Abstract
Background: There is limited evidence on the relationship between social isolation and renal outcomes. To address this gap, this study estimated the prospective relationship of social isolation with rapid kidney function decline and the development of chronic kidney disease (CKD) in middle-aged and elderly Chinese with normal kidney function.
Methods: We analyzed data from 3,031 participants aged ≥ 45 years with baseline estimated glomerular filtration rates (eGFR) ≥ 60 ml/min/1.73 m2. All data were obtained from the 2011 and 2015 waves of the Chinese Longitudinal Study of Health and Retirement (CHARLS). eGFR was estimated based on a combination of serum creatinine and cystatin C. The primary outcome was rapid decline in renal function, as defined by an eGFR decrease of > 5 ml/min/1.73 m2 per year, while the secondary outcome was the development of CKD, as defined by an eGFR decrease to a level < 60 ml/min/1.73 m2.
Results: During the follow-up of 4 years, 258 (8.5%) participants experienced a rapid decline in renal function, while 87 (2.9%) developed CKD. In the fully adjusted model, high social isolation was significantly related to an increased risk of experiencing a rapid decline in renal function (OR 1.805, 95% CI 1.310–2.487) and CKD onset (OR 1.842, 95% CI 1.084–3.129). Among the five components of social isolation, being unmarried, not participating in social activities, and living alone independently predicted declined renal function.
Conclusions: Social isolation is significantly associated with the risk of rapid eGFR decline and CKD onset in middle-aged and older adults with normal kidney function in China.
Introduction
The social networks are composed of various interactive relationships between individuals and organizations. These relationships facilitate the establishment of self-cognition and enable social support. However, older adults may gradually become separated from their social network due to factors such as retirement, disease, reduced family size, and many others. More specifically, social isolation is defined as the lack of social relationships and low levels of contact with family, friends, the community, and general social environment (1). As the national population continues to age, social isolation is becoming an increasingly serious concern in China.
There is extensive evidence that social isolation leads to both a lower quality-of-life and higher incidence of several psychological and physical diseases (2, 3). Notably, the risk of death from social isolation is comparable to that imposed by some well-established clinical factors, including alcoholism, smoking, and obesity (4). Social isolation also predicts a greater risk of cognitive decline (5), cardiovascular disease (6–8), cerebrovascular disease (7, 8), and all-cause mortality (9, 10). As for health behaviors and self-care, social isolation is associated with increased tobacco use, less vegetable and fruit intake, and less physical activity (11).
The burdens and costs resulting from chronic kidney disease (CKD) have recently begun to increase across the globe (12). This makes it imperative to identify the modifiable risk factors for CKD, especially those that may quickly be addressed to prevent or slow the progression of declining kidney function. Apart from the known clinical factors, new evidence continues to show that social factors may also affect the onset and progression of CKD. For example, Dunkler et al. suggested that a greater number of friends reduced the incidence of and delayed the progression of CKD in individuals with type 2 diabetes (13). Tomaka et al. found that family support independently predicted the outcomes of kidney disease in Hispanic participants (14). Zhang et al. emphasized the associations between depressive symptoms and the risk of kidney function decline; of particular note, loneliness was found to be an independent risk factor (15). In sum, the literature shows that increased attention should be paid to the impacts of social networks on CKD.
To date, there have been no nationally representative studies aimed at assessing the influence of social isolation on the progression of CKD. To address this gap, this prospective study investigated the relationships between social isolation, rapid kidney function decline, and CKD onset in a sample of middle-aged and older adults in China based on four-year follow-up data from the China Health and Retirement Longitudinal Study (CHARLS).
Methods
Study Design and Participants
CHARLS is a nationally representative longitudinal survey that covers 150 counties and 450 communities across 28 provinces in mainland China. The data resource profile and detailed information about blood sample taken has been reported previously(16–18). The survey aims to establish a high quality set of micro-databases that represent middle-aged and elderly individuals in China and their families. The baseline survey was conducted in 2011, with three follow-up surveys conducted in 2013, 2015, and 2018. Ethical approval was received at Peking University (IRB00001052–11015). This study used data from the 2011 and 2015 waves of CHARLS, including information from 8,859 participants who provided baseline blood data related to kidney function. Based on our study criteria, we excluded 5,828 of these participants, including 144 who were aged <45 years, 3,469 who did not provide data on social isolation, 547 with a baseline estimated glomerular filtration rate (eGFR) below 60 mL/min/1.73 m2, and 1,668 without exit eGFR. As such, a total of 3,031 participants were ultimately included for analysis (Figure 1).
Figure 1
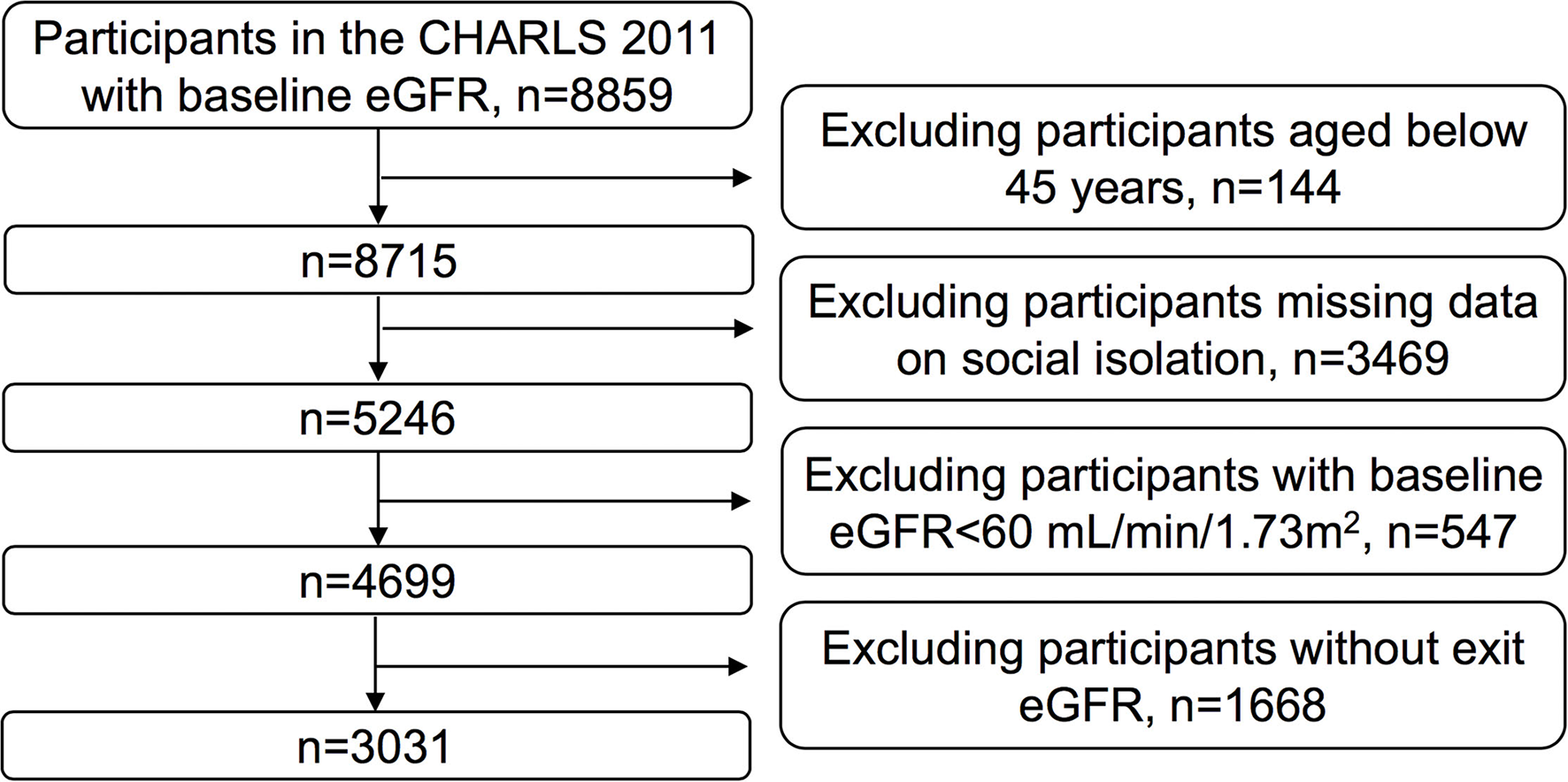
Flow diagram of participants for the study.
Assessment of Social Isolation
The social isolation index was based on the five following items: being unmarried (never married, divorced, and widowed), living alone, having in-person or phone/email contact with their children less often than once per week, living in a rural area, and no participation in social activities over the previous month (e.g., visiting social clubs, interacting with friends, voluntary work, playing cards). Total scores ranged from 0 to 5, with higher scores indicating greater social isolation. We then categorized participants based on a cutoff score of 2, thereby resulting in groups for low (<2) and high (≥2) social isolation (10, 19).
Assessment of Kidney Function
The Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) creatinine-cystatin C equation (20) was used to calculate eGFR, as follows:
eGFR (mL/min/1.73m2) = 135 × min(Cr/k, 1)α × max(Cr/k, 1)−0.601 × min(Cys/0.8, 1)−0.375 × max(Cys/0.8, 1)−0.711 ×0.995age ×0.969[if female]
where Cr refers to serum creatinine measured in mg/dL and CysC refers to serum cystatin C measured in mg/liter. k is 0.7 for females and 0.9 for males. α is −0.248 for females and −0.207 for males.
Outcomes
The primary outcome was rapid eGFR decline, as defined by a decline of > 5 mL/min/1.73 m2/year; this cutoff has been used in previous studies (15, 21). The secondary outcome was the development of CKD, as defined by an eGFR decrease to a level < 60 ml/min/1.73 m2.
Assessment of Covariates
Participants also provided their demographic data and health-related behavioral information (e.g., tobacco use, alcohol consumption, and medication usage) via the CHARLS survey. Each participant had their blood pressure measured three times using a HEM-7200 electronic monitor (Omron, Dalian); these measurements were then averaged and recorded. In this context, hypertension was defined based on systolic blood pressure ≥ 130 mmHg and/or diastolic blood pressure ≥ 80 mmHg or the use of antihypertensive drugs. Next, diabetes was described as fasting glucose ≥ 126 mg/dl, random glucose ≥ 200 mg/dl, hemoglobin A1c ≥ 6.5%, or the use of hypoglycemic drugs. The 10-question version of the Center for Epidemiological Research Depression Scale (CES-D) was used to assess depressive symptoms, which were considered present based on CES-D scores ≥ 10 (22). Drinking was defined as drinking more than once a month currently or in the past. Smoking was defined as having history of smoking including former smoking and current smoking. More specifically, having a response of “Drink more than once a month” to the question “Did you drink any alcoholic beverages, such as beer, wine, or liquor in the past year? How often?” or having a response of “I used to drink more than once a month” to the question “Did you ever drink alcoholic beverages in the past? How often?” were classified into drinking. Having a “yes” response to the question “Have you ever chewed tobacco, smoked a pipe, smoked self-rolled cigarettes, or smoked cigarettes/cigars?” was classified into smoking. The questionnaires can be found at the CHARLS website (http://charls.pku.edu.cn/pages/data/2011-charls-wave1/zh-cn.html).
Statistical Analyses
The data were expressed as means ± standard deviations (SDs) for continuous variables and as numbers and percentages for categorical variables. The level of social isolation was analyzed as a dichotomous variable. The Student's t-test or Pearson χ2 test were used to compare participant characteristics based on low or high levels of social isolation. The univariate and multivariate logistic regression models were used to describe the relationships between social isolation and kidney outcomes. For the multivariate analysis, adjusted covariates included age, sex, body mass index, smoking status, systolic blood pressure, diastolic blood pressure, glucose, total cholesterol, triglycerides, HDL cholesterol, eGFR, uric acid, and CES-D scores. All statistical analyses were conducted using IBM SPSS version 23.0 (IBM Corporation, Armonk, NY, USA).
Results
Characteristics of Participants
Table 1 shows the participant baseline characteristics based on their social isolation category (low or high). Among the 3,031 total analyzed participants, 1,353 were placed into the low social isolation group, while 1,678 were placed into the high social isolation group. The following baseline values were obtained: average age of 59.8 ± 9.2 years, 51.2% female, and mean eGFR of 87.6 ± 14.6 ml/min/1.73 m2. Participants in the high social isolation group were generally older and less educated than those in the low social isolation group; they also tended to have higher CES-D scores, lower body mass index values, and lower baseline eGFR. Supplementary Table 1 shows baseline characteristics for the participants we excluded from analysis. Compared with those who were excluded from the original sample (n = 5,828), participants included in the final analysis were younger, had higher CES-D scores, and were more educated.
Table 1
| Total | Low social isolation | High social isolation | p -value | |
|---|---|---|---|---|
| Unweighted N | 3,031 | 1,353 | 1,678 | |
| Age (year) | 59.8 ± 9.2 | 57.6 ± 8.5 | 61.5 ± 9.3 | <0.001 |
| Sex (female), N (%) | 1,553 (51.2%) | 683 (50.5%) | 870 (51.8%) | 0.454 |
| Elementary school education or above (%) | 1,628 (53.7%) | 889 (65.7%) | 739 (44.0%) | <0.001 |
| Hypertension (%) | 1,393 (46.0%) | 589 (43.5%) | 804 (47.9%) | 0.016 |
| Diabetes (%) | 403 (13.3%) | 191 (14.1%) | 212 (12.6%) | 0.232 |
| Body mass index (kg/m2) | 23.4 ± 3.6 | 24.2 ± 3.7 | 22.9 ± 3.5 | <0.001 |
| Systolic blood pressure (mmHg) | 130.5 ± 21.6 | 129.1 ± 21.0 | 131.5 ± 22.0 | 0.005 |
| Diastolic blood pressure (mmHg) | 75.4 ± 12.0 | 75.7 ± 11.9 | 75.2 ± 12.1 | 0.359 |
| eGFR (mL/min/1.73 m2) | 87.6 ± 14.6 | 89.4 ± 15.1 | 86.0 ± 14.0 | 0.001 |
| Uric acid (mg/dL) | 4.4 ± 1.2 | 4.5 ± 1.2 | 4.3 ± 1.2 | <0.001 |
| Glucose (mg/dL) | 109.2 ± 32.4 | 110.1 ± 33.6 | 108.6 ± 31.5 | 0.256 |
| Glycated hemoglobin (%) | 5.3 ± 0.8 | 5.3 ± 0.8 | 5.3 ± 0.8 | 0.204 |
| Total cholesterol (mg/dL) | 194.2 ± 37.5 | 194.9 ± 37.4 | 193.7 ± 37.6 | 0.836 |
| HDL cholesterol (mg/dL) | 51.3 ± 15.3 | 49.7 ± 14.9 | 52.6 ± 15.5 | 0.067 |
| LDL cholesterol (mg/dL) | 117.3 ± 34.6 | 117.7 ± 35.3 | 117.0 ± 34.1 | 0.382 |
| Triglycerides (mg/dL) | 132.1 ± 97.5 | 141.6 ± 111.5 | 124.4 ± 83.9 | <0.001 |
| Drinking (%) | 782 (25.8%) | 347 (25.6%) | 435 (26.0%) | 0.862 |
| Smoking (%) | 1,239 (40.9%) | 532 (39.3%) | 707 (42.1%) | 0.117 |
| Depressive symptoms score | 9.8 ± 5.5 | 9.4 ± 5.0 | 10.2 ± 5.8 | <0.001 |
| Baseline social isolation | ||||
| Not married (%) | 590 (19.5%) | 2 (0.1%) | 588 (35.1%) | <0.001 |
| Less than weekly contact with children (%) | 305 (10.1%) | 9 (0.7%) | 296 (17.6%) | <0.001 |
| Live in the rural area (%) | 2,482 (84.1%) | 693 (66.6%) | 1,431 (96.3%) | <0.001 |
| Not participate in social activities (%) | 1,440 (47.5%) | 165 (12.2%) | 1,275 (76.0%) | <0.001 |
| Live alone (%) | 584 (19.3%) | 1 (0.0%) | 445 (34.7%) | <0.001 |
Baseline characteristics of participants (n = 3,031) according to social isolation categories.
Data are shown as means ± standard deviation or numbers (percentages).
*p Values correspond two-tailed t-test for continuous variables and chi-squared test for categorical variables.
HDL Cholesterol, high density lipoprotein cholesterol; LDL Cholesterol, low density lipoprotein cholesterol; eGFR, estimated glomerular filtration rate.
Analysis of the Associations of Social Isolation With Primary and Secondary Outcomes
Based on the follow-up data, 258 (8.5%) participants underwent rapid declines in kidney function, with 87 (2.9%) having progressed to CKD. Table 2 shows the relationships between social isolation and CKD outcomes. In the fully adjusted model (Model 2), participants in the high social isolation group had higher overall risks for both rapid eGFR decline (odds ratio [OR] 1.805, 95% confidence interval[CI] 1.310–2.487) and CKD development (OR 1.842, 95% CI 1.084–3.129) than those in the low social isolation group. Table 3 shows the relationships between the five components of social isolation and rapid eGFR decline. Among these components, being unmarried (OR 1.760, 95% CI 1.199–2.583), not participating in social activities (OR 1.353, 95% CI 1.002–1.828), and living alone independently (OR 1.715, 95% CI 1.166–2.523) predicted rapid eGFR decline in the fully adjusted model. However, none of the five components independently predicted CKD development (Supplementary Table 2).
Table 2
| CKD outcomes |
Social isolation
categories |
Events/N (%) | Model 1 | Model 2 | ||
|---|---|---|---|---|---|---|
|
OR
(95% CI) |
P value |
OR
(95% CI) |
P value | |||
| Rapid decline in kidney function | Low | 103/1,353 (7.6%) | (Reference) | (Reference) | ||
| High | 155/1,678 (9.2%) | 1.787 (1.344–2.375) | <0.001 | 1.805 (1.310–2.487) | <0.001 | |
| Progression to CKD | Low | 24/1,353 (1.8%) | (Reference) | (Reference) | ||
| High | 63/1,678 (3.8%) | 2.046 (1.269–3.300) | 0.003 | 1.842 (1.084–3.129) | 0.024 | |
The relationships of social isolation and CKD outcomes.
Model 1 was adjusted for eGFR at baseline. Model 2 was adjusted for age, sex, body mass index, smoking status, drinking status, systolic BP, diastolic BP, glucose, total cholesterol, triglycerides, HDL cholesterol, eGFR, uric acid, and the depressive symptoms score.
Table 3
| Events/N (%) | Model 1 | Model 2 | |||
|---|---|---|---|---|---|
|
OR
(95% CI) |
P value |
OR
(95% CI) |
P value | ||
| Social isolation components | |||||
| Not married | |||||
| No | 204/2,441 (8.4%) | (Reference) | (Reference) | ||
| Yes | 54/590 (9.2%) | 1.956 (1.385–2.764) | <0.001 | 1.760 (1.199–2.583) | 0.004 |
| Less than weekly contact with children | |||||
| No | 231/2,726 (8.5%) | (Reference) | (Reference) | ||
| Yes | 27/305 (8.9%) | 1.158 (0.743–1.805) | 0.518 | 1.237 (0.776–1.973) | 0.371 |
| Living in the rural area | |||||
| No | 43/549 (7.8%) | (Reference) | (Reference) | ||
| Yes | 215/2,482 (8.6%) | 1.268 (0.874–1.841) | 0.211 | 1.416 (0.916–2.189) | 0.118 |
| Not participating in social activities | |||||
| No | 127/1,591 (8.0%) | (Reference) | (Reference) | ||
| Yes | 131/1,440 (9.1%) | 1.373 (1.043–1.807) | 0.024 | 1.353 (1.002–1.828) | 0.049 |
| Living alone | |||||
| No | 205/2,447 (8.4%) | (Reference) | (Reference) | ||
| Yes | 53/584 (9.1%) | 1.915 (1.353–2.710) | <0.001 | 1.715 (1.166–2.523) | 0.006 |
The relationships of social isolation and its components with rapid eGFR decline.
Model 1 was adjusted for eGFR at baseline. Model 2 was adjusted for age, sex, body mass index, smoking status, drinking status, systolic BP, diastolic BP, glucose, total cholesterol, triglycerides, HDL cholesterol, eGFR, uric acid, and the depressive symptoms score.
Stratified Analyses
We conducted a stratified logistic regression analysis to determine whether any variables had interactions that changed the impacts of social isolation on rapid eGFR decline (Table 4). None of the variables (i.e., age, gender, body mass index, educational level, smoking, drinking, hypertension, diabetes, cholesterol, uric acid or depression symptoms) significantly modified the association between high social isolation and rapid eGFR decline (P > 0.05 for all interactions).
Table 4
| Events/N (%) | OR (95% CI) | P value |
P
for
interaction |
|
|---|---|---|---|---|
| Age | 0.924 | |||
| <65 years | 209/2,209 (9.5%) | 1.841 (1.298–2.611) | 0.001 | |
| ≥65 years | 49/822 (6.0%) | 2.285 (1.015–5.143) | 0.046 | |
| Sex | 0.816 | |||
| Male | 105/1,478 (7.1%) | 1.847 (1.153–3.044) | 0.011 | |
| Female | 153/1,553 (9.9%) | 1.793 (1.157–2.777) | 0.009 | |
| Body mass index | 0.876 | |||
| <24 kg/m2 | 127/1,613 (7.9%) | 1.762 (1.132–2.741) | 0.012 | |
| ≥24 kg/m2 | 103/1,118 (9.2%) | 2.000 (1.241–3.222) | 0.004 | |
| Educational level | 0.845 | |||
| < Primary school | 119/1,403 (8.5%) | 2.188 (1.311–3.652) | 0.003 | |
| ≥Primary school | 139/1,628 (8.5%) | 1.621 (1.052–2.498) | 0.029 | |
| Smoking | 0.792 | |||
| No | 180/1,792 (10.0%) | 1.790 (1.205–2.659) | 0.004 | |
| Yes | 78/1,239 (6.3%) | 1.903 (1.081–3.351) | 0.026 | |
| Drinking | 0.097 | |||
| No | 187/2,249 (9.1%) | 1.609 (1.106–2.340) | 0.013 | |
| Yes | 71/782(9.1%) | 2.447 (1.268–4.721) | 0.008 | |
| Hypertension | 0.988 | |||
| No | 120/1,345 (8.9%) | 1.815 (1.168–2.819) | 0.008 | |
| Yes | 112/1,393 (8.0%) | 1.920 (1.186–3.107) | 0.008 | |
| Diabetes | 0.526 | |||
| No | 219/2,628 (8.3%) | 2.088 (1.460–2.987) | <0.001 | |
| Yes | 39/403 (9.7%) | 0.837 (0.377–1.861) | 0.663 | |
| Total cholesterol | 0.781 | |||
| <200 mg/dL | 130/1,790 (7.3%) | 1.793 (1.156–2.782) | 0.009 | |
| ≥200 mg/dL | 128/1,241 (10.3%) | 1.807 (1.126–2.900) | 0.014 | |
| Uric acid | 0.695 | |||
| <4.2 mg/dL | 145/1,471 (9.9%) | 1.894 (1.223–2.934) | 0.004 | |
| ≥4.2 mg/dL | 113/1,560 (7.2%) | 1.711 (1.059–2.766) | 0.028 | |
| Depression symptoms | 0.321 | |||
| No | 129/1,549 (8.3%) | 1.691 (1.079–2.651) | 0.022 | |
| Yes | 129/1,482 (8.7%) | 1.943 (1.226–3.079) | 0.005 |
Effect of social isolation on the risk of rapid eGFR decline by subgroups.
The model was adjusted, if not stratified, for age, sex, body mass index, smoking status, systolic BP, diastolic BP, glucose, total cholesterol, triglycerides, HDL cholesterol, eGFR at baseline, uric acid, and the depressive symptoms score.
Discussion
Compared with the traditional clinical risk factors for CKD, social isolation has received relatively less attention in the public health context. However, this prospective analysis demonstrated that high social isolation was significantly associated with an increased risk of both rapid eGFR decline and CKD development in middle-aged and older persons in China. To the best of our knowledge, this was the first study to report that social isolation status could be used to predict CKD progression, thus contributing to the literature on modifiable renal risk factors.
CKD has been reported to be associated with social isolation in older adults. Participants with CKD Stages 3b-5 had less social participation (23). Reduced kidney function was also independently associated with hearing loss, which may cause social isolation (24). The previous studies both revealed that CKD was associated with social isolation. However, the key message of our longitudinal study was that social isolation predicted worsening kidney function and CKD onset, which was in the other direction and indicated the possible reciprocal relationship between social isolation and CKD. Future multi-center studies should be conducted to validate the findings of our current study and confirm the reciprocal relationship between social isolation and CKD.
In recent years, the national population in China has exhibited accelerated aging. This has created some serious concerns for elderly persons, who are at a higher risk of isolation due to factors such as physical frailty (25, 26), hearing loss (27, 28), the deaths of family members (29, 30), and less frequent contact with children (30). Even more problematically, social isolation that begins earlier in life often becomes more pronounced in later years due to age-related diseases and widowhood, further highlighting the need for interventions (30). However, there is still a general lack of public awareness about social isolation in China. In fact, most findings on the adverse effects of social isolation have been produced in Western countries, and may therefore not fully pertain to the Chinese context (5, 31). In this regard, perspectives on social isolation may markedly differ according to race, religion, community function, and other demographic factors. For example, the Berkman-Syme Social Networks Index has widely been used in previous studies, but only includes four main types of social contact (32), including church group membership, which is not widely relevant in China.
In this study, we measured five dimensions of social isolation that reflect Chinese culture according to the previous CHARLS analysis (19). It is worth mentioning that the three-item index of social isolation including being unmarried, having less contact with their children, and no participation in social activities as well as the four-item index of social isolation including the three-item index plus living in rural were also computed in previous studies using CHARLS data (5, 33). We adopted the five-item index of social isolation as it incorporated living alone, which was documented as the component of social isolation in quite a lot studies (32–35). We also dichotomized scores at ≥2 vs. <2 points to indicate high vs. low social isolation based on previous studies (19), which converted social isolation to a categorical variable and provided convenience for clinical risk classification.
Among the five components of social isolation, we found that being unmarried, living alone, and not participating in social activities were independent risk factors for renal function decline. Notably, a previous study in the United States showed that both being unmarried and infrequent participation in religious activities were predictors of mortality (36). Meanwhile, adults who live alone have been found to have a higher risk of ischemic heart disease mortality (37, 38) as well as a higher risk of falling and general functional decline (39, 40). These factors point to the need for increased social support and specialized public services for elderly persons who are unmarried, live alone, and/or lack social networks, particularly including social visitations and psychological care.
Several mechanisms may be accountable for the impact of social isolation on physical health outcomes. For one, individuals who integrate into society may have more tangible resources pertaining to health care knowledge, thus promoting their ability to engage in self-care (41, 42). Moreover, socially isolated individuals typically experience less social pressure to seek medical care and have poorer medication compliance (43). Apart from directly influencing health-related behaviors, social relationships also affect health-related physiology. For example, socially isolated individuals have higher expressions of genes related to pro-inflammatory cytokine signaling and enhanced immune function in inflammatory-related diseases (44, 45). This means that social isolation may actually worsen the pro-inflammatory state of CKD. In animal studies, social isolation activates the hypothalamus-pituitary-adrenal (HPA) axis and alters the gut microbiome (46, 47). Further, the feelings of being isolated from others is related to lower serum albumin levels (48). Taken together, these reports show that social relationships influence health through several psychological, behavioral, and biological mechanisms. However, continued research is need to clarify the underlying biological mechanisms by which social isolation affects kidney functions.
This study also had several limitations. First, all information on social isolation was self-reported. Here, recall bias may have resulted in underestimated social participation behaviors due to memory loss in some elderly persons. Second, we excluded 3,469 participants who did not have social isolation data. In this regard, nonparticipation by socially isolated individuals who were therefore not detected may have affected the final results. Third, while the level of social isolation is relatively stable, the analysis was solely conducted according to baseline measurements, even though life events may have occurred during the follow-up period. Finally, this was an observational study, meaning that further investigation is needed to establish causality.
Conclusions
Based on data from a large-scale representative survey, this study found that social isolation was significantly associated with rapid declines in kidney function and CKD onset. These findings emphasize the need for interventions aimed at mitigating the effects of social isolation while also pointing out the potential clinical importance of social integration, especially for preventing CKD.
Funding
This research was supported by the National Natural Science Foundation of China and the Science (81870476, 81800596, 82103911, and 81800592); Shanghai Municipal Education Commission (2017-01-07-00-07-E00009); Shanghai ‘Rising Stars of Medical Talent’ Youth Development Program (YS); Shanghai Key Laboratory of Kidney and Blood Purification (14DZ2260200 and 20DZ2271600); Shanghai Medical Centre of Kidney (2017ZZ01015).
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Statements
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author contributions
WZ, YL, and YN for analysis and interpretation of data, statistical analysis, and drafting of the manuscript. SG, NS, BZ, and JW for statistical analysis and technical support. SZ, YS, and XD for study concept and design, analysis and interpretation of data, drafting of the manuscript, obtained funding, and study supervision. All authors read and approved the final manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2021.782624/full#supplementary-material
References
1.
Escalante E Golden RL Mason DJ . Social isolation and loneliness: imperatives for health care in a post-COVID world. JAMA. (2021) 325:520. 10.1001/jama.2021.0100
2.
Moreno-Tamayo K Manrique-Espinoza B Ramírez-García E Sánchez-García S . Social isolation undermines quality of life in older adults. Int Psychogeriatr. (2020) 32:1283–92. 10.1017/S1041610219000310
3.
Cotterell N Buffel T Phillipson C . Preventing social isolation in older people. Maturitas. (2018) 113:80–4. 10.1016/j.maturitas.2018.04.014
4.
Holt-Lunstad J Smith TB Layton JB . Social relationships and mortality risk: a meta-analytic review. PLoS Med. (2010) 7:e1000316. 10.1371/journal.pmed.1000316
5.
Yu B Steptoe A Chen Y Jia X . Social isolation, rather than loneliness, is associated with cognitive decline in older adults: the China Health and Retirement Longitudinal Study. Psychol Med. (2020) 1–8. 10.1017/S0033291720001026
6.
Hu J Fitzgerald SM Owen AJ Ryan J Joyce J Chowdhury E et al . Social isolation, social support, loneliness and cardiovascular disease risk factors: A cross-sectional study among older adults. Int J Geriatr Psychiatry. (2021) 36:1795–809. 10.1002/gps.5601
7.
Valtorta NK Kanaan M Gilbody S Ronzi S Hanratty B . Loneliness and social isolation as risk factors for coronary heart disease and stroke: systematic review and meta-analysis of longitudinal observational studies. Heart. (2016) 102:1009–16. 10.1136/heartjnl-2015-308790
8.
Hakulinen C Pulkki-Råback L Virtanen M Jokela M Kivimäki M Elovainio M . Social isolation and loneliness as risk factors for myocardial infarction, stroke and mortality: UK Biobank cohort study of 479 054 men and women. Heart. (2018) 104:1536–42. 10.1136/heartjnl-2017-312663
9.
Holt-Lunstad J Smith TB Baker M Harris T Stephenson D . Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect Psychol Sci. (2015) 10:227–37. 10.1177/1745691614568352
10.
Steptoe A Shankar A Demakakos P Wardle J . Social isolation, loneliness, and all-cause mortality in older men and women. Proc Nat Acad Sci. (2013) 110:5797–801. 10.1073/pnas.1219686110
11.
Kobayashi LC Steptoe A . Social Isolation, Loneliness, and Health Behaviors at Older Ages: Longitudinal Cohort Study. Ann Behav Med. (2018) 52:582–93. 10.1093/abm/kax033
12.
Xie Y Bowe B Mokdad AH Xian H Yan Y Li T et al . Analysis of the Global Burden of Disease study highlights the global, regional, and national trends of chronic kidney disease epidemiology from 1990 to 2016. Kidney Int. (2018) 94:567–81. 10.1016/j.kint.2018.04.011
13.
Dunkler D Kohl M Heinze G Teo KK Rosengren A Pogue J et al . Modifiable lifestyle and social factors affect chronic kidney disease in high-risk individuals with type 2 diabetes mellitus. Kidney Int. (2015) 87:784–91. 10.1038/ki.2014.370
14.
Tomaka J Thompson S Palacios R . The relation of social isolation, loneliness, and social support to disease outcomes among the elderly. J Aging Health. (2006) 18:359–84. 10.1177/0898264305280993
15.
Zhang Z He P Liu M Zhou C Liu C Li H et al . Association of depressive symptoms with rapid kidney function decline in adults with normal kidney function. CJASN. (2021) 16:889–97. 10.2215/CJN.18441120
16.
Zhao Y Hu Y Smith JP Strauss J Yang G . Cohort profile: The China health and retirement longitudinal study (CHARLS). Int J Epidemiol. (2014) 43:61–8. 10.1093/ije/dys203
17.
Chen X Crimmins E Hu P (Perry) Kim JK Meng Q Strauss J et al . Venous blood-based biomarkers in the china health and retirement longitudinal study: rationale, design, and results from the 2015 wave. Am J Epidemiol. (2019) 188:1871–7. 10.1093/aje/kwz170
18.
Wu C Newman AB Dong B-R Odden MC . Index of healthy aging in Chinese older adults: china health and retirement longitudinal study. J Am Geriatr Soc. (2018) 66:1303–10. 10.1111/jgs.15390
19.
Luo F Guo L Thapa A Yu B . Social isolation and depression onset among middle-aged and older adults in China: Moderating effects of education and gender differences. J Affect Disord. (2021) 283:71–6. 10.1016/j.jad.2021.01.022
20.
Inker LA Schmid CH Tighiouart H Eckfeldt JH Feldman HI Greene T et al . Estimating glomerular filtration rate from serum creatinine and cystatin C. N Engl J Med. (2012) 367:20–9. 10.1056/NEJMoa1114248
21.
Xie L Wang B Jiang C Zhang X Song Y Li Y et al . BMI is associated with the development of chronic kidney diseases in hypertensive patients with normal renal function. J Hypertens. (2018) 36:2085–91. 10.1097/HJH.0000000000001817
22.
Andresen EM Malmgren JA Carter WB Patrick DL . Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). Am J Prev Med. (1994) 10:77–84. 10.1016/S0749-3797(18)30622-6
23.
Moorthi RN Latham-Mintus K . Social isolation in chronic kidney disease and the role of mobility limitation. Clin Kidney J. (2019) 12:602–10. 10.1093/ckj/sfy134
24.
Liu W Meng Q Wang Y Yang C Liu L Wang H et al . The association between reduced kidney function and hearing loss: a cross-sectional study. BMC Nephrol. (2020) 21:145. 10.1186/s12882-020-01810-z
25.
Klinenberg E . Social Isolation, Loneliness, and Living Alone: Identifying the Risks for Public Health. Am J Public Health. (2016) 106:786–7. 10.2105/AJPH.2016.303166
26.
Maltby J Hunt SA Ohinata A Palmer E Conroy S . Frailty and social isolation: comparing the relationship between frailty and unidimensional and multifactorial models of social isolation. J Aging Health. (2020) 32:1297–308. 10.1177/0898264320923245
27.
Shukla A Harper M Pedersen E Goman A Suen JJ Price C et al . Hearing loss, loneliness, and social isolation: a systematic review. Otolaryngol Head Neck Surg. (2020) 162:622–33. 10.1177/0194599820910377
28.
Hodgson S Watts I Fraser S Roderick P Dambha-Miller H . Loneliness, social isolation, cardiovascular disease and mortality: a synthesis of the literature and conceptual framework. J R Soc Med. (2020) 113:185–92. 10.1177/0141076820918236
29.
Collins T . The personal communities of men experiencing later life widowhood. Health Soc Care Community. (2018) 26:e422–30. 10.1111/hsc.12542
30.
Holt-Lunstad J . The potential public health relevance of social isolation and loneliness: prevalence, epidemiology, and risk factors. Public Policy & Aging Report. (2017) 27:127–30. 10.1093/ppar/prx030
31.
Zhou Y Chen Z Shaw I Wu X Liao S Qi L et al . Association between social participation and cognitive function among middle- and old-aged Chinese: A fixed-effects analysis. J Glob Health. (2020) 10:020801. 10.7189/jogh.10.020801
32.
Tanskanen J Anttila T . A prospective study of social isolation, loneliness, and mortality in Finland. Am J Public Health. (2016) 106:2042–8. 10.2105/AJPH.2016.303431
33.
Yu B Steptoe A Niu K Jia X . Social isolation and loneliness as risk factors for grip strength decline among older women and men in China. J Am Med Dir Assoc. (2020) 21:1926–30. 10.1016/j.jamda.2020.06.029
34.
Shankar A McMunn A Banks J Steptoe A . Loneliness, social isolation, and behavioral and biological health indicators in older adults. Health Psychology. (2011) 30:377–85. 10.1037/a0022826
35.
Bu F Zaninotto P Fancourt D . Longitudinal associations between loneliness, social isolation and cardiovascular events. Heart. (2020) 106:1394–9. 10.1136/heartjnl-2020-316614
36.
Pantell M Rehkopf D Jutte D Syme SL Balmes J Adler N . Social isolation: a predictor of mortality comparable to traditional clinical risk factors. Am J Public Health. (2013) 103:2056–62. 10.2105/AJPH.2013.301261
37.
Floud S Balkwill A Canoy D Wright FL Reeves GK Green J et al . Million women study collaborators. Marital status and ischemic heart disease incidence and mortality in women: a large prospective study. BMC Med. (2014) 12:42. 10.1186/1741-7015-12-42
38.
Eaker ED Sullivan LM Kelly-Hayes M D'Agostino RB Benjamin EJ . Marital status, marital strain, and risk of coronary heart disease or total mortality: the Framingham Offspring Study. Psychosom Med. (2007) 69:509–13. 10.1097/PSY.0b013e3180f62357
39.
Ek S Rizzuto D Xu W Calderón-Larrañaga A Welmer A-K . Predictors for functional decline after an injurious fall: a population-based cohort study. Aging Clin Exp Res. (2021) 33:2183–90. 10.1007/s40520-020-01747-1
40.
Divani AA Vazquez G Barrett AM Asadollahi M Luft AR . Risk factors associated with injury attributable to falling among elderly population with history of stroke. Stroke. (2009) 40:3286–92. 10.1161/STROKEAHA.109.559195
41.
Cohen S . Psychosocial models of the role of social support in the etiology of physical disease. Health Psychol. (1988) 7:269–97. 10.1037/0278-6133.7.3.269
42.
O'Neal CW Wickrama KAS Ralston PA Ilich JZ Harris CM Coccia C et al . Examining change in social support and fruit and vegetable consumption in African American adults. J Nutr Health Aging. (2014) 18:10–4. 10.1007/s12603-013-0376-1
43.
Lu J Zhang N Mao D Wang Y Wang X . How social isolation and loneliness effect medication adherence among elderly with chronic diseases: An integrated theory and validated cross-sectional study. Arch Gerontol Geriatr. (2020) 90:104154. 10.1016/j.archger.2020.104154
44.
Cole SW Hawkley LC Arevalo JM Sung CY Rose RM Cacioppo JT . Social regulation of gene expression in human leukocytes. Genome Biol. (2007) 8:R189. 10.1186/gb-2007-8-9-r189
45.
Cole SW . Human social genomics. PLoS Genet. (2014) 10:e1004601. 10.1371/journal.pgen.1004601
46.
Hawkley LC Cole SW Capitanio JP Norman GJ Cacioppo JT . Effects of social isolation on glucocorticoid regulation in social mammals. Horm Behav. (2012) 62:314–23. 10.1016/j.yhbeh.2012.05.011
47.
Donovan M Mackey CS Platt GN Rounds J Brown AN Trickey DJ et al . Social isolation alters behavior, the gut-immune-brain axis, and neurochemical circuits in male and female prairie voles. Neurobiology of Stress. (2020) 13:100278. 10.1016/j.ynstr.2020.100278
48.
Untas A Thumma J Rascle N Rayner H Mapes D Lopes AA et al . The associations of social support and other psychosocial factors with mortality and quality of life in the dialysis outcomes and practice patterns study. CJASN. (2011) 6:142–52. 10.2215/CJN.02340310
Summary
Keywords
social isolation, chronic kidney disease, glomerular filtration rate, CHARLS, Chinese middle-aged and older adults
Citation
Zhou W, Li Y, Ning Y, Gong S, Song N, Zhu B, Wang J, Zhao S, Shi Y and Ding X (2021) Social Isolation Is Associated With Rapid Kidney Function Decline and the Development of Chronic Kidney Diseases in Middle-Aged and Elderly Adults: Findings From the China Health and Retirement Longitudinal Study (CHARLS). Front. Med. 8:782624. doi: 10.3389/fmed.2021.782624
Received
24 September 2021
Accepted
09 November 2021
Published
02 December 2021
Volume
8 - 2021
Edited by
Sebastjan Bevc, Maribor University Medical Center, Slovenia
Reviewed by
Antony Bayer, Cardiff University, United Kingdom; Dongshan Zhu, Shandong University, China
Updates
Copyright
© 2021 Zhou, Li, Ning, Gong, Song, Zhu, Wang, Zhao, Shi and Ding.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaoqiang Ding ding.xiaoqiang@zs-hospital.sh.cnYiqin Shi shi.yiqin@zs-hospital.sh.cnShuan Zhao zhao.shuan@zs-hospital.sh.cn
†These authors have contributed equally to this work
This article was submitted to Nephrology, a section of the journal Frontiers in Medicine
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.