- 1Department of Gynecology, Affiliated Hangzhou First People’s Hospital, Westlake University School of Medicine, Hangzhou, Zhejiang, China
- 2Department of Gynecology, TongLu County Maternal and Child Health Hospital, Hangzhou, Zhejiang, China
- 3Fourth Clinical School of Medicine, Zhejiang University of Chinese Medicine, Zhejiang, Hangzhou, China
Background: Typical treatments for cervical high-grade squamous intraepithelial lesion (HSIL) are invasive procedures. However, these procedures often come with several severe side effects, despite their positive effects on cervical HSIL. 5-aminolevulinic acid photodynamic therapy (ALA-PDT) is a non-invasive treatment that has been successfully used to treat cervical low-grade squamous intraepithelial lesion (LSIL). In this study, we aimed to further investigate the clinical efficacy and safety of ALA-PDT in the treatment of patients with cervical HSIL.
Methods: A total of 40 patients aged 20 - 41 years with cervical HSIL and high-risk Human Papilloma Virus (HR-HPV) infections were enrolled in this retrospective study from January 2019 to December 2022. Patients were treated with six times of ALA-PDT at intervals of 7–14 days. Three months after the treatment, the efficacy was evaluated through HPV genotyping and cervical cytology examination. If the cytological result was worse than ASC -US, the patient underwent colposcopy-directed biopsy immediately. Otherwise, patients would receive rigorous follow-up observation.
Results: Three months after receiving ALA-PDT treatment, 65% (26/40) of cervical HSIL patients at our center showed complete regression (cytological result: normal; HR-HPV: negative). This rate increased to 82.5% (33/40) at the 12-month follow-up. None of the patients experienced disease progression after ALA-PDT therapy. The risk of persistent HR-HPV infection was 32.5% (13/40) at the 3-month follow-up after ALA-PDT. Multivariate analyses identified cervical canal involvement as an independent risk factor for persistent HR-HPV infection at the 3-month follow-up after ALA-PDT treatment. During the treatment of the 40 patients with ALA-PDT, there were no reports of severe adverse reactions. Only a limited number of patients experienced slight discomfort symptoms.
Conclusion: ALA-PDT is safe and effective noninvasive therapy for patients with cervical HSIL and HR-HPV infections. It is particularly suitable for young women, who have been confirmed with cervical HSIL and have demand for fertility protection. Three months after ALA-PDT treatment, if a patient still has either ASC-US cervical cytological result and/or HR-HPV infection, rigorous observation is considered safe for her. Cervical canal involvement is an independent risk factor for persistent HR-HPV infection at the 3-month follow-up after ALA-PDT treatment.
1 Introduction
Cervical cancer is a highly prevalent and severe life-threatening malignancy among women worldwide. More than 85% of cervical cancer cases take place in developing countries (1). Notably, in China alone, there were approximately 150,700 new cases and 55,700 deaths in 2022 (2). Hence, cervical cancer is a major public health problem affecting women in China. Histologically confirmed cervical HSIL, a precursor to cervical cancer, occurs as a result of persistent HR-HPV infection, has a risk of 20-30% to progress into invasive carcinoma within 10 years (3). Conventionally, managements for cervical HSIL including cold knife conization, laser conization, laser ablation and loop electrosurgical excision procedure (LEEP) (4), which can lead to cervical distortion, excessive destruction of tissue, and subsequent obstetric complications such as preterm labor, premature rupture of amniotic membranes, chorioamnionitis, low birth weight, and increased morbidity in the newborns (5–7). In China, with the gradual liberalization of fertility policies and the younger onset age of the female lower genital tract diseases, there is an increasing demand to protect normal cervical structure and preserve fertility. Therefore, there is a desirable need to explore effective conservative treatments with minimal damage and fewer adverse reactions for managing cervical HSIL.
Photodynamic therapy (PDT) is an emerging alternative technique for the treatment of squamous intraepithelial lesions. It works through the interaction of photosensitizing agents, light and oxygen, providing a non-invasive, effective and targeted treatment (8). 5-aminolevulinic acid (5-ALA), as a second-generation photosensitizer, can accumulate in higher concentrations in pathological cells and absorb light of the appropriate wavelength. This initiates the photodynamic reactions and selective destruction of inappropriate tissues (8, 9). In recent years, several studies have reported the satisfactory efficacy and safety of PDT in treating cervical LSIL (10–13). Chinese experts in gynecology and obstetrics unanimously recognized the importance of 5-aminolevulinic acid-based photodynamic therapy and reached a consensus on its clinical application in female lower genital tract diseases in 2022 (14). However, there are insufficient studies evaluating the efficacy of ALA-PDT for patients with cervical HSIL.
Our center, being one of the early adopters of ALA-PDT for treating female lower genital tract disorders, implemented this program in 2019. In this retrospective observational survey, we aimed to investigate the effectiveness and safety of ALA-PDT as a potential option for patients with cervical HSIL, as well as identify factors that impact its efficacy.
2 Materials and methods
2.1 Patients
The ALA-PDT treatment for female lower genital tract diseases was approved by the Ethics Committee at Hangzhou First people’s Hospital (Reference Number: 2021-010-01). A total of 40 patients with pathologically confirmed cervical HSIL who had undergone ALA-PDT at Hangzhou First people’s Hospital from Jan 2019 to Dec 2022 were enrolled in this study. Biopsies were taken under colposcopy guidance from the acetowhite and iodine unstained areas to obtain pathological tissues. All participants should have a strong desire to preserve the integrity and function of the cervix and voluntarily agreed to undergo ALA-PDT treatment with good compliance. Most of the patients selected had a pathologic diagnosis of CIN II. In our institution, we generally recommended surgical treatment for CIN III, unless the patient was fully informed and insisted on PDT. Histological results were assessed according to the 2014 World Health Organization Classification of female genital tumors (15): (1) normal, (2) low-grade squamous intraepithelial lesion, (3) high-grade squamous intraepithelial lesion (CIN II or CIN III), and (4) squamous cell carcinoma. All the enrolled patients had satisfactory colposcopy examination and their cervical transformation zones were required of entire visibility. Patients with type 3 transformation zones were not recommended for inclusion in the study. During the treatment and 3-month follow-up period, patients were required to abstain from intercourse. Informed consents were obtained from all participants before treatment. Patients with suspected invasive cancers or other kinds of lower tract disorders were excluded. Women in pregnancy and lactation should not be included in this study.
2.2 Cytological tests
Cytology tests were performed using a fully automated liquid-based cytology assay technology method (BD SurePath™) to evaluate abnormal cells. The cervical cytology results were then reported according to the Bethesda System 2014 (16).
2.3 HPV genotyping
HPV genotyping was performed using the PCR reverse dot hybridization method kit (Yaneng BIO science Co., Ltd., Shenzhen, China. REG. NO: CFDA 20233400811), to identify HPV infection with 17 high-risk types (HPV 16, 18, 31, 33, 35, 39, 45, 51, 52, 53, 56, 58, 59, 66, 68, 73, 82) and 6 low-risk types (HPV 6、11、42、43、81、83) (17).
2.4 5-ALA PDT procedure
All patients were placed in the lithotomy position, and then their vagina and cervix were cleaned by sterile 0.9% sodium chloride before treatment. Lesions of the cervix and cervical canal were completely covered with a sterile and thin cotton soaked in freshly prepared 20% 5-ALA solution (Fudan-Zhang Jiang Bio-Pharmaceutical Co., Ltd., Shanghai, China) for 3 hours. After cervical topical application of 5-ALA, a condom filled with medical gauze was inserted into the vagina to fix the cotton. Patients were then free to move during the waiting time.
Subsequently, a red light with an energy density of 80 mw/cm2 at a wavelength of 635 nm was applied to the cervical surface using an intravaginal light scattering cylindrical head (LED- IBS; Wuhan Yage Photo-Electronic Co., Ltd., Wuhan, China) (Figure 1A). Simultaneously, another red light was applied to the cervical canal using an optical fiber (LD600-C; Wuhan Yage Photo-Electronic Co., Ltd., Wuhan, China) (Figure 1B) for a duration of 30 minutes. The ALA-PDT procedure was scheduled 6 times for cervical HSIL patients. Interval between each time was one week, but postponed for one week during menstruation.
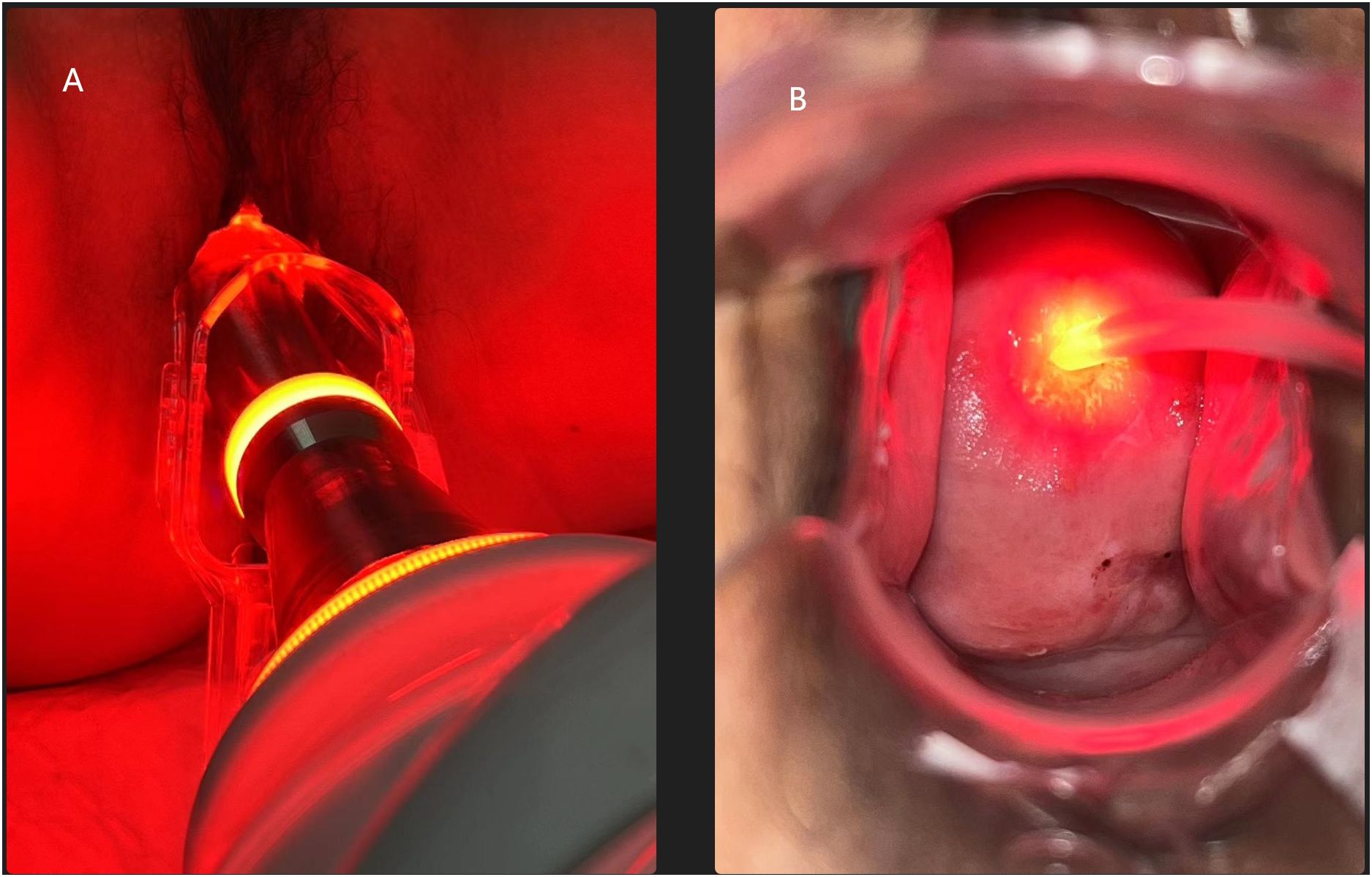
Figure 1 (A) An intravaginal light scattering cylindrical head applies to the cervical surface. (B) An optical fiber applies to the cervical canal.
2.5 Follow up and clinical assessment
The treatment efficacy was evaluated by HPV genotyping and cervical cytology test at the 3-month follow-up post-treatment. If the HR-HPV turned negative and cytological result was normal, the treatment efficacy can be defined as complete remission (CR). If the cervical cytological result was worse than ASC -US, the patient should undergo colposcopy-directed biopsy immediately to evaluate the degree of cervical lesions, regardless of HR-HPV status. For other abnormalities, patients were advised to repeat HPV and cytology tests after 3 months, and if the abnormal results persisted or even progressed, timely colposcopy-guided biopsy is necessary to assess cervical lesions. ALA-PDT related symptoms and adverse events were also recorded.
2.6 Statistical analysis
The R software (Version 4.1.3) was used for data analysis. Chi-square and Fisher’s exact tests were performed to compare HPV clearance rates at 3-month follow-up after ALA-PDT for cervical HSIL among different groups based on various factors. Multiple Linear Regression was used to mitigate the impact of different variables. P value less than 0.05 was considered statistically significant.
3 Results
3.1 Clinical characteristics of the patients before treatment
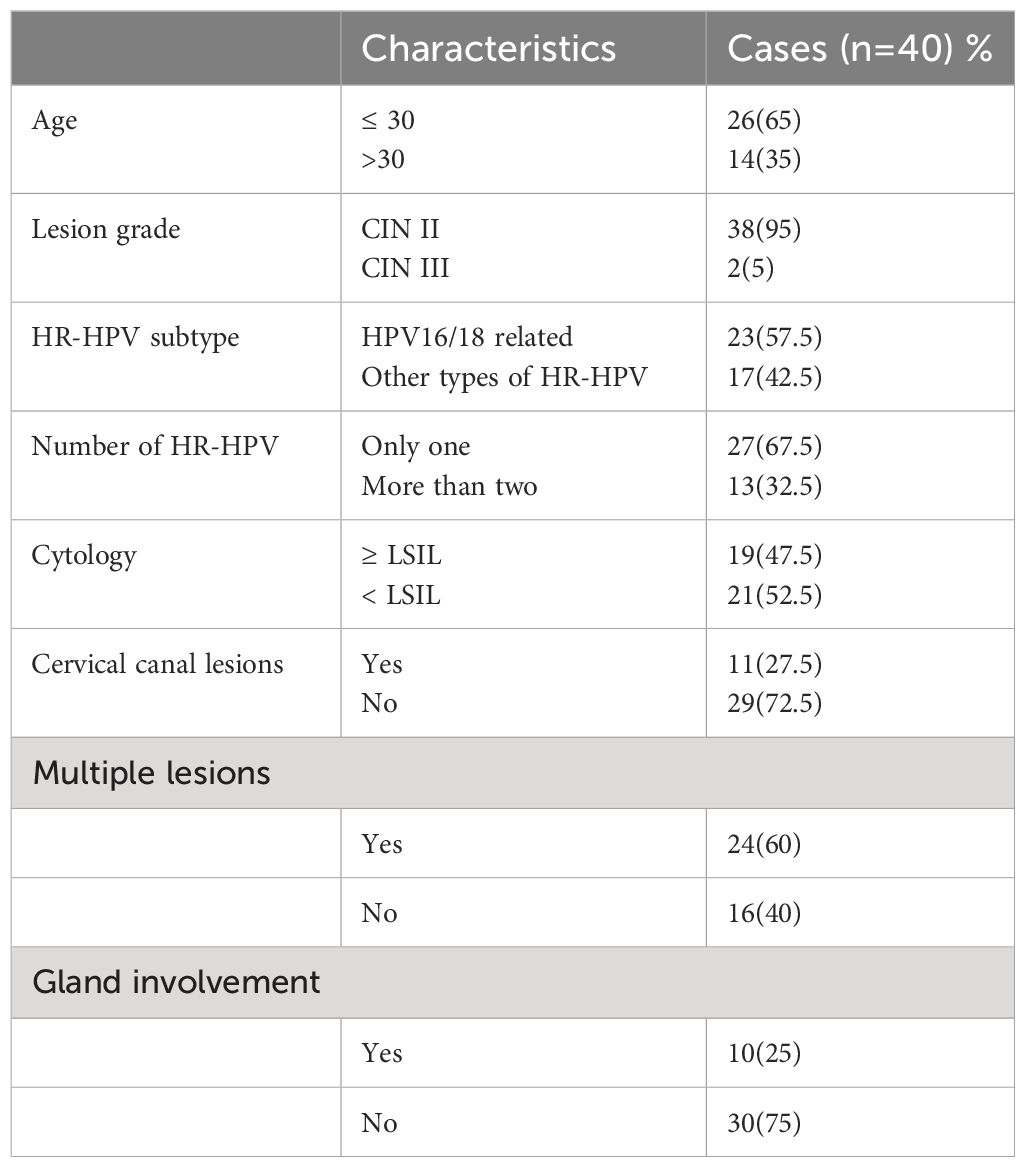
A total of 40 patients with a pathological biopsy result of cervical HSIL were treated with ALA-PDT. Among them, 38 (38/40, 95%) had CIN II, and 2 (2/40, 5%) had CIN III. The average age of the patients was 28.25 years old (20 - 41 years old), and all of them wanted to preserve their cervical structure. Notably, among these patients, 26 were ≤ 30 years old, while 14 were older than 30 years. All patients were infected with HR-HPV before treatment. Among them, 23 patients were infected with subtype HR-HPV 16/18 and 17 patients were infected with other types. 27 patients had only one type of HR- HPV infection, while 13 patients had more than 2 types of HR-HPV infections. Before ALA-PDT, 19 patients had cytology evaluation ≥ LSIL, whereas 21 patients exhibited cytology evaluation < LSIL. 11 patients exhibited cervical canal lesions, while the remaining 29 patients had no cervical canal lesions. 24 patients had multiple sites lesions and the other 16 patients had only a single site lesion. The lesion involved the cervical glands in 10 patients. The detailed clinical characteristics of these patients are presented in Table 1.
3.2 The effect of photodynamic therapy in HSIL at follow-up
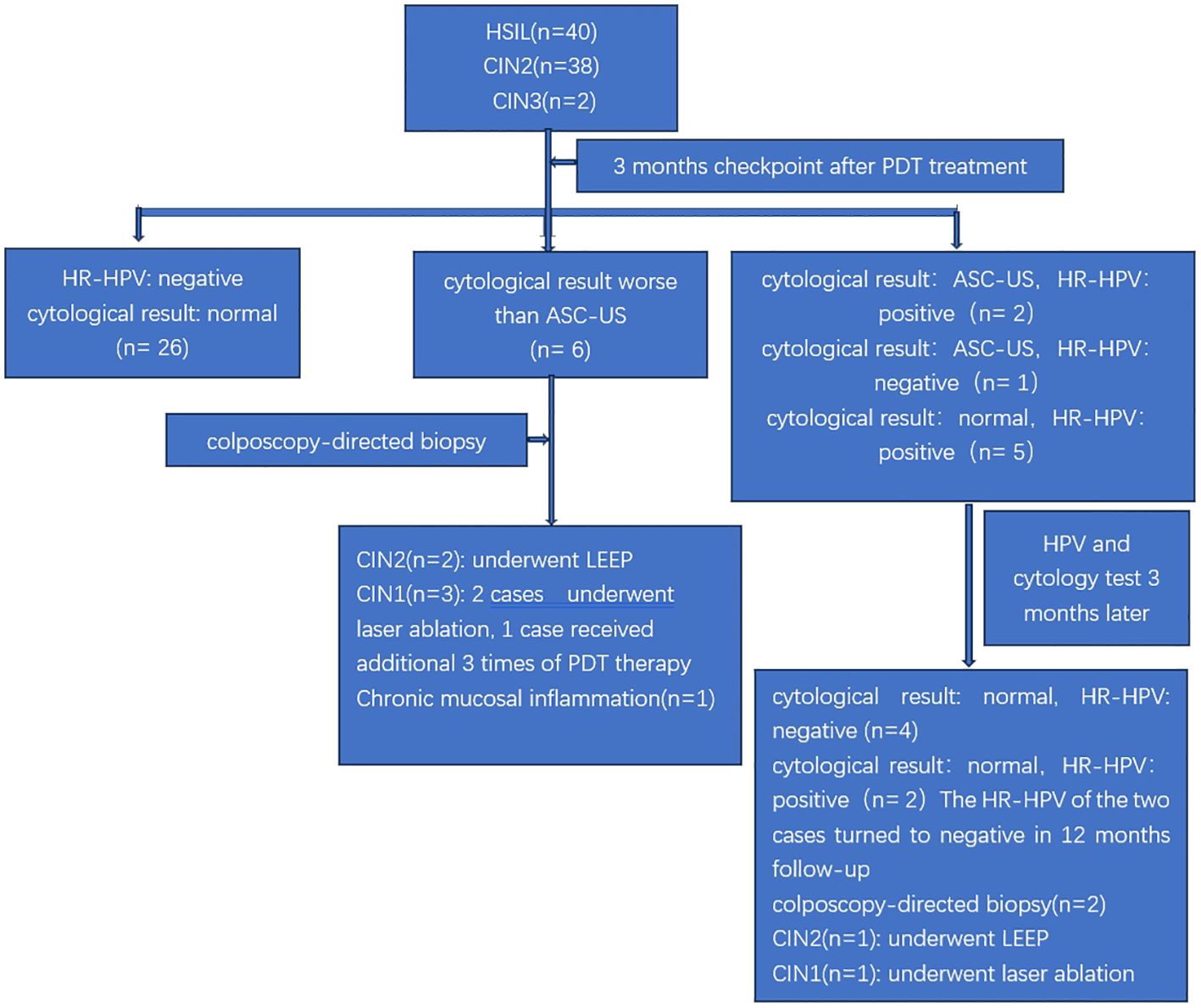
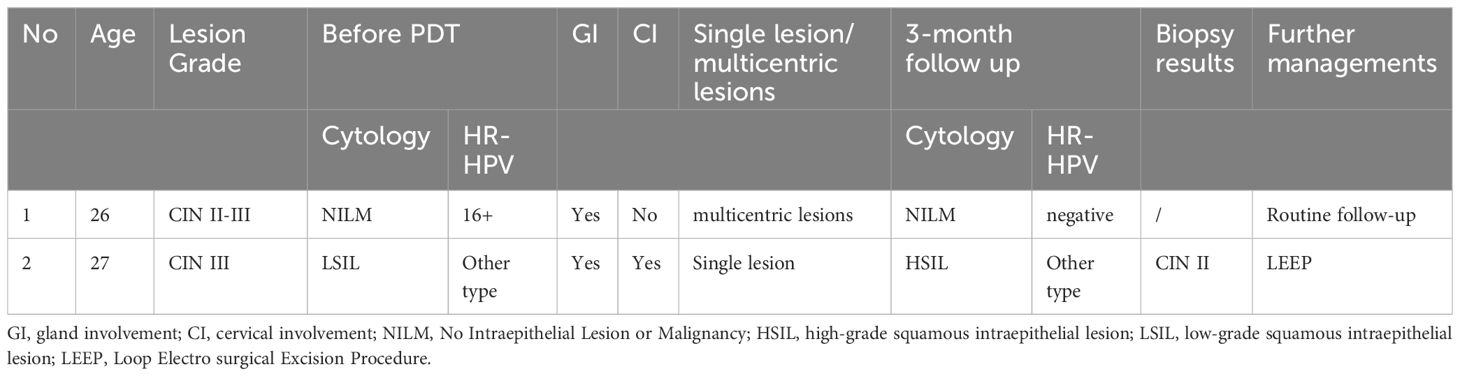
The follow-up flowchart of the studied population is illustrated in Figure 2. All of the patients were evaluated for cervical cytological result and HR-HPV at the 3-month follow-up. Both cervical cytology and HR-HPV returned to normal in 26 out of the 40 cases. Therefore, the CR rate of ALA-PDT in cervical HSIL patients at our center was 65% (26/40) assessed at the 3-month follow-up. Six patients with cervical cytologic findings greater than ASC-US at the 3-month follow-up were directly referred for colposcopy-guided biopsy. The biopsy results indicated two cases of CIN II, which underwent LEEP; three cases of CIN I, of which two were treated with laser ablation and one received an additional course of PDT; and one case was confirmed to have chronic inflammation of the cervical mucosa. Additional details about these six patients were provided in Table 2. The remaining 8 patients had cervical cytology result of ASC-US and/or positive HR-HPV at the 3-month follow-up. In this group of patients, further evaluation was performed at 6 months after ALA-PDT to determine whether they should be referred for colposcopy-guided biopsy or kept under observation. Out of the eight patients, four had normal cervical cytology as well as negative HR-HPV at the 6-month assessment. Two patients had their cervical cytological and HR-HPV results normalized at the 12-month evaluation after ALA-PDT. Two patients underwent biopsy according to the 6-month evaluation, 1 was diagnosed with CIN II and underwent LEEP, while the other was diagnosed with CIN I and underwent laser ablation. The details on these 8 patients were provided in Table 3. Among the 38 patients with CIN II, 25 achieved CR after 3 months of treatment, with cervical cytology and HR-HPV completely turning negative. In addition, there were 6 CIN II patients who although did not achieve CR after 3 months of treatment, but 4 of them, and 2 of them, respectively, achieved CR at 6-month and 12-month follow-up. 81.6% (31/38)of CIN II patients achieved CR within one year of ALA-PDT in our study. Our study included two CIN III patients who strongly insisted ALA-PDT treatment. Their clinical and prognostic data are detailed in Table 4. One of the patients showed negative results in cervical cytology and HR-HPV infection after 3 months of treatment, achieving CR. Another patient was with cervical cytology indicating HSIL and HR-HPV persistent infection at the 3-month follow up. Further colposcopy biopsy revealed CIN II. The patient undergone LEEP surgery ultimately.
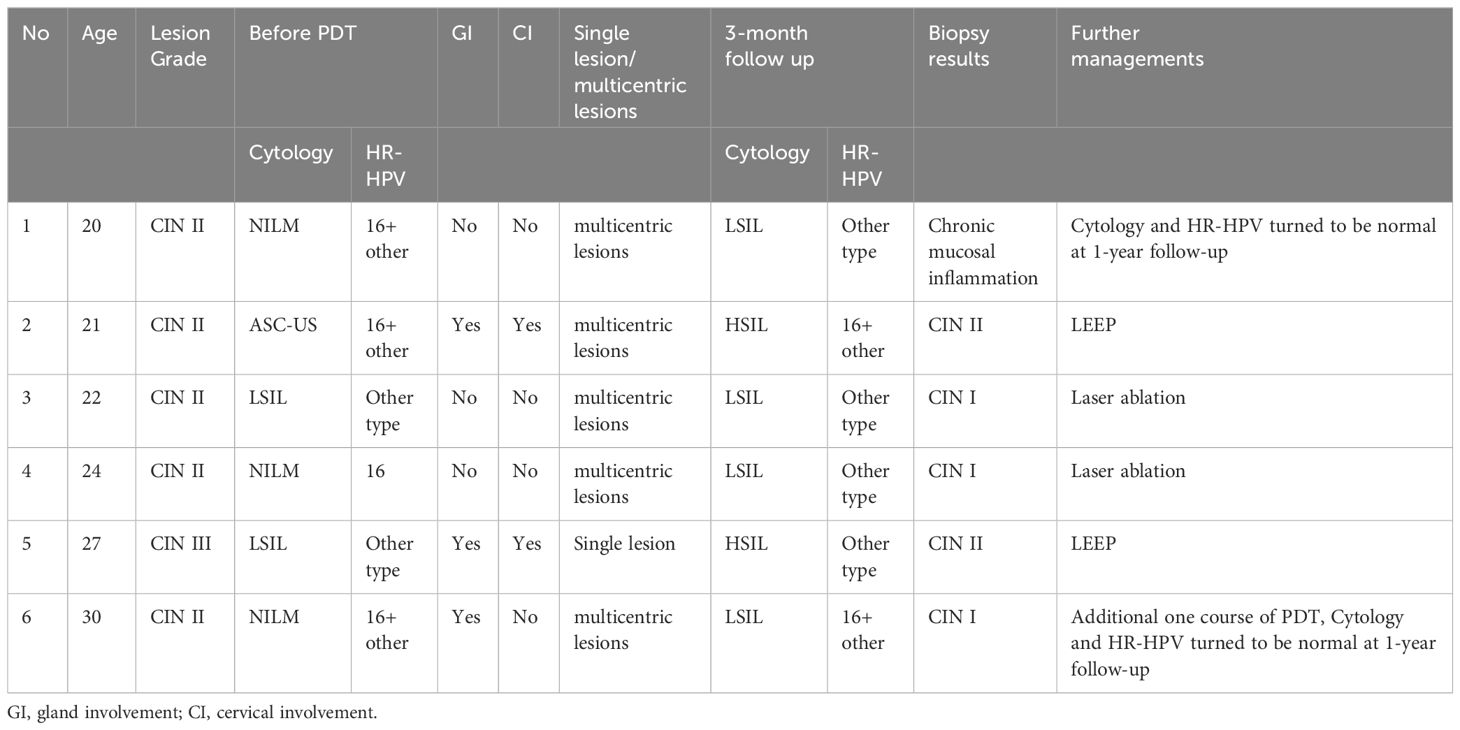
Table 2 Characteristics of the 6 patients with cytological result worse than ASC -US at 3-month follow up.

Table 3 Characteristics of the 8 patients with either cytological result ASC -US and/or HR-HPV positive at 3-month follow up.
In summary, none of the patients showed disease progression during the observation period after ALA-PDT. At the 3-month follow-up, 4 patients received other surgical methods because of incomplete remission of the disease on biopsy, and another 2 patients underwent surgical treatments at the 6-month follow-up for the same reason. Actually, among these six patients who underwent surgical treatment, four experienced partial lesion regression after ALA-PDT, while only two remained lesions that were consistent with pre-treatment. None of them experienced disease progression. The CR rate of ALA-PDT in cervical HSIL patients at our center was 65% (26/40) at the 3-month follow-up and reached 82.5% (33/40) at the 12-month follow-up.
3.3 Representative cases
Case A was a 20-year-old lady, G0P0, who had a history of abnormal vaginal bleeding after intercourse for 2 years. Her cervical cancer screening showed HPV 16,51 infection and normal cervical cytology result. The biopsy results of colposcopy indicated CIN II. Cervical cancer screening was repeated 3 months after the completion of 6 times of ALA-PDT, and the cervical cytological result showed LSIL and HPV 16 infection. The patient then received a repeated colposcopy-guided biopsy, which revealed chronic mucosal inflammation. Further observation found that her cytology and HR-HPV returned to normal at the 1-year follow-up. The colposcopy images before ALA-PDT and 3 months after ALA-PDT of this case are provided in Figure 3.
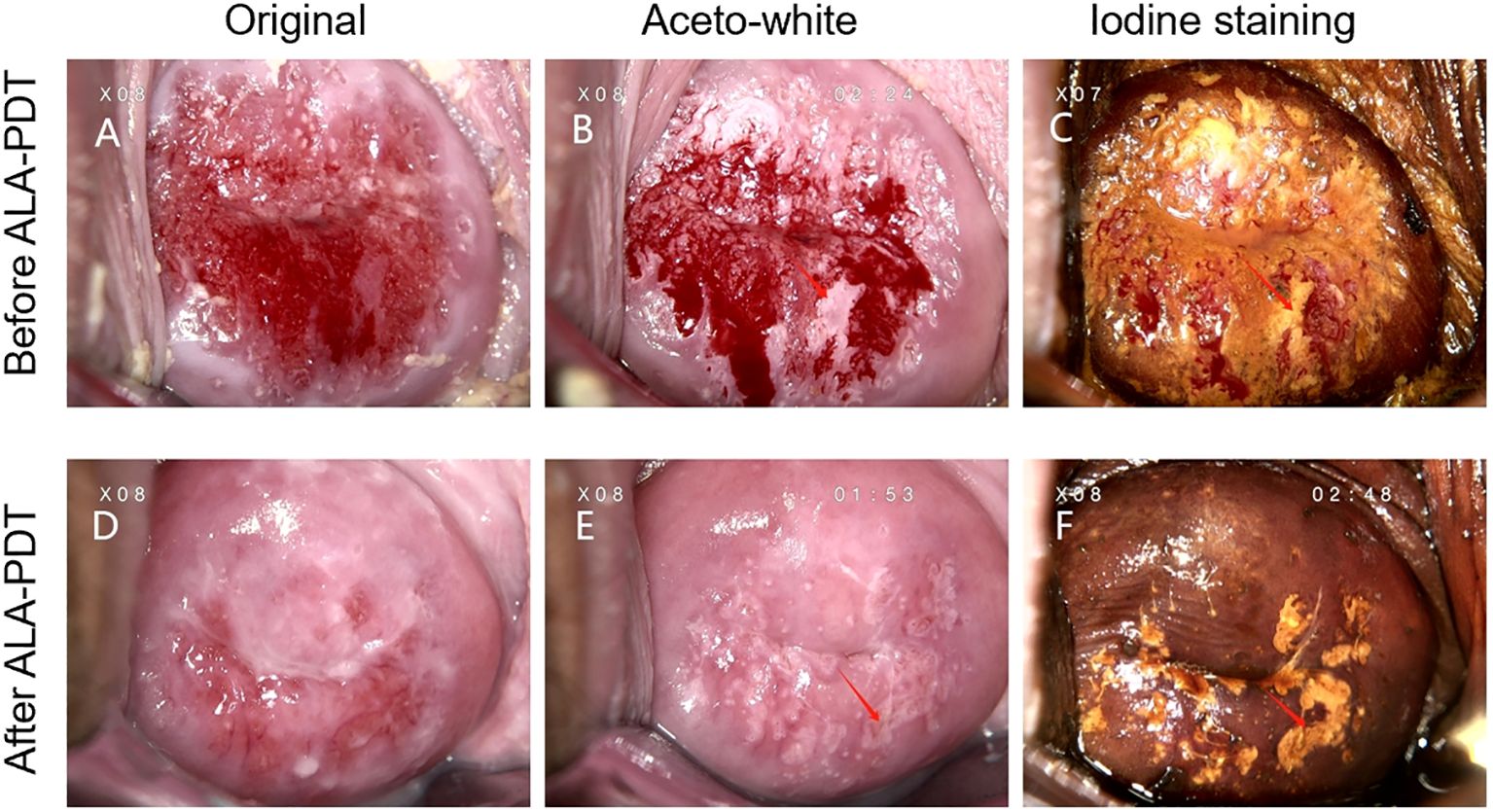
Figure 3 (A–C) Colposcopy images from case A who was diagnosed with CIN II before ALA-PDT. (D–F) Colposcopy images from case A who was diagnosed with cervical chronic mucosal inflammation 3 months after ALA-PDT treatment. The left column shows the initial performance of the cervical surface. The middle column depicts the aceto-white dysplastic lesion areas after the application of 3% acetic acid. The right column shows atypical epithelium after the use of iodine solution in the same patient. Arrows point to the appearances of the cervical high-grade squamous intraepithelial lesion before and after ALA-PDT.
Case B was a 24-year-old woman, G0P0, who was asymptomatic but tested positive for HPV 16,18,59,68 infection during a cervical screening. Her cervical cytological result was normal. The colposcopy biopsy results suggested CIN II with glandular involvement. The patient underwent six times of ALA-PDT treatment, and a repeated cervical screening 3 months later showed the disappearance of HR-HPV and normal cervical cytology. Meanwhile, colposcopy images before and 3 months after ALA-PDT of this case were provided in Figure 4.
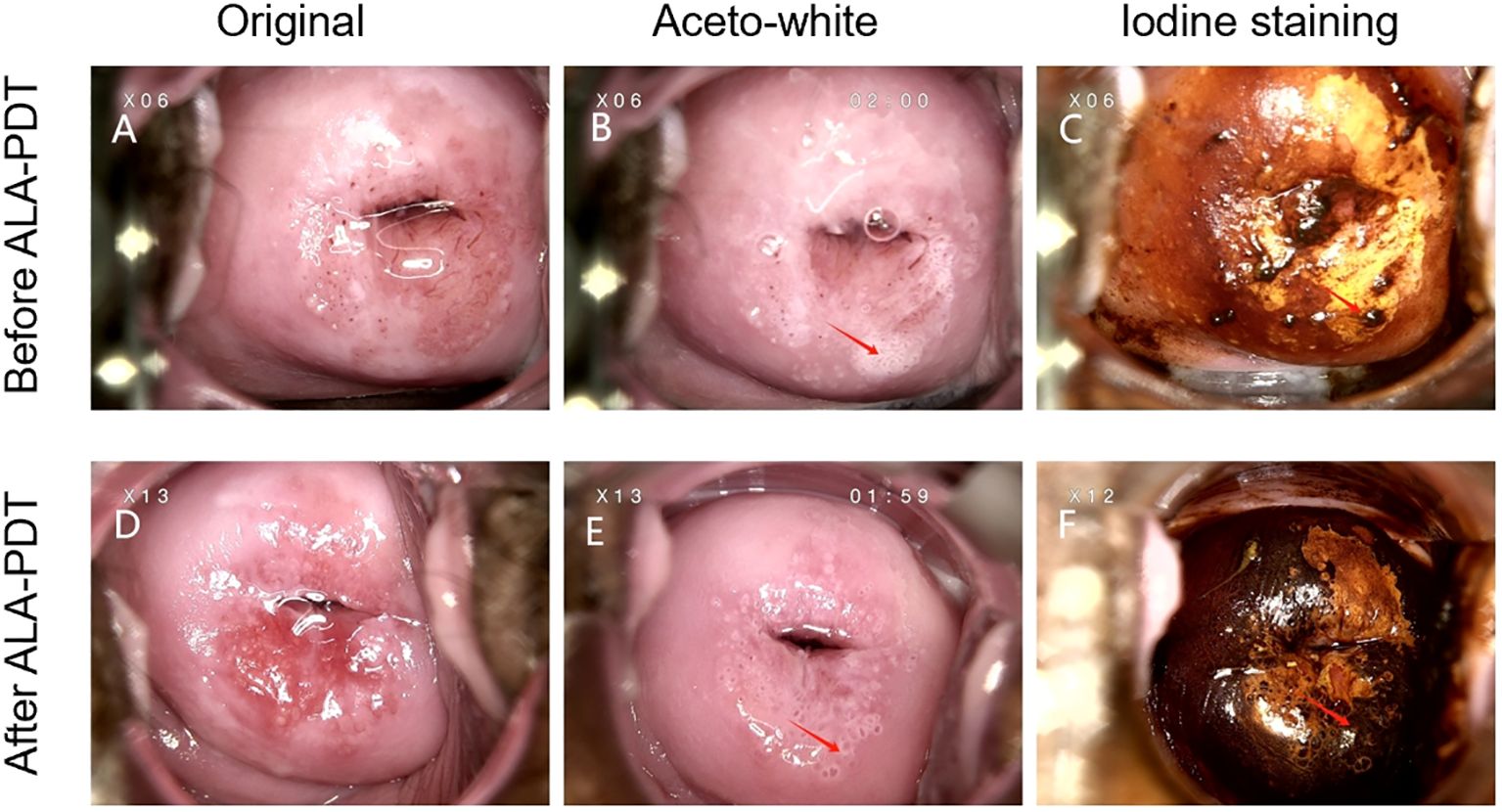
Figure 4 (A–C). Colposcopy images from case B who was diagnosed with CIN II before ALA-PDT. (D–F) Colposcopy images from case B whose cervical cytology and HR-HPV turned to be normal 3 months after ALA-PDT treatment. The left column shows the initial performance of the cervical surface. The middle column depicts the aceto-white dysplastic lesion areas after the application of 3% acetic acid. The right column shows atypical epithelium after the use of iodine solution in the same patient. Arrows point to the appearances of the cervical high-grade squamous intraepithelial lesion before and after ALA-PDT.
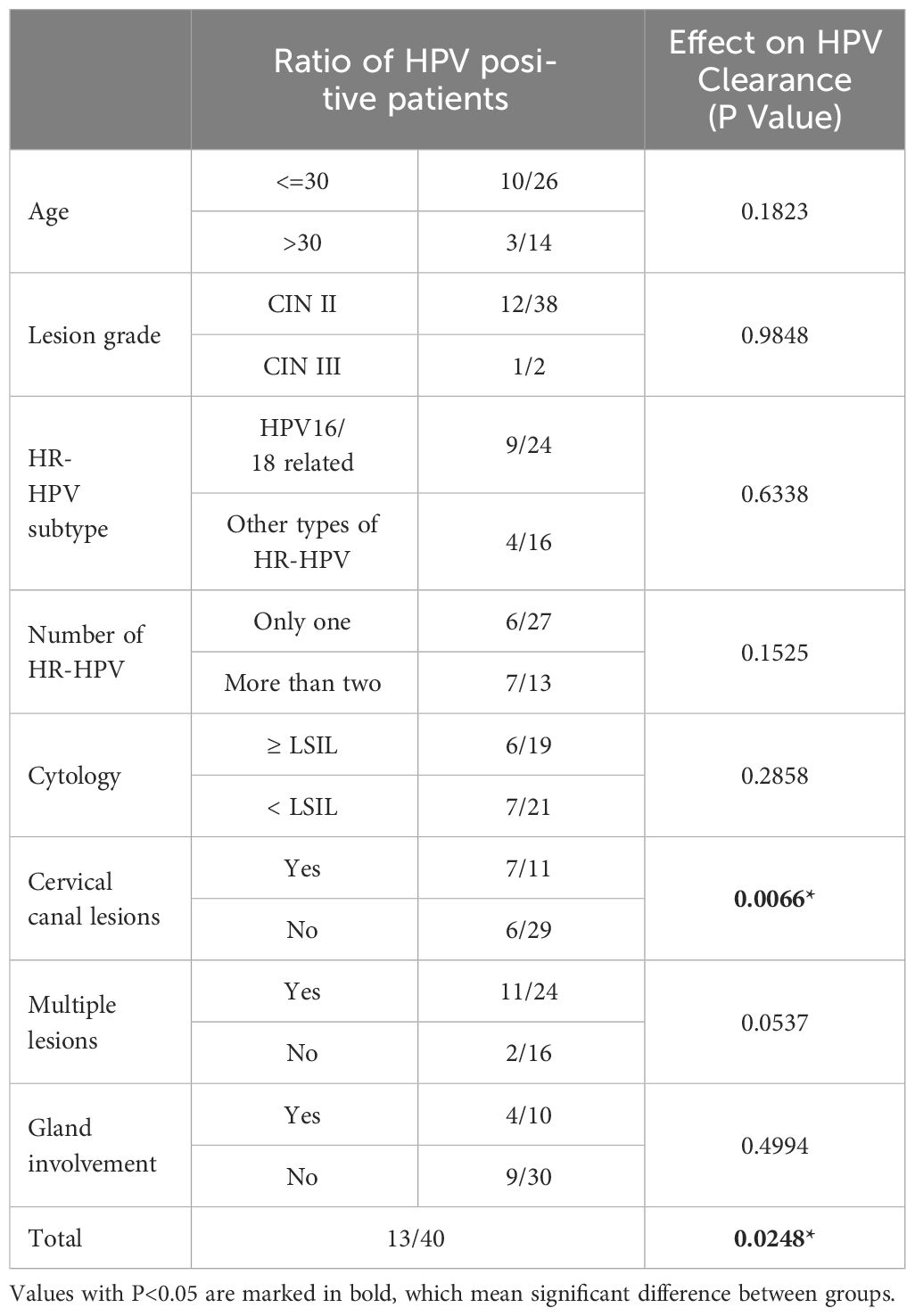
3.4 Factors affecting the rate of HPV clearance 3 months after PDT
We found that the persistent HR-HPV infection risk was 32.5% (13/40) in the 3-month follow-up. To evaluate the factors influencing the rate of HPV clearance 3 months after ALA-PDT, we conduct both univariate and multivariate analyses on age, lesion grade, HPV subtypes, number of HPV types, cervical cytological results before treatment, cervical involvement, glandular involvement, as well as the number of lesions. Univariate analyses results showed that the HPV clearance rate was significantly lower in patients with cervical canal involvement (36.36% vs 79.31%, p<0.05), multiple lesions (54.17% vs 87.5%, p<0.05) and infection with more than one species of HPV (46.15% vs 77.78%, p<0.05) when compared to those without cervical canal or glandular involvement. The analysis revealed that factors such as age, lesion grade, HPV subtype, cytology results before treatment, and number of lesions before ALA-PDT have no impact on the HPV clearance rate (Figure 5). However, after multivariate regression analyses, we found that cervical canal involvement was the only independent risk factors affecting the clearance rate of HPV 3 months after completion of PDT (Table 5).
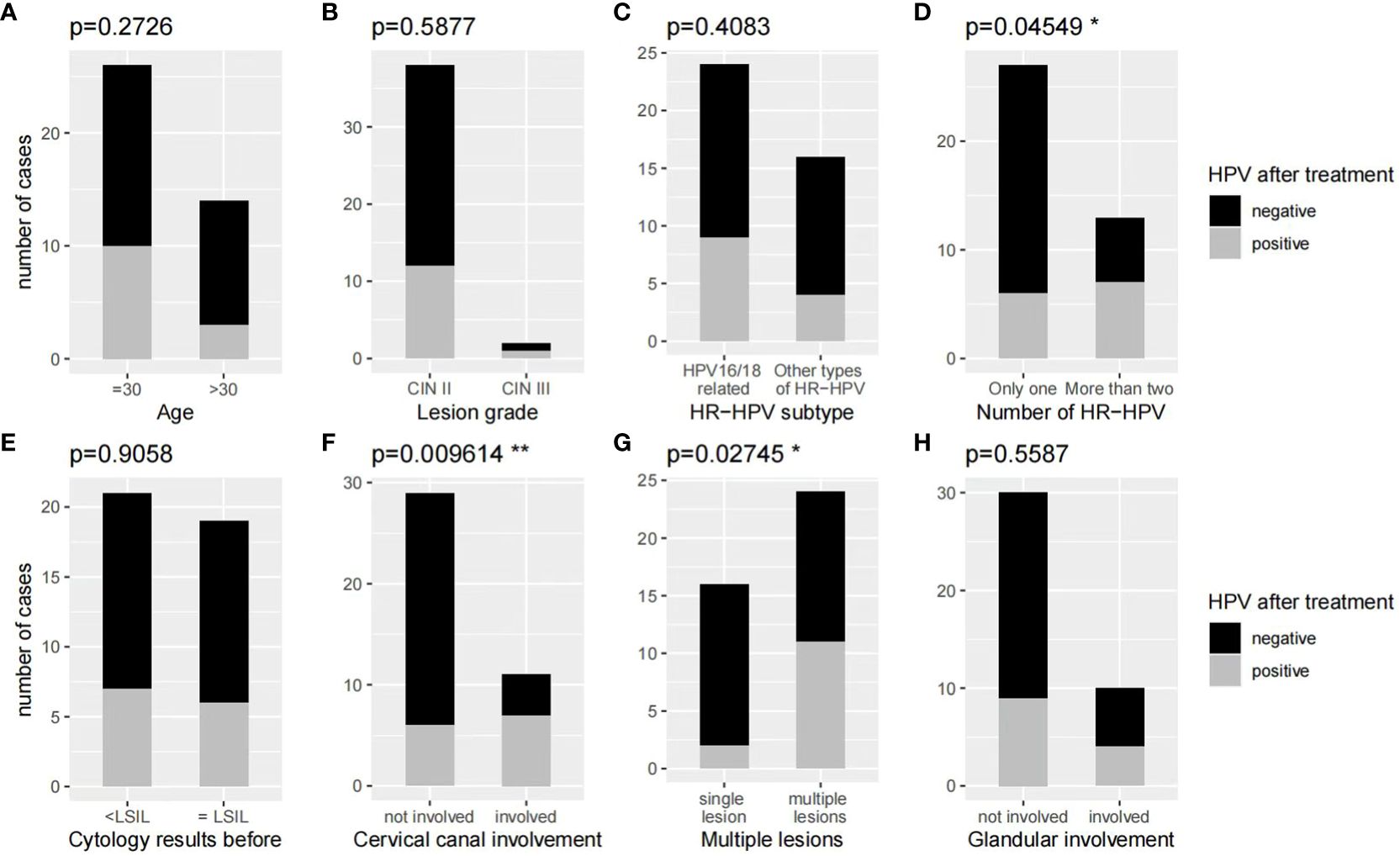
Figure 5 (A, B, C, E, H) Univariate analyses results showed that age, lesion grade, HR-HPV subtype, cytology, and cervical gland involvement before treatment of ALA-PDT have no effect on the HR-HPV clearance rate at the 3-month follow-up. (D, F, G) Univariate analyses results showed that cervical canal involvement, cervical multiple sites lesions, and more than one type of HR-HPV infection are risk factors for persistent HR-HPV infection at the 3-month follow-up.
3.5 Incidence of side effects
No patients experienced severe side effects on vital signs such as blood pressure, heart rate and breath. Most patients were observed mild local adverse effects during of a few days after ALA-PDT. These effects included increased vaginal discharge, slight abnormal pain, slight vaginal bleeding and burning sensations. Fortunately, these side effects were bearable and relieved within one-week post-treatment. Notably, some patients were observed to have mental disorders such as anxiety or insomnia during the follow-up period. This may be attributed to the fear of the disease and concerns about the efficacy of the treatment.
4 Discussion
Currently, cervical cancer is the fourth most common malignancy in women worldwide, and it is still a major cause of cancer-related death in some of the world’s poorest countries (18). In 2018, the World Health Organization issued a global call for the elimination of cervical cancer as a public health problem (19). The strategies for eliminating cervical cancer included primary prevention via HPV vaccination, secondary prevention via cervical screening, and the third prevention of timely management of precancerous lesions. HSIL of the cervix, which is induced by HR-HPV, is a premalignant disease. In the past, surgical excision using methods like cold knife conization, laser conization/ablation, or LEEP was the gold standard treatment for cervical HSIL (4). Because of young women’s low-acceptance of surgical procedures and the associated complications, as well as their strong desire for complete preservation of cervical tissues, it is imperative to explore a non-invasive and effective method for the management of cervical HSIL. ALA-PDT seems to be a good choice for this specific group of patients.
ALA-PDT involves the selective accumulation of 5-aminolevulinic acid in the CIN tissues (20), which are then illuminated to generate ROS that destroy tumor cells by inducing apoptosis and necrosis. The success of the process relies on three key points: oxygen-induced activation of photosensitizer, appropriate utilization of visible light, and proper selection of the photosensitizer (21). This process is highly tissue selective, non -invasive, and carries a low risk of severe complications, making it an ideal method for treating cervical HSIL, especially for young women. Compared to traditional surgical excisions, ALA-PDT is characterized by elimination of precancerous lesions and potential HPV infection (22) without causing damage to the normal anatomy.
Our study showed that ALA-PDT was highly effective in treating a cervical HSIL, leading to a complete remission rate of 65% at 3 months after completion of ALA-PDT. Furthermore, with an extended observation period, the complete remission rate could reach as high as 82.5% at 12 months after the completion of ALA-PDT. These findings are consistent with previous studies. Wu et al. reported a histological complete remission rate of 77.78% for CIN II after PDT at 12-month follow-up (23). Tang et al. revealed that the cervical HSIL complete remission rate after PDT was 88.9%, 92.5% at 6-months,12-months follow-up respectively (24). Qu et al. found that the total lesion regression rate of cervical HSIL after PDT was 89.58% at 3-months follow-up (25). Hu et al. reported that the disappearance rate of cervical HSIL after PDT was 81.82%, 90.91% at 3-month,6-month follow-up respectively (26). Although the above studies reported a satisfactory efficacy of PDT for HSIL treatment, there are still some limitations. The application of ALA-PDT in cervical HSIL is still in the initial exploration stage, and the included cases in the above studies were limited, which might limit the generalizability and robustness of the conclusions. Further studies with high-level of evidence, such as multicenter, large-sample, randomized controlled clinical trials, are necessary to be conducted to validate our findings. Additionally, it should be noted that our study primarily focused on patients with CIN II, only 2 patients with CIN III were included. One patient was diagnosed with CIN II-III and responded positively to ALA-PDT treatment, showing normal cervical cytological and HPV test results after three months. Conversely, the second patient, diagnosed with CIN III, did not benefit from this therapy and instead achieved recovery through LEEP. This discrepancy in treatment efficacy may be attributed to the greater lesion depth associated with CIN III, which renders non-invasive treatments such as ALA-PDT less effective than they are for CIN I and CIN II cases. Due to the lack of sufficient data, we cannot make some rigorous suggestions for CIN III patients. Further research including larger subjects is needed to demonstrate the effectiveness of PDT for patients with CIN III.
There is no consensus on the follow-up strategy after PDT. In our study, we evaluate the combination of HPV genotyping and cervical cytological results as an initial evaluation at the 3-month follow-up. Cases were then triaged according to the results. The stratification protocol in our study was to immediately refer to colposcopy-guided biopsy if the cytologic result was worse than ASC-US at the 3-month follow-up. If the cervical cytological result was ASC-US and/or there was HR-HPV infection, observation could continue with repeated cervical screening at 6-months follow-up. We designed this stratification protocol based on previous studies reporting that PDT could enhance local and systemic immunity, which plays a crucial role in clearing lesions (27–29). Therefore, we have implemented a relatively conservative observation protocol for patients with either cytology result ASC-US or HR -HPV infection 3 months after PDT treatment. We hypothesized that the activated immune response by PDT would have a long-term effect on the clearance of lesions or HR-HPV, thus ensuring the safety of this group of patients. In our study, 8 cases that met this criterion(either cytologic result ASC-US and/or HR-HPV infection). Among them, 6 patients returned to normal cytology and negative HPV within 1 year by observation, one patient regressed from CIN II to CINI, and one patient persisted in CIN II. None of the patients had a history of disease progression during the course of observation. Therefore, we consider our triage program to be reasonable.
In our study of single factor analysis, we found that cervical canal involvement, multiple lesions and infection with more than one species of HR-HPV can cause persistent viral infection at the 3-month follow-up after ALA-PDT treatment. However, multiple linear regression analysis revealed that only cervical canal involvement was an independent risk factor. These findings suggest that the effects of multiple lesions and HR-HPV species are secondary to the difference in cervical canal involvement. Consequently, even if a patient has numerous lesions and HR-HPV infection, if there is no disease in the cervical canal, ALA-PDT can effectively eliminate her HR-HPV infection. We infer that the reason maybe the optical fiber is not as efficient as the intravaginal light scattering cylindrical head. Thus, we recommend to prolong the time of irradiation by the optical fiber for patients with cervical canal lesions. The underlying association between cervical involvement and persistent HR-HPV infection requires further research. It is important to monitor women with persistence of HR-HPV infection who have underwent PDT therapy as it greatly impacts the prognosis. Our findings emphasize the need to pay extra attention to the patients with cervical involvement.
During the treatment of the 40 patients with ALA-PDT, there were no severe adverse reactions. A few patients presented with discomfort symptoms, such as burning sensations, slight pain, slight discomforts in the lower abdomen and increased vaginal discharge. These adverse reactions were bearable and were relieved within a few days after treatment, indicating the safety of ALA-PDT.
During our research, patients underwent a treatment regimen of ALA- PDT with a frequency of once per week, typically completing six sessions. The entire course of treatment spanned approximately 7 weeks to 2 months, which is notably longer than the single-session requirement of other non-invasive therapies such as laser, cryotherapy, and thermal ablation. Despite the extended duration, ALA-PDT offers the advantage of being less painful in comparison to these alternatives. Moreover, the satisfactory outcomes observed in this study can be partly attributed to the regularity of the ALA-PDT treatment sessions.
Non-invasive physical plasma (NIPP), which inhibit pathological cell growth through rapid and transient DNA damage, is another emerging approach for cervical precancerous lesions. Like ALA-PDT, NIPP is a tissue-preserving and easy-to-apply method, which can be performed in outpatient settings without the need for local or general anesthesia and is more cost-effective than ALA-PDT. Previous studies have reported that the complete remission rate of NIPP to CINI/II reached 86.2% -95% at 3-6 months after treatment (30, 31). However, these studies were single arm prospective studies and included a small sample size. Further studies are expected to include larger population and reveal the efficacy of NIPP in CINII/III patients. NIPP may be an underlying alternative to ALA-PDT for the treatment of cervical HSIL.
5 Conclusion
1. ALA-PDT is a highly effective, non-invasive, and safe therapeutic intervention for cervical HSIL. Compare to surgical procedures, it has the advantage of preserving the structural and functional integrity of the cervix. Therefore, it is an optimal choice for young women with cervical HSIL who have fertility requirements. 2. We suggest continuous observation instead of performing a colposcopy-guided biopsy in patients who have either a cervical cytological result of ASU-US and/or a HR-HPV infection at 3-month follow-up after ALA-PDT therapy. 3. Cervical canal involvement is an independent risk factor for persistent HR-HPV infection at the 3-month follow-up after PDT treatment.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by Ethics Committee of Hangzhou First people’s Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
JQ: Writing – review & editing, Writing – original draft, Formal analysis, Data curation, Conceptualization. YW: Writing – review & editing, Supervision, Investigation. GW: Writing – review & editing, Resources, Data curation. JL: Writing – review & editing, Resources. LS: Writing – review & editing, Supervision, Conceptualization. SX: Writing – review & editing, Software, Methodology, Formal analysis, Conceptualization.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Construction Fund of Key Medical Disciplines of Hangzhou.
Acknowledgments
We thank the patients who participated in this study and their families.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. (2018) 68:394–424. doi: 10.3322/caac.21492
2. Bingfeng H, Rongshou Z, Hongmei Z, Shaoming W, Kexin S, Ru C, et al. Cancer incidence and mortality in China, 2022. J Natl Cancer Center. (2024), S2667005424000061. doi: 10.1016/j.jncc.2024.01.006
3. McCredie MR, Sharples KJ, Paul C, Baranyai J, Medley G, Jones RW, et al. Natural history of cervical neoplasia and risk of invasive cancer in women with cervical intraepithelial neoplasia 3: a retrospective cohort study. Lancet Oncol. (2008) 9:425–34. doi: 10.1016/S1470-2045(08)70103-7
4. Martin-Hirsch PL, Paraskevaidis E, Kitchener H. Surgery for cervical intraepithelial neoplasia. Cochrane Database Syst Rev. (2000) CD001318. doi: 10.1002/14651858
5. Kyrgiou M, Athanasiou A, Paraskevaidi M, Mitra A, Kalliala I, Martin-Hirsch P, et al. ”Adverse obstetric outcomes after local treatment for cervical preinvasive and early invasive disease according to cone depth: systematic review and meta-analysis. BMJ. (2016) 354:i3633. doi: 10.1136/bmj.i3633
6. Jin G, LanLan Z, Li C, Dan Z. Pregnancy outcome following loop electrosurgical excision procedure (LEEP) a systematic review and meta-analysis. Arch Gynecol Obstet. (2014) 289:85–99. doi: 10.1007/s00404-013-2955-0
7. Crane JM. Pregnancy outcome after loop electrosurgical excision procedure: a systematic review. Obstet Gynecol. (2003) 102:1058–627. doi: 10.1016/s0029-7844(03)00741-5
8. Kwiatkowski S, Knap B, Przystupski D, Saczko J, Kędzierska E, Knap-Czop K, et al. Photodynamic therapy - mechanisms, photosensitizers and combinations. BioMed Pharmacother. (2018) 106:1098–107. doi: 10.1016/j.biopha.2018.07.049
9. Luby BM, Walsh CD, Zheng G. Advanced photosensitizer activation strategies for smarter photodynamic therapy beacons. Angew Chem Int Ed Engl. (2019) 58:2558–69. doi: 10.1002/anie.201805246
10. Gu L, Cheng M, Hong Z, Di W, Qiu L. The effect of local photodynamic therapy with 5-aminolevulinic acid for the treatment of cervical low-grade squamous intraepithelial lesions with high-risk HPV infection: A retrospective study. Photodiagnosis Photodyn Ther. (2021) 33:102172. doi: 10.1016/j.pdpdt.2020.102172
11. Niu J, Cheng M, Hong Z, Ling J, Di W, Gu L, et al. The effect of 5-Aminolaevulinic Acid Photodynamic Therapy versus CO2 laser in the Treatment of Cervical Low-grade Squamous Intraepithelial Lesions with High-Risk HPV Infection: A non-randomized, controlled pilot study. Photodiagnosis Photodyn Ther. (2021) 36:102548. doi: 10.1016/j.pdpdt.2021.102548
12. Li D, Zhang F, Shi L, Lin L, Cai Q, Xu Y. Treatment of HPV infection-associated low grade cervical intraepithelial neoplasia with 5-aminolevulinic acid-mediated photodynamic therapy. Photodiagnosis Photodyn Ther. (2020) 32:101974. doi: 10.1016/j.pdpdt.2020.101974
13. Hillemanns P, Garcia F, Petry KU, Dvorak V, Sadovsky O, Iversen OE, et al. A randomized study of hexaminolevulinate photodynamic therapy in patients with cervical intraepithelial neoplasia 1/2. Am J Obstet Gynecol. (2015) 212:465.e1–7. doi: 10.1016/j.ajog.2014.10.1107
14. Qiu L, Li J, Chen F, Wang Y, Wang X, Lv Q, et al. Chinese expert consensus on the clinical applications of aminolevulinic acid-based in female lower genital tract diseases (2022). Photodiagnosis Photodyn Ther. (2022) 39:102993. doi: 10.1016/j.pdpdt.2022.102993
15. Kurman RJ, Carcangiu ML, Herrington CS. World health organisation classification of tumours of the female reproductive organs. 4th Revised ed. International Agency for Research on Cancer (2014).
16. Nayar R, Wilbur DC. The pap test and bethesda 2014. Cancer Cytopathol. (2015) 123:271–81. doi: 10.1002/cncy.21521
17. Muñoz N, Bosch FX, de Sanjosé S, Herrero R, Castellsagué X, Shah KV, et al. Epidemiologic classification of human papillomavirus types associated with cervical cancer. N Engl J Med. (2003) 348:518–27. doi: 10.1056/NEJMoa021641
18. Canfell K. Towards the global elimination of cervical cancer. Papillomavirus Res. (2019) 8:100170. doi: 10.1016/j.pvr.2019.100170
19. Brisson M, Drolet M. Global elimination of cervical cancer as a public health problem. Lancet Oncol. (2019) 20:319–21. doi: 10.1016/S1470-2045(19)30072-5
20. Keefe KA, Chahine EB, DiSaia PJ, Krasieva TB, Lin F, Berns MW, et al. Fluorescence detection of cervical intraepithelial neoplasia for photodynamic therapy with the topical agents 5-aminolevulinic acid and benzoporphyrin-derivative monoacid ring. Am J Obstet Gynecol. (2001) 184:1164–9. doi: 10.1067/mob.2001.113123
21. Zhang W, Zhang A, Sun W, Yue Y, Li H. Efficacy and safety of photodynamic therapy for cervical intraepithelial neoplasia and human papilloma virus infection: A systematic review and meta-analysis of randomized clinical trials. Med (Baltimore). (2018) 97:e10864. doi: 10.1097/MD.0000000000010864
22. Fu Y, Bao Y, Hui Y, Gao X, Yang M, Chang J. Topical photodynamic therapy with 5-aminolevulinic acid for cervical high-risk HPV infection. Photodiagnosis Photodyn Ther. (2016) 13:29–33. doi: 10.1016/j.pdpdt.2015.12.004
23. Wu A, Li Q, Ling J, Gu L, Hong Z, Di W, et al. Effectiveness of photodynamic therapy in women of reproductive age with cervical high-grade squamous intraepithelial lesions (HSIL/CIN2). Photodiagnosis Photodyn Ther. (2021) 36:102517. doi: 10.1016/j.pdpdt.2021.102517
24. Tang Y, Su Y, Xu Y, Zhang Y, Shen Y, Qin L, et al. Therapeutic effects of topical photodynamic therapy with 5-aminolevulinic acid on cervical high-grade squamous intraepithelial lesions. Photodiagnosis Photodyn Ther. (2022) 39:102884. doi: 10.1016/j.pdpdt.2022.102884
25. Qu Z, Wang Z, Qiu S, Cui G, Li C. Efficacy of photodynamic therapy with 5-aminolevulinic acid for the treatment of cervical high-grade squamous intraepithelial lesions with high-risk HPV infection: A retrospective study. Photodiagnosis Photodyn Ther. (2022) 40:103068. doi: 10.1016/j.pdpdt.2022.103068
26. Hu Y, Li Y, Xu Y, Teng Y, Chen J, Ma L. Topical 5-aminolevulinic acid photodynamic therapy for cervical high-grade squamous intraepithelial lesions. Photodiagnosis Photodyn Ther. (2022) 39:103037. doi: 10.1016/j.pdpdt.2022.103037
27. Wu A, Niu J, Hong Z, Gu L, Huang Y, Qiu L. The effects of 5-aminolevulinic acid photodynamic therapy on the local immune response of women with cervical intraepithelial neoplasia grade 2. Front Immunol. (2023) 14:1211114. doi: 10.3389/fimmu.2023.1211114
28. Li W, Yang J, Luo L, Jiang M, Qin B, Yin H, et al. Targeting photodynamic and photothermal therapy to the endoplasmic reticulum enhances immunogenic cancer cell death. Nat Commun. (2019) 10:3349. doi: 10.1038/s41467-019-11269-8
29. Zhang L, Pan K, Huang S, Zhang X, Zhu X, He Y, et al. Graphdiyne oxide-mediated photodynamic therapy boosts enhancive T-cell immune responses by increasing cellular stiffness. Int J Nanomed. (2023) 18:797–812. doi: 10.2147/IJN.S392998
30. Marzi J, Stope MB, Henes M, Koch A, Wenzel T, Holl M, et al. Noninvasive physical plasma as innovative and tissue-preserving therapy for women positive for cervical intraepithelial neoplasia. Cancers (Basel). (2022) 14(8). doi: 10.3390/cancers14081933
Keywords: photodynamic therapy, 5-aminolevulinic acid, cervical high-grade squamous intraepithelial lesion, high-risk HPV, cervical cancer
Citation: Qian J, Wang Y, Wu G, Lu J, Sun L and Xu S (2024) The efficacy and safety of local 5-aminolevulinic acid-based photodynamic therapy in the treatment of cervical high-grade squamous intraepithelial lesion: a single center retrospective observational study. Front. Oncol. 14:1390982. doi: 10.3389/fonc.2024.1390982
Received: 24 February 2024; Accepted: 03 April 2024;
Published: 16 April 2024.
Edited by:
Noleb Mugisha, Uganda Cancer Institute (UCI), UgandaReviewed by:
Martin Weiss, University Hospital Tübingen, GermanyYu Ligh Liou, The First Affiliated Hospital of Guangdong Pharmaceutical University, China
Copyright © 2024 Qian, Wang, Wu, Lu, Sun and Xu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Song Xu, whxusong@163.com; Liping Sun, 13615717674@163.com
 Jing Qian
Jing Qian Yahui Wang1
Yahui Wang1 Song Xu
Song Xu