- Clinical Nutrition Department, College of Applied Medical Sciences, Taibah University, Madinah, Saudi Arabia
Background: Restricted interests and repetitive behavior are characteristics of autism spectrum disorder (ASD). The likelihood that persons with ASD will respond adversely to unfamiliar situations is great. The novel coronavirus outbreak has resulted in disruptions to all aspects of routine and behavior. Hence, this study proposed to investigate the impact of the outbreak on the eating behavior and routines of children with ASD in Saudi Arabia through the perceptions of their parents.
Method: A cross-sectional study with a quantitative approach was utilized to obtain data from 150 parents of children with ASD aged ≤18 years in Saudi Arabia. The data collected included demographic data of the parents, the ASD status of the family, impact of COVID-19 to the family, eating behavior of the children with ASD, and daily routines of the children with ASD. Moreover, parents were able to provide comments regarding their children’s eating behavior or daily routines.
Results: The study found that changes in the eating behavior of children with ASD were found to differ significantly (p<0.05) based on the number of children with ASD, the age of the children with ASD, the gender of the children with ASD, and the severity of their ASD symptoms. Moreover, changes to dinner-time routines were found to differ significantly (p<0.05) based on the age of the children with ASD. Also, changes to morning routines were found to differ significantly (p<0.05) based on the age of the children with ASD, their gender, and the severity of their ASD symptoms. Additionally, impact of COVID-19 to the family had a significant impact to eating behavior and daily routines of the children with ASD.
Conclusion: This study found that the eating behavior and daily routines of children with ASD in Saudi Arabia have been considerably worsened and changed. The study recommends the collaboration of multidisciplinary teams and parents to modify or design interventions that help to change their eating behavior and routine can be implemented in the home. It also recommends the provision of virtual helplines to aid parents of children with ASD in such cases.
Introduction
As with other countries across the globe, the Kingdom of Saudi Arabia (KSA) is in the grip of the COVID-19 pandemic. Even before its first case was confirmed on March 2, 2020, the country took several measures to restrict the spread of the disease within the kingdom (1). Eventually, schools and universities were closed on March 8, 2020, together with a ban on gatherings (2). All educational institutions were included in this decision such as, private and public schools, and establishments for vocational and technical training. In their place, online teaching and home-schooling were encouraged (1). Prior research has indicated that reactive closure of schools can dilute the system of societal dealings, diminish and defer the peak of an endemic, and lessen the propagation of influenza, whether regular or epidemic (3, 4).
These measures caused a sudden change of routine for children and their parents as they are required to stay at home in response to the government’s directives for social distancing and the closure of schools. In this context, dealing with children with special needs becomes challenging for their families and caregivers. In particular, children with autism spectrum disorder (ASD) experience a considerable change in their routines. For instance, such children typically have several intervention sessions in school, with specialist therapists, or in clinics and institutes dedicated to this purpose. However, due to the measures to contain the contagion, children with ASD have encountered significant disruption to their schedules (5).
Persons with ASD often require long-term support (6) since their symptoms impact day-to-day existence (7). Moreover, their capacity to meet the demands of new situations, learning, and problem-solving are greatly limited (8). Further, there is a greater likelihood that persons with ASD will experience anxiety and depression (9, 10), which may be exacerbated by unfamiliar situations, such as a quarantine (7).
An associated concern for children with ASD is their eating behavior, as many persons with ASD are hypo- or hypersensitive to taste and touch. This indicates that they may be either oversensitive or impervious to the temperature or texture of foods and consequently finicky about food. Consequently, their diet may be restricted to certain foods or specific brands (11). Thus, restricted preferences for food (also termed selective eating, restricted variety, food selectivity, or limited food repertoire) are the problem most frequently associated with feeding in children with ASD (12–14). Prior research in an Omani context has also reported the high occurrence of food selectivity and refusal in children with ASD (15). Moreover, the findings of Vissoker et al. (16) confirmed earlier research on the greater prevalence of eating rigid patterns and eating problems in children with ASD. Further, they highlighted the role of age in this regard. For instance, food selectivity, rituals, and sameness increased with increase in age (16). On the other hand, Patton et al. (17) found that lower consumption of unfamiliar foods, a higher number of instances of behavior that disrupted mealtimes, and a higher number of commands from parents to remind children to take bites during meals were associated with greater severity of ASD (17).
Moreover, in their exploration of the mealtime behavior of children with ASD in the school setting, Padmanabhan and Shroff (18) found that such children struggled at mealtimes if the food was not to their liking, if the food was not what they preferred to eat routinely, and if there had been any change to the schedule of the break times. Further, sensitivity to the smell of food and loudness of others during break times prevented them from consuming their meals. Another facet was related to their tactile sensitivity. That is, they would not eat if the texture of the food was not to their liking (18). Huxham et al. (19) also drew attention to the preference of children with ASD for foods of a certain appearance, for instance according to food color, food presentation and the brand and packaging of food (19). Acceptance of food was also affected by the children’s sensory features and food texture. Moreover, Mayes and Zickgraf (20) reported that children with ASD had a greater likelihood of atypical eating behavior than children with ADHD or other disorders, or typically developing children (20). Atypical eating behavior included restricted preferences for food, hypersensitivity to textures of food, other odd patterns such as eating only a certain brand of food, pocketing the food instead of swallowing it, and pica. In the present spread of several epidemics, it is possible that certain foods (or brands of food) that they eat daily may not be easily accessible, which can lead to disturbances in their eating behavior (11).
In addition, Altable (11) emphasized the criticality of routines and control to persons with ASD as they can be disturbed by the minutest and most commonplace alterations (11). Thus, in the context of the COVID-19 pandemic, where routines have been impacted, there is a great likelihood that the daily routines of children with ASD will have been impacted in different ways (11). Eshraghi et al. (21) also highlighted the preoccupation with routine of children with ASD and the high probability of upheaval (emotional and behavioral) due to COVID-19 (21). In an Australian study, Marquenie et al. (22) found that the dinner-time routines of families with young children (2–5 years) with ASD were chaotic and unstructured (22). In contrast, bedtime routines were more structured and, often, non-functional. Moreover, an investigation by Colizzi et al. (23) revealed that various new needs emerged in persons with ASD due to the COVID-19 outbreak (23). For instance, they required greater healthcare support and in-home support, in particular, together with interventions to deal with the disruption caused by the quarantine. Moreover, difficulties in coping with daily activities increased and behavior problems presented more frequently or intensively in one of out of three children with ASD as a minimum. A study conducted in Italy by degli Espinosa et al. (24) highlighted how behavioral support and reinforcement for children with ASD could be provided at home by their parents during the pandemic (24). On the other hand, Stankovic et al. (25) explored the challenges encountered by the parents of children with ASD in Serbia during the COVID-19 situation and found that the absence of support and feelings of helplessness had intensified during this time (25).
Food selection and preferences in ASD
A common related facet of children with ASD, which affects 46% to 89% of such children, is eating challenges (26, 27). Sharp et al. (28, 29) reported that the probability of children with ASD experiencing a feeding problem was five times greater than of children without ASD. Research has indicated that these feeding problems could be a demonstration of the limited interests and activities characteristic of children with ASD (26). A further explanation could be that the behavior of the family could influence the feeding problems of such children either via lowered exposure to a variety of foods (30) or via unintentional support of problem behaviors concerning mealtime (31).
Field et al. (32) highlighted the specific feeding problems encountered in children with ASD. These included refusal of food, selectivity of food by type, selectivity by food by texture, oral motor delays (e.g., chewing, repositioning the tongue, lip closure, etc.), or dysphagia (challenges with swallowing). Children with ASD typically exhibited selectivity by type or texture followed by oral-motor delay leading to mechanical challenges in eating foods; and dysphagia (32). Other studies have reported severe problems with behavior at mealtime (31, 33).
A variety of challenges related to mealtime and eating is experienced by these children and the resulting difficulties can result in insufficient nutrition, disruptive behaviors at mealtime, rigid food-related routines, and intensive effort from members of the family (34–36). The occurrence of disturbances to mealtimes is due to the need of the child with ASD for greater help and supervision, a distinct meal, or since the atmosphere at mealtime is stressful as a result of the extent of attention required by the child with ASD (37).
Ausderau and Juarez (38) noted the commonness of feeding disorders in children with ASD resulting in considerable impacts to their family mealtimes. The study found that while families gave importance to mealtimes, these were often not easy to structure and frequently resulted in the mother’s exhaustion. Moreover, the children with ASD exhibited unusual preferences for food, food selectivity, and disruptive behaviors at mealtime (38). In another study, Aponte and Romanczyk (39) examined the association between feeding problems and autism severity. They found that various feeding problems and the duration of negative vocalizations during observations of meals were predicted by autism severity.
BalikçCheck that all equations and special characters are displayed correctly.i and Çiyiltepe (40) used the BAMBI (Brief Autism Mealtime Behavior Inventory) (41, 42) to study the feeding problems of children with ASD. Their study found that the feeding problems exhibited by children with ASD included behavioral problems at mealtime, such as sobbing and screaming throughout meals followed by avoidance of certain food types and textures, selectivity of type and texture, and dislike of some food types and textures (40). In another study, Bandini et al. (43) found that in contrast to children without ASD, children with ASDs displayed more food refusal and more limited repertoire of food. A later study by Bandini et al. (14) evaluated food selectivity of children with ASD in a longitudinal study. Overall, an improvement in food refusal could be seen between baseline and follow-up. However, the food repertoire namely, number of distinctive foods partaken, did not seem to increase.
In a Turkish study, Bicer and Alsaffar (12) studied the dietary intake and feeding problems of 164 children (aged 4–18 years) and reported that the most typical feeding problems of these children were consuming a restricted range of foods (food selectivity), rapid eating, and overeating. Correspondingly, common strategies adopted by parents/caregivers to address these feeding problems included distraction, permitting more drinking of fluids, and offering preferred foods. Other approaches utilized included compelling, offering rewards, wheedling, child-led feeding, giving meals a miss, chastisement, and utilizing high-calorie supplements/formula.
Mahmoud et al. (44) contrasted the feeding behavior of 35 children aged 2 - 4 years recently diagnosed with ASD with 70 children who were typically developing (TD). This study reported that children with ASD demonstrated a greater extent of challenging feeding behaviors, such as feed neophobia, consuming non-food items, needing help when eating, and avoidance of food of certain taste or texture (44). Furthermore, Gray and Chiang (45) reported that the problematic mealtime behaviors exhibited by Chinese-American children with ASD included preference for certain food textures (e.g., crunchy), unwillingness to try new foods, and inability to stay seated at the table till the end of the meal.
Determinants of feeding difficulties
Various facets have been recognized to influence feeding difficulties of children with ASD. These include age, ASD severity, and ASD symptoms, (46) among others. The relationship between age of a child with ASD and difficulties in feeding has been studied by various researchers with two reporting that these were negatively related (14, 47), that is, eating difficulties may diminish as the child grows older; one reporting a favorable relationship (16); and three reporting no relationship (48–50). On the other hand, concerning the relationship between ASD symptoms and their severity, with difficulties in feeding, researchers have reported favorable or no relationship. For example, Pham et al. (51) reported a positive association whereas Prosperi et al. (52); Sharp et al. (28, 29); and Smith et al. (50) reported that there was no relationship between feeding difficulties and ASD symptoms and their severity. Moreover, while Pham et al. (51) noted that the incidence of food selectivity corresponded to increased ASD severity, that is, to severe from moderate and to moderate from mild. In contrast, some other studies (13, 53) reported that the method of assessment, such as the usage of Autism Diagnostic Interview-Revised (ADI-R) (54), Autism Diagnostic Observation Scale-Calibrated Severity Scale (ADOS-CSS) (55), Social Responsiveness Scale (SRS) (56), BAMBI, among others, influenced the relationship between feeding difficulties and severity of ASD symptoms.
The role of gender has also been studied, though not specifically. For instance, Seiverling et al. (57) reported that boys with ASD were more likely to have feeding challenges than girl children with ASD. Leader et al. (58) also reported that gender was significantly associated with food selectivity. On the other hand, Worley and Matson (59) found that there the differences among the genders was not significant for eating problems, such as over/under eating. Also, Babinska et al. (60) found that food selectivity, problems at mealtime, diet, and usage of food supplements had no interactions with gender. That is, high incidences of challenging behavior associated with food intake were seen in both genders regardless of age. However, severity of symptoms was found to be correlated to challenging eating behavior.
Routines and ASD
Routines are defined as “observable, repetitive behaviors which directly involve the child and at least one adult acting in an interactive or supervisory role, and which occur with predictable regularity in the daily or weekly life of the child” and “may occur at a regular time, in the presence of a regular adult, in a regular place, in a regular sequence, or a combination of these” (61, p. 243). Routines are considered to be essential in establishing the basis for development of ritual. Rituals, in their turn, are regarded as significant in developing a family unit that is robust and healthy (22). In families of children with ASD, the daily routines are often centered around the characteristic demands of the child rather than those of the family in its entirety (62). Moreover, children with ASD can frequently find it difficult to participate in daily routines in their home, such as bath or bed time (63). Boyd et al. (64) reported that there were some common facets of research related to family routines and families of children with ASD. The facets were stress related to the necessity for and challenges with routines, the connection between family routines and the family’s health, participation of the family as planned around the child with ASD, adherence to routines while encountering challenges, cumbersome routines, significant routines for bonding of the family, and adaptations made by families to routines. Henderson et al. (65) found that quality and hygiene of sleep were associated with not only routines but also externalizing behaviors in a group of 58 children with ASD.
Marquenie et al. (22) found that families of children aged 2-5 years with ASD experienced dinnertime routines that were unruly and unstructured. In contrast, bedtime routines involved routines that were more structured and often non-functional. Thus, in contrast to dinnertime routines, bedtime routines were involved significant rituals and interactions. In another study, Ibañez et al. (63) used a randomized controlled trial to scrutinize the effectiveness of an interactive, web-based tutorial for parents in enhancing the engagement of children with ASD (aged 18-60 months) in everyday routines. This study found that the use of such a tutorial enhanced child participation in routines.
Stoppelbein et al. (66) used the Child Routines Questionnaire (CRQ) (61) to compare details of the routines of 45 children with ASD and 45 typically developing children of matching ages/genders. The parents of the children in the ASD group were found to report fewer routines. Moreover, children with ASD were found to have greater internalizing and externalizing symptoms than the children without ASD. In addition, the routine levels of younger children with ASD were found to be lower than those of older children (66). Mirzaie et al. (67) reported that it was difficult for families of children with ASD to follow routines due to different reasons, such as the children’s lack of flexibility, challenging behaviors, problems with sensory-processing, anxiety or marital issues of parents, and environmental aspects including poor access to ASD-related healthcare services in areas that were remote and less populated. McAuliffe et al. (68) highlighted that the efforts needed to develop family routines were substantial and that these could be at the detriment of the health and wellbeing of mothers of children with ASD.
Impacts of COVID-19
COVID-19 disrupted routines, school activities and special programs, day programs, and also support at work (11). Baweja et al. (69) reported that the different challenges encountered by persons with ASD during the COVID-19 pandemic included disruptions owing to changes in education and vocation, challenges to routines associated with home and leisure, restricted obtainability of behavioral health services, and modifications in delivery of health services. Individuals with ASD were more vulnerable due to their characteristics and typically accompanying conditions (69).
Narzisi (5) highlighted that children with autism spectrum conditions (ASC) typically have interventions for many hours a week, either at their homes with trained therapists or in assigned institutions or hospitals. Nevertheless, due to the COVID-19 pandemic, the physical support provided by therapists to these children and their families could not be continued. Moreover, they could not go to external interventions (5). Persons with ASD typically receive therapy in different ways (e.g., speech, physical, behavioral, social, occupational, and psychological). However, with COVID-19, persisting with these therapies was largely impossible (11). Manning et al. (70) found that the predominant facets of stress in families of persons with ASD were related to disruption of therapeutic service, finances, and illness. Moreover, higher stress was reported for caregivers of persons who had received a high intensity of services prior to COVID-19. The main concerns voiced by the respondents were related to obtaining respite care during the pandemic (70).
The present study
The aim of this study was to investigate the eating behavior and routines of children with ASD in Saudi Arabia during the COVID-19 outbreak. Two research questions informed the study: (1) What is the impact of COVID-19 on the eating behavior of children with ASD in the KSA? and (2) What is the impact of COVID-19 on their daily routines? Based on these research questions, the study hypothesized that the eating behavior of children with ASD and their daily routines could have significantly worsened in comparison to their typical state prior to the closure of schools. This study is significant because it endeavors to draw attention to the current status of children with ASD in the KSA in this regard and to provide insights for appropriate supportive action.
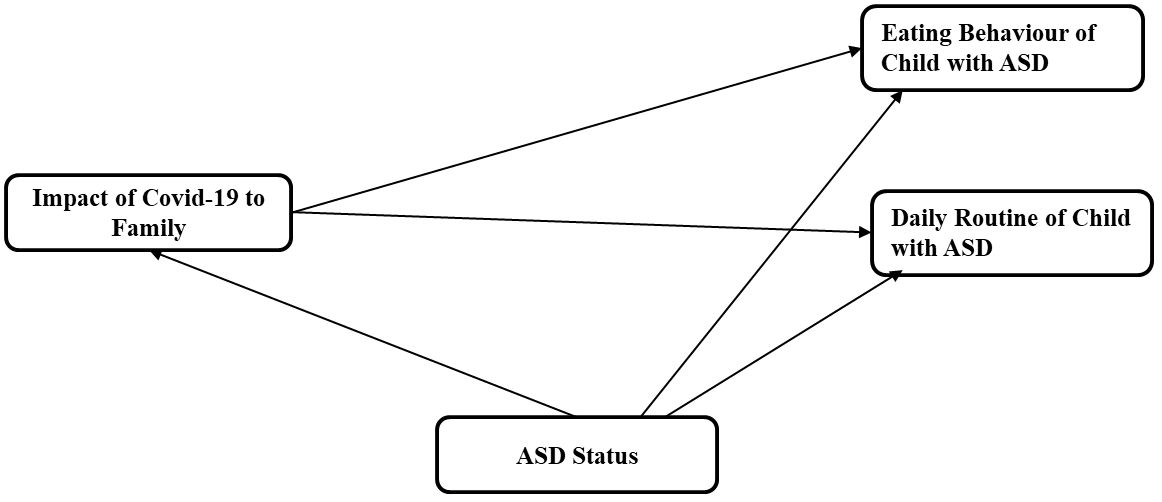
The scrutiny of prior research suggested that the pandemic would impact eating behavior and routines of children with ASD. The impact of different determinants (e.g., Age, Gender, and Severity of ASD symptoms) on children’s difficulties with feeding was another facet that has been explored in prior literature (46) and was thus included in the study for scrutiny extending the consideration to routines as well. Figure 1 depicts the proposed conceptual model for the study.
Method
Measures
A total of 150 Saudi parents of children with ASD were invited to participate in this survey as part of a cross-sectional study. The children described in the study were aged ≤18 years. The survey or questionnaire was distributed using email by contacting different Autism institutions. A questionnaire was designed in English and subsequently translated into Arabic. The following data were collected in the period April, 2020 to May, 2021:
(1) demographic data of the parents such as gender, age, marital status, educational qualifications, family income, current working situation (6 items);
(2) family ASD status such as number of children with/without ASD, age of children with ASD, gender of children with ASD, severity of ASD symptoms (5 items);
(3) impact of COVID-19 restrictions on family (10 items) adapted from COVID-related studies (23, 70). This scale used a five-item Likert scale: 1-No impact; 2-Little impact; 3-Impacted to some extent; 4-High impact; 5-Very high impact;
(4) eating behavior of children with ASD (12 items) adapted from the findings of various studies e.g., (20). This scale used a five-item Likert scale: 1–Considerably improved, 2–Slightly improved, 3–No different, 4–A little worse, and 5–Very much worse; and
(5) daily routines of children with ASD (16 items) modified from the Daily Routine and Autonomy (DRA) questionnaire and the findings of other studies e.g., (22, 71). The DRA questionnaire was developed by Lamash and Josman (71) in acknowledgement of the limited independence displayed by persons with ASD in daily activities. This study utilized sections of the questionnaire that were deemed suitable for a wider sample of children with ASD. Again, this scale used a five-item Likert scale: 1–Considerably improved, 2–Slightly improved, 3–No different, 4–A little worse, and 5–Very much worse.
At the end of the questionnaire, space was provided for the parents to add further comments or notes related to their children’s eating behavior or daily routines. This study was carried out in accordance with the Declaration of Helsinki and with the approval of ethics committee of applied medical sciences at Taibah university no, 2020/52/201/CLN.
Statistical analyses
Children’s ASD behaviors during the COVID-19 outbreak were rated by their parents using the Arabic or English version of the questionnaire. The validation was assessed. The study utilized different statistical analyses such as frequencies and percentages, descriptive statistics (mean (M) and standard deviation (SD)), and inferential statistics (one-sample t-test, one-way ANOVA, and regression). These analyses served to assess the changes to eating behavior and daily routines of the children with ASD. Moreover, the impact of the family ASD status on eating behavior and daily routines was also analyzed. All tests were performed using SPSS software version 26.0. The questionnaire was presented to a group of specialists in the field of nutrition and special education in ASD. Hence, the internal consistency coefficients were extracted for the overall instrument and for each individual domain using Cronbach’s alpha formula. The value of the alpha coefficient for the instrument as a whole unit was 0.85. The value of the alpha coefficient was 0.84 for the first domain (eating behavior), and 0.86 for the second domain (eating routines).
Results
Demographic information
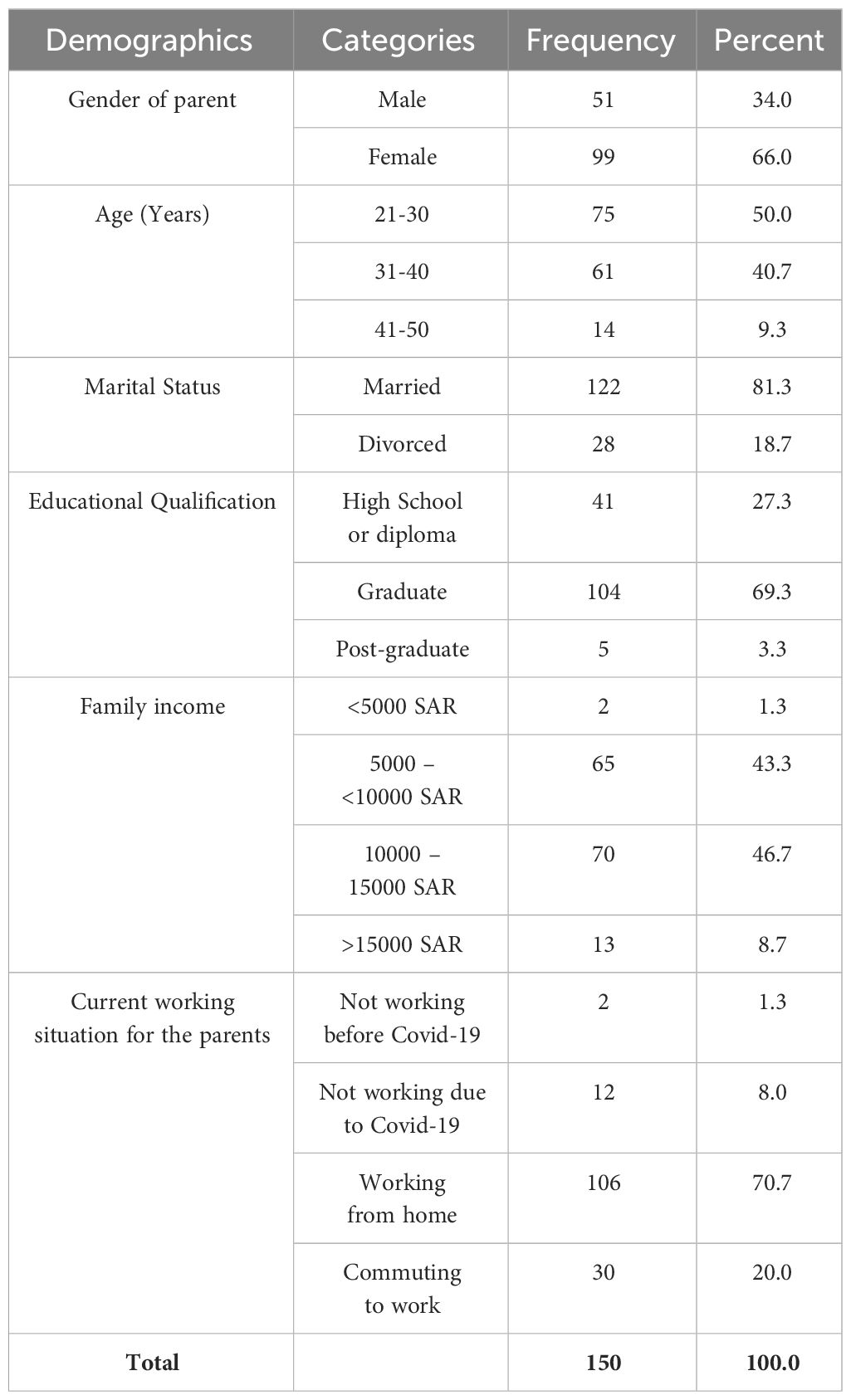
The majority of the participating parents were female (66.0%) and aged between 21 and 30 years (50.0%). Moreover, the majority of the parents were still married (81.3%), were graduates (69.3%), and had a family income between 10,000 and 15,000 SAR (46.7%). Further, 8% were not working due to COVID-19, having lost their jobs during the pandemic, indicating that the pandemic had impacted the livelihood of these parents. A large proportion of the participating parents (70.7%) were able to work from home. The demographic details of the parents are summarized in Table 1.
Family ASD status
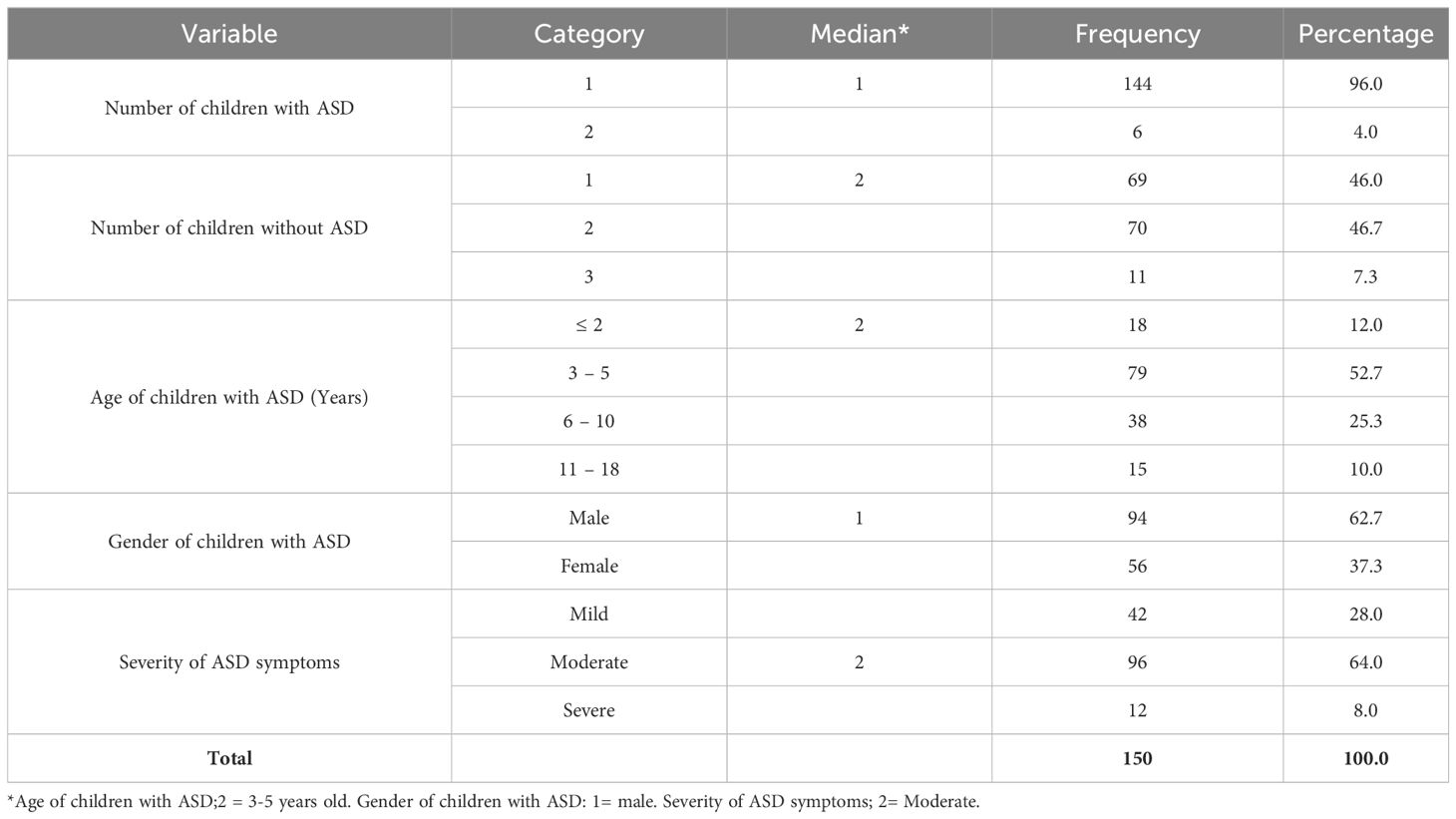
The majority of the participating families had one child with ASD (96.0%) and one or two children without ASD (70.0%). The ages of the children with ASD were mostly 3–5 years (52.7%) followed by ages of 6–10 years (25.3%). The majority of the children with ASD were male (62.7%). The severity of their symptoms was mostly moderate (64.0%), followed by mild symptoms (28.0%). There were also a few (8.0%) children with ASD who had severe symptoms. Also (Table 2).
Children’s eating behavior in the pandemic
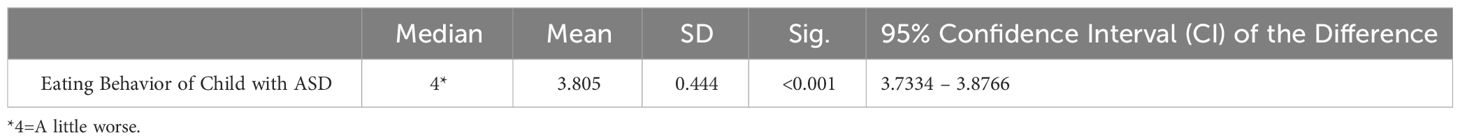
A one-sample t-test, utilized to assess the parents’ perceptions of the changes to their children’s eating behavior and daily routines in the pandemic, revealed that the children’s eating behavior (M=3.805, SD=0.444) had significantly worsened in comparison to their normal state (95% CI=3.73–3.88), which was significantly higher than the rating of “3” – (Not different) with median 4 (A little worse), p<.001 (Table 3).
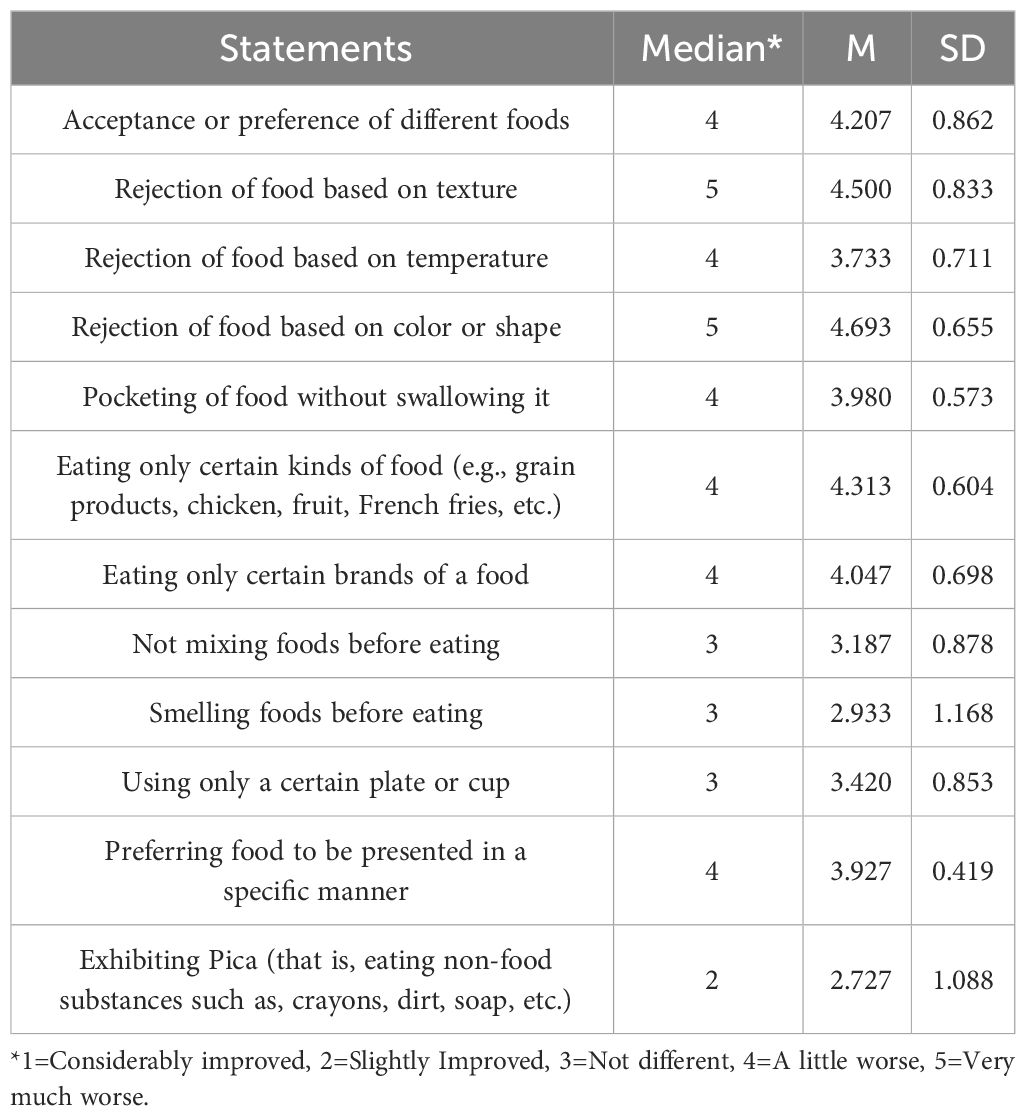
Further, from Table 4 it could be seen that the three facets of eating behavior that had changed the most were “Rejection of food based on color or shape” (M=4.693, SD=0.655); “Rejection of food based on texture” (M=4.500, SD=0.833); and “Eating only certain kinds of food (e.g., grain products, chicken, fruit, French fries, etc.)” (M=4.313, SD=0.604). The three facets of eating behavior that had changed the least were “Exhibiting pica (that is, eating non-food substances such as crayons, dirt, soap, etc.)” (M=2.727, SD=1.088); “Smelling foods before eating” (M=2.933, SD=1.168); and “Not mixing foods before eating” (M=3.187, SD=0.878).
Children’s daily routines in the pandemic
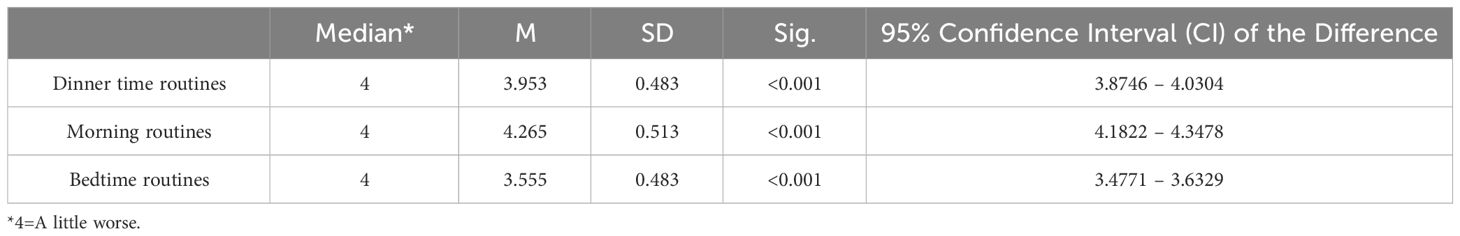
Similarly, it could be seen that the daily dinner-time routines of the children (M=3.593, SD=0.483) had significantly worsened in comparison to their state prior to the pandemic (95% CI=3.8746–4.0304, P<0.001). Likewise, the morning (M=4.265, SD=0.513, 95% CI=4.1822–4.3478, P<0.001) and bedtime (M=3.555, SD=0.483, 95% CI=3.4771–3.6329, P<0.001) routines had also significantly worsened in comparison with their state prior to the pandemic (Table 5).
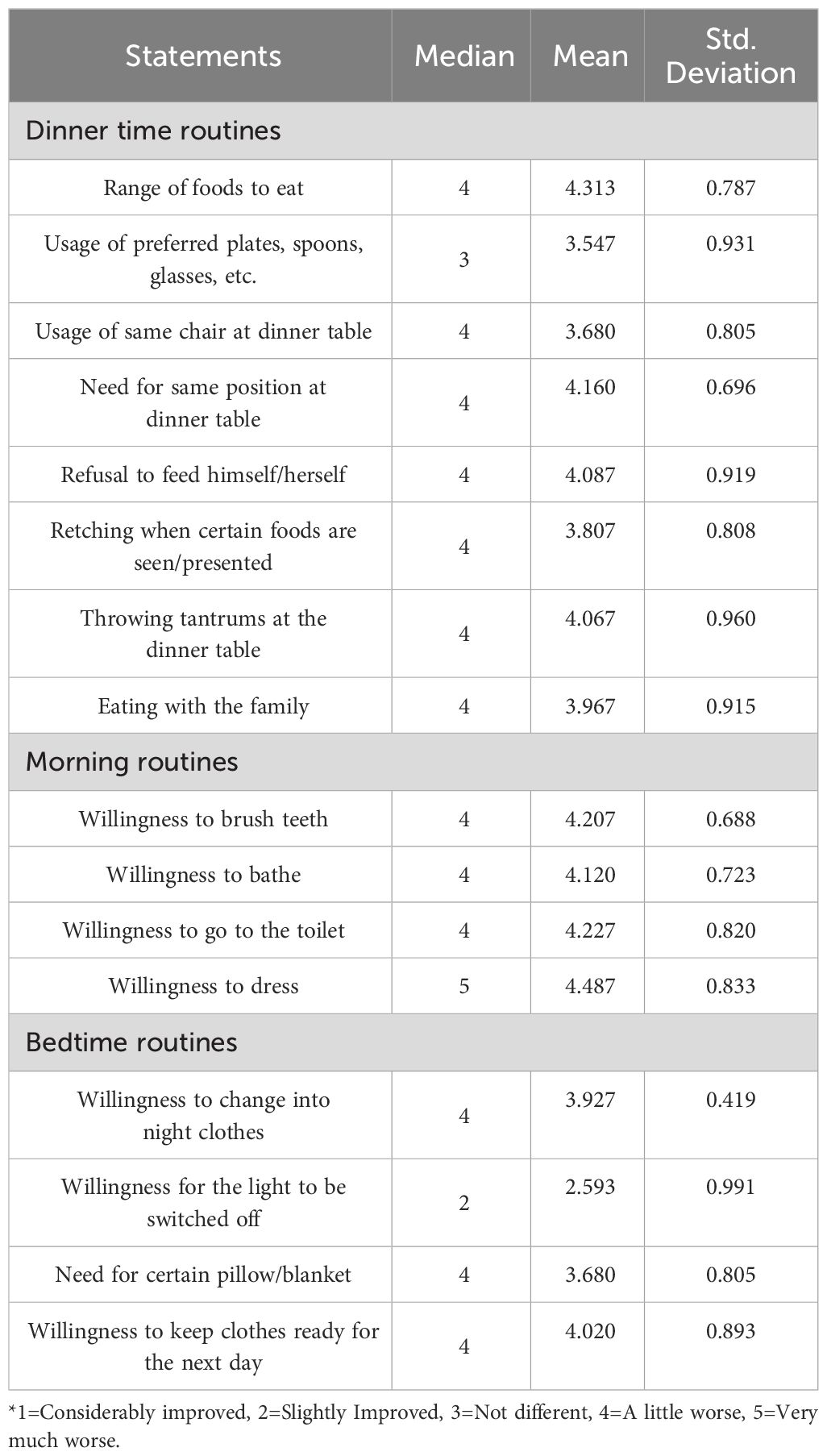
From Table 6, it could be seen that the dinner-time routine that had deteriorated the most was “Range of foods to eat” (M=4.313, SD=0.787), whereas the morning routine that had deteriorated the most was “Willingness to dress” (M=4.487, SD=0.833). The bedtime routine that had deteriorated the most was “Willingness to keep clothes ready for the next day” (M=4.020, SD=0.893). Overall, all the facets of the morning routine appeared to have deteriorated the most. Some facets of the dinner-time routines and bedtime routines had deteriorated slightly in comparison, such as “Usage of preferred plates, spoons, glasses, etc.” (M=3.547, SD=0.931) and “Need for certain pillow/blanket” (M=3.680, SD=0.805). Also, although the mean of the parents’ perceptions regarding the children’s “Willingness for the light to be switched off” indicated slight improvement to no change (M=2.593, SD=0.991).
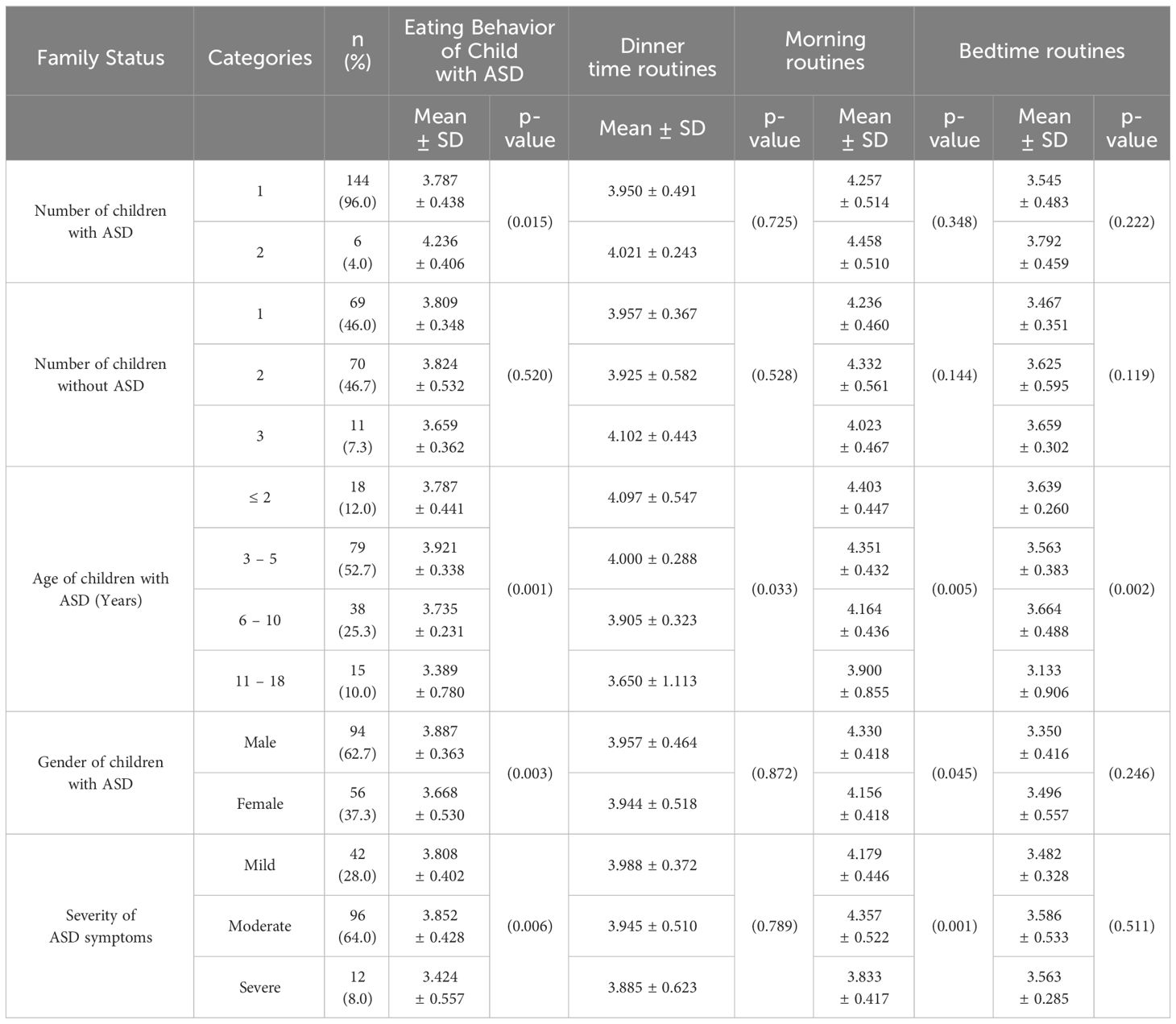
Influence of family status on eating behavior and daily routines
As can be seen in Table 7, the change in the eating behavior of a child with ASD was found to differ significantly (p<0.05) based on the number of children with ASD, age of children with ASD, gender of children with ASD, and severity of their ASD symptoms. However, change in eating behavior did not differ significantly based on number of children without ASD. Changes to dinner-time routines were found to differ significantly (p<0.05) based on the age of children with ASD, but not on the number of children with or without ASD, gender of children with ASD, and severity of their ASD symptoms. Changes to morning routines were found to differ significantly (p<0.05) based on age of children with ASD, their gender, and the severity of their ASD symptoms, but not number of children with or without ASD. Changes to bedtime routines were found to differ significantly (p<0.05) based on the age of children with ASD but not with the number of children with or without ASD, gender of children with ASD, or severity of their ASD symptoms.
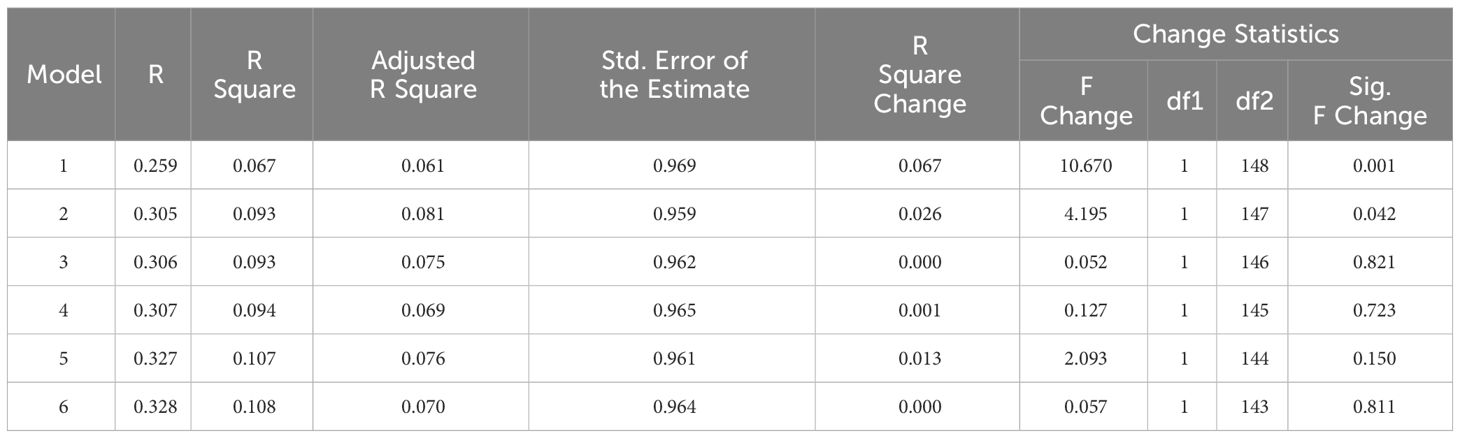
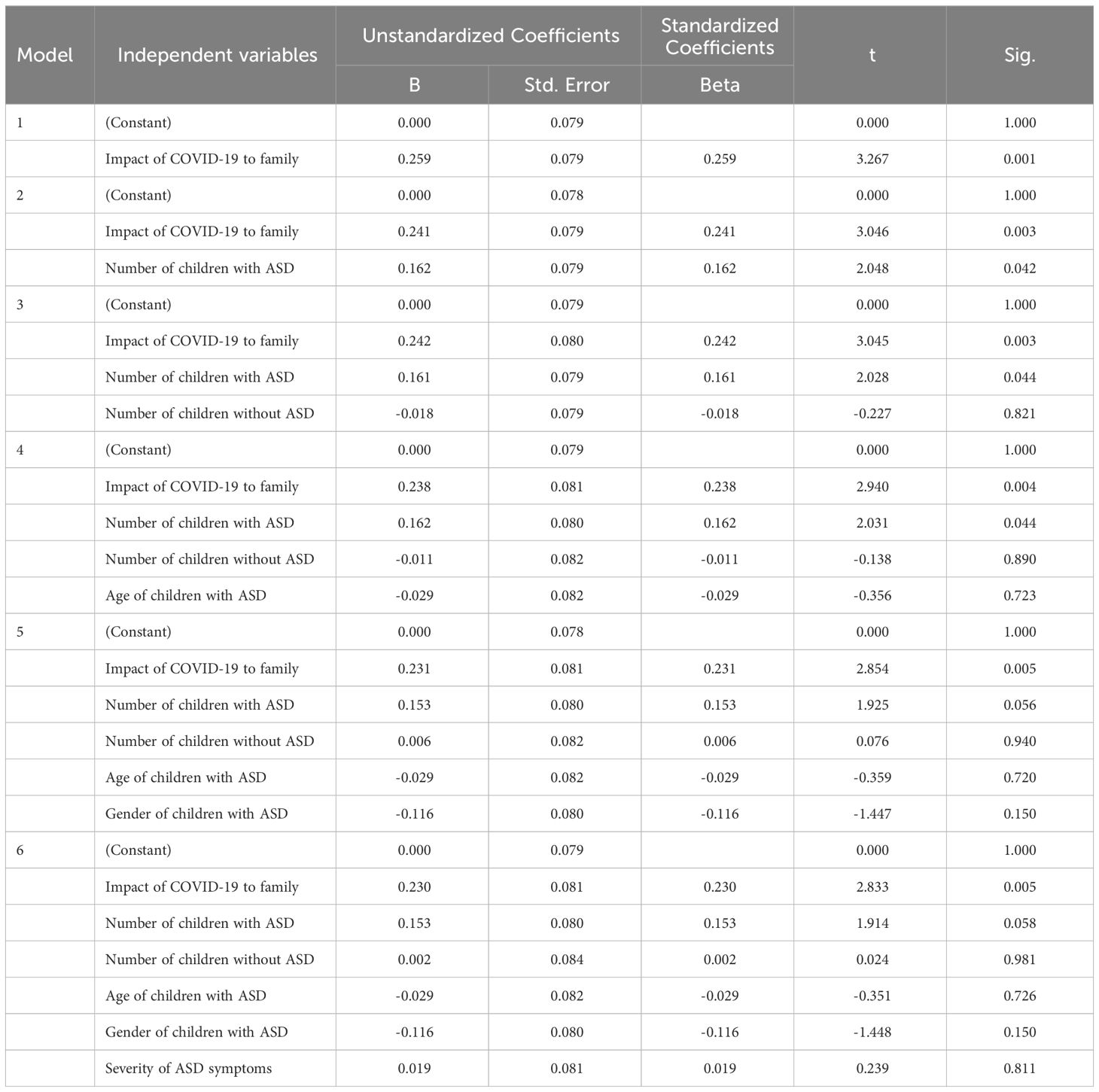
Influence of impact of COVID-19 on family eating behavior
A multiple linear regression was used to test the impact of COVID-19 on the family’s eating behavior (Tables 8, 9). This resulted in a significant model, F(1,148) = 10.670, p <.01, R2 = 0.067. The individual predictors were then scrutinized further and the outcomes indicated that while Impact of COVID-19 to family was a significant predictor (t=3.267, p<0.001), the overall facets of family ASD status were not significant predictors. The number of children with ASD was found to be a significant predictor in the early stages of the regression (t=2.048, p<0.05), but its impact was reduced when the other variables were added to the regression analysis.
Influence of impact of COVID-9 on family daily routines
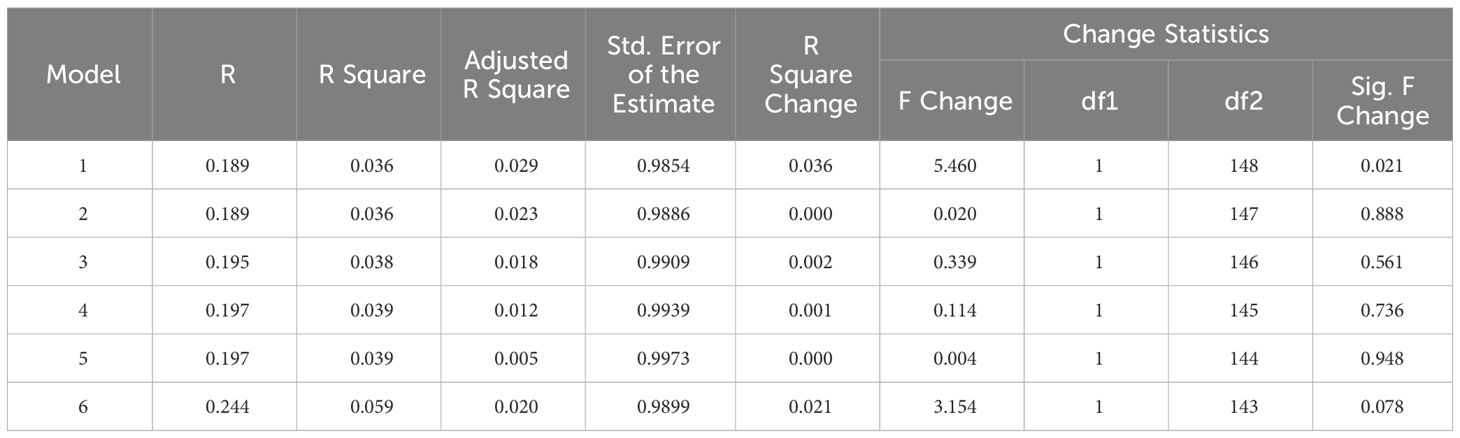
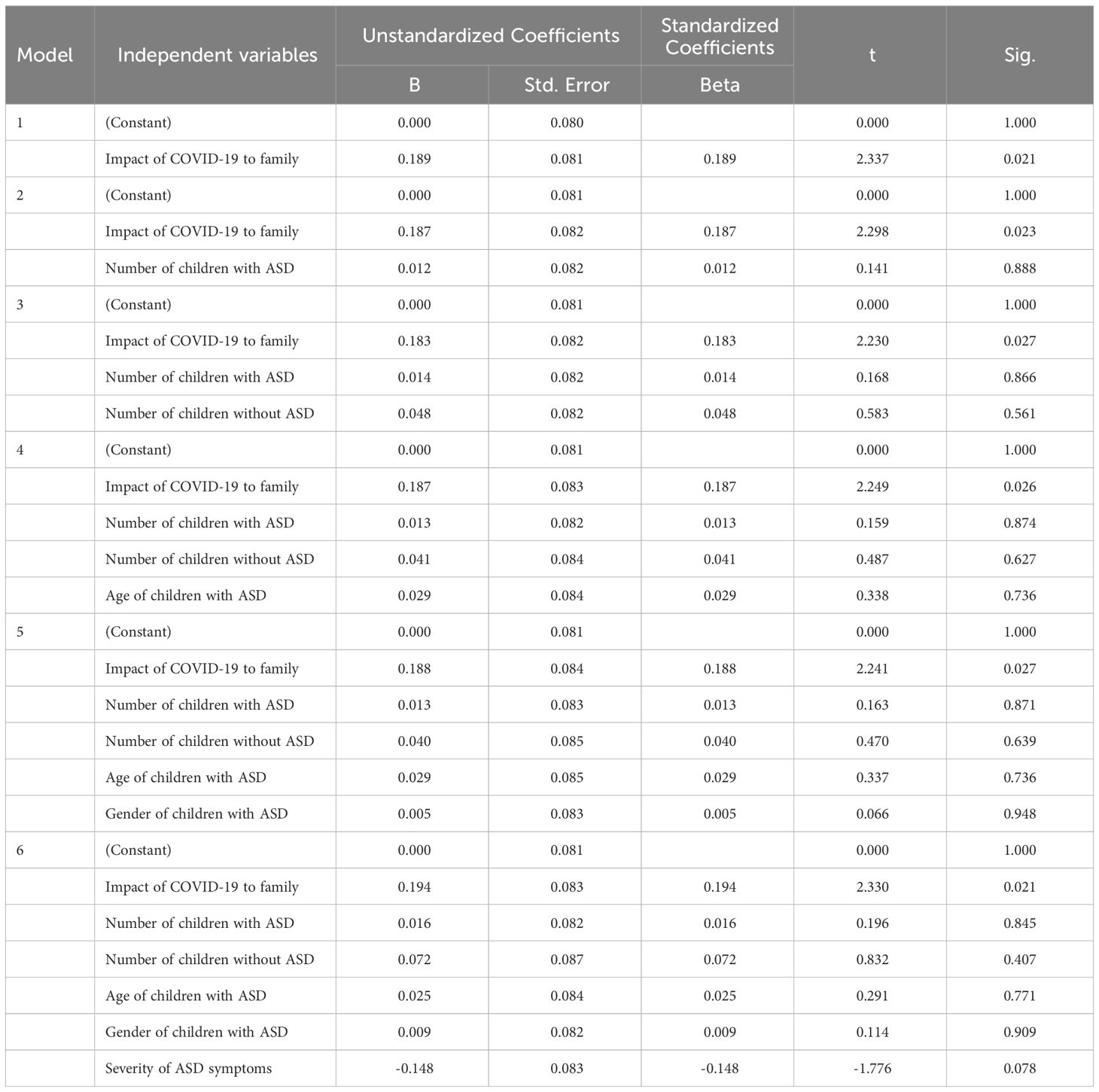
Influence of impact of COVID-19 on family dinner time routines
A multiple linear regression was used to test the impact of COVID-19 on the family’s dinner time routines (Tables 10, 11). This again resulted in a significant model, F(1, 148) = 4.460, p < 0.05, R2 = 0.036. The individual predictors were then scrutinized further and the outcomes indicated that while Impact of COVID-19 to family was a significant predictor (t=2.337, p<0.05), the facets of family ASD status were not significant predictors.
Influence of impact of COVID-19 on family morning routines
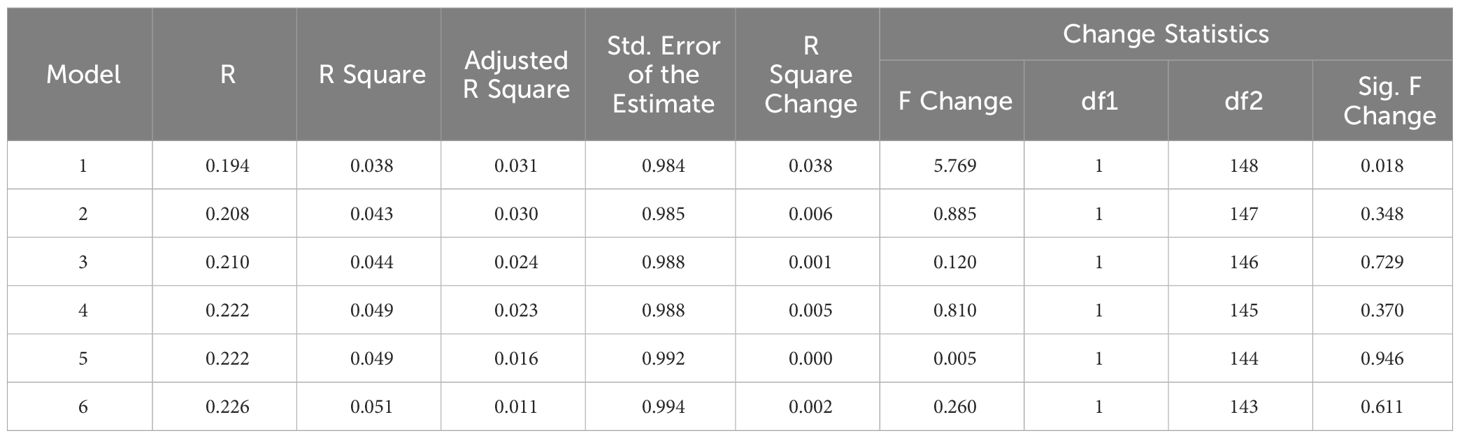
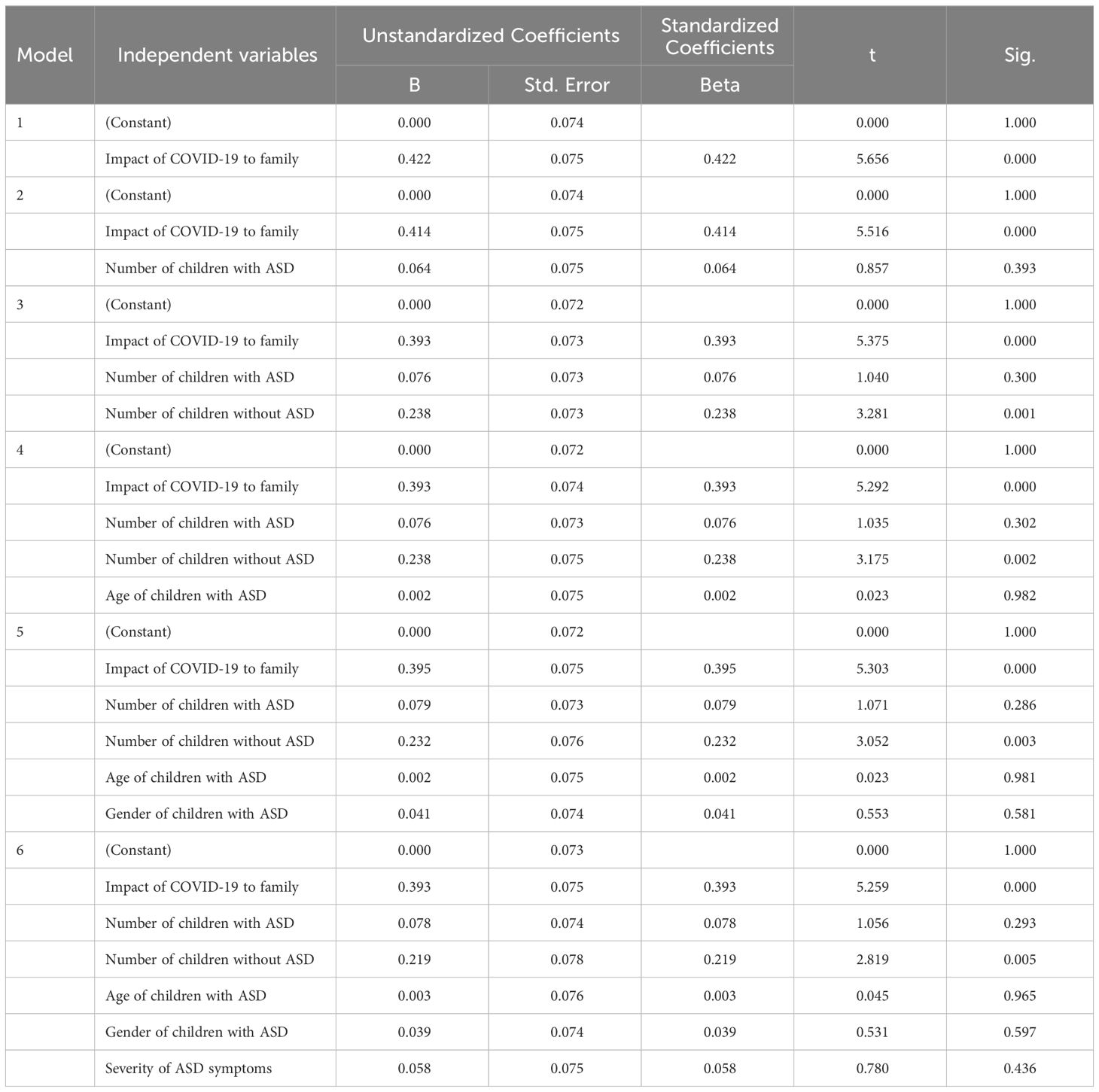
A multiple linear regression was used to test the impact of COVID-19 on the family’s morning time routines (Tables 12, 13). This again resulted in a significant model, F(1, 148) = 5.769, p < 0.05, R2 = 0.038. The individual predictors were then scrutinized further and the outcomes indicated that while Impact of COVID-19 to family was a significant predictor (t=2.402, p<0.05), the facets of family ASD status were not significant predictors.
Influence of impact of COVID-19 on family bedtime routines
A multiple linear regression was used to test the impact of COVID-19 on the family’s bed time routines (Tables 14, 15). This again resulted in a significant model, F(1, 148) = 31.986, p < 0.01, R2 = 0.178. The individual predictors were then scrutinized further and the outcomes indicated that while Impact of COVID-19 to family was a significant predictor (t=5.656, p<0.001), the facets of family ASD status were not significant predictors apart from Number of children without ASD (t=2.819, p<0.05).
Parents’ comments
About (35%) of parents’ comments at the end of the questionnaire indicated that their children lost weight compared to the period before the pandemic and they had encountered different challenges due to the COVID-19 situation, specifically with regard to procurement of the specific brands of food preferred by their children with ASD. Moreover, 40% indicated that dealing with multiple children with ASD requires planning and advice should be less cumbersome.
Discussion
To the best of the researcher’s knowledge, this is one of the first studies placing emphasis on the eating behavior and daily routines of children with ASD in Saudi Arabia during the coronavirus outbreak. Overall, the study found that parents perceived that the behaviors of their children with ASD concerning these had deteriorated due to the pandemic-related change in their situations.
Current status of eating behavior and daily routines
The study found that the children’s eating behavior had significantly worsened in comparison to their normal state in the pre-pandemic context. Eating challenges are a characteristic of most children with ASD (26, 27). The aspects of eating behavior that had changed the most were rejection of food based on color or shape, and texture and increased consumption of only certain kinds of food. This was in line with prior studies which have highlighted that selectivity of food by type and texture are common in children with ASD (32, 40). Moreover, the findings confirm that the food repertoire of a child with ASD does not typically change with time (14). This is further confirmed by the finding that the facets of eating behavior that had changed the least were related to pica; smelling foods prior to eating; and not mixing foods prior to eating.
Further, the study found that the daily routines of the children with ASD had also worsened. These findings were in line with Altable (11) and Eshraghi et al. (21), who highlighted that the daily routines of children with ASD have been impacted due to the pandemic in different ways. In particular, the parents perceived that the children’s morning routines were the most impacted, followed by the dinner-time routines and bedtime routines. It is possible that the dinner-time and bedtime routines were not impacted as much as the morning routines because the morning routines would usually have involved the child getting ready (or being readied) to leave the house to attend school or an intervention session. Prior research (22, 62, 63) has highlighted that bedtime routines were typically the most structured whereas dinnertime routines were more disordered, though children with ASD can find it difficult to participate in such routines. Nevertheless, it could be inferred that the disruption of the routines of the child with ASD had consequences for the families of the participants of the study.
Relationships between impact of COVID-19 to family, eating behavior, daily routines, and family ASD status
The study found that the change in the eating behavior of a child with ASD was found to differ significantly based on the number of children with ASD, age of children with ASD, gender of children with ASD, and severity of their ASD symptoms. Consistent with prior studies, the changes to the eating behavior of the children with ASD was related to the severity of their ASD symptoms (17) and also their age (14, 16, 47). Eating behavior was also related to the gender of the children (57, 58). Changes to the eating behavior of the children with ASD was also related to the number of children with ASD in the family. To the researcher’s best knowledge, this aspect has not been previously explored in research.
Moreover, on the lines of the findings of Huxham et al. (19) and Padmanabhan and Shroff (18), this study found that the facets of eating behavior that the children appeared to struggle with included their preference for foods of certain colors, shapes, textures, kinds, or brands, and for food to be presented in a particular manner. Other eating behavior had also deteriorated, such as pocketing of food in contrast to swallowing it (20).
The study found that the worsening of dinner-time routines was related to the age of the child with ASD but not to their gender or the severity of their symptoms. Also, it was not related to the number of children with and without ASD in the family. The worsening of morning routines was found to be related to the age of the child with ASD, their gender, and the severity of symptoms, but not to number of children with and without ASD in the family. Finally, the parents’ perceptions of the bedtime routines were found to be related to the age of the child with ASD. The study’s findings on the relationship between the age of the children with ASD and their routines were on the lines of Marquenie et al. (22) and Stoppelbein et al. (66). Moreover, the scrutiny on the associations between gender, ASD severity, and routines does not seem to have received much consideration although Stoppelbein et al. (66) did not find a significant relationship between gender and child routines and severity and child routines.
Furthermore, from the parents’ notes, this study found that the COVID situation had made it difficult for parents to obtain the brands of food their children preferred. This could have contributed to the worsening of the children’s eating behavior and consequently some of the activities involved in their mealtime routines.
Conclusion
This study found that the eating behavior and daily routines of children with ASD in Saudi Arabia considerably worsened during the coronavirus pandemic. Given that the ongoing and the attempts of governments in Saudi Arabia and across the world to contain the situation have met with mixed success, it is possible that this situation may be returned. In such case, the closing of educational institutions for children with ASD. In this context, this study highlights the impacts on the behavior of children with ASD due to changes in their regular routines, which might include regular attendance at mainstream or special schools and a variety of interventions.
Moreover, by obtaining the perceptions of the parents of children with ASD across different age groups (≤18 years) and of mixed gender and varying levels of severity of ASD symptoms, this study highlights the fact that changes in schedule or context do impact children with ASD regardless of their age, gender, or ASD severity. A downstream impact of the effects on children with ASD is the impact on their parents’ wellbeing (25). Consequently, it is imperative that measures be taken to help children with ASD deal with such epidemic-related situations and to prepare them for the changes that may lie ahead.
Limitations of the study
This study is not without limitations. Firstly, the study was undertaken after pandemic-related precautions were implemented in Saudi Arabia. Consequently, it is possible that some measures may already have been undertaken to mitigate the impact on children with ASD. Future researchers could seek to overcome these limitations by undertaking a study with a broader sample and by performing a longitudinal study where the impacts on children with ASD are scrutinized at different points in the pandemic timeline. Additionally, it appeared that the parents were experiencing some form of fatigue in responding to the questionnaire, perhaps due to the surfeit of similar studies being undertaken across the globe.
Moreover, no data were explicitly collected related to the pre-pandemic status of the children of the participating families. A future researcher could rectify this situation. An additional facet could be the involvement of external stakeholders, such as dietitians, teachers and therapists, to provide further insights regarding the eating behavior and routines of the children with ASD.
Implications for research and practice
The findings of the study indicate that it is necessary for support for children with ASD to be expanded and reconsidered during the spread of any pandemic. The following recommendations are made in this regard:
i) Parents, teachers, behavior analysts, psychologists, dieticians, or nutritionists and others associated with the welfare of persons with ASD in Saudi Arabia must take a range of measures to help them deal with the pandemic-related changes to their schedule. For instance, parents could be trained to provide behavioral support and reinforcement (24).
ii) Behavior analysts with dieticians and/or nutritionists could collaborate with parents to adapt or design interventions that can be implemented at home by either or both parents.
iii) The Saudi Ministry of Health and Ministry of Education could initiate programs to oversee the training of parents and other caretakers of children with ASD during the pandemic and/or lockdown and promote the use of online interventions to support children of different age groups.
iv) The Ministry of Health and Ministry of Education could also facilitate the development of more virtual helplines to ensure that all parents of children with ASD can access varied sources of assistance such as behavior analysts, dieticians, and nutritionists.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Ethics statement
This study was carried out in accordance with the Declaration of Helsinki and with the approval of the the Applied Medical Science committee at University of Taibah no, 2020/52/201/CLN. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
MA: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The author would like to express gratitude to all participants, as well as the autistic centers and schools. Also, the authors thanks everyone who offered to assist with the distribution of the questionnaire to the parents to children with ASD.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Yezli S, Khan A. COVID-19 social distancing in the Kingdom of Saudi Arabia: Bold measures in the face of political, economic, social and religious challenges. Travel Med Infect Dis. (2020), 101692. doi: 10.1016/j.tmaid.2020.101692
2. Al-Tawfiq JA, Memish ZA. COVID-19 in the Eastern Mediterranean Region and Saudi Arabia: prevention and therapeutic strategies. Int J Antimicrobial Agents. (2020) 55:105968. doi: 10.1016/j.ijantimicag.2020.105968
3. Bin Nafisah S, Alamery AH, Al Nafesa A, Aleid B, Brazanji NA. School closure during novel influenza: A systematic review. J Infection Public Health. (2018) 11(5):657–61. doi: 10.1016/j.jiph.2018.01.003
4. Litvinova M, Liu Q, Kulikov E, Ajelli M. Reactive school closure weakens the network of social interactions and reduces the spread of influenza. Proc Natl Acad Sci. (2019) 116(27):13174–81. doi: 10.1073/pnas.1821298116
5. Narzisi A. Handle the autism spectrum condition during coronavirus (Covid-19) stay at home period: Ten tips for helping parents and caregivers of young children. Brain Sci. (2020) 10. doi: 10.3390/brainsci10040207
6. Reichow B, Hume K, Barton EE, Boyd BA. Early intensive behavioral intervention (EIBI) for young children with autism spectrum disorders (ASD). Cochrane Database Systematic Rev. (2018) (5):CD009260. doi: 10.1002/14651858.CD009260.pub3
7. Chin W-C, Li HM, Chao KY, Chang HL. Stressors experienced by children with autism spectrum disorder in Taiwan: Perspectives of children and their parents. Nurs Health Sci. (2019) 21(2):206–13. doi: 10.1111/nhs.12583
8. Camargo SPH, Rispoli M, Ganz J, Hong ER, Davis H, Mason R, et al. A review of the quality of behaviorally-based intervention research to improve social interaction skills of children with ASD in inclusive settings. J Autism Dev Disord. (2014) 44:2096–116. doi: 10.1007/s10803-014-2060-7
9. van Steensel FJA, Bögels SM, Perrin S. Anxiety disorders in children and adolescents with autistic spectrum disorders: a meta-analysis. Clin Child Family Psychol Rev. (2011) 14:302–17. doi: 10.1007/s10567-011-0097-0
10. Strang JF, Kenworthy L, Daniolos P, Case L, Wills MC, Martin A, et al. Depression and anxiety symptoms in children and adolescents with autism spectrum disorders without intellectual disability. Res Autism Spectr Disord. (2012) 6(1):406–12. doi: 10.1016/j.rasd.2011.06.015
11. Altable M, de la Serna JM, Gavira SM. Child and adult autism spectrum disorder in COVID-19 pandemic. PsyArXiv (2020). doi: 10.31234/osf.io/kt3a4
12. Bicer AH, Alsaffar AA. Body mass index, dietary intake and feeding problems of Turkish children with autism spectrum disorder (ASD). Res Dev disabilities. United States. (2013) 34:3978–87. doi: 10.1016/j.ridd.2013.08.024
13. Postorino V, Sanges V, Giovagnoli G, Fatta LM, Peppo LD, Armando M, et al. Clinical differences in children with autism spectrum disorder with and without food selectivity. Appetite. Engl. (2015) 92:126–32. doi: 10.1016/j.appet.2015.05.016
14. Bandini LG, Curtin C, Phillips S, Anderson SE, Maslin M, Must A. Changes in food selectivity in children with autism spectrum disorder. J Autism Dev Disord. (2017) 47:439–46. doi: 10.1007/s10803-016-2963-6
15. Al-Kindi NM, Al-Farsi YM, Al-Bulushi B, Ali A, Alam Rizvi SG, Mohamed Essa M. ‘Food selection and preferences of Omani autistic children’. In: Essa M, Qoronfleh M, editors. Personalized Food Intervention and Therapy for Autism Spectrum Disorder Management. Springer, Cham (2020). p. 505—523. doi: 10.1007/978-3-030-30402-7_16
16. Vissoker RE, Latzer Y, Stolar O, Rabenbach A, Gal E. Eating problems and patterns among toddlers and young boys with and without autism spectrum disorders. Res Autism Spectr Disord. (2019) 59:1–9. doi: 10.1016/j.rasd.2018.12.001
17. Patton SR, Odar Stough C, Pan TY, Holcomb LO, Dreyer Gillette ML. Associations between autism symptom severity and mealtime behaviors in young children presented with an unfamiliar food. Res Dev Disabil. (2020) 103:103676. doi: 10.1016/j.ridd.2020.103676
18. Padmanabhan PS, Shroff H. Addressing mealtime behaviours of children with autism spectrum disorders in schools: a qualitative study with educators in Mumbai, India. Int J Dev Disabilities. Taylor Francis. (2020) 66:142–52. doi: 10.1080/20473869.2020.1738794
19. Huxham L, Marais M, van Niekerk E. Idiosyncratic food preferences of children with autism spectrum disorder in England. South Afr J Clin Nutr. (2019) 34:1–7. doi: 10.1080/16070658.2019.1697039
20. Mayes SD, Zickgraf H. Atypical eating behaviors in children and adolescents with autism, ADHD, other disorders, and typical development. Res Autism Spectr Disord. (2019), 76–83. doi: 10.1016/j.rasd.2019.04.002
21. Eshraghi AA, Li C, Alessandri M, Messinger DS, Eshraghi RS, Mittal R, et al. COVID-19: overcoming the challenges faced by individuals with autism and their families. Lancet Psychiatry. (2020) 7(6):481–3. doi: 10.1016/S2215-0366(20)30197-8
22. Marquenie K, Rodger S, Mangohig K, Cronin A. Dinnertime and bedtime routines and rituals in families with a young child with an autism spectrum disorder. Aust Occup Ther J. (2011) 58(3):145–54. doi: 10.1111/j.1440-1630.2010.00896.x
23. Colizzi M, Sironi E, Antonini F, Ciceri ML, Bovo C, Zoccante L. Psychosocial and behavioral impact of COVID-19 in autism spectrum disorder: An online parent survey. Brain Sci. (2020) 10:341. doi: 10.3390/brainsci10060341
24. Degli Espinosa F, Metko A, Raimondi M, Impenna M, Scognamiglio E. A model of support for families of children with autism living in the covid-19 lockdown: lessons from Italy. Behav Anal Pract. (2020) 13(3):550–8. doi: 10.1007/s40617-020-00438-7
25. Stankovic M, Stojanovic A, Jelena S, Stankovic M, Shih A, Stankovic S The Serbian experience of challenges of parenting children with autism spectrum disorders during the COVID-19 pandemic and the state of emergency with the police lockdown. SSRN Electronic J. (2021) 31(4):693–8. doi: 10.2139/ssrn.3582788
26. Ahearn WH, Castine T, Nault K, Green G. An assessment of food acceptance in children with autism or pervasive developmental disorder-not otherwise specified. J Autism Dev Disord. (2001) 31(5):505–11. doi: 10.1023/A:1012221026124
27. Ledford JR, Gast DL. Feeding problems in children with autism spectrum disorders: A review. Focus Autism Other Dev Disabil. (2006) 21:153–66. doi: 10.1177/10883576060210030401
28. Sharp WG, Berry RC, McCracken C, Nuhu NN, Marvel E, Saulnier CA, et al. Feeding problems and nutrient intake in children with autism spectrum disorders: A meta-analysis and comprehensive review of the literature. J Autism Dev Disord. (2013) 43(9):2159–73. doi: 10.1007/s10803-013-1771-5
29. Sharp WG, Jaquess DL, Lukens CT. Multi-method assessment of feeding problems among children with autism spectrum disorders. Res Autism Spectr Disord. (2013) 7:56–65. doi: 10.1016/j.rasd.2012.07.001
30. Schreck KA, Williams K. Food preferences and factors influencing food selectivity for children with autism spectrum disorders. Res Dev Disabil. (2006) 27:353–63. doi: 10.1016/j.ridd.2005.03.005
31. Levin L, Carr EG. Food selectivity and problem behavior in children with developmental disabilities: Analysis and intervention. Behav Modification. (2001) 25:443–70. doi: 10.1177/0145445501253004
32. Field D, Garland M, Williams K. Correlates of specific childhood feeding problems. J Paediatrics Child Health. (2003) 39:299–304. doi: 10.1046/j.1440-1754.2003.00151.x
33. Raiten DJ, Massaro T. Perspectives on the nutritional ecology of autistic children. J Autism Dev Disord. (1986) 16:133–43. doi: 10.1007/BF01531725
34. DeGrace BW. The everyday occupation of families with children with autism. Am J Occup Ther. (2004) 58:543–50. doi: 10.5014/ajot.58.5.543
35. Lukens CT, Linscheid TR. Development and validation of an inventory to assess mealtime behavior problems in children with autism. J Autism Dev Disord. (2008) 38:342–52. doi: 10.1007/s10803-007-0401-5
36. Rogers LG, Magill-Evans J, Rempel GR. Mothers’ Challenges in feeding their children with autism spectrum disorder-managing more than just picky eating. J Dev Phys Disabil. (2012) 24:19–33. doi: 10.1007/s10882-011-9252-2
37. Nadon G, Feldman DE, Dunn W, Gisel E. Mealtime problems in children with Autism Spectrum Disorder and their typically developing siblings: A comparison study. Autism. (2011) 15(1):98–113. doi: 10.1177/1362361309348943
38. Ausderau K, Juarez M. The impact of autism spectrum disorders and eating challenges on family mealtimes. Infant Child Adolesc Nutr. (2013) 5:315–23. doi: 10.1177/1941406413502808
39. Aponte CA, Romanczyk RG. Assessment of feeding problems in children with autism spectrum disorder. Res Autism Spectr Disord. (2016) 21:61–72. doi: 10.1016/j.rasd.2015.09.007
40. Balikçi Ö.S, Çiyiltepe M. Feeding problems of children with autism. PEOPLE: Int J Soc Sci. (2017) 3:870–80. doi: 10.20319/pijss.2017.s31.870880
41. Meral BF, Fidan A. A study on turkish adaptation, validity and reliability of the brief autism mealtime behavior inventory (BAMBI). Proc - Soc Behav Sci. (2014) 116:403–8. doi: 10.1016/j.sbspro.2014.01.230
42. DeMand A, Johnson C, Foldes E. Psychometric properties of the brief autism mealtime behaviors inventory. J Autism Dev Disord. (2015) 45:2667–73. doi: 10.1007/s10803-015-2435-4
43. Bandini LG, Anderson SE, Curtin C, Cermak S, Evans EW, Scampini R, et al. Food selectivity in children with autism spectrum disorders and typically developing children. J Pediatr. (2010) 157(2):259–64. doi: 10.1016/j.jpeds.2010.02.013.Food
44. Mahmoud NF, Abdelhameed RS, Abdelmonam SA, Abdelmonem AA, Khalil DM, Bakia SA. Parent-reported feeding characteristics in children with ASD vs. children who are typically developing. Egyptian J Otolaryngol. (2021) 37. doi: 10.1186/s43163-021-00152-3
45. Gray HL, Chiang HM. Brief report: Mealtime behaviors of Chinese American children with autism spectrum disorder. J Autism Dev Disord. (2017) 47:892–7. doi: 10.1007/s10803-016-2993-0
46. Page SD, Souders MC, Kral TVE, Chao AM, Pinto-Martin J. Correlates of feeding difficulties among children with autism spectrum disorder: A systematic review. J Autism Dev Disord. (2022) 52(1):255–74. doi: 10.1007/s10803-021-04947-4
47. Gray HL, Sinha S, Buro AW, Robinson C, Berkman K, Agazzi H, et al. Early history, mealtime environment, and parental views on mealtime and eating behaviors among children with ASD in Florida. Nutrients. (2018) 10(12):1867. doi: 10.3390/nu10121867
48. Suarez MA, Nelson NW, Curtis AB. Longitudinal follow-up of factors associated with food selectivity in children with autism spectrum disorders. Autism. (2014) 18:924–32. doi: 10.1177/1362361313499457
49. Sharp WG, Postorino V, McCracken CE, Berry RC, Criado KK, Burrell TL, et al. Dietary intake, nutrient status, and growth parameters in children with autism spectrum disorder and severe food selectivity: An electronic medical record review. J Acad Nutr Dietetics. (2018) 118(10):1943–50. doi: 10.1016/j.jand.2018.05.005
50. Smith B, Rogers SL, Blissett J, Ludlow AK. The relationship between sensory sensitivity, food fussiness and food preferences in children with neurodevelopmental disorders. Appetite. (2020) 150:104643. doi: 10.1016/j.appet.2020.104643
51. Pham D, Silver S, Haq S, Hashmi SS, Eissa M. Obesity and severe obesity in children with autism spectrum disorder: Prevalence and risk factors. South Med J. (2020) 113(4):168–75. doi: 10.14423/smj.0000000000001068
52. Prosperi M, Santocchi E, Balboni G, Narzisi A, Bozza M, Fulceri F, et al. Behavioral phenotype of ASD preschoolers with gastrointestinal symptoms or food selectivity. J Autism Dev Disord. (2017) 47(11):3574–88. doi: 10.1007/s10803-017-3271-5
53. Zachor DA, Ben-Itzchak E. Specific medical conditions are associated with unique behavioral profiles in autism spectrum disorders. Front Neurosci. (2016) 10:410. doi: 10.3389/fnins.2016.00410
54. Lord C, Rutter M, Le Couteur A. Autism diagnosis interview – revised (ADI-R). J Autism Dev Disord. (1994) 24:659–85. doi: 10.1007/BF02172145
55. Gotham K, Pickles A, Lord C. Standardizing ADOS scores for a measure of severity in autism spectrum disorders. J Autism Dev Disord. (2009) 39:693–705. doi: 10.1007/s10803-008-0674-3
56. Constantino JN. Social responsiveness scale. Second. Western Psychological Services (WPS) (2012).
57. Seiverling L, Towle P, Hendy HM, Pantelides J. Prevalence of feeding problems in young children with and without autism spectrum disorder: A chart review study. J Early Intervention. (2018) 40(4):335–46. doi: 10.1177/1053815118789396
58. Leader G, Tuohy E, Chen JL, Mannion A, Gilroy SP. Feeding problems, gastrointestinal symptoms, challenging behavior and sensory issues in children and adolescents with autism spectrum disorder. J Autism Dev Disord. (2020) 50(4):1401–10. doi: 10.1007/s10803-019-04357-7
59. Worley JA, Matson JL. Psychiatric symptoms in children diagnosed with an Autism Spectrum Disorder: An examination of gender differences. Res Autism Spectr Disord. (2011) 5:1086–91. doi: 10.1016/j.rasd.2010.12.002
60. Babinska K, Celusakova H, Belica I, Szapuova Z, Waczulikova I, Nemcsicsova D, et al. Gastrointestinal symptoms and feeding problems and their associations with dietary interventions, food supplement use, and behavioral characteristics in a sample of children and adolescents with autism spectrum disorders. Int J Environ Res Public Health. (2020) 17(17):6372. doi: 10.3390/ijerph17176372
61. Sytsma SE, Kelley ML, Wymer JH. Development and initial validation of the child routines inventory. J Psychopathol Behav Assess. (2001) 23:241–51. doi: 10.1023/A:1012727419873
62. McAuliffe T, Vaz S, Falkmer T, Cordier R. A comparison of families of children with autism spectrum disorders in family daily routines, service usage, and stress levels by regionality. Dev Neurorehabil. (2017) 20(8):483–90. doi: 10.1080/17518423.2016.1236844
63. Ibañez LV, Kobak K, Swanson A, Wallace L, Warren Z, Stone WL. Enhancing interactions during daily routines: A randomized controlled trial of a web-based tutorial for parents of young children with ASD. Autism Res. (2018) 11(4):667–78. doi: 10.1002/aur.1919
64. Boyd BA, McCarty CH, Sethi C. Families of children with autism: A synthesis of family routines literature. J Occup Sci. (2014) 21:322–33. doi: 10.1080/14427591.2014.908816
65. Henderson JA, Barry TD, Bader SH, Jordan SS. The relation among sleep, routines, and externalizing behavior in children with an autism spectrum disorder. Res Autism Spectr Disord. (2011) 5(2):758–67. doi: 10.1016/j.rasd.2010.09.003
66. Stoppelbein L, Biasini F, Pennick M, Greening L. Predicting internalizing and externalizing symptoms among children diagnosed with an autism spectrum disorder: The role of routines. J Child Family Stud. (2016) 25(1):251–61. doi: 10.1007/s10826-015-0218-3
67. Mirzaie H, Jamshidian E, Hosseini SA. Routines in families of children with autism. J Rehabil. (2018) 19:184–93. doi: 10.32598/rj.19.3.184
68. McAuliffe T, Thomas Y, Vaz S, Falkmer T, Cordier R. The experiences of mothers of children with autism spectrum disorder: Managing family routines and mothers’ health and wellbeing. Aust Occup Ther J. (2019) 66(1):68–76. doi: 10.1111/1440-1630.12524
69. Baweja R, Brown SL, Edwards EM, Murray MJ. COVID-19 pandemic and impact on patients with autism spectrum disorder. J Autism Dev Disord. (2022) 52(8):473–82. doi: 10.1007/s10803-021-04950-9
70. Manning J, Billian J, Matson J, Allen C, Soares N. Perceptions of families of individuals with autism spectrum disorder during the COVID-19 crisis. J Autism Dev Disord. (2021) 51(8):2920–8. doi: 10.1007/s10803-020-04760-5
Keywords: autism spectrum disorder (ASD), coronavirus, COVID-19, eating behaviors, routines, parents
Citation: Alharbi MH (2024) Parents’ perceptions of the impact of the novel coronavirus (COVID-19) on the eating behaviors and routines of children with autism spectrum disorders (ASD). Front. Psychiatry 15:1296643. doi: 10.3389/fpsyt.2024.1296643
Received: 19 September 2023; Accepted: 04 March 2024;
Published: 28 March 2024.
Edited by:
Cecilia Montiel Nava, The University of Texas Rio Grande Valley, United StatesReviewed by:
David Pérez-Jorge, University of La Laguna, SpainFrancesca Felicia Operto, University of Salerno, Italy
Copyright © 2024 Alharbi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mudi H. Alharbi, mhjharbi@taibahu.edu.sa
 Mudi H. Alharbi
Mudi H. Alharbi