- 1Department of Sociology, Psychology and Anthropology, Moi University, Eldoret, Kenya
- 2Department of Obstetrics and Gynecology, Aga Khan University, Nairobi, Kenya
- 3School of Arts and Social Sciences, Moi University, Eldoret, Kenya
- 4School of Science, Moi University, Eldoret, Kenya
- 5School of Medicine, Moi University, Eldoret, Kenya
- 6Corewell Health West, Michigan State University, Grand Rapids, MI, United States
- 7Department of Medicine, Indiana University Melvin and Bren Simon Cancer Center, Indianapolis, IN, United States
Introduction: Cervical cancer is the greatest cause of cancer-related death among women in Sub-Saharan Africa, with particularly high incidence and mortality rates in rural regions. In Kenya, Women with HIV/AIDS (WLHA) are at a greater risk of developing cervical cancer though screening rate remains low. Information, education and communication (IEC) materials play a crucial role in raising awareness, promoting screening, and supporting early detection and treatment; however, little is known about the accessibility, content, and perceived effectiveness of these materials from the perspective of WLHA.
Methods: The objective of this study was to determine the common sources, perceived communication efficacy and sufficiency of IEC materials among WLHA and attending clinics in Webuye and Mosoriot both which are health facilities in rural Kenya. Data were collected using a researcher administered questionnaire for 380 WLHA and an IEC checklist for 20 Key stakeholders resulting in a total sample size of 400 participants.
Results: Sixteen sources of information were identified, with the most common and preferred being radio, health professionals, support groups, chief's mabaraza and posters. Indicators for communicative efficacy revealed that cervical cancer IEC print materials were not effective in format (77%), the location where they are placed (60%), and graphical appeal (50%). Additionally, 66% of participants found the IEC materials insufficient, inaccessible, and inappropriate.
Discussion: While a variety of cervical cancer IEC materials exist, WLHA in rural Kenya perceive significant gaps in the availability and effectiveness of these materials. Some IEC materials are preferred because they offer direct interaction, cultural relevance, and broader outreach.
Background
Cervical cancer remains a pressing health challenge, particularly in low- and middle-income countries (LMICs), where it is the most common cancer among women and a leading cause of death in some regions (1). Globally, it ranks as the fourth most prevalent cancer among women. While effective preventive measures like the Pap smear test exist, cervical cancer continues to disproportionately affect women in low-income countries due to limited access to screening and healthcare services. An estimated 80% of women in these regions have never been screened for cervical cancer, with many being diagnosed at advanced stages (2). In Kenya, despite healthcare advancements and policies promoting cancer prevention, the utilization of cervical cancer screening services remains low, particularly in rural areas (3). This contrasts with developed nations, where robust screening programs, paired with widespread information dissemination, have significantly reduced cervical cancer incidence and mortality rates (4). The disparity underscores the urgent need for targeted interventions to improve awareness, screening, and treatment accessibility in resource-limited settings like rural Kenya.
Women with HIV/AIDS (WLHA) are at a heightened risk of developing cervical cancer due to their compromised immune systems. The prevalence of HIV/AIDS in Kenya, particularly in rural areas, compounds this vulnerability (5, 6). Limited access to healthcare, coupled with cultural stigmas and misconceptions about reproductive health, further inhibits WLHA from seeking preventive care. Late-stage cervical cancer diagnoses are common, contributing to high mortality rates in this population (7). In rural Kenya, societal norms, inadequate healthcare infrastructure, and a lack of targeted health education exacerbate the problem. WLHA require specialized care and tailored information to address their unique risks effectively. Research highlights the importance of integrating cervical cancer prevention into HIV care programs to improve health outcomes for this vulnerable group (5, 8).
Information, Education, and Communication (IEC) strategies have been recognized as effective tools for addressing health-related challenges, including cervical cancer (7). IEC materials use visual, audio, and audio-visual resources to educate target audiences, promote positive health-seeking behaviors, and dispel myths and stigma surrounding diseases (9). By delivering culturally sensitive messages, IEC initiatives can empower women with the knowledge needed to make informed decisions about their health. For cervical cancer, IEC materials play a vital role in raising awareness about risk factors, screening methods, and the importance of early detection. Studies show that well-designed IEC interventions can significantly increase screening rates, improve knowledge about cervical cancer, and encourage women to take proactive steps in managing their health (10). The World Health Organization (11) emphasizes the critical role of IEC materials in reducing cervical cancer incidence and mortality rates, particularly in LMICs where access to healthcare is limited.
In Kenya, IEC-based health education programs have been instrumental in addressing gaps in cervical cancer awareness. These programs are designed to build community capacity and improve healthcare service delivery. For instance (12), advocate for interactive strategies that encourage open discussions about fears, stigmas, and barriers to cervical cancer screening and treatment. Such initiatives not only foster community engagement but also promote behavior change by addressing misconceptions and reducing stigma. Despite the potential of IEC materials to drive change, several barriers hinder their effectiveness in rural Kenya. Existing societal norms, resource limitations, and deeply ingrained cultural practices often prevent women from accessing and utilizing health information. While the government and non-governmental organizations (NGOs) have made strides in promoting cancer awareness through campaigns like the Kenya Cancer Control Strategy 2017–2022, rural populations continue to face significant challenges in accessing preventive care and treatment. For instance, research by Akintayo and Bello (13) revealed that urban populations often rely mostly on television as their primary source of information about cancer and HIV/AIDS but in rural areas, access to such media is limited, further widening the knowledge gap. To address this disparity, IEC campaigns must leverage locally accessible communication channels.
Cervical cancer IEC materials for WLHA must go beyond merely providing information; they should aim to empower women with the tools and resources necessary to take control of their health. Effective IEC materials blend knowledge dissemination with strategies that encourage positive behavior change. For instance, community-based educational programs that use relatable examples and culturally sensitive messaging can help dispel myths and foster informed decision-making (14). Empowering women with accurate information is not only a healthcare imperative but also a fundamental human right. By addressing the unique needs of WLHA in rural Kenya, IEC initiatives can contribute to health equity and social justice, ensuring that no woman is left behind in the fight against cervical cancer.
To maximize their impact, IEC materials must be evaluated for their efficacy and sufficiency in meeting the needs of their target audiences. This involves assessing the common sources of information, the communication effectiveness of the materials, and their ability to foster knowledge and behavior change. Studies like (15) highlight the importance of tailoring communication strategies to resonate with specific audiences, particularly in resource-limited settings. In rural Kenya, efforts to improve the development and dissemination of IEC materials should prioritize community engagement, capacity building, and sustainable healthcare interventions. By understanding the barriers and facilitators of cervical cancer prevention, stakeholders can design more effective IEC campaigns that address the unique challenges faced by WLHA.
This study evaluates the common sources, communication efficacy, and sufficiency of cervical cancer IEC materials for WLHA in rural Kenya. The findings aim to inform strategies for improving the relevance and impact of these resources, ultimately enhancing cervical cancer prevention and care. By empowering women with culturally sensitive information and accessible healthcare services, IEC initiatives can play a pivotal role in reducing cervical cancer incidence and mortality rates, advancing health equity, and fostering social justice in underserved communities.
Methods
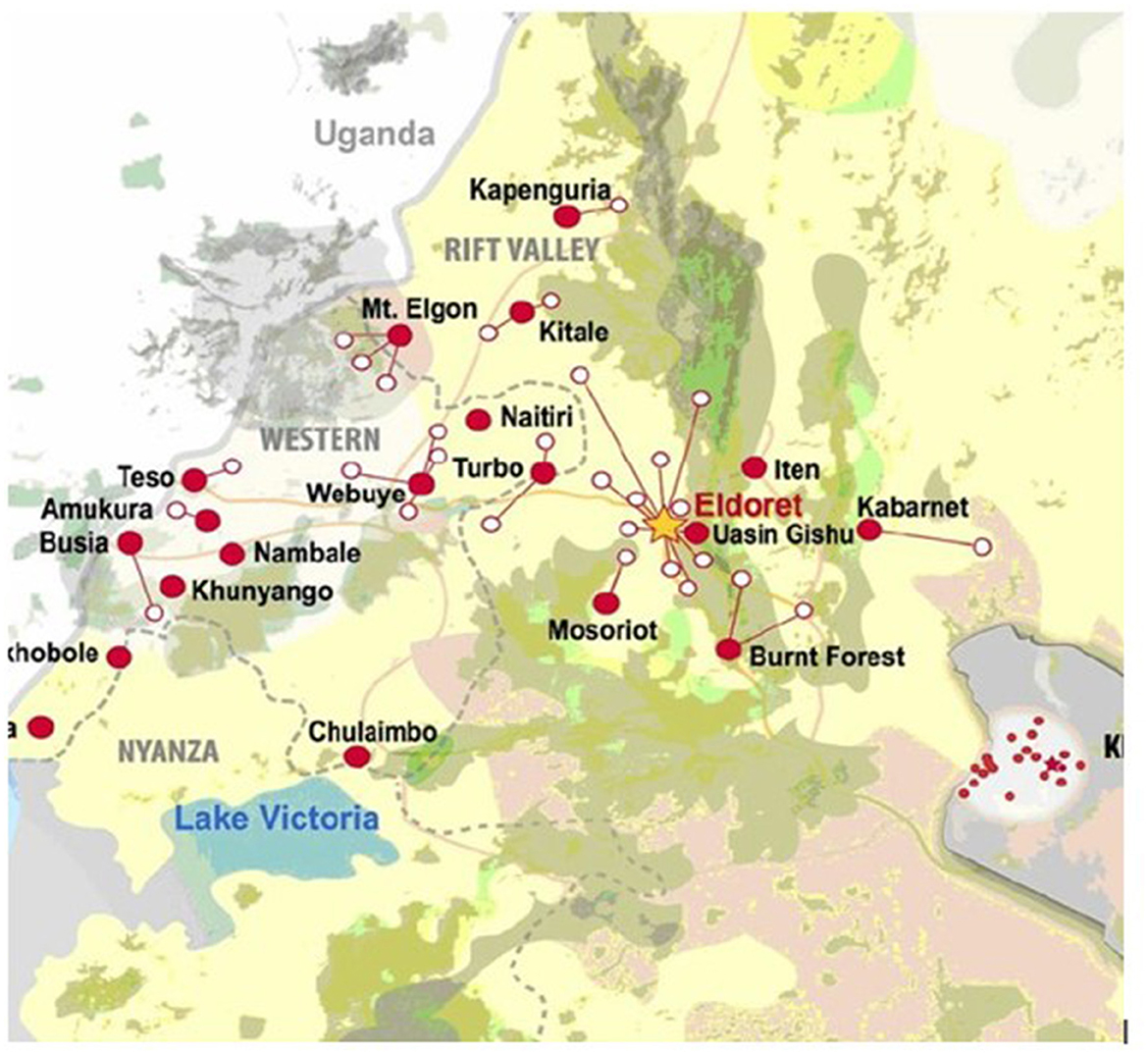
The study was carried out in two AMPATH sites in Kenya. AMPATH is an acronym for Academic Model Providing Access to Healthcare. This is a collaboration between prominent North American academic health centers (most notably Indiana University School of Medicine), Moi University (MU), and Moi Teaching and Referral Hospital (MTRH) both in Kenya. AMPATH coordinates comprehensive, integrated, and long-term activities in HIV prevention and care, primary health care, and chronic disease management and has over 300 clinical sites in Kenya providing cancer and HIV testing and care (16) (For this study, Webuye (Bungoma county) and Mosoriot (Nandi County) which are both in rural Kenya and differentiated by the rich cultural backgrounds were the selected sites (Figure 1).
Study population, sample, and recruitment
This was a facility-based cross-sectional study that made use of two categories of participants; WLHA and community stakeholders working with the women. HIV-positive women aged between 18 and 60 years, visiting the selected AMPATH clinics during the study period, and consenting to be interviewed formed the first category of participants. As of 2021, Webuye clinic had 3,785 (2,706 WLHA and 1,079 MLHA) while in Mosoriot the numbers were estimated to be 1,700 WLHA and 879 MLHA giving a total of 6,364 (men and women with HIV/AIDS in both regions). For this study, 4,406 of WLHA formed a total sample out of which 10% of the total sample was selected to participate with again 10% from each facility (271 from Webuye and 170 from Mosoriot). Out of this sample, 25 declined to participate on personal grounds or withdrew halfway during the interview. A total sample of 416 WLHA (262 from webuye and 154 from Mosoriot) was therefore engaged in this study. The selection of participants was on alternate basis for participants coming to the clinic during that period of 1 month and accepting to participate.
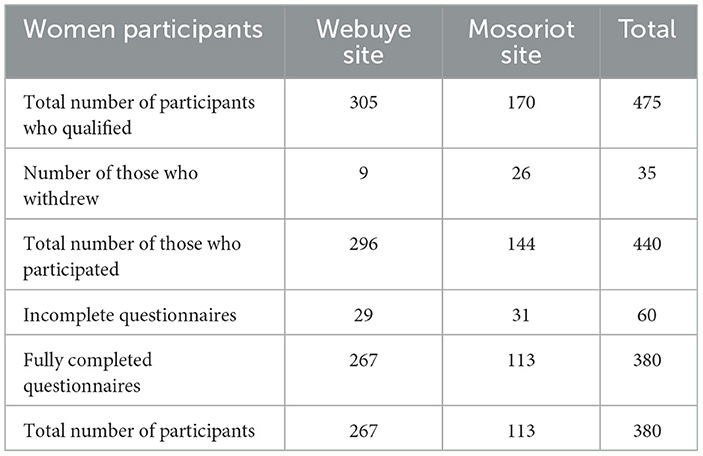
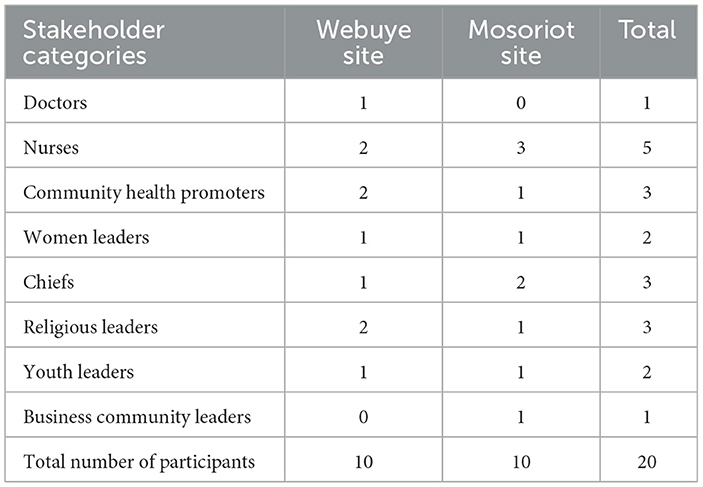
A second category of participants included 20 key stakeholders (10 from each facility). They were purposively selected based on the role they play in the community and their involvement with WLHA in the two sites. The stakeholder map was instrumental in the selection of these category of participants. They included members of the local government, religious leaders, medical personnel, community health workers, women and youth leaders, and business community leaders. They were instrumental in giving their views on the status of the available IEC materials in the regions and what was lacking. Tables 1, 2 have all the participant details.
Data collection processes
This study explored cervical cancer IEC materials for WLHA in rural Kenya. Data were collected using a structured questionnaire adapted from validated tools by FHI & PATH (17) and Amsale et al. (18). The questionnaire covered four domains: (1) socio-demographics, (2) sources of cervical cancer information, (3) perception of the IEC materials' effectiveness in enhancing understanding, and (4) sufficiency of the materials. Participants rated the usefulness of IEC materials on a 5-point Likert scale (1 = not effective, 5 = extremely effective) and indicated if the materials met their needs. Face-to-face interviews were conducted in Swahili or English based on preference. Excluded were women uninfected with HIV, those with hysterectomies, aged under 18 or over 60, or unwilling to participate. Additionally, an observation checklist documented health messaging efficacy at facilities, while stakeholders assessed the sufficiency and communication efficacy of IEC materials during a workshop.
Data management and analysis
Quantitative data was entered into a ReDcap database where data cleaning was carried out prior to data analysis. Data was then exported into STATA version 16 for analysis. Descriptive statistics were used to summarize the demographic data and the basic characteristics of the study sample. ANOVA was used to compare means and regression analysis was important in the prediction of perceived communication efficacy based on multiple independent variables (mainly; age, marital status, education level, income and career). In all the analysis a p-value, < 0.05 was considered significant. Qualitative findings collected through the abstraction of data and review of health messaging materials were coded and analyzed for thematic content.
Ethical aspects
The present study was approved by the Institutional Research and Ethics Committee (IREC) of Moi University and Moi Teaching and Referral Hospital with the Ref number IREC/2021/154 and approval number: 0003985. All participants also read and signed the informed consent document before participating in the study.
Results
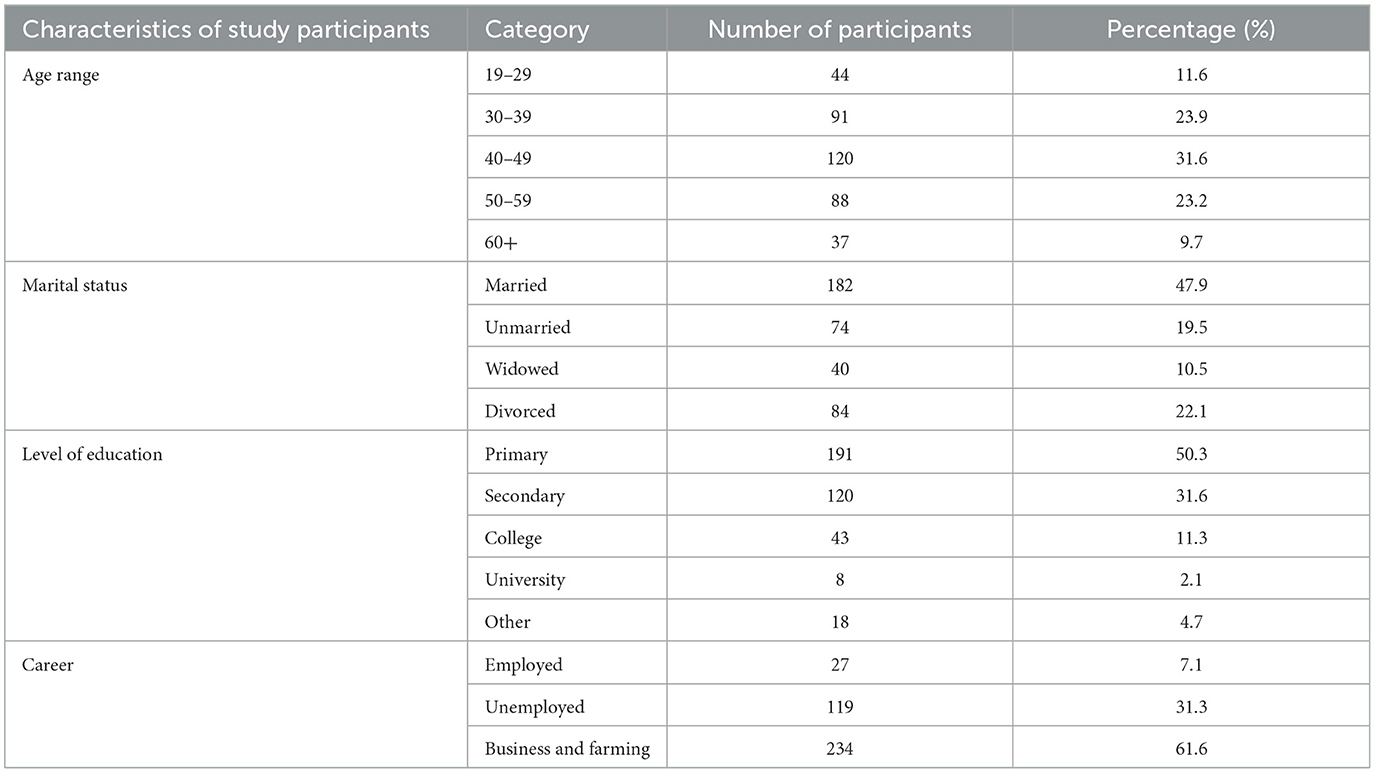
As indicated in Table 1, among the 440 questionnaires submitted, 60 were not included in the analysis because they were incomplete (29 from Webuye and 31 from Mosoriot) leaving a total of 380 dully filled questionnaires (267 from Webuye and 113 from Mosoriot) giving 86.4% return rate. All the 20 stakeholders had the checklists clearly completed. This study therefore had 400 participants (380 WLHA and 20 stakeholders). Table 3 gives the socio-demographic characteristics of the participants.
Majority (31.1%) were of the 40–49 age bracket, with the highest level of education being primary school (50.3%), 47.9% of the total population were married and over 60% were self-employed or carrying out some farming. Majority of participants (95.8%) identified as Christians, with 3.5% identifying as Muslims and < 1% wishing not to answer. About 72.0% stated that they were sexually active, while 20.8% were not and 7.2% chose not to respond. About 69.3% claimed never having been tested for cervical cancer, 30.1% had been tested, and fewer than 1% chose not to respond. Most (78%) reported that they had seen some IEC materials only at the health facility and most were text based, they contained pictures and illustrations. All of them had never seen cervical cancer brochures or booklets.
Sources of information on cervical cancer
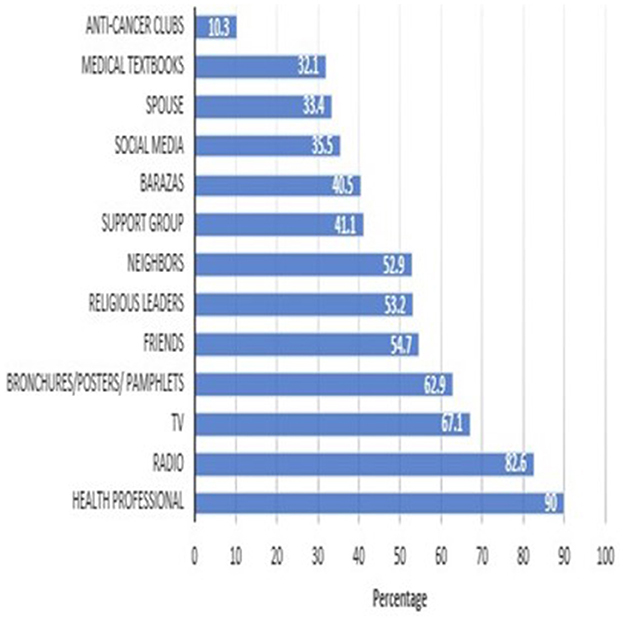
The study reveals no single preferred source for cervical cancer awareness, with participants relying on diverse channels. Healthcare professionals were the most trusted (90%), followed by radio (82.5%), TV (67.9%), and posters (62.9%). This diversity highlights the need for a multifaceted approach to awareness campaigns, catering for varied preferences and accessibility levels. Healthcare professionals and Radio are particularly effective in rural areas with lower literacy. The findings stress that combining trusted professional guidance with the reach of media and the accessibility of visual aids creates a robust awareness framework, ensuring that messages resonate across different demographics. Figure 2 summarizes these preferences, shaping effective awareness strategies.
Communication efficacy
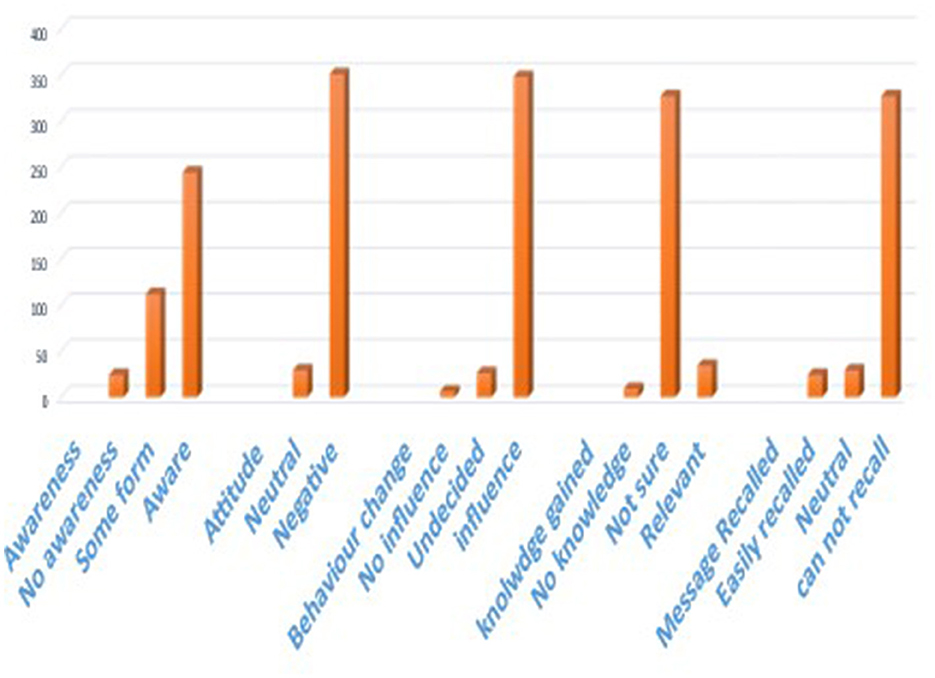
Key indicators of IEC communication efficacy included message clarity, awareness, knowledge gained, attitude change, and recall (Figure 3). While 92.15% of participants found IEC materials useful in increasing knowledge about cervical cancer, < 2.5% believed this knowledge influenced their attitude toward screening or treatment, highlighting a significant gap in effectiveness. Literacy levels played a major role, as many participants reported weak reading skills, making it difficult to engage with the materials. About 71% felt the printed materials were not easy to understand due to differences in education, socio-economic status, and age. Only 18.1% of participants could easily comprehend the messages, while 81.9% struggled, citing issues like excessive text, small font sizes, and culturally insensitive visuals.
Additionally, healthcare professionals were often seen to be too busy to disseminate information, with 72% of participants only interacting with them briefly during HIV clinic visits. Message recall was also poor, with over half unable to remember details despite exposure to various media. The most commonly recalled detail by 81% was that cervical cancer is fatal, often discussed among peers. Generally, 78% of the participants acknowledged the usefulness of IEC materials but felt that in their current state, message comprehension was difficult because of issues like cultural sensitivity, message recall communication efficacy and impact.
Perceived sufficiency of IEC materials
The sufficiency of IEC materials depends on availability, accessibility, relevance, engagement, and quality. This study found IEC materials in posters being the most common in health facilities. However, their limited presence, typically one or two posters per facility restricted their impact. Younger participants (18–39 years) favored digital platforms like mobile phones, television and to some extent radio but these formats were hindered by limited access, complex language, and insufficient content. For example, 81% found radio discussions uninformative or fear-inducing, while 63% reported misinformation on social media, leading to stigma. Cultural barriers, such as fear of spousal blame, also reduced engagement.
Critical gaps in cervical cancer information dissemination were identified. Although healthcare professionals, chief's community forums (mabarazas), radio, and support groups were preferred sources, the information was inadequate. Unlike in HIV/AIDS, cervical cancer lacked dedicated support groups and discussions in mabarazas. In hospitals, few healthcare professionals provided cervical cancer information during HIV clinic visits. Radio was a popular medium, but discussions often occurred during working hours, limiting access, while 33% preferred local language broadcasts. Cultural appropriateness was another concern, with 70% reporting that IEC materials overlooked local beliefs. Posters with culturally insensitive images and text-heavy formats were particularly ineffective, as 66% struggled with dense text and small fonts. Additionally, 72% viewed the materials as ineffective due to limited follow-up and monitoring.
Stakeholders identified insufficiencies in print materials, particularly in format (77%), placement (60%), and communication appropriateness (64%). While 65% rated the information selection positively, many materials used technical terms and small fonts, making them difficult to comprehend. Over 70% of stakeholders noted readers' unwillingness to engage with lengthy materials or apply what they had read.
Regarding relevance, only 2.6% of participants found IEC materials relevant, with 44.1% deeming them irrelevant, particularly among those aged 40–49. Although IEC materials increased knowledge about HIV/AIDS (51%), their influence on cervical cancer awareness and behavior was limited with only 34% of participants having taken a Pap smear test, and just 18% recognized routine screening as a preventive measure. All participants reported that the IEC materials do not address cultural barriers to screening procedures. Although some participants may have opted for Inspection with Acetic Acid (VIA) over Pap smears, it is scantly mentioned in IEC materials, despite its prevalence in Kenya. This study however did not establish VIA screening rates.
Sociodemographic factors also significantly influenced perceptions of IEC sufficiency. Married individuals reported higher sufficiency (48.4%) than unmarried ones (51.6%). Career type was highly significant (p < 0.001), with business (32.4%) and farming (30.3%) professionals showing greater sufficiency perceptions than the unemployed (73.9%). Higher-income earners (≥10,000 Ksh) found the IEC materials more sufficient (25.1%) compared to lower earners (74.9%), while tertiary-educated participants exhibited higher perceptions in IEC material sufficiency (19.4%) than those with primary education (44.2%). Education level however showed borderline significance (p = 0.052), indicating a potential association (Table 4 has these details).
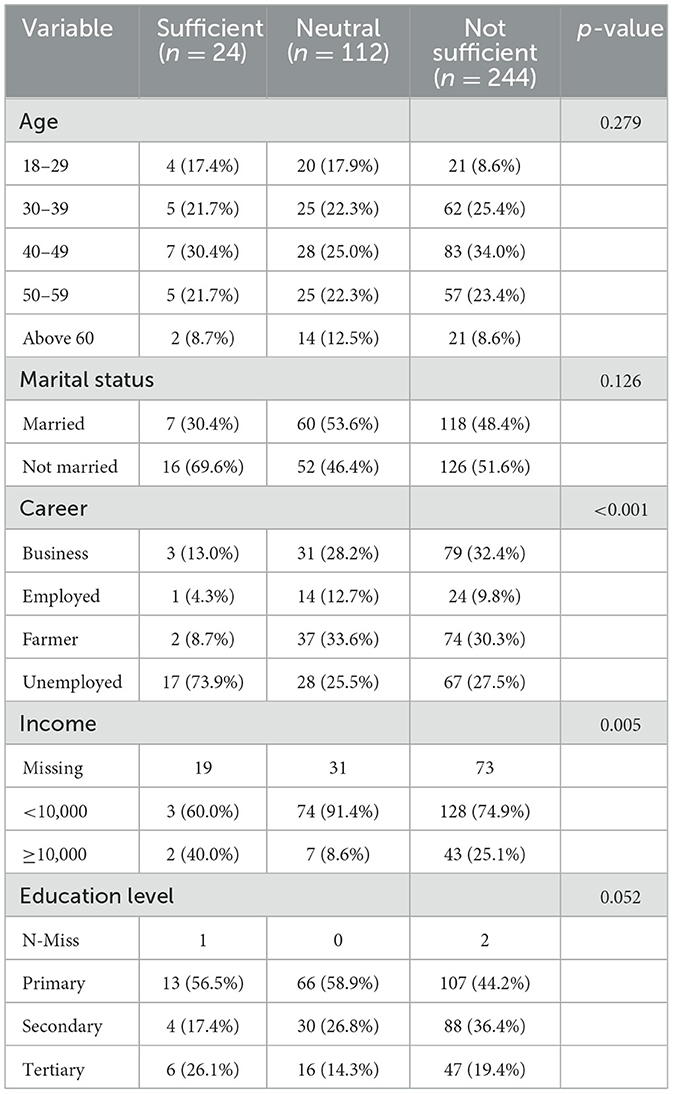
Table 4. Association between sociodemographic characteristics and perceived sufficiency of IEC materials.
Despite frequent health facility visits by HIV positive women, cervical cancer education opportunities remain underutilized. Posters were poorly placed, with Webuye displaying one and Mosoriot none at the HIV clinics. These findings highlight the need for targeted, inclusive, and culturally sensitive IEC materials to promote cervical cancer awareness and screening among WLHA in rural Kenya.
Discussion
The dissemination of health information is a fundamental aspect of improving health outcomes, especially when addressing sensitive topics like cervical cancer. This study highlights the significant role of IEC materials such healthcare providers, radio, TV, and posters as primary sources of information for WLHA in rural Kenya. It reveals key insights into the effectiveness, challenges, and gaps in the dissemination of cervical cancer-related information, emphasizing the need for a multifaceted approach that considers both the medium and the content of educational materials. The findings align with previous studies, providing valuable insights into how to improve awareness and behavior change regarding cervical cancer.
The study revealed that healthcare professionals, chief's mabarazas, radio, and support groups were preferred information sources, yet each exhibited a significant limitation. Chief's mabarazas, which are important community engagement platforms, were underutilized for cervical cancer education, despite their potential to engage community members effectively. Cervical cancer remains a taboo subject in many rural communities, further compounding challenges in information dissemination and engagement. Participants noted that the topic was rarely addressed in religious settings or community forums, such as chief's mabarazas. This silence reflects deeply rooted cultural norms and misconceptions about reproductive health, which hinder open dialogue and collective action (7). Kemper et al. (5) argue that community-based interventions are critical for increasing awareness in rural areas, and using mabarazas for cervical cancer discussions would help normalize the topic and encourage open dialogue. Similarly, the absence of cervical cancer support groups further limit opportunities for peer learning and shared experiences, which are crucial for creating an informed and empowered community. Community based interventions are therefore crucial in dealing with stigma. Rimande-Joel and Obiechina (9) point out that addressing cultural stigmas is key to successful IEC interventions, especially in conservative settings. This study established that 45% of respondents expressed concerns about spousal blame, highlighting the role of gender dynamics in shaping health-seeking behaviors. Fear of being accused of infidelity or promiscuity often discourages women from accessing cervical cancer screening services. This aligns with the findings of Rosser et al. (6) who emphasize the importance of a community addressing gendered barriers to care, including fear of judgment, in order to increase healthcare access and uptake. World Health Organization and the Centers for Disease Control and Prevention (19) indicate that the development of culturally sensitive and accessible IEC materials is vital for ensuring that women receive accurate information that empowers them to make informed decisions about their health.
Healthcare providers play a crucial role in disseminating health information, particularly for WLHA. As Amsale et al. (18) noted in their study that healthcare professionals are often the primary and most trusted sources of information for patients. This role is pivotal in rural areas where access to information might be limited. McGettigan et al. (20) similarly emphasized that personal contact with healthcare professionals is often more impactful than other forms of media, suggesting that the quality of the interaction between healthcare providers and patients can significantly influence the effectiveness of information delivery. The study found that despite healthcare providers being the preferred source of information, there are still gaps in how cervical cancer information is communicated. Nurses, in particular, were identified as a primary source of information about cervical cancer, a finding consistent with previous research by Kikondu (21) on Esophageal Cancer in Kenyatta National Hospital. This suggests that more personalized and interactive forms of education, such as group discussions and one-on-one consultations with healthcare providers, could be more impactful than passive forms of information dissemination like posters and radio broadcasts. Given that WLHA frequently visit healthcare facilities for HIV-related care, these visits provide an invaluable opportunity to educate patients about cervical cancer screening. However, inadequacy of targeted cervical cancer information in HIV care settings, as indicated by this study, suggests a missed opportunity in leveraging these interactions for preventive education.
Digital platforms, including radio, television, and social media, were increasingly relied upon, particularly by younger participants (18–39 years) and were identified as trusted sources of information. Radio, in particular, emerged as a powerful medium, with findings from this study aligning with Akintayo and Bello (13) assertion that radio is an effective strategy for disseminating health information, particularly in rural areas. However, while 85.5% of participants reported accessing cervical cancer information from radio, many expressed a preference for broadcasts in local languages to enhance comprehension, reflecting the need for culturally sensitive content. This preference is in line with Rimande-Joel and Obiechina (9), who highlighted the importance of tailoring health messages to local languages and cultural contexts to improve their impact. Results also indicate that while radio had broad reach, its content was often insufficient, with 81% of participants describing discussions on cervical cancer as superficial or fear-inducing. Social media was therefore viewed as a double-edged sword, offering accessibility but also serving as a source of misinformation for many as also noted in a study by Kemper et al. (5). Television on the other hand emerged as a significant source of information, particularly for more urban populations. Despite its potential reach, the study suggests that radio and TV broadcasts were often insufficient in terms of content, as they lacked in-depth, action-oriented messaging that could drive behavior change. This finding resonates with studies by Wang et al. (22) and Zhang et al. (23), which highlighted a gap between awareness and actual health behaviors related to cervical cancer. While IEC materials such as radio broadcasts and TV programs can effectively raise awareness, they often fall short of prompting the desired behavioral change, a challenge that was also noted by Saasa-Modise et al. (24).
Posters, though commonly used in healthcare facilities, were found to be inadequate in communicating cervical cancer prevention and screening. The placement and design of these materials were cited as problematic, as they were often not easily visible or understandable to the target population. This reinforces the need for improved design and strategic placement of IEC materials in healthcare settings, as emphasized by Ngigi and Busolo (25), who stressed the importance of visibility and accessibility in maximizing the impact of IEC printed materials. In both the health facilities for instance, posters were the most common form of IEC material, yet their placement and content undermined their effectiveness limiting their visibility and engagement.
The study also explored the association between sociodemographic characteristics and perceptions of the sufficiency of IEC materials. Career and income levels were found to have a significant impact on how participants perceived the adequacy of IEC materials. Those with higher incomes or more specialized careers expressed higher expectations for the quality and depth of information provided. This finding aligns with Ngigi and Busolo (25), who noted that professionals often have greater expectations for information accuracy and relevance compared to non-professionals. The socioeconomic status of an individual influences their ability to access more detailed, high-quality health information, which may shape their perceptions of IEC material sufficiency. It was also established that education level had a borderline significant association with the perceived sufficiency of IEC materials, with more educated individuals being more critical of the clarity and cultural appropriateness of the materials. Kangethe et al. (26) similarly found that individuals with higher education levels are better able to critically appraise the quality of health information. However, in this study, the relatively uniform design of IEC materials, which did not cater to varying educational backgrounds, may have contributed to the lack of strong statistical significance regarding education level. Interestingly, the study found no significant association between age or marital status and perceptions of IEC material sufficiency. This contradicts findings by Ngutu and Nyamongo (3) who suggested that older adults often report lower satisfaction with IEC materials due to accessibility challenges. However, the lack of significant findings for age in this study is consistent with research by Aswathy et al. (15) who argued that functional literacy and the contextual relevance of materials are more important determinants of satisfaction than demographic factors like age and marital status.
A significant finding of this study is the need for integrated IEC materials that address both HIV/AIDS and cervical cancer simultaneously. WLHA are at a higher risk of cervical cancer, and as such, they require tailored information that considers both conditions. The study identified a gap in the available IEC materials, which often failed to address the intersection of these two health issues. This suggests a need for materials that not only raise awareness of cervical cancer but also highlight the additional risks faced by WLHA and the importance of regular screening. Gatumo et al. (27) have similarly emphasized the importance of integrating cervical cancer education into HIV care programs. Given the frequent visits of WLHA to healthcare facilities for HIV related care, these settings present an ideal opportunity for delivering comprehensive health education that addresses both HIV and cervical cancer so as to improve health outcomes for WLHA.
While IEC materials were acknowledged as useful sources of information, there were significant gaps in their design, content, and placement. The findings suggest that these materials often fail to address the unique needs of WLHA, particularly in terms of language, text heaviness, and cultural sensitivity. Stakeholders proposed several improvements to enhance the effectiveness of IEC materials. Key recommendations included using clear illustrations, incorporating culturally relevant graphics, and placing materials in high-traffic areas such as the entrances of healthcare facilities. These suggestions are consistent with Ngigi and Busolo (25), who emphasized the need for culturally sensitive graphics and strategic placement to maximize the impact of printed materials. The dissemination of health information is a crucial aspect of healthcare, particularly when it comes to sensitive topics like cervical cancer.
To address these gaps in cervical cancer IEC materials, it is recommended that a multifaceted and culturally sensitive approach to IEC material development and dissemination is needed. Given the high reliance on healthcare professionals, HIV clinics present a prime opportunity for cervical cancer education. Providers should be equipped with up-to-date knowledge and resources to deliver targeted messages during routine visits. Furthermore, training healthcare providers and community health workers to deliver messages effectively can significantly improve perceived efficacy and encourage proactive health-seeking behavior. Leveraging on mabaraza, religious places and other community forums can help normalize discussions about cervical cancer and engage men and community leaders in supporting women's health. There is also need for collaboration with other local Communities in the development process to ensure materials are culturally relevant and address local needs (28). To enhance Radio campaigns this study recommends scheduling discussions during convenient times and using local stations to improve reach and comprehension. Content should also focus on demystifying screening procedures and addressing common misconceptions. There is also need to revise the existing print IEC materials to have larger font, culture specific graphics and be strategically placed in high-traffic areas. Similarly, digital platforms should be curated to provide accurate, trustworthy information. Time is also ripe to create peer-led support groups which can provide a safe space for women to share experiences, ask questions, and receive encouragement for screening and treatment. To enhance the effectiveness of cervical cancer communication strategies, it is therefore crucial to engage WLHA in the development of IEC materials based on the frequently asked questions within a particular community. Participatory approaches can ensure that the content resonates with the lived experiences of these women, promoting greater engagement and retention of information. These findings therefore underscore the importance of tailoring health communication strategies to local contexts to improve screening uptake, help dispel myths, reduce stigma, and foster informed decision-making regarding cervical cancer prevention, screening, and treatment options.
Past research has extensively explored the role of IEC materials in promoting health literacy and awareness about various diseases, including cancer (10, 28). These studies have primarily focused on high-income countries, leaving a gap in understanding how IEC materials can be adapted and effectively utilized in middle and low-resource settings such as rural Kenya (5). Building on this foundation, the present study seeks to extend these findings by examining the cultural, economic, and social dimensions that shape the development, dissemination, and use of IEC materials for cervical cancer awareness and prevention among WLHA. By doing so, this study aims to refine existing theoretical frameworks of health communication for WLHA to account for context-specific challenges and opportunities. Furthermore, integrating past research findings with data from the current study will provide insights into culturally appropriate and effective IEC strategies, thus advancing both scholarly and practical approaches to cervical cancer education in underserved contexts.
Conclusion and future direction
While the current research provides a foundation for understanding the unique barriers to effective communication in low-resource settings, future studies should explore the longitudinal impacts of IEC interventions on health outcomes, behavior change, and early detection rates. Additionally, further research could investigate the effectiveness of community-based approaches and peer education networks in enhancing the reach and impact of IEC materials. Advances in digital technologies also present opportunities for developing scalable and interactive cervical cancer IEC tools tailored to rural and underserved areas. By integrating these future directions, researchers can contribute to building a more comprehensive and sustainable framework for cervical cancer health communication among WLHA, ultimately informing policy and practice at local and national levels.
In conclusion, while IEC materials play a critical role, their effectiveness is hindered by issues of accessibility, cultural relevance, and quality particularly in rural areas. To overcome these barriers, a comprehensive and inclusive approach that integrates education into existing healthcare services, leverages community forums, enhances media campaigns, and addresses social and structural challenges is needed. Prioritizing the development of culturally relevant and easily understandable educational resources and addressing the perceived gaps in communication efficacy and the sufficiency of cervical cancer IEC materials is vital for improving health outcomes among WLHA in rural Kenya.
Strengths of the study
The study addressed critical health issues affecting a vulnerable population in rural Kenya, where access to healthcare resources may be limited. The inclusion of two distinct sites, Webuye and Mosoriot allowed for comparisons between different geographical, cultural, and healthcare contexts. This enhances the generalizability of findings and provides a broader understanding of cervical cancer information dissemination. Differences in the availability, accessibility, and sufficiency of IEC materials across the two sites offered insights into site-specific challenges and opportunities for improvement. For instance, the study highlighted how certain gaps, such as the lack of posters in Mosoriot, were unique to specific locations.
Conducting the study across different sites reduces the risk of localized biases, thereby increasing the validity and reliability of the findings. By identifying effective cervical cancer IEC materials in rural Kenya this study can serve as a model for other similar settings across the country and in other low-resource contexts globally.
Including WLHA, healthcare providers, and community stakeholders ensured that the study captured varied perspectives on cervical cancer information dissemination. Each group brought unique insights, enriching the understanding of the issue. This also allowed for the identification of systemic and community-level barriers to effective information dissemination, which might have been overlooked if only WLHA were included. The sociodemographic diversity of participants also allowed the study to explore how these factors influence perceptions of IEC materials.
Limitations of the study
The study relied on self-reported data from participants, particularly regarding perceptions and use of IEC materials. This introduces the possibility of recall bias or social desirability bias, where participants may provide answers, they believe are expected rather than their true experiences. Also, stakeholders, such as healthcare providers, may have provided responses influenced by their professional role, potentially overestimating the effectiveness of IEC materials or understating existing challenges.
The study also focused on awareness and perceptions but did not adequately explore how these translated into actual screening behaviors. This creates a gap in understanding the effectiveness of IEC materials in driving behavior change. While digital platforms were noted as key sources of information, the study did not address the disparities in access to digital devices and literacy, potentially excluding significant subgroups.
Discussions about cervical cancer and HIV/AIDS also involve sensitive and stigmatized topics. Participants might have withheld crucial information due to discomfort, despite assurances of confidentiality. Secondly cultural taboos surrounding cervical cancer and HIV/AIDS in Webuye and Mosoriot may hinder open discussions and disclosure of relevant information.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Moi Teaching and Referral Hospital/Moi University-Institutional Research and Ethics Committee. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
SA: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Validation, Visualization, Writing – original draft, Writing – review & editing. EO'O: Conceptualization, Investigation, Methodology, Project administration, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. VN: Conceptualization, Investigation, Methodology, Project administration, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. AM: Conceptualization, Data curation, Formal analysis, Methodology, Software, Validation, Visualization, Writing – original draft, Writing – review & editing. PI: Conceptualization, Supervision, Writing – original draft, Writing – review & editing. BR: Conceptualization, Formal analysis, Funding acquisition, Methodology, Supervision, Visualization, Writing – original draft, Writing – review & editing. PL: Conceptualization, Funding acquisition, Project administration, Supervision, Validation, Visualization, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study received funding from a subrecipient under Indiana's grant from the National Institute of Health (NIH), Grant number: FAIN: U54CA254518 (Grant title: East African Consortium for HPV and Cervical Cancer in Women living with HIV/AIDS. Grant manager: Dr. Patrick Loehrer).
Acknowledgments
We are grateful to everyone who has helped us complete this research project. We would like to recognize the financial support provided by Indiana's grant from the National Institute of Health (NIH) for the U54 mentorship program which made this research possible. Special thanks to Webuye and Mosoriot health facilities for providing access to the participants for this study who in turn sacrificed their time to provide tremendous contributions and rich insights. We are grateful to Sarah and Purity for their help in data collection and to Kapten for the administrative support during the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Nwankwo KC, Aniebue UU, Aguwah EN, Anarado AN, Agunwah, E. Knowledge attitudes and practices of cervical cancer screening among urban and rural Nigerian women: a call for education and mass screening. Eur J Cancer Care. (2011) 20:362–7. doi: 10.1111/j.1365-2354.2009.01175.x
2. Were E, Nyaberi Z, Buziba N. Perceptions of risk and barriers to cervical cancer screening at moi teaching and referral hospital (MTRH), Eldoret, Kenya. Afr Health Sci. (2011) 11:58–64. doi: 10.4314/ahs.v11i1.66735
3. Ngutu M, Nyamongo I. Exploring the barriers to health care and psychosocial challenges in cervical cancer management in Kenya. Int J Womens Health. (2018) 27:791–8. doi: 10.2147/IJWH.S88668
4. Hanisch R, Gustat J, Hagensee ME, Baena A, SalazarJE, Castro MV, et al. Knowledge of Pap screening and human papillomavirus among women attending clinics in Medellin, Colombia. Int J Gynecol Cancer. (2008) 18:1020–6. doi: 10.1111/j.1525-1438.2007.01131.x
5. Kemper EK, McGrath CJ, Eckert OL, Kinuthia J, Sing B, Langat A, et al. Correlates of cervical cancer screening among women living with HIV in Kenya: a cross-sectional study. Int J Gynaecol Obstet. (2022) 156:151–8. doi: 10.1002/ijgo.13690
6. Rosser JI, Njoroge B, Huchko MJ. Knowledge about cervical cancer screening and perception of risk among women attending outpatient clinics in rural Kenya. Int J Gynaecol Obstet. (2015) 128:211–5. doi: 10.1016/j.ijgo.2014.09.006
7. Whitham HK, Hawes SE, Chu H, Oakes JM, Lifson AR, Kiviat NB, et al. Comparison of the natural history of HPV infection and cervical abnormalities among HIV-positive and HIV-negative women in senegal, Africa. Cancer Epidemiol Biomarkers Prev. (2017) 26:886–94. doi: 10.1158/1055-9965.EPI-16-0700
8. Maria NS, Olwit C, Kaggwa MM, Nabirye RC, Ngabirano TD. Cervical cancer screening among HIV-positive women in urban Uganda: a cross-sectional study. BMC Womens Health. (2022) 22:148. doi: 10.1186/s12905-022-01743-9
9. Rimande-Joel R, Obiechina GO. Effects of Information Education and Communication (IEC) -based intervention on knowledge and attitude towards cervical cancer prevention among teachers in Taraba State. Adv Soc Sci Res J. (2020) 7:7421–9. doi: 10.14738/assrj.71.7520
10. Smith MA, Hall M, Lew JB, Canfell K. Potential for HPV vaccination and primary HPV screening to reduce cervical cancer disparities: example from New Zealand. J Vaccine. (2018) 36:6314–24. doi: 10.1016/j.vaccine.2018.08.063
11. World Health Organization. Global Strategy to Accelerate the Elimination of Cervical Cancer as a Public Health Problem. Geneva: Cervical Cancer Elimination Initiative (2020).
12. Bethune GR, Lewis HJ. Let's talk about smear tests: social marketing for the national cervical screening programme. Public Health. (2009) 123(e-supplement):17–22. doi: 10.1016/j.puhe.2009.06.006
13. Akintayo BJ, Bello AA. Creating Awareness on Cervical Cancer Via Radio Broadcasting in Ikenne Local Government. New Media and Mass Communication. (2015). Available online at: https://www.academia.edu/33080764/Creating_Awareness_on_Cervical_Cancer_via_Radio_Broadcasting_i (accessed December 12, 2024).
14. Mungo C, Barker E, Randa M, Ambaka J, Osongo CO. Integration of cervical cancer screening into HIV/AIDS care in low-income countries: a moral imperative. Ecancermed Sci. (2021) 20:1237. doi: 10.3332/ecancer.2021.1237
15. Aswathy S, Quereshi M, Kurian B, Leelamoni K. Cervical cancer screening: Current knowledge and practice among women in a rural population of Kerala, India. Indian J Med Res. (2012) 136:205–10. doi: 10.4103/0971-5851.103139
16. AMPATH Kenya Care Programs. (2021). Available online at: http://www.ampathkenya.org/care-programs (accessed July 13, 2024).
17. FHI & PATH. Information, Education and Communication Materials and Caring for People Living With HIV/AIDS. Family Health International (2004). Avaliable online at: https://media.path.org/documents/CP_vietnam_iec_mat_caring_plwh.pdf (accessed March 19, 2021).
18. Amsale C, Getenet M, Shabbir I, Yemane B. Perceived sufficiency and usefulness of IEC materials and methods related to HIV/AIDS among high school youth in Addis Ababa, Ethiopia Afr J Reprod Health. (2005) 9:66–77. doi: 10.2307/3583161
19. Bravington A, Chen H, Dyson J, Jones L, Dalgliesh C, Amee B, et al. Challenges and opportunities for cervical screening in women over the age of 50 years: qualitative study. Br J Gen Pract. (2021) 2:e873–81. doi: 10.3399/BJGP.2022.0036
20. McGettigan P, Golden J, Fryer J, Chan R, Feely J. Prescribers prefer people: the sources of information used by doctors for prescribing suggest that the medium is more important than the message. Br J Clin Pharmacol. (2001) 51:184–9. doi: 10.1046/j.1365-2125.2001.01332.x
21. Kikondu PM. Esophageal Cancer Awareness Among Patients Attending Out-Patient Clinics at Kenyatta National Hospital. Nairobi: University of Nairobi (2023). Available online at: http://erepository.uonbi.ac.ke/handle/11295/164992 (accessed April 21, 2024).
22. Wang J, Herweijer E, Hu K, Valdimarsdóttir UA, Adami HO, Sparén P, et al. Overall and cervical cancer survival in patients with and without mental disorders JAMA NetwOpen. (2023) 6:e2336213. doi: 10.1001/jamanetworkopen.2023.36213
23. Zhang B, Wang S, Yang X, Chen M, Ren W, Bao Y, et al. Barriers of cervical cancer screening services among Chinese adult females: a national cross-sectional survey based on a large e-commerce platform. BMC Womens Health. (2023) 23:435. doi: 10.1186/s12905-023-02554-2
24. Saasa-Modise ML, Musonda JM, Sikwese-Musonda J, Maseko NJ, Hlophe L, Kubeka G. Cervical cancer screening in women living with HIV attending primary care clinics in a health district, South Africa: a descriptive cross-sectional study. Pan Afr Med J. (2022) 43:32. doi: 10.11604/pamj.2022.43.32.33180
25. Ngigi S, Busolo DN. Behaviour change communication in health promotion: appropriate practices and promising approaches. Int J Innov Res Dev. (2018) 7:83–93. doi: 10.24940/ijird/2018/v7/i9/SEP18027
26. Kangethe JM, Monroe-Wise A, Muiruri PN, Komu JG, Mutai KK, Nzivo MM, et al. Utilization of cervical cancer screening among women living with HIV at Kenya's national referral hospital. South Afr J HIV Med. (2022) 23:1353. doi: 10.4102/sajhivmed.v23i1.1353
27. Gatumo M, Gacheri S, Sayed AR, Scheibe A. Women's knowledge and attitudes related to cervical cancer and cervical cancer screening in Isiolo and Tharaka Nithi Counties, Kenya: a cross-sectional study BMC Cancer. (2018) 18:745. doi: 10.1186/s12885-018-4642-9
Keywords: Information, Education, and Communication (IEC), materials, women with HIV/AIDS (WLHA), cervical cancer, perception
Citation: Adeli SM, Orang'O EO, Naanyu V, Mwangi A, Itsura P, Rosen B and Loehrer P (2025) Common sources, perceived communication efficacy and sufficiency of cervical cancer information, education and communication materials for women with HIV/AIDS in rural Kenya. Front. Cancer Control Soc. 3:1557363. doi: 10.3389/fcacs.2025.1557363
Received: 08 January 2025; Accepted: 19 March 2025;
Published: 01 July 2025.
Edited by:
Christian Von Wagner, University College London, United KingdomReviewed by:
Vinit Nalawade, Duke University Health System, United StatesChandrashekhar Taklikar, All India Institute of Hygiene and Public Health, India
Copyright © 2025 Adeli, Orang'O, Naanyu, Mwangi, Itsura, Rosen and Loehrer. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Adeli Scholastic Musakali, c2Nob2xhc3RpY2FkZWxpQGdtYWlsLmNvbQ==
 Scholastic Musakali Adeli
Scholastic Musakali Adeli Elkanah Omenge Orang'O
Elkanah Omenge Orang'O Violet Naanyu
Violet Naanyu Ann Mwangi
Ann Mwangi Peter Itsura5
Peter Itsura5