- Princess Srisavangavadhana College of Medicine, Chulabhorn Royal Academy, Bangkok, Thailand
A 13-year-old boy presented with a growing lump on his left clavicle for 5 months. The plain radiograph revealed an osteolytic mass with aggressive periosteal reaction, suggesting a malignant lesion. The results of advanced imaging and histopathological examinations revealed that the patient had Ewing sarcoma without metastasis. The two-stage surgery was as follows: resection–observation–reconstruction. The underlying rationale was that Ewing sarcoma has a high recurrence. After 2 years of resection, the patient had remission, and he currently has a personal 3D-printed titanium implant with intact shoulder function.
Introduction
Ewing sarcoma is the second most common bone tumor in children and young adults (1). This type of cancer can develop in any bone but usually occurs in the lower extremities, most commonly in the pelvis and femur (2). Although occurrence in the clavicle has been reported, it is considered a rare case (3). Previous studies have reported alternative surgical techniques; however, to our knowledge, a suitable management strategy has yet to be established for Ewing sarcoma of the clavicle (4).
Background
A 13-year-old boy presented with a growing lump on his left clavicle for 5 months. The patient had a 10-cm painless, smooth, and palpable mass with a rubbery-to-hard consistency on his left distal clavicle. The patient’s blood reports were normal. Plain radiography of the left clavicle showed an abnormal, enlarged osteolytic lesion with a moth-eaten, lamellated appearance. It also showed a focally disrupted aggressive periosteal reaction throughout the distal half of the clavicle, with a swollen overlying soft tissue (Figure 1). Skeletal scintigraphy revealed increased focal tracer uptake at the left clavicle, corresponding to the primary bone lesion. The magnetic resonance imaging result showed a 10.1 × 4.1 × 3.3-cm, expansible, intramedullary lesion at the left clavicle bone with intermediate T1 heterogeneous signal and hyperintensity T2 with heterogeneous enhancement, which suggested Ewing sarcoma (Figure 2). No lung and whole-abdomen abnormalities were identified. The results of a histopathologic analysis showed a round cell tumor corresponding to Ewing sarcoma of the left distal clavicle.

Figure 1 Plain radiograph of the left clavicle showing an abnormal, enlarged osteolytic lesion with a moth-eaten, lamellated appearance, and focally disrupted aggressive periosteal reaction throughout the distal half of the clavicle, with a swollen overlying soft tissue.
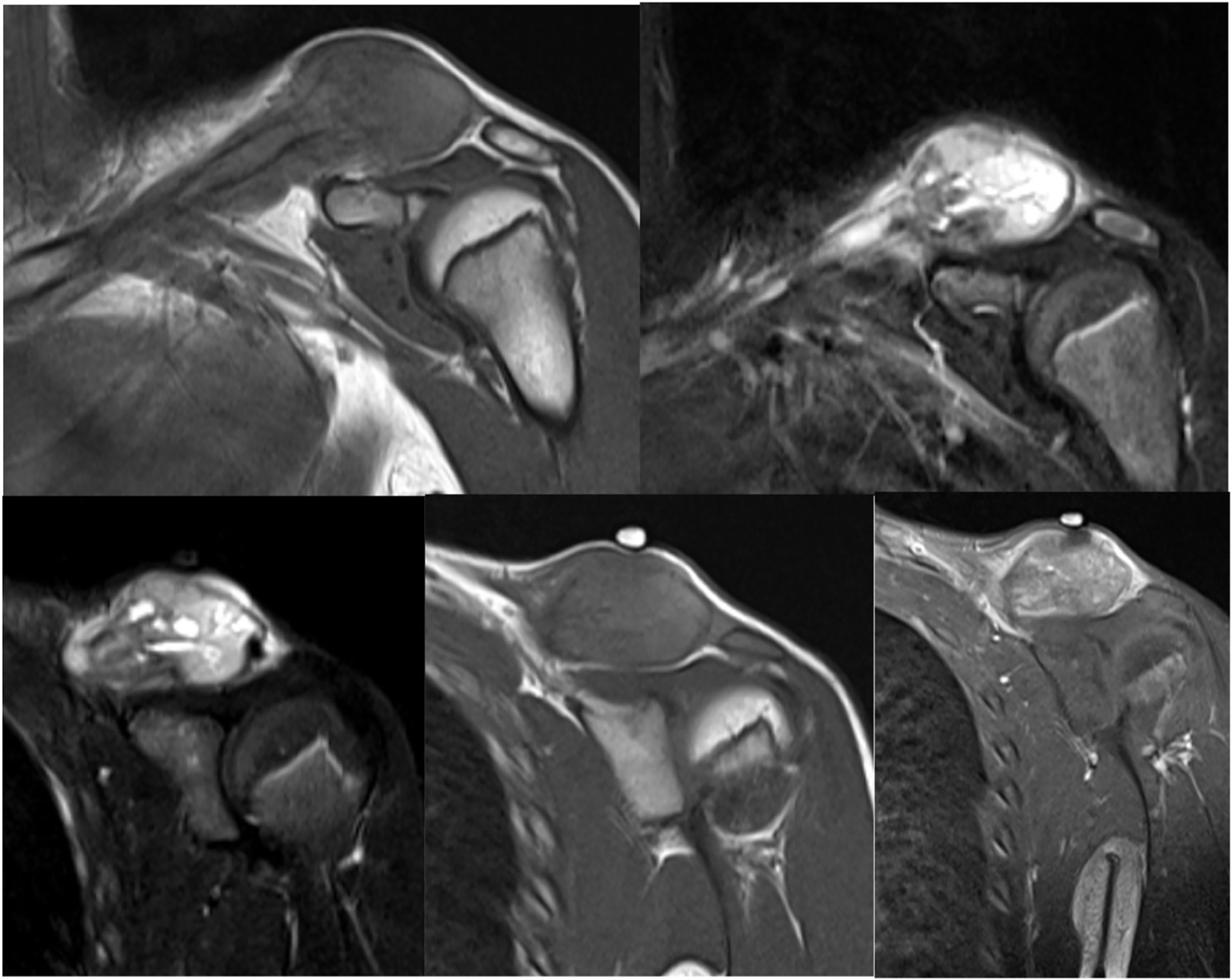
Figure 2 MRI of the shoulder revealing a 10.1 × 4.1 × 3.3-cm expansible intramedullary lesion on the left clavicle bone with intermediate T1 heterogeneous signal and low hyper T2 with heterogeneous enhancement, which likely corresponded to Ewing sarcoma.
The patient was prescribed with neoadjuvant therapy with 14 cycles of vincristine, doxorubicin, cyclophosphamide, ifosfamide, and etoposide. The first stage of operation is wide resection at the left distal clavicle and reconstruction with plate and cementation. With no evidence of recurrence noted in 2 years, the patient was subjected to the second-stage operation with a patient-specific 3D-printed personalized left distal clavicle reconstruction.
The first stage of this treatment involved the wide resection of the left distal clavicle and its subsequent reconstruction with a plate and cement. The results of a pathological analysis of the specimen collected from the intraoperative site showed neither viable nor tumor cells. The patient recovered well, and his left shoulder functions and range of motion remained intact. A year after the first surgery, the patient showed no signs of recurrent Ewing sarcoma (Figure 3).
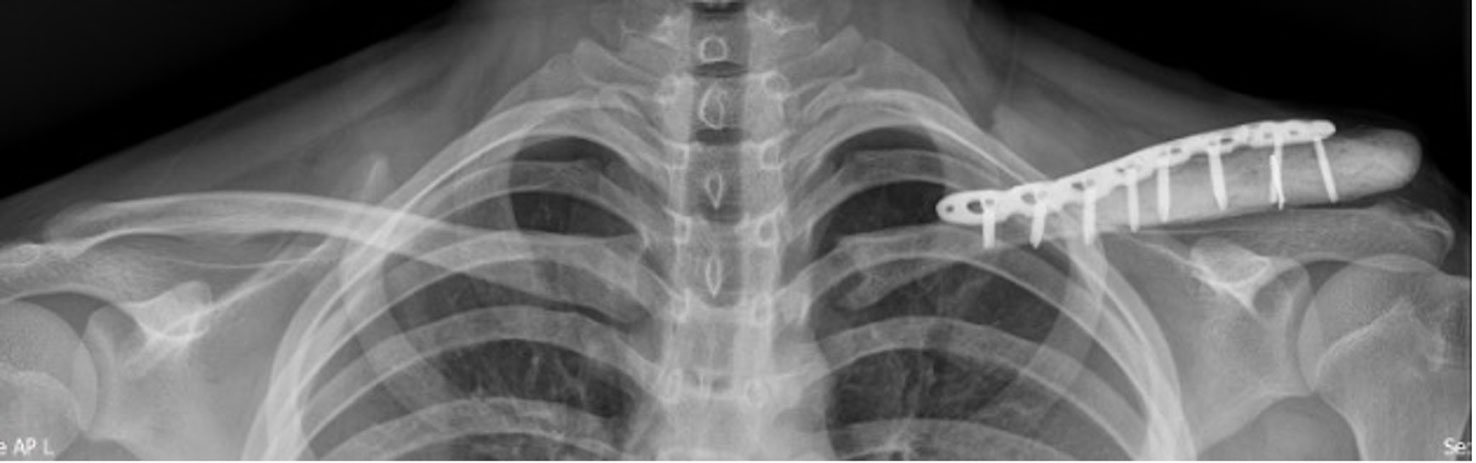
Figure 3 Radiograph of the left clavicle at 1 month after surgery and reconstruction. The patient showed no signs of recurrence or disease progression.
At 2 years later, the surgery’s second stage was performed with a personalized 3D-printed titanium prosthesis for reconstruction to ensure a long-term replacement. Immediate postoperative plain films were obtained again, which showed satisfactory results (Figures 4A–C).
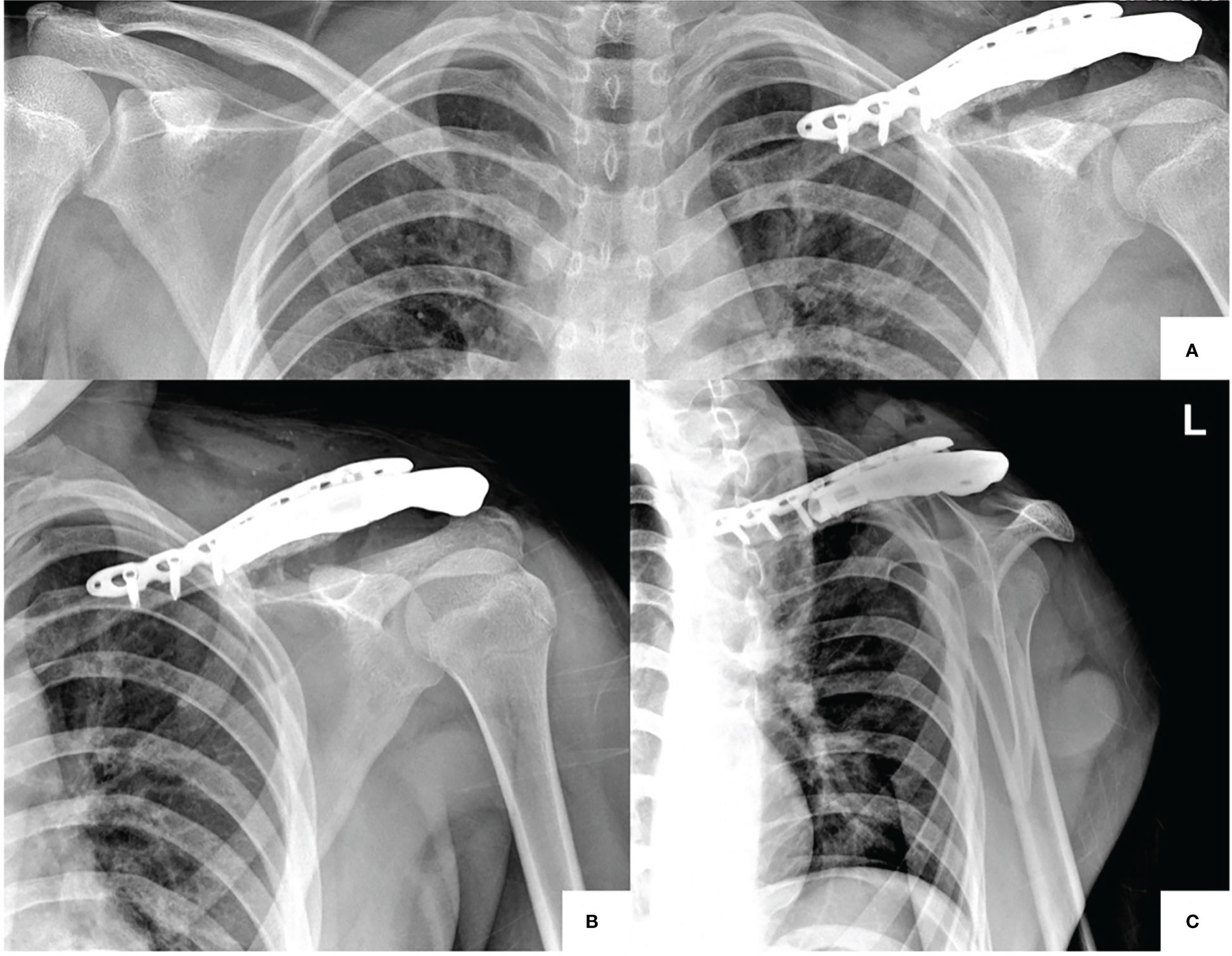
Figure 4 (A–C) Postoperative second-stage surgery with personalized 3D-printed titanium prosthesis for reconstruction. AP view, comparing both clavicles (A), AP view (B), and transcapular view (C).
At 2 months after the second-stage surgery, the wound showed good healing with minimal scarring. At 2 years after the operation, the shoulder and arm functions remained intact.
Discussion
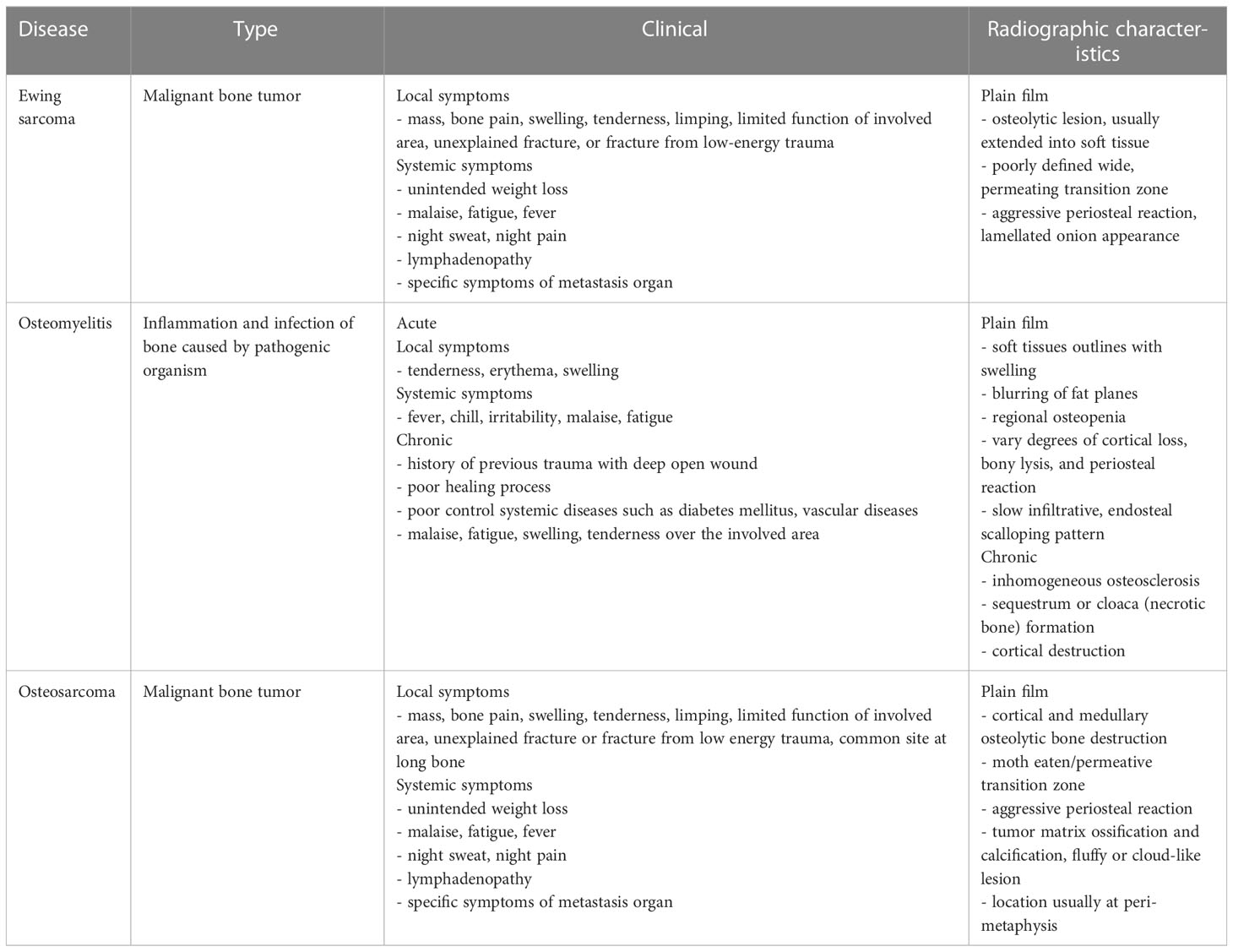
Osteosarcoma, the most common primary bone tumor, should be one of the first differential diagnoses for patients in this age group presenting with these symptoms. Osteomyelitis is an additional diagnosis characterized by inflammatory pain with or without an abnormal mass. However, retrospective studies and case reports have shown that Ewing sarcoma, one of the most common tumors of flat bones, is the most common tumor occurring at the clavicle (1). The children and adolescents presented with an abnormal clavicle mass. The differential diagnoses of Ewing sarcoma, osteomyelitis, and osteosarcoma were considered (Table 1).
The results of advanced imaging revealed the presence of a local disease at the left clavicle, likely Ewing sarcoma, without solid evidence of distant metastasis to another organ. In addition, a histopathological analysis of biopsy specimens resulted in the identification of small round cells, thus supporting the initial diagnosis that this patient had Ewing sarcoma.
A treatment protocol for Ewing sarcoma was selected following the guidelines published by Womer et al. (2012) (5). More specifically, the treatment comprised 14 cycles of alternating neoadjuvant therapy VDC/IE regimen every 2 weeks: vincristine, doxorubicin, cyclophosphamide/ifosfamide, and etoposide. The standard surgical operation for Ewing sarcoma involves a wide tumor resection with or without reconstruction. Previous studies have shown similar results and functions in total claviculectomy regardless of whether reconstruction was performed (6). The necessity of reconstruction of the clavicle after resection is still questioned, as similar functional results have been obtained in patients treated without reconstruction with a tendency to a lower incidence of complications and surgical revisions (7, 8). However, the prosthesis reconstruction was selected for esthetic reasons because it would provide the young patient with a lifelong implant instead of cementation. Previous reports on Ewing sarcoma have also attempted autograft, allograft, and cement for clavicle reconstructions in adult patients (9). Nevertheless, graft selections are limited regarding varieties and associated costs in Thailand. Owing to the high recurrence rate of this disease, it is not financially reasonable to immediately perform reconstructive surgery. Therefore, a two-stage surgery was performed: wide resection and reconstruction with medical cement, observation for possible recurrence, and definite reconstruction surgery; all procedures were explained to the patient and his family. Clavicle reconstruction with cement as a prosthesis has been previously performed as a practical and feasible short-to-medium-term therapeutic procedure with acceptable results.
A year after the first surgery, the patient showed no signs of Ewing sarcoma. His left shoulder function and range of motion remained intact and provided independence in most daily activities. However, high recurrence rates have been reported, with >70% of relapsed cases occurring approximately 24 months after diagnosis and delayed recurrence occurring 10 years after remission. In this case, remission was determined after close observations and 1-year follow-up after surgical resection. At 2 years after diagnosis and initial treatment, we then proceeded to perform the second stage of the surgery as planned.
Because of the limited graft selection mentioned above, we used a 3D-printed personalized prosthesis for reconstruction. Titanium with a hydroxyapatite surface coating was selected as the prosthetic material because it has good biocompatibility and promotes improved in vitro osteointegration. In the anterior chest wall reconstruction, the titanium representation is the flexible material suitable for chest wall movement (10). In addition, the implant was designed to be partially hollow to reduce the material cost and allow the insertion of a bone graft for improved osteointegration. The implant also had screw holes designed in such a way that they could fit onto an identical plate that the patient already had.
Concluding remarks
The two-stage surgery—the recurrence observation in the first stage and then the 3D-printed personalized prosthesis for the second stage (substantial reconstruction)—provides a reasonable balance between recurrence risk and financial risk if the tumor was recurring.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by Human Research Ethics Committee Chulabhorn Research Institute (project code 002/2565).
Author contributions
All authors have read and approved the manuscript. PA and TC: Conceptualization, Methodology, Validation, Formal analysis, Investigation, Data Curation, Writing - Original Draft, Visualization, Supervision, Project administration. PP and SW: Validation, Formal analysis, Investigation, Writing - Original Draft, Supervision, Project administration, Writing - Review and Editing. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Burchill SA. Ewing's sarcoma: Diagnostic, prognostic, and therapeutic implications of molecular abnormalities. J Clin Pathol (2003) 56(2):96–102. doi: 10.1136/jcp.56.2.96
2. Riggi N, Stamenkovic I. The biology of Ewing sarcoma. Cancer Lett (2007) 254(1):1–10. doi: 10.1016/j.canlet.2006.12.009
3. Kapoor S, Tiwari A, Kapoor S. Primary tumours and tumorous lesions of clavicle. Int Orthop (2008) 32(6):829–34. doi: 10.1007/s00264-007-0397-7
4. Xue R, Lewis VO, Moon BS, Lin PP. Local recurrence of Ewing sarcoma: Is wide excision an acceptable treatment? J Surg Oncol (2019) 120(4):746–52. doi: 10.1002/jso.25615
5. Womer RB, West DC, Krailo MD, Dickman PS, Pawel BR, Grier HE, et al. Randomized controlled trial of interval-compressed chemotherapy for the treatment of localized Ewing sarcoma: A report from the children's oncology group. J Clin Oncol (2012) 30(33):4148–54. doi: 10.1200/JCO.2011.41.5703
6. Li J, Wang Z, Fu J, Shi L, Pei G, Guo Z. Surgical treatment of clavicular malignancies. J Shoulder Elbow Surg (2011) 20(2):295–300. doi: 10.1016/j.jse.2010.05.009
7. Liu Y, Huang XY, Feng WY, Luo X-T, Wei C-W, Liu J-H, et al. Analysis of the clinical efficacy of tumor resection methods used in 20 patients with clavicular tumor. World J Surg Onc (2019) 17:106. doi: 10.1186/s12957-019-1642-4
8. Chen Y, Yu X, Huang W, Wang B. Is clavicular reconstruction imperative for total and subtotal claviculectomy? a systematic review. J Shoulder Elbow Surg (2018) 27(5):e141–8. doi: 10.1016/j.jse.2017.11.003
9. Lin B, He Y, Xu Y, Sha M. Outcome of bone defect reconstruction with clavicle bone cement prosthesis after tumor resection: A case series study. BMC Musculoskelet Disord (2014) 15:183. doi: 10.1186/1471-2474-15-183
Keywords: Ewing sarcoma, distal clavicle, personalized 3D reconstruction, patient-specific implants, clavicle reconstruction
Citation: Arunwatthanangkul P, Piyabenjarad P, Wisitthipakdeekul S and Chobpenthai T (2023) Innovative method with two-stage surgery for Ewing sarcoma with personalized distal clavicle reconstruction: A case report and diagnosis review. Front. Oncol. 13:1134324. doi: 10.3389/fonc.2023.1134324
Received: 30 December 2022; Accepted: 14 March 2023;
Published: 29 March 2023.
Edited by:
Alessandro Gonfiotti, University of Florence, ItalyReviewed by:
Duilio Divisi, University of L’Aquila, ItalyFrancesco Zaraca, Ospedale di Bolzano, Italy
Copyright © 2023 Arunwatthanangkul, Piyabenjarad, Wisitthipakdeekul and Chobpenthai. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Thanapon Chobpenthai, thanapon.cho@cra.ac.th
 Patcharapol Arunwatthanangkul
Patcharapol Arunwatthanangkul Panichanok Piyabenjarad
Panichanok Piyabenjarad Siraprapa Wisitthipakdeekul
Siraprapa Wisitthipakdeekul Thanapon Chobpenthai
Thanapon Chobpenthai