- 1Department of Midwifery, School of Health Science, Ambo University Waliso Campus, Waliso, Ethiopia
- 2Department of Midwifery, College of Medicine and Health Science, Ambo University, Ambo, Ethiopia
- 3Department of Paediatric Nursing, College of Medicine and Health Science, Ambo University, Ambo, Ethiopia
- 4School of Medicine, College of Health and Medical Science, Haromaya University, Harar, Ethiopia
- 5Department of Midwifery, College of Medicine and Health Science, MadaWalabu University, Shashamane Campus, Shashamane, Ethiopia
Background: Subfecundity is defined by a time to pregnancy of more than 12 months with unprotected sexual intercourse. Despite many couples experiencing psychological, social, and economic effects as a consequence of subfecundity, it has been inadequately explored in Ethiopia.
Objective: Since there is limited information available in Ethiopia on subfecundity and no further studies have been conducted in the study area, this study will serve as input. Therefore, this study aimed to assess the magnitude of subfecundity and associated factors in Ambo town.
Methods: A cross-sectional study was employed using systematic sampling to select 368 pregnant mothers. Data were collected through face-to-face interviews using a pre-tested structured questionnaire supplemented with a review of medical records. Bivariate and multivariable logistic regression were performed to identify factors associated with subfecundity. The statistical significance was declared using 95% CI, with a p-value <0.05.
Result: A total of 361 mothers (21.3%, 95% CI: 17.20–25.50) were interviewed, resulting in a response rate of 98%. Subfecundity was more likely among mothers aged >35 years (AOR = 3.74, 95% CI: 1.38–10.18), menstrual cycle irregularities (AOR = 3.15, 95% CI: 1.66–5.98), those whose coital frequency was 1 day per week (AOR = 4.77 95% CI: 2.22–10.23), mothers with primigravida (AOR = 2.29, 95% CI: 1.18–4.41), those who used contraceptives (AOR = 1.87, 95% CI: 1.02–3.50), and those who were stressed before conceiving (AOR = 1.95, 95% CI: 1.03–3.70).
Conclusion: This study found that the prevalence of subfecundity was 77% (21.3%, 95% CI: 17.2–25.5), which is slightly higher than previous findings in Ethiopia. Subfecundity was more likely among mothers age >35, those with primigravida, mothers who experienced menstruation irregularities, those whose coital frequency was less than twice per week, mothers using an injectable contraceptive method, and those who were stressed before the current pregnancy. Thus, health professionals should provide information for women at preconception care clinics, sexual and reproductive health clinics, and family planning clinics to those who wish to become pregnant before the age of 35 years to increase the frequency of coital practice, decrease stress, and encourage treatment for menstruation irregularities.
Background
Fecundity is the physiological capacity to have children, which occurs in the span between menarche and menopause in women refers to the physical capability to have a child (1). Fecundability, which is the monthly likelihood of pregnancy, is about 20% among fertile couples. Subfecundity is defined by a time to pregnancy of more than 12 months with unprotected sexual intercourse, i.e., when women have certain physical conditions making it possible but unlikely to conceive (2).
In epidemiological studies, waiting time to pregnancy (WTTP) measures how long a couple takes to conceive and provides an estimation of the likelihood of conceiving a clinically observable pregnancy per cycle, i.e., it is used as a measure of a couple’s fecundity (3–5). Epidemiological studies categorize fecundity status using WTTP (with fecundity within 12 cycles/months and sub-fecundity after 12 months of waiting time to conceive) (6–8). As WTTP increases, the probability of conceiving within one year decreases (9). A prolonged WTTP represents a daily problem for couples (10). Being unable to conceive for a prolonged time can cause friction between couples (11, 12). Waiting for months/years is a risk factor for a breakdown in the relationship, finding another individual to cohabit with, sexually transmitted infections (STIs), separation, dependence, psychological suffering, social stigmatization, hopelessness, worry, negative economic consequence, disrespect from husband and relatives, and neglect by in-laws, t (11).
Globally, from 2009 to 2015, around 60 to 80 million people a year experienced an inability to get a wanted pregnancy (8, 13). As a result, couples are forced to keep up the number of months/years without pregnancy to conceive a baby (13, 14). The average possibility of pregnancy after one year (subfecundity) is around 85%. In Europe, a waiting time for pregnancy greater than 12 months ranges from 10.4% to 17.58% (15, 16). The 2016 South African report of subfecundity found it to be 22% (17). The 2017 demographic and health review report of low- to middle-income countries indicated that subfecundity was 31.1% (13). In 2018 and 2020, studies conducted in Addis Ababa and Arba Minch indicated that a waiting time for pregnancy of about 12 months was 18.3% and 17.8%, respectively (6, 18).
Identifying subfecundity its and associated factors is important for individuals and health care providers to provide information and enhance awareness on the prevention and treatment of subfecundity, as well as coping strategies (16). According to some evidence, there are many different factors that may be associated with subfecundity. Socio-demographic factors such as the age of the couple are related to WTTP (19, 20). Reproductive health-related factors are also linked, for example, abortion is associated with the subjective time to conceive (21). The irregularity of the menstrual cycle and the use of injectable contraceptive methods before pregnancy are also factors associated with subfecundity (22). Substance use, such as smoking cigarettes, is related to increased waiting time to conceive (23, 24). Alcohol, chewing, and coffee drinking are also identified as factors related to subfecundity (6, 25). Lifestyle, exercise, psychological stress, and environmental pollutants are factors related to subfecundity (26).
Despite allocating resources for women, especially during pregnancy and lactation, such as advising on prevention and treatment in line with reproductive health and childbearing and counselling reproductive-age women to prevent factors causing delayed time to conceive before starting assisted reproductive technology (ART), subfecundity is still a major health problem for couples (27). Thus, in this study, we aimed to assess the magnitude of subfecundity by using WTTP and intended to address variables that are associated with subfecundity like stress, physical activity, and exposure to environmental and occupational chemicals and pollutants, and provide more information and awareness about subfecundity to overcome its prevalence among mothers receiving antenatal care in Ambo town public health facilities.
Methods
Study settings
Ambo, which was established in 1889 and is located 114 km to the west of the capital Addis Ababa, is one of the towns in central Ethiopia. According to the Ambo Town Health Administration office in 2014, the total population of the town is 97,317, of which 49,602 are males and 47,715 are females. Among those females, 10,974 are in the reproductive age group and 395 of them are pregnant. In the town, there is one referral hospital, one general hospital, two health centers, and 21 medium private clinics. The study was conducted in Ambo town, from 1st August to September 30 of 2022.
Study design and population
A facility-based cross-sectional study design was conducted. All pregnant mothers who had attended an antenatal care (ANC) service at Ambo town public health facilities were the source population, while pregnant mothers who had attended an ANC service at Ambo town public health facilities during the study period were the study population. All randomly selected pregnant mothers during the study period were the study units.
Inclusion criteria
All pregnant mothers who had attended ANC services were included in the study.
Exclusion criteria
Pregnant mothers with any medically assisted reproduction technology including Assisted Reproductive Therapy, those who were seriously ill, and those who had mental problems were excluded from the study.
Sample size determination and sampling techniques
The sample size for the first objective was determined by using a single population proportion formula using the proportion of subfecundity from the study conducted in Arba Minch, which was 17.8% (P = proportion of subfecundity = 0.178, Z(1 − α/2) = critical value for 95% confidence level, which equals to 1.96, with a 10% non-response rate, meaning the final sample size was 248) (18). Also, the sample size was calculated for factors associated with subfecundity using Epi-Info version 7.2.4.0 Stat Calc. computer software using assumptions like power 80%, confidence interval 95%, and percent of cases among exposed and unexposed individuals. Ultimately, the sample size calculated from the partner's age before the pregnancy was larger than the sample size for the first objective and taken as the final sample size of the study, which is 368 pregnant women with a 10% nonresponse rate. Last year, booked appointments in August and September for ANC in Ambo University Referral Hospital, Ambo General Hospital, Ambo Health Centre, and Awaro Health Centre were 351, 242, 235, and 204, respectively, and the total number of booked ANC appointments of all public health facilities was 1,032. So, the required sample size for each facility was allocated proportionally to all facilities based on their monthly booked ANC report figures by using the following formulas
Where SS is sample size.
Therefore, the sample size for Ambo University Referral Hospital = 351 × 368/1,032 per month = 125, for Ambo General Hospital = 242 × 368/1,032 per month = 86, for Ambo Health Centre was 235 × 368/1,032 = 84 and for Awaro Health Centre was 204 × 368/1,032 = 73. Participants were chosen from each facility according to the above sample size.
Finally, the required number (n = 368) of participants were selected using a systematic random sampling technique by using an interval (Kth) calculated from the monthly follow-up of pregnant mothers divided by the number of allocated samples to the health facilities. The first study unit was selected randomly, and then every third interval was selected for face-to-face interviews and assisted questionnaires when leaving the ANC.
Data collection
Data were collected through interviews of eligible participants using a structured questionnaire and supplemented with a review of their medical records, which was adapted by reviewing different literature of the same purpose (18, 26, 28). The tool consisted of five parts: sociodemographic characteristics of the mother, sexual and reproductive health, substance use, medical problems, and lifestyle characteristics. Data were collected by four BSc midwives and supervised by two MSc midwives in maternity nursing and reproductive health who received training on data collection and were fluent in the local language.
To ensure the quality of data, properly designed data collection instruments were prepared. Firstly, the tool was prepared in English and translated into the Afan Oromo language by a language expert and translated back to English to certify the consistency of meaning. Before data collection, pre-testing was conducted in a 5% population among pregnant mothers attending ANC services at Guder Health Center. On-site daily supervision was carried out throughout the data collection period.
Variables of the study and measurement
The dependent variable of the study, subfecundity, was measured as fecundity status; it was categorized “Yes” if fecund, “No” if not, and coded “1” and “0” respectively. Those categorized as “No” were considered as subfecund and re-coded “1”; while those categorized as “Yes” were considered as non-subfecund and re-coded “0”. The independent variables included socio-demographic conditions (age, marital status, education, mother's working hours, occupation, family income, and duration of cohabiting), reproductive health-related conditions (parity, abortion before the current pregnancy, frequency of sexual intercourse before the current pregnancy, menstrual pattern before the current pregnancy, and type of contraceptive used before the current pregnancy), substance-use-related factors before the current pregnancy (coffee intake, smoking cigarettes, alcohol drinking, and khat chewing), lifestyle factors before the current pregnancy (exercise, psychological stress, and environmental pollutants), and medical-related conditions before the current pregnancy (HIV and Diabetes mellitus).
Operational definitions
Waiting time to pregnancy (WTTP): the number of months or years that a couple waits to conceive a pregnancy by performing unprotected sexual intercourse and excluding the months of sexual abstinence due to illness, distance due to work, or other causes. In this study, WTTP was used to identify the fecundity status of a mother with naturally planned conception and was dichotomized as “Subfecundity” (WTTP greater than 12 months) and “Fecundity” (WTTP for 12 and below months) (29, 30).
Fecundity status: the physiological capacity to have children, which occurs in the period between menarche and menopause in women (1, 31).
Natural Conception: Pregnancy without Assisted Reproductive Technology (ART).
Statistical analysis
All collected data were cross-checked for completeness and consistency, coded, double-entered to Epi-Data 3.1, and exported to SPSS 26 for analysis. Descriptive statistics, binary, and multivariable logistic regression analysis were used to identify associated factors. Variables having a P-value <0.25 in the bivariable logistic regression analysis were selected for the multivariable logistic regression model for adjustment of confounding effect between independent variables and in order not to miss important variables. Multicollinearity was checked using variance inflation factor (VIF) or the tolerance test, and no multicollinearity was detected. Model fitness was also checked using Hosmer-Lemeshow tests, and the model was well-fitted. Association was described using an adjusted Odds Ratio (AOR) along with a 95% confidence interval (CI). Finally, p−<0.05 in the multivariable analysis was considered as a cut-off point for a statistically significant association.
Results
Characteristics of study participants
In this study, of a total of 368 approached mothers, 361 (98%) participated. The mean age of respondents was 26 ± 5.486 years. The majority of the respondent mothers were married 348 (96.4%). Of the mothers, 165 (45.7%) attended college or above. Eighty-eight (24.4%) of respondents were government employees (Table 1).
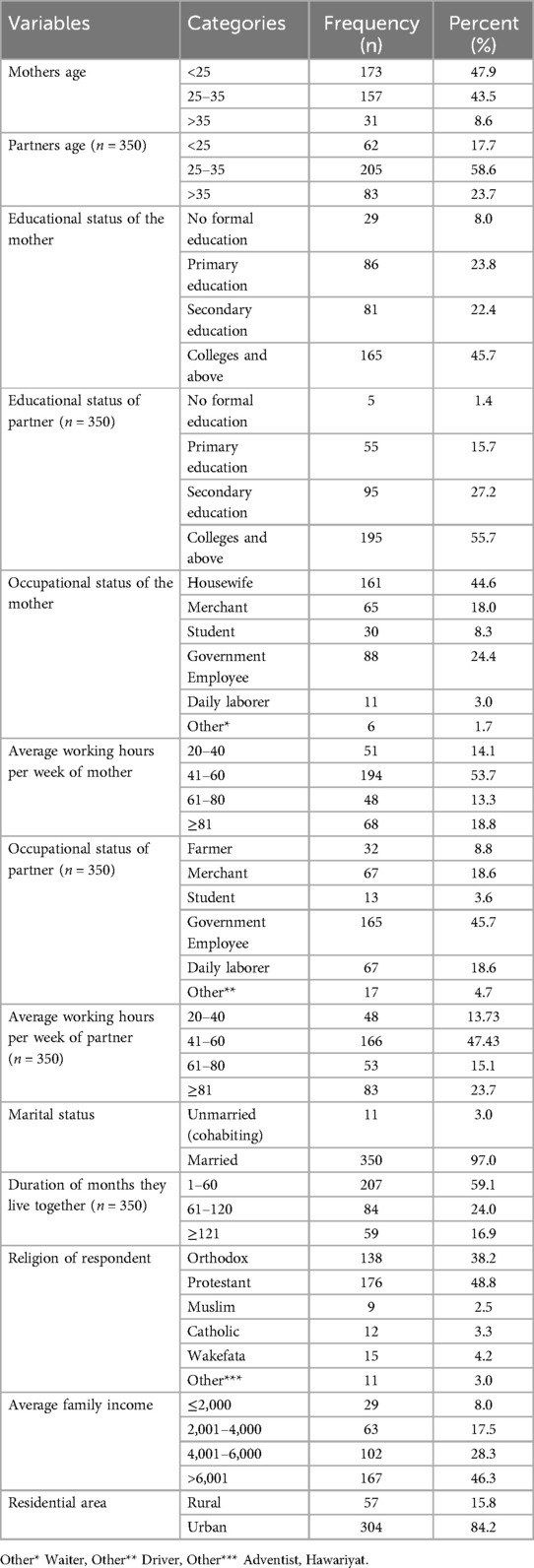
Table 1. Sociodemographic characteristics of pregnant mothers attending antenatal care services in public health facilities of Ambo town, Oromia region, Ethiopia (n = 361).
Among the respondents, almost half, 165 (45.7%), were in the second trimester, and 186 (51.5%) were primigravida. About 86 (23.8%) of mothers had a coital frequency of one day per week (Table 2).
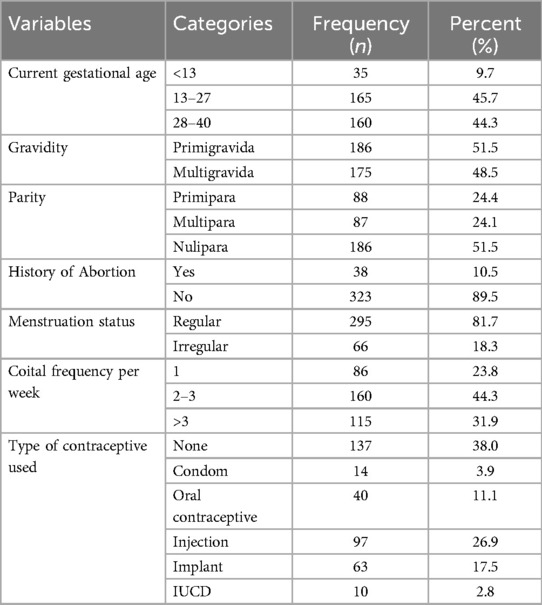
Table 2. Reproductive health-related characteristics of pregnant mothers attending antenatal care services in public health facilities of Ambo town, Oromia region, Ethiopia (n = 361).
Among the respondents, 192 (53.2%) drank four cups of coffee or more per day. 122 (33.8%) mothers had a history of drinking alcohol before the current pregnancy. 16 (4.4%) of the mothers’ partners had a history of smoking cigarettes every day before the current pregnancy (Table 3).
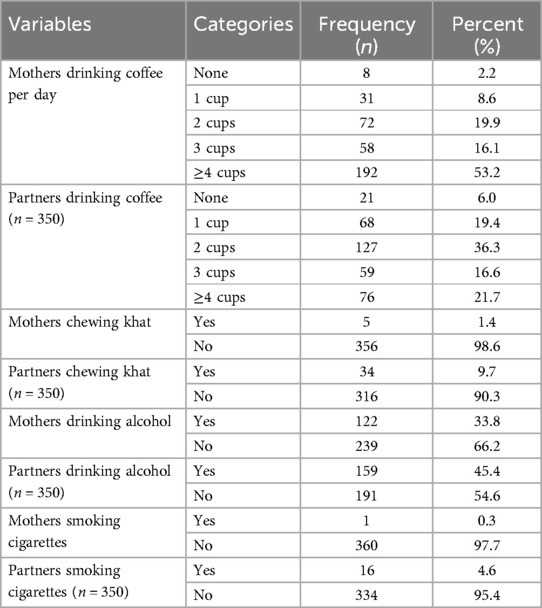
Table 3. Substance-use-related characteristics of pregnant mothers attending antenatal care services in public health facilities of Ambo town, Oromia region, Ethiopia (n = 361).
The majority of respondents 340 (94.2%) knew their HIV status before the current pregnancy. Of the total respondents, 242 (67%) performed exercise during their daily activities. About 20.3% of respondent mothers were exposed to some environmental and occupational chemicals and pollutants (Table 4).
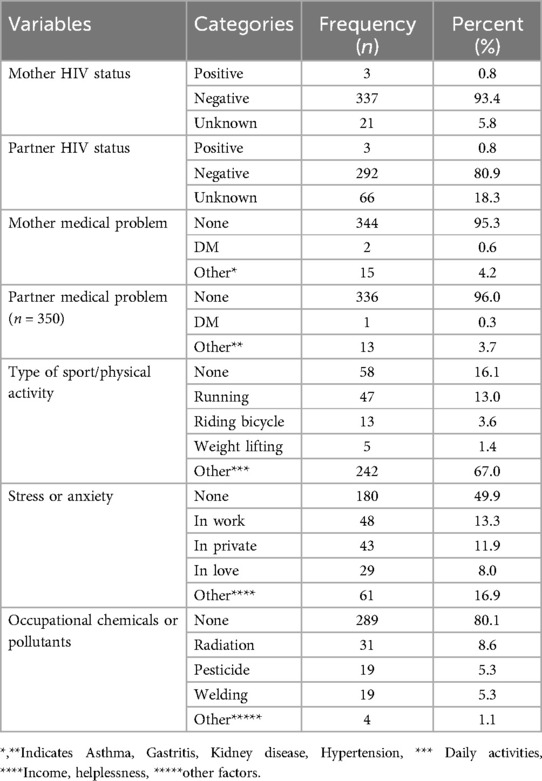
Table 4. Medical and lifestyle characteristics of pregnant mothers attending antenatal care services in public health facilities of Ambo town, Oromia region, Ethiopia (n = 361).
Magnitude of subfecundity
In this study, the magnitude of subfecundity among pregnant mothers attending antenatal care services at Ambo town public health facilities was 77% (21.3%, 95% CI: 17.2–25.5) (Figure 1).
Figure 1. Magnitude of subfecundity among pregnant mothers attending antenatal care services in public health facilities of Ambo town, Oromia region, Ethiopia, 2021.
Factors associated with subfecundity
Before and after an adjustment was made, mother's age >35, menstruation irregularities, coital frequency per week, using an injectable contraceptive method, the first pregnancy, and mothers’ stress before the current pregnancy were significantly associated factors with subfecundity. The odds of subfecundity among mothers found in the age category of >35 years before the current pregnancy were 3.7 times (AOR = 3.74, 95% CI: 1.38–10.18) compared to mothers in the age category of <25 years. Mothers who had irregular menses before the current pregnancy were three times (AOR = 3.15, 95% CI: 1.66–5.98) more likely to be subfecund than mothers who had regular menses. The likelihood of subfecundity was increased by two times (AOR = 2.28, 95% CI: 1.18–4.41) among mothers becoming pregnant for the first time than mothers who had other children. Mothers with a coital frequency of once per week before the current pregnancy were 4.8 times (AOR = 4.77, 95% CI: 2.22–10.23) more likely to be subfecund than mothers who practiced greater than three times per week. Mothers who used an injectable contraceptive were nearly two times (AOR = 1.87, 95% CI: 1.02–3.50) more likely to be subfecund than those who did not use an injectable contraceptive. Mothers who were stressed were almost two times (AOR = 1.95, 95% CI: 1.03–3.70) more likely to be subfecund than those who had no stress (Table 5).
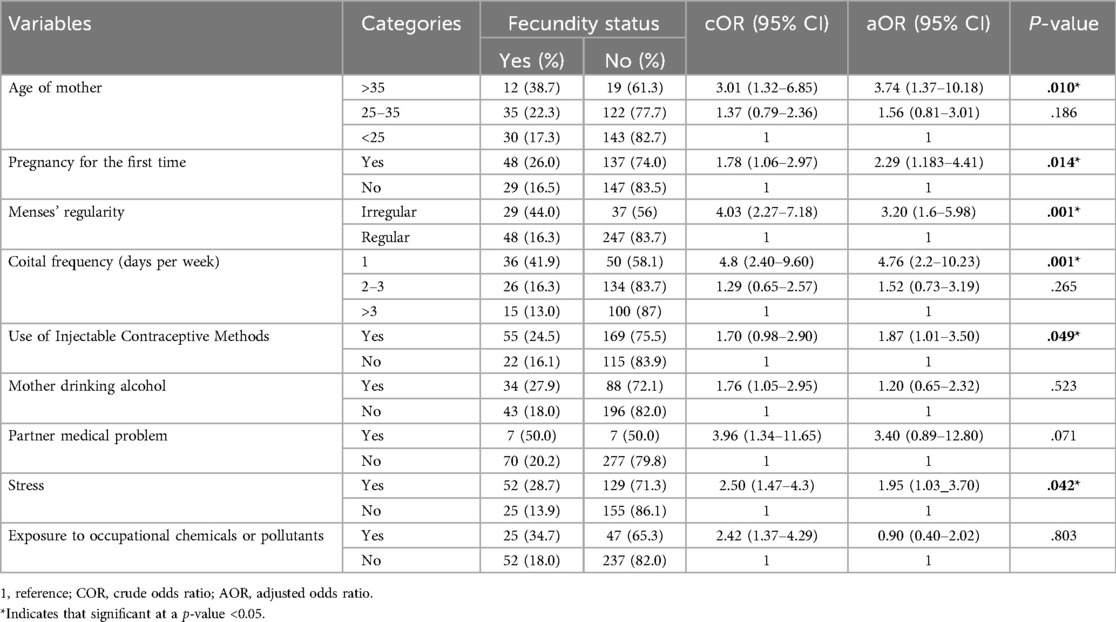
Table 5. Factors associated with Subfecundity among pregnant mothers attending antenatal care services in public health facilities of Ambo town, Oromia region, Ethiopia (n = 361).
Discussion
In this study, we assessed the prevalence of subfecundity and associated factors among pregnant mothers attending antenatal care services at Ambo town public health facilities. We found that the overall magnitude of sub-fecundity was 21.3% 95 CI: (17.20–25.50%). Our finding is a little higher than studies conducted in Addis Ababa (18.3%) and Arba Minch (17.8%) and a little lower than studies conducted in South Africa (22%) (7, 17, 18). A possible reason might be variations in the study population and the socioeconomic status of the population. The finding of subfecundity reported in this study is higher than the studies conducted in European regions (16.1%), Palestine (13.4%), and Germany (10.4%) (8, 32, 33). A possible reason might be variations in the study population, socioeconomic status, and health policy of the country. Also, the finding of subfecundity reported in this study is lower than a multicenter study of Asian countries (45%) (34). A possible reason for this might be a variation in the socioeconomic status of the study population.
In this study, subfecundity was found to be more likely among women who were aged >35, had menstruation irregularities, had low coital frequency per week, used an injectable contraceptive method, had their first pregnancy, and experienced stress before the current pregnancy. In line with several other studies, subfecundity was more likely among mothers aged >35 years before the pregnancy (7, 14, 22, 35, 36). A possible reason might be that, as age advances, the ovarian reserve and oocyte quality and quantity decline (37). The occurrences of subfecundity were more likely to increase among mothers becoming pregnant for the first time than among mothers who had experienced pregnancy. A possible reason may be a psychosocial adaptation to pregnancy and motherhood experiences for multigravida women. Consistent with other studies, women who had previously used injectable contraceptive methods had a significantly lower probability of conceiving early compared with women who did not use them (38). This might be due to the use of injectable contraceptive methods that may delay or prolong the return of the menstruation cycle and the effect of contraceptive use potentially compromising ovarian function.
In line with other studies, mothers who had sexual intercourse once per week were more likely to be subfecund than mothers who practiced sexual intercourse ≥3 days per week (18, 38). A possible explanation for this might be that when the timeof ovulation is mismatched with the time of sexual intercourse per week, couples might be unsure over the appropriate time to conceive. Consistent with prior studies, mothers who had irregular menstruation were also more likely to be subfecund (8, 10, 36, 38, 39). A possible reason may be due to ovulation day. When menstruation day is irregular, it is difficult to determine the day on which ovulation will occur, and the ability to get pregnant decreases.
In addition, mothers feeling stressed were more likely to be subfecund. This finding is in line with a prior study conducted in Cleveland, USA (40). It may be because stress can decrease libido, resulting in the couples having less frequent intercourse.
Strengths and limitations of the study
A strength of this study is that social desirability bias might be reduced since data were collected by health professionals and the client and healthcare providers have trust in each other due to confidentiality. In addition, the use of medical record reviews might reduce response bias that might have otherwise occurred when the women were asked to respond to their HIV status. However, our study also has some limitations. First, since we limited our study to only public health facilities, private hospitals and clinics that gave delivery services were not included. Second, recall bias might have occurred when mothers were asked to recall their time to pregnancy, and this study was limited to subfecundity/subfertility, excluding the infertile women population.
Conclusion
In this study, we found that the prevalence of subfecundity in the study area is high compared to the previous study. Consistent with the previous studies, subfecundity is more likely among mothers >35 years, mothers with menstruation irregularities, mothers engaging in sexual activity once per week, mothers experiencing stress, and those using an injectable contraceptive method. In addition, mothers who became pregnant for the first time were more likely to develop subfecundity. There is a need to improve women's awareness to plan pregnancy before the age of 35 years, increase the frequency of coital practice, decrease stress, and get treatment for menstruation irregularities to reduce sub-fecundity.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Institutional Review Board of Ambo University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
EA: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. GA: Conceptualization, Investigation, Methodology, Software, Supervision, Writing – original draft, Writing – review & editing. GG: Conceptualization, Data curation, Investigation, Methodology, Software, Supervision, Writing – original draft, Writing – review & editing. MA: Formal analysis, Methodology, Visualization, Writing – original draft, Writing – review & editing. MS: Conceptualization, Data curation, Writing – original draft, Writing – review & editing. JB: Data curation, Methodology, Supervision, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We would like to thank the administrators of the public health facilities for facilitating the study in their respective health facilities, the study participants, and the data collectors.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/journals/global-womens-health/articles/10.3389/fgwh.2025.1506481/full#supplementary-material
References
1. Leridon H. Studies of fertility and fecundity: comparative approaches from demography and epidemiology. C R Biol. (2007) 330:339–46. doi: 10.1016/j.crvi.2007.02.013
2. Ramlau-Hansen CH, Thulstrup AM, Nohr E, Bonde JP, Sørensen T, Olsen J. Subfecundity in overweight and obese couples. Hum Reprod. (2007) 22:1634–7. doi: 10.1093/humrep/dem035
3. Nohr E, Vaeth M, Rasmussen S, Ramlau-Hansen C, Olsen J. Waiting time to pregnancy according to maternal birthweight and prepregnancy BMI. Hum Reprod. (2009) 24:226–32. doi: 10.1093/humrep/den357
4. Habbema JDF, Collins J, Leridon H, Evers JL, Lunenfeld B, teVelde ER. Towards less confusing terminology in reproductive medicine: a proposal. Hum Reprod. (2004) 19:1497–501. doi: 10.1093/humrep/deh303
5. Bretveld R, Zielhuis GA, Roeleveld N. Time to pregnancy among female greenhouse workers. Scand J Work Environ Health. (2006) 32:359–67. doi: 10.5271/sjweh.1031
6. Sozou P, Hartshorne G. Time to pregnancy: a computational method for using the duration of non-conception for predicting. PLoS One 7(10):e46544. doi: 10.1371/journal.pone.0046544
7. Kassa EM, Kebede E. Time-to-pregnancy and associated factors among couples with natural planned conception in Addis Ababa, Ethiopia. Afr J Reprod Health. (2018) 22:33–42. doi: 10.29063/ajrh2018/v22i3.4
8. Issa Y, Sallmen M, Nijem K, Bjertness E, Kristensen P. Fecundability among newly married couples in agricultural villages in palestine: a prospective study. Hum Reprod. (2010) 25:2132–8. doi: 10.1093/humrep/deq133
9. Eisenberg ML, Sundaram R, Maisog J, Buck Louis GM. Diabetes, medical comorbidities, and couple fecundity. Hum Reprod. (2016) 31:2369–76. doi: 10.1093/humrep/dew200
10. Hörbst V. “You cannot do IVF in Africa as in Europe”: the making of IVF in Mali and Uganda. Reprod Biomed Soc Online. (2016) 2:108–15. doi: 10.1016/j.rbms.2016.07.003
11. Thoma ME, McLain AC, Louis JF, King RB, Trumble AC, Sundaram R, et al. Prevalence of infertility in the United States as estimated by the current duration approach and a traditional constructed approach. Fertil Steril. (2013) 99:1324–31. doi: 10.1016/j.fertnstert.2012.11.037
12. Mascarenhas MN, Flaxman SR, Boerma T, Vanderpoel S, Stevens GA. National, regional, and global trends in infertility prevalence since 1990: a systematic analysis of 277 health surveys. PLoS Med. (2012) 9:e1001356. doi: 10.1371/journal.pmed.1001356
13. Rothman KJ, Wise LA, Sørensen HT, Riis AH, Mikkelsen EM, Hatch EE. Volitional determinants and age-related decline in fecundability: a general population prospective cohort study in Denmark. Fertil Steril. (2013) 99:1958–64. doi: 10.1016/j.fertnstert.2013.02.040
14. Polis CB, Cox CM, Tunçalp Ö, McLain AC, Thoma ME. Estimating infertility prevalence in low-to-middle-income countries: an application of a current duration approach to demographic and health survey data. Hum Reprod. (2017) 32:1064–74. doi: 10.1093/humrep/dex025
15. Cabrera-León A, Lopez-Villaverde V, Rueda M, Moya-Garrido M. Calibrated prevalence of infertility in 30-to 49-year-old women according to different approaches: a cross-sectional population-based study. Hum Reprod. (2015) 30:2677–85. doi: 10.1093/humrep/dev226
16. Kaandorp S, Van Mens T, Middeldorp S, Hutten BA, Hof MHP, van der Post JAM, et al. Time to conception and time to live birth in women with unexplained recurrent miscarriages. Hum Reprod. (2014) 29:1146–52. doi: 10.1093/humrep/deu052
17. Bello B, Kielkowski D, Heederik D, Wilson K. Time-to-pregnancy and pregnancy outcomes in a South African population. BMC Public Health. (2010) 10:1–8. doi: 10.1186/1471-2458-10-565
18. Feyisa JW, Hebo SH, Negash FG, Sidamo NB, Gergiso KT, Shimbre MS, et al. Sub-fecundity and associated factors among mothers with natural planned conception attending antenatal care service in Arba Minch health facilities. PLoS One. (2020) 15:e0241995. doi: 10.1371/journal.pone.0241995
19. Van Geloven N, Van der Veen F, Bossuyt P, Hompes P, Zwinderman A, Mol B. Can we distinguish between infertility and subfertility when predicting natural conception in couples with an unfulfilled child wish? Hum Reprod. (2013) 28:658–65. doi: 10.1093/humrep/des428
20. Fritz R, Jindal S. Reproductive aging and elective fertility preservation. J Ovarian Res. (2018) 11:1–8. doi: 10.1186/s13048-018-0438-4
21. Sapra K, McLain A, Maisog J, Sundaram R, Buck Louis G. Successive time to pregnancy among women experiencing pregnancy loss. Hum Reprod. (2014) 29:2553–9. doi: 10.1093/humrep/deu216
22. Mutsaerts M, Groen H, Huiting H, Kuchenbecker WKH, Sauer PJJ, Land JA, et al. The influence of maternal and paternal factors on time to pregnancy—a Dutch population-based birth-cohort study: the GECKO Drenthe study. Hum Reprod. (2012) 27:583–93. doi: 10.1093/humrep/der429
23. Shrestha A, Nohr EA, Bech BH, Ramlau-Hansen CH, Olsen J. Smoking and alcohol use during pregnancy and age of menarche in daughters. Hum Reprod. (2011):26:259–65. doi: 10.1093/humrep/deq316
24. Sapra KJ, Barr DB, Maisog JM, Sundaram R, Buck Louis GM. Time-to-pregnancy associated with couples’ use of tobacco products. Nicotine Tob Res. (2016) 18:2154–61. doi: 10.1093/ntr/ntw132
25. Jensen TK, Hjollund NHI, Henriksen TB, Scheike T, Kolstad H, Giwercman A, et al. Does moderate alcohol consumption affect fertility? Follow-up study among couples planning first pregnancy. Br Med J. (1998) 317:505–10. doi: 10.1136/bmj.317.7157.505
26. Palomba S, Daolio J, Romeo S, Battaglia FA, Marci R, La Sala GB. Lifestyle and fertility: the influence of stress and quality of life on female fertility. Reprod Biol Endocrinol. (2018) 16:1–11. doi: 10.1186/s12958-018-0434-y
27. Bhasin S. Approach to the infertile man. J Clin Endocrinol Metab. (2007) 92:1995–2004. doi: 10.1210/jc.2007-0634
28. Gudmundsdottir S, Flanders W, Augestad L. Physical activity and fertility in women: the North-Trøndelag health study. Hum Reprod. (2009) 24:3196–204. doi: 10.1093/humrep/dep337
29. Zegers-Hochschild F, Adamson GD, De Mouzon J, Ishihara O, Mansour R, Nygren K, et al. The international committee for monitoring assisted reproductive technology (ICMART) and the World Health Organization (WHO) revised the glossary on ART terminology, in 2009. Hum Reprod. (2009) 24:2683–7. doi: 10.1093/humrep/dep343
30. Greil AL, McQuillan J. Help-seeking patterns among subfund women. J Reprod Infant Psychol. (2004) 22:305–19. doi: 10.1080/02646830412331298332
31. Massarotti C, Gentile G, Ferreccio C, Scaruffi P, Remorgida V, Anserini P. Impact of infertility and infertility treatments on quality of life and levels of anxiety and depression in women undergoing in vitro fertilization. Gynecol Endocrinol. (2019) 35:485–9. doi: 10.1080/09513590.2018.1540575
32. Gnoth C, Godehardt D, Godehardt E, Frank-Herrmann P, Freundl G. Time to pregnancy: results of the German prospective study and impact on the management of infertility. Hum Reprod. (2003) 18:1959–66. doi: 10.1093/humrep/deg366
33. Tuntiseranee P, Olsen J, Chongsuvivatwong V, Limbutara S. Fecundity in Thai and European regions: results based on waiting time to pregnancy. Hum Reprod. (1998) 13:471–7. doi: 10.1093/humrep/13.2.471
34. Gemmill A. Perceived subfecundity and contraceptive use among young adult US women. Perspect Sex Reprod Health. (2018) 50:119–27. doi: 10.1363/psrh.12072
35. Axmon A, Rylander L, Albin M, Hagmar L. Factors affecting time to pregnancy. Hum Reprod. (2006) 21:1279–84. doi: 10.1093/humrep/dei469
36. Stanford JB, White GL Jr, Hatasaka H. Timing intercourse to achieve pregnancy: current evidence. Obstet Gynecol. (2002) 100:1333–41. doi: 10.1016/s0029-7844(02)02382-7
37. Ubaldi FM, Cimadomo D, Vaiarelli A, Fabozzi G, Venturella R, Maggiulli R, et al. Advanced maternal age in IVF: still a challenge? The present and the future of its treatment. Front Endocrinol. (2019) 10:94. doi: 10.3389/fendo.2019.00094
38. Hassan M, Killick S. Is previous use of hormonal contraception associated with a detrimental effect on subsequent fecundity? Hum Reprod. (2004) 19:344–51. doi: 10.1093/humrep/deh058
39. Bradley D, Landau E, Jesani N, Mowry B, Chui K, Baron A, et al. Time to conception and the menstrual cycle: an observational study of fertility app users who conceived. Hum Fertil. (2021) 24:267–75. doi: 10.1080/14647273.2019.1613680
Keywords: sub-fecundity, waiting time to pregnancy, public health facilities, Ambo, Ethiopia
Citation: Andesha E, Abdissa G, Ganfure G, Adugna M, Sheleme M and Bedane J (2025) Subfecundity and associated factors among pregnant mothers receiving antenatal care at public health facilities in Ambo town Oromia region, Ethiopia: a cross-sectional study. Front. Glob. Women's Health 6:1506481. doi: 10.3389/fgwh.2025.1506481
Received: 3 November 2024; Accepted: 18 June 2025;
Published: 10 July 2025.
Edited by:
Dorota Formanowicz, Poznan University of Medical Sciences, PolandReviewed by:
Mohammad Hossein Delshad, Tarbiat Modares University, IranAnthony K. Dah, University of Health and Allied Sciences, Ghana
Anjani Kumar Srivastava, United Group of Institutions, India
Copyright: © 2025 Andesha, Abdissa, Ganfure, Adugna, Sheleme and Bedane. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Elias Andesha, ZWxpYXNhYmFkYW1hMjUwQGdtYWlsLmNvbQ==
†ORCID:
Elias Andesha
orcid.org/0009-0001-8959-7557
Gizachew Abdissa
orcid.org/0000-0003-4390-1418
Melese Adugna
orcid.org/0000-0001-7728-2980
 Elias Andesha
Elias Andesha Gizachew Abdissa
Gizachew Abdissa Gemechu Ganfure
Gemechu Ganfure Melese Adugna1,†
Melese Adugna1,†