- National Association of Insurance Commissioners, Kansas City, MO, United States
In the wake of the Affordable Care Act's coverage expansions and the COVID-19 pandemic's urgent demand for remote services, telehealth has become a critical gateway to healthcare for underserved and access-challenged populations across the United States. While telehealth offers the potential to reduce barriers related to distance, transportation, and provider shortages, persistent disparities in broadband access, digital literacy, and socioeconomic status continue to shape utilization patterns.
Method: Utilizing data from the 2024 Financial Inclusion Survey, this study applies a dual modeling strategy. Single-stage Probit, OLS, and Ologit models are used to analyze telehealth utilization and satisfaction. To address nonrandom selection into telehealth, a Heckman two-stage model–incorporating a cubic polynomial for perceived network adequacy and comprehensive controls including an urban/suburban geographic indicator–is implemented.
Results: Telehealth utilization in this nationally representative cross-sectional sample is unevenly distributed, with higher rates observed in urban and suburban communities. The analysis shows that perceived network adequacy has a nonlinear association with telehealth use: moderate adequacy increases utilization, while very high adequacy may reduce it. Administrative convenience and affordability are associated with higher satisfaction in single-stage models; however, these effects are attenuated after correcting for selection bias (Inverse Mills Ratio, β = −0.778, p < 0.05).
Discussion: Unobserved factors influencing telehealth adoption also bias satisfaction estimates, highlighting the necessity of correcting for selection effects. The cubic modeling approach effectively captures nonlinear associations between access and satisfaction.
Conclusion: Accurate assessment of telehealth's impact requires robust adjustment for selection bias. These findings have significant policy implications for improving network adequacy, digital access, and operational efficiency to ensure equitable telehealth adoption and satisfaction, particularly for underserved and non-urban communities.
1 Introduction
Telehealth usage in the United States has significantly increased over the past decade, becoming essential for providing healthcare services to various populations. This expansion has been driven by technical advancements and a rising need for accessible, affordable healthcare, particularly in underdeveloped regions (Hollander and Carr, 2020; Shigekawa et al., 2018). Furthermore, the COVID-19 pandemic accelerated a significant increase in telemedicine utilization, underscoring its capacity to alleviate interruptions in conventional healthcare provision and enhance patient outcomes (Contreras et al., 2020). Researchers have observed that telehealth improves patient happiness and engagement while offering the potential for diminishing systemic healthcare inequities (Kruse et al., 2017; Totten et al., 2016). Nonetheless, comprehending the diverse aspects that affect telehealth utilization and its assessment among users is a crucial domain of study since inequities in access and inconsistencies in service quality persist as issues (Uscher-Pines and Mehrotra, 2014). This evidence highlights the necessity of thoroughly investigating the factors influencing telehealth adoption to guide policies and practices that guarantee equitable and effective healthcare delivery.
Telehealth, characterized by using telecommunications and digital technology to provide healthcare services and information (Shigekawa et al., 2018), has become a fundamental element of contemporary healthcare. The Affordable Care Act (ACA) significantly advanced telehealth integration by prioritizing enhanced access, preventive care, and the mitigation of health inequities, hence creating a conducive atmosphere for innovative care delivery (Totten et al., 2016; Uscher-Pines and Mehrotra, 2014). Notwithstanding these policy attempts, certain issues persist in affecting telehealth utilization. Reimbursement issues, regulatory intricacies, technology constraints, and the ongoing digital divide continue to pose substantial obstacles for providers and patients (Kruse et al., 2017; Weinstein et al., 2014). The COVID-19 pandemic expedited the integration of telehealth, highlighting its essential function in ensuring continuity of care while mitigating exposure risks; nonetheless, this swift proliferation also revealed deficiencies in digital equity, provider preparedness, and long-term viability (Campion et al., 2016; Mann et al., 2020; Greenhalgh et al., 2020). Furthermore, recent studies reveal that patient demographics, socioeconomic status, and geographic disparities substantially influence participation in telehealth services (Bashshur et al., 2014; Bokolo, 2021; Koonin, 2020; Nouri et al., 2020). These findings highlight the necessity for thorough assessments and customized policy strategies to improve the efficacy, accessibility, and sustained influence of telehealth on patient outcomes within the changing healthcare environment.
This study analyzes the U.S. healthcare system in the post-ACA and post-COVID-19 era, focusing on the impact of perceived network adequacy on telehealth utilization and user satisfaction among insured patients. Perceived network adequacy denotes patients' evaluation of the sufficiency of their plan's in-network providers to fulfill their needs regarding availability, accessibility, and cultural responsiveness (Haeder and Xu, 2024). This contrasts with institutional definitions of network adequacy, established by regulators and insurers through quantitative criteria such as time-and-distance regulations, provider-to-enrollee ratios, or appointment wait times (202, 2023). Institutional adequacy relies on adherence to formal standards, whereas perceived adequacy reflects patients' experiential access in practice. This distinction is essential as patients may encounter obstacles despite the formal norms being technically satisfied, including issues with directory accuracy, transportation, or language services (Pollitz, 2022; Busch and Kyanko, 2021). Integrating perceived metrics into regulatory supervision can yield significant insights, assisting regulators in establishing benchmarks that more accurately reflect real-world access to care.
To assess these dynamics, the study applies a Heckman two-stage model, with a first-stage probit regression estimating the factors associated with telehealth adoption and a second-stage outcome equation analyzing satisfaction conditional on adoption. The analysis accounts for other attitudinal elements, including the ease of claim filing, views of psychological pricing (premium affordability), and the incidence of unexpected health-related bills in the past year, alongside the presence of a primary care physician and different demographic attributes. The data are sourced from the 2024 Financial Inclusion Survey conducted by the National Association of Insurance Commissioners (NAIC), guaranteeing a comprehensive and nationally representative sample. This study concentrates exclusively on insured populations, omitting clinical outcomes and cost-effectiveness metrics, to examine how views on network adequacy and these supplementary criteria influence telehealth engagement and assessment in the changing U.S. healthcare environment.
The main focus of the investigation is whether perceived network adequacy—characterized by the simplicity of appointment scheduling, accessible transportation, and the presence of clinicians attuned to patients' needs—affects both the utilization of telehealth services and their satisfaction. This study aims to isolate the impact of network adequacy from other attitudinal factors, including the ease of claim submission, perceptions of premium affordability (psychological pricing), unexpected billing experiences, and demographic variables. A Heckman two-stage model is employed because satisfaction data are only available for telehealth users; a standard one-stage approach would likely suffer from sample selection bias. Exclusion criteria are used to identify the model, particularly factors such as health plan type (i.e., HMO enrollment), utilization of free preventive health services under the ACA, and urban/suburban residency. Research suggests that the identified exclusion variables–specifically, health plan type (i.e., HMO enrollment), utilization of complimentary preventive services under the ACA, and urban/suburban residency—are strong predictors of structural access and the initial decision to utilize telehealth. These factors encompass systemic and environmental characteristics that impact an individual's utilization of telehealth services (Koh and Sebelius, 2010; Douthit et al., 2015); however, they are less likely to influence patient satisfaction post-adoption of telehealth (Mehrotra et al., 2021; Bashshur et al., 2014; Gajarawala and Pelkowski, 2021). This methodological selection provides a robust framework for isolating the influence of perceived network adequacy on telehealth utilization and satisfaction, ensuring that satisfaction estimates remain unbiased by factors that predominantly influence the likelihood of initial telehealth adoption (Heckman, 1979; Vella, 1998; Wooldridge, 2010; Cameron, 2005).
The study proposes three major hypotheses on the expected non-linear and multi-dimensional impacts of perceived network adequacy on telehealth behavior. The connection between perceived network adequacy and both telehealth utilization and satisfaction is anticipated to exhibit a cubic pattern. The negative coefficient of the cubic term in telehealth utilization indicates that while initial enhancements in network adequacy boost usage, subsequent improvements may result in diminishing or even negative marginal impacts, either due to market saturation or excessive complexity in networks. Conversely, regarding telehealth satisfaction, both the linear and cubic elements are anticipated to be positive, indicating that as network adequacy advances, satisfaction rises in a non-linear manner, especially at elevated levels where the advantages may accumulate. Furthermore, it is posited that the simplicity of claim submission correlates favorably with satisfaction, as efficient administrative procedures are expected to improve user experience. Psychological pricing, which aligns with beliefs of premium cost, is anticipated to enhance telehealth utilization by reducing adoption hurdles. Moreover, whereas unexpected bills in the last year are projected to increase telehealth utilization as patients pursue alternatives to conventional care to evade additional financial shocks, they are also forecast to diminish overall satisfaction. These hypotheses together seek to elucidate how perceived network adequacy and various attitudinal aspects influence the uptake and satisfaction with telehealth services.
2 Methodology
2.1 Data source and sample design
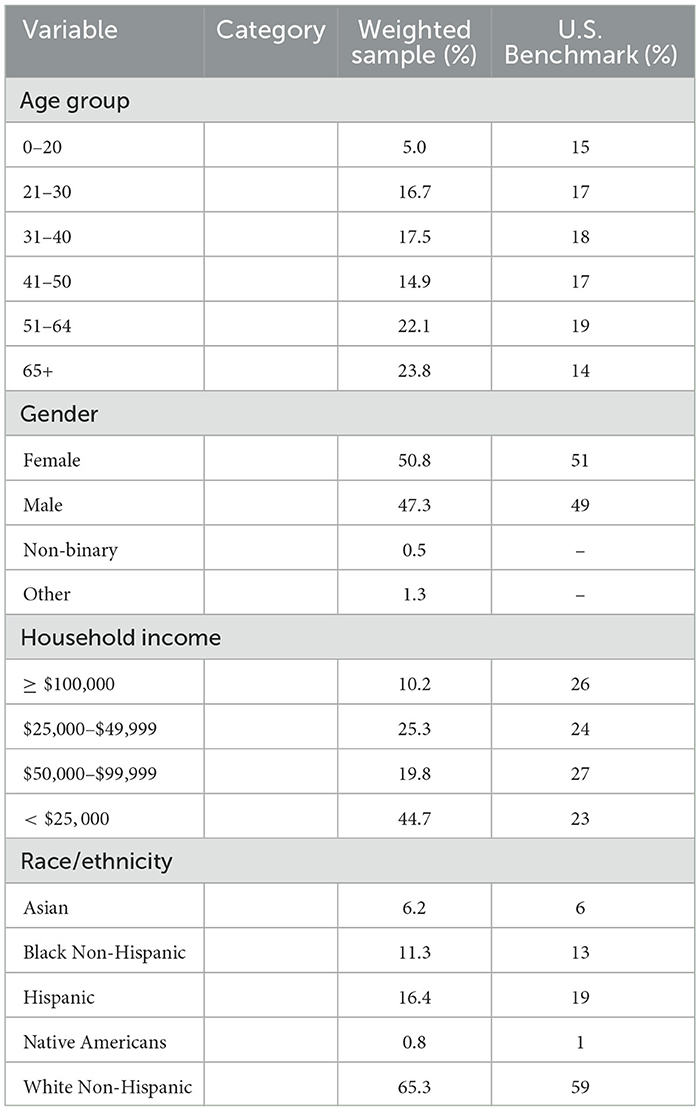
The data for this study derive from the 2024 Financial Inclusion Survey executed by the Center of Insurance Policy and Research (CIPR) at the National Association of Insurance Commissioners (NAIC) during February and March 2024. The poll, conducted online through Qualtrics, gathered responses from 3,611 participants throughout the United States. To guarantee strong representation of minority groups, prestratification weights were utilized, leading to the oversampling of these populations (Groves and Couper, 2012; Kalton, 2009; Lumley, 2011). Furthermore, post-stratification weights were calibrated utilizing the ANESRAKE method to align the sample with the revised 2024 U.S. Census Bureau data concerning factors such as region, age, education, race, income, and gender (Pasek and Pasek, 2018; DeBell and Krosnick, 2009; Battaglia et al., 2009; Kolenikov, 2014; Ansolabehere and Rivers, 2013). The poll covered many issues such as health insurance, life insurance, retirement planning, financial literacy, and risk perception, while gathering extensive demographic data to enable a thorough examination of financial behaviors and attitudes. As shown in Table 1, the weighted sample closely resembles the U.S. population on key characteristics. The lower percentage of respondents in the 0-20 age group is attributable to the survey's eligibility criteria, which, for legal and ethical reasons, restricted participation to adults aged 18 and over. This limitation is common in survey research to comply with regulations regarding minors participation. Additionally, the sample slightly over-represents individuals aged 65 and older. While this may affect the generalizability of findings to younger populations, it is important to note that adults aged 65 and above are the most highly insured age group in the United States, largely due to near-universal coverage through Medicare and related programs (Keisler-Starkey et al., 2023). This demographic characteristic should be considered when interpreting the study's results in the context of the broader U.S. insured population.
2.2 Main variables
2.2.1 Dependent variables
The study's dependent variables are telehealth usage and telehealth satisfaction. Telehealth utilization is a binary variable (yes/no), signifying whether respondents accessed telehealth services in the preceding 12 months. Telehealth satisfaction is assessed using a 1-to-5 Likert scale (Very Unsatisfied to Very Satisfied), indicating satisfaction with telehealth coverage provided by health insurance plans.
All individuals who reported using telehealth services (N = 1,116) provided a valid response to the telehealth satisfaction question, so there is no item nonresponse for this outcome among users. However, the group observed for telehealth satisfaction–those who utilized telehealth services–may differ systematically from those who did not, raising the possibility of selection bias. In this context, individuals who chose to use telehealth may have distinct characteristics or attitudes compared to non-users, potentially influencing satisfaction levels. To address this, the analysis employs a Heckman selection model, which accounts for non-random selection into telehealth usage and provides less biased estimates of the determinants of telehealth satisfaction.
Figure 1 provides insights into the two dependent variables of the study: telehealth utilization and telehealth satisfaction. The graphic depicts telehealth usage, showcasing the weighted percentage of telehealth utilization across different community types. Urban and suburban areas exhibit the highest telehealth utilization at 36.1%, followed by small cities and towns at 28.8%, and rural areas at 27.8%. This increase may signify enhanced digital infrastructure and more access to telehealth services in urban regions. The second data regarding telehealth satisfaction indicates high levels of contentment, with 54.1% of respondents selecting the highest satisfaction rating (5) and 30% opting for a rating of 4. In aggregate, lower satisfaction ratings (1, 2, and 3) account for less than 16%. The findings highlight the increased acceptability of telehealth in urban and suburban areas, along with the largely positive satisfaction ratings among users, demonstrating telehealth's effectiveness in meeting patient needs across various demographics.
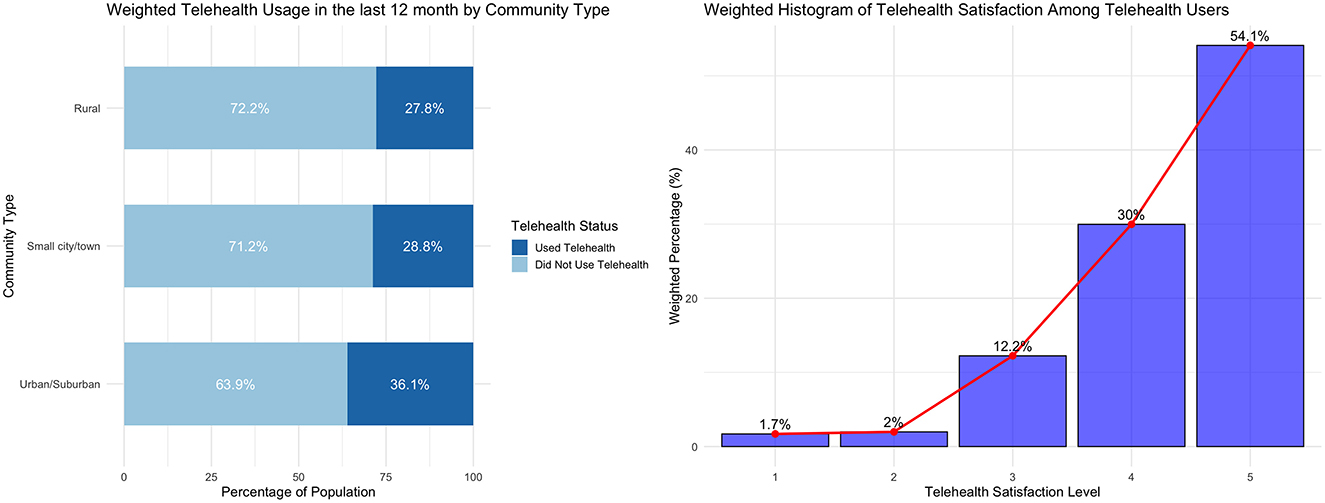
Figure 1. Weighted distribution of telehealth usage and satisfaction by community type as of July 2023. The figure is descriptive only, based on survey weights calibrated to July 2023 U.S. Census benchmarks. It illustrates how reported utilization and satisfaction differ across urban, suburban, and rural communities.
2.2.2 Key independent variables
This analysis encompasses distinctly articulated major independent variables that encapsulate multiple dimensions of consumer experience with telehealth usage. Perceived network adequacy is a composite construct that assesses consumers evaluations of the accessibility and effectiveness of their provider network (Haeder and Xu, 2024; Zhu et al., 2022, 2025). The composite index is calculated by summing three survey items: (1) ease of making an appointment with a preferred provider, (2) ease of traveling to a provider in the network, and (3) ability to find a provider with whom the respondent is comfortable. The first two items are measured on a five-point Likert scale, ranging from 1 (“Very difficult”) to 5 (“Very easy”), while the third is coded as a binary variable (0 = “No,” 1 = “Yes”). Each item is converted to a numeric value and the composite score is computed as their sum, with higher scores reflecting greater perceived network adequacy. This approach aligns with standard practices for creating summative indices from Likert-type and binary items (Zhu et al., 2023, 2017; Shortell and Kaluzny, 1994; Corlette et al., 2014; Zhu et al., 2021). The resulting index demonstrated acceptable internal consistency (Cronbach's alpha = 0.64), consistent with established thresholds for multi-dimensional constructs in health services research (Hoseini-Esfidarjani et al., 2021).
Psychological pricing refers to the strategic setting of prices based on psychological effects and consumer perceptions rather than on objective costs or market logic. This approach leverages cognitive biases—such as left-digit bias in charm pricing (e.g., 9.99vs.10.00), price anchoring, and the perception of urgency or exclusivity—to influence consumer behavior and enhance the perceived value or affordability of a product or service (Qadri and Sodhi, 2025; Kumar and Pandey, 2017). In the context of health insurance and telehealth, psychological pricing can be operationalized as consumers subjective assessment of premium affordability, rather than the actual dollar amount. In this study, affordability was measured by the survey item: “How affordable is your overall health insurance monthly premium?” Responses were recorded on a five-point Likert scale ranging from “Very unaffordable” to “Very affordable.” This subjective perception is shaped by how premiums are presented (e.g., as a monthly “charm” price, or with comparative discounts) and by consumers prior experiences and expectations (Kumar and Pandey, 2017; Stapel, 1972; Wedel and Leeflang, 1998). The variable thus captures the emotional and psychological impact of pricing strategies on consumer decision-making and satisfaction, which is critical for understanding uptake and retention in telehealth services. Finally, unexpected bills is a binary variable that denotes whether respondents or their households have faced charges that surpass their expectations, thereby functioning as a measure of financial unpredictability in healthcare costs (Hoadley and Lucia, 2022; Steinbrook, 2019).
2.2.3 Control variables
Control variables are included to address individual differences that may obscure the links between telehealth usage experiences and outcomes. Objective financial knowledge is quantified as an index based on respondents' accurate responses to financial literacy questions, thereby measuring their actual financial competence. Conversely, subjective financial knowledge is gauged by self-evaluation, indicating individuals' perceived understanding of personal finance. This distinction is essential since previous studies suggest that actual and perceived financial knowledge may differ, thereby affecting financial decisions and behaviors in unique manners (Lusardi and Mitchell, 2014; Fernandes et al., 2014; Nkouaga, 2024a,b). Furthermore, the presence of a primary care physician is accounted for, as consistent interaction with a primary care provider correlates with enhanced health outcomes and influences perceptions of healthcare accessibility (Starfield, 1998). Self-assessed mental health is incorporated to account for total well-being, which may affect both financial decision-making and healthcare utilization (Cutler and Lleras-Muney, 2010). Demographic factors, including race, gender, education, and income, are controlled due to their consistent association with disparities in health care access and financial literacy, thereby aiding in the isolation of the effects of the primary independent variables (Lusardi and Mitchell, 2014; Agarwal et al., 2007). These control variables collectively strengthen the study by addressing individual differences that could otherwise distort the observed connections among financial knowledge, health care experiences, and outcomes.
2.2.4 Exclusion restriction
Exclusion restrictions are a foundational component in the initial stage of the Heckman selection model, serving as variables that influence the probability of selection into the observed sample–in this case, the adoption of telehealth services–without directly affecting the outcome of interest, such as post-utilization satisfaction with telehealth. The validity of the Heckman correction hinges on the careful identification and justification of such variables, as they enable the model to adjust for sample selection bias and yield unbiased estimates of the outcome equation (Wolfolds and Siegel, 2019; Bushway et al., 2007). Plan type, specifically the distinction between Health Maintenance Organization (HMO) and non-HMO plans, is often employed as an exclusion restriction because HMOs are structured to facilitate access to services like telehealth through features such as coordinated care, defined provider networks, and lower out-of-pocket costs, which can increase the likelihood of telehealth uptake (National Committee for Quality Assurance (NCQA), 2020; McDonald et al., 2007). However, the organizational characteristics of a health plan, while influential in the decision to utilize telehealth, are theoretically and empirically unlikely to directly impact users satisfaction with their telehealth experience, which is more commonly determined by service quality, provider interaction, and care outcomes. Thus, the use of plan type as an exclusion restriction is supported by both methodological guidance and the logic that it affects selection into telehealth use but not the satisfaction derived from that use, thereby satisfying the requirements for model identification and credible inference in the Heckman framework.
The utilization of preventive health services under the ACA signifies an individual's proactive involvement in health management, potentially facilitating the adoption of telehealth services; however, subsequent satisfaction with telehealth is more contingent upon the quality of care received than on previous use of preventive services.
Urban and suburban residency are acknowledged as significant geographical factors in econometric models of telehealth adoption, as they correlate with the probability of telehealth usage but do not directly influence outcomes like satisfaction following telehealth engagement. Urban and suburban areas tend to have greater healthcare access, higher broadband availability, and more healthcare providers compared to rural areas, which facilitates telehealth adoption (National Rural Health Association, 2025; Zachrison et al., 2021; Chen et al., 2021; Whitacre, 2011; Harkey et al., 2020). These structural factors make urban/suburban residency a strong predictor of telehealth uptake, as documented in multiple studies employing geographic location as an instrumental variable or exclusion restriction in health services research (Whitacre, 2011; Harkey et al., 2020). Importantly, although urban and suburban residents generally have higher telehealth utilization rates, satisfaction levels among telehealth users in these areas remain comparable to those in rural regions, provided that technology and provider communication are effective (Smith et al., 2020; Whitacre, 2011; Schadelbauer, 2017; Totten et al., 2023). This distinction supports the validity of urban/suburban residency as an exclusion restriction: it affects the probability of telehealth uptake (the selection process), but not satisfaction conditional on use, which is more strongly influenced by the quality of the telehealth encounter itself.
Furthermore, being employed can serve as a valid exclusion restriction in models of telehealth utilization, as employment status is closely associated with both the decision to use telehealth and the broader context of healthcare access. Specifically, job status may influence telehealth uptake through several mechanisms: employed individuals are more likely to have employer-sponsored health insurance, which typically provides better access to telehealth services; they may also experience greater time constraints that make the convenience and flexibility of telehealth particularly appealing; and, in some cases, employers may directly promote or incentivize telehealth use as part of workplace wellness initiatives (Williams and Shang, 2023; Mittone et al., 2022; Hendy et al., 2025). Despite these factors, employment status itself does not directly determine satisfaction with the telehealth experience. Rather, satisfaction is more strongly shaped by the quality of provider interaction, the reliability of the telehealth platform, and the overall ease of use–factors that are largely independent of job status.
Empirical studies consistently find that while employed individuals are more likely to use telehealth and may report higher satisfaction, this association is largely explained by access to resources (such as technology and insurance), digital literacy, and the ability to integrate telehealth into a busy schedule, rather than by employment status per se (Williams and Shang, 2023; Mittone et al., 2022; Hendy et al., 2025). For example, research on telehealth satisfaction among patients with chronic diseases found that employment status was positively correlated with satisfaction, but this effect was likely mediated by factors such as convenience and the ability to manage healthcare alongside work and family responsibilities (Hendy et al., 2025). Similarly, studies examining the broader determinants of telehealth satisfaction have identified provider performance, system reliability, and ease of use as the most significant predictors, with employment status playing a secondary or indirect role (Mittone et al., 2022; Hendy et al., 2025). Therefore, when employment is used as an exclusion restriction, it is important to clarify that its primary effect is on the likelihood of telehealth use (through access and convenience), while its influence on satisfaction is mediated by other variables already accounted for in the model.
These exclusion restriction variables collectively influence telehealth usage decisions in the initial stage of the model without directly impacting the satisfaction equation in the subsequent stage, thereby satisfying the exclusion restriction necessary for consistent estimation in the two-stage Heckman method (Puhani, 2000; Certo et al., 2016). A comprehensive table of descriptive statistics for all variables included in the model is provided (Table 2), offering transparency regarding their distributions and aiding interpretation of the selection and outcome equations.
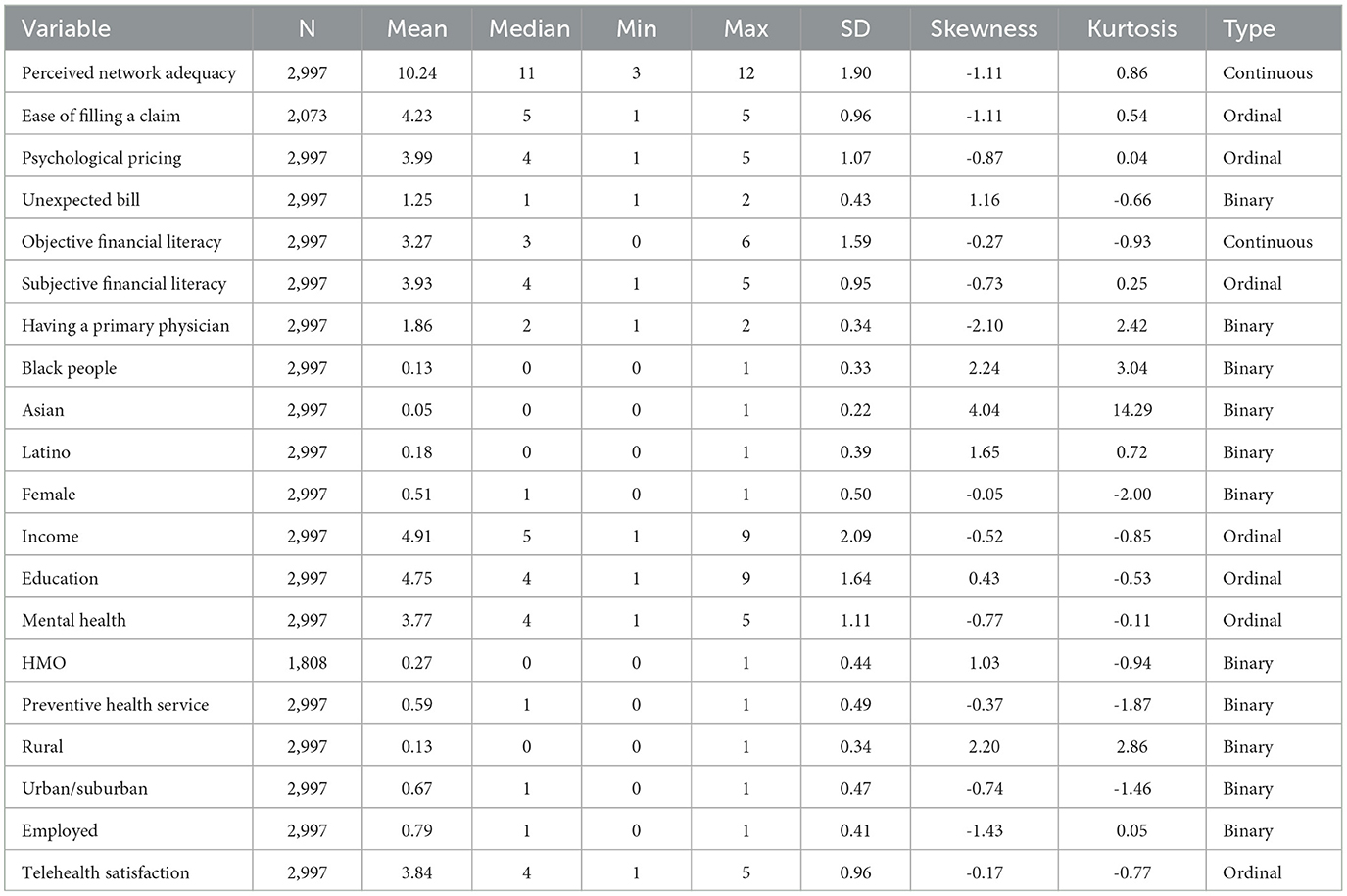
Table 2. Descriptive statistics for all variables used in the Heckman selection model, including variable types.
2.3 Model
2.3.1 Heckman two-stage sample selection
The observed outcome Yi is available only when a latent selection indicator . The model is specified by
where
denotes the Inverse Mills Ratio (IMR). Inclusion of λi in the second stage corrects for non-random selection (Heckman, 1979; Wooldridge, 2010).
Estimation procedure:
1. The selection equation parameters γ are estimated by a weighted probit on the full sample.
2. The estimated IMR, , is calculated from the fitted probit.
3. The outcome equation parameters β are estimated by weighted OLS on the selected subsample {i:Si = 1}, including as an additional regressor.
Interpretation: The IMR captures the expected value of unobserved factors driving both participation and the outcome, thereby purging the outcome equation of selection bias.
3 Results
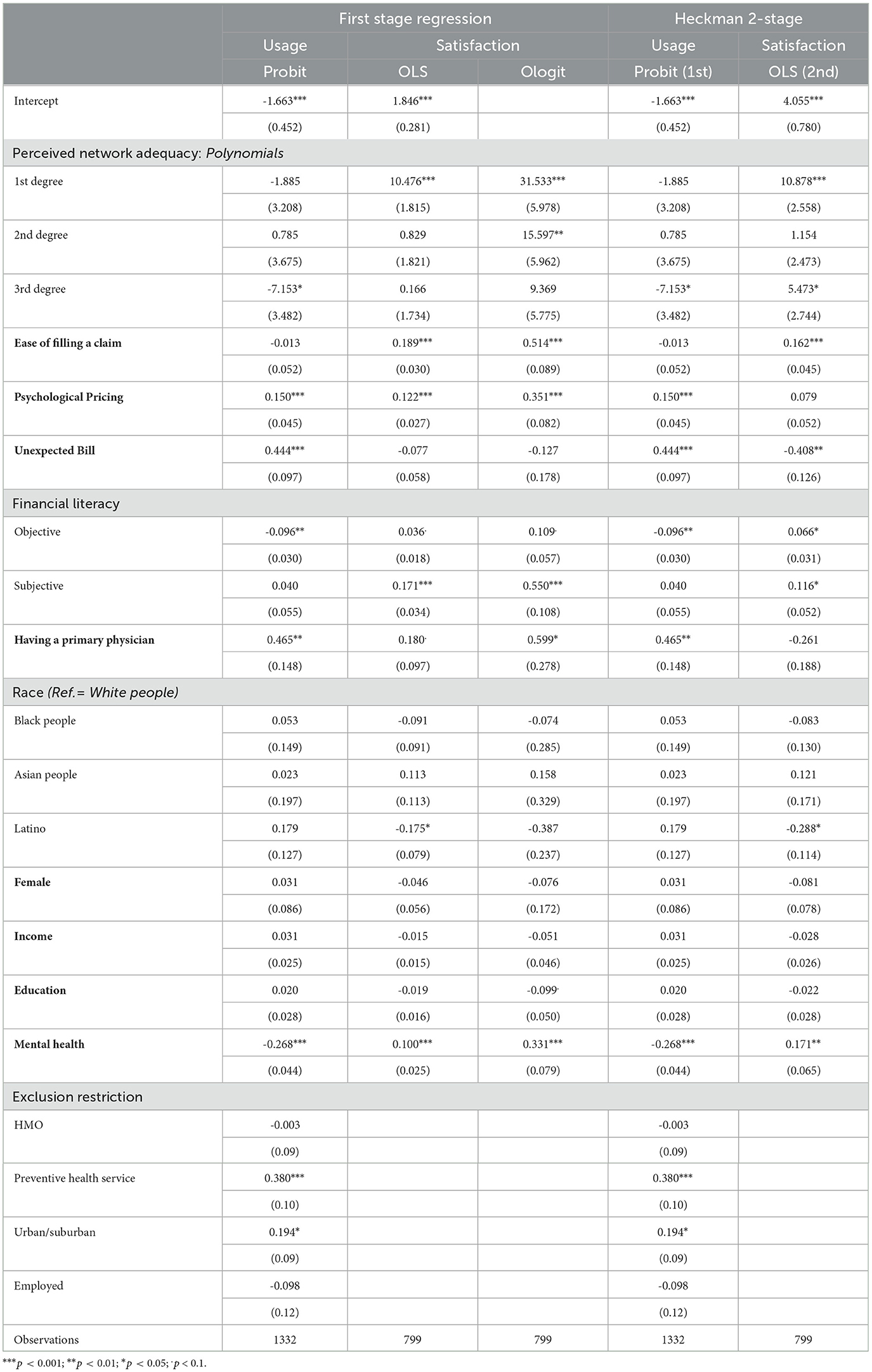
This investigation utilizes a dual modeling approach. Initially, it analyzes telehealth utilization with a single-stage weighted Probit model, then evaluates user satisfaction with telehealth using weighted Ordinary Least Square (OLS) and Ordered Logistic Regression (Ologit) models. The study employs a weighted Heckman two-stage technique to rectify potential selection bias in modeling satisfaction solely among individuals who opt for telemedicine. The Probit model for telehealth utilization reveals a significantly negative intercept (β = −1.534, p < 0.001), indicating that the typical baseline inclination to utilize telemedicine is little, as shown in Figure 1. The primary independent variable—perceived network adequacy—is incorporated as a cubic polynomial. The usage equation's third-degree term (β = −7.020, p < 0.05) indicates a nonlinear effect; users with very high perceived adequacy are less inclined to embrace telehealth than those with moderate perceptions.
The single-stage models (Table 3) for telehealth satisfaction are calculated exclusively for telehealth users. The OLS model yields a positive and significant intercept (β = 1.846, p < 0.001), whereas the Ologit model underscores the significance of perceived network adequacy, evidenced by very significant coefficients for the first-degree term (β = 31.533, p < 0.001) and the second-degree term (β = 15.597, p < 0.01). In addition to network adequacy, other critical independent variables substantially forecast satisfaction. The ease of filing a claim is significantly favorable (OLS: β = 0.189, p < 0.001; Ologit: β = 0.514, p < 0.001), indicating that efficient administrative procedures improve the user experience. The occurrence of unforeseen expenses (unexpected bills) exhibits contradictory effects: it positively influences the utilization model (β = 0.428, p < 0.001) yet negatively impacts satisfaction in the Heckman second-stage model (β = −0.430, p < 0.05), suggesting that unexpected bills may hinder ongoing participation.
Psychological pricing serves as a significant catalyst. It markedly enhances the probability of telehealth utilization (β = 0.152, p < 0.001) and elevates satisfaction in the single-stage models (OLS: β = 0.122, p < 0.001; Ologit: β = 0.351, p < 0.001), yet its effect diminishes and becomes statistically insignificant in the Heckman satisfaction equation (β = 0.075). Financial literacy demonstrates a complex relationship: objective financial literacy marginally decreases usage (β = −0.100, p < 0.001) but correlates with increased user satisfaction (OLS: β = 0.036 at marginal significance, and Heckman: β = 0.071, p < 0.05), whereas subjective financial literacy consistently enhances satisfaction (OLS: β = 0.171, p < 0.001; Ologit: β = 0.550, p < 0.001). The presence of a primary care physician is a substantial positive predictor of utilization (β = 0.494, p < 0.01) and is modestly associated with satisfaction in the single-stage models; however, its impact turns negative (though small) in the second stage of the Heckman model.
The demographic controls—race, gender, income, education, and self-assessed mental health—also play a significant role. Mental health exhibits a negative correlation with telehealth utilization (β = −0.268, p < 0.001) and a positive correlation with satisfaction (OLS: β = 0.100, p < 0.001; Ologit: β = 0.331, p < 0.001), indicating that individuals with poorer mental health are less inclined to engage with telehealth, yet those who do may perceive the service as especially advantageous. Latino respondents demonstrate reduced satisfaction levels in single-stage and Heckman models among racial categories. Gender, income, and education, although being adjusted for, exhibit relatively minor and frequently statistically negligible impacts.
The urban/suburban indicator was included as an exclusion restriction in the selection equation to capture geographic variation influencing telehealth uptake without directly affecting satisfaction conditional on use. As shown in Table 3, urban/suburban residency is a statistically significant positive predictor of telehealth utilization in both the first-stage Probit and the Heckman two-stage models (β = 0.194, p < 0.05). This finding supports its validity as an instrument affecting the likelihood of telehealth use. Preventive health service utilization also significantly predicts telehealth uptake, whereas plan type (HMO) and employment status were not statistically significant predictors in the selection equation. The stability of these exclusion restrictions and their alignment with theoretical expectations strengthen the robustness of the Heckman model correction for sample selection bias.
Figure 2 depicts the anticipated correlations between perceived network adequacy and the dependent variables, telehealth satisfaction, and telehealth usage, across two divergent situations. The upper plots depict individuals without unexpected bills, lacking a primary care physician, not enrolled in an HMO, not utilizing preventive health services, and living in non-urban/suburban regions. In contrast, the lower plots illustrate individuals exhibiting similar traits. In the optimal scenario, telehealth satisfaction progressively increases with perceived network adequacy, exhibiting a slight plateau at mid-levels before a pronounced rise at higher levels, suggesting that satisfaction is moderately sensitive to adequacy but escalates significantly as adequacy reaches its peak. Telehealth utilization exhibits a significant decrease as adequacy increases, beginning at elevated levels with poor adequacy and diminishing to minimal levels, indicating that telehealth is predominantly employed in situations with insufficient networks as a compensating strategy. Conversely, the lower scenario, depicting persons with elevated healthcare participation (unexpected expenses, a primary care physician, HMO coverage, utilization of preventive health services, and urban/suburban residency), demonstrates a more intricate pattern. Satisfaction begins at an elevated baseline and increases more significantly at high adequacy levels, indicating improved integration and alignment of telehealth services with patient requirements. In this scenario, telehealth utilization decreases significantly with rising adequacy, followed by a minor increase at intermediate adequacy levels before leveling, indicating a complex interaction between telehealth and conventional care alternatives among actively engaged healthcare populations.
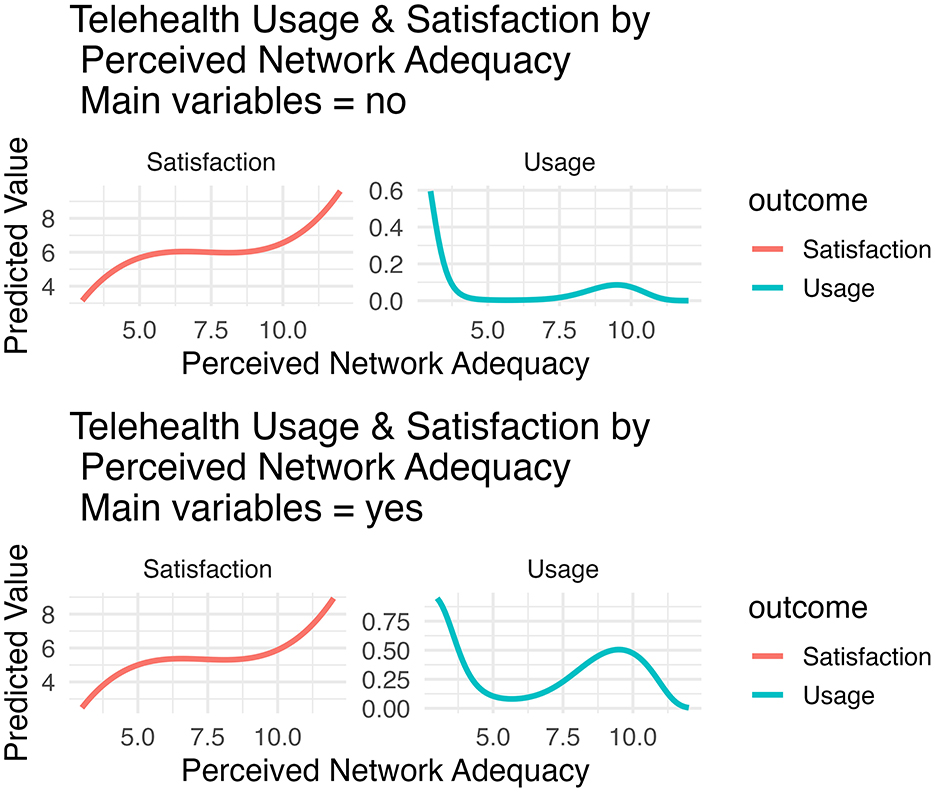
Figure 2. Predicted relationships between perceived network adequacy and both telehealth usage and satisfaction, estimated using 3rd degree orthogonal polynomials in the Heckman selection model. Model-derived predictions are shown for two hypothetical subgroups: (top panels) all key binary covariates (unexpected medical bill, primary care physician, HMO enrollment, preventive health use, urban/suburban residence, and employment) set to
Crucially, the Inverse Mills Ratio (IMR) correction term is both negative and statistically significant (β = −0.78, p = 0.019 see Table 4), with further analysis (Figure 3) demonstrating that IMR values become less negative as network adequacy increases. This pattern indicates that as network adequacy rises, the potential for unobserved selection bias diminishes–individuals with high adequacy are less likely to differ systematically from the wider insured population in unmeasured ways. These findings together demonstrate that improvements in satisfaction and reductions in telehealth usage with greater network adequacy are not artifacts of non-random selection. Instead, the model confirms that network adequacy exerts both a direct, robust influence on outcomes and an indirect benefit by reducing selection bias, reinforcing the substantive validity of the results illustrated in Figure 2.
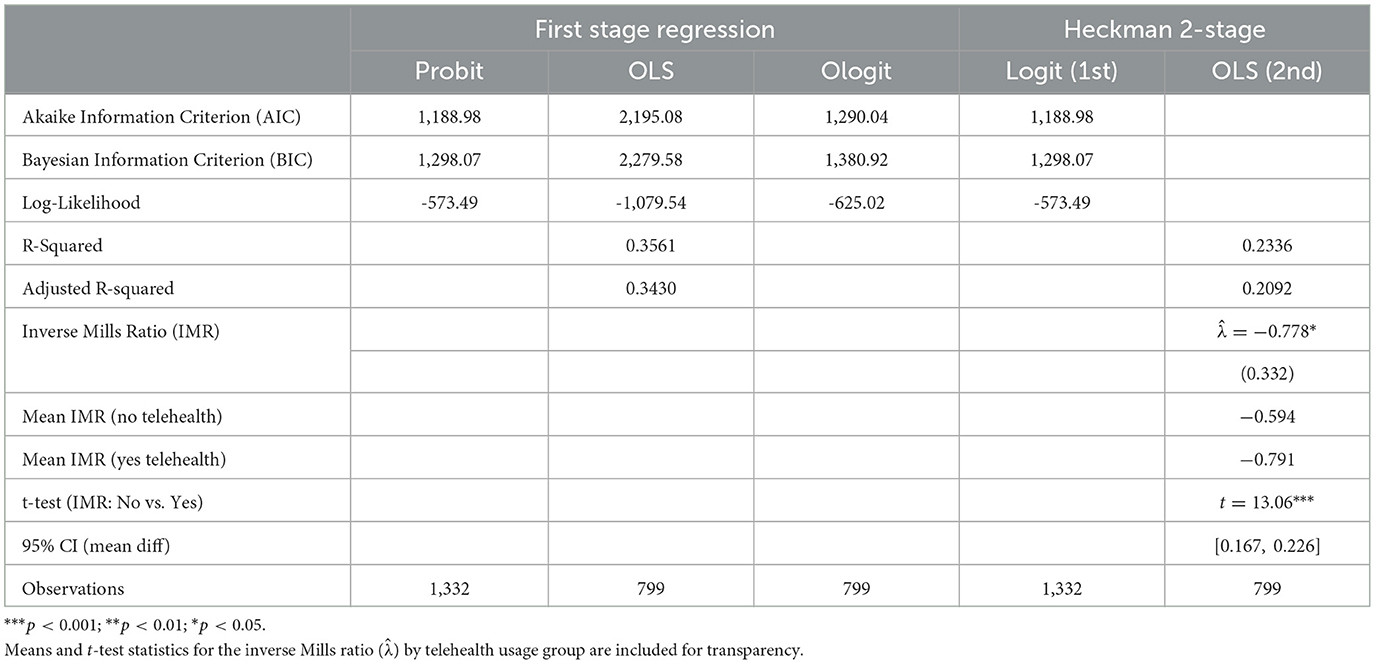
Table 4. Model comparison: AIC, BIC, log-likelihood, R-squared, adjusted R-squared, and Inverse Mills Ratio (IMR, ) with group means and t-test.
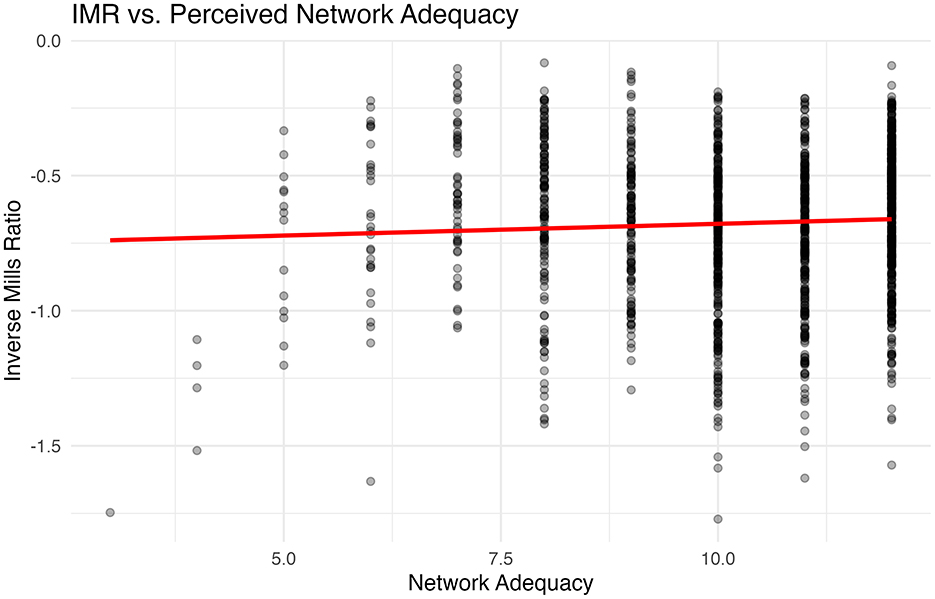
Figure 3. Scatterplot of the Inverse Mills Ratio (IMR) against perceived network adequacy. The IMR, derived from the Heckman selection model, quantifies the degree of selection bias for each observation. A fitted regression line illustrates a modest positive association, suggesting that higher perceived network adequacy is linked to slightly lower selection bias in telehealth satisfaction and usage outcomes.
Following this, Figure 3 presents the relationship between perceived network adequacy and the Inverse Mills Ratio (IMR), the key selection correction term from the Heckman model. The scatterplot and fitted line indicate a weak but discernible positive association: as perceived network adequacy increases, the IMR becomes slightly less negative. This suggests that higher network adequacy is associated with a modest reduction in selection bias–individuals perceiving greater adequacy are less likely to systematically differ from the general sample in unmeasured ways. In other words, the observed improvements in satisfaction and the decreasing reliance on telehealth with greater network adequacy are not simply artifacts of nonrandom participation; rather, the Heckman model's selection correction confirms these patterns are robust. This analysis highlights how network adequacy not only directly influences telehealth experiences but also helps to mitigate selection bias, reinforcing the validity of the observed associations in the main outcome models.
An essential element of the modeling approach is the integration of exclusion restrictions into the selection equation. The first-stage model incorporates variables such as plan type (HMO versus non-HMO), utilization of preventive health services under the ACA, and urban/suburban residency as instruments that influence telehealth uptake while being excluded from the satisfaction equation. This identification strategy is fundamental to the Heckman two-stage methodology, ensuring consistent estimation of the effects of interest.
The model comparison statistics are presented in Table 4, including AIC, BIC, Log-Likelihood, and R2. The Heckman model achieves an adjusted R2 of 0.2336 for satisfaction, compared to an R2 of 0.3561 in the single-stage OLS model. The AIC and BIC values are similar between the initial Probit and Heckman models, indicating comparable overall fit. However, the Heckman model's adjustment for selection bias is crucial, as evidenced by the statistically significant Inverse Mills Ratio (β = −0.778, p < 0.05).
To further illustrate the importance of correcting for selection bias, Figure 4 displays the distribution of the estimated Inverse Mills Ratio () by telehealth usage status. The mean IMR for non-users is −0.60, while the mean for users is −0.79. The difference is highly significant (Welch t-test: t = 13.01, p < 0.001, 95% CI [0.165, 0.224]), confirming substantial non-random selection into telehealth usage. This visual and statistical evidence underscores that single-stage models may exaggerate or distort the effects of primary predictors, and justifies the use of the Heckman correction for robust estimation.
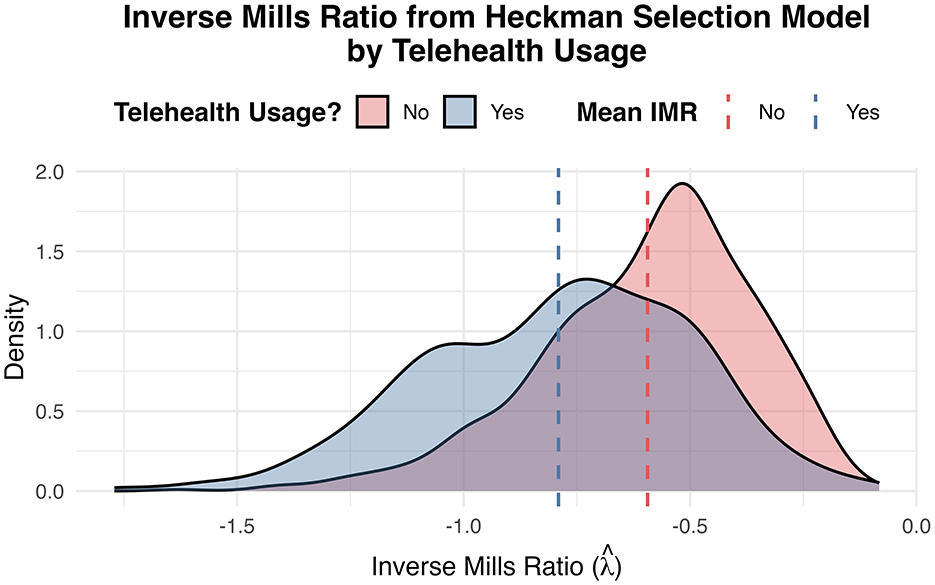
Figure 4. Density plot of the inverse Mills ratio () from the Heckman selection model, stratified by telehealth usage status. The plot demonstrates a clear and statistically significant difference in IMR distributions between telehealth users and non-users (p < 2 × 10−16), reflecting non-random selection into telehealth use. Overlap between groups indicates that unobserved factors associated with the likelihood of using telehealth also correlate with satisfaction outcomes, thereby supporting the use of the Heckman selection model to address selection bias.
4 Discussion
This research demonstrates that while single-stage models—Probit for telehealth utilization and OLS/Ologit for user satisfaction—provide useful initial insights, they can yield biased estimates by failing to account for the nonrandom selection into telehealth. The Heckman two-stage approach addresses this limitation by explicitly modeling the selection process. The significant Inverse Mills Ratio (β = −0.778, p < 0.05) in the model confirms that unobserved factors influencing telehealth uptake also affect satisfaction, underscoring the presence of selection bias. By incorporating the IMR, the analysis validates that the associations observed between key predictors and satisfaction are robust and not simply artifacts of unmeasured confounding. Furthermore, the added IMR-network adequacy analysis (see Figure 3) reveals that higher perceived network adequacy is associated with a modest reduction in selection bias, further reinforcing the credibility of the main findings.
The results from the cubic polynomial specification further clarify the intricate, nonlinear relationship between perceived network adequacy, telehealth adoption, and satisfaction. Single-stage models tend to overstate the impact of network adequacy—particularly at extreme values—due to unaddressed selection effects. However, after adjustment in the Heckman model, the effect sizes and statistical significance are moderated, revealing that individuals with particularly strong perceptions of network adequacy (either very high or very low) are overrepresented among telehealth users. This pattern is confirmed in the Figure 3 and the IMR analysis, demonstrating that improvements in network adequacy simultaneously elevate satisfaction and reduce the need for compensatory telehealth use, while also mitigating the risk of selection-driven bias in the outcome estimates. Together, these findings highlight the importance of adjusting for selection in evaluating telehealth experiences and provide new insight into the mechanisms linking network adequacy, user satisfaction, and service utilization. The use of a cubic polynomial to model the association between network adequacy and satisfaction is theoretically grounded in the literature on health service utilization, which recognizes that the effects of access-related variables on satisfaction are often nonlinear and may exhibit diminishing returns or inflection points (Royston and Sauerbrei, 2007; Austin et al., 2022). Prior research in health economics and patient experience has demonstrated that higher-order polynomials, including cubic terms, can flexibly capture complex relationships between perceived access and health outcomes, particularly when threshold or saturation effects are present (Royston and Sauerbrei, 2007). Flexible polynomial regression models, including cubic and higher-order terms, can be used to capture complex, nonlinear relationships between clinical predictors and outcomes, especially where threshold or saturation effects are present. For example, Filipow et al. (2023), demonstrated that flexible polynomial regression (up to the cubic and quartic level) provided accurate modeling of clinical outcome trajectories in electronic health record data, allowing for nuanced estimation of nonlinear effects in patient monitoring and health outcomes.
Figure 2 indicates a complex link between perceived network adequacy and telehealth outcomes, influenced by individual and contextual factors. Telehealth satisfaction typically rises with network adequacy, although the rate of increase is more pronounced for persons with greater healthcare engagement (e.g., those with a primary care physician, HMO coverage, utilization of preventive health services, and urban/suburban residence). This indicates that satisfaction is influenced by network adequacy and the extent to which telehealth integrates into a patient's healthcare experience. Telehealth utilization declines significantly with increased network adequacy in communities with little healthcare participation, suggesting that telehealth serves as a compensatory mechanism when network adequacy is insufficient. In populations with greater healthcare engagement, usage has a more intricate pattern, characterized by an early fall, a subsequent little increase at intermediate sufficiency levels, and then a tapering down. This signifies that telehealth enhances rather than replaces traditional care in well-integrated healthcare systems. The findings underscore the need to address systemic factors (e.g., network adequacy) and individual-level determinants (e.g., primary care access) to enhance telehealth uptake and satisfaction, especially in underserved or non-urban/suburban regions. This underscores the necessity for specific legislative measures to address deficiencies in network adequacy while maintaining telehealth as a successful and supplementary aspect of care delivery.
A key contribution of this study is the dual role of claim filing as both an indicator of user experience and a proxy for underlying healthcare need. The ease of claim submission, measured by a five-point Likert scale, captures the administrative burden and user-centered aspects of the insurance process, directly influencing satisfaction. At the same time, individuals who frequently file claims are likely to have greater healthcare needs, making claim filing a marker of both administrative experience and underlying health status (Hibbard et al., 2007; Mechanic and Schlesinger, 1996; Andersen, 1995). This duality is reflected in the analytic models, where claim filing is associated with both higher telehealth utilization and greater satisfaction when the process is perceived as easy. The substantial influence of administrative elements is apparent. The simplicity of claim submission frequently correlates with increased satisfaction, reinforcing the notion that operational efficiency is crucial to patient experience. Unexpected bills serve a dual function: they increase the probability of telehealth utilization (perhaps by encouraging users to explore alternatives to in-person care) while simultaneously diminishing satisfaction, suggesting that financial unpredictability detracts from the perceived value of telehealth services.
Despite its strengths, the use of claim filing as a measure in this study presents limitations. While it effectively captures the administrative dimension of user experience, it may also conflate satisfaction with underlying healthcare need, as individuals with higher medical needs are more likely to file claims. This potential confounding should be considered when interpreting the results, and future research should seek to disentangle administrative experience from healthcare utilization by incorporating more granular measures of health status and claim complexity. This limitation has now been explicitly acknowledged in the discussion to enhance transparency and interpretability.
Psychological pricing is a vital factor in the models. The single-stage satisfaction models indicate a strong positive effect. However, the Heckman-adjusted estimates imply that this effect is relatively moderate when selection is considered. This attenuation suggests that consumers views of affordability may influence the decision to use telehealth, but their satisfaction, once engaged, relies on a wider array of criteria. The significance of both objective and subjective financial literacy underscores the intricacy of consumer behavior in healthcare. While objective financial literacy marginally reduces telehealth utilization, it increases user satisfaction–a trend indicating that more informed consumers may be more discerning in their adoption choices but ultimately gain greater advantages from telehealth engagement. The presence of a primary care physician correlates positively with telehealth utilization, underscoring the significance of existing patient-provider connections in enhancing access to novel treatment models. Nonetheless, its varied impact on satisfaction suggests that although continuity of treatment is crucial, the quality of telehealth encounters relies on criteria beyond the mere presence of a primary care relationship.
Demographic controls enhance the analysis. The varying impacts noted for race, gender, income, and education corroborate previous research indicating that socioeconomic and demographic variables are crucial drivers of both access to and satisfaction with healthcare services. Self-evaluated mental health, captured as respondents subjective rating of their current psychological well-being, demonstrates an important trend in the results. Consistent with economic and health literature (Ahmad et al., 2014; Smith, 1999), higher self-evaluated mental health significantly decreases the likelihood of telehealth utilization. However, among those who do use telehealth, individuals reporting better mental health also report greater satisfaction with the service. This pattern may indicate that while those with poorer mental health are more likely to seek out telehealth as a critical, accessible option, those with better mental health are able to derive more enjoyment or benefit once they engage with these services. This aligns with prior research indicating that perceived mental health shapes not only care-seeking decisions but also the quality of health care experiences and outcomes (Dowd and Zajacova, 2010). Thus, telehealth appears to serve as both a safety net for those in greater need and as an effective tool for well-being maintenance among healthier users.
The exclusion restrictions–plan type, utilization of preventive health services, and urban/suburban residency—are crucial for delineating the selection process. Their incorporation in the initial model and omission from the satisfaction equation guarantees the accurate identification of the Heckman correction. The model comparison statistics (AIC, BIC, Log-Likelihood, R-squared) in the second table substantiate the robustness of the Heckman model since it provides a comparable overall fit while addressing selection bias. Whereas single-stage models provide useful first insights into the factors influencing telehealth usage and satisfaction, they may generate skewed estimates due to the failure to consider the nonrandom selection of telehealth users. The Heckman two-stage method not only rectifies this bias but also offers a more intricate comprehension of the influences exerted by network adequacy, administrative efficiency, cost perceptions, financial literacy, and demographic variables. With the expansion of telehealth—exacerbated by the COVID-19 pandemic and changing healthcare policies—it is crucial that forthcoming research and policy assessments consider selection bias to enhance the efficacy and equity of health service delivery.
5 Conclusion
This research indicates that telehealth usage and satisfaction are significantly affected by perceived network adequacy, administrative simplicity, and cost perceptions. The dual modeling approach, namely the Heckman two-stage correction, reveals substantial selection bias that may exaggerate the effects seen in single-stage models. A reasonable level of network adequacy encourages telehealth utilization, but excessive perceived adequacy may hinder its adoption, and satisfaction generally increases nonlinearly with heightened perceived adequacy. Administrative elements, including the simplicity of claim submission and consumer views of pricing, are also vital determinants. These findings emphasize that successful telehealth implementation relies on service availability and overcoming systemic and operational obstacles. Policy actions that improve network integration and optimize administrative processes are crucial for guaranteeing equitable access and superior patient experiences. The study underscores the necessity for enhanced telehealth research techniques to facilitate advancements in evidence-based healthcare delivery.
6 Future directions
Subsequent research should analyze the enduring effects of telehealth on clinical outcomes, scrutinize the influence of digital and financial literacy on technology adoption, evaluate the cost-effectiveness of diverse telehealth models, investigate methods for the seamless integration of telehealth with conventional care, and assess specific policies aimed at mitigating disparities in telehealth access and satisfaction.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
FN: Writing – original draft, Formal analysis, Writing – review & editing, Visualization, Conceptualization, Methodology.
Funding
The author declares that no financial support was received for the research and/or publication of this article.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author declares that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Agarwal, S., Driscoll, J. C., Gabaix, X., and Laibson, D. (2007). “The age of reason: financial decisions over the lifecycle,” in National Bureau of Economic Research. Working Paper (Cambridge, MA).
Ahmad, F., Jhajj, A. K., Stewart, D. E., Burghardt, M., and Bierman, A. S. (2014). Single item measures of self-rated mental health: a scoping review. BMC Health Serv. Res. 14, 1–11. doi: 10.1186/1472-6963-14-398
Andersen, R. M. (1995). Revisiting the behavioral model and access to medical care: does it matter? J. Health Soc. Behav. 36, 1–10. doi: 10.2307/2137284
Ansolabehere, S., and Rivers, D. (2013). Cooperative survey research. Ann. Rev. Polit. Sci. 16, 307–329. doi: 10.1146/annurev-polisci-022811-160625
Austin, P. C., Fang, J., and Lee, D. S. (2022). Using fractional polynomials and restricted cubic splines to model non-proportional hazards or time-varying covariate effects in the cox regression model. Statist. Med. 41, 612–624. doi: 10.1002/sim.9259
Bashshur, R. L., Shannon, G. W., Smith, B. R., Alverson, D. C., Antoniotti, N., Barsan, W. G., et al. (2014). The empirical foundations of telemedicine interventions for chronic disease management. Telemed. e-Health 20, 769–800. doi: 10.1089/tmj.2014.9981
Battaglia, M. P., Hoaglin, D. C., and Frankel, M. R. (2009). Practical considerations in raking survey data. Survey Pract. 2:5. doi: 10.29115/SP-2009-0019
Bokolo, A. J. (2021). Exploring the adoption of telemedicine and virtual software for care of outpatients during and after covid-19 pandemic. Irish J. Med. Sci. 190, 1–10. doi: 10.1007/s11845-020-02299-z
Busch, S. H., and Kyanko, K. (2021). Assessment of perceptions of mental health vs medical health plan networks among us adults with private insurance. JAMA Netw. Open 4, e2130770–e2130770. doi: 10.1001/jamanetworkopen.2021.30770
Bushway, S., Johnson, B. D., and Slocum, L. A. (2007). Is the magic still there? the use of the heckman two-step correction for selection bias in criminology. J. Quantit. Criminol. 23, 151–178. doi: 10.1007/s10940-007-9024-4
Cameron, A. (2005). Microeconometrics: Methods and Applications. Cambridge: Cambridge University. doi: 10.1017/CBO9780511811241
Campion, E. W., Dorsey, E., and Topol, E. (2016). State of telehealth. New Engl. J. Med. 375, 154–161. doi: 10.1056/NEJMra1601705
Certo, S. T., Busenbark, J. R., Woo, H.-s., and Semadeni, M. (2016). Sample selection bias and heckman models in strategic management research. Strat. Managem. J. 37, 2639–2657. doi: 10.1002/smj.2475
Chen, J., Amaize, A., and Barath, D. (2021). Evaluating telehealth adoption and related barriers among hospitals located in rural and urban areas. J. Rural Health 37, 801–811. doi: 10.1111/jrh.12534
Contreras, C. M., Metzger, G. A., Beane, J. D., Dedhia, P. H., Ejaz, A., and Pawlik, T. M. (2020). Telemedicine: patient-provider clinical engagement during the covid-19 pandemic and beyond. J. Gastrointest. Surg. 24, 1692–1697. doi: 10.1007/s11605-020-04623-5
Corlette, S., Volk, J., Berenson, R., and Feder, J. (2014). Narrow Provider Networks in New Health Plans: Balancing Affordability with Access to Quality Care. Washington, DC: Georgetown University Health Policy Institute.
Cutler, D. M., and Lleras-Muney, A. (2010). Understanding differences in health behaviors by education. J. Health Econ. 29, 1–28. doi: 10.1016/j.jhealeco.2009.10.003
DeBell, M., and Krosnick, J. A. (2009). Computing Weights for American National Election Study Survey Data. Ann Arbor, MI, Palo Alto, CA: ANES Technical Report Series.
Douthit, N., Kiv, S., Dwolatzky, T., and Biswas, S. (2015). Exposing some important barriers to health care access in the rural usa. Public Health 129, 611–620. doi: 10.1016/j.puhe.2015.04.001
Dowd, J. B., and Zajacova, A. (2010). Does self-rated health mean the same thing across socioeconomic groups? Evidence from biomarker data. Ann. Epidemiol. 20, 743–749. doi: 10.1016/j.annepidem.2010.06.007
Fernandes, D., Lynch, J. G. J., and Netemeyer, R. G. (2014). Financial literacy, financial education, and downstream financial behaviors. Managem. Sci. 60, 1861–1883. doi: 10.1287/mnsc.2013.1849
Filipow, N., Main, E., Tanriver, G., Raywood, E., Davies, G., Douglas, H., et al. (2023). Exploring flexible polynomial regression as a method to align routine clinical outcomes with daily data capture through remote technologies. BMC Med. Res. Methodol. 23:114. doi: 10.1186/s12874-023-01942-4
Gajarawala, S. N., and Pelkowski, J. N. (2021). Telehealth benefits and barriers. J. Nurse Practition. 17, 218–221. doi: 10.1016/j.nurpra.2020.09.013
Greenhalgh, T., Wherton, J., Shaw, S., and Morrison, C. (2020). Video consultations for COVID-19. BMJ 368. doi: 10.1136/bmj.m998
Groves, R. M., and Couper, M. P. (2012). Nonresponse in Household Interview Surveys. Hoboken, NJ: John Wiley & Sons.
Haeder, S. F., and Xu, W. Y. (2024). When is a network adequate? Consumer perspectives on network adequacy definitions. Am. J. Managed Care 30, 424–432. doi: 10.37765/ajmc.2024.89601
Harkey, L. C., Jung, S. M., Newton, E. R., and Patterson, A. (2020). Patient satisfaction with telehealth in rural settings: a systematic review. Int. J. telerehabilitat. 12:53. doi: 10.5195/ijt.2020.6303
Heckman, J. J. (1979). Sample selection bias as a specification error. Econometrica 47, 153–161. doi: 10.2307/1912352
Hendy, A., Abdelaliem, S. M. F., Zaher, A., Sadek, B. N., Nashwan, A. J., Al-Jabri, M. M. A., et al. (2025). Telehealth satisfaction among patients with chronic diseases: a cross-sectional analysis. PeerJ 13:e19245. doi: 10.7717/peerj.19245
Hibbard, J. H., Mahoney, E. R., Stock, R., and Tusler, M. (2007). Do increases in patient activation result in improved self-management behaviors? Health Serv. Res. 42, 1443–1463. doi: 10.1111/j.1475-6773.2006.00669.x
Hoadley, J., and Lucia, K. (2022). The no surprises act: a bipartisan achievement to protect consumers from unexpected medical bills. J. Health Polit. Policy Law 47, 93–109. doi: 10.1215/03616878-9417470
Hollander, J. E., and Carr, B. G. (2020). Virtually perfect? Telemedicine for covid-19. N. Engl. J. Med. 382, 1679–1681. doi: 10.1056/NEJMp2003539
Hoseini-Esfidarjani, S.-S., Negarandeh, R., Delavar, F., and Janani, L. (2021). Psychometric evaluation of the perceived access to health care questionnaire. BMC Health Serv. Res. 21:638. doi: 10.1186/s12913-021-06655-2
Kalton, G. (2009). Methods for oversampling rare subpopulations in social surveys. Survey Methodol. 35, 125–141.
Keisler-Starkey, K., Bunch, L. N., and Lindstrom, R. A. (2023). Health insurance coverage in the United States: 2022 (Current Population Reports, P60-281). Washington, DC: U.S. Census Bureau. Available online at: https://www.census.gov/content/dam/Census/library/publications/2023/demo/p60-281.pdf
Koh, H. K., and Sebelius, K. G. (2010). Promoting prevention through the affordable care act. N. Engl. J. Med. 363:1296–1299. doi: 10.1056/NEJMp1008560
Kolenikov, S. (2014). Calibrating survey data using iterative proportional fitting (raking). Stata J. 14, 22–59. doi: 10.1177/1536867X1401400104
Koonin, L. M. (2020). Trends in the use of telehealth during the emergence of the Covid-19 pandemic-united states, january-march 2020. Morbid. Mortal. Weekly Report 69:3. doi: 10.15585/mmwr.mm6943a3
Kruse, C. S., Krowski, N., Rodriguez, B., Tran, L., Vela, J., and Brooks, M. (2017). Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open 7:e016242. doi: 10.1136/bmjopen-2017-016242
Kumar, S., and Pandey, M. (2017). The impact of psychological pricing strategy on consumers' buying behaviour: a qualitative study. Int. J. Busin. Syst. Res. 11, 101–117. doi: 10.1504/IJBSR.2017.080843
Lusardi, A., and Mitchell, O. S. (2014). The economic importance of financial literacy: Theory and evidence. Am. Econ. J. 52, 5–44. doi: 10.1257/jel.52.1.5
Mann, D. M., Chen, J., Chunara, R., Testa, P. A., and Nov, O. (2020). Covid-19 transforms health care through telemedicine: evidence from the field. J. Am. Med. Inform. Assoc. 27, 1132–1135. doi: 10.1093/jamia/ocaa072
McDonald, K. M., Sundaram, V., Bravata, D. M., et al. (2007). “Closing the quality gap: a critical analysis of quality improvement strategies (Vol. 7: care coordination),” in Technical Reviews, No. 9.7. (Rockville, MD: Agency for Healthcare Research and Quality).
Mechanic, D., and Schlesinger, M. (1996). The impact of managed care on patients' trust in medical care and their physicians. JAMA 275, 1693–1697. doi: 10.1001/jama.1996.03530450083048
Mehrotra, A., Bhatia, R. S., and Snoswell, C. L. (2021). Paying for telemedicine after the pandemic. JAMA 325, 431–432. doi: 10.1001/jama.2020.25706
Mittone, D. F., Bailey, C. P., Eddy, E. L., Napolitano, M. A., and Vyas, A. (2022). Women's satisfaction with telehealth services during the covid-19 pandemic: cross-sectional survey study. JMIR Pediat. Parent. 5:e41356. doi: 10.2196/41356
National Committee for Quality Assurance (NCQA) (2020). Taskforce on Telehealth Policy: Findings and Recommendations Telehealth Effect on Total Cost of Care. Washington, DC: NCQA.
National Rural Health Association (2025). Telehealth's Impact on Rural Hospitals: A Literature Review. Washington, DC: National Rural Health Association.
Network Adequacy Standards (2023). 45 cfr 156.230 - Network Adequacy Standards. Washington, DC: Office of the Federal Register, National Archives and Records Administration (NARA).
Nkouaga, F. (2024a). Comparative effects of self-evaluated and test-based financial literacy on choosing life insurance policies in a multi-racial context. Financ. Metrics Busin. 5, 352–371. doi: 10.25082/FMB.2024.01.001
Nkouaga, F. (2024b). Pandemic-era trends in us automatic payment adoption: a 2022 behavioral analysis. Int. Busin. Res. 17:1. doi: 10.5539/ibr.v17n6p1
Nouri, S., Khoong, E. C., Lyles, C. R., and Karliner, L. (2020). Addressing equity in telemedicine for chronic disease management during the COVID-19 pandemic. NEJM Catalyst Innovat. Care Delivery 1:3. doi: 10.1056/CAT.19.1111
Pasek, J., and Pasek, M. J. (2018). “Package anesrake,” in The Comprehensive R Archive Network, 1–13.
Pollitz, K. (2022). Network Adequacy Standards and Enforcement. San Francisco, CA: Kaiser Family Foundation.
Puhani, P. (2000). The heckman correction for sample selection and its critique. J. Econ. Surveys 14, 53–68. doi: 10.1111/1467-6419.00104
Qadri, A., and Sodhi, G. D. (2025). Is psychological pricing a pricing strategy or a loophole? Int. J. Finan. Managem. Res. 7:41163. doi: 10.36948/ijfmr.2025.v07i02.41163
Royston, P., and Sauerbrei, W. (2007). Multivariable modeling with cubic regression splines: a principled approach. Stata J. 7, 45–70. doi: 10.1177/1536867X0700700103
Schadelbauer, R. (2017). Anticipating Economic Returns of Rural Telehealth. Arlington, VA: NTCA-The Rural Broadband Association.
Shigekawa, E., Fix, M., Corbett, G., Roby, D. H., and Coffman, J. (2018). The current state of telehealth evidence: a rapid review. Health Affairs 37, 1975–1982. doi: 10.1377/hlthaff.2018.05132
Shortell, S. M., and Kaluzny, A. D. (1994). Health Care Management: Organization, Design, and Behavior (Delmar series in health services administration). Albany: Delmar Publishers.
Smith, A. C., Thomas, E., Snoswell, C. L., Haydon, H., Mehrotra, A., Clemensen, J., et al. (2020). Telehealth for global emergencies: implications for coronavirus disease 2019 (covid-19). J. Telemed. Telecare 26, 309–313. doi: 10.1177/1357633X20916567
Smith, J. P. (1999). Healthy bodies and thick wallets: the dual relation between health and economic status. J. Econ. Perspect. 13, 145–166. doi: 10.1257/jep.13.2.145
Starfield, B. (1998). Primary Care: Balancing Health Needs, Services, and Technology. Oxford: Oxford University Press.
Steinbrook, R. (2019). Ending surprise medical bills. JAMA Intern. Med.179, 1465–1466. doi: 10.1001/jamainternmed.2019.3382
Totten, A., Womack, D. M., McDonagh, M. S., Davis-O'Reilly, C., Griffin, J. C., Blazina, I., et al. (2023). “Improving rural health through telehealth-guided provider-to-provider communication,” in Technical Report, Europe PMC. Rockville, MD: Agency for Healthcare Research and Quality (AHRQ).
Totten, A. M., Womack, D. M., Eden, K. B., McDonagh, M. S., Griffin, J. C., Grusing, S., et al. (2016). Telehealth: Mapping the Evidence for Patient Outcomes from Systematic Reviews. North Bethesda, MD: Agency for Healthcare Research and Quality.
Uscher-Pines, L., and Mehrotra, A. (2014). Analysis of teladoc use seems to indicate expanded access to care for patients without prior connection to a provider. Health Affairs 33, 258–264. doi: 10.1377/hlthaff.2013.0989
Vella, F. (1998). Estimating models with sample selection bias: a survey. J. Human Resour. 33, 127–169. doi: 10.2307/146317
Wedel, M., and Leeflang, P. S. (1998). A model for the effects of psychological pricing in gabor-granger price studies. J. Econ. Psychol. 19, 237–260. doi: 10.1016/S0167-4870(98)00006-3
Weinstein, R. S., Lopez, A. M., Joseph, B. A., Erps, K. A., Holcomb, M., Barker, G. P., et al. (2014). Telemedicine, telehealth, and mobile health applications that work: opportunities and barriers. Am. J. Med. 127, 183–187. doi: 10.1016/j.amjmed.2013.09.032
Whitacre, B. E. (2011). Estimating the economic impact of telemedicine in a rural community. Agricult. Resour. Econ. Rev. 40, 172–183. doi: 10.1017/S1068280500007991
Williams, C., and Shang, D. (2023). Telehealth usage among low-income racial and ethnic minority populations during the covid-19 pandemic: retrospective observational study. J. Med. Intern. Res. 25:e43604. doi: 10.2196/43604
Wolfolds, S. E., and Siegel, J. (2019). Misaccounting for endogeneity: the peril of relying on the heckman two-step method without a valid instrument. Strat. Managem. J. 40, 432–462. doi: 10.1002/smj.2995
Wooldridge, J. M. (2010). Econometric Analysis of Cross Section and Panel Data. Cambridge, MA: MIT Press.
Zachrison, K. S., Richard, J. V., and Mehrotra, A. (2021). Paying for telemedicine in smaller rural hospitals: extending the technology to those who benefit most. JAMA Health Forum 2:e211570. doi: 10.1001/jamahealthforum.2021.1570
Zhu, J. M., Breslau, J., and McConnell, K. J. (2021). Medicaid managed care network adequacy standards for mental health care access: balancing flexibility and accountability. JAMA Health Forum 2:e210280. doi: 10.1001/jamahealthforum.2021.0280
Zhu, J. M., Meiselbach, M. K., Drake, C., and Polsky, D. (2023). Psychiatrist networks in medicare advantage plans are substantially narrower than in medicaid and aca markets: study examines psychiatrist networks in medicare advantage compared with medicaid and ACA markets. Health Affairs 42, 909–918. doi: 10.1377/hlthaff.2022.01547
Zhu, J. M., Polsky, D., Johnstone, C., and McConnell, K. J. (2022). Variation in network adequacy standards in medicaid managed care. Am. J. Manag. Care 28:288. doi: 10.37765/ajmc.2022.89156
Zhu, J. M., Rowland, R., Polsky, D., Suneson, I., Haeder, S. F., Cohen, D. J., et al. (2025). Medicaid managed care organizations' experiences with network adequacy. Health Affairs Scholar 3:qxaf049. doi: 10.1093/haschl/qxaf049
Keywords: telehealth, network adequacy, Heckman model, financial literacy, patient satisfaction, healthcare access
Citation: Nkouaga F (2025) Does perceived provider network strength foster telehealth usage among insured populations? Front. Behav. Econ. 4:1617041. doi: 10.3389/frbhe.2025.1617041
Received: 23 April 2025; Accepted: 12 September 2025;
Published: 02 October 2025.
Edited by:
Abu Siddique, Royal Holloway, University of London, United KingdomReviewed by:
Henrike Sternberg, Technical University of Munich, GermanyPauline Pearcy, London School of Economics and Political Science, United Kingdom
Copyright © 2025 Nkouaga. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Florent Nkouaga, Zm5rb3VhZ2FAZ21haWwuY29t
 Florent Nkouaga
Florent Nkouaga