- 1Research Center for Psychological and Health Sciences, China University of Geosciences, Wuhan, China
- 2Affiliated Wuhan Mental Health Center, Tongji Medical College of Huazhong University of Science and Technology, Wuhan, China
- 3Peking University Clinical Research Institute, Peking University Health Science Center, Beijing, China
- 4Department of Psychiatry, The First Affiliated Hospital of Kunming Medical University, Kunming, China
Background: Cigarette smoking is associated with sexual dysfunction in the general population. Both smoking and sexual dysfunction are common in heroin-dependent patients (HDPs) receiving methadone maintenance treatment (MMT), but their association in MMT HDPs is rarely studied. This study examined the association between smoking and sexual dissatisfaction in Chinese HDPs receiving MMT.
Methods: In total, 480 Chinese HDPs, who had sex with their regular or irregular sex partners within one month prior to the study, were included from three MMT clinics in Wuhan, China. Sexual dissatisfaction was assessed with one single question. Socio-demographic and clinical data and smoking characteristics were collected with a standardized questionnaire. Multiple binary logistic regression was used to analyze the association between smoking and sexual dissatisfaction, as well as the associations between levels of smoking and nicotine dependence and sexual dissatisfaction.
Results: The prevalence of current smoking was 95.6% in HDPs receiving MMT. Rates of sexual dissatisfaction were higher in current smokers than non-smokers (32.9% vs. 14.3%) with a borderline significant P value of 0.074. After adjusting potential socio-demographic and clinical confounders, current smoking was significantly linked to sexual dissatisfaction (OR = 1.95, P = 0.026), and heavy smoking and severe nicotine dependence were significantly linked to sexual dissatisfaction (OR = 1.80, P = 0.025; OR = 3.27, P < 0.001).
Conclusion: Smoking is significantly associated with sexual dysfunction in HDPs receiving MMT. It deserves further investigation as to whether quitting smoking can improve the sexual function of methadone-maintained patients.
Introduction
Cigarette smoking is a major risk factor for elevated mortality and a variety of physical morbidities, including cardiovascular and respiratory diseases, cancer, and diabetes (1–4). Smoking also adversely affects sexual health. For example, cross-sectional and prospective studies have confirmed the independent contribution of smoking to the presence of sexual dysfunction in both men and women, and there is a dose-response relationship between cigarette exposure and the risk of sexual dysfunction (5–9). Further, growing evidence has shown significant improvement in sexual function as a result of smoking cessation (10–12).
Sexual dysfunction is highly prevalent among heroin-dependent patients (HDPs) receiving methadone maintenance treatment (MMT). For example, 66.3% and 77.5% men under MMT had sexual disorders and erectile dysfunction, respectively, while in women under MMT, 23.1% reported some forms of sexual dysfunction and 22.9% were dissatisfied with their sexual lives (13–15). Empirical studies have demonstrated that sexual dysfunction is one of the most important causes for patients’ early dropout from MMT, poor intimate relationships, and low quality of life (16–18). Due to these reasons, sexual dysfunction has been recognized as a major challenge in the clinical management of methadone-maintained HDPs.
The etiology of sexual dysfunction is complex, in particular regarding the sexual problems of patients diagnosed with heroin dependence and receiving opioid replacement therapy (ORT) (19). Commonly reported risk factors for sexual dysfunction in the general population include old age, unemployment, diabetes, heart disease, urinary tract disorders, depression, obesity, and smoking (1, 20, 21). A few recent studies have examined factors associated with sexual dysfunction in patients receiving ORT and they found that, in addition to some common factors such as old age and poor physical health, treatment-related factors such as opioid maintenance dosage and clinical factors such as pain and sleep disturbance also significantly contributed to sexual dysfunction within this patient population (17, 22–25). Nevertheless, because of the limited number of related studies, risk factors for sexual problems of methadone-maintained patients has not been fully elucidated (22).
Smoking is an extremely common health risk behavior in HDPs receiving MMT, with a prevalence of 87.2%–98.1% (26–28). Given the high prevalence of smoking and sexual dysfunction in methadone-maintained HDPs and the significant link between smoking and sexual dysfunction in the general population, we speculate that smoking is significantly associated with sexual dysfunction of methadone-maintained HDPs. However, to our knowledge, this relationship is rarely studied in MMT patients. Addressing smoking as a preventable and modifiable risk factor is a potentially useful strategy to reduce or relieve the sexual problems of MMT patients. The present study examined the relationship between smoking and sexual dissatisfaction in a sample of Chinese methadone-maintained HDPs.
Materials and Methods
Subjects
This study was a secondary data analysis using data from a large-scale cross-sectional survey, which determined the quality of life, mental health, sexual life satisfaction, and non-fatal suicidal behaviors of patients of three MMT clinics in Wuhan, China, from June 2009 to July 2010 (22, 25, 29–31). To be eligible for the current analysis, patients must be 20 years or older, be taking methadone orally at the three MMT clinics, meet DSM-IV diagnostic criteria for lifetime heroin dependence, and must have had sex with their regular or irregular sex partners within one month prior to the survey. We excluded patients with severe physical illnesses, alcohol dependence, organic mental disorders, or psychotic symptoms. During the survey period, a total of 749 patients were receiving treatment at the three MMT clinics and screened for eligibility, of which 519 fulfilled the inclusion criteria and 480 finally provided complete questionnaire data.
The study protocol was approved by the Ethical Review Board of Wuhan Mental Health Center. Declarations of anonymity and confidentiality had been made and all subjects provided written informed consent before the formal survey.
Instruments and Procedures
We used a standardized self-report questionnaire to collect data. Before the formal study, a pilot study was carried out among a sample of 48 MMT HDPs to test our data collection procedure for feasibility. After the pilot study, necessary amendments were also made to the questionnaire to ensure its acceptability and feasibility.
The formal questionnaire consisted of the following parts: 1) socio-demographics such as sex and age; 2) clinical characteristics including the main route of past heroin administration, length of heroin use, MMT duration, methadone dosage, and depressive symptoms; 3) sexual life satisfaction; and 4) characteristics of smoking including the number of cigarettes smoked daily (NCSD) and nicotine dependence.
Depressive symptoms were assessed with the validated Chinese version of the Zung’s Self-rating Depression Scale (SDS), which has 20 items, each scored on a four-point Likert scale. Its total score ranges from 20 to 80, with a score of 40 and above denoting clinically significant depressive symptoms (32).
Sexual life satisfaction was assessed with a single-item question: “Over the past month, how satisfied have you been with your overall sexual life?” Respondents were asked to rate on a five-point scale (1 = very dissatisfied, 2 = dissatisfied, 3 = fair, 4 = satisfied, and 5 = very satisfied). This simple measure of sexual function has been widely used in existing epidemiological studies of sexual health with satisfactory reliability and validity (15, 33, 34). Unlike other scales, which often assess the sexual function of one sex only, this single item has the advantage of measuring sexual function of both sexes (25). In our pilot study, the validity of this measure was tested by correlating its score with the four subscale scores of the Scale for Quality of Sexual Function. Results showed moderate-to-high correlations between the two scales, indicating that the satisfactory validity of this single-item measure (22, 25). Consistent with prior studies, respondents were categorized as having sexual dissatisfaction if they rated their sexual life as “very dissatisfied” and “dissatisfied.”
In this study, current smokers were defined as those who were currently smoking one or more cigarette a day and had smoked for at least half a year (35). Based on NCSD, current smokers were divided into light (<10/day), moderate (10–19/day), and heavy smokers (>19/day) (35). Nicotine dependence was assessed with the Chinese Fagerstrom Test for Nicotine Dependence (FTND), which consists of six questions (36). The FTND score ranges from 0 to 10, with 0–4, 5, and 6–10 representing mild, moderate, and severe levels of nicotine dependence, respectively (37).
Six treating psychiatrists of the HDPs of the three MMT clinics, were trained to be the survey investigators. These investigators invited eligible patients to join the study, read out questions for patients who had difficulties in completing the questionnaire, and checked answers in the questionnaire individually for logic errors or missing values before collection.
Statistical Analysis
Prevalence rates of sexual dissatisfaction according to smoking characteristics were calculated. Socio-demographic and clinical characteristics of smokers and non-smokers compared by χ2 test. Because smokers and non-smokers were not comparable in terms of some socio-demographic and clinical variables, the smoking-sexual dissatisfaction association was tested with multiple binary logistic regression model, which entered sexual satisfaction as the outcome variable, smoking status as the predictor, and socio-demographic and clinical variables at once to adjust for the potential confounding effects of these socio-demographic and clinical factors. By using the sample of smokers and the same analytic procedures, two multiple binary logistic regression models (one included the level of smoking as the predictor, and the other included the level of nicotine dependence as the predictor) were established to further examine the relationships between the two variables and sexual satisfaction. We used odds ratios (ORs) and 95% confidence intervals (CIs) to quantify the associations between variables and sexual satisfaction. The statistical significance level was set at P < 0.05 (two-sided). SPSS software version 15.0 package (SPSS Inc, Chicago, IL) was used for all analyses.
Results
The average age of the 480 MMT HDPs was 38.3 years (range: 21–59 years), and 31.0% were females. In total, 154 patients (32.1%) were dissatisfied with their sexual life and 459 patients (95.6%) were current smokers. Numbers of light, moderate, and heavy smokers were 117 (25.5%), 99 (21.6%), and 243 (52.9%), respectively. Numbers of smokers who were mildly, moderately, and severely dependent to nicotine were 102 (22.2%), 69 (15.0%), and 188 (62.7%), respectively. Detailed socio-demographic and clinical characteristics of the patient sample were shown in Table 1.
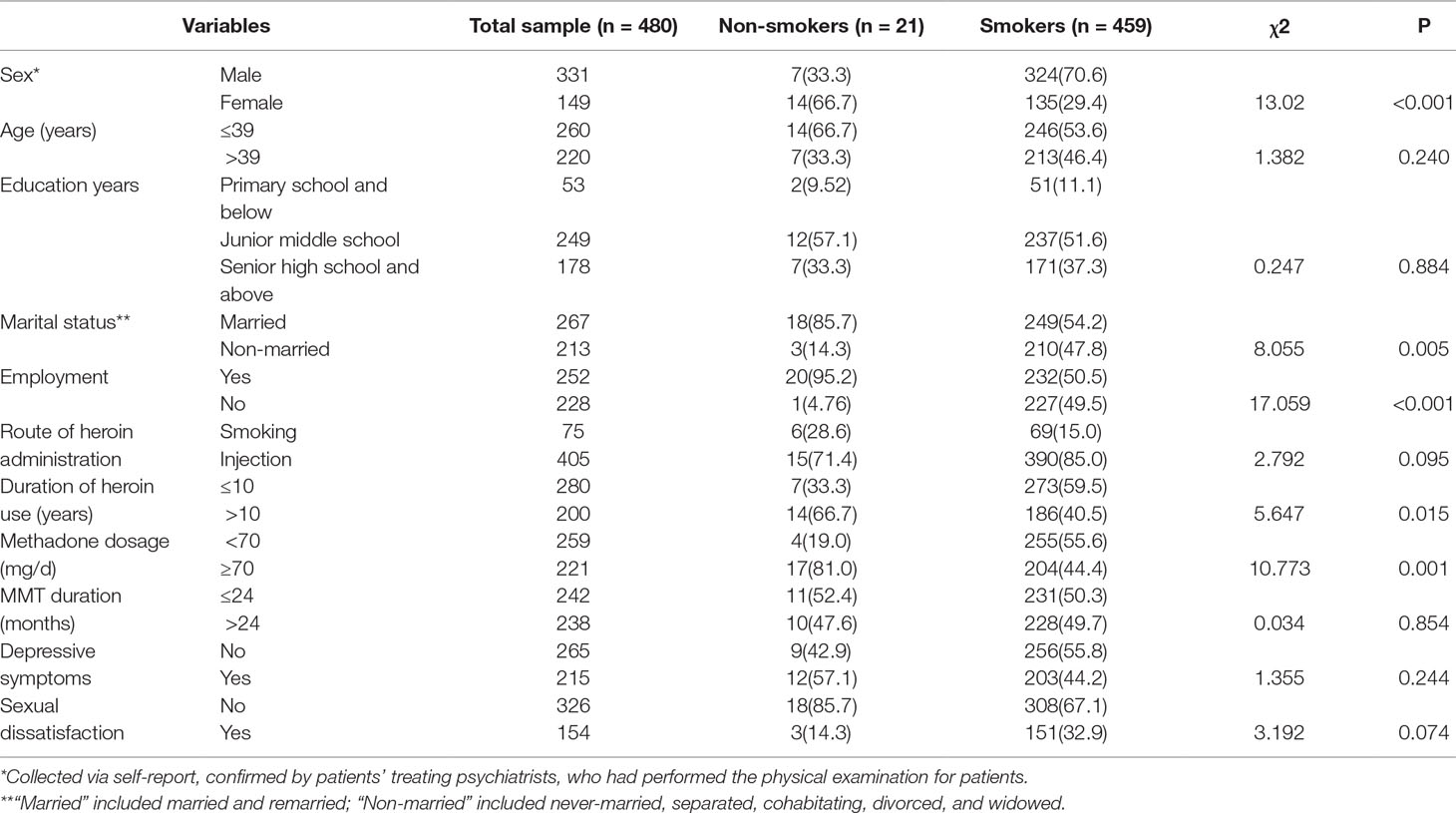
Table 1 Characteristics of methadone-maintained heroin-dependent patients, spitted by smoking status.
The prevalence rates of sexual dissatisfaction were higher in current smokers than non-smokers (32.9% vs. 14.3%) with a borderline significant P value of 0.074. As shown in Table 1, compared to non-smokers, smokers were more likely to be males, be non-married, be unemployed, have a short duration of heroin use, and take a low dose of methadone. After adjusting for socio-demographic and clinical factors (Table 2), current smoking was significantly linked to sexual dissatisfaction (OR = 1.95, P = 0.026).
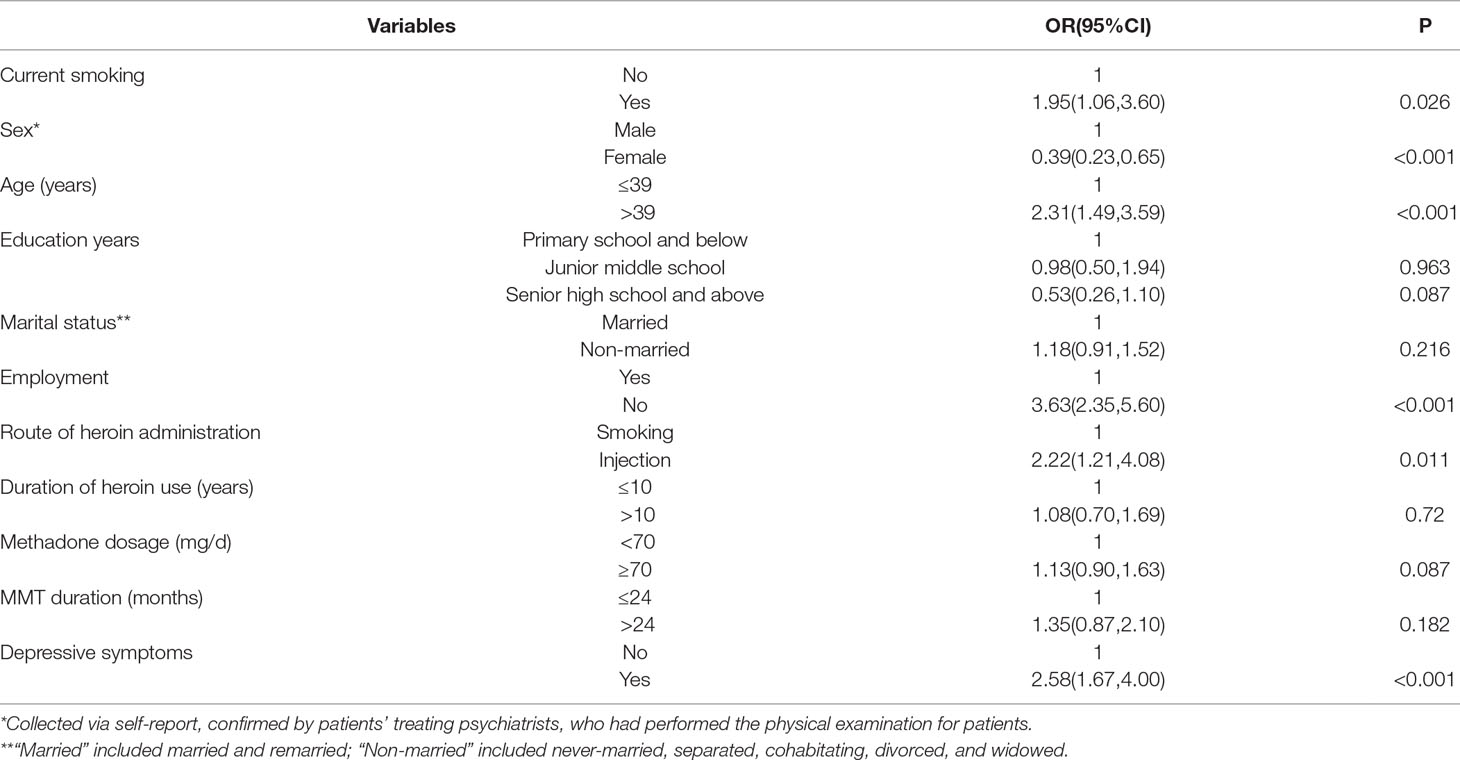
Table 2 Multiple binary logistic regression on the association between smoking and sexual dissatisfaction in methadone-maintained heroin-dependent patients, controlling for socio-demographic and clinical factors.
Socio-demographic and clinical characteristics of the 459 smokers were displayed in Table 3. Overall, rates of sexual dissatisfaction in smokers increased with levels of smoking (light: 23.9%, moderate: 28.3%, heavy: 39.1%; P = 0.008) and nicotine dependence (mild: 15.7%, moderate: 24.6%, severe: 41.6%; P < 0.001). After adjusting for socio-demographic and clinical factors (Table 3), both heavy smoking and severe nicotine dependence were significantly linked to sexual dissatisfaction (OR = 1.80, P = 0.025; OR = 3.27, P < 0.001).
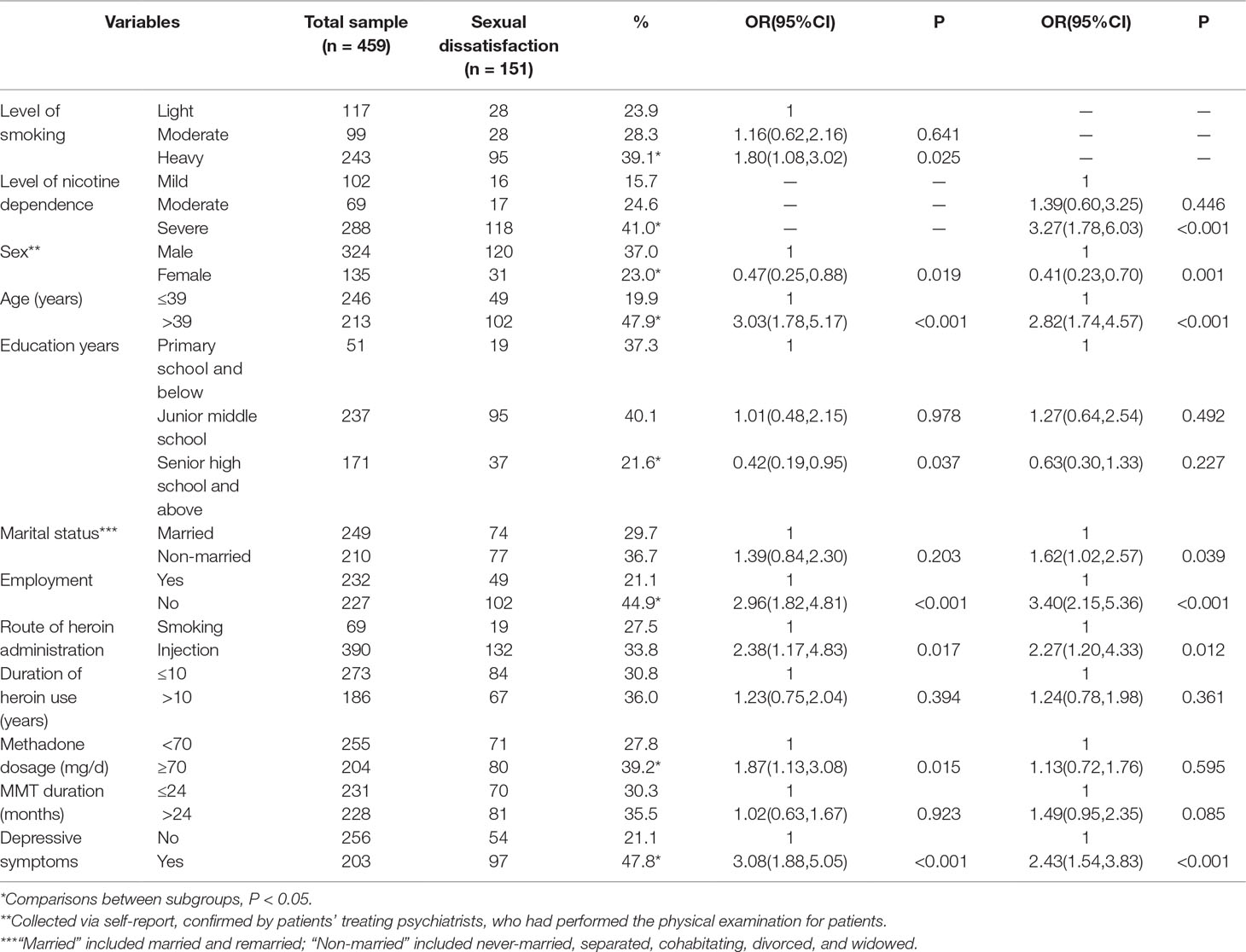
Table 3 Characteristics of methadone-maintained heroin-dependent smokers, and multiple binary logistic regression on the associations between levels of smoking and nicotine dependence and sexual dissatisfaction.
Discussion
To the best of our knowledge, this is the first large-scale study that is specifically designed to examine the association between smoking behavior and sexual dysfunction of Chinese HDPs receiving MMT. We found a 95.6% prevalence of current smoking in Chinese MMT patients, which is consistent with the high smoking rates among patients receiving ORT in other countries (87.2%–98.1%) (26, 28), suggesting that smoking is also a very common issue in HDPs of Chinese MMT clinics. Results of our multiple regression analysis revealed a 1.95 times risk of sexual dissatisfaction in heroin-dependent smokers than non-smokers of MMT clinics, replicating the higher risk of sexual dysfunction in smokers than non-smokers in the general population (5–9). This association was further strengthened by the significantly higher risk of sexual dissatisfaction in heavy than in light smokers (OR = 1.80) and in severely than in mildly nicotine-dependent smokers (OR = 3.27), after controlling for potential socio-demographic and clinical confounders.
Psychopharmacological studies have found that nicotine is a potent parasympathomimetic stimulant, which can stimulate nicotinic acetylcholine receptors in the central nervous system and promote the release of excitatory neurotransmitters (i.e., acetylcholine, serotonin, norepinephrine, and dopamine) and beta-endorphin, resulting in mood-altering and analgesic effects (38–40). There is convincing evidence that a large proportion of MMT patients, although they have stopped using heroin, are still suffering from prolonged withdrawal symptoms of heroin dependence such as depression and physical pain (27, 30). Accordingly, an empirical study has found that the main reason for smoking in heroin users was “to maintain pleasure” (41). Therefore, MMT patients may smoke to obtain nicotine to reduce or relieve withdrawal symptoms. This could explain the very high rate of smoking in MMT patients.
Although cigarette smoking has a potentially beneficial effect on the withdrawal symptoms of MMT HDPs, heavy metals in tobacco smoke can also lead to elevated levels of reproductive toxic chemicals in the blood, such as lead and cadmium (42). The accumulation of the two chemicals in the body would directly damage gonadal cells and tissues and cause sexual dysfunction (43, 44). The second possible mechanism underlying the smoking-sexual dissatisfaction is the sexual hormone imbalances resulting from the dysregulation of the hypothalamic–pituitary–gonadal (HPG) axis (45–47). For example, smoking may inhibit the ovarian function and lower the level of estrogen, which is related to the higher risk of female sexual dysfunction (5, 48). Third, smoking could impair the endothelial function of arterial vessels and promote the stiffness of genital vessels, resulting in alterations in the blood flow to genital organs (49, 50). This affects, for example, blood flow to the penis, which is critical for initiating an erection (8).
Findings from pharmacological studies have shown that methadone and other opioids could suppress the release of gonadal hormones via its inhibitory effect on HPG axis, including testosterone, which plays a critical role in maintaining sexual desire in both men and women (51–55). Therefore, in the clinical management of heroin addiction, sexual dysfunction is generally considered as one of the most common side effects associated with methadone treatment (25, 56), as confirmed by the significant association between a high dose of methadone and sexual dissatisfaction in Table 3 of the present report. However, findings from recent studies and the current study indicate that sexual dysfunction is the result of multiple factors including methadone treatment, clinical variables and cigarette smoking (17, 22–25). In this study, we found not only the significant association between smoking and sexual dissatisfaction but also the greater risk of sexual dissatisfaction in heavy smokers (relative to light smokers) and severe nicotine-dependent smokers (relative to mild nicotine-dependent smokers); the latter finding is in line with the dose-response relationship between cigarette exposure and sexual dysfunction reported in the general population (5).
This study has some limitations. First, data of this study were collected cross-sectionally; therefore, the causality of the relationship between smoking and sexual dissatisfaction needs to be further examined in longitudinal studies. Second, we did not measure the levels of blood sex hormones and nicotine; so the biological mechanisms underlying the smoking-sexual function link could not be determined. Third, since this was a self-report questionnaire survey, the prevalence of sexual dissatisfaction might be underestimated due to social desirability bias, that is, patients are more likely to under-report “bad behaviors” such as sexual dissatisfaction. Fourth, some other potential factors associated with sexual dissatisfaction such as the relationship with sex partners, number of sex partners, organic diseases (i.e., vascular disease and Peyronie’s disease), and the use of antidepressants were not measured and controlled in our adjustment analyses. It is uncertain whether or not these factors would influence the association between smoking and sexual dissatisfaction. Fifth, our study only assessed the association of smoking with an overall indicator of sexual dysfunction, sexual dissatisfaction. No data are available on the associations of smoking with specific types of sexual dysfunction such as desire and arousal disorders. Further studies are warranted to examine these associations. Finally, given the significant sex difference in the prevalence of sexual dissatisfaction, it would be more informative to present results on the smoking-sexual dissatisfaction relationship by sex. However, multiple analyses according to sex are not feasible due to the very small sample size of female patients with sexual dissatisfaction (n = 31). In this case, we had to use a combined sample of male and female patients to examine the smoking-sexual dissatisfaction relationship. Such aggregate-level results might mask the sex difference in smoking-sexual dissatisfaction relationship. Large-scale studies are needed to test whether the smoking-sexual dissatisfaction association differs between male and female patients.
In China, smoking is often regarded as a normal and socially acceptable behavior (57); thus, Chinese psychiatric physicians and nurses of MMT clinics seldom advise their patients to quit smoking. This study demonstrated the significant relationship between smoking and sexual dissatisfaction in Chinese HDPs receiving MMT, as well as the higher likelihood of sexual dissatisfaction in heavy smokers and severely nicotine-dependent smokers. Our findings may suggest the importance of smoking cessation for the clinical management of sexual dysfunction in Chinese MMT clinics. It is necessary to conduct further interventional studies to examine whether quitting smoking can improve the sexual satisfaction of methadone-maintained patients.
Ethics Statement
The study protocol was approved by the Ethical Review Board of Wuhan Mental Health Center. Declarations of anonymity and confidentiality had been made and all subjects provided written informed consent before the formal survey.
Author Contributions
JL and B-LZ were responsible for the design of the study and interpretation of data, W-XX and B-LZ for the manuscript draft and statistical analysis, Y-MX for the data collection and critical revision of the manuscript, and W-XX for statistical consultation, data extraction, and processing. All authors reviewed the data and analysis, revised the manuscript, had full access to all of the data in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis, and had authority over approval of final manuscript version and the decision to submit for publication.
Funding
This study was funded by the Subject Leadership Training Programme for Medicine Discipline of Health and Family Planning Commission of Yunnan Province (D-2017048, JL, PI), Health and Family Planning Commission of Yunnan Province [2016NS027, JL, PI], and Wuhan Health and Family Planning Commission [WX17Q30, YM Xu, PI; WG16A02, BL Zhong, PI]. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors thank all the patients involved in this study for their cooperation and support.
References
1. Kunutsor SK, Spee JM, Kieneker LM, Gansevoort RT, Dullaart RPF, Voerman AJ, et al. Self-reported smoking, urine cotinine, and risk of cardiovascular disease: findings from the PREVEND (Prevention of Renal and Vascular End-Stage Disease) prospective cohort study. J Am Heart Assoc (2018) 7(10):e008726. doi: 10.1161/JAHA.118.008726
2. Haddad L, Kelly DL, Weglicki LS, Barnett TE, Ferrell AV, Ghadban R. A systematic review of effects of waterpipe smoking on cardiovascular and respiratory health outcomes. Tob Use Insights (2016) 9:13–28. doi: 10.4137/TUI.S39873
3. Akter S, Goto A, Mizoue T. Smoking and the risk of type 2 diabetes in Japan: a systematic review and meta-analysis. J Epidemiol (2017) 27(12):553–61. doi: 10.1016/j.je.2016.12.017
4. Brookman-May SD, Campi R, Henriquez JDS, Klatte T, Langenhuijsen JF, Brausi M, et al. Latest evidence on the impact of smoking, sports, and sexual activity as modifiable lifestyle risk factors for prostate cancer incidence, recurrence, and progression: a systematic review of the literature by the european association of urology section of oncological urology (ESOU). Eur Urol Focus (2018). doi: 10.1016/j.euf.2018.02.007
5. Choi J, Shin DW, Lee S, Jeon MJ, Kim SM, Cho B, et al. Dose-response relationship between cigarette smoking and female sexual dysfunction. Obstet Gynecol Sci (2015) 58(4):302–8. doi: 10.5468/ogs.2015.58.4.302
6. Biebel MG, Burnett AL, Sadeghi-Nejad H. Male sexual function and smoking. Sex Med Rev (2016) 4(4):366–75. doi: 10.1016/j.sxmr.2016.05.001
7. Lam TH, Abdullah AS, Ho LM, Yip AW, Fan S. Smoking and sexual dysfunction in Chinese males: findings from men’s health survey. Int J Impot Res (2006) 18(4):364–9. doi: 10.1038/sj.ijir.3901436
8. Verze P, Margreiter M, Esposito K, Montorsi P, Mulhall J. The link between cigarette smoking and erectile dysfunction: a systematic review. Eur Urol Focus (2015) 1(1):39–46. doi: 10.1016/j.euf.2015.01.003
9. Wen LM, Rissel C, Cheng Y, Richters J, de Visser RO. Tobacco smoking and sexual difficulties among Australian adults: a cross-sectional study. Sex Health (2017) 14(4):313–9. doi: 10.1071/SH17005
10. Pourmand G, Alidaee MR, Rasuli S, Maleki A, Mehrsai A. Do cigarette smokers with erectile dysfunction benefit from stopping?: a prospective study. BJU Int (2004) 94(9):1310–3. doi: 10.1111/j.1464-410X.2004.05162.x
11. Harte CB, Meston CM. Association between smoking cessation and sexual health in men. BJU Int (2012) 109(6):888–96. doi: 10.1111/j.1464-410X.2011.10503.x
12. Safavy S, Kilday PS, Slezak JM, Abdelsayed GA, Harrison TN, Jacobsen SJ, et al. Effect of a smoking cessation program on sexual function recovery following robotic prostatectomy at kaiser permanente southern California. Perm J (2017) 21:16–138. doi: 10.7812/TPP/16-138
13. Babakhanian M, Haghdoost AA, Afshari M, Taghizadeh F, Moosazadeh M. Methadone replacement therapy and sexual disorders among opium dependent iranian men: a meta-analysis study. Addict Health (2017) 9(1):1–10. doi: 10.22122/ahj.v9i1.400
14. Kheradmand A, Amini Ranjbar Z, Zeynali Z, Sabahy AR, Nakhaee N. Sleep quality and sexual function in patients under methadone maintenance treatment. Int J High Risk Behav Addict (2015) 4(4):e23550. doi: 10.5812/ijhrba.23550
15. Shan J, Chen G, Kong Y, Zhang B, Xu Q, Cui M, et al. Sexual satisfaction and its related factors among heroin-dependent women receiving methadone maintenance treatment. Chin J Behav Med & Brain Sci (2015) 24(7):625–8. doi: 10.3760/cma.j.issn.1674-6554.2015.07.014
16. Xia Y, Zhang D, Li X, Chen W, He Q, Jahn HJ, et al. Sexual dysfunction during methadone maintenance treatment and its influence on patient’s life and treatment: a qualitative study in South China. Psychol Health Med (2013) 18(3):321–9. doi: 10.1080/13548506.2012.729845
17. Yee A, Loh HS, Ng CG, Sulaiman AH. Sexual desire in opiate-dependent men receiving methadone-assisted treatment. Am J Mens Health (2018) 12(4):1016–22. doi: 10.1177/1557988318759197
18. Yee A, Danaee M, Loh HS, Sulaiman AH, Ng CG. Sexual dysfunction in heroin dependents: a comparison between methadone and buprenorphine maintenance treatment. PLoS One (2016) 11(1):e0147852. doi: 10.1371/journal.pone.0147852
19. Kumsar NA, Kumsar S, Dilbaz N. Sexual dysfunction in men diagnosed as substance use disorder. Andrologia (2016) 48(10):1229–35. doi: 10.1111/and.12566
20. McCabe MP, Sharlip ID, Lewis R, Atalla E, Balon R, Fisher AD, et al. Risk factors for sexual dysfunction among women and men: a consensus statement from the fourth international consultation on sexual medicine 2015. J Sex Med (2016) 13(2):153–67. doi: 10.1016/j.jsxm.2015.12.015
21. Lewis RW, Fugl-Meyer KS, Bosch R, Fugl-Meyer AR, Laumann EO, Lizza E, et al. Epidemiology/risk factors of sexual dysfunction. J Sex Med (2004) 1(1):35–9. doi: 10.1111/j.1743-6109.2004.10106.x
22. Zhang HS, Xu YM, Zhu JH, Zhong BL. Poor sleep quality is significantly associated with low sexual satisfaction in Chinese methadone-maintained patients. Medicine (Baltimore) (2017) 96(39):e8214. doi: 10.1097/MD.0000000000008214
23. Lugoboni F, Zamboni L, Federico A, Tamburin S, Gruppo Inter SdCS. Erectile dysfunction and quality of life in men receiving methadone or buprenorphine maintenance treatment. A cross-sectional multicentre study. PLoS One (2017) 12(11):e0188994. doi: 10.1371/journal.pone.0188994
24. Teoh JB, Yee A, Danaee M, Ng CG, Sulaiman AH. Erectile dysfunction among patients on methadone maintenance therapy and its association with quality of Life. J Addict Med (2017) 11(1):40–6. doi: 10.1097/ADM.0000000000000267
25. Zhong BL, Xu YM, Zhu JH, Li HJ. Sexual life satisfaction of methadone-maintained Chinese patients: individuals with pain are dissatisfied with their sex lives. J Pain Res (2018) 11:1789–94. doi: 10.2147/JPR.S177564
26. Do HP, Nguyen LH, Thi Nguyen NP, Ngo C, Thi Nguyen HL, Le GT, et al. Factors associated with nicotine dependence during methadone maintenance treatment: findings from a multisite survey in Vietnam. BMJ Open (2017) 7(7):e015889. doi: 10.1136/bmjopen-2017-015889
27. Liu LZ, Tan LX, Xu YM, Liu XB, Chen WC, Zhu JH, et al. Significantly more intense pain in methadone-maintained patients who are addicted to nicotine. Oncotarget (2017) 8(36):60576–80. doi: 10.18632/oncotarget.19222
28. Pajusco B, Chiamulera C, Quaglio G, Moro L, Casari R, Amen G, et al. Tobacco addiction and smoking status in heroin addicts under methadone vs. Int J Environ Res Public Health (2012) 9(3):932–42. doi: 10.3390/ijerph9030932
29. Zhong BL, Xu YM, Zhu JH, Liu XJ. Non-suicidal self-injury in Chinese heroin-dependent patients receiving methadone maintenance treatment: prevalence and associated factors. Drug Alcohol Depend (2018) 189:161–5. doi: 10.1016/j.drugalcdep.2018.05.006
30. Yang YJ, Xu YM, Chen WC, Zhu JH, Lu J, Zhong BL. Prevalence of pain and its socio-demographic and clinical correlates among heroin-dependent patients receiving methadone maintenance treatment. Sci Rep (2017) 7(1):8840. doi: 10.1038/s41598-017-09404-w
31. Zhong BL, Xu YM, Xie WX, Lu J, Yu WB, Yan J. Alcohol drinking in chinese methadone-maintained clients: a self-medication for depression and anxiety? J Addict Med (2019). doi: 10.1097/ADM.0000000000000500
32. Wang XD, X.L. W, Ma H. Rating scales for mental health. Chin Ment Health J (1999) 13(Suppl):122–4.
33. Ji F, Jiang D, Lin X, Zhang W, Zheng W, Cheng C, et al. Sexual life satisfaction and its associated socio-demographic and workplace factors among Chinese female nurses of tertiary general hospitals. Oncotarget (2017) 8(33):54472–7. doi: 10.18632/oncotarget.17664
34. Kim O, Jeon HO. Gender differences in factors influencing sexual satisfaction in Korean older adults. Arch Gerontol Geriatr (2013) 56(2):321–6. doi: 10.1016/j.archger.2012.10.009
35. World Health Organization. WHO report on the global tobacco epidemic, 2009: implementing smoke – free environments. Geneva: World Health Organization Press (2010). http://whqlibdoc.who.int/publications/2009/9789241563918_eng_full.pdf?ua=1
36. Wang Y, Li X, Huang Z, Li Y, Gao B. The chinese version of fagerstrom test for nicotine dependence scale for cigarette smokers from methadone maintenance treatment outpatient clinics: a reliability and validity study. Chin J Drug Depend (2012) 21(6):439–43. doi: 10.3969/j.issn.1007-9718.2012.06.009
37. Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The fagerstrom test for nicotine dependence: a revision of the fagerstrom tolerance questionnaire. Br J Addict (1991) 86(9):1119–27. doi: 10.1111/j.1360-0443.1991.tb01879.x
38. Picciotto MR, Lewis AS, van Schalkwyk GI, Mineur YS. Mood and anxiety regulation by nicotinic acetylcholine receptors: a potential pathway to modulate aggression and related behavioral states. Neuropharmacology (2015) 96(Pt B):235–43. doi: 10.1016/j.neuropharm.2014.12.028
39. Cao YJ, Surowy CS, Puttfarcken PS. Nicotinic acetylcholine receptor-mediated [3H]dopamine release from hippocampus. J Pharmacol Exp Ther (2005) 312(3):1298–304. doi: 10.1124/jpet.104.076794
40. Gudehithlu KP, Duchemin AM, Tejwani GA, Neff NH, Hadjiconstantinou M. Nicotine-induced changes of brain beta-endorphin. Neuropeptides (2012) 46(3):125–31. doi: 10.1016/j.npep.2012.03.001
41. Liu S, Zhou W, Zhang J, Wang Q, Xu J, Gui D. Differences in cigarette smoking behaviors among heroin inhalers versus heroin injectors. Nicotine Tob Res (2011) 13(11):1023–8. doi: 10.1093/ntr/ntr115
42. Ashraf MW. Levels of heavy metals in popular cigarette brands and exposure to these metals via smoking. Sci World J (2012) 2012:729430. doi: 10.1100/2012/729430
43. Nampoothiri LP, Gupta S. Simultaneous effect of lead and cadmium on granulosa cells: a cellular model for ovarian toxicity. Reprod Toxicol (2006) 21(2):179–85. doi: 10.1016/j.reprotox.2005.07.010
44. Pandya C, Pillai P, Nampoothiri LP, Bhatt N, Gupta S, Gupta S. Effect of lead and cadmium co-exposure on testicular steroid metabolism and antioxidant system of adult male rats. Andrologia (2012) 44(Suppl 1):813–22. doi: 10.1111/j.1439-0272.2010.01137.x
46. Kapoor D, Jones TH. Smoking and hormones in health and endocrine disorders. Eur J Endocrinol (2005) 152(4):491–9. doi: 10.1530/eje.1.01867
47. Jandikova H, Duskova M, Starka L. The influence of smoking and cessation on the human reproductive hormonal balance. Physiol Res (2017) 66(Suppl 3):S323–31. http://www.biomed.cas.cz/physiolres/pdf/2017/66_S323.pdf
48. Dennerstein L, Randolph J, Taffe J, Dudley E, Burger H. Hormones, mood, sexuality, and the menopausal transition. Fertil Steril (2002) 77(Suppl 4):S42–8. doi: 10.1016/S0015-0282(02)03001-7
49. Simonsen U, Garcia-Sacristan A, Prieto D. Penile arteries and erection. J Vasc Res (2002) 39(4):283–303. doi: 10.1159/000065541
50. Huang YC, Chin CC, Chen CS, Shindel AW, Ho DR, Lin CS, et al. Chronic cigarette smoking impairs erectile function through increased oxidative stress and apoptosis, decreased nNOS, endothelial and smooth muscle contents in a rat Mmodel. PLoS One (2015) 10(10):e0140728. doi: 10.1371/journal.pone.0140728
51. Brown RT, Zueldorff M. Opioid substitution with methadone and buprenorphine: sexual dysfunction as a side effect of therapy. Heroin Addict Relat Clin Probl (2007) 9(1):35–44. https://www.gacguidelines.ca/site/GAC_Guidelines/assets/pdf/104_Brown_2007.pdf
52. Kingsberg S. Testosterone treatment for hypoactive sexual desire disorder in postmenopausal women. J Sex Med (2007) 4(Suppl 3):227–34. doi: 10.1111/j.1743-6109.2007.00449.x
53. Tenhola H, Sinclair D, Alho H, Lahti T. Effect of opioid antagonists on sex hormone secretion. J Endocrinol Invest (2012) 35(2):227–30. doi: 10.3275/8181
54. Bolona ER, Uraga MV, Haddad RM, Tracz MJ, Sideras K, Kennedy CC, et al. Testosterone use in men with sexual dysfunction: a systematic review and meta-analysis of randomized placebo-controlled trials. Mayo Clin Proc (2007) 82(1):20–8. doi: 10.4065/82.1.20
55. Yee A, Loh HS, Ong TA, Ng CG, Sulaiman AH. Randomized, double-blind, parallel-group, placebo-controlled trial of bupropion as treatment for methadone-emergent sexual dysfunction in men. Am J Mens Health (2018) 12(5):1705–18. doi: 10.1177/1557988318784152
56. Yee A, Loh HS, Hisham Hashim HM, Ng CG. The prevalence of sexual dysfunction among male patients on methadone and buprenorphine treatments: a meta-analysis study. J Sex Med (2014) 11(1):22–32. doi: 10.1111/jsm.12352
Keywords: smoking, sexual dysfunction, heroin dependence, methadone maintenance treatment
Citation: Zhong B-L, Xu Y-M, Xie W-X and Lu J (2019) Cigarette Smoking Is Significantly Linked to Sexual Dissatisfaction in Chinese Heroin-Dependent Patients Receiving Methadone Maintenance Treatment. Front. Psychiatry 10:306. doi: 10.3389/fpsyt.2019.00306
Received: 24 October 2018; Accepted: 17 April 2019;
Published: 22 May 2019.
Edited by:
Carlos Roncero, University of Salamanca Health Care Complex, SpainReviewed by:
Raul Felipe Palma-Alvarez, Vall d’Hebron University Hospital, SpainCélia Costa Franco, Hospital and University Center of Coimbra, Portugal
Copyright © 2019 Zhong, Xu, Xie and Lu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jin Lu, jinlu2000@163.com
 Bao-Liang Zhong
Bao-Liang Zhong Yan-Min Xu2
Yan-Min Xu2 Jin Lu
Jin Lu