- 1Psychology Program, Social Science Department, College of Arts & Sciences, Qatar University, Doha, Qatar
- 2Psychology Department, College of Education, King Khalid University, Abha, Saudi Arabia
- 3Psychology Department, College of Education, Qassim University, Qassim, Saudi Arabia
Background: Vaccine hesitancy is a significant global problem resulting from the interaction of multiple factors, including mental health factors. However, the association of COVID-19 vaccine hesitancy with mental health has not been well-examined, especially in Arab culture. This study aims to identify the correlation between anxiety/fear of COVID-19 and vaccine hesitancy among Saudi adults.
Methods: An online-based survey was administered to 558 participants from all regions of Saudi Arabia using the snowball technique. However, this sample may not be representative of the Saudi adult population. Participants responded to the Questionnaire of Vaccine Hesitancy, the COVID-19-Anxiety Questionnaire (C-19-A), and the Fear of COVID-19 Scale (FCV-19S). Data were analyzed on vaccine uptake, vaccine hesitancy, coronavirus infection, and demographic variables. The predictive factors of vaccine hesitancy were examined in one model using multiple regression analysis by the Enter method (P= 0.05).
Results: COVID-19 anxiety and fear have significant correlations with vaccine hesitancy (Phi=0.33, P=0.017; Phi=0.29, P=0.013, respectively). Anxiety and fear were higher among unhesitating participants (t =2.469, P=0.014; t=2.025, P=0.043, respectively). Participants who had previously been infected with coronavirus were more likely to be hesitant (X2 = 23.126, P=0.000). Participants who scored high in anxiety were more likely to be vaccinated (F=3.979, P=0.019) and have a secondary school or college education (F=4.903 P=0.002). COVID-19 anxiety, gender, and coronavirus infection significantly predicted vaccine hesitancy.
Conclusion: Anxiety and fear of COVID-19 are among the most important factors correlated with vaccine hesitancy; unhesitant people are more likely to have anxiety and fear. COVID-19 anxiety significantly predicted vaccine hesitancy. We recommend integrating psychological care into vaccination plans to help increase the uptake rate during potential subsequent pandemics. Relevant intervention programs can be designed to help increase vaccine acceptance, deal with vaccine hesitancy, and relieve psychological symptoms during major pandemics. Psychologists can provide awareness messages, counselling seminars, online mentoring, or telemental health outreach.
Introduction
The Coronavirus continues to pose major challenges to public health globally, with the emergence of new variants that need further efforts to contain and manage the virus. In this case, vaccinations are an important way to limit the spread of the COVID-19 pandemic. However, vaccine hesitancy is one of the most important and influential issues impeding efforts to contain the coronavirus; it is associated with other factors that have a direct or indirect impact on vaccine uptake, including psychological factors (1, 2). However, the association of COVID-19 vaccine hesitancy with mental health has not been well-examined in the Middle East and Arab countries. Therefore, it is important to identify these psychological factors to derive interventions and promote vaccine acceptance (3).
Several studies have found, during the COVID-19 pandemic, an increased prevalence of mental health disturbances, particularly anxiety, fears, and depression, among the general public or healthcare workers (1, 4). Although useful, the results of these studies did not go beyond the outbreak of the epidemic to the stage of vaccination, they addressed mental health disturbances without making a direct link to COVID-19 vaccine hesitancy, and their ability to explain why some individuals are reluctant to vaccinate is still limited (5).
Consistently, researchers have indicated that the observed increase in symptoms of anxiety and depression reported during the COVID-19 pandemic could have implications for vaccine hesitancy (6). However, there is a significant discrepancy in the results of previous studies that addressed this issue. For example, participants who reported feeling anxious, sad, and agitated every day due to social restrictions had high vaccine hesitancy, while those who reported the same feelings on only some days were less hesitant (7). Other studies documented that those reporting symptoms of anxiety or depression were less vaccine-hesitant (5).
Although it appears that anxiety, fear, and other psychological disorders are among the causes of vaccine hesitancy, the relationship between mental disorders and hesitation may be reciprocal. Concerns about the safety and effectiveness of the vaccine, and possible side effects, trigger vaccine hesitancy and resistance. Therefore, hesitant individuals are in direct confrontation with society and, as a result, are exposed to more stress and anxiety, the anticipation of potential risks, and other forms of psychological distress. Consistent with this point, it was found that individuals with a high risk of developing depression were more concerned about the efficacy and safety of the COVID-19 vaccine, which made them more reluctant to get vaccinated (8). Therefore, the most informative and effective approach in this area may be to recognize the underlying mechanisms of psychological morbidity that distinguish individuals who are reluctant to receive the vaccine from those who are not (5) – an approach based on studying the association of psychological symptoms with vaccine hesitancy. However, studies of mental health and its association with vaccine hesitancy are scarce; the evidence of significant correlations between symptoms of psychological disturbances and hesitation also remains limited (8), especially in the Middle East and Arab countries.
Given these gaps in the literature, this study aims to identify (1) the relationship between anxiety/fear of COVID-19 and vaccine hesitancy, (2) the relationship between COVID-19 infection and vaccine hesitancy, and (3) the degree to which COVID-19 anxiety and fear of COVID-19 predict vaccine hesitancy.
Methods
Participants and recruitment procedures
This study was based on the survey method to assess the relationship between COVID-19 anxiety/fear of COVID-19 and vaccine hesitancy. The survey was conducted online in the Arabic language in July 2021 and relied on self-reported data from a Saudi population who had already been offered vaccination (9). Participants were recruited online using the snowball technique, as the questionnaire was advertised in psychotherapy and mental health forums in Saudi Arabia. The questionnaire was sent via SMS message or email to individuals who provided their phone numbers or email addresses. Of the 2,113 individuals who were contacted via phone message or email, 558 participated in this study (with a response rate of 27.44%). All 558 respondents fully completed the questionnaire and there are no missing data in this study. However, the sample of this study may not be representative of the Saudi adult population.
Ethical considerations
All procedures in this study were consistent with the ethical standards of the 1964 Declaration of Helsinki or similar ethical standards. Participation in this research was voluntary, and the participants provided informed consent. The inclusion criteria included express written consent; a minimum age of 18 years; Arabic language proficiency; and current residency in Saudi Arabia.
Measures
Demographics
Demographic variables include (a) age, gender, education level, and marital status; and (b) vaccine-related variables including vaccine uptake, number of vaccine doses, vaccine hesitancy, and whether the participant was previously infected with the coronavirus. Age was classified into three gropes; young adults (18-37), middle-aged adults (38-47), and older adults (48-65) years. Gender was coded as “male” vs. “female.” Education level was coded as “secondary school,” “college graduate,” and “higher degree holders.” Marital status was classified as “single,” married, and “divorced/widowed.” Vaccine uptake was classified into three groups; “vaccinated,” “unvaccinated,” and “not decided yet”.
Vaccine hesitancy questionnaire
This questionnaire consists of four items designed in Arabic to assess COVID-19 vaccine hesitancy and related variables (e.g., COVID-19 infection, whether or not the person was vaccinated with a COVID-19 vaccine or was still hesitating, and the number of doses received if they were vaccinated). The response options are (“yes,” “no,” and “not sure”). Vaccine hesitancy was assessed with responses of “no” or “not sure”, while vaccine willingness was assessed with responses of “yes”.
COVID-19-anxiety questionnaire
The 10-item questionnaire was developed by Petzold et al. (10) to assess COVID-19 anxiety. The response options include five points on the Likert scale (1= ”strongly disagree,” 2=“disagree,” 3=“not sure,” 4=“agree,” and 5 = ”strongly agree”). The total score ranges from 10 to 50. The higher the overall score, the greater the anxiety. Petzold et al. (10) examined the psychometric properties of the scale and found good validity and reliability coefficients.
Fear of COVID-19 scale
This 7-item scale was developed by Ahorsu and his colleagues (11) to assess fear related to the coronavirus. The response options are on a 5-point Likert scale (1=“strongly disagree” to 5=“strongly agree”). The total score ranges from 7 to 35. The higher the overall score, the greater the fear of the coronavirus. This scale is valid, and its psychometric properties have been confirmed in several cultures (11).
In this study, we translated and validated the C-19-A and the FCV-19S into Arabic. The back-translated items were verified by two independent language experts who were bilingual in Arabic and English. The reliability of the scales was also examined in this study using Cronbach’s alpha. The scales showed good internal consistency (α=0.91) in the C-19-A, (α=0.91) in the FCV-19S, and (α=0.60) in the questionnaire of vaccine hesitancy. The Arabic versions of these scales are shown in the Appendix A.
Data analysis plan
Statistical analysis was conducted with IBM SPSS software (version 25). Descriptive analysis was calculated for all demographic variables (i.e., age, gender, education, and marital status) and vaccine-related variables (e.g., vaccination, number of vaccine doses, vaccine hesitation, and whether the participant was previously infected with the coronavirus). Pearson’s chi-square test (X2) was used to investigate the relationship between COVID-19 infection and vaccine uptake. The relationship between COVID-19 anxiety/fear of COVID-19 and vaccine hesitancy was calculated by the “Phi” coefficient. ANOVA and t-tests were used to examine the differences between participants in terms of anxiety and fear of COVID-19 according to demographic and vaccine-related variables (i.e., gender, age groups, education level, marital status; vaccine uptake, number of vaccine doses, and vaccine hesitancy). In the regression analysis, vaccine hesitancy was treated as a dependent variable and the predictive factors (COVID-19 anxiety, fear of COVID-19, demographics, and previous infection with the coronavirus) of vaccine hesitancy were examined in one model using multiple regression analysis by the Enter method (P= 0.05). The variables of age, gender, education, marital status, and coronavirus infection were included in the statistical analysis as categorical variables. These independent variables were entered into the analysis one by one, and the final model was obtained based on retaining the significant variables in the analysis (P= 0.05).
Results
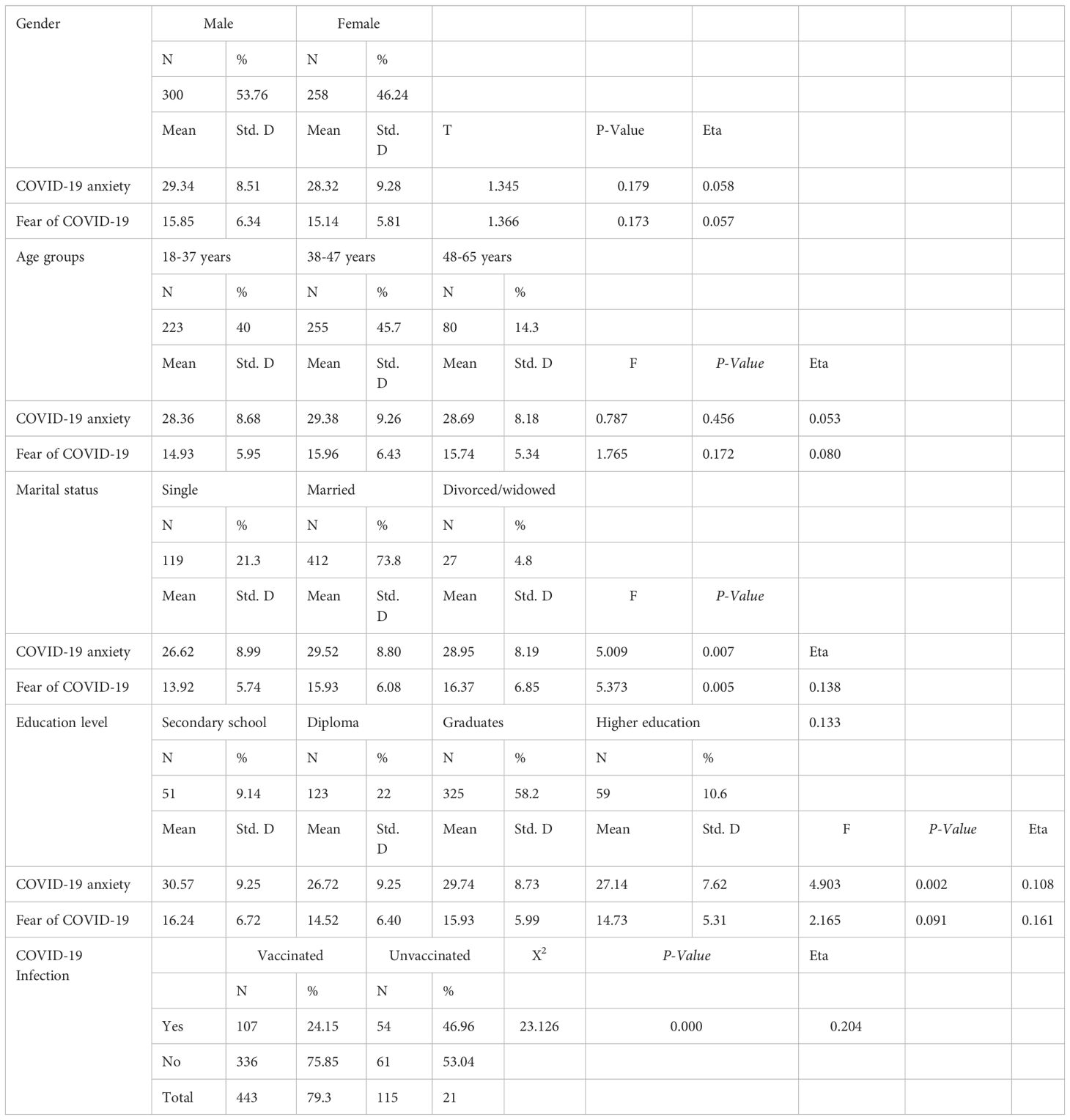
Table 1 presents the descriptive statistics of the sample (n= 558). The mean age was 38.66 ± 9.067 years (ranging from 18 to 65) and 53.8% of respondents were men. The majority of respondents (79%) indicated vaccine willingness, while 21% showed vaccine hesitancy.
As per Table 1, out of 443 (79.39%) vaccinated participants, 107 (24.15%) had previously been infected with the coronavirus, compared to 54 (46.95%) among the non-vaccinated. The differences in COVID-19 anxiety according to marital status and education levels were significant. COVID-19 anxiety was higher among married participants (F=5.009, P= 0.007), and among those who have a secondary school or college education (F=4.903, P= 0.002). Participants who had high fear of COVID-19 were more likely to be divorced (F=5.373, P= 0.005), while the differences in fear of COVID-19 according to education level were not significant (F=2.156, P= 0.091). The differences in anxiety and fear of COVID-19 were not significant according to the variables of age (F=0.787, P= 0.456; F= 1.765, P= 0.172, respectively), gender (t=1.345, P= 0.179; t=1.366, P< 0.173, respectively), and previous infection with the coronavirus (t=0.040, P= 0.968; t=1.913, P= 0.056, respectively).
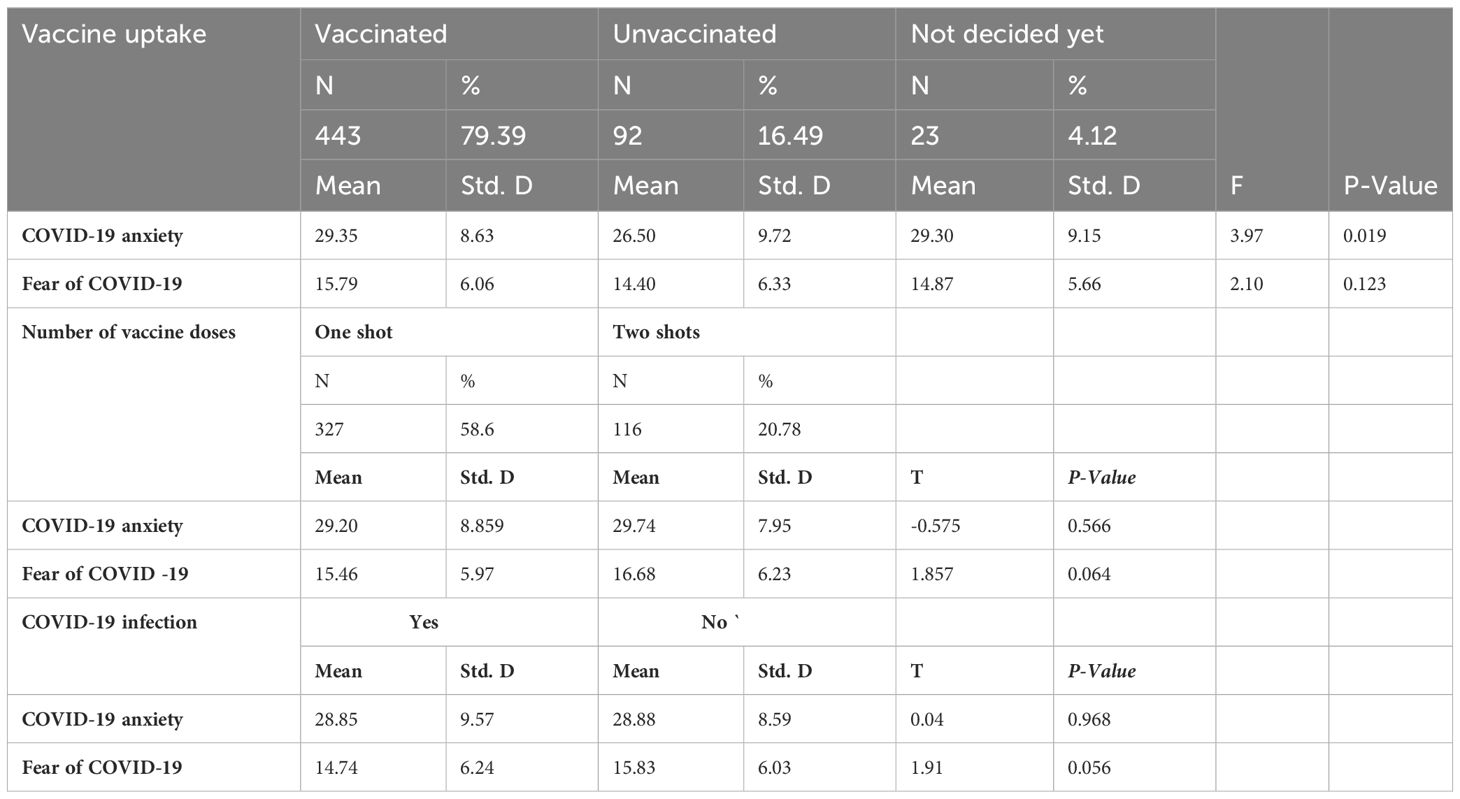
Table 2 presents the differences in Anxiety/fear of COVID-19 according to Vaccine-Related Variables.
As can be seen in Table 2, the differences in COVID-19 anxiety according to vaccine uptake (vaccinated, unvaccinated, and those who have not decided) were significant (F=3.979, P= 0.019). Vaccinated participants were more anxious than unvaccinated participants, while the differences in fear of COVID-19 according to vaccine uptake were not significant (F=2.102, P= 0.123). Meanwhile, the differences in anxiety and fear of COVID-19 according to COVID-19 infection were not significant (t= 0.040, P=0.968; t=1.913, P=0.056, respectively).
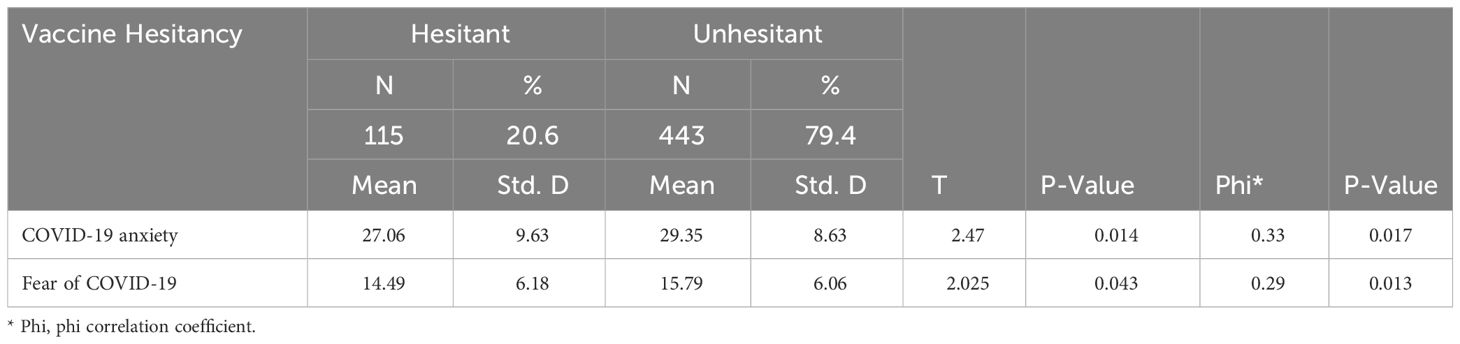
Correlations between anxiety/fear of COVID-19 and vaccine-related variables
Phi correlation (Phi) showed significant correlations between anxiety/fear of COVID-19 and vaccine hesitancy, as shown in Table 3:
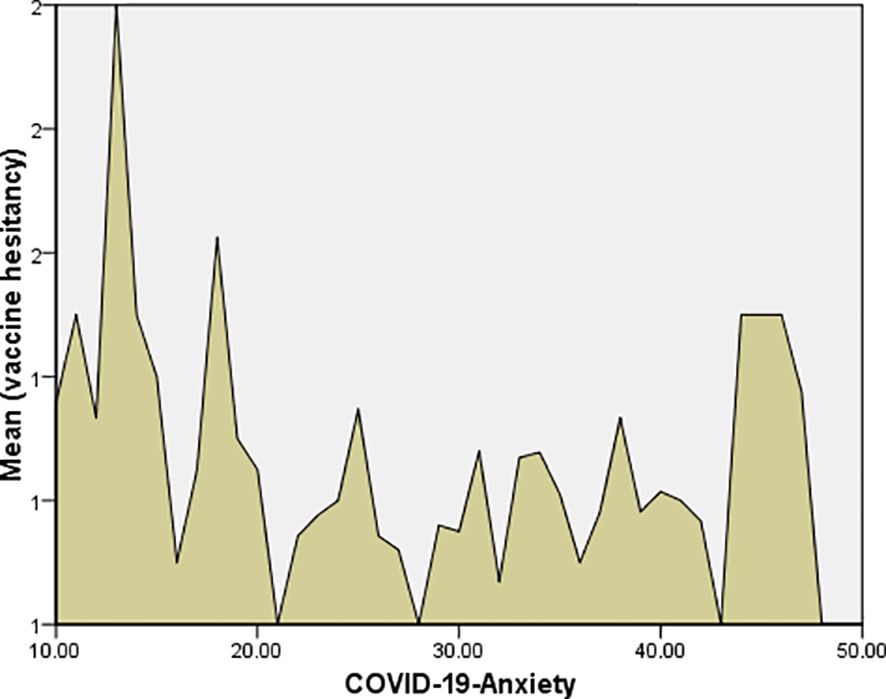
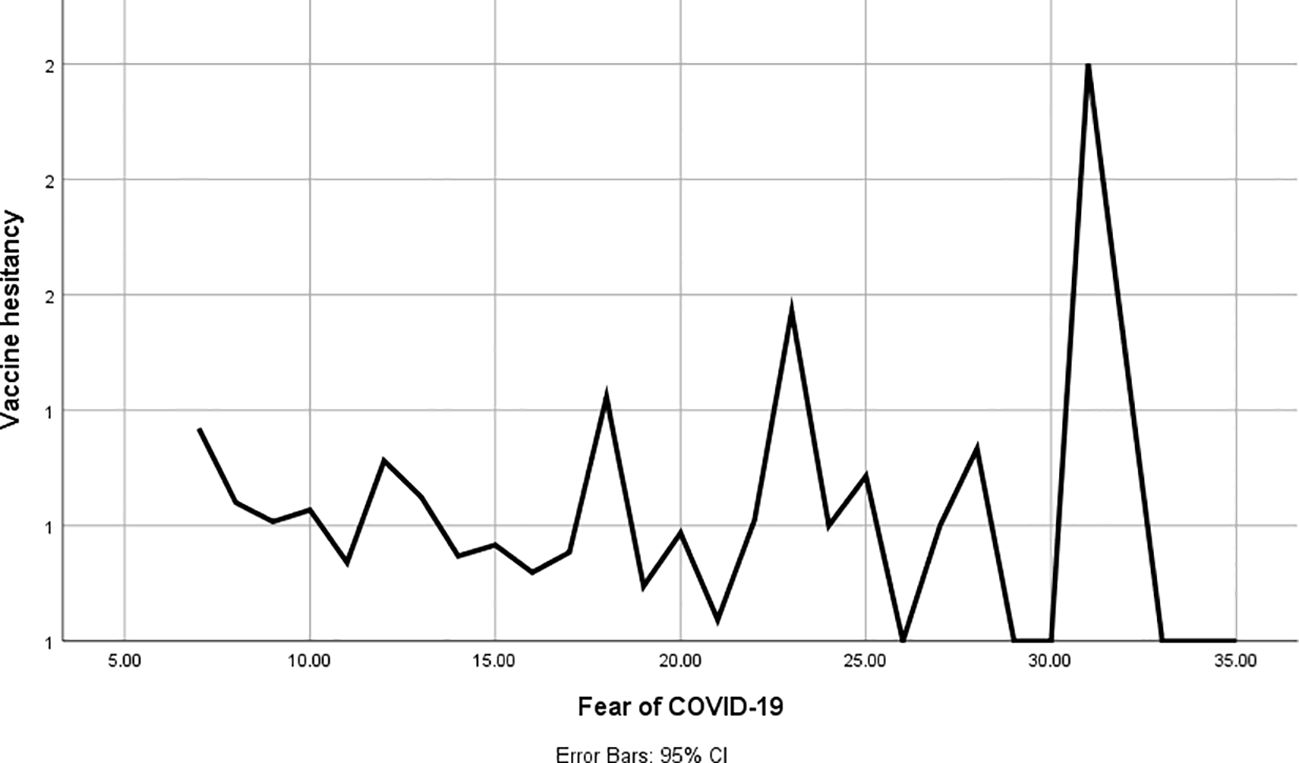
As per Table 3, the correlations between COVID-19 anxiety and fear of COVID-19 with vaccine hesitancy were significant (Phi=0.33, P=0.017; Phi=0.29, P=0.013). In addition, COVID-19 anxiety and fear of COVID-19 were higher among unhesitating participants, and the differences were significant (t= 2.469, P=0.014; t= 2.025, P=0.043, respectively), as shown in Figures 1 and 2.
Meanwhile, participants who had previously been infected with COVID-19 were more likely to be hesitant, and the differences were significant (X2 = 23.126, P= 0.000).
Degree to which COVID-19 anxiety and fear of COVID-19 predict vaccine hesitancy
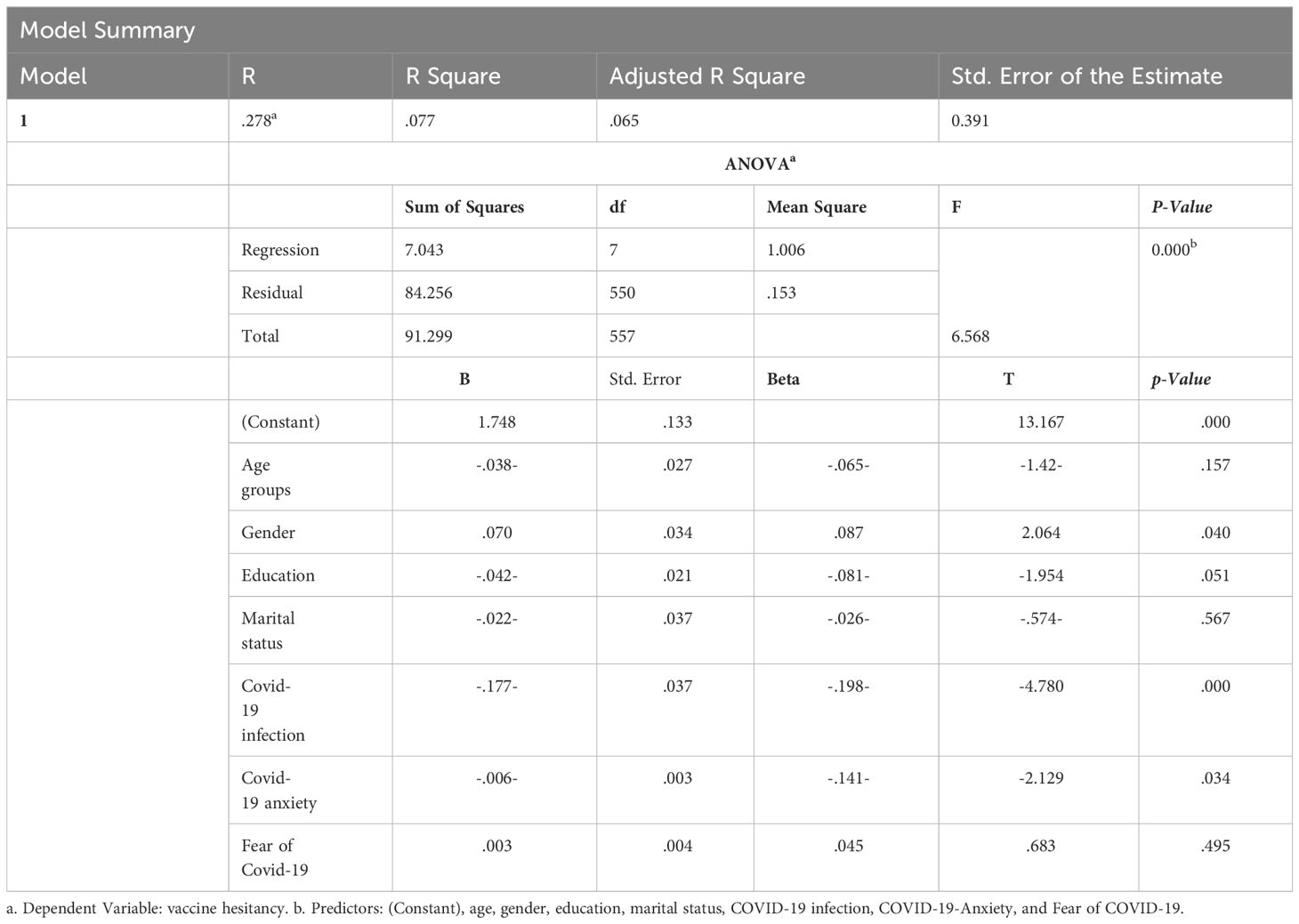
The predicting factors of vaccine hesitancy include COVID-19 anxiety, gender, and COVID-19 infection. These results are presented in Table 4.
As per Table 4, COVID-19 anxiety, gender, and previous coronavirus infection were significant predicted COVID-19 vaccine hesitancy.
Discussion
The present study examined the correlation between COVID-19 anxiety/fear of COVID-19 and vaccine hesitancy. The findings indicated that anxiety and fear of COVID-19 significantly explained vaccine hesitancy among Saudi adults. Anxiety and fear were high among unhesitating participants. Likewise, vaccinated people were more anxious than unvaccinated people, while there were no significant differences between vaccinated and unvaccinated participants regarding fear of COVID-19. These results should be reasonable, increased COVID-19 anxiety among vaccinated participants may be partly attributed to concerns about the efficacy and safety of the vaccine (2). It is expected that the side effects of COVID-19 vaccines will be higher among vaccinated people. As a result, unvaccinated persons may have fewer concerns regarding vaccine safety and effectiveness, which partly contributed to the significant differences between vaccinated and unvaccinated participants in the present findings.
Moreover, COVID-19 anxiety, gender, and previous infection with the Coronavirus statistically significantly predicted vaccine hesitancy, while COVID-19 fear and the variables of education and marital status did not predict vaccine hesitancy.
Although the regression model in Table 4 indicates relatively low values in the R-squared value at 0.077 and the adjusted R-squared value at 0.065, the total F value at (6.568) was high and significant at the 0.001 level, and this significance was reversed on the prediction values of the COVID-19 anxiety, gender, and previous infection with the Coronavirus that significantly predicted vaccine hesitancy. These results demonstrate the importance of the model despite the observed weaknesses which may be attributed to the role of variation among participants in the variables of fear of COVID-19, age, education, and marital status, as evidenced by the low predictive value of these demographic variables in explaining vaccine hesitancy in the current model. We acknowledge a limitation regarding the modest R-squared and adjusted R-squared values reported in our study, we have undertaken a comprehensive evaluation of our model’s capacity to account for variance in vaccine hesitancy. These values, while on the lower end of the spectrum, reflect the complex and multifactorial nature of vaccine hesitancy as a behavioral phenomenon. Despite the apparent limitations suggested by the R-squared values, the statistical significance of the predictors identified underscores their importance in understanding vaccine hesitancy.” Further studies will be urgently needed to clarify these effects.
On the other hand, these results are consistent with the results of previous studies that found that mental health problems are among the predictive factors of vaccine hesitancy (12, 13). Wang et al. (14) found that generalized anxiety disorder increased directly with vaccine hesitancy. Studies also have documented higher levels of psychological problems related to COVID-19 vaccinations, including anxiety, fear, and suicidal thoughts (15, 16). People with high levels of worry or anxiety were less hesitant about the COVID-19 vaccine, and vice versa (17). Other studies reported a significant correlation between fear of COVID-19 and vaccine hesitancy; the higher the fear of COVID-19, the lower the vaccine hesitancy (18, 19). Researchers also realize that people with anxiety or depression symptoms are less vaccine-hesitant (5). A total of 40% of those vaccinated against influenza indicated that they feared contracting COVID-19 (20), and the relationship between anxiety/fear of COVID-19 and vaccine acceptance was significant (3).
The significant correlations between COVID-19 anxiety/fear of COVID-19 and vaccine hesitancy that revealed in our results and indicated that anxiety and fear were high among unhesitating participants does not necessarily reflect a causal relationship between vaccine hesitancy and these psychological factors. Other factors may have played an important role in this relationship, including cultural variables and the social context in the Middle East and Arab countries, which led to the contradiction between our results and the results of some previous studies.
Contrary to the results of the current study, research found that the absence or presence of little fear of COVID-19 was significantly associated with vaccine hesitancy (21), and lower levels of depression were significantly associated with vaccine acceptance (22), while lower anxiety was associated with vaccine hesitancy (3, 19). Meanwhile, psychological distress was higher among COVID-19 vaccine-hesitating individuals (23), while a pre-pandemic diagnosis of anxiety, depression, or distress was unrelated to vaccine uptake (24). In addition, people who reported anxiety and anger during the lockdown and social restrictions were more hesitant, while those who experienced these feelings at specific periods were less hesitant (7).
The relationship between fear of COVID-19 and vaccine acceptance were not significant (3). Other studies did not find a significant relationship between COVID-19 vaccine hesitancy and mental health (25).
Our findings showed that COVID-19-Anxiety, gender, and coronavirus infection were significant predictors of vaccine hesitancy. Moreover, the correlation between COVID-19 anxiety and vaccine hesitancy was significant, indicating that an increase in hesitation corresponds with a decrease in COVID-19 anxiety, and vice versa. These results suggest that COVID-19 anxiety and fear may be among the reasons for receipt of the vaccine. Therefore, the higher the anxiety (or fear), the lower the vaccine hesitancy. We believe that anxiety is forcing people to protect themselves through vaccines. However, most causes of this phenomenon remain complex and unclear, as they include social, demographic, psychological, behavioral, and cultural factors (1, 2). Therefore, understanding the psychological factors that explain vaccine hesitancy is important for psychologists, healthcare workers, and authorities to improve vaccine acceptance. As reported in prior studies (1–4), psychological variables play a prominent role during the COVID-19 pandemic.
Consequently, it would be helpful to use these psychological variables to enhance the uptake rate in the future. In line with our results, lower level of fear and worsening health status were the predictive factors of vaccine hesitancy (7, 21). Prior studies indicated that anxiety, fears, and perceived psychological state had positive indirect effects on vaccine hesitancy (3, 26). Another study found a significant indirect effect of psychological distress on vaccine hesitancy via other factors, including risk perception and vaccine distrust (8). Predictive factors of vaccine willingness include fear of COVID-19 (27), age (2), more concerns about COVID-19, and few concerns about the vaccination (28). Additionally, anxiety, the fear of COVID-19, and perceived COVID-19 infectability were associated significantly with (3, 27).
The findings of the current study showed that coronavirus infection had a significant effect on vaccine hesitancy, as those who were previously infected were more hesitant than those who had never been infected with the coronavirus. These results may be partly attributed to the fact that those who have been infected with the coronavirus (particularly during the first wave of the pandemic) believe that they had acquired immunity against COVID-19, which will protect them from further infections in the future. In line with these findings, Hwang et al. (21) found that participants who perceived little risk of COVID-19 were more likely to be hesitant.
On the Contrary, studies showed that the lower perceived risk of coronavirus infection was associated with vaccine hesitancy (3, 7, 29). Participants who had previously been tested for COVID-19 were less likely to be vaccine-hesitant (30). The discrepancy between the results of these studies and our results may be due to methodological differences or to the differences in cultural and social contexts in which these studies were conducted.
The results of the present study showed that anxiety and fear of COVID-19 differ according to educational level in that they were higher among persons with a secondary school or college education than among persons with higher education, while COVID-19 anxiety was higher among married people. Meanwhile, participants who had high fear of COVID-19 were more likely to be divorced. These results may be because married people worry about their families contracting the coronavirus and because those with low educational levels are more likely to accept misinformation about the coronavirus and vaccination, as it was found that fear of COVID-19 decreased with higher levels of education (20). Increased fear of COVID-19 among divorced participants may be attributed to concerns about infection, particularly when alone (31). Contrary to the findings of the current study, the risk of anxiety was lower among married people (32).
Our findings provide important evidence about a potential mechanism regarding the significant effects of COVID-19 anxiety and fear of COVID-19 on vaccine hesitancy. These results present the importance of studying the association between psychological factors and vaccine hesitancy during major pandemics. Follow-up studies may be needed to evaluate symptoms of COVID-19 anxiety and fear after vaccinations, especially because it was pointed out that the first dose of the COVID-19 vaccine led to a significant improvement in the mental health of adults (33).
Conclusions
The results of this study indicate that anxiety and fear of COVID-19 are among the most important factors related to vaccine hesitancy; people who have received the coronavirus vaccine are more likely to have anxiety and fear, while anxiety and fear were high among unhesitating participants. Our results showed that COVID-19 anxiety and fear of COVID-19 differ according to the variables of marital status and educational level in that COVID-19 anxiety was high among married people and among those with secondary or university degrees. While the fear of COVID-19 was high among divorced individuals.
COVID-19-Anxiety, gender, and previous coronavirus infection were significant predictors of vaccine hesitancy. Participants who were previously infected were more hesitant than those who had never been infected with the coronavirus. Our findings could be valuable in a wide-ranging and better understanding of the psychological impacts of the COVID-19 pandemic. Therefore, we recommend integrating psychological care into vaccination plans in the future. Relevant intervention programs can be designed to help increase vaccine acceptance, deal with vaccine hesitancy, and relieve psychological symptoms during major pandemics. Psychologists can provide awareness messages, seminars and psychological counselling posters, or teletherapy outreach. Research evaluating the associations between psychological symptoms and vaccine hesitancy is highly needed to improve psychotherapy and mental health care planning during potential subsequent pandemics.
Strengths and limitations
The strength of the current study is that it seeks to reveal the relationship between anxiety/fear of COVID-19 and vaccine hesitancy, especially given that few studies exist in this area. However, this study has some limitations. In general, reliance on the self-report questionnaire has many shortcomings and deficiencies. Also, the non-representative sample of the Saudi community is a limitation that can be overcome in the methodologies of similar studies in the future. These limitations hinder the possibility of generalizing the results of the current study to the general adult population in the KSA. Moreover, the interactions of vaccination with anxiety and fear of COVID-19 may arise from one or several mechanisms. These effects are likely to be diverse and depend on characteristics beyond those analyzed in this study. In addition, the fact that people who receive the vaccines at different times differ in several psychological and socio-demographic characteristics suggests that the effects may differ from those of individuals vaccinated after the period of this study, as noted by Perez-Arce et al. (33). It is advisable to go beyond the limitations of the current research in similar prospective studies.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by The Research Ethics Committee at King Khalid University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
FF: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. NS: Conceptualization, Data curation, Investigation, Methodology, Project administration, Resources, Writing – original draft. MA: Data curation, Methodology, Project administration, Resources, Writing – original draft. AA: Data curation, Methodology, Project administration, Resources, Conceptualization, Investigation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1376567/full#supplementary-material
References
1. Palamenghi L, Barello S, Boccia S, Graffigna G. Mistrust in biomedical research and vaccine hesitancy: the forefront challenge in the battle against COVID-19 in Italy. Eur J Epidemiol. (2020) 35:785–8. doi: 10.1007/s10654-020-00675-8
2. Fadhel FH. Vaccine hesitancy and acceptance: an examination of predictive factors in COVID-19 vaccination. Health Promotion Int. (2022) 38(4). doi: 10.1093/heapro/daab209
3. Bendau A, Plag J, Petzold MB, Ströhle A. COVID-19 vaccine hesitancy and related fears and anxiety. Int Immunopharmacol. (2021) 97:107724. doi: 10.1016/j.intimp.2021.107724
4. Fadhel FH, Alqahtania MMJ, Arnout BA. Working with patients and the mental health of health care workers during the COVID-19 pandemic. WORK: A J Prevention Assess Rehabil. (2022) 72:27–38. doi: 10.3233/WOR-211134
5. Murphy J, Vallières F, Bentall RP, Shevlin M, McBride O, Hartman TK, et al. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat Commun. (2021) 12:29. doi: 10.1038/s41467-020-20226-9
6. Klinkhammer KE, Romm KF, Kerrigan D, McDonnell KA, Vyas A, Wang Y, et al. Sociopolitical, mental health, and sociodemographic correlates of COVID-19 vaccine hesitancy among young adults in 6 US metropolitan areas. Prev Med Rep. (2022) 27:101812. doi: 10.1016/j.pmedr.2022.101812
7. Soares P, Rocha JV, Moniz M, Gama A, Laires PA, Pedro AR, et al. Factors associated with COVID-19 vaccine hesitancy. Vaccines. (2021) 9:300. doi: 10.3390/vaccines9030300
8. Kollamparambil U, Oyenubi A, Nwosu CO. Mental Health, COVID-19 Vaccine Distrust and Vaccine Hesitancy in South Africa. USA: NIDS-CRAM (2021). Available at: https://mdpi-res.com/d_attachment/sustainability/sustainability-13-10248/article_deploy/sustainability-13-10248.pdf.
9. Ministry of Health. Daily statement. Saudi Arabia: Ministry of Health (2021). Available at: https://twitter.com/SaudiMOH/status/1455988274640588805.
10. Petzold MB, Bendau A, Plag J, Pyrkosch L, Maricic LM, Rogoll J, et al. Development of the COVID-19-Anxiety Questionnaire and first psychometric testing. BJPsych Open. (2020) 6:e91. doi: 10.1192/bjo.2020.82
11. Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH. The fear of COVID-19 scale: development and initial validation. Int J Ment Health Addict. (2020) 20:1537–45. doi: 10.1007/s11469-020-00270-8
12. Zheng YB, Sun J, Liu L, Zhao YM, Yan W, Yuan K, et al. COVID-19 vaccine-related psychological stress among general public in China. Front Psychiatry. (2021) 12:774504. doi: 10.3389/fpsyt.2021.774504
13. Maciaszek J, Lenart-Bugla M, Szcześniak D, Gawłowski P, Borowicz W, Misiak B, et al. Does mental health affect the decision to vaccinate against SARS-coV-2? A cross-sectional nationwide study before the vaccine campaign. Front Psychiatry. (2022) 13:810529. doi: 10.3389/fpsyt.2022.810529
14. Wang B, Zhong X, Fu H, He M, Hu R. COVID-19 vaccine hesitancy and GAD: The role of risk perception and vaccination status. Front Public Health. (2022) 10:994330. doi: 10.3389/fpubh.2022.994330
15. Pramukti I, Strong C, Sitthimongkol Y, Setiawan A, Pandin M, Yen CF, et al. Anxiety and suicidal thoughts during the COVID-19 pandemic: cross-country comparative study among Indonesian, Taiwanese, and thai university students. J Med Internet Res. (2020) 22:e24487. doi: 10.2196/24487
16. Alqahtani MMJ, Arnout BA, Fadhel FH, Sufian NS. Risk perceptions of COVID-19 and its impact on precautionary behavior: A Qualitative Study. Patient Educ Couns. (2021) 104:1860–7. doi: 10.1016/j.pec.2021.02.025
17. Kejriwal M, Shen K. COVID-19 vaccine hesitancy is positively associated with affective wellbeing. PsyArXiv. (2021). doi: 10.31234/osf.io/nkvhs
18. Huang Y, Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. (2020) 288:112954. doi: 10.1016/j.psychres.2020.112954
19. Chou W-YS, Budenz A. Considering Emotion in COVID-19 vaccine communication: addressing vaccine hesitancy and fostering vaccine confidence. Health Commun. (2020) 35:1718–22. doi: 10.1080/10410236.2020.1838096.14
20. Cori L, Curzio O, Adorni F, Prinelli F, Noale M, Trevisan C, et al. Fear of COVID-19 for individuals and family members: indications from the national cross-sectional study of the EPICOVID19 web-based survey. IJERPH. (2021) 18:3248. doi: 10.3390/ijerph18063248
21. Hwang SE, Kim WH, Heo J. Socio-demographic, psychological, and experiential predictors of COVID-19 vaccine hesitancy in South Korea, October-December 2020. Hum Vaccines immunotherapeutics. (2021) 18:1–8. doi: 10.1080/21645515.2021.1983389
22. Ryu S, Kang H, Jung HR, Yun H, Kang SH, Kim TS, et al. COVID-19 vaccine acceptance and related behavioral and psychological characteristics in individuals with mental disorders in Korea. Front Psychiatry. (2023) 14:1195103. doi: 10.3389/fpsyt.2023.1195103
23. Batty GD, Deary IJ, Fawns-Ritchie C, Gale CR, Altschul D. Pre-pandemic cognitive function and COVID-19 vaccine hesitancy: cohort study. Brain behavior Immun. (2021) 96:100–5. doi: 10.1016/j.bbi.2021.05.016
24. Batty GD, Deary IJ, Altschul D. Pre-pandemic mental and physical health as predictors of COVID-19 vaccine hesitancy: evidence from a UK-wide cohort study. medRxiv: preprint server Health Sci. (2021) 1:21256185. doi: 10.1101/2021.04.27.21256185
25. Butter S, McGlinchey E, Berry E, Armour C. Psychological, social, and situational factors associated with COVID-19 vaccination intentions: A study of UK key workers and non-key workers. Br J Health Psychol. (2022) 27:13–29. doi: 10.1111/bjhp.12530
26. Giuliani M, Ichino A, Bonomi A, Martoni R, Cammino S, Gorini A. Who is willing to get vaccinated? A study into the psychological, socio-demographic, and cultural determinants of COVID-19 vaccination intentions. Vaccines. (2021) 9:810. doi: 10.3390/vaccines9080810
27. Yahaghi R, Ahmadizade S, Fotuhi R, Taherkhani E, Ranjbaran M, Buchali Z, et al. Fear of COVID-19 and perceived COVID-19 infectability supplement theory of planned behavior to explain Iranians’ Intention to get COVID-19 vaccinated. Vaccines. (2021) 9:684. doi: 10.3390/vaccines9070684
28. Vollmann M, Salewski C. To Get Vaccinated, or Not to Get Vaccinated, That Is the Question: Illness Representations about COVID-19 and Perceptions about COVID-19 Vaccination as Predictors of COVID-19 Vaccination Willingness among Young Adults in The Netherlands. Vaccines. (2021) 9:941. doi: 10.3390/vaccines9090941
29. Fridman A, Gershon R, Gneezy A. COVID-19 and vaccine hesitancy: a longitudinal study. PloS One. (2021) 16:e0250123. doi: 10.1371/journal.pone.0250123.16
30. Salerno L, Craxì L, Amodio E, Lo Coco G. Factors Affecting Hesitancy to mRNA and Viral Vector COVID-19 Vaccines among College Students in Italy. Vaccines. (2021) 9:927. doi: 10.3390/vaccines9080927
31. Cullen W, Gulati G, Kelly BD. Mental health in the COVID-19 pandemic. QJM: Monthly J Assoc Physicians. (2020) 113:311–2.
32. Harjana N, Januraga PP, Indrayathi PA, Gesesew HA, Ward PR. Prevalence of Depression, Anxiety, and Stress among Repatriated Indonesian Migrant Workers during the COVID-19 Pandemic. Front Public Health. (2021) 9:630295. doi: 10.3389/fpubh.2021.630295
Keywords: anxiety, vaccine hesitancy, interrelationship, predicting factors, COVID-19
Citation: Fadhel FH, Sufyan NS, Alqahtani MMJ and Almaamari AA (2024) Anxiety and fear of COVID-19 as potential mechanisms to explain vaccine hesitancy among adults. Front. Psychiatry 15:1376567. doi: 10.3389/fpsyt.2024.1376567
Received: 25 January 2024; Accepted: 12 April 2024;
Published: 03 May 2024.
Edited by:
Haojie Fu, Tongji University, ChinaReviewed by:
Tarik Algalaly, Al-Azhar University, EgyptNajat Sayem Khalil, IRCICA Research Centre For Islamic History, Art and Culture, Türkiye
Copyright © 2024 Fadhel, Sufyan, Alqahtani and Almaamari. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fahmi H. Fadhel, fahmi@qu.edu.qa; fahmi4n@yahoo.com
†ORCID: Fahmi H. Fadhel, orcid.org/0000-0002-4497-7628
 Fahmi H. Fadhel
Fahmi H. Fadhel Nabil Saleh Sufyan
Nabil Saleh Sufyan Mohammed M. J. Alqahtani
Mohammed M. J. Alqahtani Ahmed Ali Almaamari
Ahmed Ali Almaamari