- 1Department of Endocrinology and Metabolism, The Second Affiliated Hospital of Guilin Medical University, Guilin, Guangxi, China
- 2Guangxi Clinical Research Center for Diabetes and Metabolic Diseases, The Second Affiliated Hospital of Guilin Medical University, Guilin, Guangxi, China
- 3Guangxi Health Commission Key Laboratory of Glucose and Lipid Metabolism Disorders, The Second Affiliated Hospital of Guilin Medical University, Guilin, Guangxi, China
Background: Obesity is a major global public health crisis but remains inadequately addressed during clinical encounters. In China, the primary healthcare system plays a vital role in managing chronic; however, the knowledge, attitude, and practice (KAP) of primary care physicians (PCPs) regarding obesity have not been previously described.
Methods: This cross-sectional study surveyed 240 PCPs in Southwest China using self-administered KAP questionnaires. The questionnaires assessed obesity-related KAP and were measured using SPSS software. Descriptive statistics and univariate analyses were used to analyze the data.
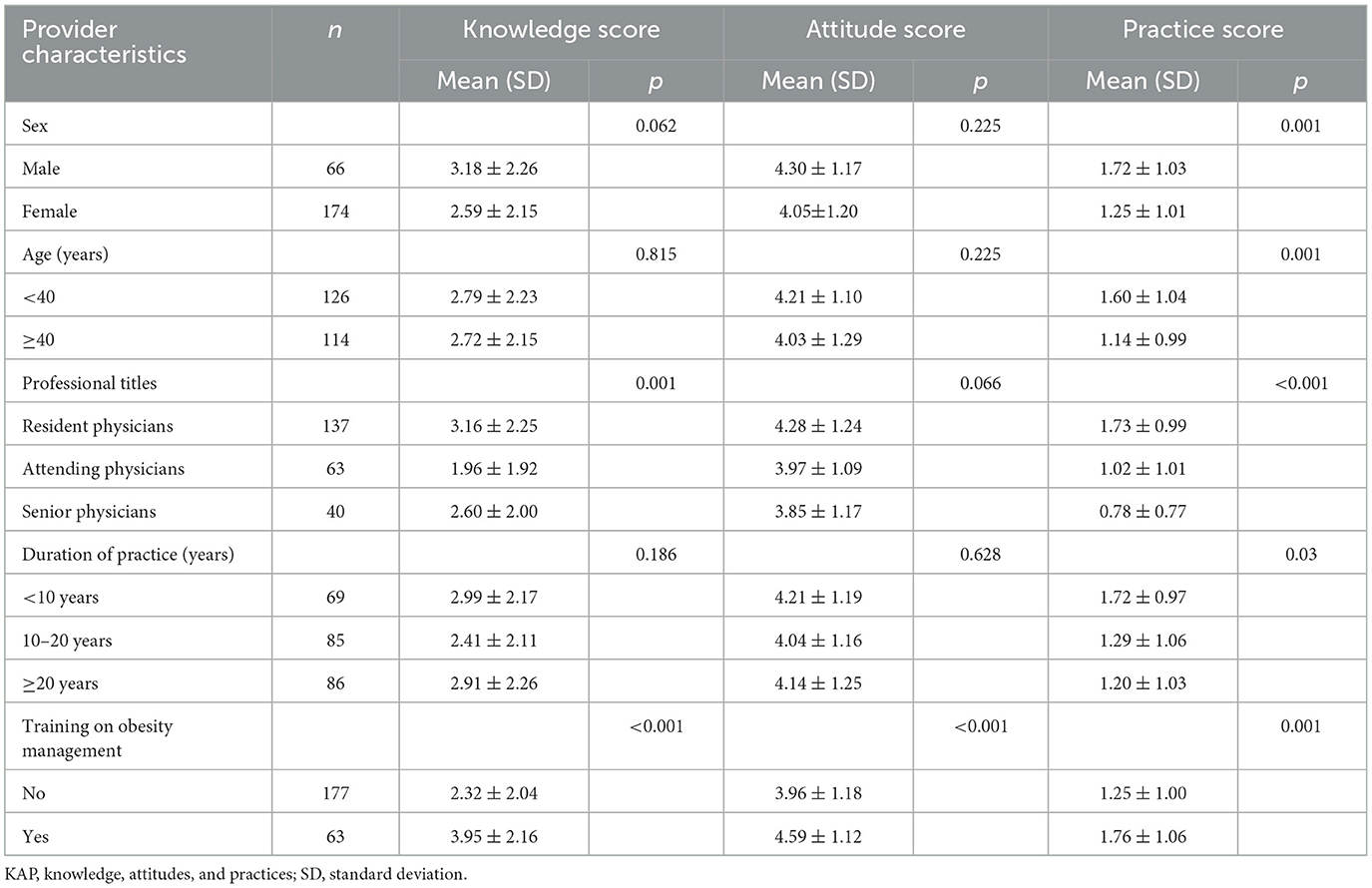
Results: In total, 240 PCPs completed the survey. While the majority (75.0%) reported awareness of the adverse health effects of obesity, their attitudes toward obesity management were generally negative. Notably, significant gaps were found in both knowledge and practice. Obesity knowledge of PCPs and practice subscale scores were 45.9% and 23.1% of the corresponding optimal scores, respectively. Exposure to formal obesity-related training was associated with significantly higher scores in knowledge (3.95 ± 2.04 vs. 2.32 ± 2.16, p < 0.001), attitudes (4.59 ± 1.12 vs. 3.96 ± 1.18, p < 0.001), and practices (1.76 ± 1.06 vs. 1.25 ± 1.00, p = 0.001).
Conclusion: Substantial gaps exist in the KAP of PCPs regarding obesity in Southwest China. Formal training appears to significantly improve obesity-related KAP and may enhance the primary care management of patients with obesity.
Background
Obesity is a chronic disease that poses serious health risks and constitutes a major public health crisis globally (1). Consistent with global trends, obesity has become increasingly prevalent in China due to rapid economic and social changes since the 1990s. According to data from the recent national survey indicated that the prevalence of obesity and overweight were 14.1% and 34.8%, respectively among adults living in China (2).
Obesity has substantial health, economic, and social consequences. It is associated with a high risk of numerous chronic conditions, including diabetes, hypertension, dyslipidemia, cardiovascular disease, non-alcoholic fatty liver disease, and various cancers (1, 3). A high body mass index is also associated with increased premature mortality (4), with more than five million deaths globally attributed to overweight and obesity annually (5). Obesity is prevalent among special group, such as seafarers (6, 7), childhood obesity (8), etc. Specific initiatives should be taken to curb the rising tide of obesity.
In response to the escalating obesity burden, the Chinese government has made numerous efforts to raise awareness, promote healthy lifestyles, and improve dietary habits (9, 10). Despite these efforts, the prevalence of obesity among Chinese adults has not been curbed. Recently, the government of China launched the “Weight Management Year” plan as a more targeted effort to curb rising obesity rates (11). Physicians are expected to play a central role in obesity management; however, obesity often remains inadequately addressed in clinical encounters, primarily due to inadequate physician knowledge and training (12–14).
Primary healthcare (PHC) systems are pivotal in addressing chronic diseases in China (15), with most patients, including those with obesity, receive healthcare services from PHC facilities (16). Nevertheless, many primary care physicians (PCPs) in China lack obesity-related training, and obesity is often overlooked in routine care. Studies conducted in the United States have indicated lack of confidence in managing obesity among PCPs (13). Related studies in China have shown that nurses (17), rural residents (18) and university students (19) generally possess limited knowledge about obesity and its metabolic complications. A recent study conducted to identify the perceptions, attitudes, and barriers to effective obesity care among healthcare professionals in China found that while most acknowledged obesity as a chronic disease, they often refrained from discussing it with patients for lacking of confidence in managing obesity (20).
To the best of our knowledge, no studies have yet evaluated the knowledge, attitudes, and practices (KAP) related to obesity among PCPs in China. Therefore, this study aimed to assess obesity-related KAP among PCPS in Southwest China and to examine associations between provider characteristics and these outcomes.
Methods
Sample and survey administration
This descriptive cross-sectional study used a convenience sampling approach and was conducted among PCPs affiliated with 14 township health centers in Guilin City, Guangxi Zhuang Autonomous Region, from February 12 to May 20, 2025. Board-certified PCPs actively providing primary care services were included. Those holding solely administrative roles or working in support departments, such as pharmacies and laboratory services, were excluded.
Using the OpenEpi web-based calculator, a minimum sample size of 195 PCPs was estimated, assuming a margin of error of 0.05 and 95% confidence interval, and a population size of 800. Considering 10% contingency, the minimum required sample size was 216. A simple random sampling method was used to select 500 PCPs from the 14 health centers.
Survey instrument
A structured questionnaire was developed to assess the KAP of participants regarding obesity, based on previous literature with minor modifications (21, 22). The questionnaire consisted of five sections. The first collected demographic characteristics, including sex, age, education level, professional title, years of clinical experience, and prior participation in obesity-related training programs. The second section assessed knowledge of obesity using six main questions, such as those addressing the pathophysiological mechanisms of obesity. The third section evaluated attitudes toward obesity, while the fourth section evaluated the clinical practices of PCPs related to obesity management.
Responses were recording using a 4-point Likert scale tailored to each domain (1 = high/moderate, strongly agree/agree, frequently/sometimes; 0 = low/very low, strongly disagree/disagree, rarely/never). Two experts in endocrinology evaluated the questionnaire items for difficulty and clarity and five lay participants reviewed the questionnaire to confirm that it accurately covered all aspects of the topic. Reliability was assessed using Cronbach's alpha, which demonstrated acceptable internal consistency, confirming that the questionnaire's scales consistently measured the intended constructs. A pre-test was conducted among 20 PCPs to refine the questionnaire for reliability, clarity, and interpretability. The instrument demonstrated good internal consistency, with an overall Cronbach's alpha value of 0.835 (0.825, 0.867, and 0.842 for knowledge, attitudes, and practices, respectively).
Ethical approval
This study was conducted in accordance with the Declaration of Helsinki and received ethical approval from The Second Affiliated Hospital of Guilin Medical University. An informed consent statement was included at the beginning of the online questionnaire, outlining the voluntary nature of participation and the confidentiality of responses. All participants provided informed consent.
Statistical analysis
Data were extracted and analyzed using SPSS version 25.0 (IBM Corporation, Armonk, NY). Descriptive data were expressed as numbers, percentages, means, and standard deviations, as appropriate. Associations between PCP characteristics and KAP scores were evaluated using chi-square tests and t-tests, as appropriate. Statistical significance was set at p < 0.05.
Results
General characteristics of the study sample
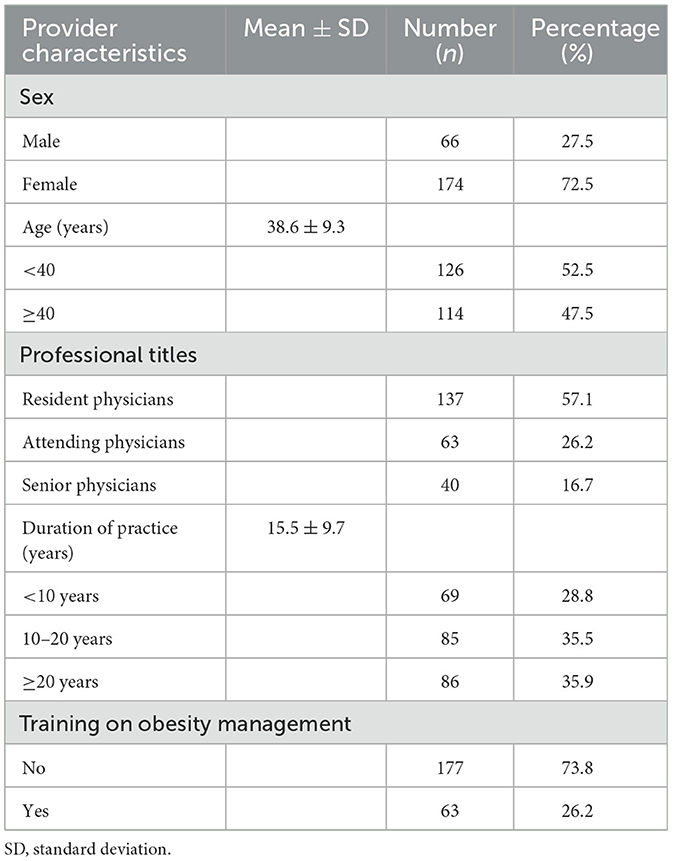
Of the 500 PCPs invited, 240 voluntarily participated and returned completed questionnaires, yielding a response rate of 48.0%. The characteristics of the study participants are summarized in Table 1. The mean age was 38.6 ± 9.3 years, with nearly half of the participants aged ≥40 years (n = 114, 47.5%). Most participants were females (n = 174, 65.5%). The PCPs included 137 residents, 63 attending physicians, and 40 senior physicians. Those with more than 20 years of clinical experience represented the largest subgroup (n = 86, 35.9%). Only 26.2% of respondents reported having received formal obesity-related training.
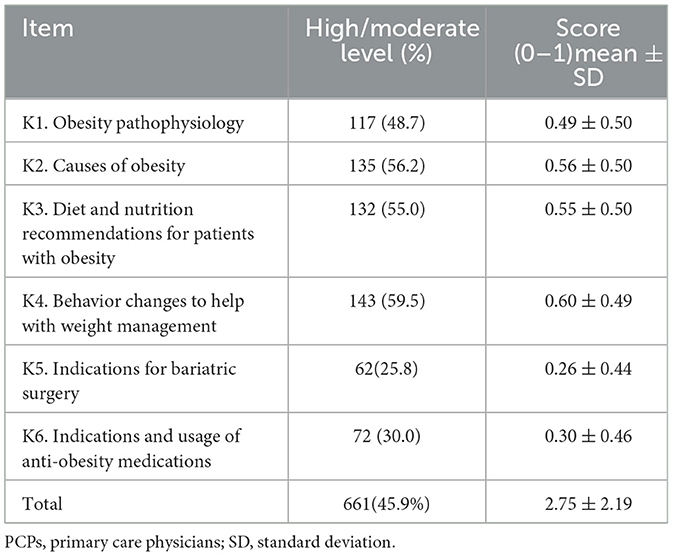
Self-reported knowledge of PCPs regarding obesity
As shown in Table 2, nearly half of the participants reported having a high or moderate level of knowledge regarding obesity pathophysiology (48.7%), causes of obesity (56.2%), dietary and nutritional recommendations for obese patients (55.0%), and behavioral strategies for weight management (59.5%). However, knowledge was lower concerning indications for bariatric surgery and anti-obesity medications, with only 25.8% and 30.0% reporting high or moderate knowledge levels, respectively.
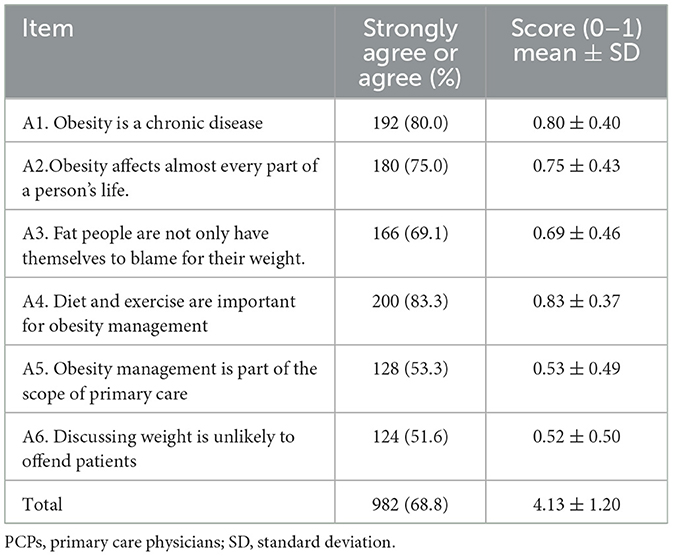
Attitudes of PCPs regarding obesity
As shown in Table 3, majority of PCPs recognized obesity as a chronic disease (n = 192, 80.0%) that affects almost every aspect of the life of the patient (n = 180, 75.0%). Meanwhile, 166 (69.1%) agreed that obesity involves multifactorial causes and that obese people should not be solely blamed for their weight. The majority of participants (n = 200, 83.3%) considered diet and exercise as the cornerstone of obesity management. However, only 128 (53.3%) viewed obesity management as part of their routine duties, and half of the PCPs felt that discussing weight issues was likely to offend patients.
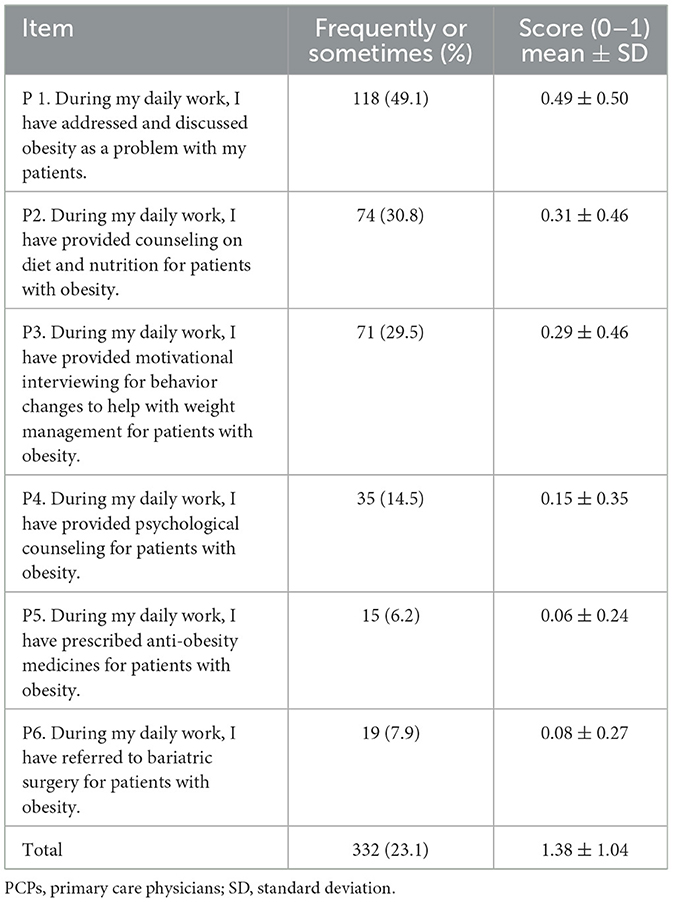
Practice of PCPs regarding obesity
As shown in Table 4, 118 (49.1%) PCPs reported addressing obesity during daily consultations. Comprehensive counseling on diet and nutrition was provided by 30.8% of PCPs, and 29.5% offered behavioral and medication advice. In addition to lifestyle changes, only 6.2% had prescribed anti-obesity medicines, and 7.9% had referred patients for bariatric surgery. Only 34 (14.5%) participants acknowledged the psychological impact of obesity and provided relevant counseling to patients.
Factors associated with the overall KAP scores
As shown in Table 5, significant associations were found between professional title and formal obesity training with knowledge scores. Resident physicians had the highest knowledge scores, whereas attending physicians had the lowest. Physicians with formal obesity training scored significantly higher than those without training. Formal obesity training was also a significant predictor of better attitudes toward obesity management. In terms of practice, male gender, age <40 years, lower professional title, shorter duration of practice, and formal training were all positively correlated with better obesity-related practices among PCPs.
Discussion
Obesity is a major global public health crisis (1). PCPs are the first point of contact for patients and are expected to have sufficient KAP regarding obesity management. Previous studies have shown that PCPs often find obesity management challenging and do not consistently address it during clinical encounters (14, 23, 24). This study aimed to evaluate the KAP of PCPs in China regarding obesity management. Our findings demonstrated that most physicians claimed to be aware of the harmful effects of obesity, but their attitudes usually deemed obesity management is out of the scope of primary care and discussing weight is unlikely to offend patients, possibly due to heavy workloads or a lack of competence. Notably, a substantial gap was noted in knowledge and practices. Formal training in obesity management emerged as a significant predictor of KAP.
Although obesity is recognized as a consequence of caloric surplus (25), emerging evidence highlights the role of complex, interconnected etiological drivers, such as genetic predispositions, gut dysbiosis, and obesogenic environments that disrupt metabolic homeostasis (26). Our study demonstrated that PCPs only had a moderate level of self-reported knowledge regarding the pathophysiology and cause of obesity: 48.7% and 56.2% of participants rated their understanding of obesity pathophysiology and causes, respectively, as high or moderate. Another study conducted in Sweden indicated that most physicians deemed obesity was a chronic disease (91%), obesity regulation sits in the hypothalamus (70%) and obesity was due to disorders of appetite regulation (69%), which was higher than this study, this may be attributed to difference in methodologies and variations in geographical and economic characteristics (27). Our study utilized a 4-point Likert scale, while the study conducted in Sweden used multiple-choice questions. Regarding obesity management, around half of the participants were familiar with lifestyle interventions, such as diet and behavioral modifications, aligning with prior research among healthcare professionals in China (20). However, PCPs demonstrated poor knowledge of pharmacotherapy and bariatric surgery for obesity, possibly due to the absence of national guidelines and limited training opportunities. Our findings are comparable with studies from the United States (21) and Poland (28) which also reported large gaps in obesity management. Exposure to formal obesity-related training was a significant predictor of better knowledge, consistent with previous reports (21).
Most PCPs viewed obesity as a chronic disease and acknowledged its serious impact. Furthermore, half of the PCPs agreed that obesity involves multifactorial causes and that individuals are not solely responsible for their weight. These attitudes are consistent with findings from studies in Lebanon (29) and Saudi Arabia (30). Most respondents also considered diet and exercise as fundamental components of obesity management (29–31). However, only half of the participants thought that obesity management was part of their daily work and many were concerned that discussing weight was likely to offend patients. A Swedish study showed a similar attitude, with many physicians believing that weight management was primarily the responsibility of the patient (27). In contrast, a study in Norway found that most physicians regarded obesity management as part of their daily work. These discrepancies can be attributed to variations in geographical and socioeconomic factors. As in previous research (21), our study confirmed that formal training positively influenced the attitudes of PCPs toward obesity management.
This study also revealed generally poor obesity-related practices among PCPs. Only half of the PCPs routinely discuss obesity with patients, and even fewer have provided comprehensive counseling on diet and nutrition, behavioral changes, and psychological counseling. Prescribing anti-obesity medication and referring patients for bariatric surgery were also uncommon. These deficiencies may be attributed to the following reasons: (1) the lack of time and resources during consultations and lack of obesity-related training, which has also been postulated by previous studies (13, 27); (2) possibly due to the absence of national guidelines and limited training opportunities. Interestingly, male PCPs performed better than female PCPSs. In contrast to our findings, a study conducted in the United States reported that female PCPs had superior practices toward obesity management than male (32), while another study found no sex-based differences (33). Our results also indicated that younger age, lower professional titles, and shorter duration of practice were positively associated with better practice. In the PHC system of China, these factors are often interrelated. The association between age and obesity-related practice is consistent with a study conducted in Sweden (27). Younger physicians may be more open to recent guidelines and more willing to engage in training, which could explain these associations. Exposure to formal obesity training also emerged as a strong predictor of improved practice (21).
This study has several limitations. First, it was conducted in Southwest China, and its findings may not be generalizable due to geographic and sociocultural differences. Second, the self-reported nature of the KAP survey may have introduced recall and social desirability biases, potentially leading respondents to overstate positive attitudes and practices toward obesity. Further studies addressing these limitations should be done to validate our findings.
Conclusion
This study highlights substantial gaps in the KAP of PCPs regarding obesity management in Southwest China. The results underscore the importance of formal training to enhance the capacity of PCPs to better manage and treat patients with obesity. Future efforts aimed at improving knowledge and attitudes regarding obesity treatment among PCPs could have important public health implications.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
JT: Project administration, Formal analysis, Data curation, Writing – review & editing, Methodology. HC: Project administration, Formal analysis, Writing – review & editing, Methodology, Data curation. LP: Formal analysis, Conceptualization, Investigation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2025.1668886/full#supplementary-material
References
1. Bray GA, Kim KK, Wilding JPH. Obesity: a chronic relapsing progressive disease process. A position statement of the World Obesity Federation. Obes Rev. (2017) 18:715–23. doi: 10.1111/obr.12551
2. Chen K, Shen Z, Gu W, Lyu Z, Qi X, Mu Y, et al. Prevalence of obesity and associated complications in China: a cross-sectional, real-world study in 15.8 million adults. Diabetes Obes Metab. (2023) 25:3390–9. doi: 10.1111/dom.15238
3. Garvey WT, Mechanick JI, Brett EM, Garber AJ, Hurley DL, Jastreboff AM, et al. American association of clinical endocrinologists and American college of endocrinology comprehensive clinical practice guidelines for medical care of patients with obesity. Endocr Pract. (2016) 22:1–203. doi: 10.4158/EP161365.GL
4. Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, Lee A, et al. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. (2017) 377:13–27. doi: 10.1056/NEJMoa1614362
5. GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. (2020) 396:1223–49. doi: 10.1016/S0140-6736(20)30752-2
6. Sagaro GG, Angeloni U, Marotta C, Nittari G, Rezza G, Silenzi A, et al. Risk prediction model of self-reported hypertension for telemedicine based on the sociodemographic, occupational and health-related characteristics of seafarers: a cross-sectional epidemiological study. J Pers Med. (2023) 13:070146. doi: 10.1136/bmjopen-2022-070146
7. Nittari G, Tomassoni D, Di Canio M, Traini E, Pirillo I, Minciacchi A, et al. Overweight among seafarers working on board merchant ships. BMC Public Health. (2019) 19:45. doi: 10.1186/s12889-018-6377-6
8. Nittari G, Scuri S, Petrelli F, Pirillo I, di Luca NM, Grappasonni I. Fighting obesity in children from European World Health Organization member states. Epidemiological data, medical-social aspects, and prevention programs. Clin Ter. (2019) 170:e223–30. doi: 10.7417/CT.2019.2137
9. Wang H, Zhai F. Programme and policy options for preventing obesity in China. Obes Rev. (2013) 14:134–40. doi: 10.1111/obr.12106
10. State Council of the People's Republic of China. National nutrition plan 2017–2030. Available online at: https://extranet.who.int/nutrition/gina/en/node/24710 (accessed May 26, 2025).
11. Central People's Government of the People's Republic of China. The Implementation Plan for the “Weight Management Year”. Available online at: https://www.gov.cn/zhengce/zhengceku/202406/content_6959543.htm (accessed May 26, 2025).
12. Petrin C, Kahan S, Turner M, Gallagher C, Dietz WH. Current attitudes and practices of obesity counselling by health care providers. Obes Res Clin Pract. (2017) 11:352–9. doi: 10.1016/j.orcp.2016.08.005
13. Salinas GD, Glauser TA, Williamson JC, Rao G, Abdolrasulnia M. Primary care physician attitudes and practice patterns in the management of obese adults: results from a national survey. Postgrad Med. (2011) 123:214–9. doi: 10.3810/pgm.2011.09.2477
14. Tsai AG, Remmert JE, Butryn ML, Wadden TA. Treatment of obesity in primary care. Med Clin North Am. (2018) 102:35–47. doi: 10.1016/j.mcna.2017.08.005
15. CPC Central Committee, State Council. The plan for “Healthy China 2030” (2016). Available online at: http://www.gov.cn/xinwen/2016-10/25/content_5124174.htm (Accessed May 18, 2025).
16. Li X, Lu J, Hu S, Cheng KK, De Maeseneer J, Meng Q, et al. The primary health-care system in China. Lancet. (2017) 390:2584–94. doi: 10.1016/S0140-6736(17)33109-4
17. Fan M, Hong J, Cheung PN, Tang S, Zhang J, Hu S, et al. Knowledge and attitudes towards obesity and bariatric surgery in Chinese nurses. Obes Surg. (2020) 30:618–29. doi: 10.1007/s11695-019-04173-z
18. Zhang W, Chen X, Wang C, Gao L, Chen W, Yang W. Perceptions and attitudes toward obesity and its management in migrants and rural residents in China: a cross-sectional pilot study. Obes Surg. (2022) 32:152–9. doi: 10.1007/s11695-021-05755-6
19. Diao X, Gao L, Yang Y, Chen X, Gong J, Qian Y, et al. Knowledge and attitudes towards obesity and bariatric surgery in university students: a national survey. Obes Surg. (2022) 32:2869–79. doi: 10.1007/s11695-022-06157-y
20. Ji L, Mu Y, Chang C, Wang H, Zhao D, Liu D, et al. Perceptions, attitudes and barriers to effective obesity care among people living with obesity and healthcare professionals in China: the ACTION-China study. Diabetes Obes Metab. (2024) 26:4694–704. doi: 10.1111/dom.15837
21. Anees A, Saeed ZI, Kemper S, Haggerty T, Davisson L. Surveying the knowledge and practices of primary care residents in managing adult patients with obesity. J Gen Intern Med. (2024) 39:1698–703. doi: 10.1007/s11606-024-08777-9
22. Rurik I, Torzsa P, Ilyés I, Szigethy E, Halmy E, Iski G, et al. Primary care obesity management in Hungary: evaluation of the knowledge, practice and attitudes of family physicians. BMC Fam Pract. (2013) 14:156. doi: 10.1186/1471-2296-14-156
23. Ma J, Xiao L, Stafford RS. Adult obesity and office-based quality of care in the United States. Obesity. (2009) 17:1077–85. doi: 10.1038/oby.2008.653
24. Kaplan LM, Golden A, Jinnett K, Kolotkin RL, Kyle TK, Look M, et al. Perceptions of barriers to effective obesity care: results from the national ACTION study. Obesity. (2018) 26:61–9. doi: 10.1002/oby.22054
25. Ilyas Z, Perna S, Al-Thawadi S, Alalwan TA, Riva A, Petrangolini G, et al. The effect of Berberine on weight loss in order to prevent obesity: a systematic review. Biomed Pharmacother. (2020) 127:110137. doi: 10.1016/j.biopha.2020.110137
26. Meldrum DR, Morris MA, Gambone JC. Obesity pandemic: causes, consequences, and solutions-but do we have the will? Fertil Steril. (2017) 107:833–9. doi: 10.1016/j.fertnstert.2017.02.104
27. Carrasco D, Thulesius H, Jakobsson U, Memarian E. Primary care physicians' knowledge and attitudes about obesity, adherence to treatment guidelines and association with confidence to treat obesity: a Swedish survey study. BMC Prim Care. (2022) 23:208. doi: 10.1186/s12875-022-01811-x
28. Mojkowska A, Sobczak K, Leoniuk K, Henzler M, Jackowski M. Medical or common knowledge? Knowledge of medical professionals on obesity diagnosis criteria and treatment. Obes Facts. (2023) 16:216–23. doi: 10.1159/000529266
29. Antoun J, Kfoury C, Chamaa Y, Saade Y, El Tannir S. Acceptance, knowledge, and attitude of family physicians towards obesity as a chronic disease: a multinational cross-sectional study. Int J Obes. (2025) 49:682–7. doi: 10.1038/s41366-024-01693-2
30. Alatawi AM, Alanazi MA, Almohammadi MA. Family physicians' knowledge, beliefs, and practices in promoting healthy lifestyles and weight management for obese patients in Tabuk, Saudi Arabia. Front Endocrinol. (2024) 15:1456086. doi: 10.3389/fendo.2024.1456086
31. Agarwal M, Nadolsky K. Attitudes, perceptions, and practices among endocrinologists managing obesity. Endocr Pract. (2022) 28:179–84. doi: 10.1016/j.eprac.2021.10.006
32. Foster GD, Wadden TA, Makris AP, Davidson D, Sanderson RS, Allison DB, et al. Primary care physicians' attitudes about obesity and its treatment. Obes Res. (2003) 11:1168–77. doi: 10.1038/oby.2003.161
Keywords: obesity, knowledge, attitude, practice, primary care providers, Southwest China, cross-sectional study
Citation: Tang J, Chen H and Pi L (2025) Obesity-related knowledge, attitude, and practices among primary care physicians in China: a cross-sectional study. Front. Med. 12:1668886. doi: 10.3389/fmed.2025.1668886
Received: 18 July 2025; Accepted: 05 September 2025;
Published: 25 September 2025.
Edited by:
Cain Craig Truman Clark, Birmingham City University, United KingdomCopyright © 2025 Tang, Chen and Pi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Linhua Pi, MTgxMjY5NzAxOTlAMTYzLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Jusumei Tang1†
Jusumei Tang1† Linhua Pi
Linhua Pi