Abstract
Background:
Intraoperative neuromonitoring (IONM) is widely used to preserve recurrent laryngeal nerve (RLN) function during thyroid surgery. However, patients undergoing thyroidectomy with IONM may experience a higher incidence of postoperative nausea and vomiting (PONV) and poorer recovery quality. Both acupuncture and propofol anesthesia have been investigated as potential strategies to prevent PONV, but clinical evidence on their combined use in thyroidectomy is limited. This study aimed to evaluate the effects of propofol-based anesthesia combined with postoperative acupuncture on PONV and early recovery within 24 h after thyroidectomy with IONM.
Methods:
A total of 135 adult patients were randomly assigned to one of four groups: sevoflurane with sham acupuncture (n = 32), sevoflurane with active acupuncture (n = 33), propofol with sham acupuncture (n = 35), or propofol with active acupuncture (n = 35). The primary outcomes were the incidence and severity of PONV and early recovery quality within 24 h. Secondary outcomes included sore throat, headache, and dizziness.
Results:
Compared with sevoflurane, propofol anesthesia significantly reduced PONV severity (OR = 0.313; 95% CI, 0.123–0.797; p = 0.014) and the frequency of postoperative vomiting (OR = 0.329; 95% CI, 0.115–0.939; p = 0.038). Active acupuncture also significantly reduced PONV severity compared with sham acupuncture (p = 0.008). However, combining propofol anesthesia with active acupuncture did not provide additional benefits beyond each intervention alone.
Conclusion:
Both propofol anesthesia and postoperative acupuncture independently reduced the incidence and severity of PONV after thyroidectomy with IONM. No synergistic effect was observed, possibly due to mechanistic differences or the limited intensity of the acupuncture protocol. Further research is warranted to optimize acupuncture parameters and clarify the clinical utility of combined approaches across broader surgical settings.
Clinical trial registration:
The clinical trial was registered in the Chinese Clinical Trial Registry under the identifier ChiCTR2400082127.
1 Introduction
PONV is a common and distressing complication after thyroidectomy, with an incidence of 20–60% despite the use of prophylactic anti-emetics (1, 2). Beyond impairing comfort and satisfaction, PONV may precipitate serious consequences, including postoperative hemorrhage, delayed recovery, and increased healthcare costs (3, 4).
IONM is widely adopted during thyroid surgery to reduce the risk of RLN injury (5). However, IONM has been associated with a higher incidence of PONV (5, 6), likely reflecting anesthetic adjustments made to optimize monitoring—such as minimizing neuromuscular blockade, increasing opioid use to prevent movement, and prolonging operative time. Although guidelines for PONV prevention are available, their effectiveness in routine practice remains suboptimal (7). In addition, the limited efficacy and potential adverse effects of antiemetic drugs underscore the need for safer, non-pharmacological strategies.
Propofol-based TIVA, which has intrinsic antiemetic properties, is recommended for patients at high risk of PONV (7). Acupuncture has also attracted interest as a non-pharmacological intervention for postoperative gastrointestinal symptoms (8, 9). Common sensations during acupuncture—such as soreness, heaviness, or numbness at the stimulation site—are regarded by some practitioners as markers of physiological response and have been explored as behavioral indicators in research (8, 9). Stimulation at Neiguan (PC6), Zusanli (ST36), and Zhongwan (RN12) has been reported to alleviate nausea and gastrointestinal discomfort (10). These acupoints were selected according to traditional Chinese medicine theory; while prior trials support their clinical use, putative mechanisms remain largely theoretical and lack validation by modern biomedical research. Notably, clinical evidence on combining acupuncture with propofol-based anesthesia during thyroidectomy is limited.
This study aimed to evaluate whether propofol-based anesthesia combined with postoperative acupuncture reduces the incidence of PONV and improves early postoperative recovery in patients undergoing IONM-assisted thyroidectomy. We also explored whether the combination confers any additional benefit compared with either intervention alone.
2 Methods
2.1 Study design and ethical approval
This single-center, randomized, controlled trial evaluated the effects of propofol-based anesthesia combined with active acupuncture on nausea, vomiting, and early recovery quality after thyroid surgery. The protocol was approved by the Ethics Review Committee of the Fourth Hospital of Hebei Medical University (approval No. 2024012) and registered in the Chinese Clinical Trial Registry (ChiCTR2400082127). Written informed consent was obtained from all participants before enrollment.
2.2 Patient selection
Adults aged 18–80 years with ASA physical status I–III scheduled for elective thyroidectomy were eligible. Exclusion criteria were infection or eczema over acupoints; cervical vertebral disease; motion sickness or vertebrobasilar insufficiency; history of opioid use; severe renal or hepatic dysfunction; coagulopathy or other hematologic disease; pregnancy or breastfeeding; and allergy to any study medication.
2.3 Randomization and group allocation
Participants were randomly assigned (1:1:1:1) using a computer-generated sequence to one of four groups: sevoflurane + sham acupuncture (n = 32), sevoflurane + active acupuncture (n = 33), propofol + sham acupuncture (n = 35), or propofol + active acupuncture (n = 35). Randomization was stratified by anesthesia type (sevoflurane vs. propofol) and acupuncture (active vs. sham). Allocation was concealed with sealed, opaque envelopes, opened immediately before induction of anesthesia and initiation of acupuncture, respectively.
2.4 Anesthesia protocol
Anesthesia was induced with intravenous sufentanil (0.5–0.6 μg·kg−1), remimazolam (0.3 mg·kg−1), and cisatracurium (0.05 mg·kg−1), followed by tracheal intubation 7 min after supraglottic topical application of 4 mL 2% lidocaine. Maintenance was either inhaled sevoflurane (1.5–2.0%) in 50% oxygen/air or intravenous propofol (6–10 mg·kg−1·h−1), titrated to a bispectral index of 40–55. Remifentanil (0.1–0.2 μg·kg−1·min−1) was administered for analgesia. Pharmacologic antagonism for neuromuscular recovery was not routinely used. For postoperative analgesia, flurbiprofen axetil (50 mg) was given 30 min before the end of surgery. Tracheal extubation was performed in the operating room or post-anesthesia care unit when spontaneous breathing was adequate and SpO₂ exceeded 90%.
2.5 Acupuncture intervention
Participants received active or sham acupuncture 10 min to 2 h after returning to the ward. Treatments were delivered by a single experienced acupuncturist. Acupoints included bilateral Neiguan (PC6), Zusanli (ST36), Fengchi (GB20), Tianrong (SI17), and Zhongwan (RN12) (10–14). We selected a PC6–ST36–GB20 montage to target core mechanisms and common accompaniments of PONV: PC6 is the best-evidenced antiemetic point, acting via vagal–nucleus tractus solitarius pathways and modulation of gastric rhythm and 5-HT3–related signaling (15, 16); ST36 augments vagal tone/gastrointestinal motility and improves gastric slow waves/HRV (16, 17); GB20 addresses vestibular–occipital circuitry relevant to postoperative dizziness/headache (18).
After skin antisepsis, sterile filiform needles (0.25 mm; Hwato, 0.25 × 40 mm or 0.25 × 25 mm) were inserted vertically at PC6 (10–20 mm) and ST36 (20–30 mm), and obliquely antero-medially at GB20 (10–15 mm). Mild manual stimulation (de-qi) for 10–15 s every 10 min was applied; retention 25–30 min covering emergence. Intensity was kept below the movement threshold. Predefined stopping rules included movement, discomfort, bleeding, or monitoring interference. All patients were supine. Sham acupuncture used validated blunt-tipped needles in guide tubes at the same acupoints, mimicking penetration without skin puncture, to reproduce the tactile experience without physiological stimulation.
Reporting standards: The intervention follows STRICTA 2010 (CONSORT extension) and TIDieR recommendations, detailing point selection/rationale, needling (location, depth/angle, response sought), regimen (dose, timing, frequency), practitioner background, and control procedures (19–21). See Supplementary Table S_STRICTA.
2.6 Blinding procedures
Participants in each group received active or sham acupuncture individually in a private room and were instructed not to communicate with other participants or disclose allocation to outcome assessors. All acupuncture procedures were performed by a single experienced acupuncturist who was not involved in postoperative assessments. A trained research assistant, blinded to allocation, conducted bedside evaluations 24 h after surgery.
Because full participant blinding in acupuncture studies is inherently challenging, a standardized sham procedure was used to simulate the tactile experience of real needling without physiological stimulation. In the sham group, modified blunt-tipped needles were applied at the same acupoints using validated guide tubes; these devices mimicked needle penetration without skin puncture, minimizing sensory differences between sham and active interventions.
2.7 Outcome measures
The primary outcomes were the occurrence and severity of PONV within the first 24 h after surgery, as well as the quality of early recovery at 24 h. The time of return to the ward was defined as time 0. PONV occurrence was defined as any episode of nausea, retching, or vomiting, with vomiting counted irrespective of nausea. PONV severity was assessed using a 0–10 numeric rating scale (NRS; 0 = none, 10 = worst imaginable) and categorized into bands of 1–3, 4–6, and 7–10. Early recovery was evaluated with a 0–70 short-form recovery score, constructed from seven items derived from the QoR-15 (breathing comfort, appetite, energy, sleep quality, self-care/hygiene, communication/voice, and sadness/depression). This instrument is not equivalent to the standard 15-item QoR-15 (0–150). Full item wording, anchors, and scoring rules are provided in Supplementary Table Sx.
Secondary outcomes within the first 24 h included sore throat, headache, dizziness, and sleep quality on the night of surgery, and intra-operative opioid consumption (expressed as intravenous morphine-equivalent dose). Sore throat was rated on a four-point ordinal scale (0 = none; 1 = mild, reported only when questioned; 2 = moderate, reported spontaneously without prompting; 3 = severe, accompanied by hoarseness or voice change). Headache was assessed on a 0–10 NRS and similarly archived in bands (1–3, 4–6, 7–10), then classified as none, mild, moderate, or severe, with severe defined as NRS ≥ 7. Dizziness was recorded as a binary yes/no outcome. Sleep quality was assessed on a four-point scale (0 = better than at home; 1 = similar to at home; 2 = slightly worse; 3 = much worse).
2.8 Sample size calculation
This was a 2 × 2 factorial trial with equal allocation to four arms (propofol + active acupuncture, propofol + sham acupuncture, sevoflurane + active acupuncture, and sevoflurane + sham acupuncture). Based on routine practice, the sevoflurane-based regimen was associated with an incidence of any PONV of approximately 58% in thyroidectomy with IONM. We hypothesized that the combined intervention of propofol-based anesthesia plus active acupuncture would reduce the incidence of any PONV to 30%, corresponding to an absolute reduction of 28% relative to the most emetogenic arm. Using a two-sided α of 0.05 and 80% power, this difference required 29 patients per arm (total 116). Allowing for about 10% attrition, the target sample size was 129 participants (≈32 per arm). Ultimately, 160 patients were screened and 135 participants were included in the final analysis (Figure 1). Under the standard no-interaction assumption for factorial designs, this sample size also provided adequate power to detect main effects of comparable magnitude. Baseline characteristics were summarized as mean (SD) or median [IQR] for continuous variables and n (%) for categorical variables, with between-group balance shown in Table 1.
Figure 1
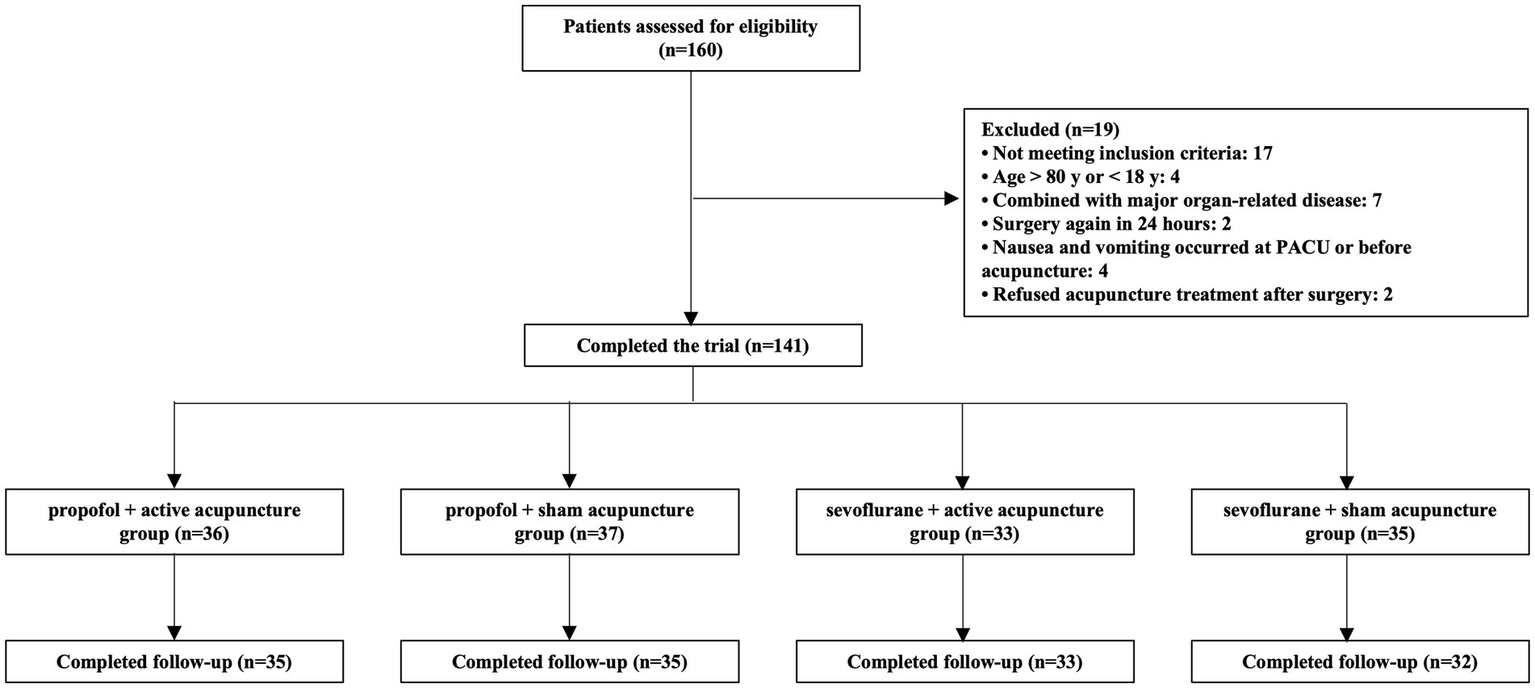
Study flowchart. A total of 160 patients were assessed for eligibility. After exclusions, 141 participants were enrolled and randomized into four groups: propofol + real acupuncture (n = 36), propofol + sham acupuncture (n = 37), sevoflurane + real acupuncture (n = 33), and sevoflurane + sham acupuncture (n = 35). Final follow-up was completed for 135 participants.
Table 1
| Characteristic | RP (n = 35) | SP (n = 35) | RS (n = 33) | SS (n = 32) | All participants (n = 135) |
|---|---|---|---|---|---|
| Gender, n(%) | |||||
| Male | 10(28.57) | 4(11.43) | 4(12.12) | 10(31.25) | 28(20.74) |
| Female | 25(71.43) | 31(88.57) | 29(87.88) | 22(68.75) | 107(79.26) |
| Mean age (SD), y | 45.57(11.64) | 44.06(10.81) | 50(11.83) | 44.94(11.60) | 46.11(11.57) |
| Mean BMI(SD), kg/m2 | 25.43(2.30) | 24.54(3.08) | 24.88(2.59) | 24.69(2.89) | 24.89(2.72) |
| ASA, n(%) | |||||
| ASA II | 34(97.14) | 35(100) | 32(96.97) | 32(100) | 133(98.52) |
| ASA III | 1(2.86) | 0(0) | 1(3.03) | 0(0) | 2(1.48) |
| Postoperative pathological types n(%) | |||||
| Papillary thyroid carcinoma | 32(91.43) | 29(82.86) | 26(78.79) | 25(78.13) | 112(82.96) |
| Nodular goiter with adenomatous hyperplasia | 1(2.86) | 6(17.14) | 7(21.21) | 5(15.62) | 19(14.07) |
| Hashimoto’s thyroiditis | 2(5.71) | 0(0) | 0(0) | 2(6.25) | 4(2.97) |
Baseline demographic and clinical characteristics of patients data are presented as mean ± SD or number (percentage), as appropriate.
BMI = body mass index; ASA = ASA physical status classification system, ASA II: a patient with mild systemic disease; ASA III: a patient with severe systemic disease; Papillary thyroid carcinoma = the most common type of thyroid cancer; Nodular goiter with adenomatous hyperplasia = it is the category of thyroid adenoma, which is a benign tumor; Hashimoto’s thyroiditis = a chronic autoimmune inflammation of the thyroid gland.
2.9 Statistical analysis
Prespecified factorial models were used for the primary outcomes, including the main effects of anesthesia (propofol vs. sevoflurane) and acupuncture (active vs. sham), as well as the anesthesia × acupuncture interaction. Main effects were estimated from reduced models without the interaction unless otherwise specified, and the interaction was tested using a Wald term. Any PONV and vomiting ≥1 episode were analyzed with logistic regression; PONV severity was treated as an ordered outcome using proportional-odds models; and the 24-h early recovery score (0–70) was analyzed with linear models. For secondary outcomes, sore throat (0–3) and headache (NRS archived into bands of 1–3, 4–6, and 7–10) were first analyzed as binary outcomes (any vs. none) using logistic models, while dizziness was analyzed as yes/no. As sensitivity analyses, ordered severity distributions (none/mild/moderate/severe) for sore throat and headache were compared using the Mann–Whitney rank-sum test. Intra-operative opioid consumption was compared among groups using ANOVA or Kruskal–Wallis tests as appropriate.
To complement the factorial analysis, omnibus and multiplicity-adjusted pairwise tests were performed across the four arms (propofol + active, propofol + sham, sevoflurane + active, and sevoflurane + sham). ANOVA was used for continuous outcomes (0–70 score), Kruskal–Wallis for ordered outcomes (PONV severity and sore throat), and chi-square or Fisher’s exact test for binary outcomes (any PONV, vomiting ≥1, sore throat, headache, and dizziness). Pairwise contrasts were adjusted using the Holm step-down procedure. Full results, including effect sizes, 95% confidence intervals, and adjusted p values, are provided in Supplementary Tables S1–S3; factorial models remain the primary analysis. Effect sizes are presented as adjusted odds ratios (aORs) with 95% confidence intervals and exact p-values for binary outcomes, and as mean differences with 95% confidence intervals for continuous outcomes. Two-sided α = 0.05 defined statistical significance. Analyses were performed using SPSS version 26.
Equation 1 (binary logistic model; any PONV, vomiting ≥1, sore throat, headache, dizziness):
The reference levels were sevoflurane and sham acupuncture; odds ratios were calculated as exp.(β), with values <1 indicating a protective effect of propofol or active acupuncture when the outcome (Y) denoted an adverse event. Post-hoc power was also computed for each factorial term using the observed coefficient and standard error with a Wald noncentral χ2 approximation (α = 0.05), and results are presented in Supplementary Table S4.
3 Results
Between April 9 and June 28, 2024, 160 patients were screened; 17 failed eligibility and 2 declined postoperative acupuncture. Six participants were lost to follow-up, leaving 135 participants who completed the trial (propofol + active n = 35; propofol + sham n = 35; sevoflurane + active n = 33; sevoflurane + sham n = 32) (Figure 1). Baseline characteristics were well balanced across groups (Table 1).
For the primary outcomes, the four-arm risks of any PONV were 78.1% (25/32) for sevoflurane + sham, 60.6% (20/33) for sevoflurane + active, 45.7% (16/35) for propofol + sham, and 28.6% (10/35) for propofol + active. In factorial models, propofol compared with sevoflurane reduced the risk of any PONV (aOR 0.25, 95% CI 0.12–0.52; p = 0.0002) and vomiting ≥1 episode (aOR 0.329, 95% CI 0.115–0.939; p = 0.038), and was associated with lower PONV severity (proportional-odds aOR 0.313, 95% CI 0.123–0.797; p = 0.015). Active compared with sham acupuncture also reduced any PONV (aOR 0.45, 95% CI 0.22–0.95; p = 0.035). No anesthesia × acupuncture interaction was detected for any PONV endpoints (Wald p = 0.897), indicating additive rather than synergistic effects (Table 2).
Table 2
| Outcome | Propofol vs. Sevoflurane (aOR, 95% CI) | p | Active vs. Sham (aOR, 95% CI) | p | Interaction (Wald p) |
|---|---|---|---|---|---|
| Any PONV (yes/no) | 0.248 (0.119–0.518) | 0.0002 | 0.454 (0.218–0.946) | 0.0349 | 0.897 |
| Vomiting ≥ 1 episode | 0.258 (0.120–0.552) | 0.0005 | 1.116 (0.528–2.360) | 0.7735 | 0.811 |
| PONV severity (ordinal 0–3) | 0.313 (0.123–0.797) | 0.0149 | 0.216 (0.083–0.567) | 0.0018 | 0.956 |
Primary outcomes at 24 h — prespecified 2 × 2 factorial models.
Reference levels are sevoflurane and sham acupuncture. For adverse outcomes (any PONV, vomiting ≥1, higher severity), values <1 favor propofol and/or active acupuncture. Interaction p values are from the corresponding full model with the product term. aOR = adjusted odds ratio; CI = confidence interval; PONV = postoperative nausea and vomiting.
Early recovery at 24 h, measured by the 0–70 short-form score (higher = better), did not differ by anesthesia (mean difference [propofol–sevoflurane] + 1.39, 95% CI − 0.75 to +3.54; p = 0.204) or by acupuncture (active–sham +1.34, 95% CI − 0.80 to +3.48; p = 0.221); the interaction term was non-significant (p = 0.553). Medians [IQR] were 64 [60–67] vs. 62 [58–67] for propofol vs. sevoflurane and 62.5 [59–68] vs. 63 [58–66] for active vs. sham (Table 3).
Table 3
| Arm | n | Mean ± SD | Median [IQR] |
|---|---|---|---|
| Propofol + Active | 35 | 63.2 ± 6.4 | 64 [62–68] |
| Propofol + Sham | 35 | 62.5 ± 6.0 | 64 [60–67] |
| Sevoflurane + Active | 33 | 62.4 ± 5.7 | 62 [58–68] |
| Sevoflurane + Sham | 32 | 60.4 ± 7.3 | 62 [55–66] |
| Factorial model estimates (linear models) | ||
|---|---|---|
| Contrast | Mean difference (95% CI) | p |
| Propofol – Sevoflurane | +1.39 (−0.75 to 3.53) | 0.204 |
| Active – Sham acupuncture | +1.34 (−0.80 to 3.48) | 0.221 |
Early recovery at 24 h — 0–70 short-form recovery score (higher = better).
Interaction (anesthesia × acupuncture): p = 0.553. The 0–70 short form is a non–QoR-15 instrument constructed from seven items; higher scores indicate better recovery. IQR = interquartile range; CI = confidence interval.
Regarding secondary outcomes within 24 h, sore throat (any vs. none) showed no significant differences (propofol vs. sevoflurane aOR 0.56, 95% CI 0.18–1.78; p = 0.330; active vs. sham aOR 1.01, 95% CI 0.33–3.07; p = 0.983). Similarly, headache did not differ significantly (propofol aOR 0.90, 95% CI 0.42–1.94; p = 0.847; active aOR 1.33, 95% CI 0.62–2.86; p = 0.560), nor did dizziness (propofol aOR 0.49, 95% CI 0.20–1.22; p = 0.125; active aOR 1.83, 95% CI 0.74–4.58; p = 0.194). Severity distributions for sore throat and headache were comparable across main effects (both p > 0.40, Mann–Whitney), and severe headache (NRS ≥ 7) was rare (Table 4). Intra-operative opioid consumption, converted to morphine milligram equivalents, differed significantly across the four groups (Kruskal–Wallis H = 14.8, p = 0.002). Pairwise Mann–Whitney tests showed no difference between active and sham acupuncture within either anesthetic regimen (propofol p = 1.000; sevoflurane p = 1.000), whereas propofol-based TIVA required significantly higher MME than sevoflurane across both acupuncture strata (all Bonferroni-adjusted p < 0.001) (Table 5).
Table 4
| (A) Any vs. none (factorial logistic models). | ||||
|---|---|---|---|---|
| Outcome | Propofol vs. Sevoflurane (aOR, 95% CI) | p | Active vs Sham (aOR, 95% CI) | p |
| Sore throat (any vs. none) | 0.56 (0.18–1.78) | 0.330 | 1.01 (0.33–3.07) | 0.983 |
| Headache (any vs. none) | 0.91 (0.42–1.95) | 0.799 | 1.33 (0.62–2.86) | 0.469 |
| Dizziness (yes/no) | 0.49 (0.20–1.22) | 0.125 | 1.83 (0.73–4.58) | 0.194 |
| (B) Severity distributions (Mann–Whitney p) and severe headache incidence. | |||
|---|---|---|---|
| Outcome/Analysis | Anesthesia p | Acupuncture p | Severe headache incidence |
| Sore throat severity distribution | 0.509 | 0.442 | — |
| Headache severity distribution | 0.800 | 0.415 | 1/65 (1.5%) vs. 1/70 (1.4%); 1/67 (1.5%) vs. 1/68 (1.5%) |
Secondary outcomes at 24 h — factorial models and severity distributions.
Logistic models report adjusted odds ratios (aORs) for main effects from reduced models without the interaction term. Mann–Whitney tests compare ordinal severity distributions between factor levels. Reference levels are sevoflurane and sham acupuncture. For adverse outcomes, aOR < 1 favors propofol and/or active acupuncture. aOR = adjusted odds ratio; CI = confidence interval; NRS = numeric rating scale; IQR = interquartile range.
Table 5
| Comparison | U | p_raw | p_Bonferroni |
|---|---|---|---|
| Propofol + Active vs. Propofol + Sham | 649.5 | 0.668 | 1.000 |
| Propofol + Active vs. Sevoflurane + Active | 1044.0 | <0.0001 | <0.0001 |
| Propofol + Active vs. Sevoflurane + Sham | 963.0 | <0.0001 | <0.0001 |
| Propofol + Sham vs. Sevoflurane + Active | 1015.5 | <0.0001 | <0.0001 |
| Propofol + Sham vs. Sevoflurane + Sham | 934.0 | <0.0001 | <0.0001 |
| Sevoflurane + Active vs. Sevoflurane + Sham | 470.5 | 0.454 | 1.000 |
Pairwise comparisons of intra-operative opioid consumption (MME, mg).
Pairwise group comparisons were performed using the Mann–Whitney U test. P-values were adjusted for multiple testing using the Bonferroni method.
Omnibus four-arm tests confirmed these patterns. The omnibus χ2 test for any PONV was significant (χ2(3) = 16.01, p = 0.00113); after Holm adjustment, the only significant pairwise contrast was sevoflurane + sham vs. propofol + active (OR 7.50, p_adj = 0.0013). For vomiting ≥1, the omnibus χ2 was significant (χ2(3) = 12.98, p = 0.00469), but no pairwise contrast remained significant after adjustment. Omnibus tests for sore throat, headache, and dizziness were not significant (all p ≥ 0.06). Full results are provided in Supplementary Tables S1–S3.
Post-hoc power analyses indicated that, for the primary nausea NRS outcome, power was 68% for the anesthesia main effect, 76% for the acupuncture main effect, and only 5% for the anesthesia × acupuncture interaction (β = 0.041, SE = 0.739), showing that the trial was underpowered to detect modest synergy; similarly low interaction power was observed for other outcomes (Supplementary Tables S4). No severe adverse events occurred, and no participant discontinued because of an adverse event.
4 Discussion
This randomized controlled trial demonstrated that both propofol-based anesthesia and postoperative acupuncture significantly reduced the incidence of PONV within 24 h after thyroidectomy with intraoperative neuromonitoring. However, the combination of the two interventions did not confer synergistic benefits, indicating additive rather than interactive effects.
The observed incidence of PONV in the sevoflurane groups exceeded that reported in previous thyroidectomy studies (≈44%) (2, 22, 23), reaching up to 60% without acupuncture. This higher rate may reflect the anesthetic adjustments required for IONM, including low-dose cisatracurium and higher opioid administration (24, 25). In this trial, intra-operative opioid consumption, expressed as morphine milligram equivalents, was significantly higher with propofol-based TIVA than with sevoflurane anesthesia, whereas acupuncture did not alter opioid requirements. This suggests that the antiemetic benefit of acupuncture is independent of opioid sparing, and may instead relate to modulation of vagal activity, serotonergic signaling, β-endorphin release or central emetic pathways, consistent with mechanisms proposed in previous experimental studies. These multi-target mechanisms help explain why acupuncture remained effective in reducing PONV even under propofol anesthesia, despite higher opioid consumption. Moreover, despite higher opioid use, propofol anesthesia still reduced the incidence of PONV, indicating that its intrinsic antiemetic effect outweighed the potential emetogenic impact of increased opioid exposure.
As a safe non-pharmacological intervention, acupuncture has increasingly been integrated into multimodal therapy (26–28). Previous studies have shown that bilateral Zusanli (ST36) acupuncture combined with ondansetron significantly reduced PONV in patients undergoing laparoscopic surgery (29). Yan et al. also found that combined acupuncture at Neiguan (PC6), Hegu, Zusanli (ST36), and Sanyinjiao was more effective than ondansetron alone in preventing postoperative nausea in high-risk patients (30). Our findings extend this evidence by confirming that acupuncture remains beneficial even alongside propofol-based anesthesia, although without synergy.
Propofol’s antiemetic effects are well recognized and may involve multiple mechanisms, including enhancement of GABA_A receptor activity, suppression of neuronal excitability in the nucleus tractus solitarius and chemoreceptor trigger zone, modulation of 5-HT3 and dopamine D2 signaling, and anti-inflammatory actions (31). Our finding that propofol reduced postoperative dizziness aligns with prior studies (32).
Acupuncture’s anti-PONV effects may involve the modulation of central and peripheral 5-HT levels, enhancement of vagal tone, and promotion of β-endorphin release in cerebrospinal fluid. Stimulation at PC6 has been shown to modulate vagal activity and gastric slow waves, regulate serotonergic signaling, and promote β-endorphin release in cerebrospinal fluid, thereby attenuating nausea and improving gastrointestinal motility (15, 17). ST36 complements PC6 by enhancing vagal tone and HRV, while GB20 targets vestibular–occipital circuits implicated in postoperative dizziness and headache. Prior studies combining acupuncture with antiemetics such as ondansetron demonstrated additive efficacy (10, 29). These multi-target mechanisms explain why acupuncture remained effective even in the presence of propofol-based anesthesia.
However, in this factorial RCT, the anesthesia × acupuncture interaction for the PONV endpoints was not significant (e.g., any PONV, Wald p = 0.897), indicating additive rather than synergistic effects. This pattern is biologically plausible: propofol-based TIVA already lowers baseline emetogenicity through overlapping antiemetic pathways and by avoiding volatile agents, creating a ceiling once risk is suppressed (7). Acupuncture can reduce PONV and modulate vagal/gastrointestinal signaling (e.g., PC6 stimulation), but the added value on top of effective anesthesia strategies is variable (15, 17). Moreover, propofol may attenuate stimulus-evoked central responses, potentially blunting acupuncture-evoked neural effects (33). Finally, acupuncture is likely dose-dependent (intensity, duration, frequency) (34). Consistent with these mechanisms, post-hoc power for the interaction was low across outcomes (~5–15%; peak 34% for dizziness), implying that only very large interaction effects (interaction OR ≈ 0.07–0.16 or 6–15) would have been detectable; our single, brief perioperative session may have provided insufficient activation. Future trials should test pre-operative initiation, longer or repeated sessions, and standardized stimulation parameters, and be a priori powered for an interaction (35).
Early recovery, assessed with a 0–70 short-form score, did not differ between groups (36, 37). The results revealed no significant differences between acupuncture and propofol in improving sleep quality or alleviating sore throat. This could be related to the specific nature of thyroid surgery, including use of large electrophysiological monitoring tubes and required neck hyperextension, which could exacerbate postoperative throat discomfort. In addition, acupuncture was performed only once, and the limited stimulation intensity and frequency may not have been sufficient to yield therapeutic effects within such a short period. The choice of recovery assessment tools may also influence outcomes.
This study has several unique strengths. The active acupuncture procedures were consistently performed by a single experienced acupuncturist, who has extensive clinical experience in managing postoperative gastrointestinal dysfunction (38). Standardized manipulation techniques were applied to ensure consistent stimulation intensity across participants. Additionally, a validated sham acupuncture control was implemented to minimize performance and detection bias.
Several limitations should be acknowledged. First, this was a single-center factorial RCT conducted under uniform IONM workflows with one acupuncturist, which may limit external validity. Routine antiemetic prophylaxis was omitted primarily to isolate the effects of the interventions; local practice constraints, including limited insurance coverage and cost, also contributed. This approach did not fully align with guideline recommendations (7) and represents an important limitation of the trial. Second, the trial was powered for main effects rather than interaction, and the anesthesia × acupuncture interaction estimate was imprecise, so modest synergistic effects cannot be excluded. Third, early recovery was assessed using a 0–70 short form that showed a 24-h ceiling, potentially attenuating differences; future studies could employ more comprehensive tools such as the QoR-40 or Pittsburgh Sleep Quality Index. Fourth, outcomes were assessed to 24 h only, whereas a substantial proportion of PONV occurs within 48 h (39). Fifth, despite rigorous blinding, placebo and expectancy effects cannot be entirely ruled out (15). Finally, the acupuncture protocol involved a single, brief perioperative session; as efficacy is dose- and timing-dependent, preoperative initiation, longer duration, or repeated stimulation may yield stronger effects (34).
In conclusion, this study demonstrated that both acupuncture and propofol anesthesia are effective in reducing PONV. However, their combined application did not demonstrate synergistic advantages, potentially due to differences in intervention mechanisms, limited stimulation frequency, or individual variability. Future research should focus on optimizing acupuncture timing (pre- vs. postoperative), frequency, and intensity, while integrating serological, physiological, and neuroimaging studies to elucidate mechanisms. Additionally, multicenter large-sample randomized trials are needed to confirm the applicability and cost-effectiveness of this approach across different surgeries and populations.
5 Conclusion
Acupuncture and propofol-based anesthesia each reduced the incidence of PONV in patients undergoing thyroidectomy with intraoperative neuromonitoring. However, their combination did not demonstrate superiority over either intervention alone.
Statements
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics statement
The studies involving humans were approved by the Ethics Committee of the Fourth Hospital of Hebei Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
WZ: Writing – review & editing, Writing – original draft, Methodology, Formal analysis, Data curation, Funding acquisition. SJ: Writing – original draft, Data curation, Methodology, Writing – review & editing. BP: Formal analysis, Data curation, Writing – original draft, Methodology. SZ: Methodology, Writing – original draft, Writing – review & editing. TT: Resources, Data curation, Writing – review & editing. TH: Data curation, Writing – review & editing, Supervision. NA: Data curation, Supervision, Writing – original draft. SW: Methodology, Data curation, Writing – original draft. HL: Resources, Writing – original draft, Funding acquisition, Project administration, Writing – review & editing, Supervision.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was funded by the Project for the Administration of Traditional Chinese Medicine (2025346).
Acknowledgments
We would like to thank F. Liu for her consultancy during this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2025.1650403/full#supplementary-material
Abbreviations
PONV, postoperative nausea and vomiting; IONM, intra-operative neuromonitoring; RLN, recurrent laryngeal nerve; TIVA, total intravenous anesthesia; ASA, American Society of Anesthesiologists; CONSORT, Consolidated Standards of Reporting Trials.
References
1.
Eberhart LH Mauch M Morin AM Wulf H Geldner G . Impact of a multimodal anti-emetic prophylaxis on patient satisfaction in high-risk patients for postoperative nausea and vomiting. Anaesthesia. (2002) 57:1022–7. doi: 10.1046/j.1365-2044.2002.02822.x
2.
Wang D Sun Y Zhu YJ Shan XS Liu H Ji FH et al . Comparison of opioid-free and opioid-inclusive propofol anaesthesia for thyroid and parathyroid surgery: a randomised controlled trial. Anaesthesia. (2024) 79:1072–80. doi: 10.1111/anae.16382
3.
Myles PS Williams DL Hendrata M Anderson H Weeks AM . Patient satisfaction after anaesthesia and surgery: results of a prospective survey of 10,811 patients. Br J Anaesth. (2000) 84:6–10. doi: 10.1093/oxfordjournals.bja.a013383
4.
Parra-Sanchez I Abdallah R You J Fu AZ Grady M Cummings K 3rd et al . A time-motion economic analysis of postoperative nausea and vomiting in ambulatory surgery. Can J Anaesth. (2012) 59:366–75. doi: 10.1007/s12630-011-9660-x
5.
Moon J Kim JK Shin HJ Park J Kim NY Nam KH . Effects of endotracheal tube with adhesive superficial laryngeal electrodes for intraoperative nerve monitoring on laryngopharyngeal complications during thyroidectomy. Biomedicine. (2023) 11:2544. doi: 10.3390/biomedicines11092544
6.
Chen H Lu Z . Effects of intraoperative neuromonitoring (IONM) technology on early recovery quality in patients after thyroid surgery: a randomized controlled trial. PLoS One. (2023) 18:e0292036. doi: 10.1371/journal.pone.0292036
7.
Gan TJ Belani KG Bergese S Chung F Diemunsch P Habib AS et al . Fourth consensus guidelines for the Management of Postoperative Nausea and Vomiting. Anesth Analg. (2020) 131:411–48. doi: 10.1213/ANE.0000000000004833
8.
Hui KK Nixon EE Vangel MG Liu J Marina O Napadow V et al . Characterization of the "deqi" response in acupuncture. BMC Complement Altern Med. (2007) 7:33. doi: 10.1186/1472-6882-7-33
9.
Yang XY Shi GX Li QQ Zhang ZH Xu Q Liu CZ . Characterization of deqi sensation and acupuncture effect. Evid Based Complement Alternat Med. (2013) 2013:319734
10.
Yan S Xu M Zou X Xiong Z Li H Yang J et al . Acupuncture combined with ondansetron for prevention of postoperative nausea and vomiting in high-risk patients undergoing laparoscopic gynaecological surgery: a randomised controlled trial. United European Gastroenterol J. (2023) 11:564–75. doi: 10.1002/ueg2.12421
11.
Cheong KB Zhang JP Huang Y Zhang ZJ . The effectiveness of acupuncture in prevention and treatment of postoperative nausea and vomiting--a systematic review and meta-analysis. PLoS One. (2013) 8:e82474. doi: 10.1371/journal.pone.0082474
12.
Chernyak GV Sessler DI . Perioperative acupuncture and related techniques. Anesthesiology. (2005) 102:1031–49. doi: 10.1097/00000542-200505000-00024
13.
Lee A Chan S . Acupuncture and anaesthesia. Best Pract Res Clin Anaesthesiol. (2006) 20:303–14. doi: 10.1016/j.bpa.2005.10.009
14.
Zhang MT Liang YF Dai Q Gao HR Wang H Chen L et al . A spinal neural circuit for electroacupuncture that regulates gastric functional disorders. J Integr Med. (2025) 23:56–65. doi: 10.1016/j.joim.2024.11.005
15.
Lee A Chan SK Fan LT . Stimulation of the wrist acupuncture point PC6 for preventing postoperative nausea and vomiting. Cochrane Database Syst Rev. (2015) 2015:Cd003281.
16.
Wang SM Kain ZN White P . Acupuncture analgesia: I. The scientific basis. Anesth Analg. (2008) 106:602–10. doi: 10.1213/01.ane.0000277493.42335.7b
17.
Witt CM Meissner K Pach D Thiele C Lüdtke R Ghadiyali Z et al . Stimulation of gastric slow waves with manual acupuncture at acupuncture points ST36 and PC6--a randomized single blind controlled trial. Neurogastroenterol Motil. (2012) 24:438-445, e211-432.
18.
Streitberger K Ezzo J Schneider A . Acupuncture for nausea and vomiting: an update of clinical and experimental studies. Auton Neurosci. (2006) 129:107–17. doi: 10.1016/j.autneu.2006.07.015
19.
Boutron I Altman DG Moher D Schulz KF Ravaud P . CONSORT statement for randomized trials of nonpharmacologic treatments: a 2017 update and a CONSORT extension for nonpharmacologic trial abstracts. Ann Intern Med. (2017) 167:40–7. doi: 10.7326/M17-0046
20.
MacPherson H Altman DG Hammerschlag R Li Y Wu T White A et al . Revised standards for reporting interventions in clinical trials of acupuncture (STRICTA): extending the CONSORT statement. Acupunct Med. (2010) 28:83–93. doi: 10.1136/aim.2009.001370
21.
Moher D Hopewell S Schulz KF Montori V Gøtzsche PC Devereaux PJ et al . CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. BMJ. (2010) 340:c869. doi: 10.1136/bmj.c869
22.
Chen W Li G Jiang K Song J Du R Yang H et al . Dexamethasone for postoperative nausea and vomiting in papillary thyroid carcinoma patients: a randomized clinical trial. J Am Coll Surg. (2022) 235:454–67. doi: 10.1097/XCS.0000000000000309
23.
Sonner JM Hynson JM Clark O Katz JA . Nausea and vomiting following thyroid and parathyroid surgery. J Clin Anesth. (1997) 9:398–402. doi: 10.1016/S0952-8180(97)00069-X
24.
Nam SW Do SH Hwang JW Park I Hwang I Na HS . Effects of opioid-sparing general anesthesia on postoperative nausea and vomiting in laparoscopic gynecological surgery. Korean J Anesthesiol. (2024) 77:605–13. doi: 10.4097/kja.24336
25.
Feng CD Xu Y Chen S Song N Meng XW Liu H et al . Opioid-free anaesthesia reduces postoperative nausea and vomiting after thoracoscopic lung resection: a randomised controlled trial. Br J Anaesth. (2024) 132:267–76. doi: 10.1016/j.bja.2023.11.008
26.
Albooghobeish M Mohtadi A Saidkhani V Fallah H Behaein K Nesionpour S et al . Comparison between effects of acupuncture and metoclopramide on postoperative nausea and vomiting after gynaecological laparoscopy: a randomized controlled trial. Anesth Pain Med. (2017) 7:e12876. doi: 10.5812/aapm.12876
27.
Han XR Yue W Chen HC He W Luo JH Chen SX et al . Treatment duration of wrist-ankle acupuncture for relieving post-thyroidectomy pain: a randomized controlled trial. J Integr Med. (2023) 21:168–75. doi: 10.1016/j.joim.2023.02.001
28.
Han Z Zhang X Yang H Yuan P Wang H Du G . Suggested electroacupuncture for postoperative nausea and vomiting: a comprehensive Meta-analysis and systematic review of randomized controlled trials. Med Sci Monit. (2023) 29:e941262
29.
Chen ZY Lin L Wang HH Zhou Y Yan JQ Huang YL et al . Ondansetron combined with ST36 (Zusanli) acupuncture point injection for postoperative vomiting. Acupunct Med. (2014) 32:124–31. doi: 10.1136/acupmed-2013-010340
30.
Yan Y López-Alcalde J Zhang L Siebenhüner AR Witt CM Barth J . Acupuncture for the prevention of chemotherapy-induced nausea and vomiting in cancer patients: a systematic review and meta-analysis. Cancer Med. (2023) 12:12504–17. doi: 10.1002/cam4.5962
31.
Cechetto DF Diab T Gibson CJ Gelb AW . The effects of propofol in the area postrema of rats. Anesth Analg. (2001) 92:934–42. doi: 10.1097/00000539-200104000-00027
32.
Li S Song B Li Y Zhu J . Effects of intravenous Anesthetics vs inhaled Anesthetics on early postoperative sleep quality and complications of patients after laparoscopic surgery under general Anesthesia. Nat Sci Sleep. (2021) 13:375–82. doi: 10.2147/NSS.S300803
33.
Logginidou HG Li BH Li DP Lohmann JS Schuler HG DiVittore NA et al . Propofol suppresses the cortical somatosensory evoked potential in rats. Anesth Analg. (2003) 97:1784–8. doi: 10.1213/01.ANE.0000090318.16879.A8
34.
Armour M Smith CA . Treating primary dysmenorrhoea with acupuncture: a narrative review of the relationship between acupuncture 'dose' and menstrual pain outcomes. Acupunct Med. (2016) 34:416–24. doi: 10.1136/acupmed-2016-011110
35.
Bauer M McDonald JL Saunders N . Is acupuncture dose dependent? Ramifications of acupuncture treatment dose within clinical practice and trials. Integr Med Res. (2020) 9:21–7. doi: 10.1016/j.imr.2020.01.003
36.
Myles PS Shulman MA Reilly J Kasza J Romero L . Measurement of quality of recovery after surgery using the 15-item quality of recovery scale: a systematic review and meta-analysis. Br J Anaesth. (2022) 128:1029–39. doi: 10.1016/j.bja.2022.03.009
37.
Sethi N Dutta A Puri GD Sood J Choudhary PK Gupta M et al . Evaluation of quality of recovery with quality of Recovery-15 score after closed-loop Anesthesia delivery system-guided propofol versus desflurane general Anesthesia in patients undergoing transabdominal robotic surgery: a randomized controlled study. Anesth Analg. (2024) 138:1052–62. doi: 10.1213/ANE.0000000000006849
38.
Zhao W Xun J Yuan X Huang J Bai J . Efficacy of traditional Chinese medicine in the conservative management of complete small intestinal obstruction post-gastric cancer surgery: a case report. Explore (NY). (2025) 21:103080. doi: 10.1016/j.explore.2024.103080
39.
Choi EK Seo Y Lim DG Park S . Postoperative nausea and vomiting after thyroidectomy: a comparison between dexmedetomidine and remifentanil as part of balanced anesthesia. Korean J Anesthesiol. (2017) 70:299–304. doi: 10.4097/kjae.2017.70.3.299
Summary
Keywords
acupuncture, propofol anesthesia, thyroidectomy, postoperative nausea and vomiting, recovery quality
Citation
Zhao W, Jiao S, Peng B, Zhang S, Tong T, Hu T, An N, Wei S and Liu H (2025) Clinical trial effects of acupuncture combined with different general anesthesia on postoperative nausea and vomiting and early recovery after thyroidectomy with intra-operative neuromonitoring: a randomized controlled trial. Front. Med. 12:1650403. doi: 10.3389/fmed.2025.1650403
Received
19 June 2025
Accepted
29 September 2025
Published
16 October 2025
Volume
12 - 2025
Edited by
Marco Fiore, Università degli Studi della Campania 'Luigi Vanvitelli', Italy
Reviewed by
Haihua Shu, Guangdong Provincial People's Hospital, China
Xuli Ren, Jilin University, China
Updates
Copyright
© 2025 Zhao, Jiao, Peng, Zhang, Tong, Hu, An, Wei and Liu.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Huaqin Liu, liuhuaqin@hebmu.edu.cn
†These authors have contributed equally to this work
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.