Abstract
Background:
Pediatric mortality after being admitted to a pediatric intensive care unit in Ethiopia is high when compared to high-income countries. There are limited studies regarding pediatric mortality in Ethiopia. This systematic review and meta-analysis aimed to assess the magnitude and predictors of pediatric mortality after being admitted to an intensive care unit in Ethiopia.
Methods:
This review was conducted in Ethiopia after retrieving peer-reviewed articles and evaluating their quality using AMSTAR 2 criteria. An electronic database was used as a source of information, including PubMed, Google Scholar, and Africa Journal of Online Databases, using AND/OR Boolean operators. Random effects of the meta-analysis were used to show the pooled mortality of pediatric patients and its predictors. A funnel plot was used to assess the publication bias, and heterogeneity was also checked. The final result were expressed as an overall pooled percentage and odds ratio with a 95% confidence interval (CI) of < 0.05%.
Results:
In our review, eight studies were used for the final analysis with a total population of 2,345. The overall pooled mortality of pediatric patients after being admitted to the pediatric intensive care unit was 28.5% (95% CI: 19.06, 37.98). The pooled mortality determinant factors were included the use of a mechanical ventilator with an odds ratio (OR) of 2.64 (95% CI: 1.99, 3.30); the level of Glasgow Coma Scale <8 with an OR of 2.29 (95% CI: 1.38, 3.19); the presence of comorbidity with an OR of 2.18 (95% CI: 1.41, 2.95); and the use of inotropes with an OR of 2.36 (95% CI: 1.65, 3.06).
Conclusion:
In our review, the overall pooled mortality of pediatric patients after being admitted to the intensive care unit was high. Particular caution should be taken in patients on the use of mechanical ventilators, the level of Glasgow Coma Scale of <8, the presence of comorbidity, and the use of inotropes.
Systematic review registration:
https://www.researchregistry.com/browse-the-registry#registryofsystematicreviewsmeta-analyses/, identifier: 1460.
Introduction
According to the World Health Organization (WHO), acute pediatric critical illness is defined as “any severe problem with the airway, breathing, or circulation, or acute deterioration of conscious state; [which] includes apnea, upper airway obstruction, hypoxemia, central cyanosis, severe respiratory distress, total inability to feed, shock, severe dehydration, active bleeding requiring transfusion, unconsciousness, or seizures” (1). Children are frequently admitted to the intensive care unit (ICU), where advanced organ, hemodynamic, and airway support are required.
In recent decades, tremendously lower mortality and morbidity following admission to pediatric intensive care units (PICUs) have been reported in high-income countries due to medical care advancements (2). However, the mortality of children admitted to ICU remained higher in low- and middle-income countries such as Ethiopia (3). Most hospitals in low- and middle-income countries lack dedicated ICUs for pediatric patients, and there is a scarcity of trained medical specialists allocated to PICUs (4). In addition, essential drugs and equipment are not readily available (3, 5).
Although there are limited published data on mortality and its risk factors in critically ill pediatric patients admitted to PICUs in low-resource countries, few studies identified demographic, clinical, and physiological factors contributing to the death of patients in PICUs. Malnutrition, length of the PICU stay, multiorgan failure, shock, infection, mechanical ventilation, and vasopressor support are among the risk factors reported (6–11).
In Ethiopia, few studies are available concerning pediatric critical care outcomes and predictors of mortality in PICU. Using currently available evidence in Ethiopia, this systematic review aimed to study the incidence of mortality among patients admitted to PICUs and factors associated with mortality in PICUs. This review's findings can help stakeholders improve the critical care provided to the patients admitted to PICU by using evidence-based, more effective, and comprehensive treatments. It aids and simplifies allocating resources to patients who need them the most, depending on the risks they pose as identified by this review. In addition, this review will help fill the information gap and guide further pediatric and critical care studies. Therefore, this review aims to estimate the pooled magnitude and determinant factors for pediatric mortality in the intensive care unit of Ethiopia.
Methods
Eligibility criteria
Inclusion criteria
This review includes observational studies conducted in the Ethiopia population that investigated the incidence and/or mortality risk factors among pediatric patients admitted to PICU, published until 1 September 2022. The age group was between 1 month and 16 years, and studies conducted in English were included in this review.
Exclusion criteria
Studies conducted on the adult population (age ≥ 16), case reports/case series studies, systematic reviews, studies conducted outside Ethiopia, preprint, and articles without full text were excluded.
Information source and searching process
PubMed, Google Scholar, and African Journals Online Databases were searched using the following combinations of keywords: (“pediatrics” OR “children” OR “child” OR “pediatrics”) AND (“ICU” OR “intensive care unit” OR “critical care unit”) AND (“mortality” OR “morbidity” OR “outcome” OR “survival”) AND (“Ethiopia”). We identified and recorded the article that was eligible for our review.
Protocol and registration
This systematic review was conducted based on Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (12). We formulated a search strategy and eligibility criteria using PRISMA guidelines before the review. The retrieved articles were then assessed based on pre-defined eligibility criteria. After finding relevant studies, data from each study were collected. This review was carried out in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 statement (Figure 1). This review was registered in the Research Registry with a unique identifying number of review registry 1460, and the link is https://www.researchregistry.com/browse-the-registry#registryofsystematicreviewsmeta~analyses/.
Figure 1

PRISMA flow chart.
Screening and selection process
In two stages, selected articles were identified. First, two authors reviewed titles and abstracts for eligibility, followed by full-text reviews. The other two reviewers extracted the data, and its completeness was cross-checked with each other who read the full text. When the two researchers disagreed, they openly discussed the disagreement and identified the inconsistency; all reviewers provided evidence and resolved the deviation based on scientific justification. Finally, after a thorough selection and screening of eligible articles, we obtained eight articles for analysis and reporting of this review.
Study quality assessment
All authors checked the article's quality in retrieving each article for methodological quality that met the inclusion criteria in our review. All authors agreed on the quality of the studies. The methodological quality of our systematic review and meta-analysis compliance were evaluated using AMSTAR 2 criteria, and it was found to be of high quality (13).
Outcome of interest
The incidence of mortality among pediatric patients admitted to PICU was the primary outcome of this systematic review. The mortality risk factors among pediatric patients admitted to PICU were reported as the secondary outcome in the studies that met the inclusion criteria.
Data extraction and analysis
Using Microsoft Excel, eight articles that met the eligibility were retrieved from each study: the authors, publication years, study region, study period, sample size, study design, incidence, association measure, P-value, and mortality risk factors, including the use of a mechanical ventilator, use of inotropes, level of GCS < 8, length of ICU stay, presence of comorbidity, multiorgan dysfunction, medical case, weekend admission, and critical illness diagnosis data among pediatric patients admitted to PICU were selected. After entering the data, we transform it to Stata/MP version 17 (64-bit) software for analysis. A random effect meta-analysis was used for this review. DerSimonian and Laird's heterogeneity variance estimator was used, and a confidence interval was used for heterogeneity variance. The pooled magnitude of mortality and its determinants in pediatric patients admitted to PICU were analyzed as an overall pooled analysis and a factor analysis. The result was expressed using pooled mortality, along with its 95% confidence interval, P-value, and I2.
Results
Description of studies
During our systematic review, we included eight articles with a total sample size of 2,345 study subjects, which matched our objective. The final analysis included two articles from Addis Ababa, three from Amhara, two from Oromia, and one from the Tigray region (11, 14–20). All the studies were conducted from 2015 to 2022. One article was conducted with a cohort study design, while the other was conducted with a crossectional study design. In our review, the analysis method used for the three articles was chi-square analysis (14, 17, 20), while the analysis method for the five articles was logistic regression, and one article used the survival model (11, 15, 16, 18, 19, 21); it helps to minimize confounding factors, and this study includes the determinate factors for pediatric mortality in PICU (Table 1).
Table 1
| References | Study design | Study region | Publication year | Sample size | Death | Mortality in (%) |
|---|---|---|---|---|---|---|
| Edae et al. (15) | Cross-sectional | Addis Ababa | 2022 | 260 | 55 | 21.2 |
| Tazebew et al. (14) | Cross-sectional | Amhara | 2019 | 330 | 102 | 30.9 |
| Seifu et al. (16) | Cross-sectional | Addis Ababa | 2022 | 361 | 158 | 43.8 |
| Ahmed (17) | Cross-sectional | Amhara | 2022 | 305 | 72 | 23.6 |
| Haftu et al. (18) | Cross-sectional | Tigray | 2018 | 400 | 34 | 8.5 |
| Teshager et al. (21) | Cohort | Amhara | 2020 | 313 | 102 | 32.6 |
| Bacha et al. (19) | Cross-sectional | Oromia | 2022 | 206 | 59 | 28.6 |
| Abebe et al. (20) | Cross-sectional | Oromia | 2015 | 170 | 68 | 40 |
Characteristics of included studies of pediatric patients admitted to a pediatric intensive care unit in Ethiopia.
The characteristics of the determinant factors include the use of mechanical ventilators, length of stay, presence of comorbidity, and level of GCS < 8 were among those involved in the pooled analysis (Table 2).
Table 2
| Factors | Numbers of death | Percentage | Measure of association | 95% CI | P-value | References |
|---|---|---|---|---|---|---|
| Level of GCS < 8 | 90 | 24.93 | OR (10.5) | 3.81–29.1 | 0.001 | Seifu et al. (16) |
| Presence of comorbidity | 127 | 35.18 | OR (8.38) | 3.42–20.5 | 0.001 | Seifu et al. (16) |
| Use of mechanical ventilator | 142 | 39.34 | OR (11.2) | 4.3–28.9 | 0.001 | Seifu et al. (16) |
| Use of inotropes | 99 | 24.43 | OR (10.7) | 4.09–27.81 | 0.001 | Seifu et al. (16) |
| Patients admitted for medical case | 112 | 50.9 | OR (0.127) | 0.37–0.41 | < 0.05 | Bacha et al. (19) |
| Weekend admission | 31 | 23.66 | HR (1.63) | 1.02–2.60 | < 0.05 | Teshager et al. (11) |
| Use of mechanical ventilator | 23 | 22.54 | HR (2.36) | 1.39–4.01 | < 0.05 | Teshager et al. (11) |
| Critical illness diagnosis | 49 | 15.65 | HR (1.79) | 1.13–2.85 | < 0.05 | Teshager et al. (11) |
| Multiorgan dysfunction | 97 | 44.09 | OR (0.181) | 0.08–0.41 | < 0.05 | Bacha et al. (19) |
| ICU stay duration 2–7 days | 64 | 17.72 | OR (7.27) | 1.73–30.55 | 0.007 | Seifu et al. (16) |
| ICU stay duration 7–14 days | 43 | 11.91 | OR (5.42) | 1.18–24.80 | 0.029 | Seifu et al. (16) |
| ICU stay duration 14–28 days | 19 | 5.26 | OR (7.02) | 1.08–45.19 | 0.04 | Seifu et al. (16) |
| Level of GCS < 8 | 6 | 16.2 | OR (7.74) | 1.1–54 | 0.04 | Haftu et al. (18) |
| Use of inotropes | 17 | 12.7 | OR (10.4) | 3.7–29 | 0.000 | Haftu et al. (18) |
| Use of mechanical ventilator | 6 | 37.5 | OR (17.6) | 2.2–14 | 0.007 | Haftu et al. (18) |
| Presence of comorbidity | 27 | 14.8 | OR (10.2) | 2.2–44 | 0.004 | Haftu et al. (18) |
| ICU stay duration 2–7 days | 16 | 6.6 | OR (0.09) | 0.023–0.39 | 0.001 | Haftu et al. (18) |
| ICU stay duration 7–14 days | 3 | 7 | OR (0.094) | 0.1–0.78 | 0.02 | Haftu et al. (18) |
| ICU stay duration 14–28 days | 1 | 6.7 | OR (0.019) | 0.01–0.45 | 0.01 | Haftu et al. (18) |
Characteristics of determinant factors of pediatric mortality in a pediatric intensive care unit, Ethiopia.
The magnitude of pediatric mortality in PICU
In this systematic review and meta-analysis, the mortality rate of pediatric patients after being admitted to PICU was varying between the lowest, which was 8.5%, reported by Haftu et al. (18), and the highest, 43.8% reported by Bacha et al. (19). In our systematic review and meta-analysis, the overall pooled mortality rate among pediatric patients after being admitted to PICU was 28.5% (95% CI: 19.06, 37.98; Figure 2).
Figure 2

Pooled pediatric mortality.
Assessment of heterogeneity
In this review, we used subgroup analysis to assess heterogeneity, and the P-value and I2 statistics were used to assess the heterogeneity between the studies. The P-value for a subgroup heterogeneity of 0.000 and the I2-test of heterogeneity of 96.8% were obtained. In order to assess heterogeneity between subgroups, we performed a subgroup analysis using the regional administrative state and the sample size of the included studies. From the subgroup analysis, the overall pooled mortality in Oromia was high with 34.14% (95% CI: 23.01, 45.26) and I2 = 81.4%, followed by a study conducted in Addis Ababa was 32.45% (95% CI: 10.28, 54.62) and I2 = 97.4%, a study conducted in Amhara was 28.97% (95% CI: 23.48, 34.45) and I2 = 72.6%, and a study in Tigray administrative state with an overall mortality of 8.50% (95% CI: 5.77, 11.23; Figure 3).
Figure 3

Subgroup analysis by sample size and region.
Assessment of publication bias
The funnel plot was used to check the publication bias and shows deviation from the symmetrical line. However, Egger's regression and Beggs correlation coefficients show a difference and a low possibility of publication bias with a P-value of 2.234 (Figure 4).
Figure 4
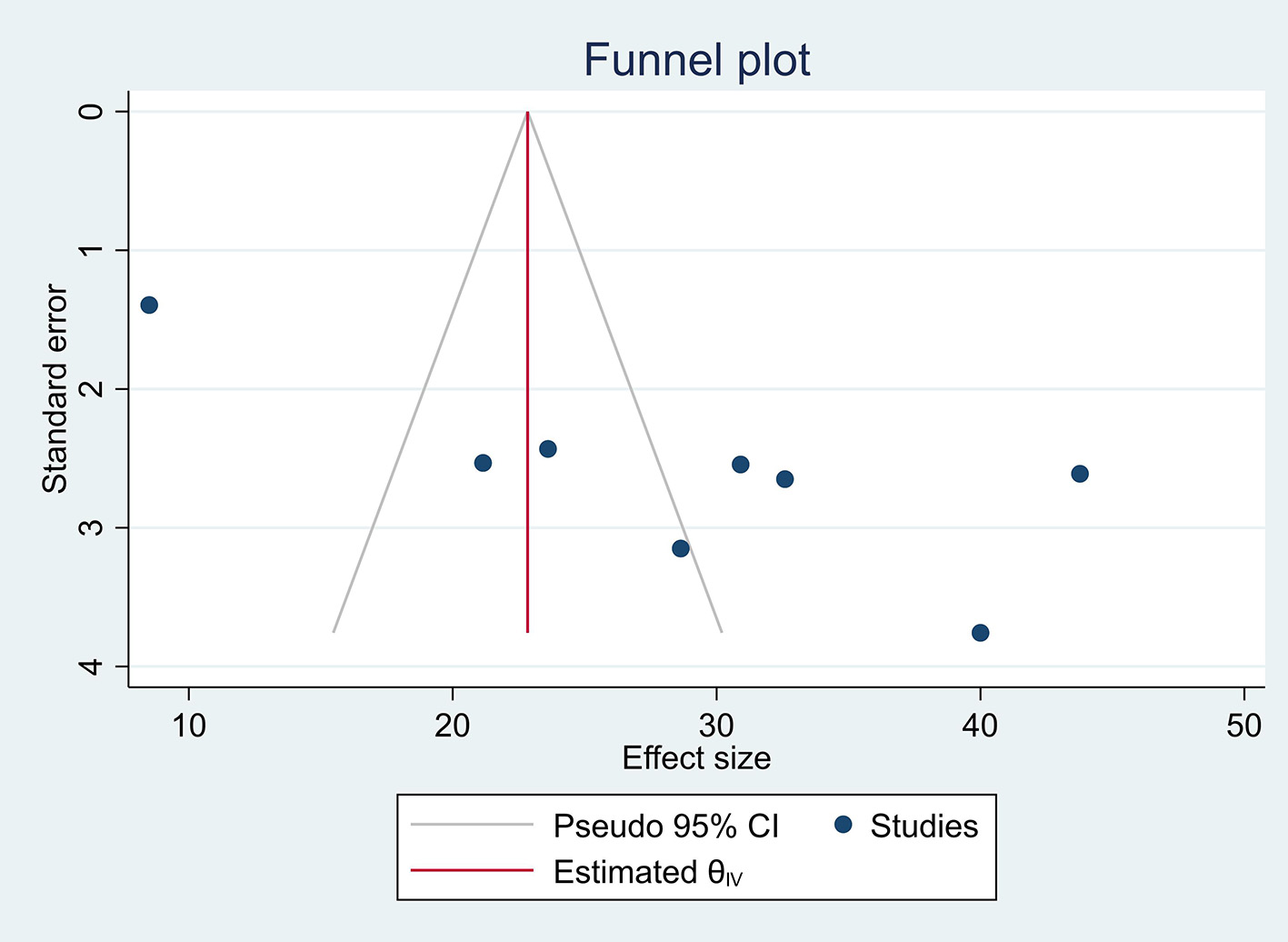
Funnel plot.
Sensitivity analysis
We conducted a sensitivity analysis by removing a study with a lower and higher value on the review to show the effect of one study on the overall pooled summary effect, and we found that removing a study did not result in a significant summary effect on the overall outcome (Figure 5).
Figure 5

Sensitivity analysis.
Pooled analysis for determinant factors
Use of a mechanical ventilator
The use of a mechanical ventilator for pediatric patients at PICU was the contributing factor stated by two studies (16, 18), with 2.64 times increases in overall pooled mortality in pediatric patients (OR, 2.64 CI: 1.99, 3.30; Figure 6A). Moreover, most patients required a mechanical ventilator due to shock, acute respiratory distress syndrome, and trauma.
Figure 6

Determinant factors for pediatric mortality. (A) Use of a mechanical ventilator. (B) Level of GCS < 8. (C) Presence of comorbidity. (D) Use of inotropes.
Level of GCS < 8
The level of GCS of <8 was a factor for pediatric mortality in the PICU, as reported by two studies in our review (16, 18), with a pooled analysis of 2.29 times more likely to increase mortality (OR, 2.29 CI: 1.38, 3.19; Figure 6B). Considering that most patients brought to the ICU had low GCS of <8 and required intubation, it is a determinant for increased mortality.
Presence of comorbidity
In our review of pooled analysis, as stated by two studies (16, 18), the presence of multiple comorbidities increases the mortality of pediatric patients by 2.18 (OR, 2.18 CI: 1.41, 2.95; Figure 6C). In addition to the primary illness, comorbidities have been shown to have a significant impact on the clinical course, complications rate, and outcomes in the ICU, increasing the patient's criticality and physiologic derangement.
Use of inotropes
The pooled analysis review, stated by two studies (16, 18), shows 2.36 times more likely increase in the mortality of pediatric patients (OR, 2.36, CI: 1.65, 3.06).
Even if other determinate factors affect the mortality of pediatric patients, only the above factors are common in pooling analysis as determinate factors for pediatric mortality admitted to PICU (Figure 6D).
Discussion
Studies conducted in Ethiopia on pediatric mortality admitted to PICU were high compared to high-income countries. In our review, the pooled mortality rate of pediatric patients after being admitted to the PICU was 28.5%. The use of a mechanical ventilator, level of GCS < 8, the presence of comorbidity, and the use of inotropes were the pooled determinant factors for the mortality of pediatric patients admitted to the PICU of Ethiopia.
The analysis of the article conducted on pediatric mortality at PICU in this review remains high. For instance, from two studies conducted in Addis Ababa, the pooled mortality of pediatric patients after being admitted to PICU was 32.45%. Three studies were conducted in the Amhara region, yielding a pooled mortality rate of 28.97%. Two studies were conducted in the Oromia region of Ethiopia, and the pooled mortality rate of pediatric patients was 34.14%. One study from the Tigray region of Ethiopia showed 8.5%. The difference in mortality among pediatric patients admitted to PICU was due to sample size difference, duration, and the number of studies included.
A study conducted on pediatric mortality after being admitted to PICU in low-income countries ranges from 6.7 to 51.1% (7, 22–25), but in developed countries, such as Europe and America, it ranges from 1.85 to 5.8% (26), and in Latin America, it reached up to 13.1% (27). The difference in the mortality of pediatric patients is due to the reason that there is limited availability of ICU setups, scarcity of trained staffing, and lack of availability of materials (14).
In our review, two articles stated that the use of mechanical ventilators was the factor for pooled mortality of pediatric patients at PICU. This review is supported by studies conducted in Jordan (23) and the Netherlands (28). The possible explanation is that most patients who require mechanical ventilators are more critical than those who do not, and it stays in for a couple of days, thereby increasing mortality. In addition, patients using a mechanical ventilator will be immobile for a prolonged time, raising the risk of venous thromboembolism. They are also more likely to acquire ventilator-associated pneumonia, which could lower their likelihood of survival (29).
The level of GCS of <8 has a factor in the mortality of PICU in our review. This finding is supported by studies conducted in Iran (30) and the Netherlands (31). The possible explanation for this factor was that decreased GCS level results in more critical patients and increased mortality. Another explanation could be that patients with low GCS have a higher mortality risk in the PICU due to the increased risk of hypoxia caused by compromised airway patency. In addition, cerebral hypoxia caused by hypotension in a decompensated illness process indicates multiorgan failure, which will have a serious impact on survival (32). In addition, the low GCS shows that the central nervous system is dysfunctional, which is the cause of the patient's slow recovery after being admitted to the ICU (33).
In our study, comorbidity was one of the determinant factors contributing to pediatric patients' mortality in PICU. This finding is supported by studies conducted in Jordan (23) and India (34). Comorbidities have been shown to have a significant impact on the clinical course, complications rate, and outcomes in the ICU. In addition to the primary illness, comorbidities increase the patient's criticality, and physiologic derangement is suggested as a possible explanation for the contributing factor of mortality (35).
In our study, the usage of inotropes medication in the PICU contributed to the mortality of pediatric patients. This study was supported by a study conducted in Indonesia (36). Since most of the ICU patients had severe illnesses and required inotropes, mortality was likely increased. The patient was admitted to the intensive care unit for persistent hypotension, who was resistant to volume replacement and experienced a refractory state and a worsening prognosis due to the administration of inotropes for a prolonged time and at a higher dose (37).
This review will provide information for further study, inquire about overall mortality, and identify the common determinant factors of pediatric patients' mortality admitted to the PICU. A limitation of this review is that a small number of studies were included in this review due to the limited availability of studies conducted in Ethiopia.
Conclusion
Pediatric mortality admitted to Ethiopia's PICU is high compared to middle- and high-income countries. The determinant factors for pediatric mortality in PICU were the use of a mechanical ventilator, use of inotropes, level of GCS of < 8, and the presence of comorbidity. Therefore, there is a need for attention to reducing pediatric patients' mortality. Furthermore, this needs collaborative work with the policymaker, the government, the hospitals, and the health professionals working at PICU.
Statements
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
MM and AE contributed to the conception of the review, writing of the review, interpretation of the literature based on the level of evidence, preparation, and critical review of the manuscripts. FK and TL interpreted the literature based on the level of evidence, preparation, and critical review of the manuscripts. All authors read and approved the manuscript.
Acknowledgments
We thank Bahir Dar University, College of Medicine, and Health Sciences Anesthesia Department staff for their unlimited support in this review.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
CI, Confidence interval; GCS, Glasgow Coma Scale; ICU, Intensive care unit; MV, Mechanical ventilator; OR, Odds ratio; PICU, Pediatrics intensive care unit; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
References
1.
Organization WH . Updated Guideline: Paediatric Emergency Triage, Assessment and Treatment: Care of Critically-Ill Children. Geneva: WHO (2016).
2.
Randolph AG Gonzales CA Cortellini L Yeh TS . Growth of pediatric intensive care units in the United States from 1995 to 2001. J Pediatr. (2004) 144:792–8. 10.1016/S0022-3476(04)00218-5
3.
Kortz TB Nielsen KR Mediratta RP Reeves H O'Brien NF Lee JH et al . The burden of critical illness in hospitalized children in low-and middle-income countries: Protocol for a systematic review and meta-analysis. Front Pediatr. (2022) 10:756643. 10.3389/fped.2022.756643
4.
Tripathi S Kaur H Kashyap R Dong Y Gajic O Murthy S et al . survey on the resources and practices in pediatric critical care of resource-rich and resource-limited countries. J Intensive Care. (2015) 3:1–5. 10.1186/s40560-015-0106-3
5.
Slusher TM Kiragu AW Day LT Bjorklund AR Shirk A Johannsen C et al . Pediatric critical care in resource-limited settings—Overview and lessons learned. Front Pediatr. (2018) 6:49. 10.3389/fped.2018.00049
6.
Khilnani P Sarma D Singh R Uttam R Rajdev S Makkar A et al . Demographic profile and outcome analysis of a tertiary level pediatric intensive care unit. Apollo Med. (2004) 1:161–6. 10.1016/S0976-0016(11)60242-1
7.
Ballot DE Ramdin T White DA Lipman J . A comparison between raw and predicted mortality in a paediatric intensive care unit in South Africa. BMC Res Notes. (2018) 11:1–6. 10.1186/s13104-018-3946-9
8.
Gandhi J Sangareddi S Varadarajan P Suresh S . Pediatric index of mortality 2 score as an outcome predictor in pediatric Intensive Care Unit in India. Ind J Crit Care Med. (2013) 17:288. 10.4103/0972-5229.120320
9.
Becerra MR Tantaleán JA Suárez VJ Alvarado MC Candela JL Urcia FC . Epidemiologic surveillance of nosocomial infections in a Pediatric Intensive Care Unit of a developing country. BMC Pediatr. (2010) 10:1–9. 10.1186/1471-2431-10-66
10.
Hendricks CL McKerrow N . Factors present on admission associated with increased mortality in children admitted to a paediatric intensive care unit (PICU). South Afri J Child Health. (2016) 10:57–62. 10.7196/SAJCH.2016.v10i1.1048
11.
Teshager NW Amare AT Tamirat KS . Incidence and predictors of mortality among children admitted to the pediatric intensive care unit at the University of Gondar comprehensive specialized hospital, northwest Ethiopia: A prospective observational cohort study. Br Med J Open. (2020) 10:e036746. 10.1136/bmjopen-2019-036746
12.
Page MJ McKenzie JE Bossuyt PM Boutron I Hoffmann TC Mulrow CD et al . The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst Rev. (2021) 10:1–11. 10.1186/s13643-021-01626-4
13.
Shea BJ Reeves BC Wells G Thuku M Hamel C Moran J et al . AMSTAR 2: A critical appraisal tool for systematic reviews that include randomized or non-randomized studies of healthcare interventions, or both. Br Med J. (2017) 358:j4008. 10.1136/bmj.j4008
14.
Tazebew A Tilahun B Heye T . Admission pattern and outcome in a pediatric intensive care unit of Gondar University Hospital. Ethiop Med J. (2019) 57.
15.
Edae G Tekleab AM Getachew M Bacha T . Admission pattern and treatment outcome in pediatric intensive care unit, Tertiary Hospital, Addis Ababa, Ethiopia. Ethiop J Health Sci. (2022) 32:497–504. 10.4314/ejhs.v32i3.4
16.
Seifu A Eshetu O Tafesse D Hailu S . Admission pattern, treatment outcomes, and associated factors for children admitted to pediatric intensive care unit of Tikur Anbessa specialized hospital, 2021: A retrospective cross-sectional study. BMC Anesthesiol. (2022) 22:13. 10.1186/s12871-021-01556-7
17.
Ahmed SA . Admission patterns and outcome in a pediatric intensive care unit of the University of Gondar Comprehensive Specialized Hospital, Northwest Ethiopia: A retrospective study. Int J Surg. (2022) 5:e66. 10.1097/GH9.0000000000000066
18.
Haftu H Hailu T Medhaniye A G/tsadik T . Assessment of pattern and treatment outcome of patients admitted to pediatric intensive care unit, Ayder Referral Hospital, Tigray, Ethiopia, 2015. BMC Res Notes. (2018) 11:339. 10.1186/s13104-018-3432-4
19.
Bacha T Tsegaye N Tuli W . Characteristics and outcomes of mechanically ventilated pediatric patients in a Tertiary Referral Hospital, Addis Ababa, Ethiopia: Cross sectional study. Ethiop J Health Sci. (2021) 31:915–24. 10.4314/ejhs.v31i5.2
20.
Abebe T Girmay MGGM Tesfaye M . The epidemiological profile of pediatric patients admitted to the general intensive care unit in an Ethiopian University Hospital. Int J General Med. (2015) 8:63–7. 10.2147/IJGM.S76378
21.
Teshager NW Amare AT Tamirat KS Zemene MA . Wasting and associated factors among critically ill children admitted to pediatric intensive care unit in Ethiopia. BMC Nutr. (2022) 8:11. 10.1186/s40795-022-00506-x
22.
El Halal MG Barbieri E Filho RM Trotta Ede A Carvalho PR . Admission source and mortality in a pediatric intensive care unit. Indian J Crit Care Med. (2012) 16:81–6. 10.4103/0972-5229.99114
23.
Daher AH Al-Ammouri I . All-cause mortality in a pediatric intensive care unit at a teaching hospital in Amman, Jordan. Pediatr Int. (2021) 64:e14940. 10.1111/ped.14940
24.
Nupen TL Argent AC Morrow B . Characteristics and outcome of long-stay patients in a paediatric intensive care unit in Cape Town, South Africa. S Afr Med J. (2016) 107:70–5. 10.7196/SAMJ.2017.v107i1.11279
25.
Parasher V Shaha S Khatri R Yadav S Das S Mittal U . Pattern of admission and clinical outcome of patients admitted in pediatric intensive care unit of a rural tertiary health care centre. Int J Contemp Pediatr. (2021) 8:849. 10.18203/2349-3291.ijcp20211675
26.
Burns JP Sellers DE Meyer EC Lewis-Newby M Truog RD . Epidemiology of death in the PICU at five US teaching hospitals. Crit Care Med. (2014) 42:2101–8. 10.1097/CCM.0000000000000498
27.
Campos-Miño S Sasbón JS von Dessauer B . Pediatric intensive care in Latin America. Med Intensiva. (2012) 36:3–10. 10.1016/j.medine.2012.02.004
28.
Verlaat CW Visser IH Wubben N Hazelzet JA Lemson J van Waardenburg D et al . Factors associated with mortality in low-risk pediatric critical care patients in the Netherlands. Pediatr Crit Care Med. (2017) 18:e155–e61. 10.1097/PCC.0000000000001086
29.
Tesema HG Lema GF . Patterns of admission and clinical outcomes among patients admitted to medical intensive care unit of a Teaching and Referral Hospital, Northwest Ethiopia. Glob Adv Health Med. (2021) 10:2164956121989258. 10.1177/2164956121989258
30.
Valavi E Aminzadeh M Shirvani E Jaafari L Madhooshi S . The main causes of mortality in pediatric intensive care unit in South West of Iran. Zahedan J Res Med Sci. (2018) 2018:63006. 10.5812/zjrms.63006
31.
Verlaat CW Wubben N Visser IH Hazelzet JA van Waardenburg D van Dam NA et al . Retrospective cohort study on factors associated with mortality in high-risk pediatric critical care patients in the Netherlands. BMC Pediatr. (2019) 19:274. 10.1186/s12887-019-1646-9
32.
Knettel BA Knettel CT Sakita F Myers JG Edward T Minja L et al . Predictors of ICU admission and patient outcome for traumatic brain injury in a Tanzanian referral hospital: Implications for improving treatment guidelines. Injury. (2022) 53:1954–60. 10.1016/j.injury.2022.03.043
33.
Fathi M Moghaddam NM Balaye Jame SZ Darvishi M Mortazavi M . The association of Glasgow Coma Scale score with characteristics of patients admitted to the intensive care unit. Informat Med Unlocked. (2022) 29:100904. 10.1016/j.imu.2022.100904
34.
Netto AL Muniz VM Zandonade E Maciel EL Bortolozzo RN Costa NF et al . Performance of the Pediatric Index of Mortality 2 in a pediatric intensive care unit. Revista Brasileira de terapia intensiva. (2014) 26:44–50. 10.5935/0103-507X.20140007
35.
Esper AM Martin GS . The impact of comorbid [corrected] conditions on critical illness. Crit Care Med. (2011) 39:2728–35. 10.1097/CCM.0b013e318236f27e
36.
Rusmawatiningtyas D Rahmawati A Makrufardi F Mardhiah N Murni IK Uiterwaal CSPM et al . Factors associated with mortality of pediatric sepsis patients at the pediatric intensive care unit in a low-resource setting. BMC Pediatr. (2021) 21:471. 10.1186/s12887-021-02945-0
37.
Gao F Zhang Y . Inotrope use and intensive care unit mortality in patients with cardiogenic shock: An analysis of a large electronic intensive care unit database. Front Cardiovasc Med. (2021) 8:696138. 10.3389/fcvm.2021.696138
Summary
Keywords
pediatric, mortality, intensive care, factors, Ethiopia
Citation
Molla MT, Endeshaw AS, Kumie FT and Lakew TJ (2023) The magnitude of pediatric mortality and determinant factors in intensive care units in a low-resource country, Ethiopia: a systematic review and meta-analysis. Front. Med. 10:1117497. doi: 10.3389/fmed.2023.1117497
Received
06 December 2022
Accepted
15 March 2023
Published
17 April 2023
Volume
10 - 2023
Edited by
Ata Murat Kaynar, School of Medicine, University of Pittsburgh, United States
Reviewed by
Stefan Irschik, Medical University of Vienna, Austria; Shashikanth Ambati, Albany Medical College, United States
Updates
Copyright
© 2023 Molla, Endeshaw, Kumie and Lakew.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Misganew Terefe Molla misganterefe@gmail.com
This article was submitted to Intensive Care Medicine and Anesthesiology, a section of the journal Frontiers in Medicine
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.