- 1Suki AI, Redwood City, CA, United States
- 2Santa Clara Valley Medical Center, San Jose, CA, United States
- 3Division of General Surgery, Department of Surgery, Stanford University School of Medicine, Stanford, CA, United States
- 4Hippocratic AI, Palo Alto, CA, United States
- 5The Permanente Medical Group, Oakland, CA, United States
- 6Stanford Cardiovascular Institute, Stanford University School of Medicine, Stanford, CA, United States
Background: Generative artificial intelligence (AI) tools are increasingly being used as “ambient scribes” to generate drafts for clinical notes from patient encounters. Despite rapid adoption, few studies have systematically evaluated the quality of AI-generated documentation against physician standards using validated frameworks.
Objective: This study aimed to compare the quality of large language model (LLM)-generated clinical notes (“Ambient”) with physician-authored reference (“Gold”) notes across five clinical specialties using the Physician Documentation Quality Instrument (PDQI-9) as a validated framework to assess document quality.
Methods: We pooled 97 de-identified audio recordings of outpatient clinical encounters across general medicine, pediatrics, obstetrics/gynecology, orthopedics, and adult cardiology. For each encounter, clinical notes were generated using both LLM-optimized “Ambient” and blinded physician-drafted “Gold” notes, based solely on audio recording and corresponding transcripts. Two blinded specialty reviewers independently evaluated each note using the modified PDQI-9, which includes 11 criteria rated on a Likert-scale, along with binary hallucination detection. Interrater reliability was assessed using within-group interrater agreement coefficient (RWG) statistics. Paired comparisons were performed using t-tests or Mann–Whitney tests.
Results: Paired analysis of 97 clinical encounters yielded 194 notes (2 per encounter) and 388 paired reviews. Overall, high interrater agreement was observed (RWG > 0.7), with moderate concordance noted in pediatrics and cardiology. Gold notes achieved higher overall quality scores (4.25/5 vs. 4.20/5, p = 0.04), as well as superior accuracy (p = 0.05), succinctness (p < 0.001), and internal consistency (p = 0.004) compared to ambient notes. In contrast, ambient notes scored higher in thoroughness (p < 0.001) and organization (p = 0.03). Hallucinations were detected in 20% of gold notes and 31% of ambient notes (p = 0.01). Despite these limitations, reviewers overall preferred ambient notes (47% vs. 39% for gold).
Conclusion: LLM-generated Ambient notes demonstrated quality comparable to physician-authored notes across multiple specialties. While Ambient notes were more thorough and better organized, they were also less succinct and more prone to hallucination. The PDQI-9 provides a validated, practical framework for evaluating AI-generated clinical documentation. This quality assessment methodology can inform iterative quality optimization and support the standardization of ambient AI scribes in clinical practice.
Introduction
Physicians and health systems are rapidly adopting software applications that employ large language models (LLMs) to support clinical note writing during patient encounters (Cain et al., 2025; Shah et al., 2025b; Stults et al., 2025). Available software functions similarly to medical scribes—previously shown to improve physician satisfaction and productivity (Gidwani et al., 2017)—but offers lower cost and greater scalability. In principle, scribe software is most beneficial when it generates a high-quality draft note, as physicians must still review and edit the draft before finalizing it in the medical record. Despite its numerous advantages, the introduction of LLM-generated clinical notes raises important questions about documentation quality, particularly given the field-specific requirements and expectations of medical records. Prior studies have established two validated instruments for evaluating physician note quality: PDQI-9 (Stetson et al., 2012) and Q-Note (Burke et al., 2014). However, these tools have not yet been systematically applied to LLM-generated notes or assessed through specialist review.
Ambient scribes are LLMs that passively capture and interpret conversations to extract meaningful, structured content, enabling clinicians to focus on the patient interactions. Suki is an ambient clinical documentation system that summarizes audio-recorded medical interactions into structured clinical notes. This scribing process involves three major steps: (1) integrating with the physician’s electronic health record (EHR) to retrieve information about the patient and encounter context, (2) transcribing the conversation between the doctor, patient, and any other visit participants, and (3) generating a summary of this information, as appropriate for the Suki user’s specialty, in the form of a structured clinical note. Both proprietary and fine-tuned third-party language models are employed to perform this functionality.
In this study, we assessed the utility of a standardized quality assessment tool to compare the perceived quality of LLM-generated “Ambient” clinical notes with notes drafted by board-certified specialists across five clinical domains. Notes were then evaluated by blinded experts within each respective field.
Methods
We retrospectively queried Suki’s production database from October 2024 to compile de-identified clinical encounters across five specialties: general medicine, pediatrics, obstetrics and gynecology, orthopedic surgery, and adult cardiology. Audio recordings for these encounters were transcribed using automated speech recognition (ASR) via Amazon Web Services (AWS), with medical diarization applied to separate speaker turns. To ensure that all audio recordings were fully anonymized, a team of operations specialists systematically reviewed both the audio recordings and their transcripts, selecting only the encounters that had no personal health information (PHI) capable of identifying patients. We also excluded encounters with audio duration shorter than 1 min, recordings with very poor audio quality that prevented the ability to produce a transcript, and encounters conducted in a non-English language. Of 930 visits screened, 126 met the eligibility criteria. From these, the first 20 qualifying encounters per specialty were randomly selected, reserving the remaining visits as back-ups. The software then provided the visit transcript, along with limited information about the patient and clinician, to an LLM to create an “Ambient” note for each encounter. In obstetrics and gynecology (OB/Gyn), three visits were subsequently excluded because patient audio was not recorded during telehealth visits.
Note reviewers
To provide reference documentation for each encounter, physician specialists were recruited from each medical field to draft notes, termed “Gold notes.” The Gold note author had access to the same inputs as the LLM, including the audio recording and transcript. No Gold note authors were directly involved in the index patient encounter to ensure that both the Gold and Ambient notes were generated from identical source material.
Quality assessments
Two board-certified clinicians were recruited to evaluate the Ambient and Gold notes. As with the Gold note authors, the evaluators represented the relevant medical specialties and included board-certified physicians, fellows, residents, and non-physician advanced practice providers. Evaluators had access to the encounter audio, transcript, and patient and clinician information, but were blinded to the origin of the two notes—they were asked to evaluate notes written by “Model 1” and “Model 2.”
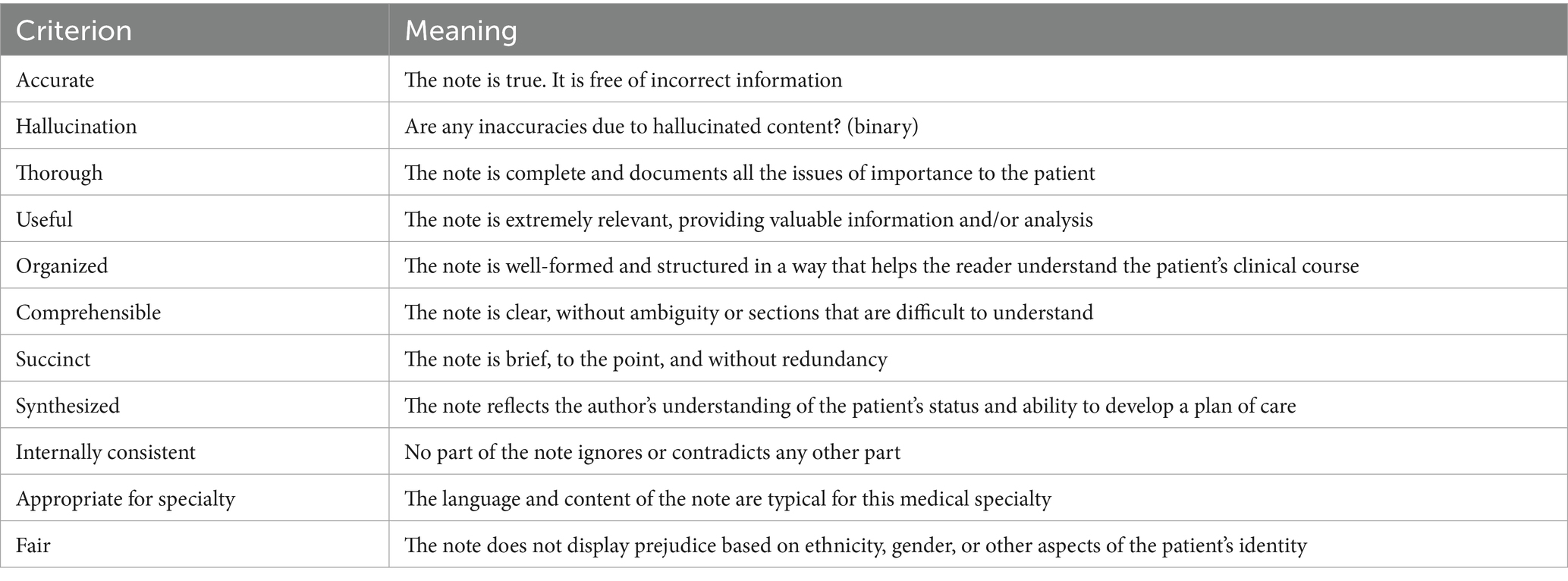
Evaluators rated each note using the criteria outlined in Table 1, based largely on the PDQI-9 instrument. PDQI-9 was selected over Q-Note due to its greater flexibility across diverse clinical settings. Notably, PDQI-9 was “not designed to assess the presence or absence of specific note components (e.g., “reason for admission” in an admission note),” ensuring broader applicability. Instead, it uses subjective Likert-scale ratings by physicians, similar to other frameworks proposed for the evaluation of LLMs in healthcare (Tam et al., 2024). A prior validation exercise of PDQI-9 was carried out using internal medicine admission notes (Stetson et al., 2012).
Quality assessment
For note quality assessment, we adopted 8 of the 9 questions from the original PDQI-9, excluding the “Up to date” criterion owing to lack of relevance to the AI scribe context. We also added “Appropriateness for specialty” and “Fair” as additional criteria, along with a qualifier for “Accuracy” to indicate whether any inaccuracies were due to “Hallucination.” Each criterion was rated on a Likert scale from 1 to 5, where 5 = “Extremely” and 1 = “Not at all,” except the Hallucination criterion, which was either “Present” or “Absent.” Evaluators also provided their overall preference between the two notes by specifying “Model 1,” “Model 2,” or “I prefer both equally.”
Statistical analysis
For all pairwise comparisons, the Shapiro–Wilk test for normality was performed to determine the most appropriate statistical test. All pairwise factors exhibiting a parametric distribution were evaluated using the Student’s t-test with Benjamini-Hochberg adjustment; otherwise, a Mann–Whitney test was used. All data are reported as mean ± standard deviation unless otherwise specified. Statistical analyses and data visualization were performed using GraphPad Prism version 10.4.0 for macOS (GraphPad Software, San Diego, CA) and R version 4.4.2 (R Foundation for Statistical Computing, Vienna, Austria). Statistical significance was assigned when p < 0.05 unless otherwise specified. Within-group agreement was assessed using the RWG score, which quantifies consensus among raters by comparing observed variance to expected random variance, as previously described (James et al., 1984). Specifically, the rWG statistic is defined as rWG = 1 – (Sx2 / σEU2), where Sx2 is the observed variance and σEU2 is the expected variance under a uniform distribution.
Results
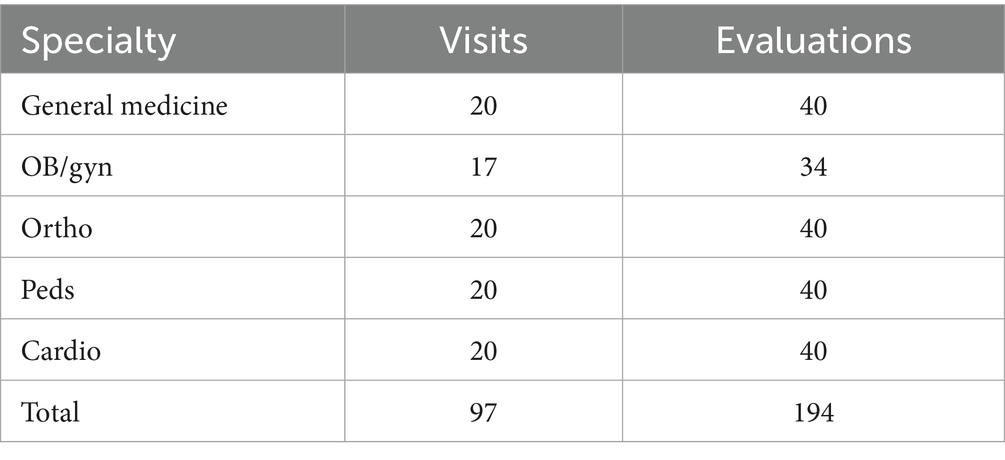
To better characterize the relative performance of our AI-generated medical dictation platform, termed “Ambient” notes, compared to those written by clinical experts, audio and transcripts from 97 patient visits were included in this study (Figure 1). Experts from five medical specialties drafted notes based on the 20 patient encounters (17 in OB/Gyn) within their field, termed “Gold” notes (Table 2). For each visit, a Gold note and an Ambient note were scored, each by two clinical expert evaluators, yielding a total sample size of 388 notes for our analysis.
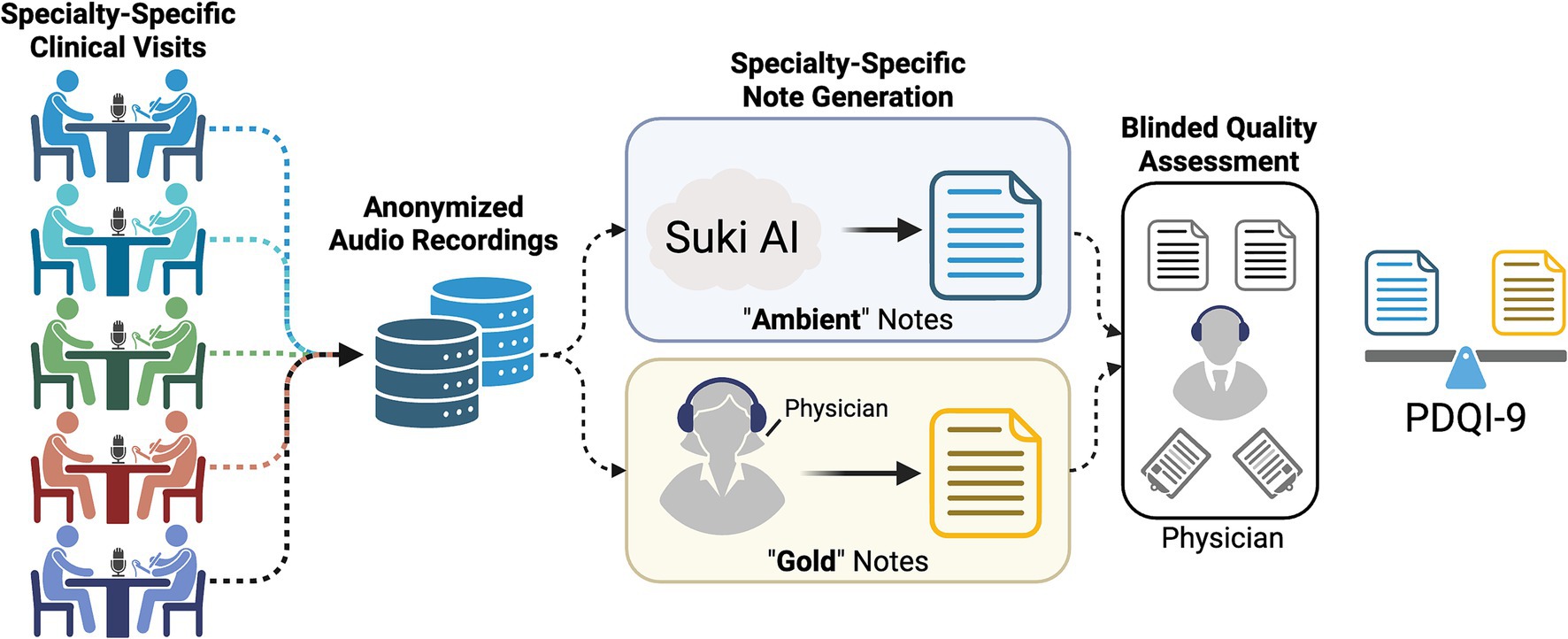
Figure 1. Graphical summary of cloud-based (Ambient) quality assessment relative to field expert (Gold) clinical documentation. Clinical encounters were audio-recorded and anonymized prior to distribution for a paired clinical summary via Suki-based AI and a board-certified physician. The clinical encounter notes were then assessed for quality using the modified PDQI-9 metric.
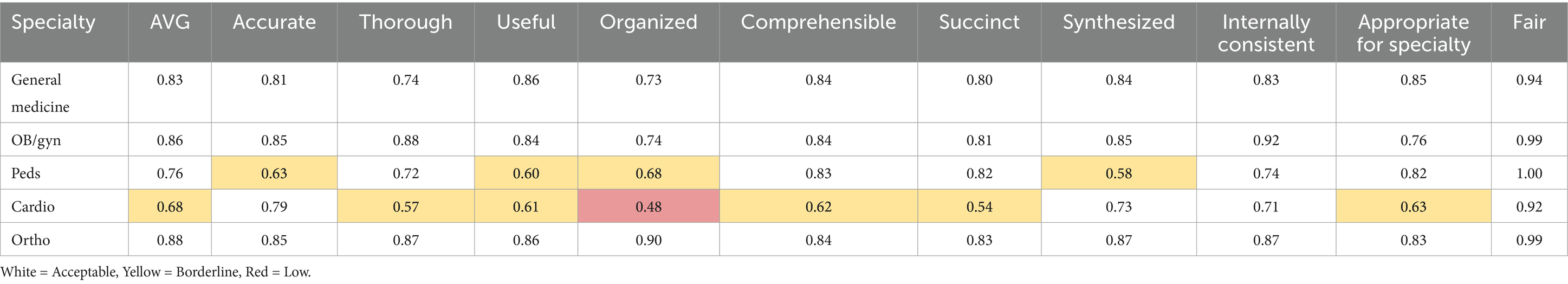
Agreement between the two evaluators was uniformly high (RWG > 0.7) across all criteria in general medicine, OB/Gyn, and orthopedic notes (Table 3). In pediatrics, there was moderate interrater agreement (RWG 0.5–0.7) for 4 of 11 criteria, and other criteria had high agreement. In cardiology, there was moderate agreement for 6 of 11 criteria, and poor interrater agreement (RWG < 0.5) for the Organized criterion.
Average scores across all notes and between the two evaluators within each specialty are listed for each of the modified PDQI-9 criteria (Table 4). There was a statistically significant preference for Gold notes over Ambient notes on the Accurate (p = 0.05), Succinct (p < 0.001), and Internally Consistent (p = 0.004) criteria. Ambient notes were preferred over Gold notes on the Thorough (p < 0.001) and Organized (p = 0.03) criteria. For other criteria (Useful, Comprehensible, Synthesized, Appropriate for Specialty, and Fair), the differences were not statistically significant. An overall average of score across all of the modified PDQI items slightly favored Gold notes at 4.25, vs. 4.20 for Ambient notes (p = 0.04).
Regarding Hallucination, evaluators identified Hallucinations in both Gold and Ambient notes, with the presence of Hallucination identified in 20% of Gold notes, vs. 31% of Ambient notes (p = 0.01). The average RWG score for the binary Hallucination criterion was 0.94, confirming high interrater agreement for this question.
Analysis of per-specialty average scores for each quality criterion showed that all specialties consistently viewed Ambient notes as more thorough, although this difference reached statistical significance only in cardiology and pediatrics (Figure 2). In general, specialists in OB/Gyn and pediatrics tended to favor the Gold notes, whereas those in general medicine, orthopedics, and cardiology tended to favor the Ambient notes. The specialty preference observed in the modified PDQI-9 criteria aligned with the single-question response from evaluators regarding their overall note preferences specifically.
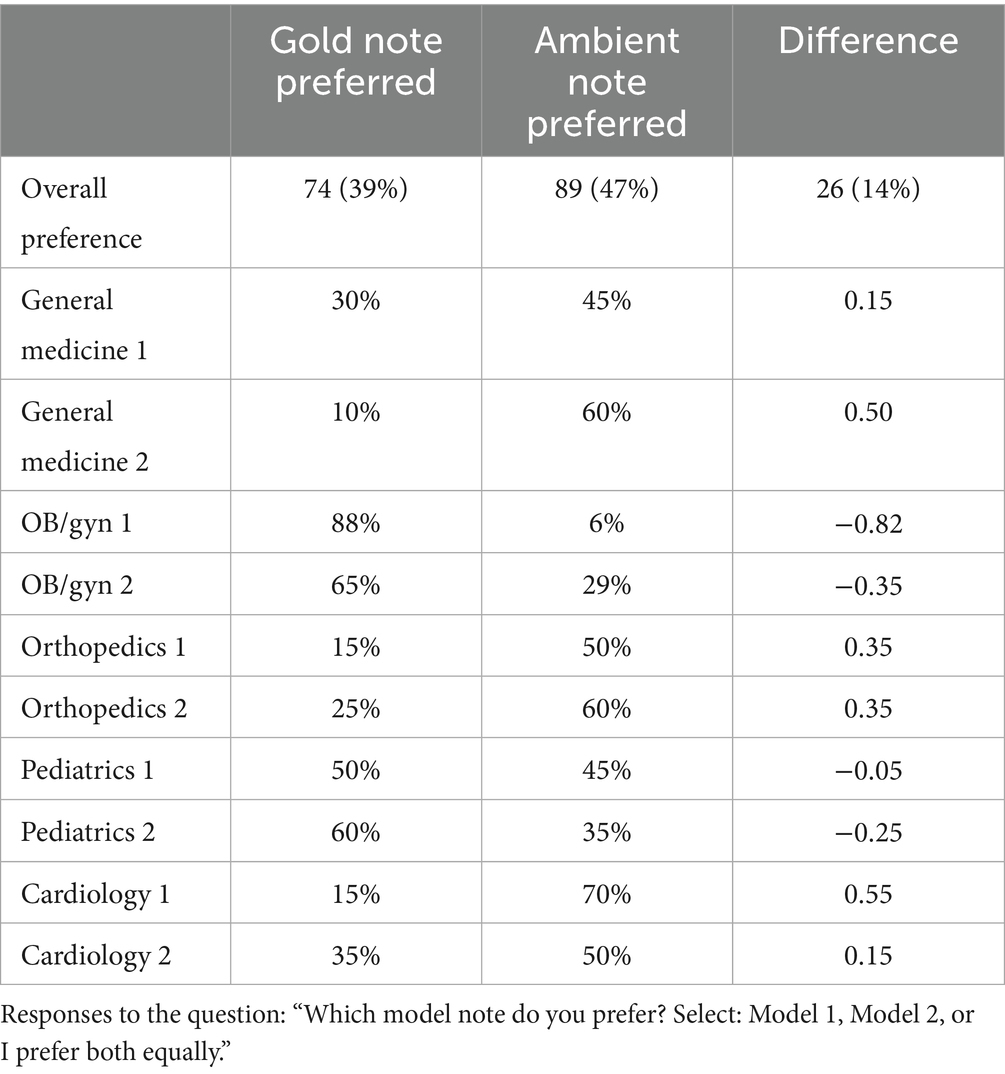
The Overall Note Preference question favored Ambient notes more often (Table 5). This preference contrasts with the average PDQI scores, which favored the Gold notes (4.25 vs. 4.20 for Ambient notes, p = 0.04). Differences in average ratings across specialties, shown in Figure 1, vary between different specialties and are not reflected in the overall averages for the combined sample.
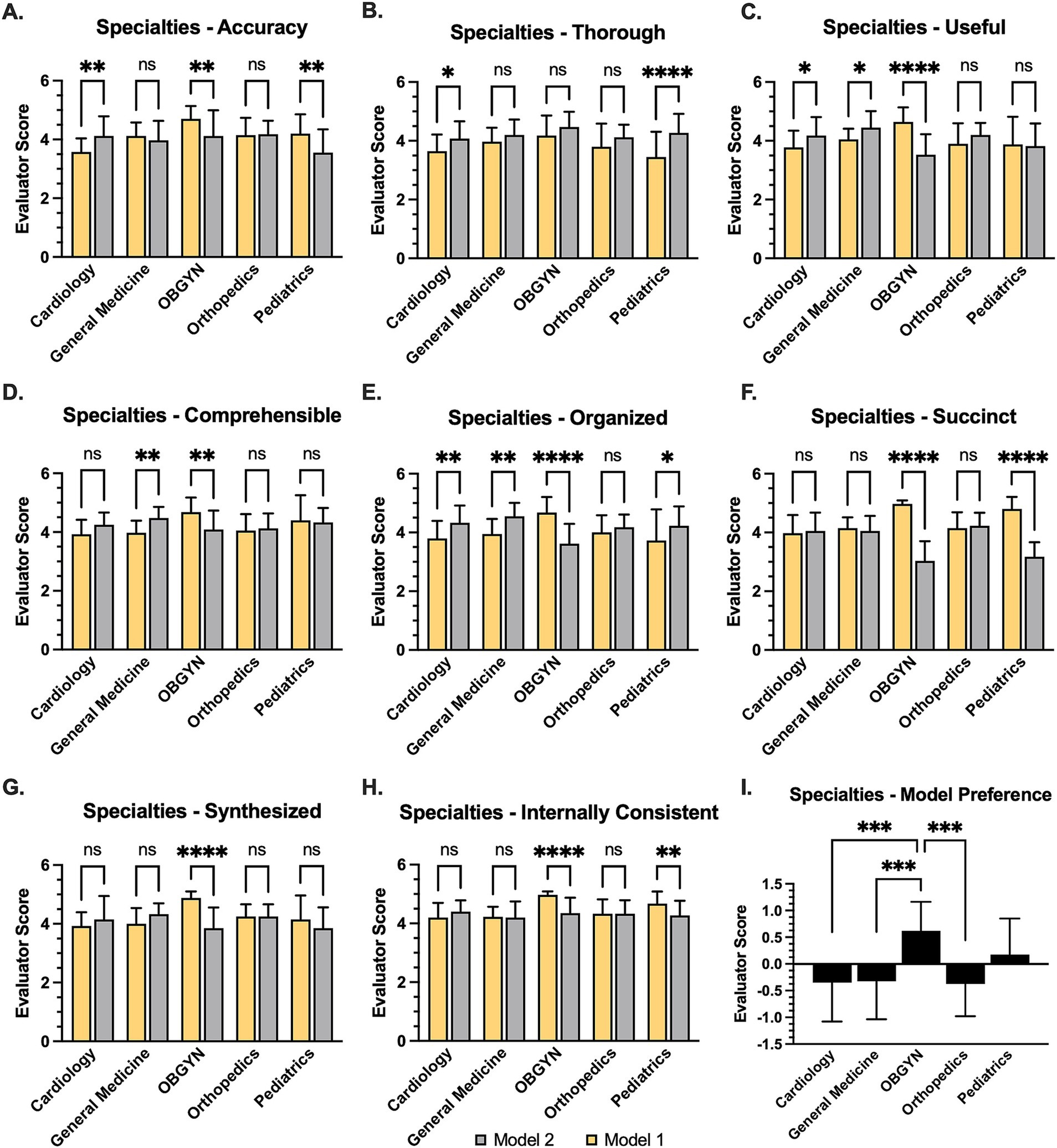
Figure 2. Relative evaluations for AI-generated notes across medical specialties. (A) Bar graph of AI-generated “Ambient” (Model 1) note relative to reference “Gold” note (Model 2) according to Likert scale, also showing (B) Thoroughness, (C) Usefulness, (D) Comprehensibility, (E) Organization, (F) Succinctness, (G) degree of synthesis, and (H) internal consistency. *statistical significance was assumed at p < 0.05 based on paired Student’s t-test (A–H) or 1-way analysis of variance (I) Bar graph illustrating evaluator preference, wherein 1 = Gold note and -1 = Ambient note. Statistical significance was based on student’s t-test at p < 0.01, **p < 0.01, ***p < 0.001, p < 0.0001.
Discussion
The introduction of automated note-writing and clinical summary tools has the potential to streamline the administrative burden facing clinicians by generating clinical documents that accurately summarize patient encounters. Early reports suggest that ambient AI scribes can improve workflow efficiency and physician satisfaction while decreasing after-hours charting demands (Duggan et al., 2025; Ma et al., 2025; Shah et al., 2025b; Stults et al., 2025). These results align with long-standing evidence that electronic health record (EHR)-related clerical load contributes to after-hours work and clinician burnout, underscoring the motivation for automation that can safely offload documentation tasks (Shanafelt et al., 2016; Sinsky et al., 2016; Tai-Seale et al., 2017). Nevertheless, the accuracy and safety of notes generated by large language models (LLMs) remain currently limited by known issues, including hallucinations and excessive detail. Recent reviews and methodological papers emphasize the need for standardized validation frameworks to evaluate content quality and safety before widespread deployment (Asgari et al., 2025; Shool et al., 2025; Ergun and Sefer, 2025). This highlights the urgent necessity for standardized validation frameworks to assess clinical documentation produced by AI (Leung et al., 2025). In this study, we adopted an externally validated note quality instrument to assess the relative quality of LLM-generated ambient clinical scribes.
In our results, Ambient notes did not consistently underperform relative to physician-authored notes. Although Gold notes had a modestly higher average quality score overall (4.25 vs. 4.20), Ambient notes outperformed Gold notes on specific criteria, particularly Thoroughness and Organization, indicating that LLMs excel at capturing comprehensive encounter details. Conversely, physician notes scored higher on Succinctness, reflecting greater concision, and on Accuracy and Internal Consistency, underscoring the human advantage in synthesizing information while avoiding redundancy or contradictions. These findings align with recent evaluations of ambient AI documentation systems, which demonstrated improvements in completeness (Chong et al., 2022; Duggan et al., 2025; Genes et al., 2025), but highlighted challenges with accuracy and verbosity (Burke et al., 2014; Cain et al., 2025; Shah et al., 2025a; Wang et al., 2025). Recognizing these trade-offs underscores current implementation strategies, where ambient AI can reduce drafting time yet still necessitate clinician review to ensure clarity and precision (Duggan et al., 2025; Shah et al., 2025a, 2025b).
By implementing a peer-review process of comparing Ambient and Gold clinical notes, we have established a reproducible method for understanding note quality and identifying areas for improvement. The finding that Gold notes did not consistently perform better than Ambient notes was unexpected. Although Gold notes scored slightly higher on global average scores, Ambient notes outperformed the human-authored notes on certain criteria, such as Thoroughness, indicating Ambient notes captured more details of the discussion. Conversely, Gold notes were rated higher for Succinctness, reflecting the tendency of the LLM to be more verbose. Further qualitative research is required to better understand physicians’ preferences regarding the balance between Thoroughness and Succinctness.
Strengths of this study include adopting a previously validated instrument, the PDQI-9 (Stetson et al., 2012), which applies well to this generative AI use case with few modifications, similar to approaches in other contexts (Stetson et al., 2008; Walker et al., 2017; Lyons et al., 2024). By applying blinded, specialty-matched reviewers and reporting interrater agreement with rWG, we provide a reproducible process for comparative assessment of AI-generated and clinician notes. By analyzing interrater agreement for both the externally validated PDQI criteria and the three criteria that were added, we provide a reproducible process for comparative assessment of AI-generated and clinician notes. We did find a lower level of agreement between our cardiology evaluators, and on further exploration, we found that one of the cardiology evaluators was a “hard grader”—their scores were consistently lower than the other evaluators’ scores. In the context of our comparison between Gold and Ambient notes, which used the average of the two evaluators’ scores to compare note quality, the “hard grader” issue is not a limitation. However, it limits the ability to compare scores across specialties. In the future, mitigations such as evaluator training or score normalization can be explored. Nevertheless, the rWG-type agreement indices and multiple-comparison controls remain appropriate for Likert-scale rater data and multi-endpoint analyses, respectively (Benjamini et al., 2001; Cohen et al., 2001).
This study has several important limitations that warrant future studies to address them. Each specialty relied on a single “Gold” note author, which raises the possibility that observed differences reflect variation in individual documentation quality rather than inherent differences between specialties; for this reason, our ability to assess within-specialty comparative quality is limited. This effect was particularly pronounced in OB/Gyn. Second, our analysis was limited to a single production LLM pipeline, which ensured internal validity by assessing a system in active clinical use, and yet this approach precludes both benchmarking across LLM architectures and formal ablation of system components. Finally, although our sample size of 97 is modest, future applications should include larger and multi-institutional studies to reflect the spectrum of clinical variation across clinical contexts.
Conclusion
This study has demonstrated how a previously validated instrument for evaluating note quality, the PDQI-9, can be used with minor adaptations to evaluate the quality of LLM-generated clinical notes. It further establishes a methodology for comparing the quality of physician-authored notes to LLM-authored notes via expert clinical review. As expected, physician-authored notes outperformed LLM-authored notes overall, although LLM-authored notes were found to be more Thorough and Organized. More important than the numeric quality results for this static dataset—comprising notes authored in October 2024 and already somewhat outdated due to rapid advancements in LLM technology—is the establishment of a methodology that developers can leverage to identify opportunities for improving the quality of LLM-generated clinical notes.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical approval was not required for the studies involving humans because Ethical approval was not required for this study because all data consisted of de-identified, retrospective audio recordings and transcripts that were systematically screened to ensure the absence of protected health information (PHI). No patient identifiers were included, and no interventions or direct patient contact occurred. As such, the study did not meet the criteria for human subjects research requiring institutional review board (IRB) approval. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
EP: Data curation, Validation, Investigation, Conceptualization, Methodology, Software, Supervision, Writing – review & editing, Resources, Visualization, Project administration, Writing – original draft, Funding acquisition, Formal analysis. AM: Methodology, Data curation, Writing – review & editing, Formal analysis. HM: Methodology, Writing – review & editing, Project administration, Conceptualization. SB: Formal analysis, Methodology, Software, Writing – review & editing, Investigation. MP: Supervision, Project administration, Conceptualization, Investigation, Validation, Data curation, Writing – review & editing, Methodology, Writing – original draft, Formal analysis, Software, Visualization.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. Publication fees for this work were funded in part by Suki AI. The funder was not involved in the study design, collection, analysis, interpretation of data, the writing of this article, or the decision to submit it for publication.
Conflict of interest
All authors disclose consulting or other commercial relationships with Suki AI. HM was employed at Hippocratic AI.
Generative AI statement
The authors declare that Gen AI was used in the creation of this manuscript. The authors have used generative AI for proof-reading to ensure typos and grammatic errors have been addressed.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Asgari, E., Montaña-Brown, N., Dubois, M., Khalil, S., Balloch, J., Yeung, J. A., et al. (2025). A framework to assess clinical safety and hallucination rates of LLMs for medical text summarisation. NPJ Digit. Med. 8:274. doi: 10.1038/s41746-025-01670-7
Benjamini, Y., Drai, D., Elmer, G., Kafkafi, N., and Golani, I. (2001). Controlling the false discovery rate in behavior genetics research. Behav. Brain Res. 125, 279–284. doi: 10.1016/s0166-4328(01)00297-2
Burke, H. B., Hoang, A., Becher, D., Fontelo, P., Liu, F., Stephens, M., et al. (2014). QNOTE: an instrument for measuring the quality of EHR clinical notes. J. Am. Med. Inform. Assoc. 21, 910–916. doi: 10.1136/amiajnl-2013-002321
Cain, C. H., Davis, A. C., Broder, B., Chu, E., DeHaven, A. H., Domenigoni, A., et al. (2025). Quality assurance during the rapid implementation of an AI-assisted clinical documentation support tool. NEJM AI 2. doi: 10.1056/aics2400977
Chong, A. Z., Lee, B., Hollenbach, K., and Kuelbs, C. L. (2022). Disappearing help text: implementing a note-based tool for in-line clinical decision support and note bloat reduction. Appl. Clin. Inform. 13, 1033–1039. doi: 10.1055/a-1934-8323
Cohen, A., Doveh, E., and Eick, U. (2001). Statistical properties of the rWG(J) index of agreement. Psychol. Methods 6, 297–310. doi: 10.1037/1082-989x.6.3.297
Duggan, M. J., Gervase, J., Schoenbaum, A., Hanson, W., Howell, J. T. 3rd, Sheinberg, M., et al. (2025). Clinician experiences with ambient scribe technology to assist with documentation burden and efficiency. JAMA Netw. Open 8:e2460637. doi: 10.1001/jamanetworkopen.2024.60637
Ergun, Z. E., and Sefer, E. (2025). Finsentiment: predicting financial sentiment through transfer learning. Intell. Syst. Account. Finance Manag. 32. doi: 10.1002/isaf.70015
Genes, N., Sills, J., Heaton, H. A., Shy, B. D., and Scofi, J. (2025). Addressing note bloat: solutions for effective clinical documentation. J. Am. Coll. Emerg. Phys. Open 6:100031. doi: 10.1016/j.acepjo.2024.100031
Gidwani, R., Nguyen, C., Kofoed, A., Carragee, C., Rydel, T., Nelligan, I., et al. (2017). Impact of scribes on physician satisfaction, patient satisfaction, and charting efficiency: a randomized controlled trial. Ann. Fam. Med. 15, 427–433. doi: 10.1370/afm.2122
James, L. R., Demaree, R. G., and Wolf, G. (1984). Estimating within-group interrater reliability with and without response bias. J. Appl. Psychol. 69, 85–98. doi: 10.1037/0021-9010.69.1.85
Leung, T. I., Coristine, A. J., and Benis, A. (2025). AI scribes in health care: balancing transformative potential with responsible integration. JMIR Med. Inform. 13:e80898. doi: 10.2196/80898
Lyons, P. G., Rojas, J. C., Bewley, A. F., Malone, S. M., and Santhosh, L. (2024). Validating the physician documentation quality instrument for intensive care unit-ward transfer notes. ATS Sch. 5, 274–285. doi: 10.34197/ats-scholar.2023-0094OC
Ma, S. P., Liang, A. S., Shah, S. J., Smith, M., Jeong, Y., Devon-Sand, A., et al. (2025). Ambient artificial intelligence scribes: utilization and impact on documentation time. J. Am. Med. Inform. Assoc. 32, 381–385. doi: 10.1093/jamia/ocae304
Shah, S. J., Crowell, T., Jeong, Y., Devon-Sand, A., Smith, M., Yang, B., et al. (2025a). Physician perspectives on ambient AI scribes. JAMA Netw. Open 8:e251904. doi: 10.1001/jamanetworkopen.2025.1904
Shah, S. J., Devon-Sand, A., Ma, S. P., Jeong, Y., Crowell, T., Smith, M., et al. (2025b). Ambient artificial intelligence scribes: physician burnout and perspectives on usability and documentation burden. J. Am. Med. Inform. Assoc. 32, 375–380. doi: 10.1093/jamia/ocae295
Shanafelt, T. D., Dyrbye, L. N., Sinsky, C., Hasan, O., Satele, D., Sloan, J., et al. (2016). Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin. Proc. 91, 836–848. doi: 10.1016/j.mayocp.2016.05.007
Shool, S., Adimi, S., Saboori Amleshi, R., Bitaraf, E., Golpira, R., and Tara, M. (2025). A systematic review of large language model (LLM) evaluations in clinical medicine. BMC Med. Inform. Decis. Mak. 25:117. doi: 10.1186/s12911-025-02954-4
Sinsky, C., Colligan, L., Li, L., Prgomet, M., Reynolds, S., Goeders, L., et al. (2016). Allocation of physician time in ambulatory practice: a time and motion study in 4 specialties. Ann. Intern. Med. 165, 753–760. doi: 10.7326/M16-0961
Stetson, P. D., Bakken, S., Wrenn, J. O., and Siegler, E. L. (2012). Assessing electronic note quality using the physician documentation quality instrument (PDQI-9). Appl. Clin. Inform. 3, 164–174. doi: 10.4338/aci-2011-11-ra-0070
Stetson, P. D., Morrison, F. P., Bakken, S., and Johnson, S. B.eNote Research Team (2008). Preliminary development of the physician documentation quality instrument. J. Am. Med. Inform. Assoc. 15, 534–541. doi: 10.1197/jamia.M2404
Stults, C. D., Deng, S., Martinez, M. C., Wilcox, J., Szwerinski, N., Chen, K. H., et al. (2025). Evaluation of an ambient artificial intelligence documentation platform for clinicians. JAMA Netw. Open 8:e258614. doi: 10.1001/jamanetworkopen.2025.8614
Tai-Seale, M., Olson, C. W., Li, J., Chan, A. S., Morikawa, C., Durbin, M., et al. (2017). Electronic health record logs indicate that physicians split time evenly between seeing patients and desktop medicine. Health Aff. (Millwood) 36, 655–662. doi: 10.1377/hlthaff.2016.0811
Tam, T. Y. C., Sivarajkumar, S., Kapoor, S., Stolyar, A. V., Polanska, K., McCarthy, K. R., et al. (2024). A framework for human evaluation of large language models in healthcare derived from literature review. NPJ Digit. Med. 7:258. doi: 10.1038/s41746-024-01258-7
Walker, K. J., Wang, A., Dunlop, W., Rodda, H., Ben-Meir, M., and Staples, M. (2017). The 9-item physician documentation quality instrument (PDQI-9) score is not useful in evaluating EMR (scribe) note quality in emergency medicine. Appl. Clin. Inform. 8, 981–993. doi: 10.4338/ACI2017050080
Keywords: large language models, artificial intelligence, medical scribe, clinical quality improvement, dictation accuracy
Citation: Palm E, Manikantan A, Mahal H, Belwadi SS and Pepin ME (2025) Assessing the quality of AI-generated clinical notes: validated evaluation of a large language model ambient scribe. Front. Artif. Intell. 8:1691499. doi: 10.3389/frai.2025.1691499
Edited by:
Shikha Kukreti, National Cheng Kung University, TaiwanReviewed by:
Emre Sefer, Özyeğin University, TürkiyeBirger Moell, KTH Royal Institute of Technology, Sweden
Copyright © 2025 Palm, Manikantan, Mahal, Belwadi and Pepin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mark E. Pepin, cGVwaW5tZUBnbWFpbC5jb20=
 Erin Palm1,2,3
Erin Palm1,2,3 Mark E. Pepin
Mark E. Pepin