- Louisiana State University Health Sciences Center, New Orleans, LA, United States
Sarcina ventriculi is a rare bacterium that has the potential to cause severe disease in the gastric mucosa. According to our search, there are less than 100 prior published case reports. This case discusses a 69-year-old man who presented to the hospital with severe gastric distention noted on CT of the abdomen with intractable nausea and emesis, for which endoscopy was performed and ruled out gastric outlet obstruction, with biopsies resulting as S. ventriculi. This bacterium has previously been reported to cause gastric dysmotility, as well as severe side effects including gastric perforation.
Introduction
Sarcina ventriculi is a rare, Gram-positive anaerobic bacterium with carbohydrate fermentation ability that is commonly found in unwashed vegetables. It was first coined in 1842 by Wilson and Goodsir after isolation from a patient with intractable emesis (1). S. ventriculi has been studied in limited research cases as causing a significant delay in motility with gastric outlet obstruction concerns, gastric ulcerations, gastric erythema, and even documented cases of gastric perforation. It is unknown how this bacterium causes such dysmotility, but it is theorized that it alters the normal muscularis mucosa via carbohydrate fermentation. Notably, this bacterium can survive in extremely low pH environments, such as the gastric acid in the stomach.
As of 2013, only eight cases of this rare bacterium have been published (2). In 2021, it was expressed that only 48 cases of this bacterium have been documented. Prior to the documented cases in humans, this bacterium was isolated from animal intestines and is commonly studied in veterinary medicine as an etiology for gastritis, gastric perforation, and dysmotility (3). Due to the limited number of cases and the many unknowns about the disease course of this bacterium, we present a case of isolated S. ventriculi in a patient with severe gastric dysmotility.
Case report
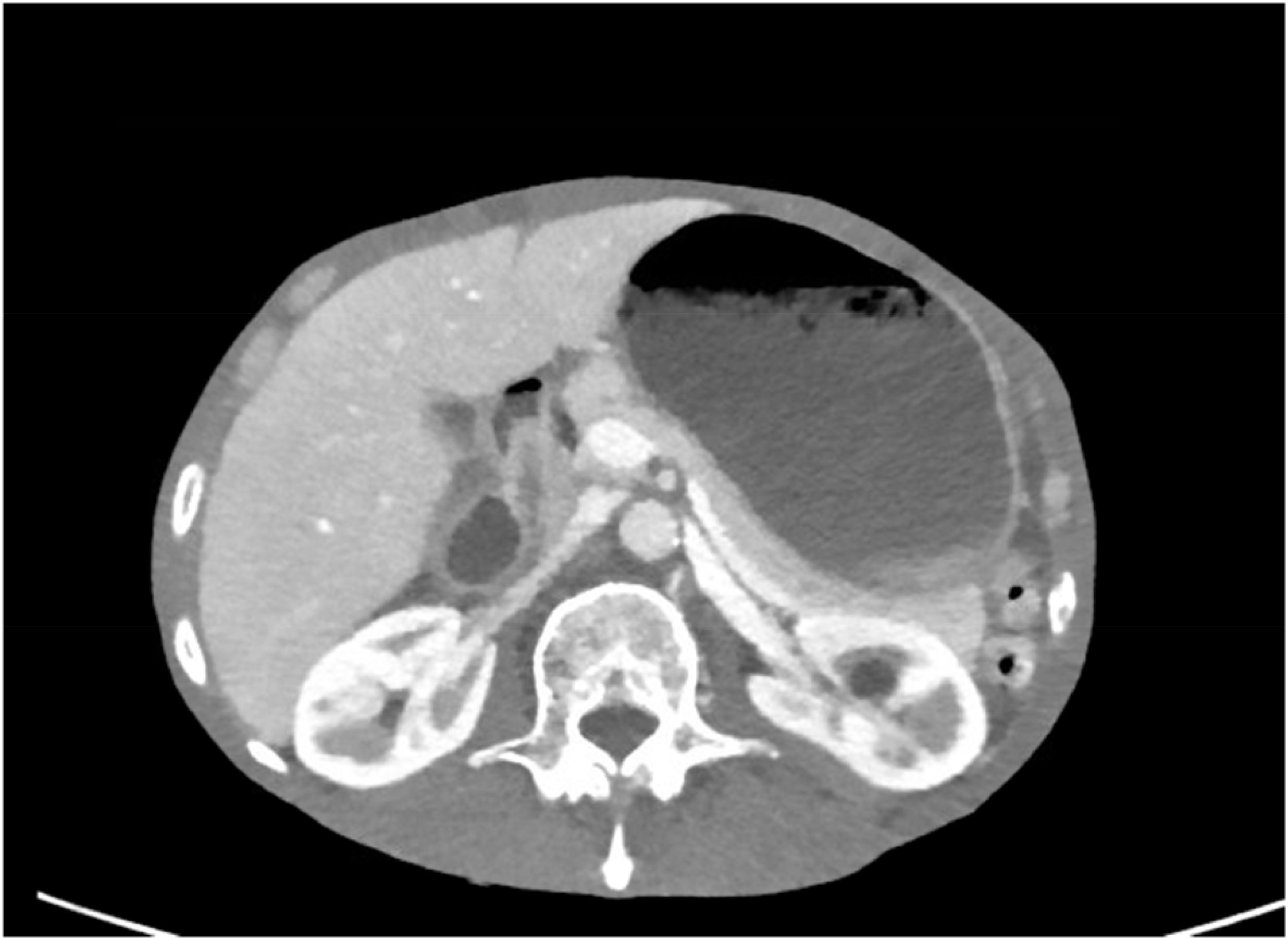
We present a 69-year-old man with grade D esophagitis, hypertension, duodenal angioectasias, chronic obstructive pulmonary disease, pulmonary mass, and recurrent small bowel obstructions who presented to the emergency department (ED) with intractable nausea and bilious vomiting with severe abdominal pain in the epigastric region of 2 day’s duration. CT scan of the abdomen and pelvis was performed, revealing concern for gastric outlet obstruction with severe gastric distention.
At 2 months prior to presentation, the patient was hospitalized for hematemesis. Subsequent esophagogastroduodenoscopy (EGD) revealed grade D esophagitis and erosive gastropathy, which was biopsied with the pathology resulting as rare S. ventriculi. The patient was prescribed outpatient ciprofloxacin for 10 days, with patient-reported completion of therapy without missed doses. He returned after completion of the ciprofloxacin treatment with recurrent nausea with vomiting and abdominal pain.
On the CT scan showing gastric outlet obstruction, there was a significant amount of food noted on the radiographic images (Figures 1, 2), for which a nasogastric tube was placed and intermittent wall suction started. This produced significant output over a span of 3 days, in which his symptoms of nausea and vomiting improved. The EGD performed following nasogastric tube decompression showed food residue and no evidence of gastric outlet obstruction, making dysmotility the most likely etiology. Repeat biopsies were taken during endoscopy, which were negative for S. ventriculi for a second time. Decision to empirically treat with ciprofloxacin plus metronidazole combination therapy was deferred as the pathology was negative on repeat EGD. The patient continued to clinically improve and was able to advance diet without repeat gastric distention.
Discussion
In the limited previously published literature on S. ventriculi, the majority of the documented cases are consistent with similar presentations to our patient with gastric dysmotility, gastric distention, and correlating epigastric pain. After days of nasogastric tube decompression, the patient underwent endoscopy with removal of the residual food content, and gastric outlet obstruction was ruled out. This made the underlying S. ventriculi the likely etiology of the gastric distention and dysmotility. The mechanism by which this bacterium causes the dysmotility is unclear. It is important to note that this patient had no other comorbidities that could have led to this gastric dysmotility, such as gastroparesis or diabetes as a couple of examples. It is also pertinent that he had no offending medications after medication review to cause this presentation or dysmotility, supporting S. ventriculi as the inciting factor for the presentation of this patient.
It is also important to discuss that this patient’s presentation was after completion of a full course of ciprofloxacin with negative repeat biopsy. This was prescribed approximately 2 months prior to hospital presentation, and the patient reported completing the entire course of antibiotic. The utility of empirically retreating with ciprofloxacin plus metronidazole versus no further treatment was discussed with the infectious disease consulting physician during inpatient stay. The final decision was to hold off on therapy and re-biopsy during upcoming endoscopy. A previous documented pediatric case resulted in the complete resolution of infection after ciprofloxacin and metronidazole combination therapy, including repeat negative biopsies (4).
The negative biopsies on repeat EGD could be secondary to the completed course of ciprofloxacin or could be attributed to a false-negative biopsy result. The patient experiencing symptoms of dysmotility for several weeks after biopsy confirmed that the exposure supports the theory of the muscularis layer of the gastric mucosa being targeted as the pathogenesis of S. ventriculi. This could indicate that this bacterium causes lingering effects to the mucosa after the initial infection, or this may support S. ventriculi being more of an incidental bacterium to a secondary process. More studies are needed to support this theory, in particular those on human cases (2). In a study characterizing several cases of this bacterium in animals, the pH tolerance of the bacterium was emphasized, making another theory consistent with the bacterial overgrowth of S. ventriculi causing the correlating symptoms as seen in our case (5).
While this bacterium is becoming more prevalent among humans, this case is relevant to the growing knowledge of isolation, treatment, and course of disease for S. ventriculi. It is particularly important to understand how this bacterium causes severe disease and notably affects the gastric mucosa. This is imperative to understand the clinical course for patients with symptoms secondary to S. ventriculi, as well as for the recurrence of symptoms. More studies are needed to standardize the approach to care for this patient population.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
KC: Investigation, Software, Data curation, Writing – original draft, Funding acquisition, Resources, Conceptualization, Visualization, Validation, Methodology, Supervision, Project administration, Formal analysis. CH: Validation, Writing – review & editing, Funding acquisition, Resources, Supervision, Investigation, Project administration, Visualization, Data curation, Software, Methodology, Conceptualization, Formal analysis.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Goodsir J and Wilson G. History of a case in which a fluid periodically ejected from the stomach contained vegetable organisms of an undescribed form. Edinb Med Surg J. (1842) 57:430–43.
2. Ratuapli SK, Lam-Himlin DM, and Heigh RI. Sarcina ventriculi of the stomach: a case report. World J Gastroenterol. (2013) 19:2282–5. doi: 10.3748/wjg.v19.i14.2282
3. Marcelino LP, Valentini DF, MaChado SMDS, Schaefer PG, Rivero RC, and Osvaldt AB. Sarcina ventriculi a rare pathogen. Autops Case Rep. (2021) 11:e2021337. doi: 10.4322/acr.2021.337
4. Bell HL, Santos R, Varshney N, and Camacho-Gomez S. Sarcina ventriculi of the esophagus and stomach in a pediatric patient with severe gastroparesis. Pediatr Infect Dis J. (2024) 43:e25–6. doi: 10.1097/INF.0000000000004131
Keywords: bacteria, motility, Sarcina, gastroenterology, infectious disease
Citation: Cates KW and Hudson C (2025) Case Report: Sarcina ventriculi, a masquerade of motility. Front. Gastroenterol. 4:1607667. doi: 10.3389/fgstr.2025.1607667
Received: 07 April 2025; Accepted: 27 June 2025;
Published: 05 August 2025.
Edited by:
Fabio Grizzi, Humanitas Research Hospital, ItalyReviewed by:
Abhinav Tiwari, PeaceHealth Sacred Heart Medical Center, United StatesMukesh Kumar Ranjan, Tribhuvan University, Nepal
Copyright © 2025 Cates and Hudson. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Katherine Westbrook Cates, ZHJrYXR3ZXN0YnJvb2tAZ21haWwuY29t
 Katherine Westbrook Cates
Katherine Westbrook Cates Catherine Hudson
Catherine Hudson