- 1Department of Traditional Chinese Medicine, Peking University Third Hospital, Beijing, China
- 2Dongzhimen Hospital, Beijing University of Chinese Medicine, Beijing, China
Introduction: Post-COVID syndrome is characterized by persistent, unexplained symptoms including chronic cough, palpitations, insomnia, and fatigue that develop following SARS-CoV-2 infection without identifiable causes. Current treatments show limited efficacy, requiring alternative options. This study aims to observe the effectiveness of Five-Element Regulation Therapy (FERT), a Traditional Chinese medicine (TCM) intervention, in managing post-COVID syndrome.
Methods: A retrospective cohort study was conducted using clinical records of 127 post-COVID syndrome patients from the TCM outpatient department of Peking University Third Hospital. The participants were divided into two groups: 81 cases receiving FERT treatment were assigned to the exposure group, while 46 cases undergoing conventional TCM therapy served as the control group. The treatment duration was 2 weeks for both groups, followed by immediate follow-up. The outcomes included the clinical cure rate and clinical response rate at 2 weeks after the treatment initiation.
Results: The FERT group demonstrated superior clinical outcomes, achieving a 61.7% cure rate and 88.9% response rate, significantly higher than the control group’s 21.7% (p < 0.001) and 67.4% (p < 0.01), respectively.
Conclusion: This study provides preliminary evidence that FERT may be superior to conventional TCM therapy in managing post-COVID syndrome. Results should be interpreted with heightened caution due to the study’s inherent limitations.
1 Introduction
While the global COVID-19 pandemic has been declared over, its various sequelae continue to afflict the physical and mental health of a large number of patients in China (1–6). A systematic review covered 194 studies and 735,006 participants found that the five most common symptoms of post-COVID infection were fatigue (28.4%), pain/discomfort (29.7%), sleep disturbances (23.5%), breathing difficulties (22.6%), and activity limitations (22.3%) (7). A recent large-scale study on COVID-19 sequelae provided a systematic definition of “long COVID” for the first time (8). The research found that approximately 10% of individuals develop long COVID after infection with the Omicron variant, with up to 12 different symptoms including fatigue, cough, palpitations, hair loss, loss of sense of smell and taste, brain fog, chest pain, and changes in libido.
Current scientific understanding of long COVID suggests a complex, multi-system condition, with symptoms persisting for months or even years after the initial infection. The mechanisms remain incompletely understood but involve multiple interconnected pathways, including viral persistence (9), chronic inflammation (10), endothelial damage (11), mitochondrial (12), and autonomic nervous system dysregulation (13). Additionally, SARS-CoV-2’s broad tissue tropism via ACE2 receptors contributes to multi-organ damage, with cardiovascular, pulmonary, and metabolic sequelae being particularly prevalent (14). Emerging evidence also highlights the overlap with post-infectious syndromes, characterized by post-exertional malaise and unrefreshing sleep, with COVID-19 increasing the risk of post-infectious syndromes (15).
Current treatments for long COVID being investigated in clinical trials include non-pharmacological interventions such as physical exercise, rehabilitation therapy, and behavioral therapy, as well as pharmacological therapies like herbs, Paxlovid, and fluvoxamine (16). Psychological interventions like “awe therapy” also demonstrate benefits in reducing depression and stress (17). However, targeted and clinically proven therapies remain limited, with most current approaches focusing primarily on symptom management rather than treating the root pathological mechanisms.
Traditional Chinese Medicine (TCM) formulations including Shenhuang granule (18), JingYinGuBiao Formula (19), and Bufei Huoxue capsules (20) have demonstrated therapeutic potential in COVID-19 management within the Chinese clinical context. In the treatment of post-COVID sequelae, these TCM formulations have also exhibited significant therapeutic potential (21). Five-Element Regulation Therapy (FERT) is a set of therapeutic methods summarized by our team based on the theory of TCM constitution and clinical practice (22, 23). It classifies patients into five syndrome types (wood, fire, earth, metal, water) according to different main symptoms, and adopts different treatment approaches for groups with different syndrome types. Our research team has employed FERT for post-COVID syndrome management and observed certain therapeutic effects in case studies. However, these preliminary findings remain at the anecdotal evidence level and cannot provide evidence-based support for FERT’s clinical application in post-COVID treatment. To investigate the clinical effects of FERT in managing post-COVID symptoms, we conducted a retrospective cohort study analyzing its application at the COVID Recovery Clinic within the Department of Traditional Chinese Medicine at Peking University Third Hospital.
2 Materials and methods
2.1 Study design
The research conducted a retrospective analysis on patients with post-COVID-19 sequelae who received outpatient care at the Department of Traditional Chinese Medicine in Peking University Third Hospital. The research period extended from January 1, 2023, to May 31, 2023, during which all patients underwent TCM treatment. Patients receiving FERT intervention were assigned to the experimental group, while those undergoing conventional TCM treatment served as the control group. Patients were followed up at 2-weeks post-treatment to document symptom alleviation levels. Ethical approval was obtained from the Peking University Third Hospital Medical Science Research Ethics Committee (No. S2023541), and the study adhered to the principles of the Declaration of Helsinki.
2.2 Patients
Eligible patients were stratified into exposure and control groups, with FERT serving as the exposure factor-the experimental group received FERT intervention while the control group underwent conventional TCM treatment. Both patient groups maintained medication regimens for 2 weeks, with continuous treatment unless complete symptom resolution was achieved. This study imposed no gender-based restrictions on participant eligibility.
2.3 Inclusion and exclusion criteria
The inclusion criteria included: (1) Patients with a confirmed history of COVID-19 diagnosis verified by either PCR testing or SARS-CoV-2 antibody detection. (2) The interval between COVID-19 diagnosis and the current visit must be at least 1 month. (3) Symptoms such as cough, breathlessness, panic, palpitations, chest tightness, sleep disturbances, anxiety and depression, chronic fatigue, lumbar and knee pain can be caused by COVID infection. (4) Age ≥ 18 years.
The exclusion criteria were as follows: (1) Patients with less than 5 days of TCM treatment. (2) Patients with secondary infections. (3) Pregnant or lactating women.
2.4 Exposure and control
All participants in this study received TCM interventions. The experimental group was treated with FERT-based herbal formulations, while the control group received conventional TCM therapy guided by syndrome differentiation. For instance, Xiao Qing Long Tang was prescribed for cough, while Jiao Tai Wan was utilized for insomnia in the control group. The FERT group received customized Chinese herbal formulas and the control group was given either individualized herbal decoctions or standard Chinese patent medicines. Dosages followed conventional guidelines: herbal decoctions were prepared at standard therapeutic doses, while patent medicines were administered according to manufacturer-recommended dosages.
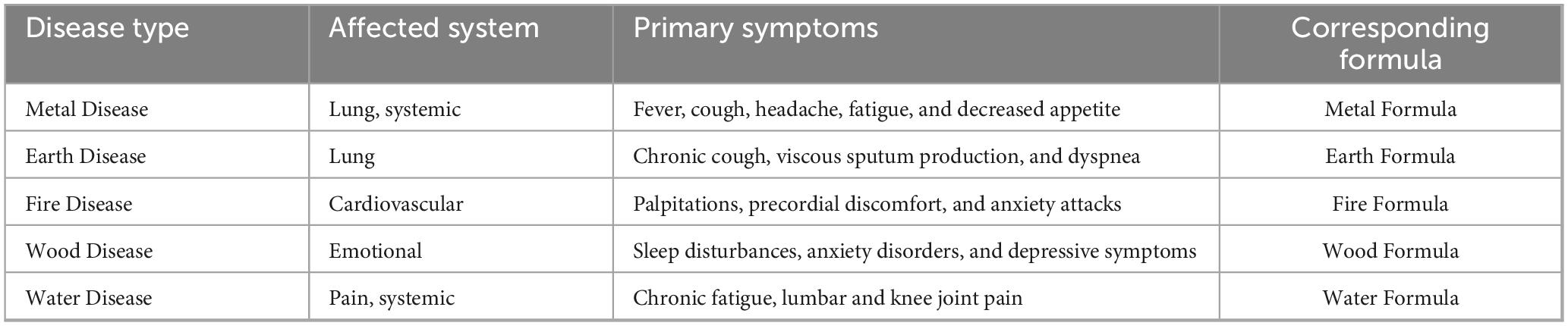
Patients in the FERT group were classified into five distinct categories according to their clinical manifestations. In the earliest stage of diseases, they are classified as Metal Disease in FERT therapy, characterized primarily by fever with accompanying symptoms including cough, headache, fatigue and decreased appetite. Respiratory symptoms, including chronic cough, viscous sputum production, and dyspnea, were classified as Earth Disease. Cardiac symptoms such as palpitations, precordial discomfort, and anxiety attacks were categorized as Fire Disease. The Wood Disease classification encompassed sleep disturbances, anxiety disorders, and depressive symptoms, while Water Disease included chronic fatigue syndrome along with lumbar and knee joint pain. The standard FERT formulations were appropriately modified based on individual symptom patterns (Table 1). Detailed compositions of the modified herbal formulations are provided in Supplementary Tables 1–4. All herbal materials were sourced from Peking University Third Hospital (Beijing, China). The treatment protocol consisted of one daily dose, administered twice daily (morning and evening) as 200 mL decoctions. The standard therapeutic course was established at 2 weeks, with a minimum required treatment duration of 5 consecutive days.
2.5 Follow-up
Clinical data were collected via outpatient follow-up consultations and retrospective medical record reviews. The dataset encompassed: (1) demographic characteristics, (2) consultation timelines, (3) comprehensive symptom profiles, (4) dates of COVID-19 diagnosis confirmation, and (5) longitudinal tracking of significant symptom improvement. Follow-up assessments were conducted at the 2-weeks post-consultation interval to document symptomatic relief outcomes.
2.6 Outcomes
The primary outcome measures of this study were clinical cure rate and clinical response rate. A patient was considered clinically cured if all COVID-19 sequelae completely resolved during the observation period. Clinical response was defined as symptomatic improvement with residual minor symptoms, while treatment failure was determined if symptoms showed no improvement or worsened. Patients who were lost to follow-up or non-compliant were classified as dropout cases. Clinical cure rate (%) = (Number of clinically cured cases/Total cases) × 100%. Clinical response rate (%) = [(Clinically cured cases + Cases with clinical response)/Total cases] × 100%.
2.7 Statistical analysis
The data was statistically analyzed using the GraphPad Prism 9.5.1 software. For normally distributed measurements, the mean ± standard deviation was reported, and independent samples t-test was performed. Frequencies and percentages were reported for counts, and x2 test was used. Fisher’s exact probability method was used if the theoretical value of T was less than 1 or the total number of samples n was less than 40. Differences were considered statistically significant at p < 0.05.
3 Results
3.1 Patient characteristics
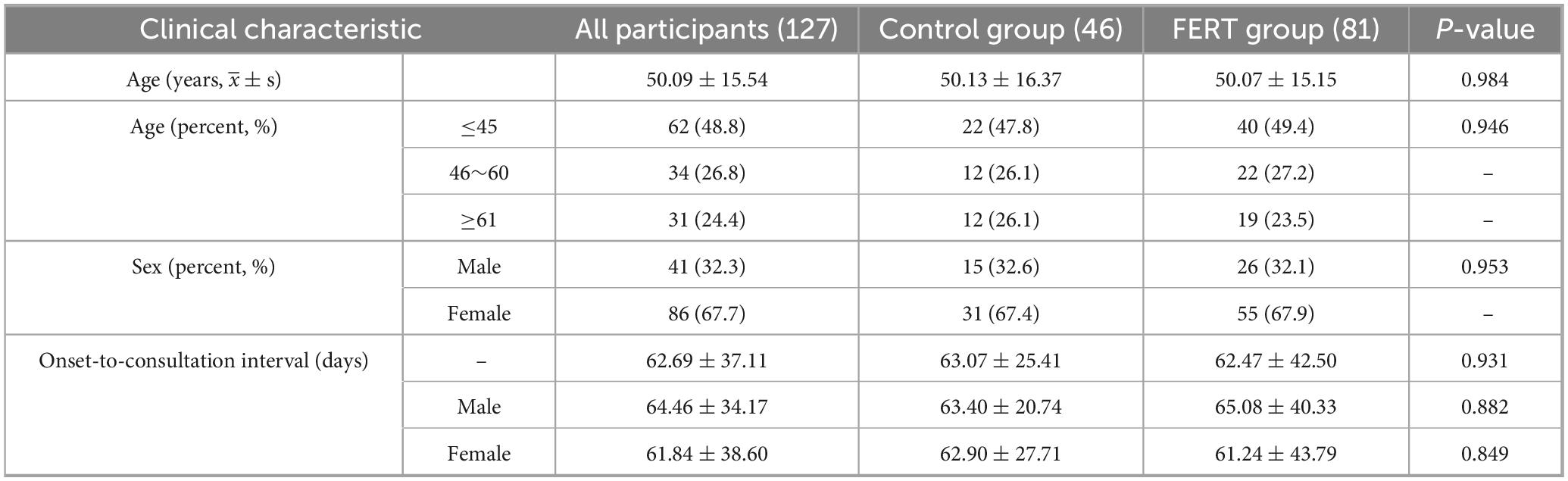
According to the inclusion and exclusion criteria, 127 patients were eventually enrolled in the study. The study flow chart is shown in Figure 1. There were 81 cases in the FERT group and 46 cases in the control group. The baseline clinicopathological characteristics of the patients are described in Table 2. No significant differences were observed in baseline characteristics, including age, gender, and onset-to-consultation interval between the two groups (p = 0.984, 0.953, and 0.931, respectively).
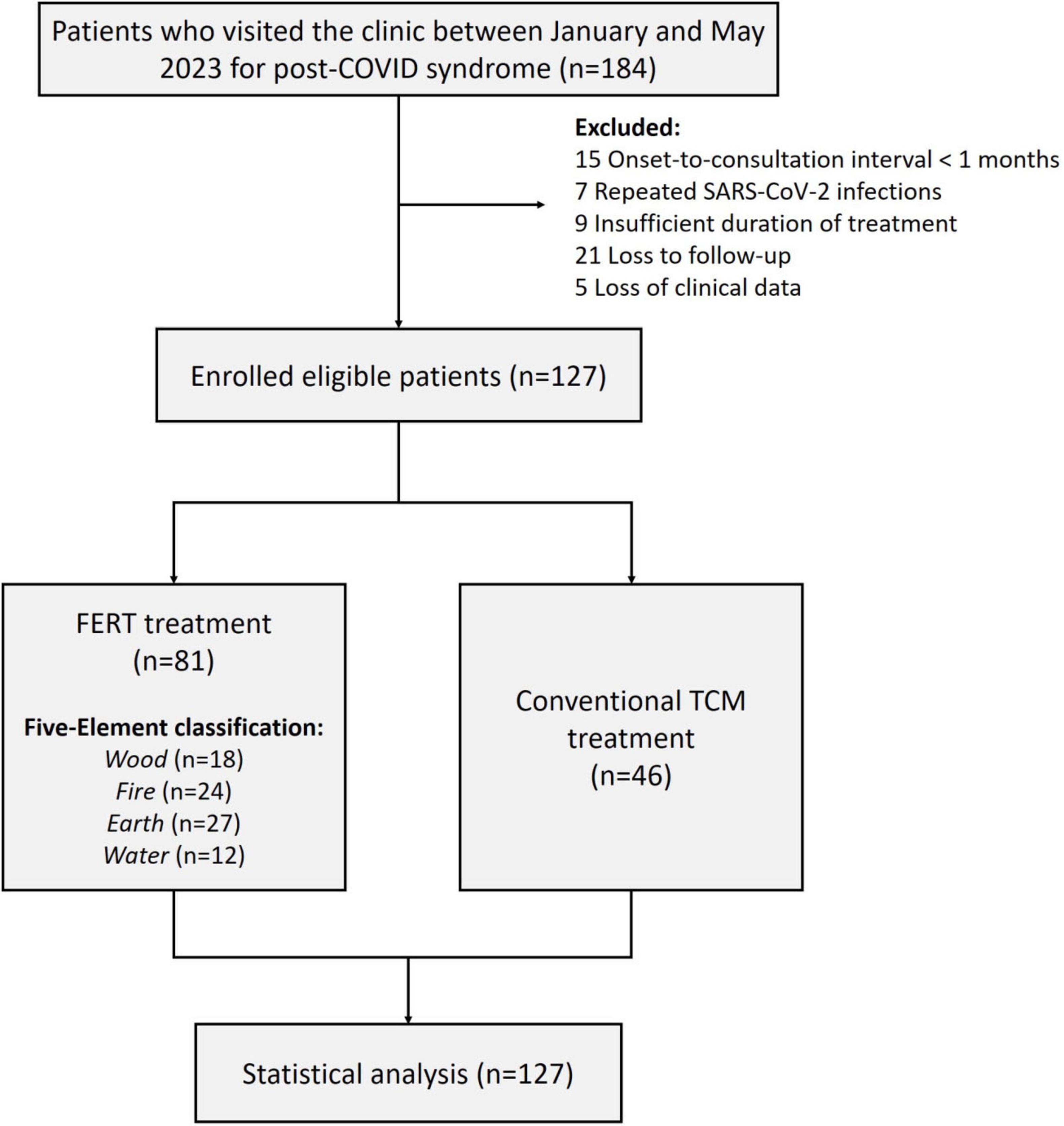
Figure 1. Flowchart of the study. FERT, Five-Element Regulation Therapy; TCM, Traditional Chinese Medicine.
3.2 Outcomes
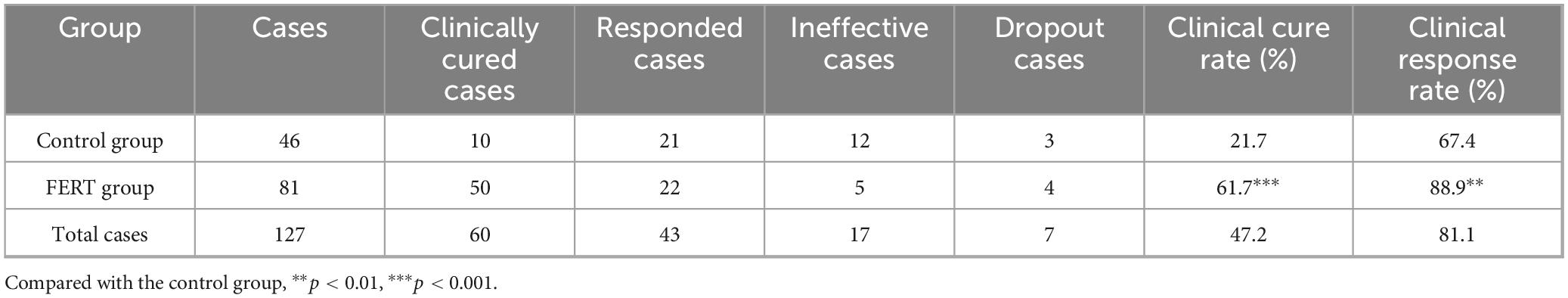
The clinical outcomes of both groups are shown in Table 3. The clinical cure rate and response rate were significantly better in the FERT group compared to the control group (p < 0.001 and p < 0.01, respectively). Specifically, the clinical cure rate was 61.7% (50/81) and the clinical response rate was 88.9% (72/81) in the FERT group, while the clinical cure rate was only 21.7% (10/46) and the overall effective rate was 67.4% (31/46) in the control group.
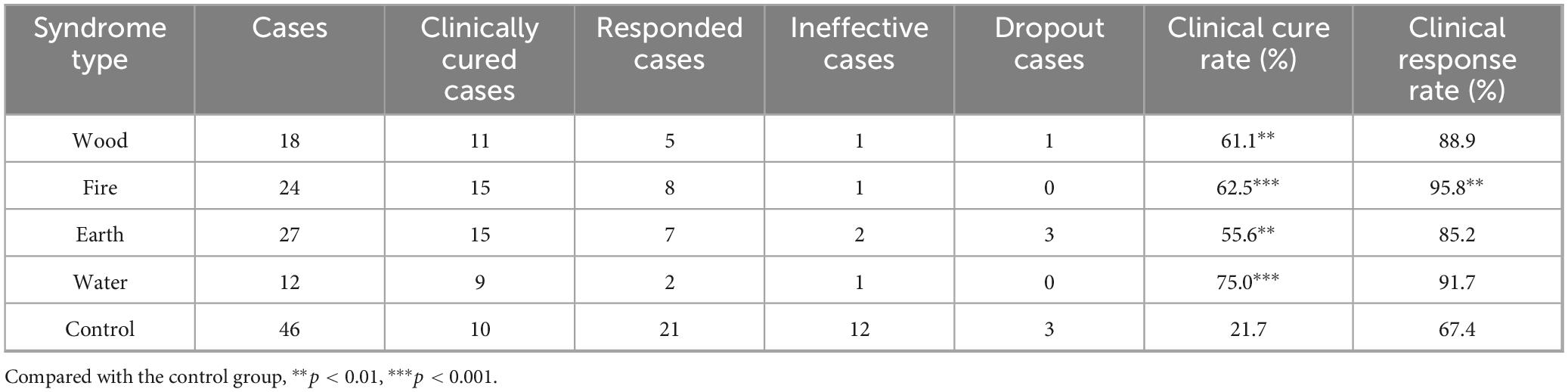
In the FERT group, 33.3% (27/81) of patients had “Earth Disease,” 29.6% (24/81) had “Fire Disease,” 22.2% (18/81) had “Wood Disease,” and 14.8% (12/81) had “Water Disease “(Table 4). The order of effectiveness for different types of evidence is as follows: Water (75%), Fire (62.5%), Wood (61.1%), and Earth (55.6%). The response rates of different evidence types were compared, and the results showed that Fire (95.8%) and Water (91.7%) were the most effective, followed by Wood (88.9%) and Earth (85.2%). Compared with the control group, the clinical cure rates of all other groups have been significantly improved. In terms of clinical response rates, only the improvement in the Fire Disease group is statistically significant (p < 0.01; Figure 2 and Table 4).
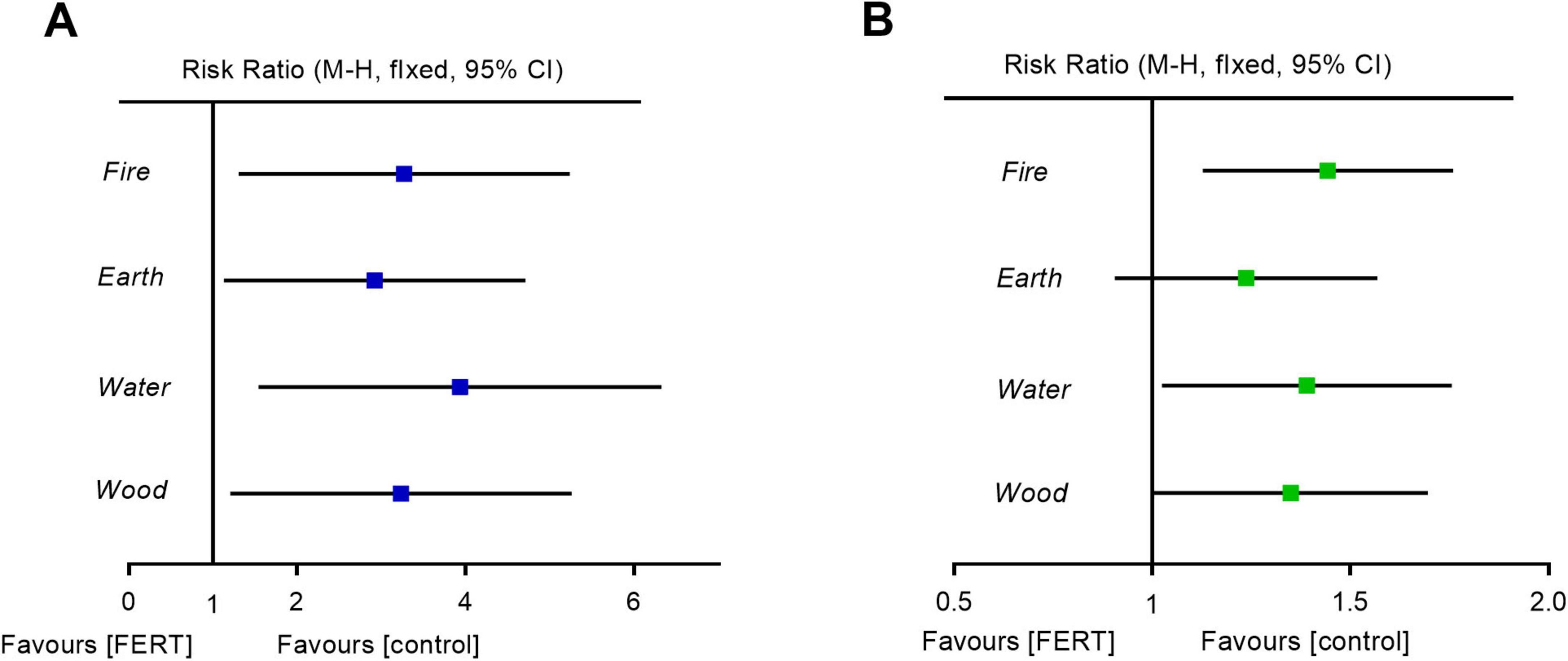
Figure 2. Forest plot of FERT for different syndromes. (A) Clinical cure rate. (B) Clinical response rate. CI, confidence interval; FERT, Five-Element Regulation Therapy.
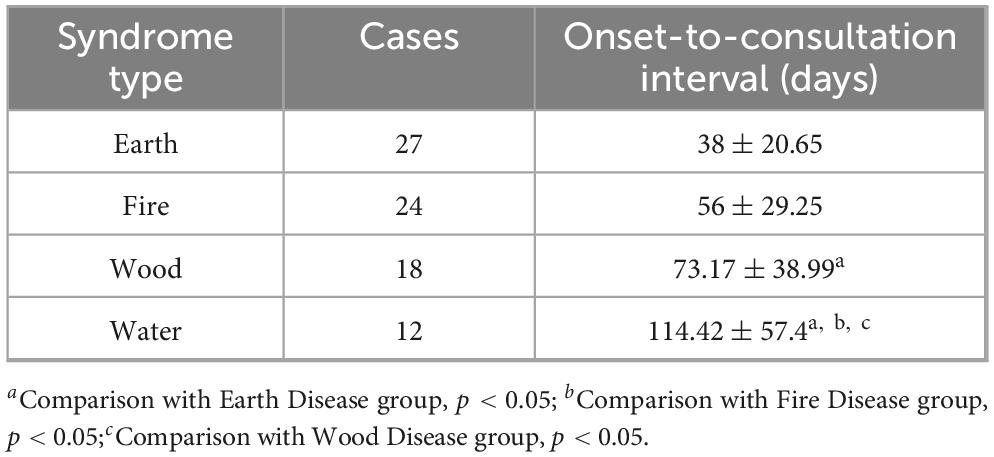
Table 5 shows the time intervals between patient complaints and the onset of COVID for each syndrome type. The “Earth Diseases” have the fastest onset, with an average of 38 days. This is followed by “Fire Diseases,” which have an average onset of 56 days. The “Wood Diseases” have a slightly later onset at 73 days, and the “Water Diseases” have the latest onset, with an average of 114 days.
4 Discussion
Five-Element Regulation Therapy originates from TCM constitution theory and is a therapeutic method developed through our team’s clinical practice. During the COVID-19 outbreak in Beijing in 2022, the Department of TCM at Peking University Third Hospital established a dedicated COVID clinic. In its later stages, this clinic treated a large number of patients suffering from post-COVID sequelae. Based on the symptom profiles observed in this patient population, our team applied FERT as a treatment. However, the comparative effectiveness of FERT versus conventional TCM treatment remained unclear. This study employed a retrospective cohort design to analyze the differences in efficacy between FERT and conventional TCM therapy. The findings suggest that FERT may be more effective than conventional TCM treatment for alleviating post-COVID symptoms.
During the early battle against COVID-19 in Wuhan in 2020, TCM experts identified the disease as a “cold-dampness syndrome,” providing direction for its TCM treatment (24–27). In our clinical observations of Beijing patients, we identified distinct manifestations at different stages of post-COVID sequelae. Initially, most patients self-medicated, with some developing cough. Subsequently, patients primarily sought medical attention for cough and dyspnea. Later, their chief complaints shifted toward panic attacks, chest tightness, and palpitations. In later stages, psychological symptoms such as insomnia, irritability, anxiety, and depression were frequently observed. Some patients progressed to develop chronic fatigue, dry mouth, low-grade fever, or even reproductive dysfunction. These manifestations align with the TCM Five Elements Theory, and the data confirmed the progression sequence (Metal → Earth → Fire → Wood → Water), supporting our hypothesis. Patients were categorized into one of the Five Phase groups, and tailored body recuperative formulas were designed accordingly.
Five-Element Regulation Therapy employs five distinct prescriptions corresponding to the five symptom patterns. In this study, we observed the effects of four prescriptions, but data for the Metal Formula is lacking. This is because the Metal Formula, derived from a modified Qingfei Paidu Decoction (28, 29), primarily targets early-stage infection symptoms, including fever, cough, headache, and fatigue. However, as most patients self-administered antipyretic drugs during the initial COVID-19 phase, subsequent fever symptoms were generally mild. Consequently, the application of this specific formula in the outpatient setting was limited, resulting in an insufficient number of patients categorized under the Metal phase for observation.
The potential reasons for FERT’s superiority over conventional TCM treatment lie in its innovative integration of the dynamic pattern differentiation framework from TCM Five Elements theory with the unique pathological progression of post-COVID sequelae. The therapy precisely categorizes symptom progression into five sequential syndrome patterns according to the generative cycle of the Five Phases: Early-stage pulmonary symptoms (Metal Disease, mean 38 days), Persistent respiratory impairment (Earth Disease, mean 38 days), Cardiovascular disturbances (Fire Disease, mean 56 days), Emotional dysregulation (Wood Disease, mean 73 days), Systemic exhaustion in advanced stages (Water Disease, mean 114 days). FERT employs tailored prescriptions targeting the core pathogenesis of each stage, with individualized modifications based on specific symptoms. This temporally stratified intervention strategy effectively aligns with the characteristic sequential multi-system damage observed in post-COVID sequelae. In contrast, conventional TCM’s static pattern differentiation fails to capture this dynamic progression. Consequently, FERT demonstrates significant advantages, evidenced by a 75% clinical cure rate for the Water Disease and a 95.8% response rate for the Fire Disease – markedly higher than the control group. These benefits are particularly pronounced in middle-to-late-stage patients.
We acknowledge several limitations in this study. First, as an observational retrospective cohort study, it is inherently prone to selection bias and confounding factors, which may compromise the validity of results. Retrospective data reliance on existing records may lack standardized documentation for some variables, increasing information bias and distorting FERT-outcome associations. Non-randomized design also leaves baseline group differences unbalanced, causing residual confounding. Second, the small sample size, especially when stratified by TCM syndrome types, reduces statistical power to detect subgroup differences and raises type II error risk. Third, lacking long-term follow-up beyond 2 weeks hinders conclusions on FERT’s durability and long-term efficacy. Fourth, the single-tertiary-hospital outpatient population in Beijing limits generalizability to other regions, settings, or ethnic groups. Fifth, the primary endpoints of observation were all based on subjective symptom reports, lacking objective indicators. Finally, the absence of placebo control prevents isolating FERT’s specific effects, as other factors may contribute.
5 Conclusion
This retrospective cohort study investigated the potential role of FERT in managing post-COVID-19 sequelae. The results demonstrated that FERT may be superior to conventional TCM therapy in improving post-COVID symptoms including chronic cough, fatigue, insomnia, and pain. However, given the study’s retrospective design and limitations such as the lack of a blank control group, these findings should be interpreted with caution. Future high-quality studies are warranted to further analyze the therapeutic effects of FERT.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethics Committee of Peking University Third Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
ND: Methodology, Conceptualization, Formal Analysis, Writing – original draft. YZ: Formal analysis, Writing – original draft, Software. HZ: Writing – review & editing. XX: Writing – review & editing. YY: Writing – original draft, Conceptualization, Software, Methodology, Writing – review & editing. DL: Funding acquisition, Conceptualization, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research and/or publication of this article. This study was supported by the National Natural Science Foundation of China (No. 82074193) and Clinical Key Project of Peking University Third Hospital (No. BYSY2023049).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2025.1621948/full#supplementary-material
References
1. Rusu L, Ardelean L, Tigmeanu C, Matichescu A, Sauciur I, Bratu EA. COVID-.19 and its repercussions on oral health: a review. Medicina. (2021) 57:1189. doi: 10.3390/medicina57111189
2. Mehandru S, Merad M. Pathological sequelae of long-haul COVID. Nat Immunol. (2022) 23:194–202. doi: 10.1038/s41590-021-01104-y
3. Parotto M, Gyongyosi M, Howe K, Myatra S, Ranzani O, Shankar-Hari M, et al. Post-acute sequelae of COVID-19: understanding and addressing the burden of multisystem manifestations. Lancet Respir Med. (2023) 11:739–54. doi: 10.1016/S2213-2600(23)00239-4
4. Xiong Q, Xu M, Li J, Liu Y, Zhang J, Xu Y, et al. Clinical sequelae of COVID-19 survivors in Wuhan, China: a single-centre longitudinal study. Clin Microbiol Infect. (2021) 27:89–95. doi: 10.1016/j.cmi.2020.09.023
5. Asakawa T, Cai Q, Shen J, Zhang Y, Li Y, Chen P, et al. Sequelae of long COVID, known and unknown: a review of updated information. Biosci Trends. (2023) 17:85–116. doi: 10.5582/bst.2023.01039
6. Baroni C, Potito J, Perticone M, Orausclio P, Luna C. How does long-COVID impact prognosis and the long-term sequelae? Viruses. (2023) 15:1173. doi: 10.3390/v15051173
7. O’mahoney L, Routen A, Gillies C, Ekezie W, Welford A, Zhang A, et al. The prevalence and long-term health effects of long Covid among hospitalised and non-hospitalised populations: a systematic review and meta-analysis. EClinicalMedicine. (2023) 55:101762. doi: 10.1016/j.eclinm.2022.101762
8. Thaweethai T, Jolley S, Karlson E, Levitan E, Levy B, Mccomsey G, et al. Development of a definition of postacute sequelae of SARS-CoV-2 infection. JAMA. (2023) 329:1934–46. doi: 10.1001/jama.2023.8823
9. Chen B, Julg B, Mohandas S, Bradfute S, Force R. Viral persistence, reactivation, and mechanisms of long COVID. Elife. (2023) 12:e86015. doi: 10.7554/eLife.86015
10. Blondeau J. Long COVID: a consequence of chronic post-infectious inflammation! Expert Rev Respir Med. (2024) 18:939–45. doi: 10.1080/17476348.2024.2438104
11. Wu X, Xiang M, Jing H, Wang C, Novakovic V, Shi J. Damage to endothelial barriers and its contribution to long COVID. Angiogenesis. (2024) 27:5–22. doi: 10.1007/s10456-023-09878-5
12. Molnar T, Lehoczki A, Fekete M, Varnai R, Zavori L, Erdo-Bonyar S, et al. Mitochondrial dysfunction in long COVID: mechanisms, consequences, and potential therapeutic approaches. Geroscience. (2024) 46:5267–86. doi: 10.1007/s11357-024-01165-5
13. Colombo J, Weintraub M, Munoz R, Verma A, Ahmad G, Kaczmarski K, et al. Long COVID and the autonomic nervous system: the journey from dysautonomia to therapeutic neuro-modulation through the retrospective analysis of 152 patients. NeuroSci. (2022) 3:300–10. doi: 10.3390/neurosci3020021
14. Iwasaki M, Saito J, Zhao H, Sakamoto A, Hirota K, Ma D. Inflammation triggered by SARS-CoV-2 and ACE2 augment drives multiple organ failure of severe COVID-19: molecular mechanisms and implications. Inflammation. (2021) 44:13–34. doi: 10.1007/s10753-020-01337-3
15. Stoian M, Procopiescu B, Seitan S, Scarlat G. Post-COVID-19 syndrome: insights into a novel post-infectious systemic disorder. J Med Life. (2023) 16:195–202. doi: 10.25122/jml-2022-0329
16. Ramonfaur D, Ayad N, Liu P, Zhou J, Wu Y, Li J, et al. The global clinical studies of long COVID. Int J Infect Dis. (2024) 146:107105. doi: 10.1016/j.ijid.2024.107105
17. Monroy M, Amster M, Eagle J, Zerwas F, Keltner D, Lopez J. Awe reduces depressive symptoms and improves well-being in a randomized-controlled clinical trial. Sci Rep. (2025) 15:16453. doi: 10.1038/s41598-025-96555-w
18. Zhou S, Feng J, Xie Q, Huang T, Xu X, Zhou D, et al. Traditional Chinese medicine shenhuang granule in patients with severe/critical COVID-19: a randomized controlled multicenter trial. Phytomedicine. (2021) 89:153612. doi: 10.1016/j.phymed.2021.153612
19. Chen B, Geng P, Shen J, Liangpunsakul S, Lyu H, Zhang J, et al. Traditional Chinese medicine JingYinGuBiao formula therapy improves the negative conversion rate of SARS-CoV2 in patients with mild COVID-19. Int J Biol Sci. (2022) 18:5641–52. doi: 10.7150/ijbs.76699
20. Chen Y, Liu C, Wang T, Qi J, Jia X, Zeng X, et al. Efficacy and safety of Bufei Huoxue capsules in the management of convalescent patients with COVID-19 infection: a multicentre, double-blind, and randomised controlled trial. J Ethnopharmacol. (2022) 284:114830. doi: 10.1016/j.jep.2021.114830
21. Pang W, Yang F, Zhao Y, Dai E, Feng J, Huang Y, et al. Qingjin Yiqi granules for post-COVID-19 condition: a randomized clinical trial. J Evid Based Med. (2022) 15:30–8. doi: 10.1111/jebm.12465
22. Li L, Yao H, Wang J, Li Y, Wang Q. The aole of Chinese medicine in health maintenance and disease prevention: application of constitution theory. Am J Chin Med. (2019) 47:495–506. doi: 10.1142/S0192415X19500253
23. Li L, Wang Z, Wang J, Zheng Y, Li Y, Wang Q. Enlightenment about using TCM constitutions for individualized medicine and construction of Chinese-style precision medicine: research progress with TCM constitutions. Sci China Life Sci. (2021) 64:2092–9. doi: 10.1007/s11427-020-1872-7
24. Zhang S, Yan X, Gao P, Zeng Z, Yang H, Ding P, et al. [Analysis of traditional Chinese medicine syndromes in patients with coronavirus disease 2019 in plateau areas]. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. (2022) 34:1330–2. doi: 10.3760/cma.j.cn121430-20220829-00794
25. Feng Z, Xie Y, Chun L, Li J. [Study on traditional Chinese medicine common syndrome characteristic of coronavirus disease 2019 based on latent structure combined with system clustering analysis]. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. (2020) 32:537–43. doi: 10.3760/cma.j.cn121430-20200506-00620
26. Li X, Liu W, He W, Xie Y, Li J. [Meta-analysis of single-group rate of the distribution of traditional Chinese medicine syndromes in 2 139 patients with coronavirus disease 2019]. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. (2020) 32:664–70. doi: 10.3760/cma.j.cn121430-202000509-00372
27. Lyu M, Fan G, Xiao G, Wang T, Xu D, Gao J, et al. Traditional Chinese medicine in COVID-19. Acta Pharm Sin B. (2021) 11:3337–63. doi: 10.1016/j.apsb.2021.09.008
28. Shi N, Liu B, Liang N, Ma Y, Ge Y, Yi H, et al. Association between early treatment with Qingfei Paidu decoction and favorable clinical outcomes in patients with COVID-19: a retrospective multicenter cohort study. Pharmacol Res. (2020) 161:105290. doi: 10.1016/j.phrs.2020.105290
Keywords: Five-Element Regulation Therapy, corona virus disease 2019, post-COVID syndrome, retrospective study, Traditional Chinese Medicine
Citation: Ding N, Zhou Y, Zhang H, Xin X, Ye Y and Li D (2025) Effectiveness of Five-Element Regulatory Therapy for post-COVID syndrome: a retrospective cohort study. Front. Med. 12:1621948. doi: 10.3389/fmed.2025.1621948
Received: 06 May 2025; Accepted: 20 October 2025;
Published: 06 November 2025.
Edited by:
Indrajit Banerjee, SSR Medical College, MauritiusReviewed by:
Guang Chen, The University of Hong Kong, Hong Kong SAR, ChinaWen Zhu, Fudan University, China
Copyright © 2025 Ding, Zhou, Zhang, Xin, Ye and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yang Ye, eWV5YW5nODlAMTI2LmNvbQ==; Dong Li, bGlkb25nNjUxMkBzaW5hLmNvbQ==
 Ning Ding1
Ning Ding1 Haolin Zhang
Haolin Zhang Yang Ye
Yang Ye Dong Li
Dong Li