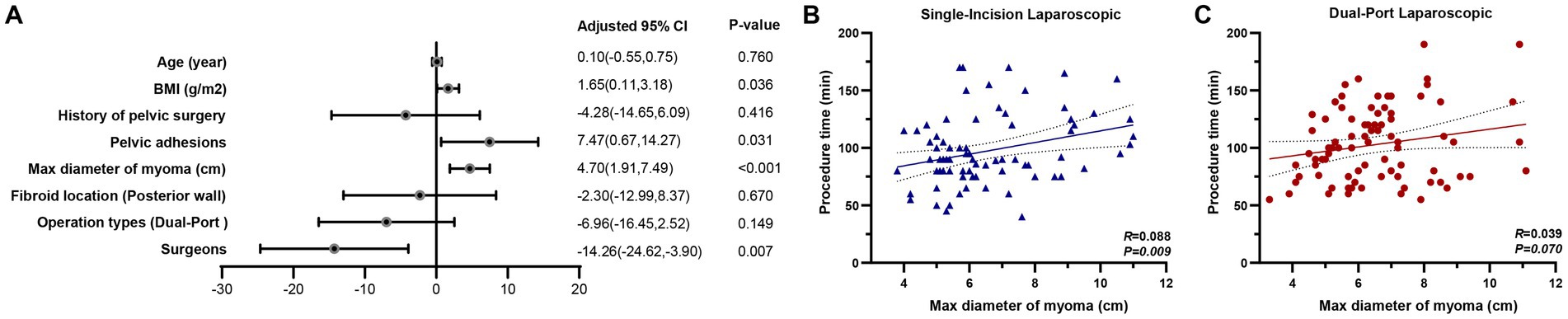
Figure 2. Impact of perioperative characteristics on procedure time. (A) In the multivariate linear regression analysis, larger fibroid size (β = 4.70, 95% CI: 1.91 to 7.49, p < 0.001), higher body mass index (BMI) (β = 1.65, 95% CI: 0.11 to 3.18, p = 0.036), and the presence of pelvic adhesions (β = 7.47, 95% CI: 0.67 to 14.27, p = 0.031) were significantly associated with prolonged operative time. In contrast, surgeries performed by more senior surgeons were associated with shorter operative durations (β = −14.26, 95% CI: −24.62 to −3.90, p = 0.007). (B) Subgroup analyses stratified by surgical approach revealed differential associations between fibroid size and operative time. A significant positive correlation was observed between the maximum diameter of fibroid and procedure time in the single-incision laparoscopic group (R = 0.088, p = 0.009). (C) However, this association was not statistically significant in the dual-port laparoscopic group (R = 0.039, p = 0.070), suggesting that dual-port laparoscopy may attenuate the operative time increase typically associated with larger fibroid size.
Subgroup analyses stratified by surgical approach revealed differential associations between fibroid size and operative time. As illustrated in Figure 2B, a significant positive correlation was observed between the maximum diameter of fibroid and procedure time in the single-incision laparoscopic group (R = 0.088, p = 0.009). However, this association was not statistically significant in the dual-port laparoscopic group (R = 0.039, p = 0.070; Figure 2C), suggesting that dual-port laparoscopy may attenuate the operative time increase typically associated with larger fibroid size.
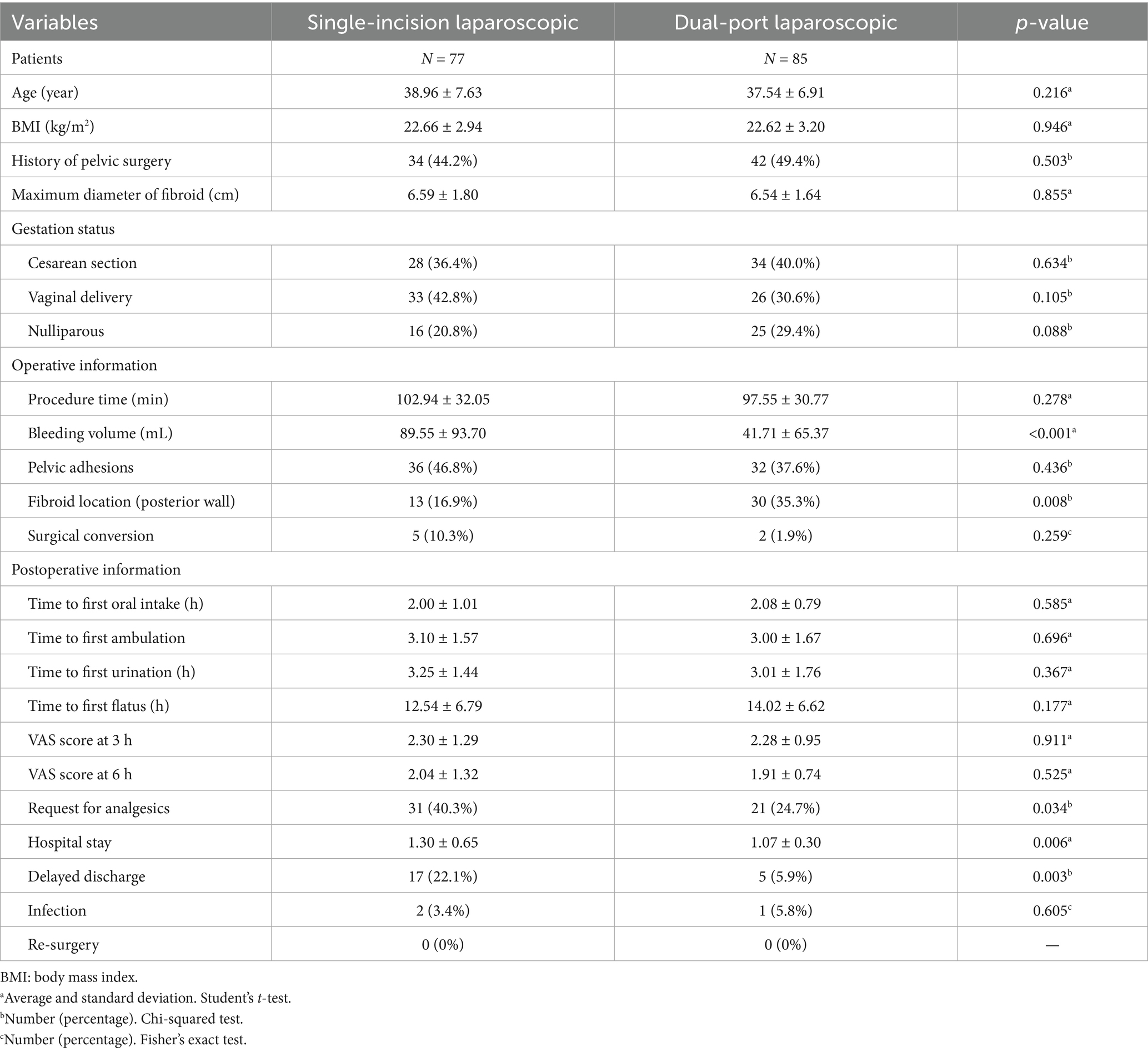
Factors associated with intraoperative blood loss were explored using multivariate linear regression analysis, as shown in Table 2. The results showed that operation type (β = 48.18, 95% CI: 23.15 to 73.22, p < 0.001) and procedure time (β = 0.75, 95% CI: 0.33 to 1.17, p = 0.001) were significantly associated with increased bleeding. Specifically, undergoing single-incision laparoscopy (reference: dual-port) was associated with an estimated 48.18 mL increase in blood loss, and each additional minute of procedure time resulted in approximately 0.75 mL of additional bleeding. Other variables, including age, BMI, surgical history, pelvic adhesions, fibroid size, fibroid location, and surgeon experience, were not significantly associated with bleeding volume (all p > 0.05).
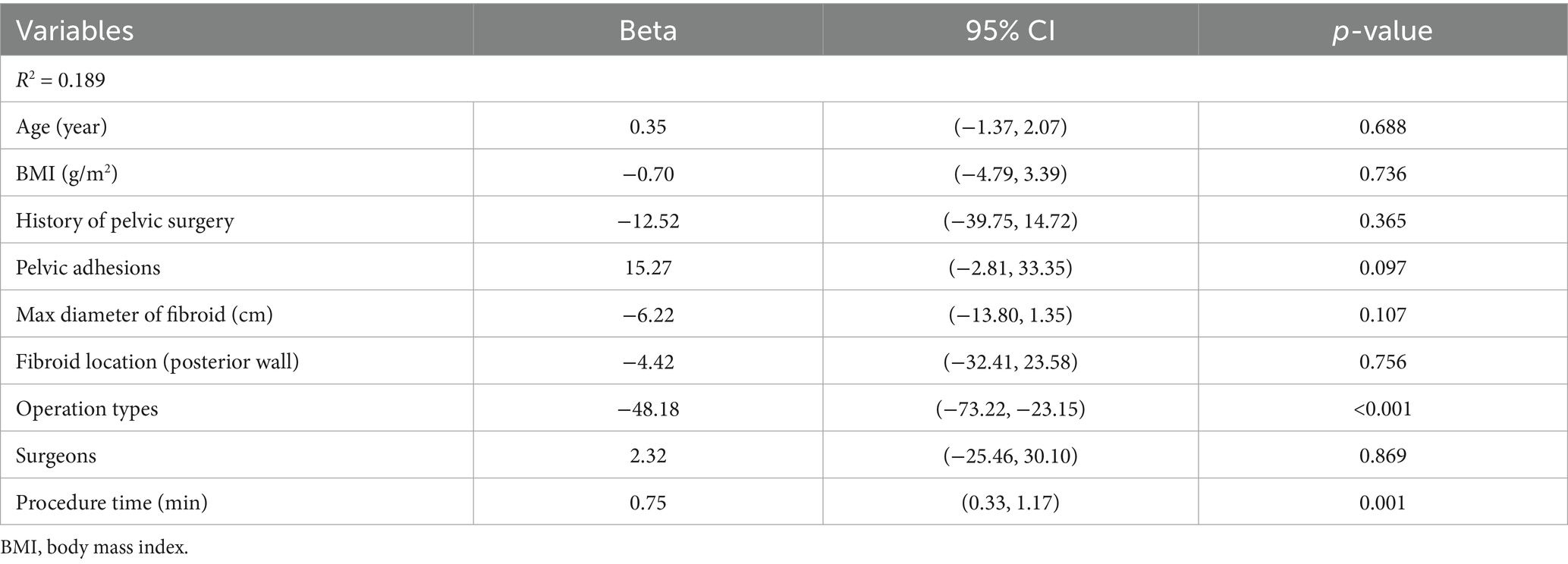
The multivariate logistic regression analysis identifying predictors of postoperative analgesic medication use is summarized in Table 3. Among the variables examined, only fibroid location on the posterior uterine wall was significantly associated with increased odds of requiring postoperative analgesics (OR = 2.97, 95% CI: 1.31–6.77, p = 0.009). This indicates that patients with posterior wall fibroids were approximately three times more likely to require analgesic medication after surgery compared to those with fibroids in other locations. Other factors, including age, BMI, history of pelvic surgery, procedure time, intraoperative bleeding volume, presence of pelvic adhesions, fibroid size, surgical approach, and surgeon experience, were not significantly associated with postoperative analgesic use (p > 0.05 for all).
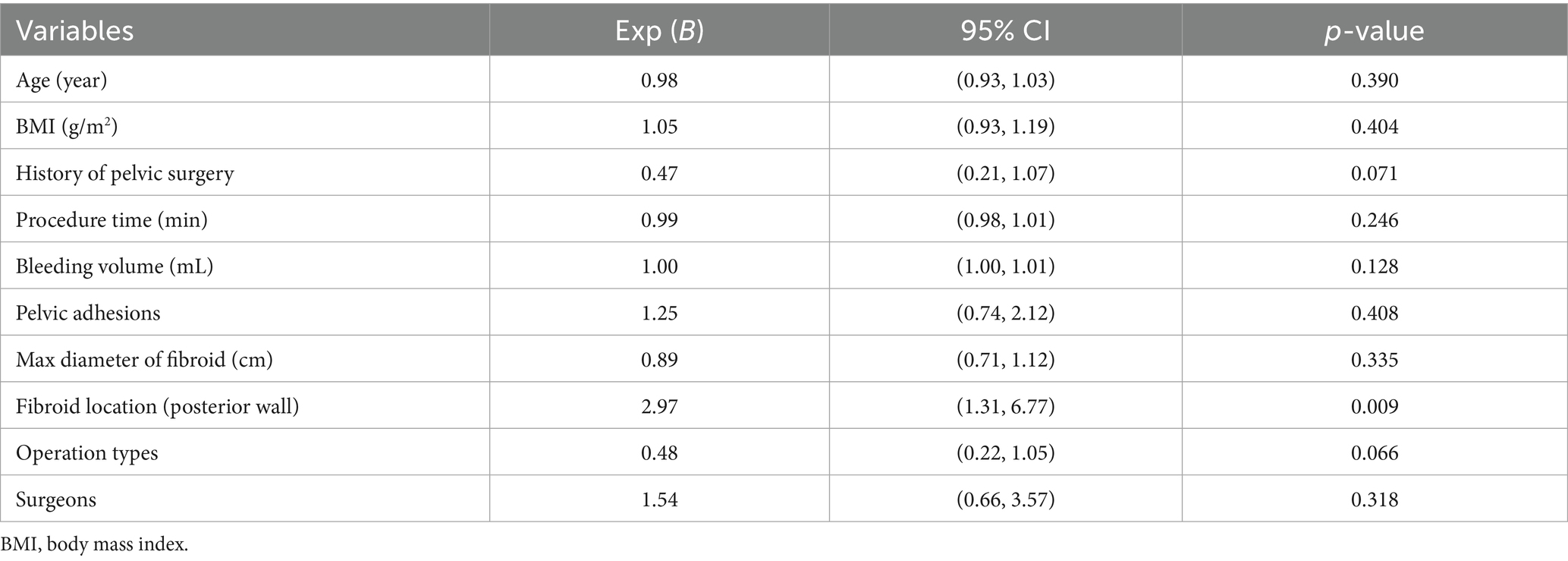
Table 3. Association between postoperative analgesic medication use and perioperative characteristics.
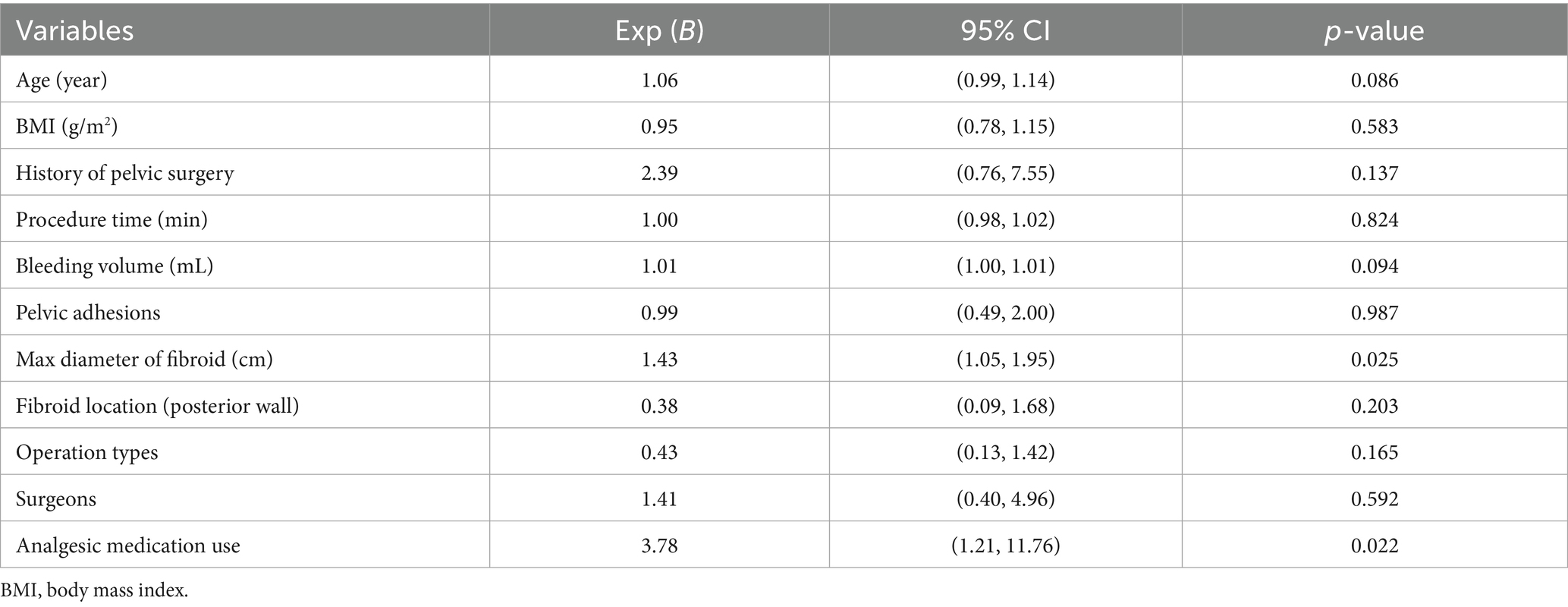
Table 4 shows the results of the multivariate logistic regression analysis assessing factors associated with delayed hospital discharge. Two factors were found to be independently associated with an increased risk of delayed discharge. First, a larger maximum diameter of fibroid was significantly correlated with delayed discharge (OR = 1.43, 95% CI: 1.05–1.95, p = 0.025), indicating that each 1 cm increase in fibroid size was associated with a 43% increase in the odds of prolonged hospitalization. Second, postoperative use of analgesic medication was also significantly associated with delayed discharge (OR = 3.78, 95% CI: 1.21–11.76, p = 0.022), suggesting that patients who required postoperative analgesics were approximately four times more likely to experience delayed discharge. Other perioperative variables—including age, BMI, pelvic surgical history, pelvic adhesions, intraoperative blood loss, procedure time, fibroid location, operation type, and surgeon—were not significantly associated with discharge timing (p > 0.05 for all).
Figure 3 compares the instrument configuration and postoperative incision appearance between single-incision and dual-port laparoscopic approaches. Figure 3A illustrates the instrument configuration in the single-incision laparoscopic approach, where all instruments are inserted through a single umbilical port. This setup results in limited triangulation and a narrower operative angle, which may restrict instrument maneuverability. In contrast, Figure 3B demonstrates the dual-port laparoscopic approach, in which the use of two separate ports enables a wider triangular working space, thereby enhancing surgical precision and ease of operation. Figures 3C,D show the healing status of the umbilical and auxiliary port incisions 1 week after dual-port laparoscopic surgery. The auxiliary incision is relatively small, indicating limited impact on surgical trauma and postoperative cosmetic appearance.
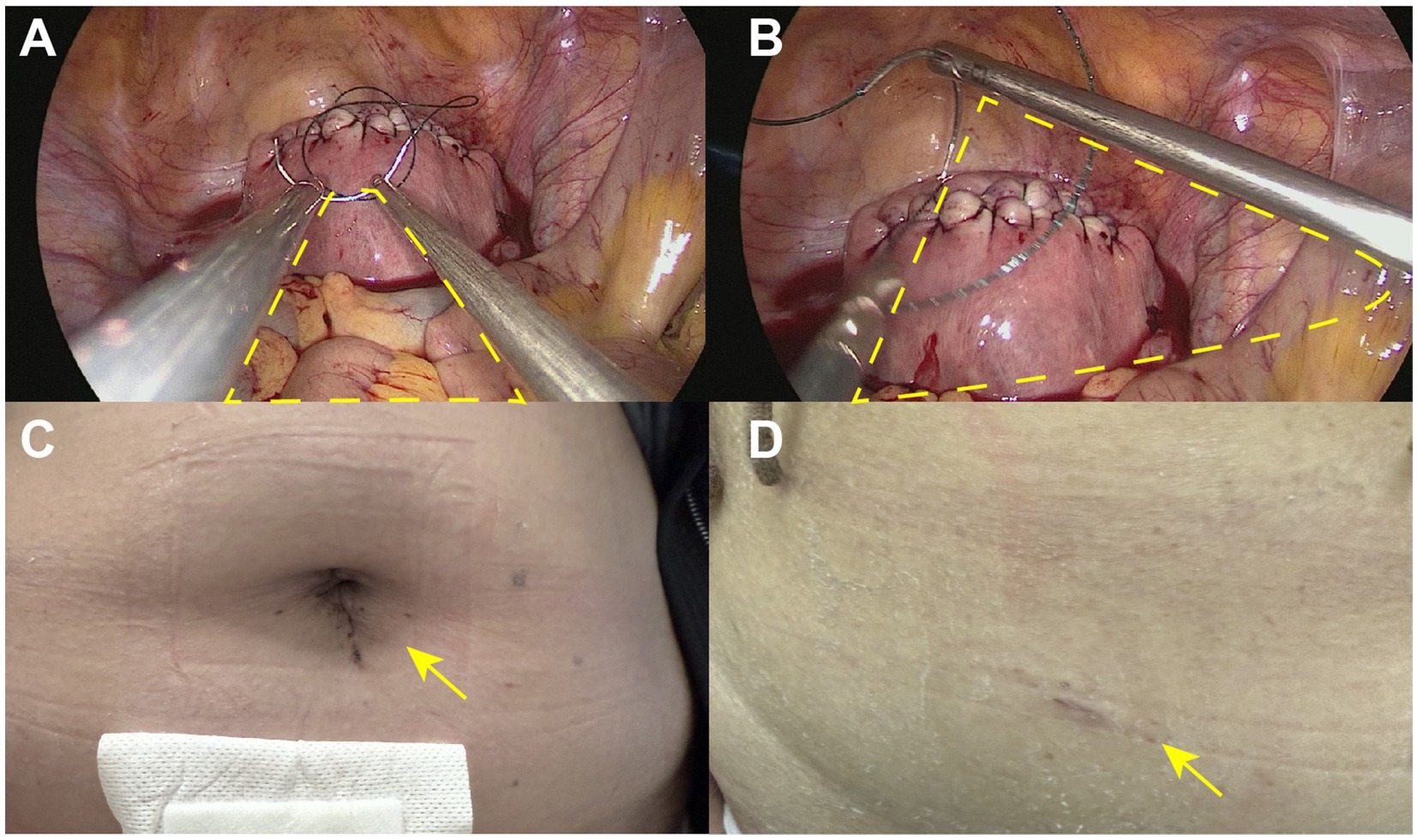
Figure 3. Instrument configuration and postoperative incision appearance between single-incision and dual-port laparoscopic approaches. (A) The instrument configuration in the single-incision laparoscopic approach, where all instruments are inserted through a single umbilical port. This setup results in limited triangulation and a narrower operative angle, which may restrict instrument maneuverability. (B) The dual-port laparoscopic approach, in which the use of two separate ports enables a wider triangular working space, thereby enhancing surgical precision and ease of operation. (C,D) The healing status of the umbilical and auxiliary port incisions 1 week after dual-port laparoscopic surgery.
Discussion
This study compared the perioperative outcomes of single-incision laparoscopic myomectomy (SILS) and dual-port laparoscopic myomectomy in patients with solitary uterine fibroids. The findings indicate that while both approaches are feasible and safe, the dual-port technique offers advantages in terms of reduced intraoperative blood loss, lower postoperative analgesic requirements, and shorter hospital stay, particularly in patients with larger fibroids or posterior wall lesions.
A key observation was that the single-incision approach was independently associated with increased intraoperative bleeding volume, even after adjusting for fibroid size and procedure time. This may be attributed to the ergonomic limitations of SILS, which include reduced triangulation, limited instrument range of motion, and suboptimal visualization in certain uterine positions (17, 18). In contrast, the dual-port technique—by allowing a more favorable triangular configuration—enhances the surgeon’s ability to dissect, cauterize, and suture more efficiently, thereby contributing to better hemostatic control. These findings are consistent with prior reports in the gynecologic surgery literature, which have demonstrated that limited access angles in SILS can compromise operative precision and increase blood loss, particularly in complex procedures such as myomectomy (19, 20).
Moreover, the analysis revealed that posterior wall fibroids were significantly associated with increased postoperative analgesic use. This likely reflects the greater surgical difficulty involved in accessing and excising fibroids located in the posterior uterus, especially through a single umbilical port (21, 22). Notably, the dual-port configuration seems to mitigate this difficulty, as suggested by the absence of a significant correlation between fibroid size and operative time in the dual-port group, in contrast to the SILS group, where a clear positive association was observed (23). These results highlight the utility of the auxiliary port in improving exposure and reducing surgeon stress during challenging dissections.
Another important outcome of this study was the association between larger fibroid diameter and delayed hospital discharge. While this finding may partly reflect increased surgical complexity and recovery burden, it also underscores the need to consider fibroid characteristics when selecting the most appropriate surgical approach. In addition, postoperative analgesic use independently predicted prolonged hospitalization, which is in line with previous studies showing that postoperative pain not only delays mobilization but also affects gastrointestinal function and discharge readiness (24). The reduced analgesic requirement and shorter hospital stay observed in the dual-port group further support the ergonomic and clinical benefits of this approach.
From a cosmetic perspective, dual-port laparoscopy preserved excellent aesthetic outcomes. Although an additional incision was required, the auxiliary port was only 5 mm in diameter and showed minimal scarring 1 week after surgery. This suggests that dual-port laparoscopy offers a practical balance between surgical performance and patient satisfaction (25, 26). While SILS has traditionally been promoted for its superior cosmetic results, our findings indicate that the trade-off in technical difficulty and perioperative burden may outweigh its limited aesthetic advantage, especially in cases involving larger or posterior fibroids.
The strengths of this study include its focused cohort of patients with solitary fibroids, reducing confounding by fibroid number or uterine distortion, and its detailed multivariate modeling accounting for a range of anatomical and clinical factors. Furthermore, all surgeries were performed by experienced laparoscopic surgeons, minimizing variability due to technical proficiency. Photographic documentation of incision healing also provided an objective measure of cosmetic outcomes, which are increasingly valued by patients undergoing minimally invasive gynecologic surgery.
Nevertheless, several limitations should be acknowledged. First, the retrospective and non-randomized nature of the study introduces the possibility of selection bias. Although baseline characteristics were well balanced, surgeon preference likely influenced the choice of surgical approach. Second, the study was conducted at a single institution, potentially limiting generalizability to other clinical settings with different patient populations or surgical practices. Third, the absence of long-term follow-up data on fertility preservation, symptom recurrence, and adhesion formation, as well as the inability to perform propensity score matching due to limited sample size, further restrict the generalizability and causal inference of our findings. Fourth, our findings may not be generalizable to women with multiple fibroids or complex pelvic anatomy, who were not included in this study. Future prospective or randomized controlled trials are needed to further confirm the results of this study.
Conclusion
In summary, dual-port laparoscopic myomectomy appears to offer a balanced and potentially more optimal alternative to single-incision surgery, particularly in cases with larger fibroids or posterior uterine wall involvement. It combines the minimally invasive advantages of SILS with enhanced operative ergonomics and improved perioperative outcomes. These findings support the broader clinical adoption of dual-port techniques in appropriate patients and suggest that individualized surgical planning—taking into account fibroid characteristics, patient anatomy, and surgeon expertise—remains critical to optimizing outcomes in minimally invasive myomectomy.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by the Institutional Ethics Committee of Chengdu Women’s and Children’s Central Hospital (No. 2022207), and informed consent was obtained from all participants prior to surgery. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
YiL: Writing – review & editing, Writing – original draft. QZ: Writing – review & editing, Writing – original draft. BH: Writing – review & editing, Writing – original draft. XLi: Writing – review & editing, Writing – original draft. TL: Writing – original draft, Writing – review & editing. LX: Writing – original draft, Writing – review & editing. XLia: Writing – review & editing, Writing – original draft. JL: Writing – original draft, Writing – review & editing. WC: Writing – original draft, Writing – review & editing. HW: Writing – original draft, Writing – review & editing. JH: Writing – review & editing, Writing – original draft. TW: Writing – review & editing, Writing – original draft. YaL: Writing – review & editing, Writing – original draft. JY: Writing – original draft, Writing – review & editing. YoL: Writing – review & editing, Writing – original draft. XG: Writing – review & editing, Writing – original draft.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. Financial support of this work was provided by Chengdu Science and Technology Bureau (Nos. 2021-YF0500530-SN and 2021-YF0500868-SN), National Natural Science Foundation of China (82071651), National Key Research and Development Program (2022YFC3600304 and 2022YFC2704700), National Key Clinical Specialty Construction Project (Obstetrics and Gynecology, 2022), and Sichuan Provincial Department of Science and Technology (2023YFS0219 and 2023YFS0228).
Acknowledgments
The authors would like to thank all the participants and researchers who contributed to this cohort study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2025.1617194/full#supplementary-material
References
1. Kim, HM, and Chung, C. The integrative health status of women with uterine fibroids wishing to maintain fertility: a cross-sectional study based on Levine’s conservation model. Womens Health Nurs. (2025) 31:9–21. doi: 10.4069/whn.2025.03.02
2. Charifson, M, Beaton-Mata, G, Lipschultz, R, Robinson, I, Sasse, SA, Hur, HC, et al. Using electronic health record data to identify incident uterine fibroids and endometriosis within a large, urban academic medical center: a validation study. Am J Epidemiol. (2025):kwaf058. doi: 10.1093/aje/kwaf058
3. Bulun, SE, Yin, P, Wei, JJ, Zuberi, A, Iizuka, T, Suzuki, T, et al. Uterine fibroids. Physiol Rev. (2025) 105:1947–88. doi: 10.1152/physrev.00010.2024
4. Ahmad, F, Khan, AI, Asif, A, Ahmed, S, Nisar, M, Fatima, E, et al. Clinical efficacy of percutaneous microwave ablation in treating uterine fibroids: a comprehensive systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol. (2025) 310:113954. doi: 10.1016/j.ejogrb.2025.113954
5. Yamanishi, Y, Kotani, Y, Kido, A, Otani, T, Himoto, Y, Kurata, Y, et al. Differentiation of uterine fibroids and sarcomas by MRI and serum LDH levels: a multicenter study of the KAMOGAWA study. J Gynecol Oncol. (2025) 36:e58. doi: 10.3802/jgo.2025.36.e58
6. Puscasiu, L, Vollenhoven, B, Nagels, HE, Melinte, IM, Showell, MG, and Lethaby, A. Preoperative medical therapy before surgery for uterine fibroids. Cochrane Database Syst Rev. (2025) 4:CD000547. doi: 10.1002/14651858.CD000547.pub2
7. Marlina, D, Utomo, A, Susilo, AFP, Aditiyono, A, Adriansyah, PNA, and Aziz, MA. An unusual and successful pregnancy with multiple large uterine fibroids delivered by cesarean myomectomy. J Med Cases. (2025) 16:95–101. doi: 10.14740/jmc5073
8. Sami Walid, M, and Heaton, RL. The role of laparoscopic myomectomy in the management of uterine fibroids. Curr Opin Obstet Gynecol. (2011) 23:273–7. doi: 10.1097/GCO.0b013e328348a245
9. Geschwind, JF, Afsari, B, Nezami, N, White, J, Shor, M, and Katsnelson, Y. Quality of life assessment after uterine artery embolization in patients with fibroids treated in an ambulatory setting. Diagnostics. (2025) 15:739. doi: 10.3390/diagnostics15060739
10. Peregrino, PFM, Messina, ML, Junior, JMS, and Baracat, EC. Magnetic resonance-guided focused ultrasound for uterine fibroids. Clinics. (2025) 80:100603. doi: 10.1016/j.clinsp.2025.100603
11. Chen, Y, Yi, J, Lin, S, Xie, X, Liu, X, and Guo, SW. Reproductive outcomes of high-intensity focused ultrasound ablation and myomectomy for uterine fibroids: a systematic review and meta-analysis. Reprod Biomed Online. (2025) 50:104436. doi: 10.1016/j.rbmo.2024.104436
12. Cottrell, CM, and Stewart, EA. Use of uterine artery embolization for the treatment of uterine fibroids: a comparative review of major national guidelines. J Minim Invasive Gynecol. (2024) 32:418–24. doi: 10.1016/j.jmig.2024.11.006
13. Zhu, W, Mao, S, Chen, Y, and Kong, X. Analysis of clinical efficacy of laparoendoscopic single-site surgery for uterine fibroids. J Healthc Eng. (2022) 2022:5606998. doi: 10.1155/2022/5606998
14. Cheng, W, Li, X, Liu, T, Xie, A, Wu, X, Liao, J, et al. Transvaginal natural orifice transluminal endoscopic surgery for myomectomy: a more suitable surgical approach for enhanced recovery after surgery. Eur J Obstet Gynecol Reprod Biol. (2024) 295:143–9. doi: 10.1016/j.ejogrb.2024.02.005
15. Hou, Q, Li, X, Huang, L, Xiong, Y, Feng, D, Zhang, Q, et al. Transvaginal natural orifice endoscopic surgery for myomectomy: can it be a conventional surgery? Front Surg. (2022) 9:1013918. doi: 10.3389/fsurg.2022.1013918
16. Hou, Q, Li, X, Li, Y, Zhang, Q, Liu, T, Huang, L, et al. Analysis and suggestions on the complications in 2000 cases of transvaginal natural orifice transluminal endoscopic surgery: can it be a conventional surgery? Int J Gynaecol Obstet. (2024) 164:541–9. doi: 10.1002/ijgo.15035
17. Jiang, Z, Jia, S, Zhang, J, Liu, C, Luo, X, Tang, Y, et al. Preoperative identification from occult leiomyosarcomas in laparoscopic hysterectomy and laparoscopic myomectomy: accuracy of the ultrasound scoring system (PRESS-US). Radiol Med. (2024) 129:1864–75. doi: 10.1007/s11547-024-01903-x
18. Kathopoulis, N, Prodromidou, A, Douligeris, A, Diakosavvas, M, Zacharakis, D, Kypriotis, K, et al. Barbed sutures compared with conventional sutures during laparoscopic myomectomy: a systematic review and meta-analysis. Obstet Gynecol. (2024) 144:e81–e100. doi: 10.1097/AOG.0000000000005695
19. Deipolyi, AR, Annie, F, Bush, SH 2nd, and Spies, J. Hysterectomy and myomectomy vs uterine artery embolization for symptomatic fibroids and adenomyosis: national and regional trends and adverse events in 70,000 patients. J Vasc Interv Radiol. (2025) 36:1011–1018.e4. doi: 10.1016/j.jvir.2025.02.026
20. Choi, SH, Won, S, Lee, N, Shim, SH, Kim, MK, Kim, ML, et al. Robotic single-site plus one-port myomectomy versus robotic single-site plus two-port myomectomy: a propensity score matching analysis. Yonsei Med J. (2024) 65:406–12. doi: 10.3349/ymj.2023.0434
21. Niu, G, Zhao, H, Wang, H, Zhao, L, and Zhai, Y. Single-incision plus one port laparoscopic surgery for myomectomy: a retrospective study. J Investig Surg. (2023) 36:2221738. doi: 10.1080/08941939.2023.2221738
22. Sabt, FY, Isa, HM, Khudair, ZA, Khedr, EE, Alkhan, FA, and Hammad, JS. Incidence and predictors of unexpected malignancy in benign myomectomy or hysterectomy. Cureus. (2024) 16:e66880. doi: 10.7759/cureus.66880
23. Lee, N, Choi, SH, Won, S, Jung, YW, Kim, SH, Lee, JY, et al. Comparison of surgical outcomes of two new techniques complementing robotic single-site myomectomy: coaxial robotic single-site myomectomy vs. hybrid robotic single-site myomectomy. J Pers Med. (2024) 14:439. doi: 10.3390/jpm14040439
24. Wu, YC, Hong, MK, and Ding, DC. Comparison of postoperative pain in robotic and laparoscopic myomectomy: a retrospective cohort study. J Robot Surg. (2024) 18:345. doi: 10.1007/s11701-024-02105-3
25. Lee, SY, Lee, SR, and Song, JY. Single-port versus reduced-port (1 + 1) robotic myomectomy and hysterectomy. J Clin Med. (2024) 13:6563. doi: 10.3390/jcm13216563
Keywords: dual-port laparoscopy, single-incision laparoscopy, myomectomy, minimally invasive surgery, perioperative outcomes
Citation: Liu Y, Zhang Q, Huang B, Li X, Liu T, Xu L, Liao X, Liao J, Cheng W, Wang H, Huang J, Wu T, Liu Y, Yu J, Lin Y and Gan X (2025) Dual-port laparoscopic myomectomy: a balanced yet potentially more optimal surgical approach. Front. Med. 12:1617194. doi: 10.3389/fmed.2025.1617194
Edited by:
Antonio Simone Laganà, University of Palermo, ItalyReviewed by:
Myriam Jerbaka, Saint Joseph University, LebanonTongfu Feng, Huazhong University of Science and Technology, China
Copyright © 2025 Liu, Zhang, Huang, Li, Liu, Xu, Liao, Liao, Cheng, Wang, Huang, Wu, Liu, Yu, Lin and Gan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yonghong Lin, bGlueWhjZDIwMTFAMTYzLmNvbQ==; Xiaoqin Gan, YW1hbmRpbmUyMDIxQDE2My5jb20=
†These authors have contributed equally to this work
 Ying Liu1†
Ying Liu1† Qiang Zhang
Qiang Zhang Xin Li
Xin Li Juan Huang
Juan Huang Yonghong Lin
Yonghong Lin