- 1Department of Oncology, The First Affiliated Hospital of Anhui Medical University, Hefei, China
- 2Anhui Medical University, Hefei, China
- 3Department of Otolaryngology, Head and Neck Surgery, The First Affiliated Hospital of Anhui Medical University, Hefei, China
- 4Department of Gastroenterology, The Third Affiliated Hospital of Anhui Medical University (Hefei first people’s Hospital), Hefei, China
Background: This network meta-analysis aimed to comprehensively compare the operative and postoperative outcomes of different parotidectomy incisions.
Methods: Embase, PubMed, Web of Science, and Cochrane Central Register of Controlled Trials were searched up to April 2022. A complete Bayesian network meta-analysis was performed using the Markov Monte Carlo method in OpenBUGS.
Results: Seventeen studies with 1609 patients were included. Thirteen were retrospective cohort studies, three were prospective cohort studies, and one was a randomized controlled study. The quality of evidence was rated as very low in most comparisons. The incision satisfaction score of the modified facelift incision (MFI), retroauricular hairline incision (RAHI), V-shaped incision (VI) were higher than that of the modified Blair incision (MBI) (MBI vs. MFI: mean difference [MD] -1.39; 95% credible interval [CrI] -2.23, -0.57) (MBI vs. RAHI: MD -2.25; 95% CrI -3.40, -1.12) (MBI vs. VI: MD -2.58; 95% CrI -3.71, -1.46); the tumor size treated by VI was smaller than that by MBI (MD 5.15; 95% CrI 0.76, 9.38) and MFI (MD 5.16; 95% CrI 0.34, 9.86); and the risk of transient facial palsy in the MFI was lower than that in the MBI (OR 2.13; 95% CrI 1.28, 3.64). There were no differences in operation time, drainage volume, wound infection, hematoma, salivary complications, Frey syndrome, or permanent facial palsy between incision types.
Conclusion: The traditional MBI is frequently used for large tumor volumes, but the incision satisfaction score is low and postoperative complication control is poor. However, emerging incisions performed well in terms of incision satisfaction scores and control of complications. More randomized controlled trials are needed to compare the different parotidectomy incisions. Patients should be fully informed about the characteristics of each incision to make the most informed decision, along with the physician’s advice.
Systematic Review Registration: PROSPERO, identifier CRD42022331756
1 Introduction
The parotid glands, being the largest pair of salivary glands in the human body, are the location of approximately 80% of salivary gland cancer (1). According to the International Agency for Research on Cancer, there were 53,583 new cases of salivary gland cancer globally in 2020, accounting for 0.3% of all cancers (2). Most parotid tumors are benign, and parotidectomy is the preferred treatment option because of recurrence and potential malignant transformation (3, 4). Since the classic cervicomastoidfacial incision was proposed by Blair in 1912, the operative approach for parotid gland resection has undergone continuous improvement and innovation (5). Endoscopy- and robot-assisted parotidectomy techniques have also progressed in recent years, but their safety and ease of use need to be further proven in practice.
Currently, four incision types are commonly used for parotidectomy. The modified Blair incision (MBI) is the most widely used surgical incision in the clinic, while the modified facelift incision (MFI), retroauricular hairline incision (RAHI), and V-shaped incision (VI) are becoming increasingly prevalent. A large-scale surgical incision allows for full exposure of the parotid gland tissue to minimize facial nerve injury, but the ensuing huge facial scar inevitably inflicts a psychological load on the patient (6, 7). In contrast, smaller incisions with better cosmetic results require persuasive data representation to control complications.
There has been ongoing discussion regarding the different incision types for parotidectomy. Unfortunately, the number of relevant meta-analyses is limited (8). This study compared four incision options for parotidectomy based on a Bayesian network meta-analysis with the aim of providing evidence for surgical and patient incision selection.
2 Methods
2.1 Search strategy
This study was registered a priori with PROSPERO (CRD42022331756). We conducted a systematic literature search of Embase, PubMed, Web of Science, and Cochrane Central Register of Controlled Trials in April 2022 and were not restricted with regard to publication language and date. The complete search strategy is presented in Supplementary Material. We also reviewed the references of the included articles to identify additional potential studies. Because all analyses were based on previously published studies, ethical approval and patient consent were not required.
2.2 Study selection
Following the Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines, studies were included based on the population, intervention, comparison, outcome, and study design (PICOS). The PICOS components of this study were as follows: P (patients who underwent parotidectomy with speculated benign parotid tumors on preoperative examination), I (use of MBI [Figure 1A], MFI [Figure 1B], RAHI [Figure 1C], or VI [Figure 1D] in parotidectomy), C (pairwise comparisons between the four incisions), O (intraoperative and postoperative parameters, including operation time, incision satisfaction score, drainage volume, permanent facial palsy, bleeding volume, transient facial palsy, Frey syndrome, salivary complications, wound infection, and hematoma), and S (randomized clinical trials [RCTs] or original research articles with prospective or retrospective designs).
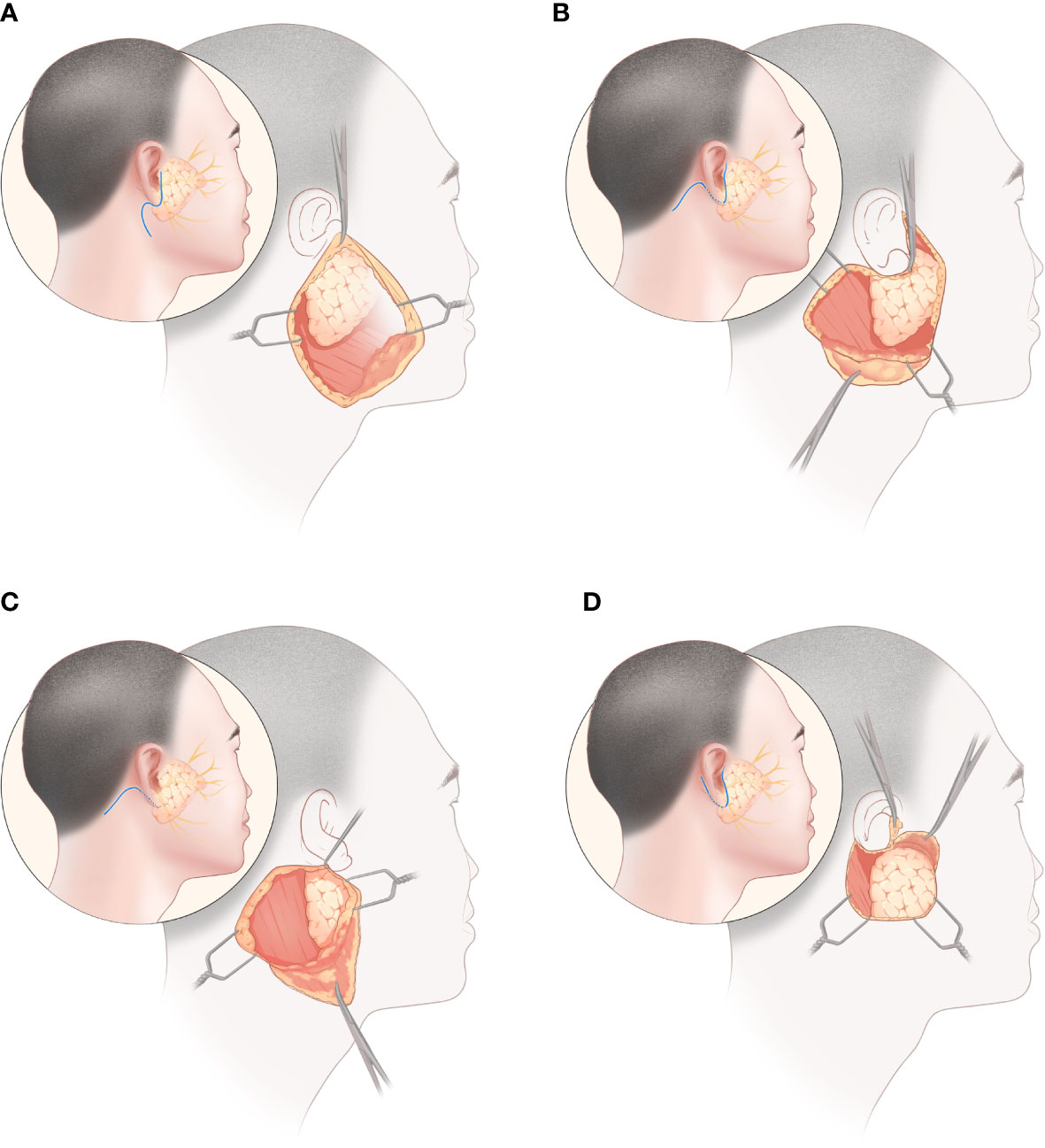
Figure 1 Parotidectomy via four incisions: (A) modified Blair incision, (B) modified facelift incision, (C) retroauricular hairline incision, (D) V-shaped incision.
The inclusion criteria were as follows: 1) RCTs or original research articles with prospective or retrospective designs, 2) articles that included patients who underwent parotidectomy and who had speculated benign parotid tumors by preoperative examination, and 3) studies that reported the outcome of parotidectomy and included at least one required outcome measure. The exclusion criteria were as follows: 1) studies using endoscopes or robots to assist with surgery, 2) studies with no control group, 3) studies related to flap or fascia reconstruction, 4) articles not published in English, and 5) review articles, short reports, and letters to the editor.
2.3 Data extraction and quality assessment
Data were independently extracted by two investigators. All divergences that arose throughout the procedure were reviewed by a third investigator, and a decision was made. The extracted data included the name of the first author, year of publication, country, study type, age, sex, duration of follow-up, surgical approach, tumor size, operation time, and postoperative outcomes. The primary outcomes were incision satisfaction score, operation time, drainage volume, and permanent facial palsy. Secondary outcomes were tumor size, transient facial palsy, Frey syndrome, salivary complications, wound infection, and hematoma. If relevant data were missing, an approximate formula was used for the calculation. The quality of the included RCTs was evaluated using the Cochrane Collaboration Tool, while the Newcastle-Ottawa scale (NOS) and the risk of bias in non-randomized studies of interventions (ROBINS-I) were used to assess the quality of the cohort studies. The evaluation criteria for the RCT tool included the randomization procedure, allocation concealment, baseline comparability of the research groups, blinding, and completeness of follow-up (9). NOS evaluates and scores study bias out of 9 points, including 4 for patient selection, 2 for research group comparability, and 3 for outcome evaluation. The ROBINS-I assesses bias due to confusion, subject selection, intervention classification, deviations from expected interventions, missing data, outcome measures, and reported outcome selection.
2.4 Statistical analysis
This network meta-analysis was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines (10). For continuous variables, the mean difference (MD) was calculated. As the variables in the categorical data were all adverse event outcomes and the positive rate was low, the odds ratio (OR) was used to calculate the effect size. For zero positive event outcomes, 0 was replaced by 0.5 to prevent a large confidence interval (11). A pairwise comparison meta-analysis was performed to obtain direct comparison results. To visualize all head-to-head comparisons for each outcome, we created network plots. Our study was based entirely on the random effects of the Bayesian approach and was analyzed using the Monte Carlo Markov chain (MCMC) method in OpenBUGS Version 3.2.3. The auxiliary statistical analysis and mapping were performed using software R 4.1.3 (main packages including gemtc and rjags) and Stata V.14. The fit of the model was verified using totresdev, and convergence was ensured using trace plots, Autocorr, Brooks-Gelman-Rubin diagnostic diagrams, and Potential Scale Reduction Factor (PSRF). The deviance information criterion (DIC) of the consistent and inconsistent models was compared to select a better model (12). If the inconsistent model had a better fit (low DIC value), the results were interpreted with caution (13). League tables were used to show the pooled comparisons for each outcome. We tested the overall heterogeneity of the outcomes and compared local inconsistencies using the node-splitting method. The evaluation criteria for statistical heterogeneity were as follows: I2 index values below 25% were considered as low heterogeneity, 50% as moderate heterogeneity, and 75% as high heterogeneity. Statistical significant was set at P<0.05. The surface under the cumulative ranking (SUCRA) was used to rank the inspected interventions (14). Furthermore, we evaluated publication bias using a funnel plot for outcomes in more than 10 studies. Finally, we used the network meta-analysis recommendations for grading and developed GRADE to assess the certainty of evidence (15).
3 Results
3.1 Search results and methodological quality
The selected databases were searched for 334 potentially related articles. Following the removal of duplicate studies, the titles and abstracts of 166 selected studies were examined and 121 unqualified papers were eliminated. After reading the full text, 1609 patients were included across 17 qualified articles, including one RCT, 13 retrospective cohort studies, and three prospective cohort studies. Figure 2 shows literature selection procedure in this study.
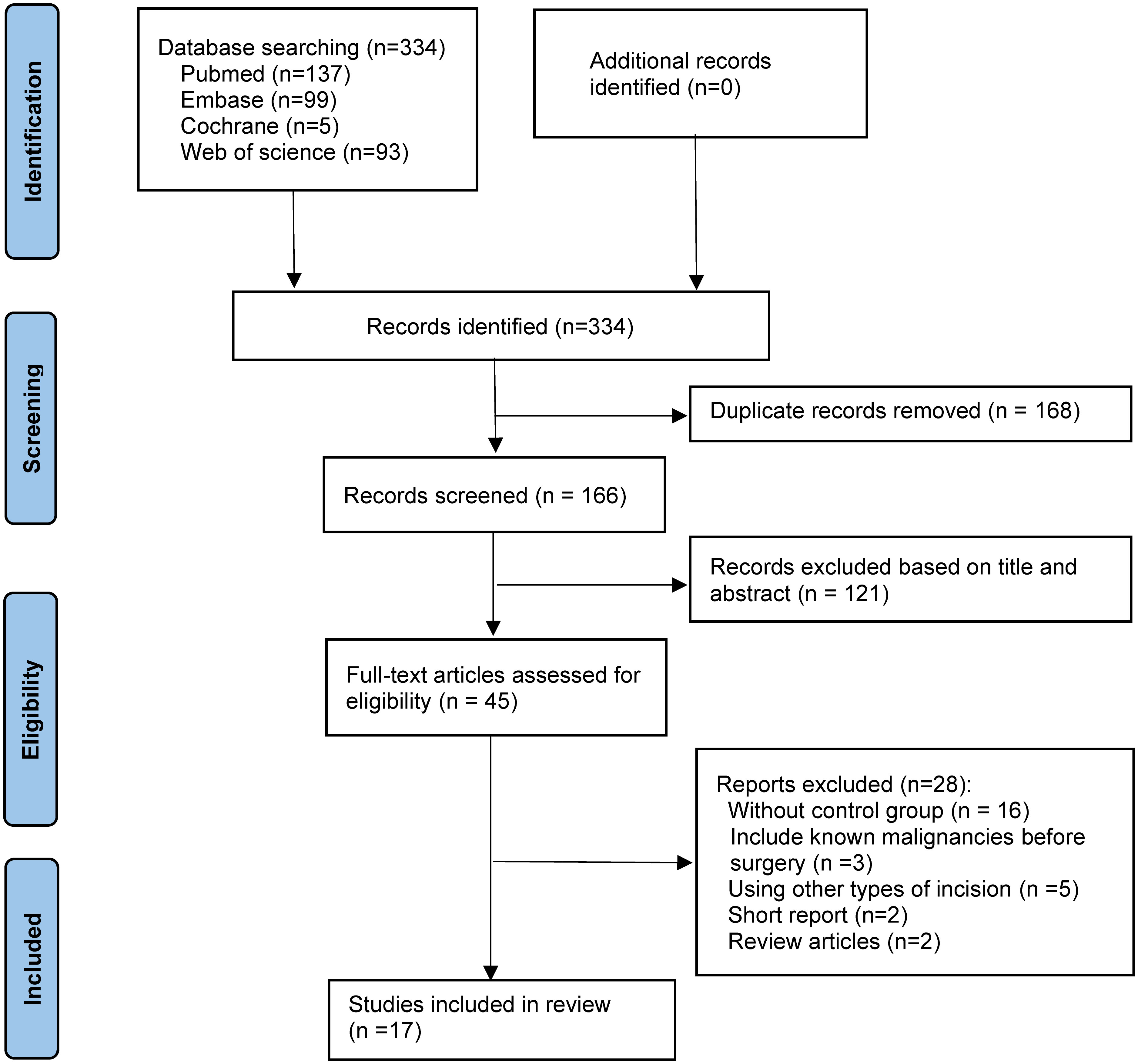
Figure 2 The Preferred Reporting Items for Systematic Reviews and network meta-analyses checklist (PRISMA-NMA) diagram.
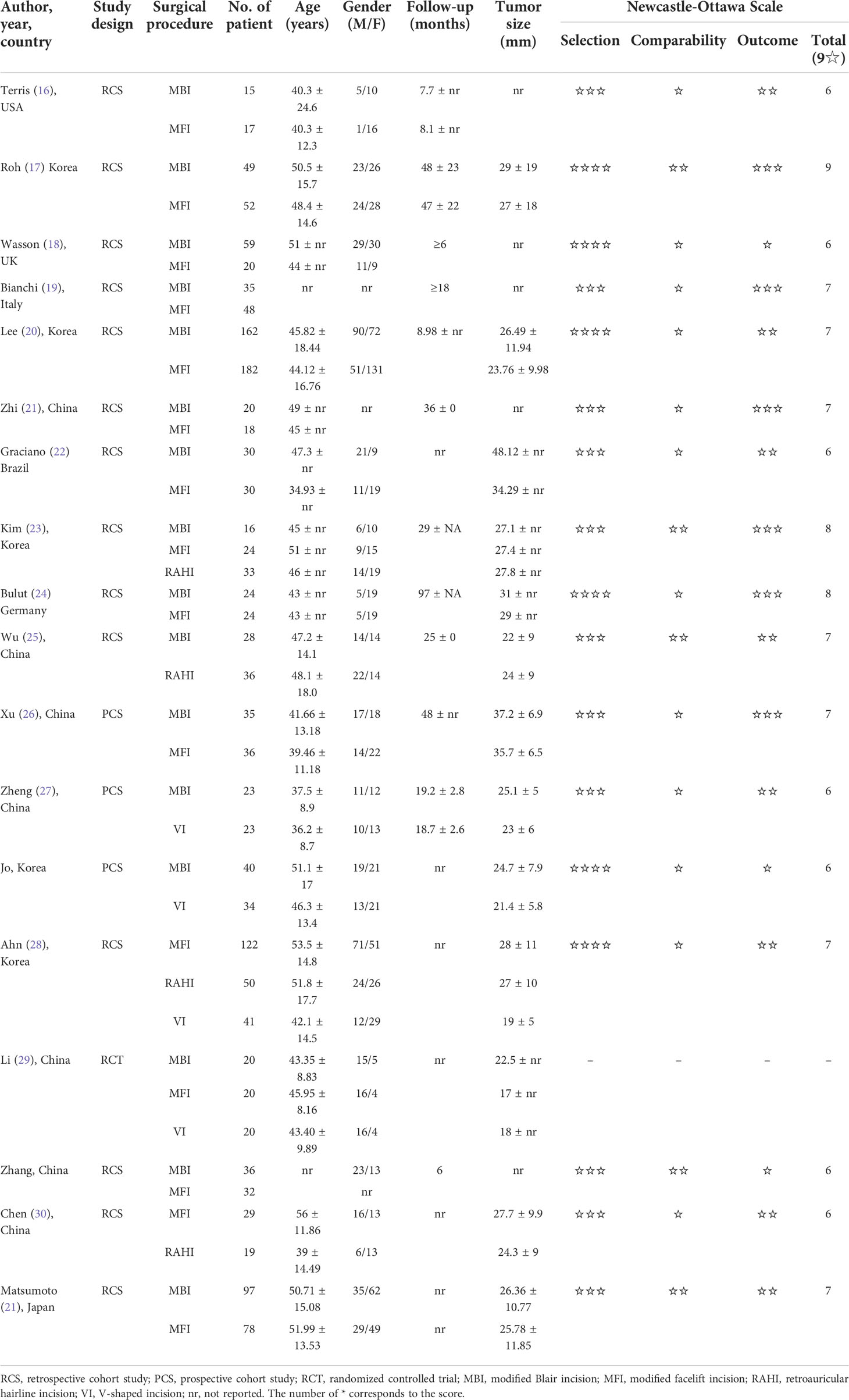
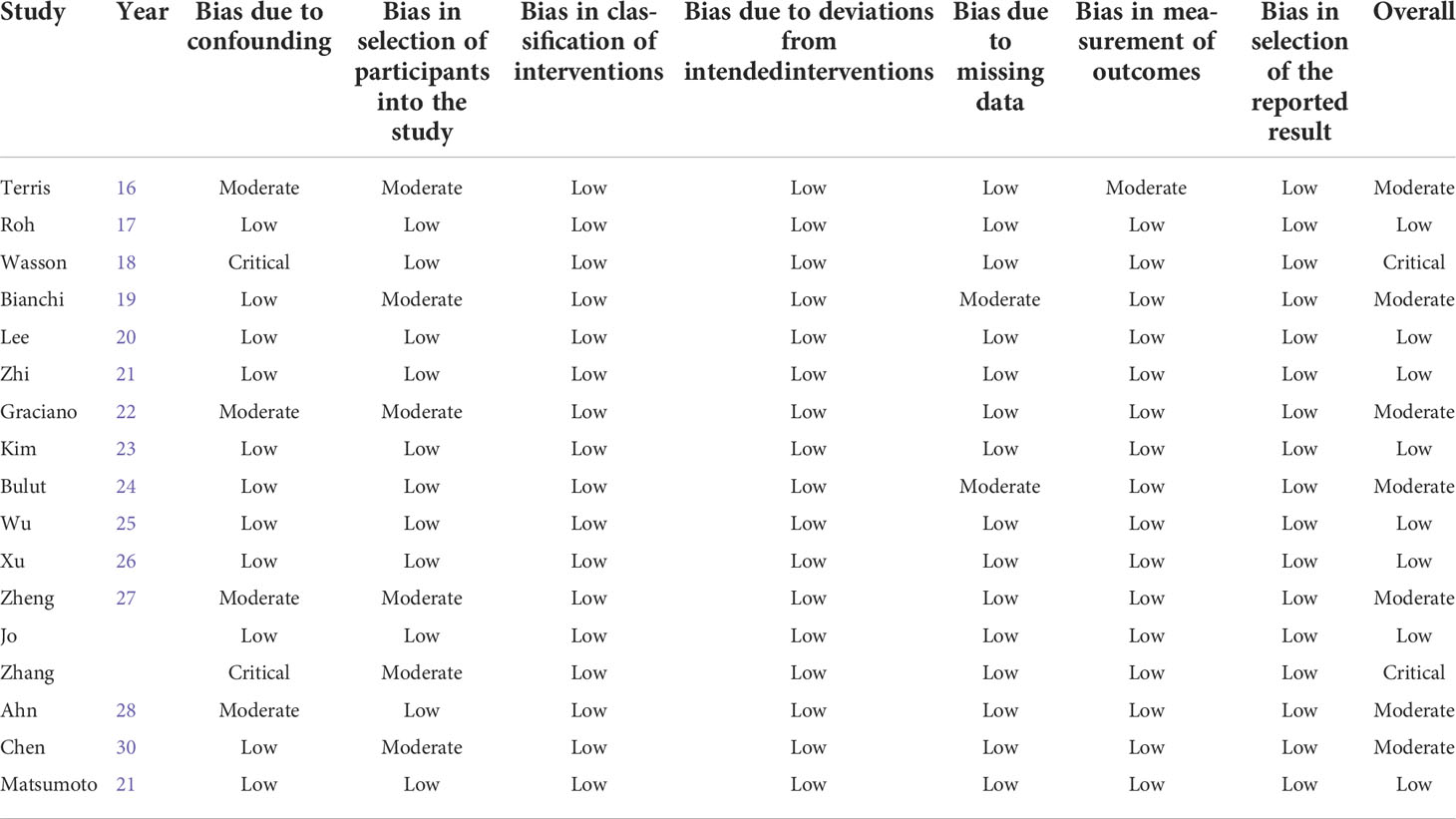
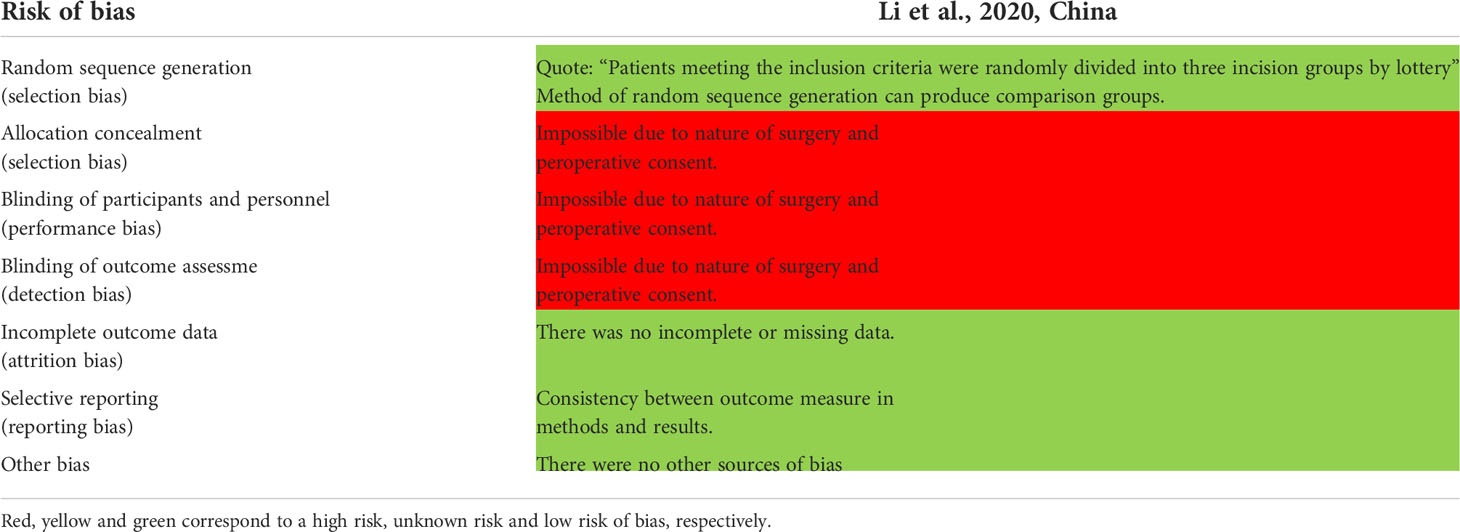
The baseline characteristics of the 17 types of research included in the network meta-analysis are presented in Table 1 (16–32). In our analysis, 14 of the studies were two-arm trials and three were three-arm trials involving four different surgical procedures. Nine cohort studies were considered to be of high quality, with NOS scores of 7 or greater. Specific scores are presented in Table 1. Table 2 shows the findings of the bias risk assessment for cohort studies using the ROBINS-I, with eight studies having a low overall bias. The results of RCT evaluated by the Cochrane Collaboration Tool are shown in Table 3.
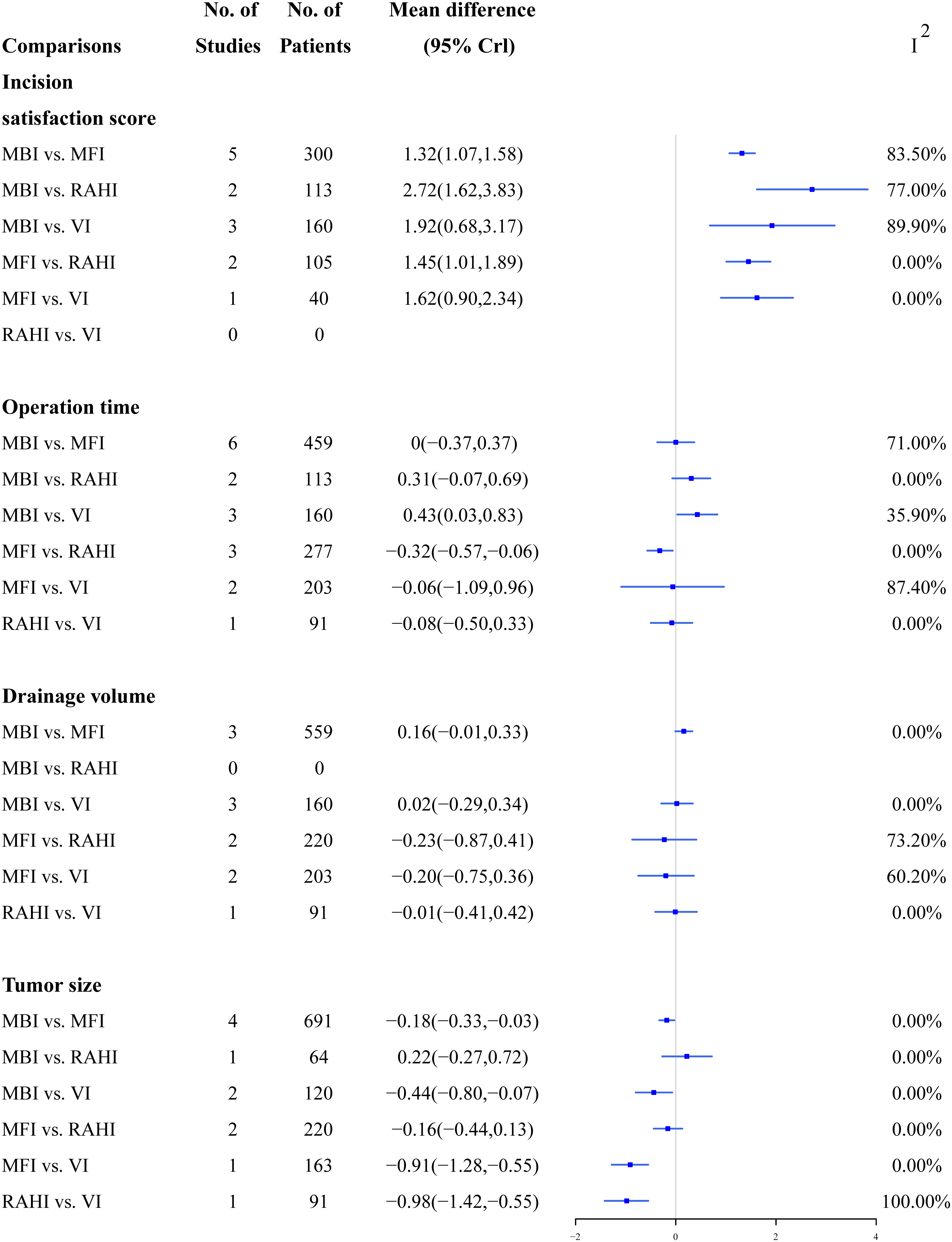
3.2 Traditional meta-analyses
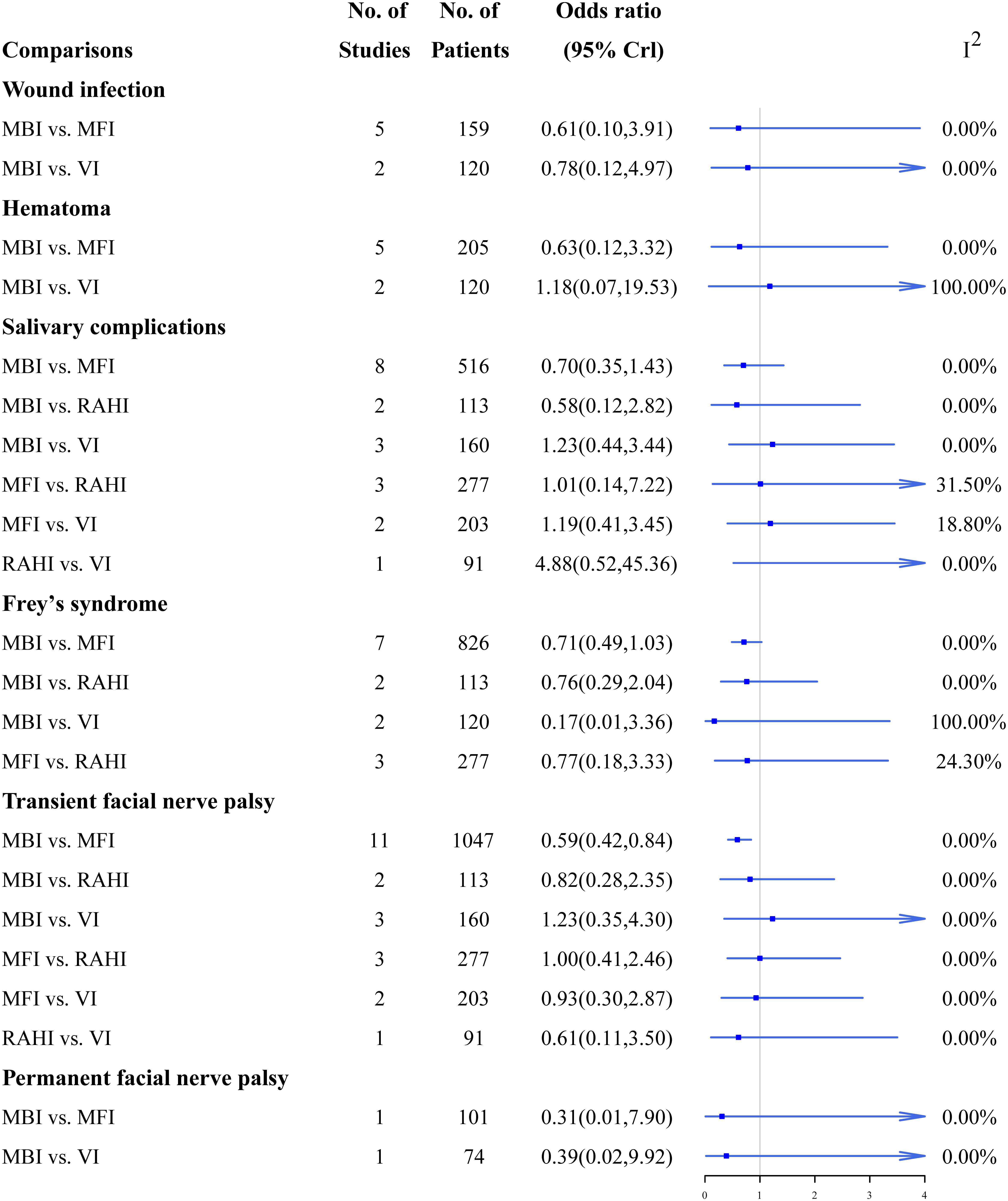
Figures 3, 4 summarize the direct comparison results of the pairwise meta-analyses of continuous and dichotomous outcomes from the 17 studies, respectively. The MFI, RAHI and VI had significantly higher incision satisfaction scores than the MBI; the RAHI and VI had significantly higher incision satisfaction scores than the MFI; however, no study has directly compared the RAHI and VI. VI required substantially longer time to operate than MBI, whereas MFI lasted significantly longer than RAHI. MBI had a significantly larger tumor size than MFI, whereas VI was significantly smaller than the other three incisions. The incidence of transient facial palsy was significantly higher only in the MBI group when compared with the MFI group, and there was no statistical significance in a pairwise direct comparison of other complications. Overall, the heterogeneity was low, although several groups had high values, reflecting differences in surgical skills among physicians or the small number of studies included in these pairwise comparisons.
3.3 Bayesian network meta-analyses
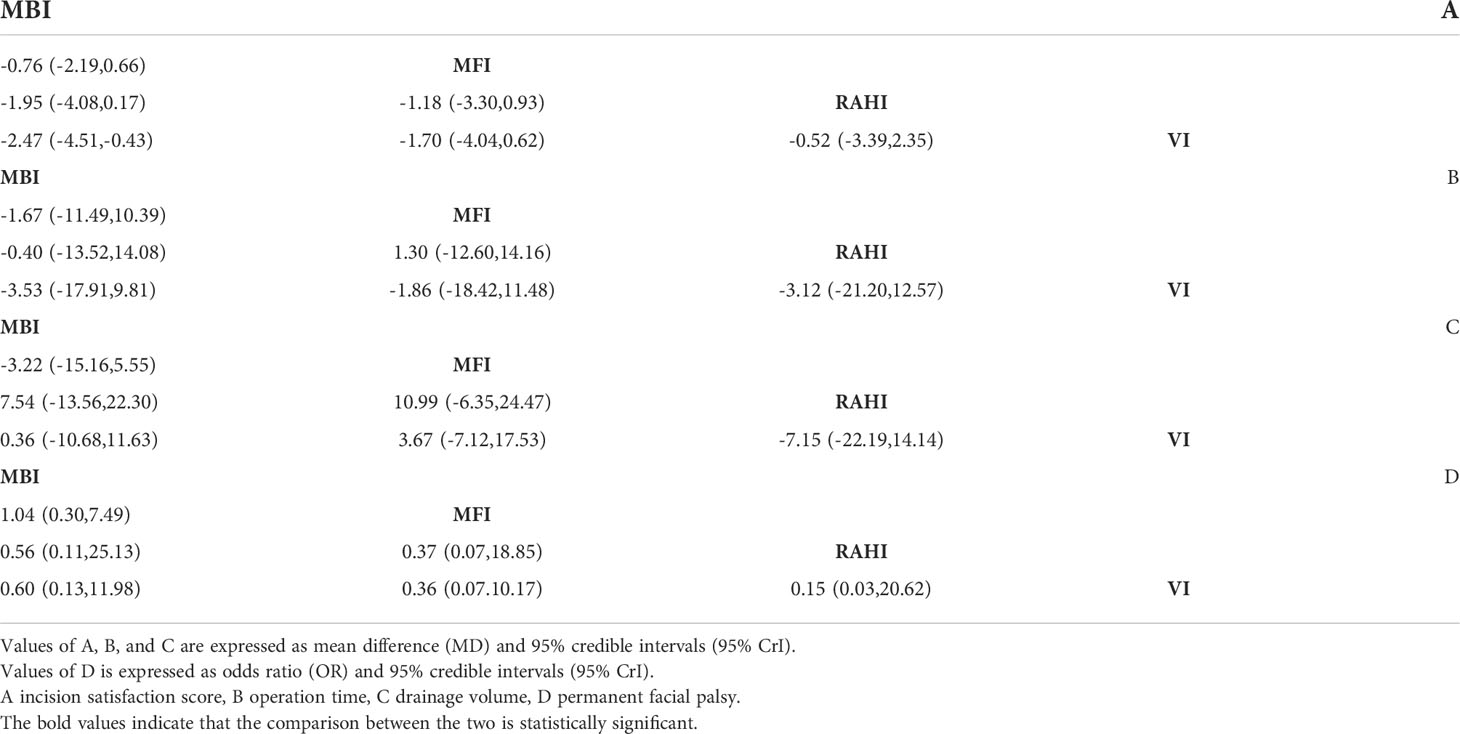
Figure 5 shows the network relationships between the different incisions. The area of each circle denotes the number of patients included, and the thickness of the lines linking the two surgical incisions represents the number of articles. Table 4 displays the pooled comparison findings, with the statistically significant values highlighted in bold.
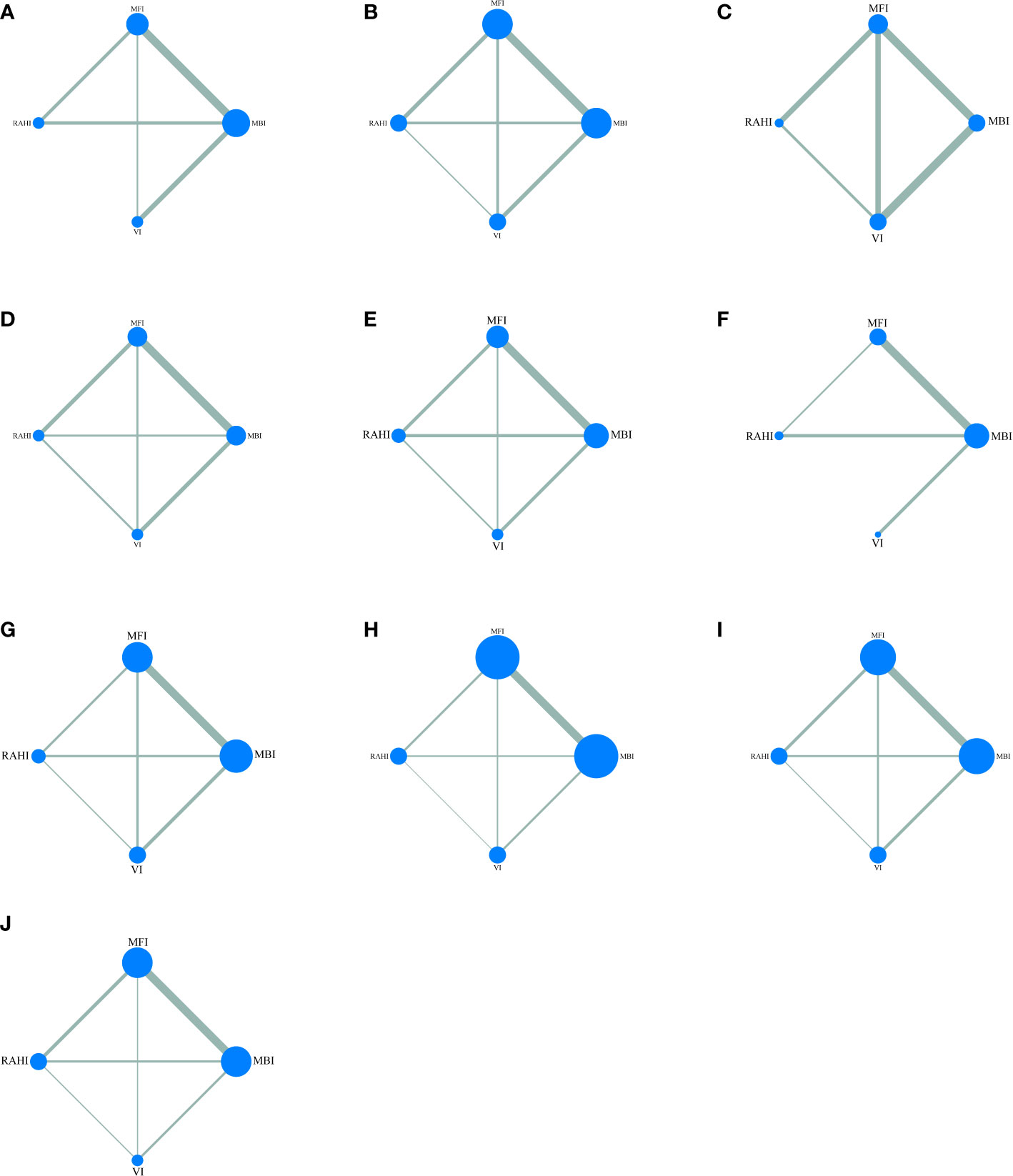
Figure 5 Network maps of all outcomes: (A) incision satisfaction score, (B) operation time, (C) drainage volume, (D) tumor size, (E) hematoma, (F) wound infection, (G) permanent facial palsy, (H) transient facial palsy, (I) salivary complications, (J) Frey syndrome.
3.3.1 Incision satisfaction score
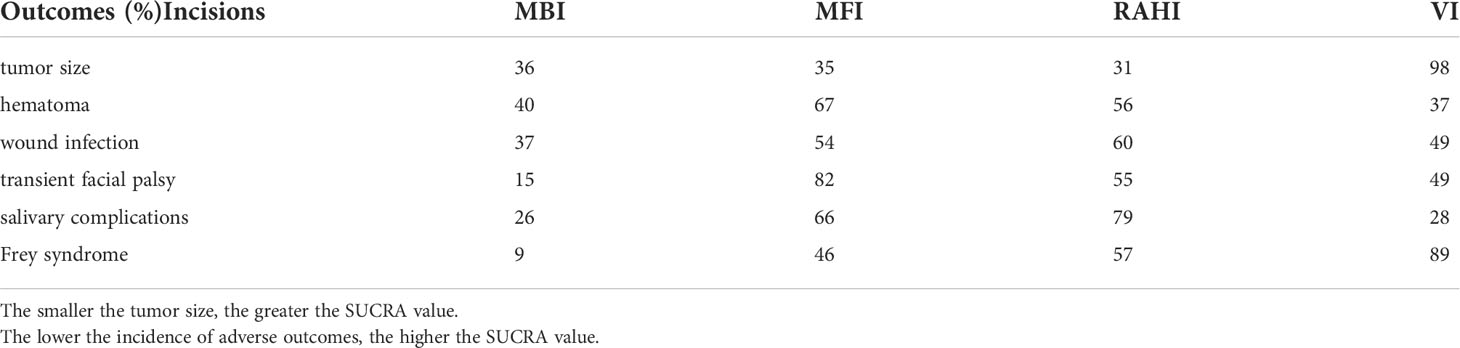
Nine studies including 585 patients provided data on incision satisfaction scores. Meta-analysis of pooled network showed similar MDs when comparing MFI vs. RAHI (MD -0.85; 95% credible interval [CrI] -2.00, 0.28), MFI vs. VI (MD -1.18; 95% CrI -2.49, 0.11), RAHI vs. VI (MD -0.33; 95% CrI -1.88, 1.23), while MBI vs. MFI (MD -1.39; 95% CrI -2.23, -0.57), MBI vs. RAHI (MD -2.25; 95% CrI -3.40, -1.12), and MBI vs. VI (MD -2.58; 95% CrI -3.71, -1.46) were signifificant (Table 4A). No statistical difference was observed between direct and indirect comparisons (MFI vs. MBI, p=0.08; RAHI vs. MBI, p=0.36; RAHI vs. MFI, p=0.21; VI vs. MFI, p=0.14). The overall heterogeneity was low (I2 = 6%). The SUCRA rankings were 0.1% for MBI, 36% for MFI, 75% for RAHI, and 88% for VI.
3.3.2 Operation time
Eleven studies involving 957 patients reported the operation time. Meta-analysis of the pooled network showed similar MDs when comparing MBI vs. MFI (MD -1.67; 95% CrI -11.49, 10.39), MBI vs. RAHI (MD -0.40; 95% CrI -13.52, 14.08), MBI vs. VI (MD -3.53; 95% CrI -17.91, 9.81), MFI vs. RAHI (MD 1.30; 95% CrI -12.60, 14.16), MFI vs. VI (MD -1.86; 95% CrI -18.42, 11.48), RAHI vs. VI (MD -3.12; 95% CrI -21.20, 12.57) (Table 4B). No statistical difference was observed between the direct and indirect comparisons (MFI vs. MBI, p=0.09; RAHI vs. MBI, p=0.52; VI vs. MBI, p=0.09; RAHI vs. MFI, p=0.29; VI vs. MFI, p=0.35; VI vs. RAHI, p=0.40). The overall heterogeneity was low (I2 = 13%). The SUCRA rankings were 63% for MBI, 46% for MFI, 58% for RAHI, and 33% for VI.
3.3.3 Drainage volume
Seven studies with a total of 960 patients reported the drainage volume. Meta-analysis of the pooled network showed similar MDs when comparing MBI vs. MFI (MD -3.22; 95% CrI -15.16, 5.55), MBI vs. RAHI (MD 7.54; 95% CrI -13.56, 22.30), MBI vs. VI (MD 0.36; 95% CrI -10.68, 11.63), MFI vs. RAHI (MD 10.99; 95% CrI -6.35, 24.47), MFI vs. VI (MD 3.67; 95% CrI -7.12, 17.53), RAHI vs. VI (MD -7.15; 95% CrI -22.19, 14.14) (Table 4C). No statistical difference was observed between the direct and indirect comparisons (MFI vs. MBI, p=0.41; V vs. MBI, p=0.35; VI vs. MFI, p=0.92; VI vs. RAHI, p=0.70). The overall heterogeneity was low (I2 = 14%). The SUCRA rankings were 50% for MBI, 15% for MFI, 84% for RAHI, and 51% for VI.
3.3.4 Permanent facial palsy
Eleven studies of 969 patients reported permanent facial palsy. Meta-analysis of the pooled network showed similar ORs when comparing MBI vs. MFI (OR 1.04; 95% CrI 0.30, 7.49), MBI vs. RAHI (OR 0.56; 95% CrI 0.11, 25.13), MBI vs. VI (OR 0.60; 95% CrI 0.13, 11.98), MFI vs. RAHI (OR 0.37; 95% CrI 0.07, 18.85), MFI vs. VI (OR 0.36; 95% CrI 0.07, 10.17), RAHI vs. VI (OR 0.15; 95% CrI 0.03, 20.62) (Table 4D). No statistical difference was observed between the direct and indirect comparisons (MFI vs. MBI, p=0.71; RAHI vs. MBI, p=0.90; V vs. MBI, p=0.61; RAHI vs. MFI, p=0.40; VI vs. MFI, p=0.60; VI vs. RAHI, p=0.65). The overall heterogeneity was low (I2 = 0%). The SUCRA rankings were 7% for MBI, 57% for MFI, 61% for RAHI, and 76% for VI.
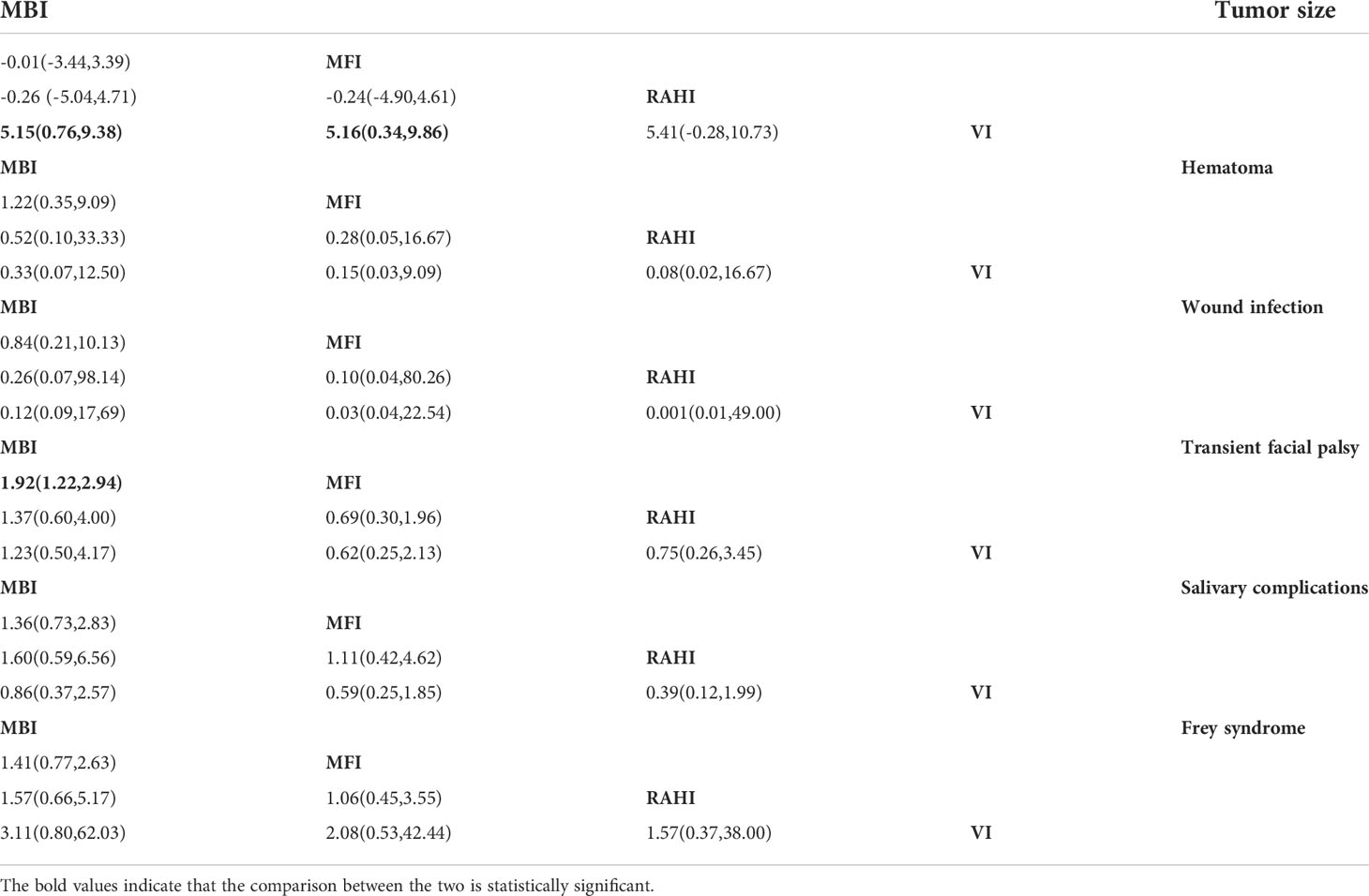
3.3.5 Secondary outcomes
Tables 5 and 6 provide a mixed comparison and SUCRA rankings of the secondary outcomes, respectively. Meta-analysis of the pooled network did not show statistically significant OR comparing MBI vs. MFI, MBI vs. RAHI, MBI vs. VI, MFI vs. RAHI, MFI vs. VI, and RAHI vs. VI in terms of hematoma (OR 1.22, 95% CrI 0.35, 9.09; OR 0.52, 95% CrI 0.10, 33.33; OR 0.33, 95% CrI 0.07, 12.50; OR 0.28, 95% CrI 0.05, 16.67; OR 0.15, 95% CrI 0.03, 9.09; OR 0.08, 95% CrI 0.02, 16.67, respectively). The SUCRA rankings were 40% for MBI, 67% for MFI, 56% for RAHI, and 37% for VI. Comparisons of the OR between MBI vs. MFI, MBI vs. RAHI, MBI vs. VI, MFI vs. RAHI, MFI vs. VI, and RAHI vs. VI were also not statistically significant for wound infection (OR 0.84, 95% CrI 0.21, 10.13; OR 0.26, 95% CrI 0.07, 98.14; OR 0.12, 95% CrI 0.09, 17.69; OR 0.10, 95% CrI 0.04, 80.26; OR 0.03, 95% CrI 0.04, 22.54; OR 0.001, 95% CrI 0.01, 49.00, respectively). The SUCRA rankings were 37% for MBI, 54% for MFI, 60% for RAHI, and 49% for VI. In addition, the pooled network meta-analysis did not find statistically significant ORs comparing MBI vs. MFI, MBI vs. RAHI, MBI vs. VI, MFI vs. RAHI, MFI vs. VI, and RAHI vs. VI in terms of salivary complications and Frey syndrome (salivary complications: OR 1.36, 95% CrI 0.73, 2.83; OR 1.60, 95% CrI 0.59, 6.56; OR 0.86, 95% CrI 0.37, 2.57; OR 1.11, 95% CrI 0.42, 4.62; OR 0.59, 95% CrI 0.25, 1.85; OR 0.39, 95% CrI 0.12, 1.99, respectively) (Frey syndrome: OR 1.41, 95% CrI 0.77, 2.63; OR 1.57, 95% CrI 0.66, 5.17; OR 3.11, 95% CrI 0.80, 62.03; OR 1.06, 95% CrI 0.45, 3.55; OR 2.08, 95% CrI 0.53, 42.44; OR 1.57, 95% CrI 0.37, 38.00, respectively). The SUCRA rankings of the former were 26% MBI, 66% MFI, 79% RAHI, and 28% VI, while that of the latter were 9%, 46%, 57%, and 89%, respectively. The overall heterogeneity of the four complications was zero (I2 = 0%). Similarly, pooled network meta-analysis did not demonstrate statistically significant ORs comparing MBI vs. RAHI, MBI vs. VI, MFI vs. RAHI, MFI vs. VI, and RAHI vs. VI in terms of transient facial palsy (OR 1.37, 95% CrI 0.60, 4.00; OR 1.23, 95% CrI 0.50, 4.17; OR 0.69, 95% CrI 0.30, 1.96; OR 0.62, 95% CrI 0.25, 2.13; OR 0.75, 95% CrI 0.26, 3.45, respectively). In contrast, MFI was associated with a statistically significant lower facial palsy compared to MBI (OR, 1.92; 95% CrI, 1.22, 2.94). The SUCRA rankings were 15% for MBI, 82% for MFI, 55% for RAHI, and 49% for VI. Overall heterogeneity was low (I2 = 0). Finally, meta-analysis of pooled networks showed similar MDs in terms of tumor size when comparing MBI vs. MFI (MD -0.01; 95% CrI -3.44, 3.39), MBI vs. RAHI (MD -0.26; 95% CrI -5.04, 4.71), MFI vs. RAHI (MD -0.24; 95% CrI -4.90, 4.61) and RAHI vs. VI (MD 5.41; 95% CrI -0.28, 10.73). However, MBI vs. VI (MD 5.15; 95% CrI 0.76, 9.38), and MFI vs. VI (MD 5.16; 95% CrI 0.34, 9.86) were significant. The SUCRA rankings were 36% for MBI, 35% for MFI, 31% for RAHI, and 98% for VI. Overall heterogeneity was low (I2 = 4).
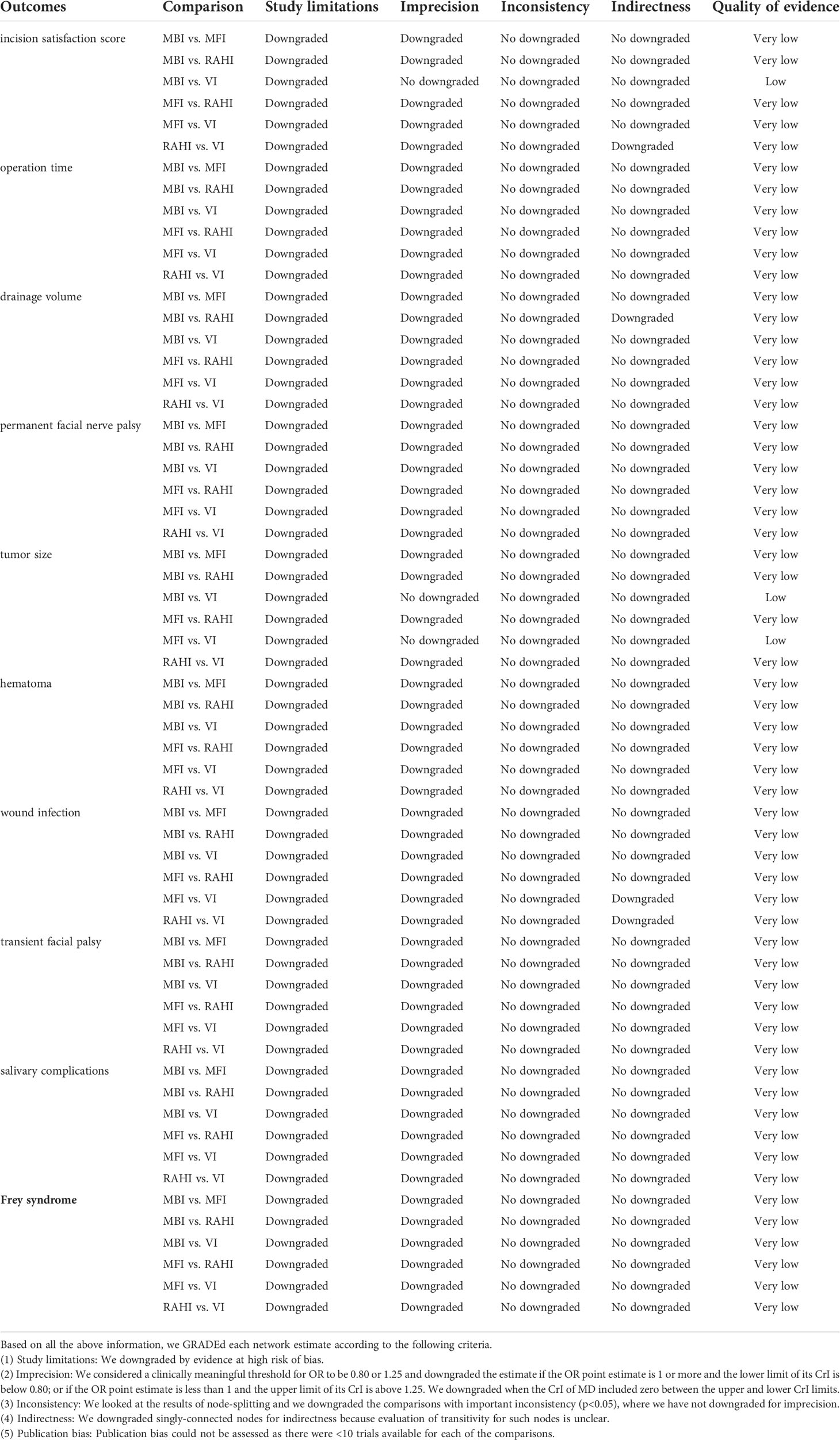
3.4 Validation and evaluation of models and results
The model fit using the diagnostic approach described in the methodology was good, and there was no evidence that any results were non-MCMC convergent. Furthermore, the node-splitting method did not exhibit any local inconsistencies. By comparing the adjusted funnel plots, no publication bias was observed in operation time, transient facial palsy, permanent facial palsy, or salivary gland complications; however, publication bias was found regarding the incision satisfaction score and Frey syndrome. Funnel plots were not drawn for the other outcomes because fewer than 10 studies were included. The GRADE rating results are listed in Table 7. The quality of evidence was rated as very low in most comparisons.
4 Discussion
This is the first systematic review and network meta-analysis to compare the surgical outcomes and complications of four major parotidectomy incisions. There were no significant differences in operation time, drainage volume, or permanent facial palsy. Similarly, no differences were found in salivary complications, wound infection, hematoma, or Frey syndrome. The incision satisfaction score was statistically significant in the comparison between the VI and MBI. Moreover, the VI had a smaller tumor size than MBI and MFI, and MFI had a significantly lower risk of transient facial palsy than MBI.
Generally, the following considerations govern the surgical incision design: full surgical field exposure and operability of lesion resection. Based on the above principles, the traditional Blair incision was gradually established as the most common parotidectomy method after modification. Unfortunately, these S-shaped incisions may leave a visible scar on the face and cause psychological distress (33). People are paying more attention to the requirements of beauty as their quality of life improves, and medical research has begun to investigate the potential for a good aesthetic effect while maintaining safety (5). The outcomes of primary incisions have been widely discussed; however, there has been a lack of convincing evidence on which procedure is optimal. Relevant RCTs and pairwise meta-analyses are few and far between, and previously published observational studies have had inconsistent results, which may be related to heterogeneity in the population and surgical technique. We performed a comprehensive Bayesian network meta-analysis to compare the outcomes of major surgical incisions in parotidectomy.
Scarring after parotidectomy is estimated to be between 54% and 60% based on prior research (34, 35). Traditional MBI incisions inevitably leave scarring on the face and neck, and numerous studies have noted significant patient dissatisfaction with scarring, which affects long-term quality of life (36). Although some techniques, such as skin flap and fascia reconstruction, can help prevent this issue, locating a better concealed incision can also help lessen the cosmetic negative impacts of scars (37). The novel VI, consisting of only anterior and posterior auricular incisions, has shown good cosmetic results in some previous studies (27, 31, 38). Similarly, based on the results of the SUCRA, our study rated VI as an approach with a higher incision satisfaction score and found it significantly superior to MBI. Furthermore, VI was significantly associated with tumor size when compared with MBI and MFI, indicating that tumor size is one of the parameters used by surgeons to choose surgical incisions. However, SUCRA data revealed that VI required the most operation time and MBI the least, despite no statistically significant difference between the four incisions. This might be attributed to a higher level of mastery of classical procedures; therefore, as proficiency increases, the surgical times for emerging incisions can be expected to decrease.
Owing to the substantial blood supply in the parotid gland region, much of the leaking blood, as well as saliva released by the remaining gland, would be collected in the cavity generated following parotidectomy (39). The presence of these fluids can cause complications such as seroma, and head and neck wounds should be drained with a drainage tube, according to the national consensus (39). Excessive drainage flow is likely to cause complications, such as infection and salivary fistula, resulting in prolonged hospital stays and increased medical costs (40). Notably, although there was no statistically significant difference in drainage volume between the four types of incisions, the RAHI was classified in the SUCRA ranking as the incisions with the least drainage.
Transient facial palsy is the most frequent early complication of parotidectomy (41). Permanent facial palsy after parotidectomy is the most serious complication that affects patients’ quality of life. According to previous studies, the incidences of early transient facial palsy and long-term permanent facial palsy are 42-45% and 0-3.9%, respectively (34, 35). With the gradual standardization of parotid surgery for the dissection and protection of facial nerves, and the wide application of intraoperative facial nerve monitoring, the incidence of facial paralysis has been greatly reduced; this in turn reduces the difference in the incidence of facial paralysis caused by different incisions (42, 43). In this review, the SUCRA results showed that conventional MBI had the highest risk of facial palsy. Furthermore, MBI’s SUCRA ranking in complications such as hematoma, wound infection, and salivary gland damage remained low, although the difference was not statistically significant in the pooled comparison results.
Frey syndrome occurs in 4-62% of patients 6 to 18 months after parotidectomy and is characterized by gustatory sweating and flushing (44). The incidence of Frey syndrome was documented in 12 of the included studies; however, none of these studies described the use of objective methods for diagnosis, which may result in the reported incidence being lower than the true value (45). A number of surgical techniques have been described to prevent this complication, and studies have attempted to determine the best way to reduce its incidence (46). Studies have shown that the size of the parotid gland tumor affects the incidence of Frey syndrome, which is explained by the fact that the less parotid tissue that needs to be dissected, the lower the likelihood of parasympathetic supply disruption (18, 47, 48). This view is seemingly supported by our findings, which shows that the SUCRA ranking of Frey syndrome and tumor size are consistent among the four incisions.
Although our meta-analysis yielded several novel results, it had certain limitations. First, this study contained only one RCT, with the remainder being single-center observational studies with potential selection and reporting bias. Second, two-thirds of the studies were conducted in East Asia, limiting the worldwide generalizability of our findings. Third, there was significant heterogeneity between MBI and the other three incisions in the pairwise meta-analyses. Fourth, some of the primary outcomes were rated as low or very low in evidential strength, based on the GRADE evaluation. Therefore, this may undermine the strength of the current findings. However, it is important to understand that high-quality evidence might be difficult to obtain because grade judgments can be overly cautious (49).
Conclusion
Based on published studies, our network meta-analysis provides updated evidence for the multiple outcomes of MBI, MFI, RAHI, and VI. The most important advantages of VI are good incision satisfaction and better performance in the management of complications. Further randomized controlled trials and complementary outcome data are needed to test the credibility of our findings.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Author contributions
All the authors worked together to complete the paper. YJ, SY, and CS did the literature search; YJ, SY, and YL formed the study design; Data collection was done by SY, YL, YH, and ZF. SY, ZF, and YL analyzed the data; BC, SS, JW and XW interpreted the data; YJ, SY, and CS wrote the manuscript; YJ, SY, and BC critically reviewed the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This project was supported by applied medicine research project of Hefei Health Committee (hwk2019zc004).
Acknowledgments
We thank the original studies included for providing data for our study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2022.972498/full#supplementary-material
References
1. Pinkston JA, Cole P. Incidence rates of salivary gland tumors: Results from a population-based study. Otolaryngol–head Neck Surg Off J Am Acad Otolaryngol-Head Neck Surg (1999) 120(6):834–40. doi: 10.1016/s0194-5998(99)70323-2
2. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: Globocan estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: Cancer J Clin (2021) 71(3):209–49. doi: 10.3322/caac.21660
3. Tian Z, Li L, Wang L, Hu Y, Li J. Salivary gland neoplasms in oral and maxillofacial regions: A 23-year retrospective study of 6982 cases in an Eastern Chinese population. Int J Oral Maxillofac Surg (2010) 39(3):235–42. doi: 10.1016/j.ijom.2009.10.016
4. Bradley PJ, McGurk M. Incidence of salivary gland neoplasms in a defined uk population. Br J Oral Maxillofac Surg (2013) 51(5):399–403. doi: 10.1016/j.bjoms.2012.10.002
5. Aggarwal V. Incisions for parotidectomy: A narrative review. Ann Plast Surg (2021) 87(4):e71–e8. doi: 10.1097/sap.0000000000002757
6. Nouraei SA, Al-Yaghchi C, Ahmed J, Kirkpatrick N, Mansuri S, Singh A, et al. An anatomical comparison of Blair and facelift incisions for parotid surgery. Clin Otolaryngol Off J ENT-UK ; Off J Netherlands Soc Oto-Rhino-Laryngol Cervico-Facial Surg (2006) 31(6):531–4. doi: 10.1111/j.1365-2273.2006.01334.x
7. Fiacchini G, Cerchiai N, Tricò D, Sellari-Franceschini S, Casani AP, Dallan I, et al. Frey Syndrome, first bite syndrome, great auricular nerve morbidity, and quality of life following parotidectomy. Eur Arch oto-rhino-laryngol Off J Eur Fed Oto-Rhino-Laryngol Societies (EUFOS) affiliated German Soc Oto-Rhino-Laryngol - Head Neck Surg (2018) 275(7):1893–902. doi: 10.1007/s00405-018-5014-4
8. Lee YC, Liao WC, Yang SW, Luo CM, Tsai YT, Tsai MS, et al. Systematic review and meta-analysis of modified facelift incision versus modified Blair incision in parotidectomy. Sci Rep (2021) 11(1):24106. doi: 10.1038/s41598-021-03483-6
9. Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The cochrane collaboration's tool for assessing risk of bias in randomised trials. BMJ (Clinical Res ed) (2011) 343:d5928. doi: 10.1136/bmj.d5928
10. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The prisma statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ (Clinical Res ed) (2009) 339:b2700. doi: 10.1136/bmj.b2700
11. Brignardello-Petersen R, Murad MH, Walter SD, McLeod S, Carrasco-Labra A, Rochwerg B, et al. Grade approach to rate the certainty from a network meta-analysis: Avoiding spurious judgments of imprecision in sparse networks. J Clin Epidemiol (2019) 105:60–7. doi: 10.1016/j.jclinepi.2018.08.022
12. Dias S, Welton NJ, Sutton AJ, Ades AE. Nice decision support unit technical support documents. nice dsu technical support document 2. In: A generalised linear modelling framework for pairwise and network meta-analysis of randomised controlled trials. London: National Institute for Health and Care Excellence (NICE (2014).
13. Dias S, Welton NJ, Sutton AJ, Caldwell DM, Lu G, Ades AE. Nice decision support unit technical support documents. nice dsu technical support document 4. In: Inconsistency in networks of evidence based on randomised controlled trials. London: National Institute for Health and Care Excellence (NICE (2014).
14. Salanti G, Ades AE, Ioannidis JP. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: An overview and tutorial. J Clin Epidemiol (2011) 64(2):163–71. doi: 10.1016/j.jclinepi.2010.03.016
15. Puhan MA, Schünemann HJ, Murad MH, Li T, Brignardello-Petersen R, Singh JA, et al. A grade working group approach for rating the quality of treatment effect estimates from network meta-analysis. BMJ (Clinical Res ed) (2014) 349:g5630. doi: 10.1136/bmj.g5630
16. Terris DJ, Tuffo KM, Fee WE Jr. Modified facelift incision for parotidectomy. J laryngol otol (1994) 108(7):574–8. doi: 10.1017/s002221510012746x
17. Roh JL. Retroauricular hairline incision for removal of upper neck masses. Laryngoscope (2005) 115(12):2161–6. doi: 10.1097/01.Mlg.0000181496.22493.5a
18. Wasson J, Karim H, Yeo J, Panesar J. Cervicomastoidfacial versus modified facelift incision for parotid surgery: A patient feedback comparison. Ann R Coll Surgeons Engl (2010) 92(1):40–3. doi: 10.1308/003588410x12518836440009
19. Bianchi B, Ferri A, Ferrari S, Copelli C, Sesenna E. Improving esthetic results in benign parotid surgery: Statistical evaluation of facelift approach, sternocleidomastoid flap, and superficial musculoaponeurotic system flap application. J Oral Maxillofac Surg (2011) 69(4):1235–41. doi: 10.1016/j.joms.2010.03.005
20. Lee SY, Koh YW, Kim BG, Hong HJ, Jeong JH, Choi EC. The extended indication of parotidectomy using the modified facelift incision in benign lesions: Retrospective analysis of a single institution. World J Surg (2011) 35(10):2228–37. doi: 10.1007/s00268-011-1209-1
21. Zhi KQ, Ren WH, Gao L, Zhao L, Huang S, Li JW, et al. Face-lift incision combined with sternomastoid muscular flap in parotidectomy. Aesthetic Plast Surg (2011) 35(4):558–62. doi: 10.1007/s00266-011-9663-6
22. Graciano AJ, Chone CT, Fischer CA. Cervicomastoidfacial versus modified rhytidectomy incision for benign parotid tumors. Braz J otorhinolaryngol (2013) 79(2):168–72. doi: 10.5935/1808-8694.20130030
23. Kim DY, Park GC, Cho YW, Choi SH. Partial superficial parotidectomy Via retroauricular hairline incision. Clin Exp otorhinolaryngol (2014) 7(2):119–22. doi: 10.3342/ceo.2014.7.2.119
24. Bulut OC, Plinkert P, Federspil PA. Modified facelift incision for partial parotidectomy versus bayonet-shaped incision: A comparison using visual analog scale. Eur Arch Oto-Rhino-Laryngol (2016) 273(10):3269–75. doi: 10.1007/s00405-015-3878-0
25. Wu PA, Lu ZQ, Guan YF, Zhu HL, Liang XN, Liang WY, et al. [Application of functional parotidectomy Via retroauricular hairline incision in the excising superficial parotid tumor]. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi (2017) 52(12):905–8. doi: 10.3760/cma.j.issn.1673-0860.2017.12.006
26. Xu ZJ, Chen LS, Zhan JD, Xu MM, Zhang B, Huang SL, et al. [Modified rhytidectomy incision and modified Blair incision contrast research in superficial parotid gland tumor resection]. Lin chuang er bi yan hou tou jing wai ke za zhi = J Clin otorhinolaryngol head Neck Surg (2017) 31(21):1684–7. doi: 10.13201/j.issn.1001-1781.2017.21.015
27. Zheng ZW, Li J, Wang JB, Sun J. Hidden scar dissection of benign parotid gland tumors Via a V-shaped minimal facelift incision. J Craniofacial Surg (2018) 29(8):2299–303. doi: 10.1097/scs.0000000000004670
28. Ahn DB, Lee GJ, Sohn JH. Individualized use of facelift, retroauricular hairline, and V-shaped incisions for parotidectomy. J Oral Maxillofac Surg (2020) 78(12):1–7. doi: 10.1016/j.joms.2020.08.021
29. Li MM, Li SS, Tang QL, Yang XM, He XB. Feasibility and efficacy of partial superficial parotidectomy with V-shaped incision. Zhonghua er bi yan hou tou jing wai ke za zhi [Chinese J otorhinolaryngol Head Neck surgery] (2020) 55(7):658–63. doi: 10.3760cma.j.cn115330-20191109-00678
30. Chen F, Li Y, Ke X, Wu PF, Guo LY, Lei ZG, et al. Application analysis of a modified retroauricular hairline incision in the resection of a benign parotid gland tumor. Hua xi kou qiang yi xue za zhi = Huaxi kouqiang yixue zazhi = West China J stomatol (2021) 39(3):293–9. doi: 10.7518/hxkq.2021.03.008
31. Jo MG, Lee DJ, Cha W. A modified V-shaped incision combined with superficial musculo-aponeurotic system flap for parotidectomy. Acta oto-laryngol (2019) 139(2):178–83. doi: 10.1080/00016489.2018.1562216
32. Matsumoto F, Ohba S, Fujimaki M, Kojima T, Sakyo A, Kojima M, et al. Efficacy of modified face lift incision for the resection of benign parotid gland tumor located anteriorly or superiorly. Auris nasus larynx (2021) 48(5):978–82. doi: 10.1016/j.anl.2021.01.014
33. Kaya BV, Kılıç C, Özlügedik S, Tuncel Ü, Cömert E. Long-term effects of parotidectomy. Eur Arch oto-rhino-laryngol Off J Eur Fed Oto-Rhino-Laryngol Societies (EUFOS) affiliated German Soc Oto-Rhino-Laryngol - Head Neck Surg (2016) 273(12):4579–83. doi: 10.1007/s00405-016-4173-4
34. Gaillard C, Périé S, Susini B, St Guily JL. Facial nerve dysfunction after parotidectomy: The role of local factors. Laryngoscope (2005) 115(2):287–91. doi: 10.1097/01.mlg.0000154735.61775.cd
35. Mehle ME, Kraus DH, Wood BG, Benninger MS, Eliachar I, Levine HL, et al. Facial nerve morbidity following parotid surgery for benign disease: The Cleveland clinic foundation experience. Laryngoscope (1993) 103(4 Pt 1):386–8. doi: 10.1002/lary.5541030404
36. Lambiel S, Dulguerov N, Courvoisier DS, Dulguerov P. Minor parotidectomy complications: A systematic review. Laryngoscope (2021) 131(3):571–9. doi: 10.1002/lary.28912
37. Dell'aversana Orabona G, Salzano G, Petrocelli M, Iaconetta G, Califano L. Reconstructive techniques of the parotid region. J craniofacial Surg (2014) 25(3):998–1002. doi: 10.1097/scs.0000000000000664
38. Ahn D, Sohn JH, Lee GJ. Feasibility of a new V-shaped incision for parotidectomy: A preliminary report. Br J Oral Maxillofac Surg (2018) 56(5):406–10. doi: 10.1016/j.bjoms.2018.03.014
39. Chen WC, Chuang HC, Su YY, Chien CY. Predictive factors for post-operative drainage after partial superficial parotidectomy: A case-control study. J laryngol otol (2015) 129(10):1020–4. doi: 10.1017/s002221511500211x
40. Woods RS, Woods JF, Duignan ES, Timon C. Systematic review and meta-analysis of wound drains after thyroid surgery. Br J Surg (2014) 101(5):446–56. doi: 10.1002/bjs.9448
41. Venkatesh S, Srinivas T, Hariprasad S. Parotid gland tumors: 2-year prospective clinicopathological study. Ann Maxillofac Surg (2019) 9(1):103–9. doi: 10.4103/ams.ams_179_18
42. Brennan J, Moore EJ, Shuler KJ. Prospective analysis of the efficacy of continuous intraoperative nerve monitoring during thyroidectomy, parathyroidectomy, and parotidectomy. Otolaryngol–head Neck Surg Off J Am Acad Otolaryngol-Head Neck Surg (2001) 124(5):537–43. doi: 10.1067/mhn.2001.115402
43. Sood AJ, Houlton JJ, Nguyen SA, Gillespie MB. Facial nerve monitoring during parotidectomy: A systematic review and meta-analysis. Otolaryngol–head Neck Surg Off J Am Acad Otolaryngol-Head Neck Surg (2015) 152(4):631–7. doi: 10.1177/0194599814568779
44. Motz KM, Kim YJ. Auriculotemporal syndrome (Frey syndrome). Otolaryngol Clinics North America (2016) 49(2):501–9. doi: 10.1016/j.otc.2015.10.010
45. Neumann A, Rosenberger D, Vorsprach O, Dazert S. [the incidence of Frey syndrome following parotidectomy: Results of a survey and follow-up]. Hno (2011) 59(2):173–8. doi: 10.1007/s00106-010-2223-6
46. De Virgilio A, Costantino A, Russo E, Ferreli F, Pellini R, Petruzzi G, et al. Different surgical strategies in the prevention of Frey syndrome: A systematic review and meta-analysis. Laryngoscope (2021) 131(8):1761–8. doi: 10.1002/lary.29414
47. Myssiorek D. Removal of the inferior half of the superficial lobe is sufficient to treat pleomorphic adenoma in the tail of the parotid gland. Arch otolaryngol–head Neck Surg (1999) 125(10):1164–5. doi: 10.1001/archotol.125.10.1164
48. Gordon AB, Fiddian RV. Frey's syndrome after parotid surgery. Am J Surg (1976) 132(1):54–8. doi: 10.1016/0002-9610(76)90290-7
Keywords: parotidectomy, surgical incision, Bayesian network meta-analysis, modified Blair incision, modified facelift incision, retroauricular hairline incision, V-shaped incision
Citation: Yin S, Han Y, Liu Y, Chen B, Fu Z, Sheng S, Wang J, Shen C, Wang X and Jia Y (2022) Comparison of various surgical incisions in parotidectomy: A systematic review and network meta-analysis. Front. Oncol. 12:972498. doi: 10.3389/fonc.2022.972498
Received: 18 June 2022; Accepted: 13 July 2022;
Published: 05 August 2022.
Edited by:
Cesare Ruffolo, University Hospital of Padua, ItalyReviewed by:
Giovanni Cristalli, Ospedali Riuniti Padova Sud Madre Teresa di Calcutta, ItalyFabio Ferreli, Humanitas University, Italy
Copyright © 2022 Yin, Han, Liu, Chen, Fu, Sheng, Wang, Shen, Wang and Jia. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yiwen Jia, tbjyw1990@126.com
†These authors have contributed equally to this work and share first authorship
 Siyue Yin
Siyue Yin Yanxun Han
Yanxun Han Yuchen Liu
Yuchen Liu Bangjie Chen
Bangjie Chen Ziyue Fu2
Ziyue Fu2 Shuyan Sheng
Shuyan Sheng Jianpeng Wang
Jianpeng Wang Yiwen Jia
Yiwen Jia