Abstract
Background:
The global aging population has led to a public health crisis, with cardiovascular disease, hypertension, arterial stiffness, and obesity becoming major concerns. Resistance training (RT) has been shown to improve cardiovascular health, but traditional RT has certain limitations.
Objective and data sources:
The present systematic review and meta-analysis aims to assess the effects of circuit-based resistance training (CBRT) on blood pressure, arterial stiffness as well as body composition in community-dwelling older adults. PubMed, Cochrane library, Embase, Scopus, and Web of Science, five databases in total, were searched until January 2025. The analysis was restricted to randomized controlled trials.
Methods:
A total of 14 studies, involving 704 participants, were included in the meta-analysis. The primary outcomes assessed were arterial stiffness, blood pressure, and body composition.
Results:
Significant intervention effects were identified in systolic blood pressure (WMD = −6.10 mmHg, 95% CI: −8.07 to −4.12), diastolic blood pressure (WMD = −2.88 mmHg, 95% CI: −3.96 to −1.81), brachial-ankle pulse wave velocity (WMD = −101.81 cm/s, 95% CI: −136.92 to −66.70), percentage of body fat (WMD = −3.21%, 95% CI: −4.20 to −2.22), fat mass (WMD = −4.83 kg, 95% CI: −8.80 to −0.86), lean body mass (WMD = 1.36 kg, 95% CI: 0.83–1.89), and femoral neck bone mineral content (WMD = 0.27 g, 95% CI: 0.14–0.39). Subgroup analysis by training frequency showed that participants with high training frequency (>3 sessions/week) reduce systolic blood pressure more significantly compared to moderate to low training frequency (≤2 sessions/week) while diastolic blood pressure show no difference between subgroups.
Conclusion:
CBRT interventions improve blood pressure, arterial stiffness, and body composition in community-dwelling older adults significantly. Additionally, three sessions of CBRT per week show a superior systolic blood pressure lowering effect.
Systematic Review Registration:
PROSPERO, identifier CRD42025646360.
1 Introduction
By 2050, the population aged 60 and older worldwide is projected to double, reaching 22% of the global population in the world (Kanasi et al., 2016). The aging process is accompanied by elevated blood pressure and increased arterial stiffness, along with unfavorable changes in body composition (Steen, 1988; Wu et al., 2019). Along with insufficient physical activity, these factors exacerbate chronic health conditions such as hypertension, and cardiovascular disease (Merchant et al., 2021).
Hypertension in the older population is primarily attributed to a decline in arterial wall elasticity, characterized by increased SBP and decreased DBP in older adults (Westhoff et al., 2007). As large arteries progressively stiffen, DBP continues to decline, further elevating SBP and contributing to isolated systolic hypertension (ISH), the most prevalent subtype among the elderly (Asmar, 2003).
Pulse wave velocity (PWV) is widely recognized as the gold standard for assessing arterial stiffness (Laurent et al., 2006). It also serves as an independent indicator of cardiovascular disease in both individuals with existing conditions and in healthy ones (Blacher et al., 1999; Mattace-Raso et al., 2006). Given its strong association with cardiovascular events, PWV has become a key focus in chronic disease prevention among the elderly.
According to the report, 80%–92% of the elderly have at least one chronic illness, while 50%–77% experience multiple chronic conditions (Chiaranai et al., 2018). Additionally, more than 66% of adults aged 65 and older suffered from hypertension (Chobanian et al., 2003). Furthermore, chronic diseases have a significant impact on life expectancy. Eliminating deaths from major cardiovascular diseases could extend life expectancy by approximately 5.5 years (Arias et al., 2013), and alleviate significant burden on the medical system and on relevant departments (Control and Prevention, 2003). Moreover, after the age of 30 in women and 40 in men, bone mineral density begins to decline and continues to decrease throughout life (Santos et al., 2017). With aging, the progressive loss of bone mass and reduced bone strength make the skeleton increasingly susceptible to osteoporosis, thereby raising the risk of fragility fractures (Demontiero et al., 2012). The BMD of femoral neck measured by DXA is a strong predictive indicator of hip fractures (Johnell et al., 2005), which are associated with more than a threefold increase in 1-year motality risk (Klop et al., 2017). Bone mineral content (BMC) refers to the total mass of mineral content within the bone as measured by DXA, expressed in grams (g). BMD, on the other hand, indicates the mineral density per unit area, with the widely used unit being g/cm2. From a clinical perspective, however, T-scores and Z-scores, which are derived from raw BMD values, are more commonly used. The T-score is primarily applied to older individuals and represents the number of SDs a person’s BMD deviates from the mean BMD of a healthy young adult population. Defined by the WHO, the T-score is considered the gold standard for diagnosing osteoporosis: a T-score ≥ −1 SD is considered normal, between −1 and −2.5 SDs indicates osteopenia, and ≤−2.5 SDs indicates osteoporosis. The Z-score, in contrast, reflects how much a person’s BMD deviates from the average BMD of individuals of the same age and sex, and is used to evaluate whether a person’s BMD is lower than expected for their age group (Dimai, 2017).
Substantial evidence suggests that exercise, as non-pharmacological interventions, can effectively benefit older adults on their cardiovascular fitness and body composition (Blair, 1996; Ryan et al., 1998; Chodzko-Zajko et al., 2009), enabling them to maintain independence, actively participate in their families and communities, and sustain overall health (Koopman and Van Loon, 2009). The chronic effect of traditional RT on blood pressure management has been widely recognized. However, traditional RT generally show limited improvement on arterial stiffness (Miyachi, 2013; Ashor et al., 2014; Ceciliato et al., 2020; Lopes et al., 2021). Therefore, comprehensive exercise interventions need to be further explored. CBRT is a time-efficient training model that integrates elements of both resistance and aerobic training (Gotshalk et al., 2004; Kolahdouzi et al., 2019). Consequently, CBRT offers various benefits, including enhanced cardiovascular fitness, decreased body fat, improved lean body mass (Gotshalk et al., 2004; Brentano et al., 2008; Camargo et al., 2008; Kolahdouzi et al., 2019). These lower training intensity can minimize muscle soreness and reduce rate of perceived exertion, thereby enhancing compliance and safety among aged individuals (Sparling et al., 1990; Waller et al., 2011).
Community-dwelling older adults, who maintain greater physical independence than hospitalized counterparts, can be well-suited for exercise interventions. However, previous meta-analyses overlooked the effects of CBRT on blood pressure, arterial stiffness. To address this research gap, our systematic review with meta-analysis will evaluate the intervention effects of CBRT on those overlooked outcomes. Additionally, we will evaluate the effects of CBRT on key health indicators across participants with different BMI ranges, as BMI is the most widely used anthropometric measure in clinical practice and research, associating with cardiovascular disease-related mortality (Nuttall, 2015). By systematically evaluating the effects of CBRT on cardiovascular health and body composition in community-dwelling older adults, this study aims to fill the gap in existing knowledge with respect to the effects of this specific form of resistance training in older populations.
2 Methods
2.1 Protocol and guidance
Following Preferred Reporting Items for Systematic Reviews and Meta Analysis (PRISMA) (Liberati et al., 2009), this study has been registered with PROSPERO (CRD42025646360) to ensure transparency and rigor.
2.2 Inclusion criteria
The inclusion criteria were established following the PICOS principles (Liberati et al., 2009). A study was considered eligible if it met the following criteria: all recruited participants were physically independent older adults aged 60 years or older and were community-dwelling rather than hospitalized or institutionalized; CBRT was the only intervention; the control group consisted of individuals who had no exercise intervention; outcome variables included measures related to blood pressure, body composition, and functional autonomy; and only RCTs were included.
2.3 Exclusion criteria
Studies were excluded if they met any of the following conditions: Animal studies were used; the study was an abstract, review, or conference article; the study was published in a non-English language; the study contained incomplete data reporting; the study applied other interventions concurrently with CBRT.
2.4 Outcomes
The primary outcomes included systolic blood pressure (SBP), diastolic blood pressure (DBP), brachial-ankle pulse wave velocity (baPWV), percentage of body fat (%BF), fat mass (FM), lean body mass (LBM), body mass index (BMI), femoral neck bone mineral density and content (BMDFN and BMCFN).
2.5 Search strategy
In order to examine the effects of CBRT on cardiovascular and body composition in community-dwelling adults, One of the authors (JSH) conducted the search of several databases: PubMed, Cochrane library, Embase, Scopus, and Web of Science, from the inception of databases to 10 January 2025. The search strategy consists of both specific MESH terms and entry terms “Circuit-based,” “Training” or “Exercise,” and “older adults,” which are combined with Boolean logic terms “AND,” “OR,” “NOT.”
2.6 Data collection process
After removing duplicates, two independent reviewers (SBA and HCH) screened titles and abstracts to exclude ineligible studies. If an abstract lacked sufficient information to determine eligibility, the full text was retrieved and assessed. Data from all included studies were then extracted using a standardized data extraction form. Any disagreements were resolved through consensus.
2.7 Assessment of risk of bias and publication bias
Two researchers independently assessed the quality of all included trials using the Cochrane Collaboration’s Risk of Bias Tool (Higgins and Altman, 2008). The quality of the included articles was assessed using RevMan 5.4, which evaluates seven domains: random sequence generation, allocation concealment, participant blinding, assessor blinding, completeness of outcome data, selective reporting, and other potential biases.
Due to the limited number of studies per outcome (maximum of six studies), publication bias was not assessed using funnel plots or Egger’s test, as these methods require a minimum of 10 studies for reliable interpretation, according to Cochrane recommendations (Liberati et al., 2009). Any discrepancies were discussed among the three reviewers until a consensus was reached.
2.8 Data synthesis
All the outcomes included in this meta-analysis were continuous, and we standardized all the outcomes into means ± SD if they were demonstrated as means ± SE, or means with 95% CI (Altman and Bland, 2005). For each study, effect sizes were calculated for both the CBRT and control groups. A correlation coefficient of 0.50 was used, and effect sizes were computed using the following formula (Higgins et al., 2008):
We conducted statistical analyses using R (version 4.4.3). I2 test was used to assess heterogeneity, where I2 values indicated the degree of heterogeneity (Higgins and Thompson, 2002). If any degree of heterogeneity was detected (I2 > 0%) and subgroup analyses failed to adequately explain the heterogeneity, both fixed-effect and random-effects models were applied. The results from both models were demonstrated in forest plots to ensure transparency. However, in line with a conservative approach, the random-effects model was adopted for reporting the main findings to account for potential heterogeneity across studies. This approach enhances the robustness and transparency of the meta-analysis by considering the model-based uncertainty.
2.9 Subgroup analysis
In order to further investigate the BP-lowering effect of CBRT with different training frequency, the studies were categorized into two subgroups: high training frequency (3 sessions/week) and moderate to low training frequency (≤2 sessions/week). The effect of the CBRT intervention was then analyzed separately for each subgroup.
2.10 Sensitivity analysis
To assess the robustness of our findings, we conducted a series of sensitivity analyses.
Leave-one-out analysis: Each study was systematically removed one at a time to determine its influence on the pooled effect size and heterogeneity; Comparison of fixed-effects and random-effects models: To evaluate the consistency of our findings across statistical models, we compared the results obtained using fixed-effects and random-effects models. If any of these analyses resulted in substantial changes in the pooled effect size or statistical significance, these findings were documented and discussed.
3 Results
3.1 Eligible studies and study characteristics
The initial search identified 1,558 articles, with 591 duplicates were removed. The titles and abstracts of the remaining 967 articles were screened, leading to the exclusion of 919 articles. A full-text review for the 48 articles remained was conducted, identifying 14 studies that satisfy the inclusion criteria for this systematic review (Rhodes et al., 2000; Miura et al., 2008; Bocalini et al., 2012; Romero-Arenas et al., 2013; Miura et al., 2015; Venturelli et al., 2015; Roberson et al., 2018; Jung et al., 2019; Marcos-Pardo et al., 2019; Choi et al., 2020; Camacho-Cardenosa et al., 2022; Jung et al., 2022; Al-Mhanna et al., 2024; Simms et al., 2024). The meta-analysis was then conducted using outcome measures from these included studies (Figure 1).
FIGURE 1
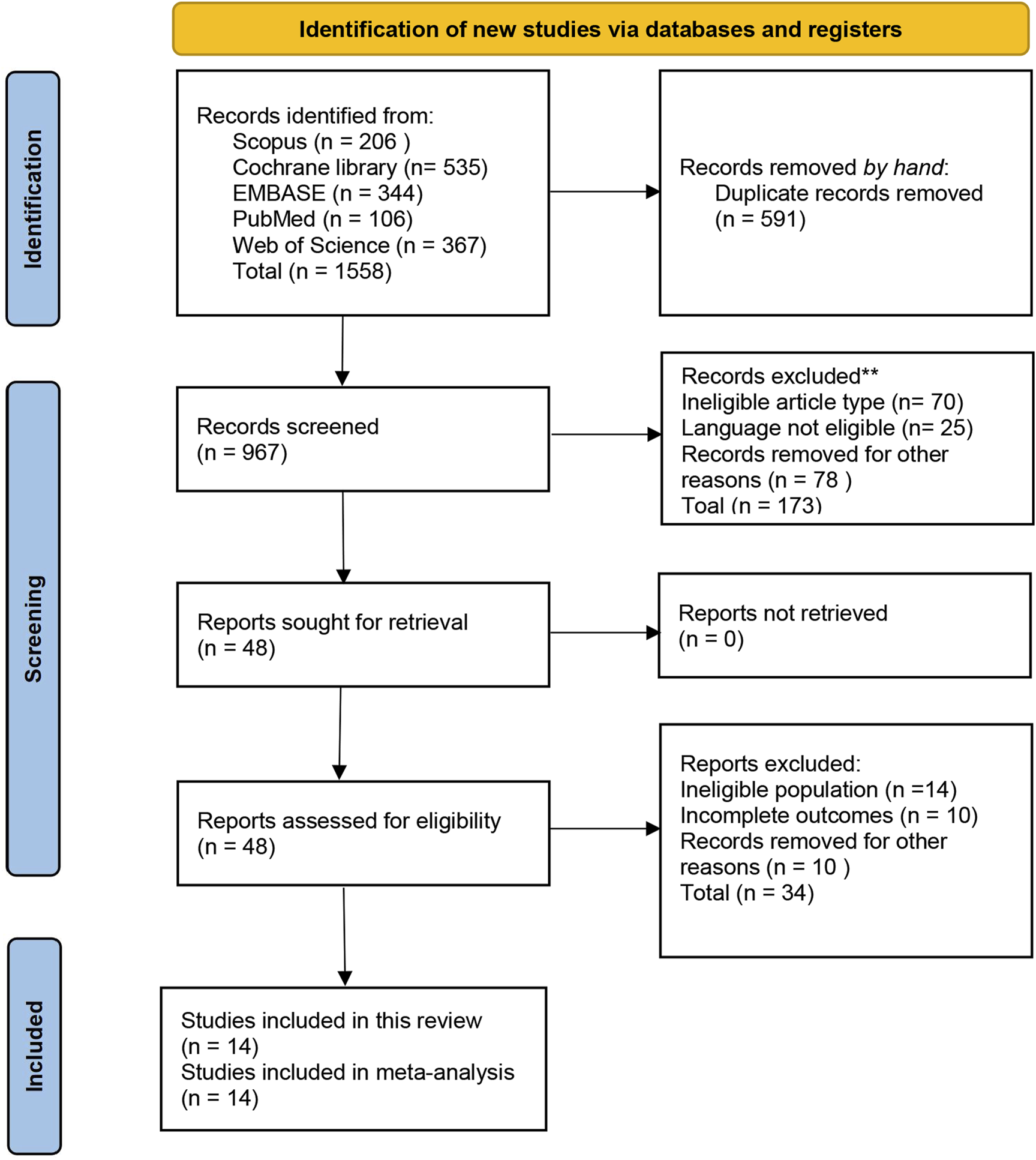
PRISMA flow diagram of study selection process.
Of the 14 included articles, a total of 704 participants aged 60–75 years were involved. There were 19 CBRT intervention groups (390 individuals) and 17 control groups (314 individuals). Table 1 summarizes the main characteristics of all included studies.
TABLE 1
| Study | Group (n) | F% | Age | BMI | Summary of intervention details | |||
|---|---|---|---|---|---|---|---|---|
| Intervention | Duration | Exercises/sets/reps | Outcomes | |||||
| Al-Mhanna et al. (2024) | TG(34) | 55.7% | 62.60 ± 6.90 | 32.41 ± 4.30 | 12/3/36 | 20–60 | 7/2-4/15-30 | BMI |
| CG(35) | 61.70 ± 5.20 | 32.81 ± 5.60 | - | - | ||||
| Bocalini et al. (2012) | TG_AW(18) | 100% | 66 ± 4 | 18.5–24.9 | 12/3/36 | 50 | 12/NR/NR | %BF, FM, LBM |
| TG_OW(14) | 64 ± 4 | 25.0–29.9 | 12/3/36 | 50 | ||||
| TG_O(9) | 62 ± 2 | >30.0 | 12/3/36 | 50 | ||||
| CG_AW(9) | 67 ± 9 | 18.5–24.9 | - | - | ||||
| CG_OW(10) | 63 ± 2 | 25.0–29.9 | - | - | ||||
| CG_O(9) | 62 ± 1 | >30.0 | - | - | ||||
| Camacho-Cardenosa et al. (2022) | TG_N(17) | 59% | 70.35 ± 3.37 | 24.82 ± 2.45 | 24/3/72 | 45 | 9/3/12-15 | BMDFN, BMCFN |
| TG_H(13) | 68.46 ± 3.82 | 26.41 ± 3.46 | 24/3/72 | 45 | ||||
| CG(20) | 70.55 ± 4.10 | 28.23 ± 3.06 | - | - | ||||
| Choi et al. (2020) | TG(15) | NR | 75.1 ± 1.4 | 25.3 ± 0.5 | 12/3/36 | 60 | 19/NR/10-12 | SBP, DBP, MAP, PP |
| CG(12) | 72.3 ± 1.4 | 25.5 ± 0.4 | - | - | ||||
| Jung et al. (2019) | TG(13) | 100% | 75.0 ± 3.9 | 21.8 ± 1.5 | 12/3/36 | 25–75 | PRO 10/1-3/NR | %BF, FM, LBM, BMI |
| CG(13) | 74.9 ± 5.2 | 21.9 ± 1.5 | - | - | ||||
| Jung et al. (2022) | TG(13) | 100% | 75.36 ± 4.50 | 22.50 ± 1.75 | 12/3/36 | 45–75 | PRO 10/1-3/NR | SBP, DBP, MAP, PP, baPWV, %BF, LBM, BMI |
| CG(13) | 74.64 ± 5.77 | 22.58 ± 1.69 | - | - | ||||
| Marcos-Pardo et al. (2019) | TG(24) | 60% | M: 69 ± 3.2 | 27.97 ± 3.74 | 12/3/36 | Not fixed | 6/NR/8-12 | %BF, LBM, BMI, FA |
| F: 70 ± 4.1 | 26.67 ± 4.51 | - | - | |||||
| CG(21) | M: 69 ± 3.2 | 27.57 | 12/3/36 | Not fixed | ||||
| F: 70 ± 4.1 | 26.09 ± 3.34 | - | - | |||||
| Miura et al. (2008) | TG_1DW(29) | 100% | 69.0 ± 6.5 | 22.8 ± 2.4 | 12/1/12 | 40 | 8/3/8 | SBP, DBP, baPWV, BMI |
| TG_2DW(25) | 69.5 ± 7.0 | 23.5 ± 2.7 | 12/2/24 | 40 | ||||
| CG(23) | 68.9 ± 7.5 | 23.7 ± 3.0 | - | - | ||||
| Miura et al. (2015) | TG_HTN(45) | 100% | 72.0 ± 7.1 | NR | 12/2/24 | 90 | PRO 6-8/3-5/15-20 | SBP, DBP, baPWV, %BF |
| CG_HTN(47) | 71.8 ± 5.6 | NR | - | - | ||||
| TG_NT(55) | 72.9 ± 5.7 | NR | 12/2/24 | 90 | ||||
| CG_NT(53) | 69.7 ± 6.7 | NR | - | - | ||||
| Rhodes et al. (2000) | TG(20) | 100% | 68.8 ± 3.2 | NR | 52/3/156 | 60 | 8/3/8 | BMDFN, BMCFN |
| CG(18) | 68.2 ± 3.5 | NR | - | - | ||||
| Roberson et al. (2018) | TG(9) | 73.3% | 72 ± 3 | 33.0 ± 1.0 | 12/3/36 | Not fixed | 11/NR/12 | SBP, DBP |
| CG(7) | 70 ± 3 | 31.1 ± 2.4 | - | - | ||||
| Romero-Arenas et al. (2013) | TG(16) | NR | 62.1 ± 6.3 | 29.7 ± 4.1 | 12/2/24 | 35–47 | PRO 6/1-3/6-12 | BMDFN |
| CG(7) | 58.0 ± 5.0 | 29.9 ± 5.8 | - | - | ||||
| Simms et al. (2024) | TG(11) | 55.5% | 70.3 ± 5.7 | NR | 8/3/24 | 40–45 | PRO 10/1-3/10-12 | SBP, DBP, MAP |
| CG(7) | 71.6 ± 5.2 | NR | - | - | ||||
| Venturelli et al. (2015) | TG(10) | 50% | 67 ± 4 | 27 ± 3 | 12/3/36 | 60 | 4/NR/NR | BMI |
| CG(10) | 66 ± 7 | 27 ± 6 | - | - | ||||
Main characteristics of included studies in the meta-analysis.
“-” stands for not receiving intervention, TG, training group; CG, control group; NR, not reported; PRO, progressive training; AW, appropriate weight; OW, overweight; O, obese; 1DW, 1 day per week; 2DW, 2 days per week; N, normoxic training condition; H, hypoxic training condition; HTN, hypertensive population; NT, normotensive population; M, male; F, female.
Due to data limitations, one study (Romero-Arenas et al., 2013) reported that the mean age of the control group was 58 years, while that of the experimental group was 62.1 years. Since their mean age met the inclusion criteria (≥60 years), we still considered the study eligible. Eight included studies focused exclusively on community-dwelling older female (100% female participants), while the remaining studies adopted a mixed-gender approach, and no study specifically examined older male.
3.2 Quality (risk of bias) assessment
Detailed risk of bias assessment results are provided (Figures 2, 3). In exercise intervention studies, blinding of participants is generally not feasible; therefore, this domain was assessed as unclear risk. Among the included studies, five did not provide information on the randomization method (unclear risk of bias), while two did not use randomization and were therefore rated as high risk. None of the included studies reported on allocation concealment (unclear risk of bias). Additionally, two studies did not report their pre-registration information, leading to a high risk rating for selective reporting.
FIGURE 2
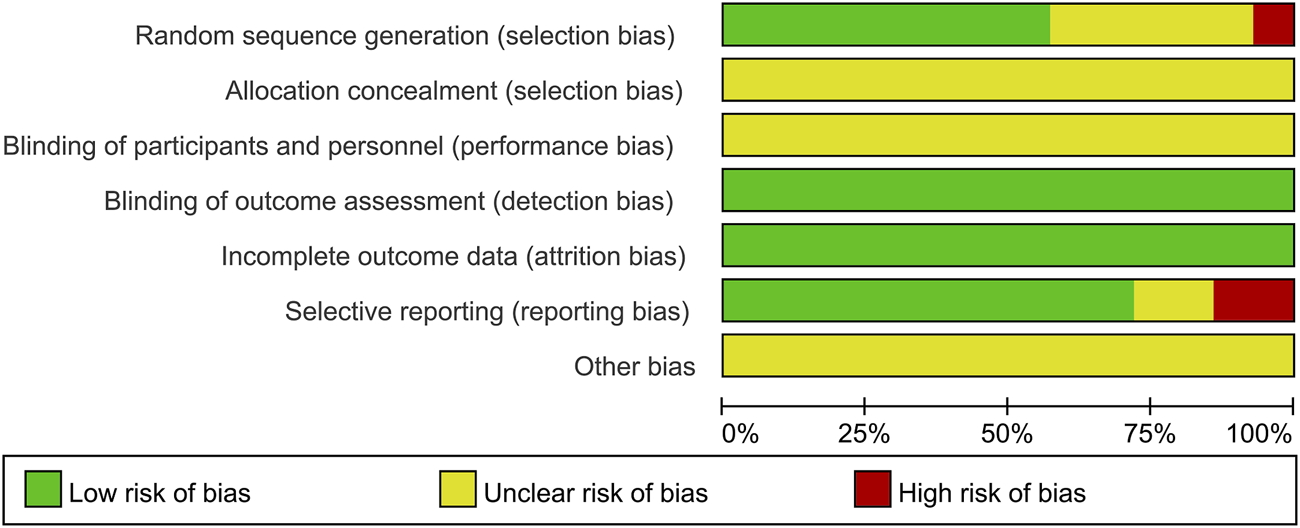
Proportional representation of risk of bias assessment in included trials.
FIGURE 3
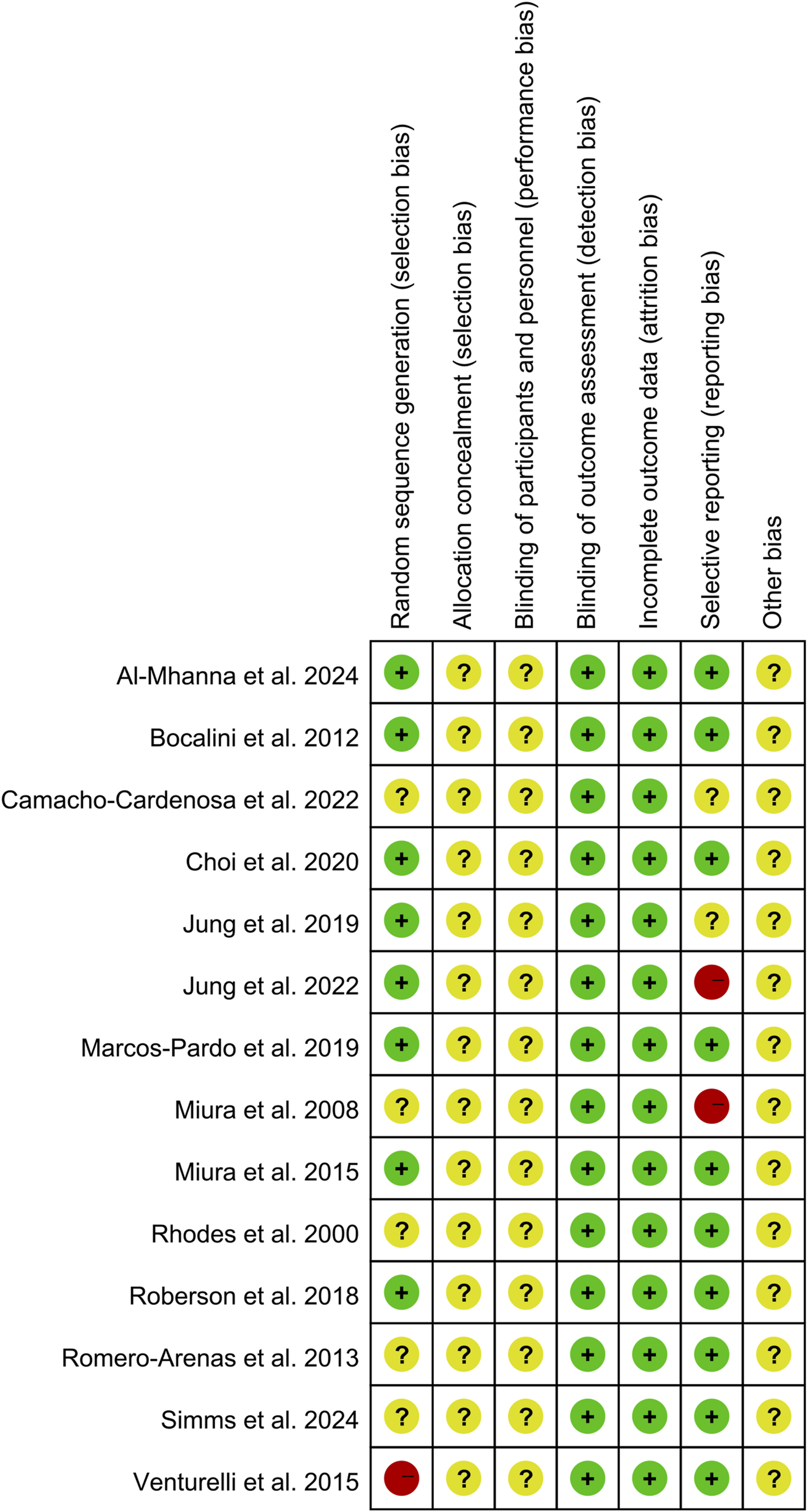
Risk of bias summary: review authors’ judgments about each risk of bias item for each of the 14 included studies.
3.3 Results of the meta-analysis
3.3.1 Effect of circuit-based resistance training on blood pressure
After conducting the analysis of data from all included studies, we found that the CBRT group showed a significant reduction in SBP (WMD = −6.10 mmHg, 95% CI: −8.07 to −4.12, I2 = 25.2%), DBP (WMD = −2.88 mmHg, 95% CI: −3.96 to −1.81, I2 = 0%) compared to the control group (Figure 4).
FIGURE 4
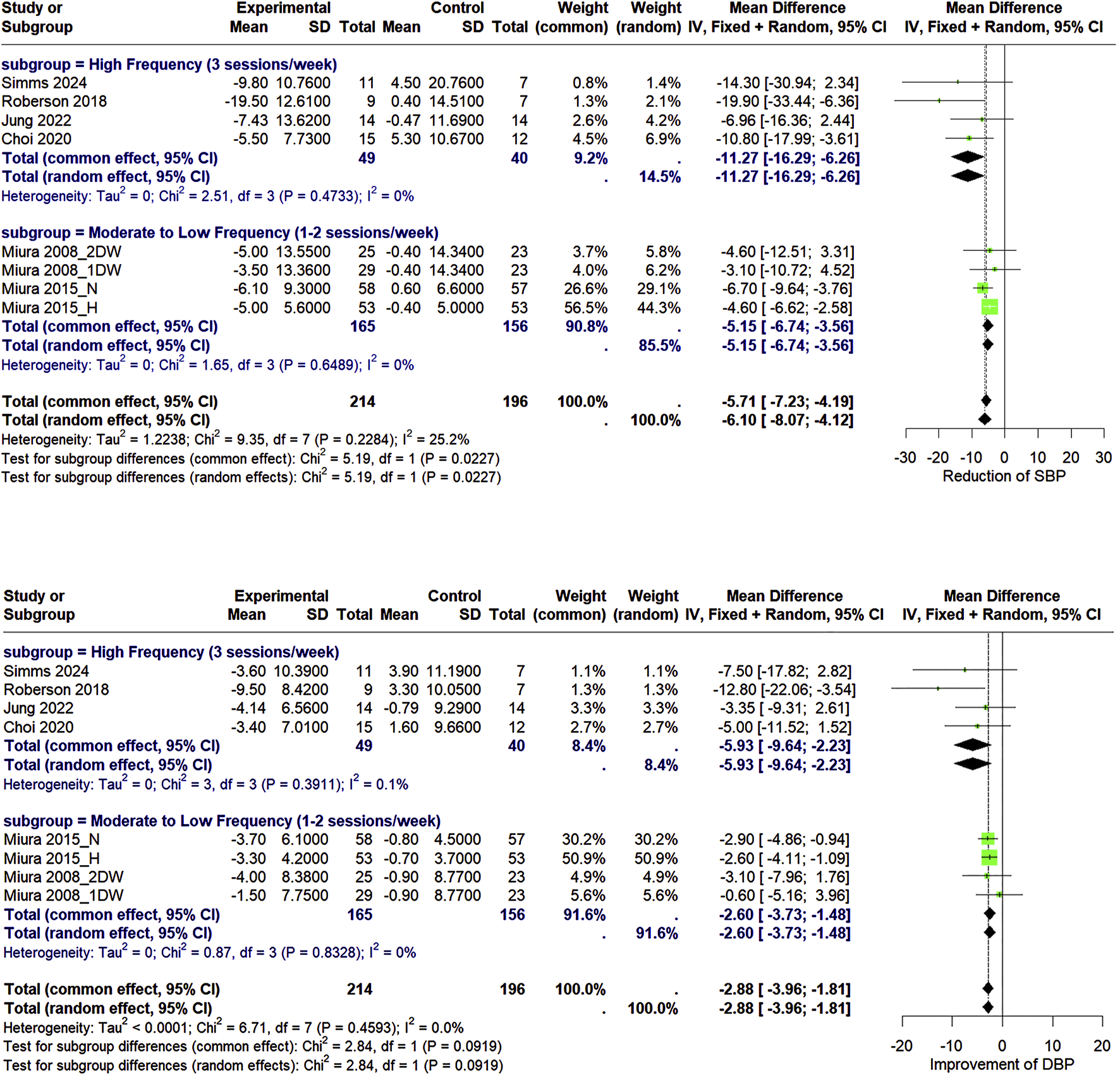
Forest plot of the pooled effects of CBRT versus control on SBP, DBP in older adults living in the community using both fixed-effects and random-effects model. “1DW” and “2DW” indicate training frequencies of 1 or 2 days per week, while “H” and “N” represent hypertensive and normotensive populations.
3.3.2 Effect of circuit-based resistance training on arterial stiffness
The meta-analysis (Figure 5) of three included studies of baPWV revealed that CBRT reduces baPWV (WMD = −101.81 cm/s, 95% CI: −136.92 to −66.70, I2 = 29.5%).
FIGURE 5
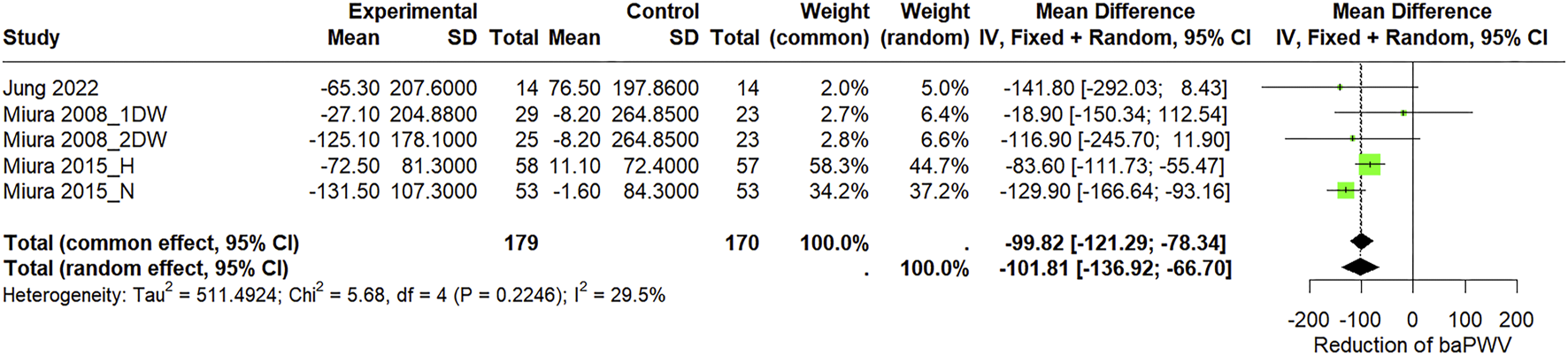
Forest plot of the pooled effects of CBRT versus control on baPWV in community-dwelling older individuals using both fixed-effects and random-effects model. “1DW” and “2DW” refer to training frequencies (1 or 2 days per week), while “H” and “N” indicate hypertensive and normotensive populations.
3.3.3 Effect of circuit-based resistance training on body composition
The meta-analysis revealed a significant overall effect of CBRT in decreasing %BF (WMD = −3.21%, 95% CI: −4.20 to −2.22, I2 = 44.6%), FM (WMD = −4.83 kg, 95% CI: −8.80 to −0.86, I2 = 88.2%), BMI (WMD = 0.03 kg/m2, 95% CI: −0.71 to −0.76, I2 = 0%), and increasing LBM (WMD = 1.36 kg, 95% CI: 0.83–1.89, I2 = 0%), BMDFN (WMD = 0.01 g/cm2, 95% CI: −0.02 to 0.05, I2 = 12.7%), BMCFN (WMD = 0.27 g, 95% CI: 0.14–0.39, I2 = 0%) (Figure 6).
FIGURE 6
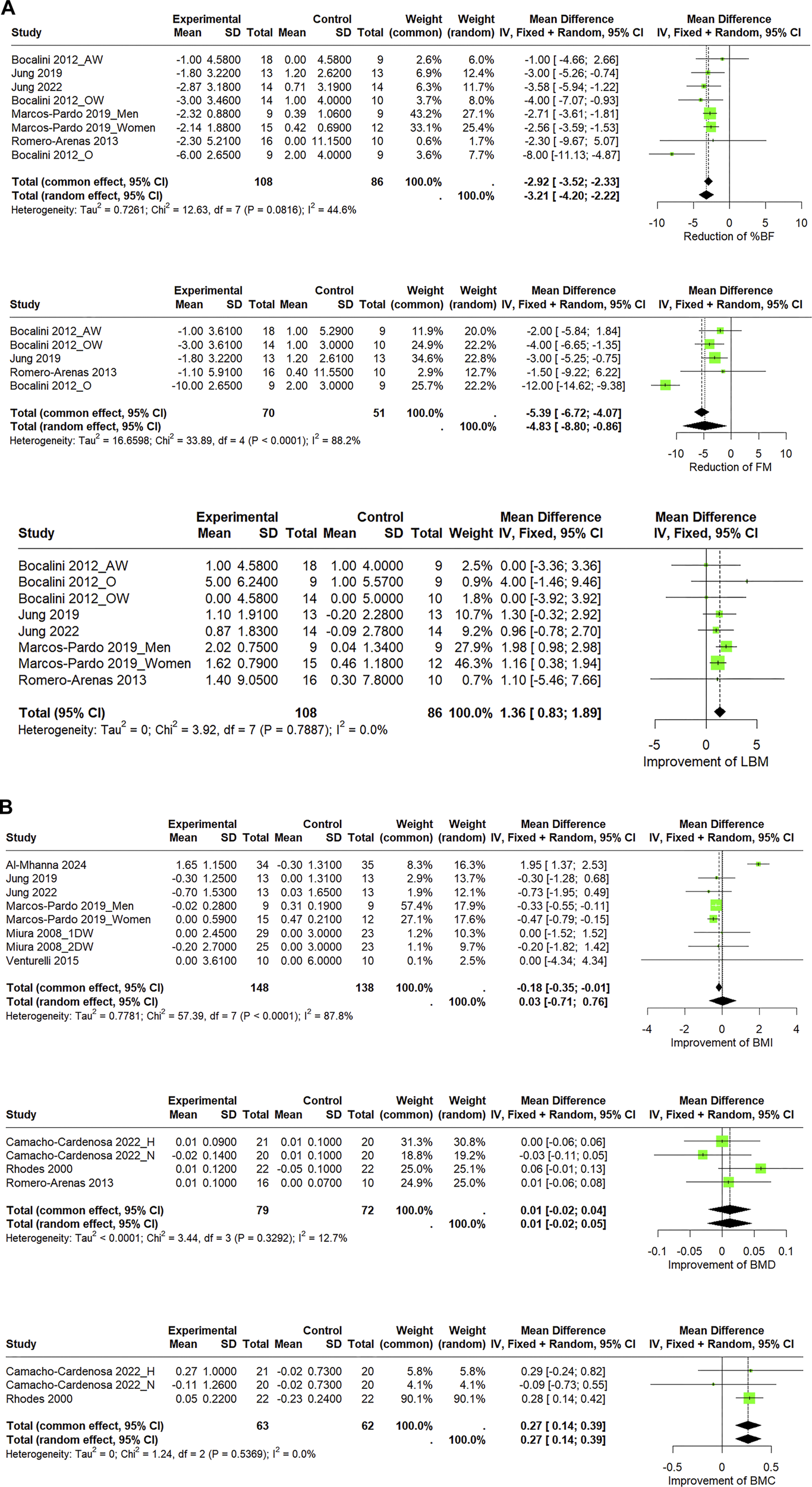
(A) Forest plot of the pooled effects of CBRT versus control on body composition in community-dwelling older adults using both fixed-effects and random-effects model. “AW,” “OW,” and “O” denote BMI categories. (B) Forest plot of the pooled effects of CBRT versus control on body composition in community-dwelling older adults using both fixed-effects and random-effects model. “1DW” and “2DW” indicate training frequencies; “H” and “N” represent interventions under hypoxic and normoxic conditions.
3.4 Sensitivity analyses
We conducted leave-one-out sensitivity analyses for outcomes of BMI (Supplementary Figure S1), %BF (Supplementary Figure S2), and FM (Supplementary Figure S3), to explore potential sources of heterogeneity. The analyses demonstrated that the exclusion of this study significantly reduced heterogeneity (from I2 = 87.8%–0%) and changed the overall effect estimate from a non-significant mean difference of 0.03 (95% CI: −0.71 to 0.76) to a significant reduction of −0.37 (95% CI: −0.55 to −0.20). Given the determinant influence of this single study, the conclusion should be interpreted with caution.
Leave-one-out sensitivity analysis for %BF and FM identified the experimental arm “Obese group” from Bocalini et al. (2012) as a potential contributor to the observed moderate-to-high heterogeneity (I2 = 44.6% and 88.2%). However, the exclusion of this study or any other single study from both outcomes, did not substantially alter the overall effect size or change the statistical significance of the pooled results. Therefore, all studies were retained in the main analysis. Given the presence of moderate heterogeneity, a random-effects model was adopted to provide a more conservative and robust estimate of the effect size.
3.5 Subgroup analysis
In order to further investigate the BP-lowering effect of CBRT with different training frequency, the studies were categorized into two subgroups: high training frequency (3 sessions/week) and moderate to low training frequency (≤2 sessions/week). Subgroup analyses demonstrated that high-frequency CBRT was significantly more effective in reducing systolic blood pressure (SBP) compared to moderate-to-low frequency CBRT (p for subgroup differences <0.05). Although high-frequency CBRT also showed greater reductions in diastolic blood pressure (DBP), the difference between the two subgroups was not statistically significant (p = 0.09).
4 Discussion
To the best of our knowledge, this is the first meta-analysis systematically evaluating the effects of CBRT on blood pressure, arterial stiffness, and bone health in community-dwelling older adults.
Our findings suggest that CBRT can be safely applied to improve cardiovascular health and body composition in older populations. Notably, seven studies included participants aged 70 years or more, yet still demonstrated beneficial effects. Among the 14 studies included in this meta-analysis, 11 focused on the effects of exercise interventions on cardiovascular health and body composition. The intervention period for these studies was uniformly 12 weeks, except for Simms et al. (2024), which lasted 8 weeks. In contrast, studies targeting bone health typically required longer intervention durations of 12, 24, or 52 weeks (Rhodes et al., 2000; Romero-Arenas et al., 2013; Camacho-Cardenosa et al., 2022). Therefore, discussions regarding the improvements in cardiovascular function are based solely on short-to medium-term interventions. CBRT, as an “optimal combination” of training modalities, led to a significant reduction in SBP (−6.10 mmHg), DBP (−2.88 mmHg), and baPWV (−101.81 cm s−1). This may be due to the nature of CBRT, where lighter weights are lifted with shorter recovery time between sets and result in greater cardiovascular stimulation (Gotshalk et al., 2004).
Our meta-analysis demonstrated that CBRT significantly improves both blood pressure and arterial stiffness at the same time. In consistent with ours, a meta-analysis reported that low-intensity short-rest resistance training significantly reduces baPWV by improving endothelial function (Okamoto et al., 2011). Moreover, resistance training, regardless of intensity, has been shown to effectively improve blood pressure, including both peripheral and central blood pressure (Figueroa et al., 2019). In contrast, traditional resistance training with heavy weights has no significant effect on arterial stiffness in middle-aged and older adults (Miyachi, 2013; Ashor et al., 2014; Lopes et al., 2021). One potential mechanism potentially interpreting the effect of CBRT is that the CBRT-induced muscle hypoxia stimulates nitric oxide (NO) production, enhances endothelial function, and subsequently reduces arterial stiffness, whereas high-intensity resistance training with longer recovery periods does not improve this function (Okamoto et al., 2009). It is suggested that lower-intensity resistance training with shorter rest intervals may be more effective in simultaneously improving baPWV and blood pressure. In terms of training organization, CBRT inherently possesses these characteristics.
It is reported that 10 mmHg reduction in SBP or SBP decrease to lower than 130 mmHg can greatly lower the risk of major cardiovascular disease and coronary heart disease (Ettehad et al., 2016). Additionally, a meta-analysis stated that every 1 m/s increase in baPWV can compound the risk of developing cardiovascular increases by 12% (Vlachopoulos et al., 2012). In this meta-analysis, CBRT significantly lower the baPWV by around 1 m/s, which can be interpreted as a significant lowered risk of cardiovascular disease. However, Since the included studies in this meta-analysis reported blood pressure-related outcomes only lasted 8–12 weeks, the long-term sustainable effect of CBRT-induced cardiovascular fitness improvements in community-dwelling older adults remains unclear. Furthermore, the significant reduction in baPWV observed in this study were restricted to suggest that CBRT may improve peripheral arterial elasticity, while its effects on central aortic compliance remain to be elucidated. Future studies should incorporate carotid-femoral pulse wave velocity (cfPWV) assessments to further investigate the effect of CBRT on lowering central arterial stiffness.
Body composition primarily includes fat, muscle, bone, and water. These components together constitute the total body mass. The relative proportion of body composition can reflect the physiological status and overall health of an individual (Heymsfield et al., 2005). The present meta-analysis indicates that CBRT has positive effects in reducing body fat and improving LBM. This effect may be attributed to the CBRT model, which enhances glucose uptake by skeletal muscle, reduces fat storage in adipose tissue, and helps maintain or increase basal metabolic rate (Donnelly et al., 2009).
Although the meta-analysis revealed a significant improvement in BMCFN, no significant change was observed in BMDFN. The increase in BMCFN suggests a potential enhancement in bone quality at the femoral neck; however, due to the absence of clinically diagnostic indicators such as T-scores, this finding can only be interpreted as evidence of the physiological potential of CBRT to improve bone mineral content. Its clinical relevance in terms of osteoporosis prevention or treatment remains unclear. This is in line with previous findings suggesting that low-impact resistance training may not produce significant changes in BMDFN or BMD at lumber spine in older adults (Marques et al., 2012). In contrast, a 6-month high-intensity resistance training intervention has shown that BMDFN could be improved significantly (Vincent and Braith, 2002). This may be attributed to the relatively light weights used in CBRT, which may not impose the mechanical stress to stimulate BMD increases, thereby limiting the potential for BMD improvement.
5 Limitation
Although this study provides important evidence. Some limitations in the present meta-analysis also need to be acknowledged.
Firstly, the included studies showed overall low quality with quite a few unclear or unreported risk of bias, which may have compromised the robustness of our findings and limited the generalizability of the results. Secondly, only a few studies reported on several outcomes variables, such as baPWV, which restricted our ability to conduct more comprehensive subgroup analyses. Another potential limitation of this meta-analysis is the inability to assess publication bias due to the small number of included studies. Future studies with sufficient number of included study could confirm the robustness of these findings and further evaluate possible publication bias.
6 Conclusion
This meta-analysis suggests that CBRT is a safe and effective intervention in community-dwelling older adults, which can significantly improve elevated blood pressure, stiffened arteries, and exacerbated body composition with age. An 8–12-week CBRT program can effectively improve systolic and diastolic blood pressure, as well as body fat percentage and lean body mass in community-dwelling older adults. A higher training frequency (three sessions per week) appears to exert a more pronounced effect on blood pressure management in this population. Exercise prescriptions based on the modality of CBRT can be designed for community-dwelling older adults to promote public health in communities.
Statements
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
ZH: Formal Analysis, Conceptualization, Writing – original draft. SJ: Writing – review and editing, Conceptualization. CH: Writing – review and editing, Investigation, Conceptualization. BS: Conceptualization, Writing – review and editing, Investigation. JG: Writing – review and editing, Conceptualization.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphys.2025.1609013/full#supplementary-material
References
1
Al-Mhanna S. B. Batrakoulis A. Mohamed M. Alkhamees N. H. Sheeha B. B. Ibrahim Z. M. et al (2024). Home-based circuit training improves blood lipid profile, liver function, musculoskeletal fitness, and health-related quality of life in overweight/obese older adult patients with knee osteoarthritis and type 2 diabetes: a randomized controlled trial during the COVID-19 pandemic. BMC Sports Sci. Med. Rehabilitation16 (1), 125. 10.1186/s13102-024-00915-4
2
Altman D. G. Bland J. M. (2005). Standard deviations and standard errors. BMJ331 (7521), 903. 10.1136/bmj.331.7521.903
3
Arias E. Heron M. P. Tejada-Vera B. (2013). United States life tables eliminating certain causes of death, 1999-2001.
4
Ashor A. W. Lara J. Siervo M. Celis-Morales C. Mathers J. C. (2014). Effects of exercise modalities on arterial stiffness and wave reflection: a systematic review and meta-analysis of randomized controlled trials. PLoS One9 (10), e110034. 10.1371/journal.pone.0110034
5
Asmar R. (2003). Benefits of blood pressure reduction in elderly patients. J. Hypertens.21, S25–S30. 10.1097/00004872-200307006-00005
6
Blacher J. Asmar R. Djane S. London G. R. M. Safar M. E. (1999). Aortic pulse wave velocity as a marker of cardiovascular risk in hypertensive patients. Hypertension33 (5), 1111–1117. 10.1161/01.hyp.33.5.1111
7
Blair S. N. Kampert J. B. Kohl H. W. 3rd Barlow C. E. Macera C. A. Paffenbarger R. S. Jr et al (1996). Influences of cardiorespiratory fitness and other precursors on cardiovascular disease and all-cause mortality in men and women. JAMA J. Am. Med. Assoc.276 (3), 205–210. 10.1001/jama.1996.03540030039029
8
Bocalini D. S. Lima L. S. de Andrade S. Madureira A. Rica R. L. dos Santos R. N. et al (2012). Effects of circuit-based exercise programs on the body composition of elderly obese women. Clin. Interventions Aging7, 551–556. 10.2147/CIA.S33893
9
Brentano M. A. Cadore E. L. Da Silva E. M. Ambrosini A. B. Coertjens M. Petkowicz R. et al (2008). Physiological adaptations to strength and circuit training in postmenopausal women with bone loss. J. Strength Cond. Res.22 (6), 1816–1825. 10.1519/jsc.0b013e31817ae3f1
10
Camacho-Cardenosa A. Camacho-Cardenosa M. Martinez-Guardado I. Leal A. Andrada J. M. V. Timon R. (2022). Resistance circuit training combined with hypoxia stimulates bone system of older adults: a randomized trial. Exp. Gerontol.169, 111983. 10.1016/j.exger.2022.111983
11
Camargo M. D. Stein R. Ribeiro J. P. Schvartzman P. R. Rizzatti M. O. Schaan B. D. (2008). Circuit weight training and cardiac morphology: a trial with magnetic resonance imaging. Br. J. Sports Med.42 (2), 141–145. 10.1136/bjsm.2007.038281
12
Ceciliato J. Costa E. C. Azevêdo L. Sousa J. C. Fecchio R. Y. Brito L. C. (2020). Effect of resistance training on arterial stiffness in healthy subjects: a systematic review and meta-analysis. Curr. Hypertens. Rep.22 (8), 51. 10.1007/s11906-020-01065-x
13
Chiaranai C. Chularee S. Srithongluang S. (2018). Older people living with chronic illness. Geriatr. Nurs.39 (5), 513–520. 10.1016/j.gerinurse.2018.02.004
14
Chobanian A. V. Bakris G. L. Black H. R. Cushman W. C. Green L. A. Izzo J. L. et al (2003). Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension42 (6), 1206–1252. 10.1161/01.hyp.0000107251.49515.c2
15
Chodzko-Zajko W. J. Proctor D. N. Fiatarone Singh M. A. Minson C. T. Nigg C. R. Salem G. J. et al (2009). American college of sports medicine position stand. Exercise and physical activity for older adults. Med. Sci. Sports Exerc.41 (7), 1510–1530. 10.1249/mss.0b013e3181a0c95c
16
Choi H. M. Hurr C. Kim S. (2020). Effects of elastic band exercise on functional fitness and blood pressure response in the healthy elderly. Int. J. Environ. Res. Public Health17 (19), 7144. 10.3390/ijerph17197144
17
Control C. F. D. Prevention (2003). Trends in aging--United States and worldwide. MMWR. Morb. Mortal. Wkly. Rep.52 (6), 101–106. Available online at: https://stacks.cdc.gov/view/cdc/11397https://beta.cdc.gov/mmwr/preview/mmwrhtml/mm5206a2.htm.
18
Demontiero O. Vidal C. Duque G. (2012). Aging and bone loss: new insights for the clinician. Ther. Adv. Musculoskelet. Dis.4 (2), 61–76. 10.1177/1759720x11430858
19
Dimai H. P. (2017). Use of dual-energy X-ray absorptiometry (DXA) for diagnosis and fracture risk assessment; WHO-criteria, T- and Z-score, and reference databases. Bone104, 39–43. 10.1016/j.bone.2016.12.016
20
Donnelly J. E. Blair S. N. Jakicic J. M. Manore M. M. Rankin J. W. Smith B. K. et al (2009). American college of sports medicine position stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med. Sci. Sports Exerc.41 (2), 459–471. 10.1249/mss.0b013e3181949333
21
Ettehad D. Emdin C. A. Kiran A. Anderson S. G. Callender T. Emberson J. et al (2016). Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet387 (10022), 957–967. 10.1016/s0140-6736(15)01225-8
22
Figueroa A. Okamoto T. Jaime S. J. Fahs C. A. (2019). Impact of high- and low-intensity resistance training on arterial stiffness and blood pressure in adults across the lifespan: a review. Pflügers Archiv - Eur. J. Physiology471 (3), 467–478. 10.1007/s00424-018-2235-8
23
Gotshalk L. A. Berger R. A. Kraemer W. J. (2004). Cardiovascular responses to a high-volume continuous circuit resistance training protocol. J. Strength Cond. Res.18 (4), 760–764. 10.1519/14954.1
24
Heymsfield S. Lohman T. Wang Z. Going S. B. (2005). Human body composition. Champaign, IL: Human Kinetics.
25
Higgins J. P. Altman D. G. (2008). “Assessing risk of bias in included studies,” in Cochrane handbook for systematic reviews of interventions: Cochrane book series, 187–241. 10.1002/9780470712184.ch8
26
Higgins J. P. Deeks J. J. Altman D. G. (2008). “Special topics in statistics,” in Cochrane handbook for systematic reviews of interventions: Cochrane book series, 481–529. 10.1002/9780470712184.ch16
27
Higgins J. P. Thompson S. G. (2002). Quantifying heterogeneity in a meta-analysis. Statistics Med.21 (11), 1539–1558. 10.1002/sim.1186
28
Johnell O. Kanis J. A. Oden A. Johansson H. De Laet C. Delmas P. et al (2005). Predictive value of BMD for hip and other fractures. J. Bone Mineral Res.20 (7), 1185–1194. 10.1359/jbmr.050304
29
Jung W. S. Kim Y. Y. Kim J. W. Park H. Y. (2022). Effects of circuit training program on cardiovascular risk factors, vascular inflammatory markers, and insulin-like growth factor-1 in elderly obese women with sarcopenia. Rev. Cardiovasc. Med.23 (4), 134. 10.31083/j.rcm2304134
30
Jung W. S. Kim Y. Y. Park H. Y. (2019). Circuit training improvements in Korean women with sarcopenia. Percept. Mot. Ski.126 (5), 828–842. 10.1177/0031512519860637
31
Kanasi E. Ayilavarapu S. Jones J. (2016). The aging population: demographics and the biology of aging. Periodontol 200072 (1), 13–18. 10.1111/prd.12126
32
Klop C. Van Staa T. P. Cooper C. Harvey N. C. De Vries F. (2017). The epidemiology of mortality after fracture in England: variation by age, sex, time, geographic location, and ethnicity. Osteoporos. Int.28 (1), 161–168. 10.1007/s00198-016-3787-0
33
Kolahdouzi S. Baghadam M. Kani-Golzar F. A. Saeidi A. Jabbour G. Ayadi A. et al (2019). Progressive circuit resistance training improves inflammatory biomarkers and insulin resistance in obese men. Physiol. Behav.205, 15–21. 10.1016/j.physbeh.2018.11.033
34
Koopman R. Van Loon L. J. C. (2009). Aging, exercise, and muscle protein metabolism. J. Appl. Physiol.106 (6), 2040–2048. 10.1152/japplphysiol.91551.2008
35
Laurent S. Cockcroft J. Van Bortel L. Boutouyrie P. Giannattasio C. Hayoz D. et al (2006). Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur. Heart J.27 (21), 2588–2605. 10.1093/eurheartj/ehl254
36
Liberati A. Altman D. G. Tetzlaff J. Mulrow C. Gøtzsche P. C. Ioannidis J. P. et al (2009). The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann. Intern. Med.151 (4), W65–W94. 10.7326/0003-4819-151-4-200908180-00136
37
Lopes S. Afreixo V. Teixeira M. Garcia C. Leitão C. Gouveia M. et al (2021). Exercise training reduces arterial stiffness in adults with hypertension: a systematic review and meta-analysis. J. Hypertens.39 (2), 214–222. 10.1097/hjh.0000000000002619
38
Marcos-Pardo P. J. Orquin-Castrillón F. J. Gea-García G. M. Menayo-Antúnez R. González-Gálvez N. Vale R. G. D. et al (2019). Effects of a moderate-to-high intensity resistance circuit training on fat mass, functional capacity, muscular strength, and quality of life in elderly: a randomized controlled trial. Sci. Rep.9, 7830. 10.1038/s41598-019-44329-6
39
Marques E. A. Mota J. Carvalho J. (2012). Exercise effects on bone mineral density in older adults: a meta-analysis of randomized controlled trials. AGE34 (6), 1493–1515. 10.1007/s11357-011-9311-8
40
Mattace-Raso F. U. van der Cammen T. J. Hofman A. van Popele N. M. Bos M. L. Schalekamp M. A. et al (2006). Arterial stiffness and risk of coronary heart disease and stroke: the Rotterdam Study. Circulation113 (5), 657–663. 10.1161/circulationaha.105.555235
41
Merchant R. A. Morley J. E. Izquierdo M. (2021). Editorial: exercise, aging and frailty: guidelines for increasing function. J. Nutr. health aging25 (4), 405–409. 10.1007/s12603-021-1590-x
42
Miura H. Nakagawa E. Takahashi Y. (2008). Influence of group training frequency on arterial stiffness in elderly women. Eur. J. Appl. Physiol.104 (6), 1039–1044. 10.1007/s00421-008-0860-1
43
Miura H. Takahashi Y. Maki Y. Sugino M. (2015). Effects of exercise training on arterial stiffness in older hypertensive females. Eur. J. Appl. Physiol.115 (9), 1847–1854. 10.1007/s00421-015-3168-y
44
Miyachi M. (2013). Effects of resistance training on arterial stiffness: a meta-analysis. Br. J. Sports Med.47 (6), 393–396. 10.1136/bjsports-2012-090488
45
Nuttall F. Q. (2015). Body mass index: obesity, BMI, and health: a critical review. Nutr. Today50 (3), 117–128. 10.1097/nt.0000000000000092
46
Okamoto T. Masuhara M. Ikuta K. (2009). Effects of muscle contraction timing during resistance training on vascular function. J. Hum. Hypertens.23 (7), 470–478. 10.1038/jhh.2008.152
47
Okamoto T. Masuhara M. Ikuta K. (2011). Effect of low-intensity resistance training on arterial function. Eur. J. Appl. Physiol.111 (5), 743–748. 10.1007/s00421-010-1702-5
48
Rhodes E. C. Martin A. D. Taunton J. E. Donnelly M. Warren J. Elliot J. (2000). Effects of one year of resistance training on the relation between muscular strength and bone density in elderly women. Br. J. Sports Med.34 (1), 18–22. 10.1136/bjsm.34.1.18
49
Roberson K. B. Potiaumpai M. Widdowson K. Jaghab A. M. Chowdhari S. Armitage C. et al (2018). Effects of high-velocity circuit resistance and treadmill training on cardiometabolic risk, blood markers, and quality of life in older adults. Physiol. Appliquee Nutr. metabolisme Appl. Physiol. Nutr. Metab.43 (8), 822–832. 10.1139/apnm-2017-0807
50
Romero-Arenas S. Blazevich A. J. Martínez-Pascual M. Pérez-Gómez J. Luque A. J. López-Román F. J. et al (2013). Effects of high-resistance circuit training in an elderly population. Exp. Gerontol.48 (3), 334–340. 10.1016/j.exger.2013.01.007
51
Ryan A. S. Nicklas B. J. Dennis K. E. (1998). Aerobic exercise maintains regional bone mineral density during weight loss in postmenopausal women. J. Appl. Physiol.84 (4), 1305–1310. 10.1152/jappl.1998.84.4.1305
52
Santos L. Elliott-Sale K. J. Sale C. (2017). Exercise and bone health across the lifespan. Biogerontology18 (6), 931–946. 10.1007/s10522-017-9732-6
53
Simms A. G. Signorile J. F. Gameiro G. R. Allaf A. M. Wang J. Jiang H. (2024). Choriocapillaris perfusion after 8 Weeks of high-speed circuit training in older healthy adults. Curr. Eye Res.49 (8), 888–894. 10.1080/02713683.2024.2346538
54
Sparling P. B. Cantwell J. D. Dolan C. M. Niederman R. K. (1990). Strength training in a cardiac rehabilitation program: a six-month follow-up. Archives Phys. Med. Rehabilitation71 (2), 148–152. Available online at: https://pubmed-ncbi-nlm-nih-gov.eux.idm.oclc.org/2302049/.
55
Steen B. (1988). Body composition and aging. Nutr. Rev.46 (2), 45–51. 10.1111/j.1753-4887.1988.tb05386.x
56
Venturelli M. Cè E. Limonta E. Schena F. Caimi B. Carugo S. et al (2015). Effects of endurance, circuit, and relaxing training on cardiovascular risk factors in hypertensive elderly patients. Age (Dordr)37 (5), 101. 10.1007/s11357-015-9835-4
57
Vincent K. R. Braith R. W. (2002). Resistance exercise and bone turnover in elderly men and women. Med. Sci. Sports Exerc.34 (1), 17–23. 10.1097/00005768-200201000-00004
58
Vlachopoulos C. Aznaouridis K. Terentes-Printzios D. Ioakeimidis N. Stefanadis C. (2012). Prediction of cardiovascular events and all-cause mortality with brachial-ankle elasticity index: a systematic review and meta-analysis. Hypertension60 (2), 556–562. 10.1161/hypertensionaha.112.194779
59
Waller M. Miller J. Hannon J. (2011). Resistance circuit training: its application for the adult population. Strength Cond. J.33 (1), 16–22. 10.1519/ssc.0b013e3181f45179
60
Westhoff T. H. Franke N. Schmidt S. Vallbracht-Israng K. Meissner R. Yildirim H. et al (2007). Too old to benefit from sports? The cardiovascular effects of exercise training in elderly subjects treated for isolated systolic hypertension. Kidney Blood Press. Res.30 (4), 240–247. 10.1159/000104093
61
Wu S. Jin C. Li S. Zheng X. Zhang X. Cui L. et al (2019). Aging, arterial stiffness, and blood pressure association in Chinese adults. Hypertension73 (4), 893–899. 10.1161/hypertensionaha.118.12396
Summary
Keywords
community-dwelling, aging, resistance training, cardiovascular health, body composition
Citation
Hu Z, Jiang S, Hu C, Shen B and Gu J (2025) The effects of circuit-based resistance training on blood pressure, arterial stiffness, and body composition in community-dwelling older adults: a systematic review and meta-analysis. Front. Physiol. 16:1609013. doi: 10.3389/fphys.2025.1609013
Received
09 April 2025
Accepted
08 May 2025
Published
20 May 2025
Volume
16 - 2025
Edited by
Mário Cunha Espada, Instituto Politecnico de Setubal (IPS), Portugal
Reviewed by
Yu Lun Tai, Texas A&M University Central Texas, United States
Henhen Heryaman, Padjadjaran University, Indonesia
Updates
Copyright
© 2025 Hu, Jiang, Hu, Shen and Gu.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jinfa Gu, gujinfa@student.usm.my
ORCID: Jinfa Gu, orcid.org/0009-0006-8260-2145
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.