- Department of Diagnostic Radiology, College of Applied Medical Sciences, University of Hail, Hail, Saudi Arabia
Background: The utilization of gonad shields in interventional radiology (IR) settings plays a pivotal role in minimizing radiation risk for practitioners.
Purpose: This study aims to assess the impact of experience, practitioners’ opinion, education in radiation protection, practitioners’ gender, workload, and educational level on the use of gonad shields.
Methods: This cross-sectional questionnaire study comprised six hypotheses that were designed to fulfill the study’s aim. Normality was assessed using skewness and kurtosis values within a specified threshold. Categorical variables were assessed using cross-tabulation and the chi-square (χ2) test of independence. A p-value of <0.05 was considered statistically significant.
Results: The study included 527 participants (307 female and 220 male). There was a significant inverse association between years of experience and the frequency of gonad shield use (p < 0.05). A direct relationship was observed between practitioners’ opinions on the importance of gonad shields and shield usage frequency (p < 0.05). It was clear that attending radiation protection training was more likely to encourage practitioners to follow gonad shielding protocols (p < 0.05). No significant effect of gender and gonad shield usage was observed (p = 0.086). Practitioners with higher annual caseloads (>200 cases/year) reported more consistent use of gonad shields (p < 0.05).
Conclusion: Practice length, but not workload, is inversely related to IR staff’s attitude toward gonad shield use. Continuous radiation protection training is crucial for improving IR staff commitment to safety standards. No impact of gender on gonad shield usage was observed. Targeted refresher training, reinforcement of local guidance, and ensuring shield availability/workflow integration may strengthen occupational radiation-safety adherence in IR units.
1 Introduction
Charles Dotter first conceptualized interventional radiology (IR) in 1963 (1), with the first arterial angioplasty performed in 1964 on an 82-year-old woman using a guide wire and coaxial Teflon catheters (2). This marked the successful introduction of a new minimally invasive medical imaging and therapy technology that uses ionizing radiation for diagnosis and treatment (3).
Fluoroscopy-guided interventions necessitate the practitioner’s proximity to the patient for real-time visualization and guidance; therefore, maintaining distance, a primary radiation safety measure, is not always feasible. Although radiation offers significant benefits in diagnosing and treating patients, it also carries inherent risks for healthcare practitioners, including cancer and reproductive hazards (4–7). Consequently, IR practitioners should carefully consider the balance between the merits of high-fidelity imaging and the risks inherent to radiation exposure to maintain radiation doses as low as reasonably achievable (ALARA) (8). Contemporary studies report disparities in the application of radiation-protection behaviors, thus reinforcing the need for operator-focused shielding within ALARA-based programs and local protocols (9–16).
For IR practitioners, protective shields help reduce occupational radiation exposure during fluoroscopy-guided IR. Gonad shields are designed to minimize radiation exposure to sensitive reproductive organs, lowering the risk of genetic damage and reproductive problems; this is crucial in interventional radiology, especially for men, because of the vulnerability of male reproductive tissue to radiation (17, 18). However, evidence on operators’ actual use of gonad shields remains limited, particularly in Saudi Arabia. Prior surveys have focused on general radiation safety knowledge or patient shielding rather than operator gonad shielding. Few studies measure how other factors, such as training, years of IR experience, gender, and annual workload, relate to practice in real clinical environments (9, 10, 12–14).
To address this gap, we conducted a multi-institutional survey of IR practitioners in Saudi Arabia focusing on knowledge, attitudes, and practices (KAP) regarding operator gonad shields and potential determinants, such as training, experience, workload, education, availability, local guidance, and gender. Unlike previous studies that concentrated on broad safety education or patient safeguards, our research quantifies the use of operator shields by the interventional radiology workforce in Saudi Arabia.
2 Materials and methods
2.1 Study design and setting
This analytical cross-sectional study was conducted across multiple healthcare institutions in Saudi Arabia. The study aims to identify the factors influencing gonad shield utilization during fluoroscopy-guided IR procedures. A structured, self-administered electronic questionnaire was distributed to 527 IR practitioners. Data were collected between September 2024 and February 2025.
2.2 Participations
Eligible participants were practicing radiology professionals involved in fluoroscopy-guided IR, including radiologists, IR fellows/registrars, and technologists/radiographers, who were working in Saudi Arabia during the study period. Individuals outside IR, those not engaged in fluoroscopy-guided procedures, and incomplete submissions were excluded. A total of 527 practitioners completed the questionnaire.
Using a conservative single-proportion approach (p = 0.50, margin of error d = 0.05, Z = 1.96), the minimum required sample size (N) was 384, based on the Charan and Biswas formula. The actual sample size (N = 527) exceeds this requirement, resulting in narrower confidence intervals for prevalence/awareness estimates and supporting the planned subgroup and multivariable analyses. The formula and derivation are shown in Supplementary file.
2.3 Data collection
Using a structured self-report questionnaire, data were collected through institutional contacts and professional networks. Participation was voluntary and anonymous, and questionnaires were specifically designed to capture demographics, professional profile, experience, knowledge, attitudes, departmental guidance, and practices related to gonad shield use in IR.
2.4 Research instrument
The questionnaire was developed through a targeted literature review and researcher-created items tailored to fluoroscopy-guided IR. It comprises three sections: informed consent, participant demographics, and IR practices with gonad shield use (Supplementary Table S1). We hypothesized that viewing shielding as important, alongside higher caseloads, would be linked to increased use, and greater experience would correlate with lower use. Training and local guidance would encourage greater protocol adherence, in addition to the influences of educational level and gender (Supplementary Table S2).
2.5 Statistical analysis
Data analysis was performed using IBM SPSS Statistics Version 20 and Microsoft Excel. The formula developed by Charan and Biswas was used to determine the sample size (Supplementary file) (19). The reliability was assessed using the Cronbach’s Alpha Reliability Test. Skewness and kurtosis values were assessed to confirm the normality of the data. Normality was assumed when the skewness and kurtosis values were within the ranges of ±2 and ±4, respectively (20). Cross-tabulation and the chi-square test of independence (χ2) were used to analyze categorical data and evaluate the relationships between practitioner characteristics and shielding-related outcomes (21), in addition to proportional-odds ordinal logistic regression (OLR) with a 95% confidence interval. Gender was analyzed using χ2 only, because the corresponding outcome was nominal and lacked an inherent order, making OLR inappropriate. Cramér’s V was used to analyze the effect size. Responses were summarized as n (%) using available-case denominators. A p-value of < 0.05 was considered statistically significant.
2.6 Ethical consideration
The Research Ethics Committee (REC) reviewed and approved this research (H-2024-407, 02/09/2024 G). Informed consent was obtained from every participant before their involvement. Participant anonymity was preserved; no names or identifying data were included.
3 Results
3.1 Participant characteristics and key responses
The study involved 527 interventional radiology practitioners (Supplementary file), of which there were 307 (58.3%) women and 220 (41.7%) men. Key shield-related variables are summarized in Table 1 (availability, use frequency, training, and local guidance). Additional demographics, including marital status, educational level, years of experience, and annual workload, are reported in the Supplementary file and Supplementary Table S1.
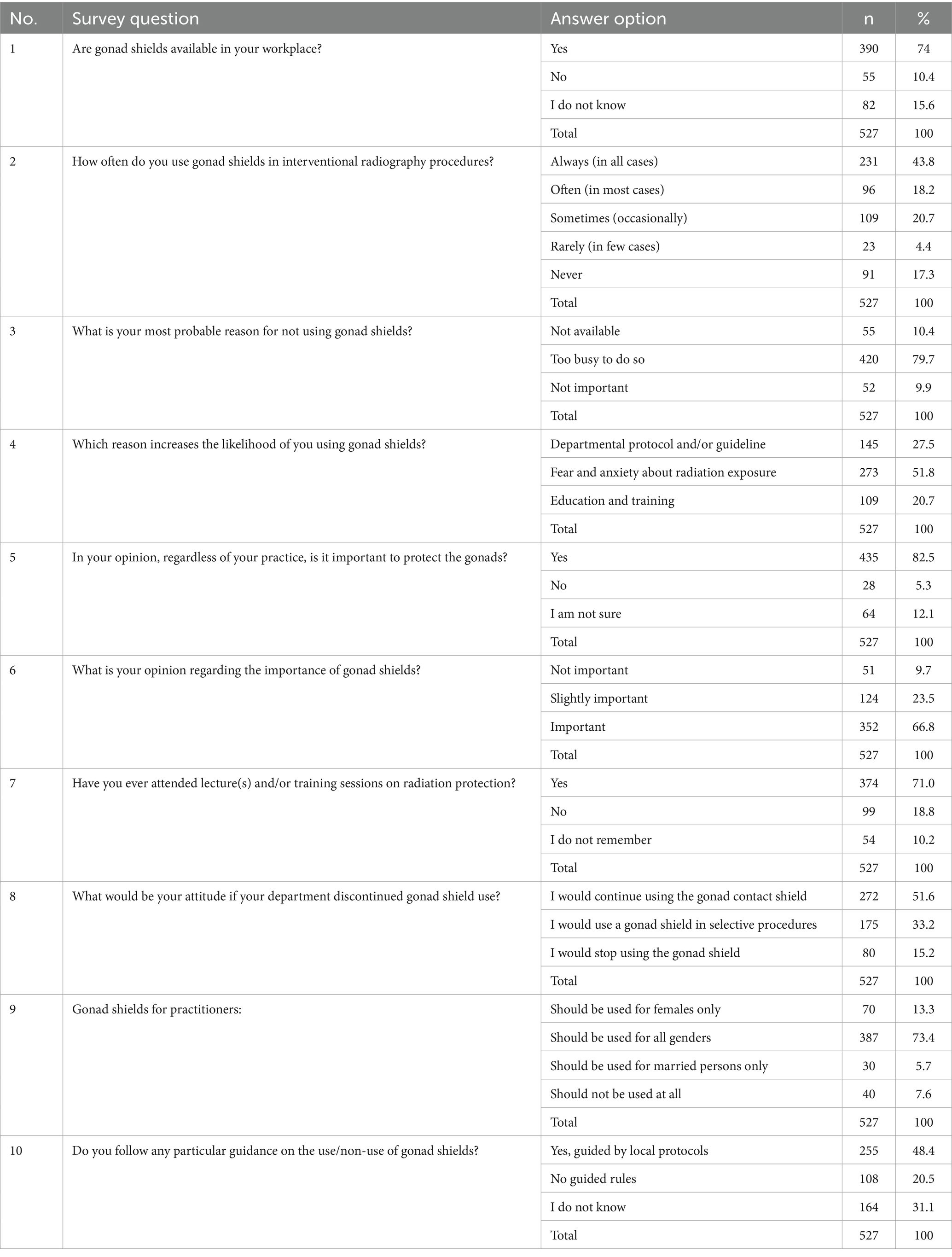
Table 1. Questionnaire responses to structured items for measuring practitioner behaviors and perspectives in gonad shield usage (N = 527).
3.2 Data analysis
Table 1 summarizes participants’ responses to 10 questionnaire items that cover the availability, frequency, attitudes, awareness, and institutional guidance related to gonad shield use in IR. The consistency was assessed using Cronbach’s alpha, and the Cronbach’s alpha value was 0.874 [>0.7 (22)]. Therefore, it is reasonable to state that the study questionnaire demonstrates high reliability. The normality test was performed on the items listed in Table 1, using the skewness and kurtosis thresholds (±2 and ±4, respectively). Most of the items exhibited skewness and kurtosis within the expected range, which implies a normal distribution.
In the analysis of the effect of experience on gonad shield usage, cross-tabulation showed an apparent decline in gonad shield usage as experience increased (Figure 1). A chi-square test confirmed a statistically significant association between experience and usage frequency, χ2 = 88.83, p = 8.3 × 10−14 (p < 0.05), Cramér’s V = 0.24. Years of experience were inversely related to gonad shield usage frequencies. Ordinal logistic regression further demonstrated that all experience groups of more than 0–4 years were significantly less likely to report higher usage frequencies (p < 0.05). The regression coefficients and confidence intervals demonstrate the decreasing likelihood of consistent shield use with increasing years of experience (Supplementary Figure S1).
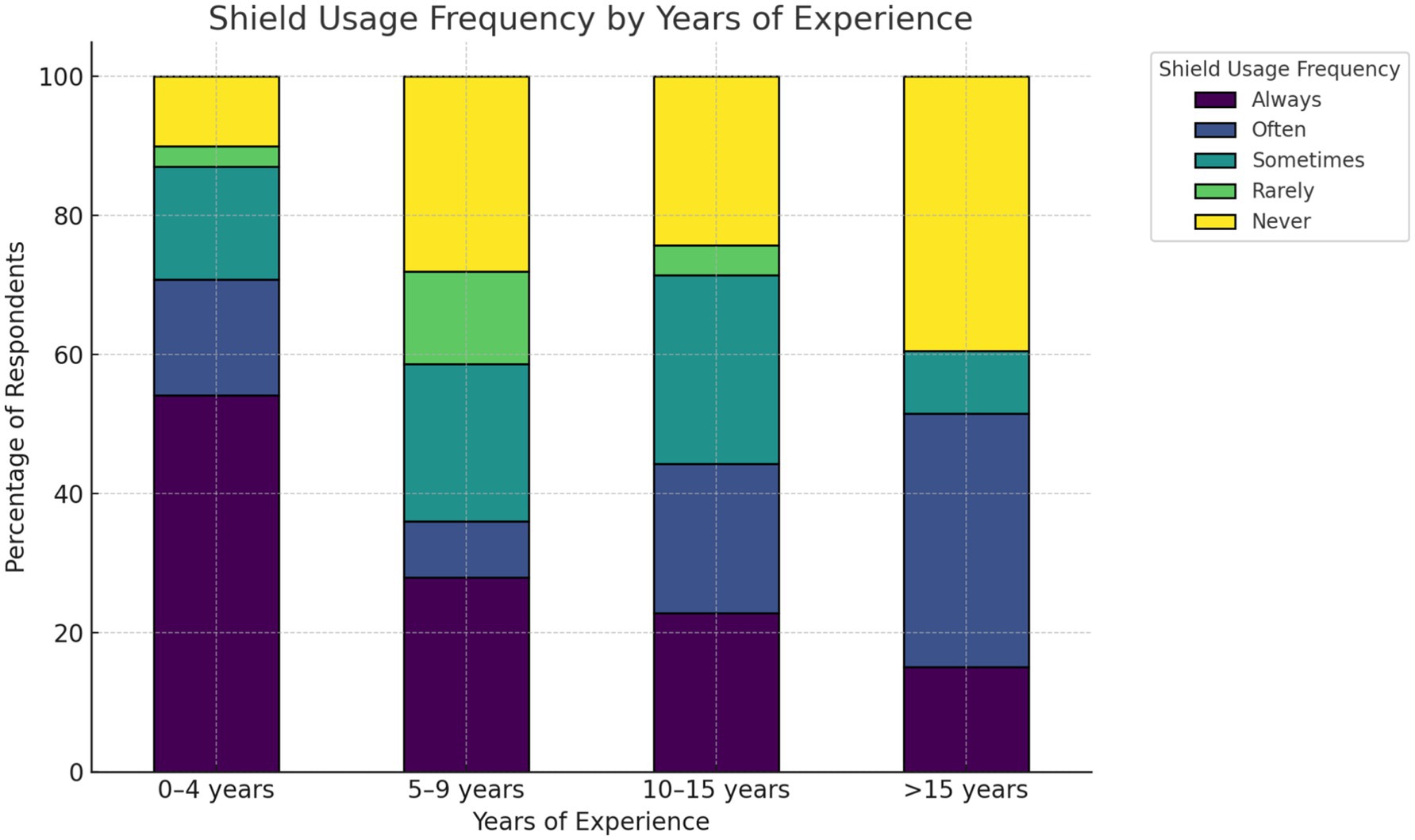
Figure 1. Years of experience vs. frequency of gonad-shield use. Stacked columns show column-wise percentages of usage within each experience group.
In terms of attitudinal salience, recognizing the need to protect the gonads strongly correlates with more frequent use (Figure 2). Respondents who were unsure (and, to a lesser extent, those not in favor) clustered in lower-use categories: χ2 = 94.19, p = 6.53 × 10−17 (<0.05), Cramér’s V = 0.30. The relationship is moderate in strength and is supported in direction by OLR (Supplementary Figure S2).
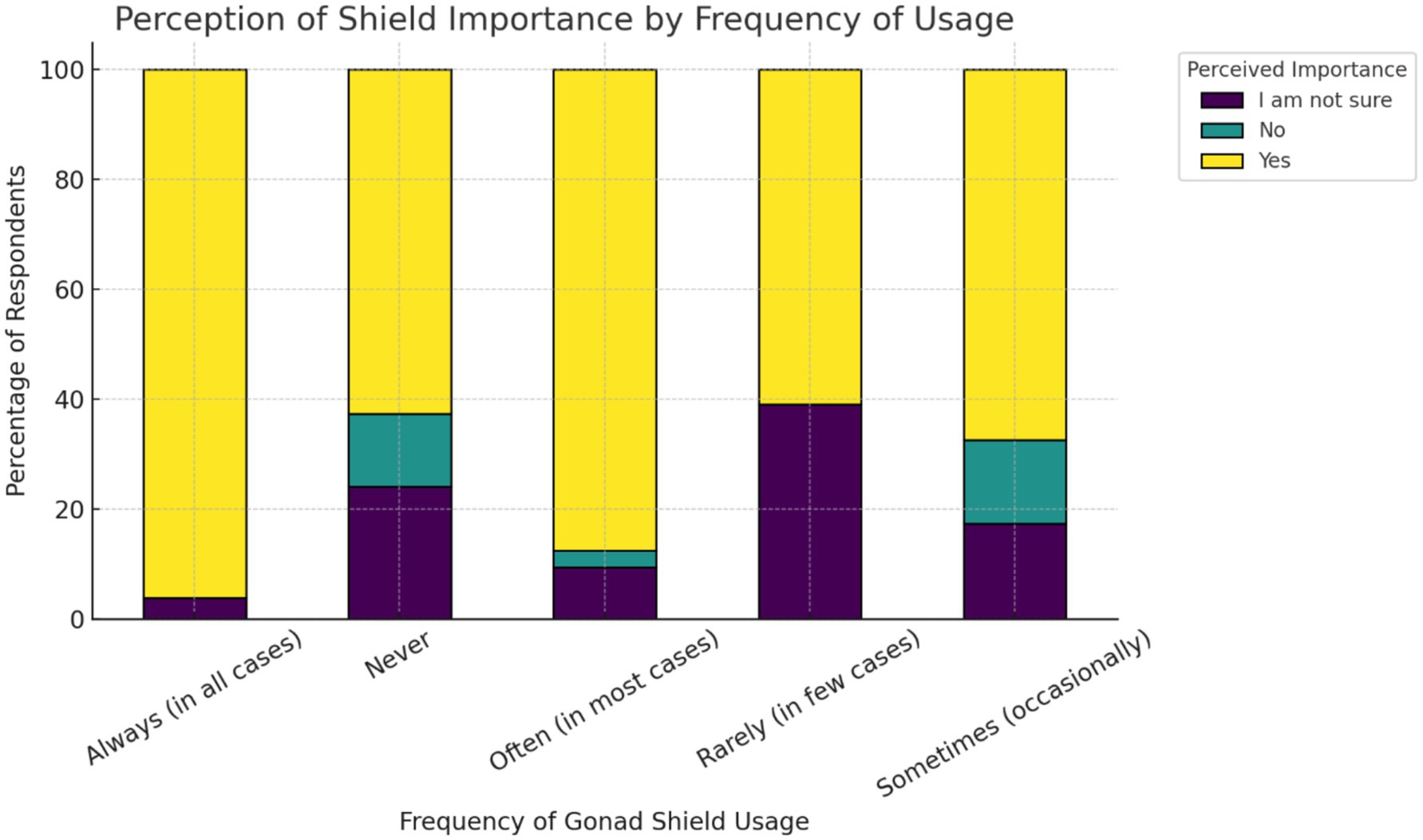
Figure 2. Stacked percentage bar chart illustrates the perceived importance of shielding by frequency of usage.
Regarding radiation protection awareness and gonad shield use, cross-tabulation revealed that practitioners who reported attending radiation protection training were significantly more likely to follow local gonad shielding protocols (Figure 3).
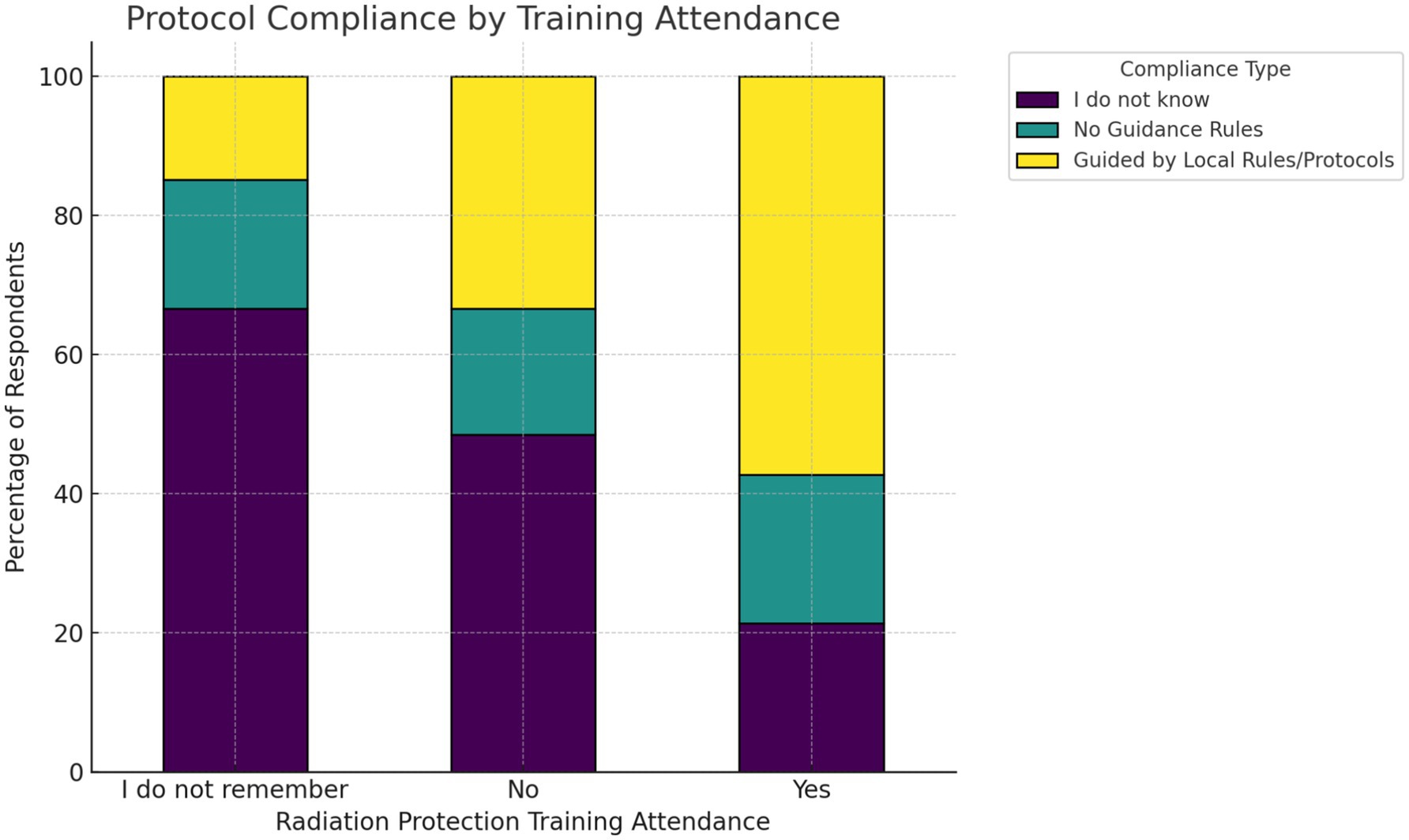
Figure 3. The stacked percentage bar chart displays the distribution of protocol compliance as a function of radiation protection training attendance.
Furthermore, among those trained, more than half indicated adherence to official guidance, whereas those who did not attend or could not recall attending training showed greater uncertainty or lack of awareness of protocols. The chi-square test confirmed a strong association between training attendance and compliance behavior (χ2 = 66.65, df = 4, p = 1.16 × 10−13 (<0.0001), Cramér’s V = 0.25). This small to moderate correlation corresponds with higher adjusted odds of compliance among trained practitioners (Supplementary Figure S3).
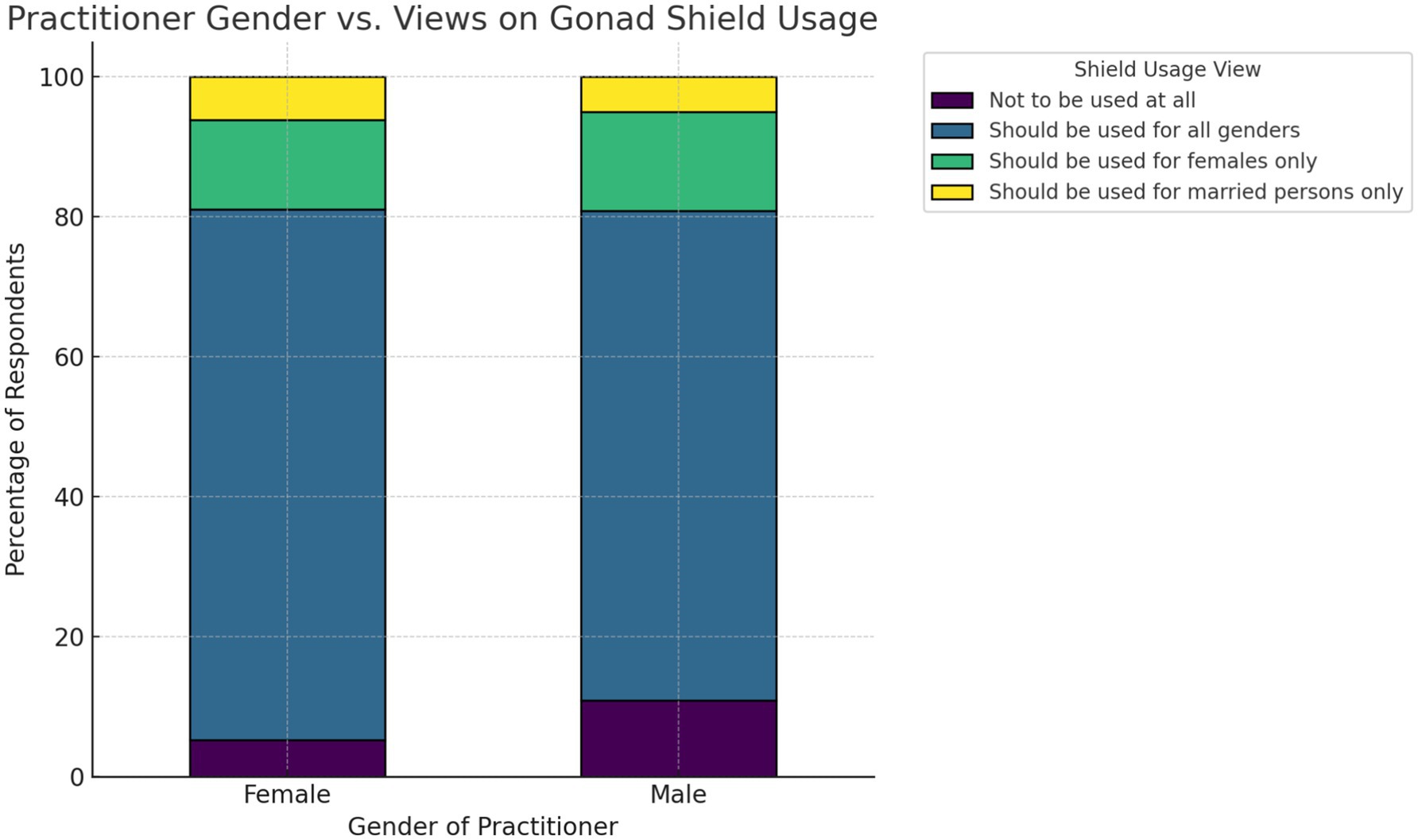
The analysis of gender type and adherence to gonad shield usage through cross-tabulation showed that both male and female practitioners primarily favor the use of gonad shields (Figure 4). The chi-square test indicated no statistically significant association between practitioner gender and views on shield usage (χ2 = 6.59, df = 3, p-value = 0.086, Cramér’s V = 0.11); furthermore, no OLR was fitted.
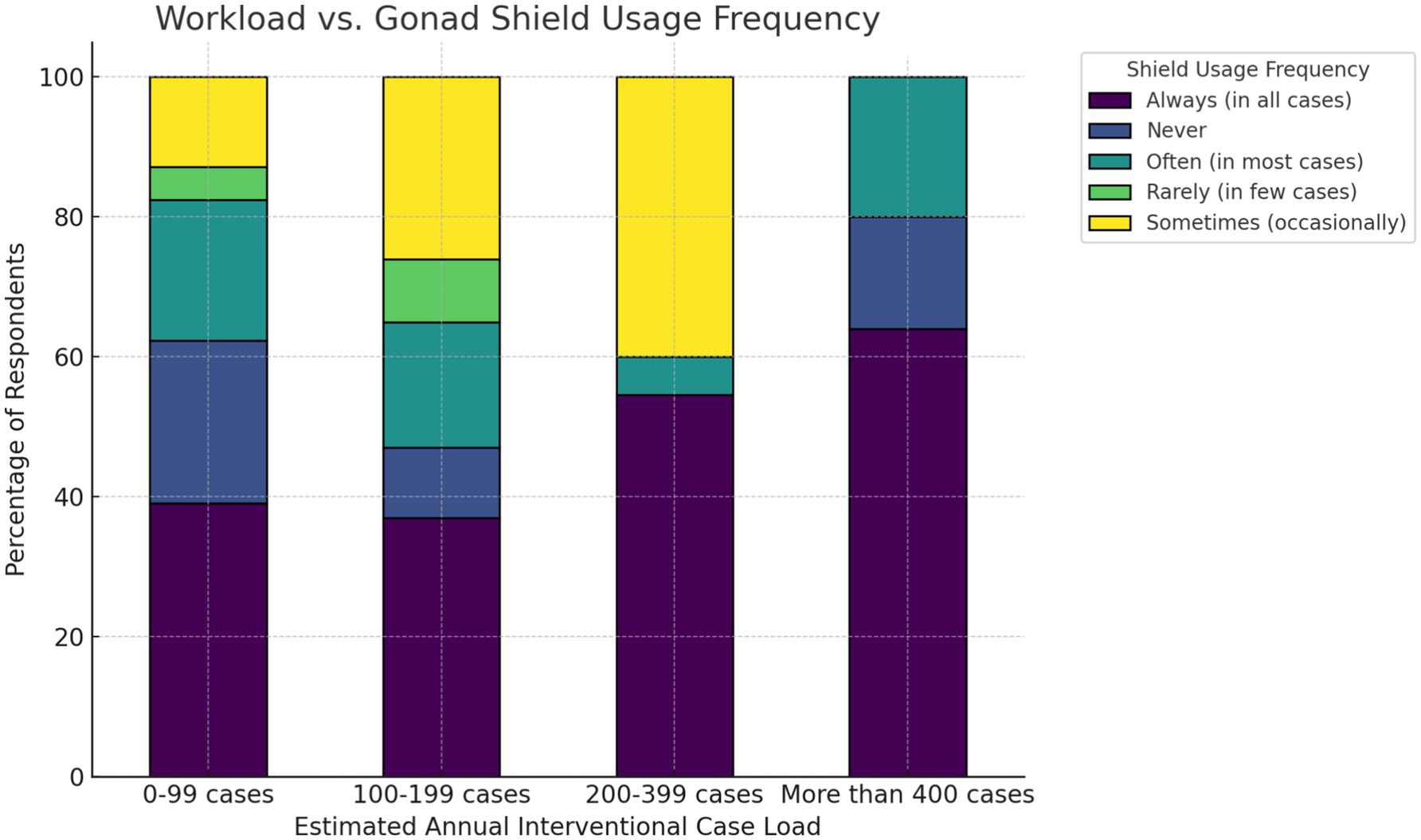
Considering the workload and use of the gonad shield, it is evident that workload was negatively linked to shield usage (Figure 5). Practitioners with higher annual caseloads (>200 cases/year) reported more consistent use of gonad shields, whereas those with lower volumes (0–99 cases/year) showed a greater variation in shield use, including more instances of non-use or occasional use. The chi-square test confirmed a statistically significant association between workload and shield usage frequency (χ2 = 85.27, df = 12, p = 4.03 × 10−13 (<0.05), Cramér’s V = 0.23). Ordinal logistic regression supported this pattern (Supplementary Figure S4).
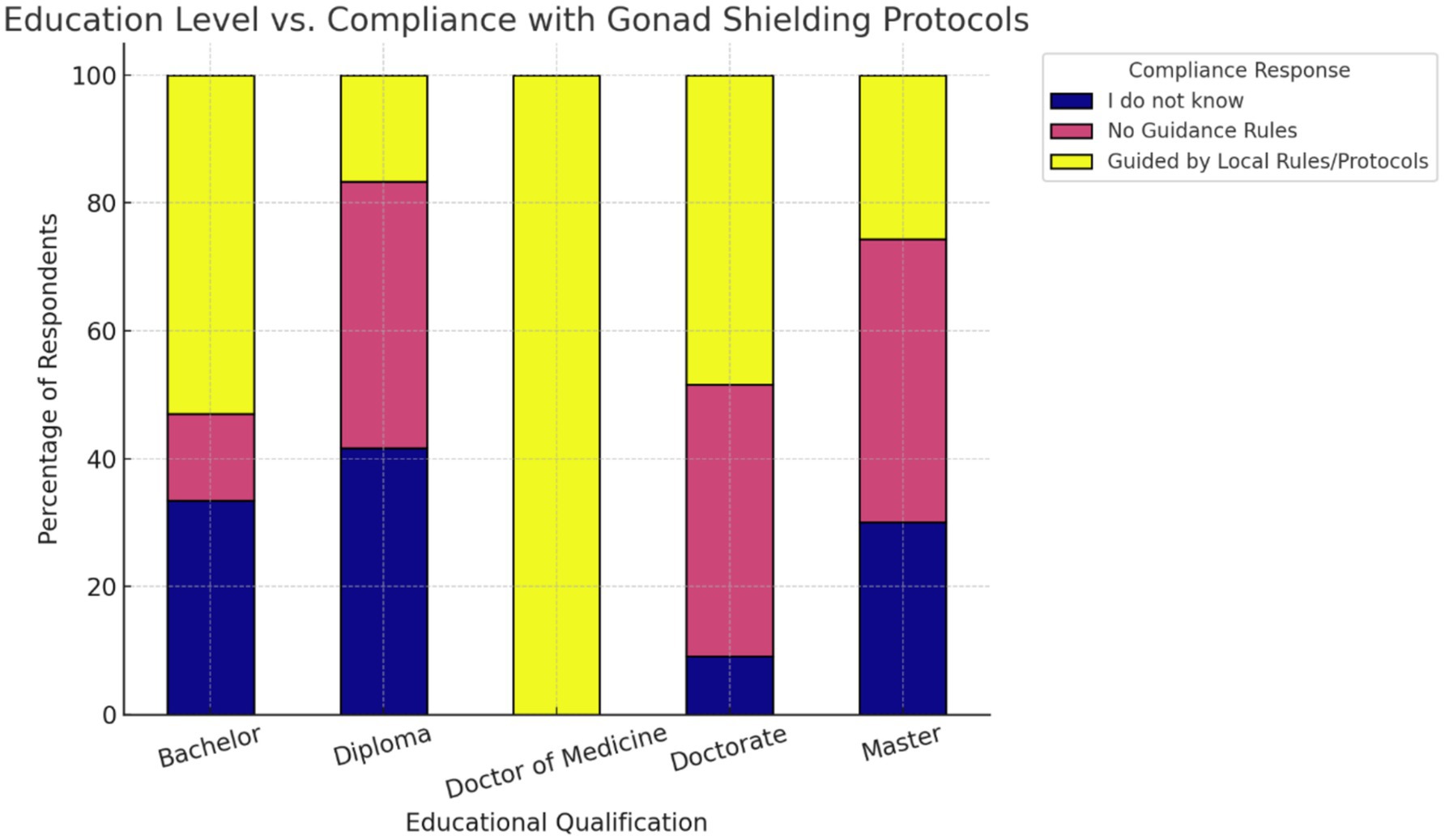
Finally, we examined whether educational attainment was connected to protocol adherence. Bachelor’s degree holders exhibited the highest proportion reporting guided practice. In contrast, those with diplomas and master’s degrees showed a broader distribution, with a greater proportion selecting “No Guidance Rules” or “I do not know” (Figure 6). The chi-square test indicated a statistically significant relationship between education level and compliance behavior (χ2 = 73.82, df = 8, p-value = 8.5 × 10−13 (<0.05), Cramér’s V = 0.26). Counts for Doctor of Medicine were very small, so these proportions should be interpreted cautiously (Supplementary Figure S5).
4 Discussion
The most significant source of man-made radiation is medical imaging, which uses radiation for diagnosis and other purposes. IR is an emerging technology that enables accurate diagnosis and targeted therapy, thereby effectively enhancing patient care (23). The gonads are among the most sensitive organs to radiation and may be prone to stochastic risks [ICRP 103; (24)]. The main source of gonadal exposure for staff is the non-primary X-ray beam, which results from internal scatter radiation within the patient (11, 15, 25). Even when a lead apron is used, exposure to the gonads from scattered radiation during upper limb surgical procedures with C-arm fluoroscopy has been documented (26). Furthermore, radiation exposure to the gonads before conception may increase the incidence of hereditary effects (27, 28). Although wearing gonad shields can reduce gonadal exposure by up to 98% (29), staff use of gonad shields has been reported as occasional (30).
This cross-sectional multi-center study was designed to explore the level of awareness regarding the use of gonad shields during fluoroscopy-guided IR procedures.
According to practitioners’ feedback, years of experience were found to be inversely associated with the commitment to gonad shield usage (p-value < 0.05). Studies on the staff (with no consideration for the year of experience) reported a lack of significant commitment to the usage of radiation protection shielding (12, 14). A recent study has reported a similar inverse association of years of experience as a function of commitment to radiation protection practices (31), which was in agreement with our findings. Another study involving medical radiation workers in multi-unit facilities found a direct link between the two factors (32). Our study was conducted on IR unit workers, potentially clarifying the contradictions. Therefore, this finding suggests that educational and policy interventions should not only focus on early-career practitioners (Figure 1) but also on more experienced professionals.
Regarding the opinion of practitioners on the importance of gonad shield usage, the analysis of the feedback indicated a clear relationship between perceived importance and actual usage behavior (Figure 2). Practitioners who acknowledged the importance of shielding were more likely to use gonad shields consistently, while those who were unsure of its relevance exhibited minimal behavioral distinction from those who outright dismissed it. This implies that educational efforts must focus on reshaping underlying beliefs to effectively drive protective behaviors. This has also been observed in another hypothesis of the study, where radiation protection training was shown to play a formative role in enhancing adherence to protocols. Practitioners who received formal training were substantially more likely to comply with gonad shield usage guidelines (Figure 3). Thus, institutions should ensure that safety training is both structured and periodically refreshed to maximize retention and clinical application. This finding is in agreement with numerous studies (9, 10, 13, 16, 33, 34). Additionally, a study concerning the occupational radiation dose for IR staff demonstrated significant variation in radiation exposure to different body parts. Thus, a departmental protocol for radiation protection practices may be essential (35). In the gender-based analysis, it was shown that gender has no statistically significant effect on the use of gonad shields (p = 0.0.086). This finding has also been demonstrated in other studies (12, 14, 16, 31, 36, 37).
The workload and frequency of the gonad shield showed a linear relationship (Figure 5). A higher workload (>200 cases/year) may affect staff commitment to radiation protection practices. This may also explain the significant association observed in the second hypothesis, where practitioners’ opinions on the importance of gonad shield usage could reflect caseloads rather than their awareness of safety practices. Therefore, targeted educational intervention and training on shielding application may lead to improved consistency in the use of gonad protective shielding among practitioners (38).
Finally, a significant relationship between educational attainment and gonad shield protocol compliance was observed, where diploma- and master’s-level practitioners were less likely to adhere to the protocol compared to bachelor’s, while doctorate holders did not significantly differ. This non-linear association suggests that higher qualifications do not always translate into better radiation protection practices, potentially due to gaps between theoretical knowledge and adherence to clinical protocols (13, 39).
Consistent with the literature, the findings highlight the importance of education and structured training that could enhance compliance and address gaps in knowledge, suggesting that targeted and stratified training programs for various educational backgrounds could improve the alignment of radiation protection practices with institutional protocols. Thus, awareness and implementation of proper radiation protection practices are paramount to minimize the radiation risk and negative biological effects among practitioners on the IR unit (40). Additionally, a similar study could be conducted to examine staff’s perceptions of the recently published guidelines on the use of gonad shields (not only for patients).
This study has limitations. Its cross-sectional design restricts causative interpretations. Additionally, reliance on self-reported questionnaires introduces potential response bias. The findings are also geographically limited, which may affect their broader applicability. Future research should expand on these aspects by including longitudinal designs, broader sampling, and qualitative methods to deepen the understanding of radiation safety practices in IR units.
5 Conclusion
Interventional radiology staff views on gonad shields are inversely related to their years of practice but not to workload. Maintaining radiation protection training is crucial for better compliance with safety standards in interventional radiology. The impact of gender on gonad shield use was insignificant. Educational attainment was found to be associated with adherence to gonad shield protocols. Radiation protection protocols in interventional radiology are essential. This study could assist radiation safety officers in developing strategies to enhance staff adherence to safety regulations.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material; further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Research Ethics Committee (REC) at University of Hail (H-2024-407, 02/09/2024 G). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
MA: Resources, Supervision, Data curation, Project administration, Writing – original draft, Conceptualization, Writing – review & editing, Visualization, Investigation, Methodology, Validation. AA: Data curation, Methodology, Writing – original draft, Conceptualization. MH: Writing – review & editing, Software, Methodology, Investigation, Project administration, Formal analysis, Data curation.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2025.1655457/full#supplementary-material
References
1. Costello, JS, Soldozy, S, Norat, P, Sokolowski, JD, Yağmurlu, K, Sharifi, K, et al. Endovascular approach to cerebral revascularization: historical vignette. World Neurosurg. (2020) 136:258–62. doi: 10.1016/j.wneu.2020.01.072
2. Mottareale, R, Manna, F, Carmosino, PA, Fiore, F, Correra, M, Stilo, S, et al. Exposure time dependence of operators’ head entrance air kerma in interventional radiology measured by TLD-100H chips. Sensors. (2025) 25:3666. doi: 10.3390/s25123666
3. Weiss, CR, and Hafezi-Nejad, N. Interventional radiology: past, present, and future. Radiology. (2023) 308:e230809. doi: 10.1148/radiol.230809
4. Hauptmann, M, Daniels, RD, Cardis, E, Cullings, HM, Kendall, G, Laurier, D, et al. Epidemiological studies of low-dose ionizing radiation and Cancer: summary Bias assessment and Meta-analysis. JNCI Monographs. (2020) 2020:188–200. doi: 10.1093/jncimonographs/lgaa010
5. Garcia-Sayan, E, Jain, R, Wessly, P, Mackensen, GB, Johnson, B, and Quader, N. Radiation exposure to the interventional Echocardiographers and sonographers: a call to action. J Am Soc Echocardiogr. (2024) 37:698–705. doi: 10.1016/j.echo.2024.03.002
6. Preda, A, Bonvicini, E, Coradello, E, Testoni, A, Gigli, L, Baroni, M, et al. The Fluoroless future in electrophysiology: a state-of-the-art review. Diagnostics. (2024) 14:182. doi: 10.3390/diagnostics14020182
7. Little, MP, Bazyka, D, de Gonzalez, AB, Brenner, AV, Chumak, VV, Cullings, HM, et al. A historical survey of key epidemiological studies of ionizing radiation exposure. Radiat Res. (2024) 202:432–87. doi: 10.1667/RADE-24-00021.1
8. Boice, J, Dauer, LT, Kase, KR, Mettler, FA, and Vetter, RJ. Evolution of radiation protection for medical workers. Br J Radiol. (2020) 93:282. doi: 10.1259/bjr.20200282
9. O’Rourke, M, et al. An investigation into the knowledge, attitudes, and practice of radiation protection in interventional radiology and cardiac catheter-laboratories. J Med Imaging Radiat Sci. (2024) 55:101440. doi: 10.1016/j.jmir.2024.101440
10. Patel, S, Jenkins, P, Zhong, J, Liu, W, Harborne, K, Modi, S, et al. Better safe than so ray: national survey of radiation protection amongst interventional radiology trainees in the United Kingdom. Br J Radiol. (2023) 96:71. doi: 10.1259/bjr.20230071
11. NCRP. NCRP recommendations for ending routine gonadal shielding during abdominal and pelvic radiography. NCRP. (2021) 13:1–8. Available at: https://ncrponline.org/wp-content/themes/ncrp/PDFs/Statement13.pdf
12. Elzaki, M, Osailan, R, Almehmadi, R, Zulaibani, A, Kamal, E, Gareeballah, A, et al. Knowledge and comprehension of radiation protection among radiography professionals and interns in western Saudi Arabia. J Radiat Res Appl Sci. (2025) 18:101243. doi: 10.1016/j.jrras.2024.101243
13. Elmorabit, N, Marrakchi, A, Chelh, FZ, Zaizoune, S, Azougagh, M, and Ennibi, O. Knowledge and practices of interventional radiology staff regarding radiation protection. Multidisciplinary Rev. (2024) 8:2025062. doi: 10.31893/multirev.2025062
14. Dias Cardoso, CEM, Bezzina, P, and Portelli, JL. Gonad contact shielding in digital radiography: a questionnaire survey. Eur J Radiol. (2023) 158:110620. doi: 10.1016/j.ejrad.2022.110620
15. British Institute of Radiology. Exposure. Pediatr Radiol. (2021) 51:152–4. doi: 10.1007/s00247-020-04887-8
16. Bazzi, M, Afram, SS, Ndipen, IM, Kåreholt, I, and Bjällmark, A. Factors affecting radiographers’ use of dose-reduction measures. J Radiol Prot. (2024) 44:011506. doi: 10.1088/1361-6498/ad1fde
17. Rizik, DG, Gosselin, KP, Burke, RF, and Goldstein, JA. Comprehensive radiation shield minimizes operator radiation exposure in coronary and structural heart procedures. Cardiovasc Revasc Med. (2024) 64, 70–75. doi: 10.1016/j.carrev.2024.02.015
18. Rizik, DG, Riley, RD, Burke, RF, Klassen, SR, Nigoghosian, AM, Gosselin, KP, et al. Comprehensive radiation shield minimizes operator radiation exposure and obviates need for Lead aprons. J Soc Cardiovasc Angiogr Intervent. (2023) 2:100603. doi: 10.1016/j.jscai.2023.100603
19. Charan, J, and Biswas, T. How to calculate sample size for different study designs in medical research? Indian J Psychol Med. (2013) 35:121–6. doi: 10.4103/0253-7176.116232
20. Nurul Hidayana Mohd, N, and Amirah Mohamad, F. Assessment of validity, reliability, and normality in quantitative study: a survey instrument analysis with IBM SPSS. Asian J Res Educ Soc Sci. (2025) 7:438–52. doi: 10.55057/ajress.2025.7.3.37
21. Agresti, A, and Kateri, M. Categorical data analysis In: M. Lovric (ed), International encyclopedia of statistical science. Berlin, Heidelberg: Springer Berlin Heidelberg (2025). 408–11.
22. Xu, X, Hong, WCH, Kolletar-Zhu, K, Zhang, Y, and Chi, C. Validation and application of the human aspects of information security questionnaire for undergraduates: effects of gender, discipline and grade level. Behav Inform Technol. (2024) 43:2799–820. doi: 10.1080/0144929X.2023.2260876
23. Brock, KK, Chen, SR, Sheth, RA, and Siewerdsen, JH. Imaging in interventional radiology: 2043 and beyond. Radiology. (2023) 308:e230146. doi: 10.1148/radiol.230146
24. The 2007 Recommendations of the International Commission on Radiological Protection. ICRP publication 103. Annals of the ICRP (2007) 37:1–332. doi: 10.1016/j.icrp.2007.10.003
25. Daniels, C, and Furey, E. The effectiveness of surface lead shielding of gonads outside the primary X-ray beam. J Med Imaging Radiat Sci. (2008) 39:189–91. doi: 10.1016/j.jmir.2008.09.001
26. Dadabhoy, M, Waldock, P, Brammar, T, Pryke, S, and Coomber, R. Gonad irradiation from fluoroscopy during upper limb orthopaedic procedures in a UK District general hospital. Br J Radiol. (2022) 95:87. doi: 10.1259/bjr.20211087
27. Stahl, CM, Meisinger, QC, Andre, MP, Kinney, TB, and Newton, IG. Radiation risk to the fluoroscopy operator and staff. Am J Roentgenol. (2016) 207:737–44. doi: 10.2214/AJR.16.16555
28. Green, LM, Dodds, L, Miller, AB, Tomkins, DJ, Li, J, and Escobar, M. Risk of congenital anomalies in children of parents occupationally exposed to low level ionising radiation. Occup Environ Med. (1997) 54:629–35. doi: 10.1136/oem.54.9.629
29. Kwok, K, Hasan, N, Duloy, A, Murad, F, Nieto, J, and Day, LW. American Society for Gastrointestinal Endoscopy radiation and fluoroscopy safety in GI endoscopy. Gastrointest Endosc. (2021) 94:685–697.e4. doi: 10.1016/j.gie.2021.05.042
30. Mohd Radzi, J, and Ananda Raj, ND. Assessment of knowledge and practice on radiation protection in radiological imaging among healthcare professionals at HPUniSZA. Asian J Med Biomed. (2023) 2023:9–20. doi: 10.37231/ajmb.2023.1.S.655
31. Esfahani, AJ, and Cheraghi, S. Radiation protection evaluation of medical X-ray imaging centers in Qazvin, Iran. Health Phys. (2021) 121:454–62. doi: 10.1097/HP.0000000000001453
32. Alavi, SS, Dabbagh, ST, Abbasi, M, and Mehrdad, R. Medical radiation workers’ knowledge, attitude, and practice to protect themselves against ionizing radiation in Tehran Province, Iran. J Educ Health Promot. (2017) 6:58. doi: 10.4103/jehp.jehp_126_15
33. Uthirapathy, I, Dorairaj, P, Ravi, S, and Somasundaram, S. Knowledge and practice of radiation safety in the catherization laboratory among interventional cardiologists – an online survey. Indian Heart J. (2022) 74:420–3. doi: 10.1016/j.ihj.2022.08.001
34. Moshfegh, S, et al. Evaluation of knowledge, attitude and practice of personnel in operating room, ERCP, and ESWL towards radiation hazards and protection. Middle East J Rehabil Health. (2017) 2017:354. doi: 10.5812/mejrh.12354
35. Kim, KP, Miller, DL, de Gonzalez, AB, Balter, S, Kleinerman, RA, Ostroumova, E, et al. Occupational radiation doses to operators performing fluoroscopically-guided procedures. Health Phys. (2012) 103:80–99. doi: 10.1097/HP.0b013e31824dae76
36. Ranada, RT, Tilson, E, and Clark, K. Factors affecting gonadal shielding use among technologists in California. Radiol Technol. (2024) 95:263–70.
37. Shabani, F, Hasanzadeh, H, Emadi, A, Mirmohammadkhani, M, Bitarafan-Rajabi, A, Abedelahi, A, et al. Radiation protection knowledge, attitude, and practice (KAP) in interventional radiology. Oman Med J. (2018) 33:141–7. doi: 10.5001/omj.2018.26
38. MacKay, M, Hancy, C, Crowe, A, D’Rozario, R, and Ng, C. Attitudes of medical imaging technologists on use of gonad shielding in general radiography. Radiographer. (2012) 59:35–9. doi: 10.1002/j.2051-3909.2012.tb00172.x
39. Behzadmehr, R, Doostkami, M, Sarchahi, Z, Saleh, LD, and Behzadmehr, R. Radiation protection among health care workers: knowledge, attitude, practice, and clinical recommendations: a systematic review. Rev Environ Health. (2021) 36:223–34. doi: 10.1515/reveh-2020-0063
Keywords: fluoroscopy, interventional radiology, gonad, occupational hazards, radiation exposure, healthcare attitudes
Citation: Alenezi MS, Alshammari AM and Hassib MB (2025) Knowledge, attitudes, and practices of radiology practitioners in Saudi Arabia toward the use of gonad shields during fluoroscopy-guided interventional radiography. Front. Med. 12:1655457. doi: 10.3389/fmed.2025.1655457
Edited by:
Hamid Osman, Taif University, Saudi ArabiaReviewed by:
Zuhal Hamd, Princess Nourah bint Abdulrahman University, Saudi ArabiaAwadia Gareeballah, Taibah University, Saudi Arabia
Mustafa Mahmoud, King Khalid University, Saudi Arabia
Copyright © 2025 Alenezi, Alshammari and Hassib. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mamdouh S. Alenezi, bXMuYWxlbmV6aUB1b2guZWR1LnNh
 Mamdouh S. Alenezi
Mamdouh S. Alenezi Abdulaziz M. Alshammari
Abdulaziz M. Alshammari Mazin B. Hassib
Mazin B. Hassib