Abstract
Background:
Physicians usually consider that sodium bicarbonate (SB) infusion can be used for metabolic acidosis; however, there is little evidence available to assess its effect on hospital mortality in large AKI cohorts. Here, we investigated the effect of SB infusion in patients with AKI complicated by metabolic acidosis.
Method:
Patients with AKI complicated by metabolic acidosis were screened from the MIMIC-IV database. A propensity score analysis (PSA) was used to decrease baseline differences in the probability of receiving SB. The marginal structural Cox model (MSCM) was employed to adjust for both baseline and time-varying confounding factors.
Results:
A total of 1853 patients with AKI complicated with metabolic acidosis were included in our study. A total of 390 pairs of patients were divided into an SB infusion group and a non-SB infusion group. The SB infusion group had more serious and worse laboratory indicators, including lower pH [7.19 (0.11) vs. 7.26 (0.07)] and bicarbonate concentration (BC) [12.36 (4.26) vs. 15.96 (3.25) mmol/l]. While there was no significant effect on overall hospital mortality in AKI patients complicated with metabolic acidosis (p = 0.056), SB infusion was observed to have beneficial correlation on hospital mortality in patients with high AG acidosis (AG > 18 mmol/L) (p = 0.012). Similar results were replicated with the MSCM.
Conclusion:
We found that SB infusion in AKI patients with metabolic acidosis is not beneficial for hospital mortality. However, SB infusion for AKI patients and high AG metabolic acidosis significantly improved hospital mortality. Further larger randomized controlled trials are needed to confirm these results.
Introduction
Over the past few decades, the incidence of acute kidney injury (AKI) has increased, and it is a common complication in patients admitted to intensive care units (ICUs), and is closely associated with adverse outcomes such as prolonged ICU and hospital stay, development of chronic kidney disease (CKD), and increased risk of short-and long-term mortality (1–3). In ICUs, the probability of AKI leading to death is up to 50% (4).
AKI is not a single disease, but a syndrome consisting of multiple clinical conditions. The prognosis of AKI depends on the underlying disease, the severity and duration of renal impairment, the patient’s renal baseline condition, and the treatment status (5). Fluids are one of the most commonly used therapies for critically ill patients and represent the cornerstone of hemodynamic management in ICUs. The use of fluids to optimize hemodynamics during the perioperative and early stages of sepsis has been shown to improve patient outcomes (6). On the other hand, liberal administration of fluids may lead to a positive fluid balance, and recent observational studies have demonstrated an association between positive fluid balance, renal non-recovery, and mortality in children and adults with AKI (7).
Acidosis is the most common acid–base disturbance seen in AKI, and recent studies have shown that AKI with metabolic acidosis potentially indicates a more severe course and worse outcome, including high mortality and increased length of stay in the hospital and ICU (8). On the one hand, AKI can cause metabolic acidosis; on the other hand, accumulating evidence identifies metabolic acidosis not only as a consequence of, but also as a contributor to the progression of kidney dysfunction (9). Anion gap (AG), an indicator that reflects the unmeasured anion concentration, is applied to detect and evaluate the presence and severity of metabolic acidosis. While AKI has been investigated widely for hospital mortality, AKI in association with metabolic acidosis has been less well studied.
Sodium bicarbonate (SB) infusion is mostly administered to treat severe metabolic acidosis. However, it is controversial whether SB should be used and which dosage should be used in clinical practice (10, 11). A retrospective observational study revealed that SB infusion may reduce ICU mortality in septic patients who presented with AKI stage 2 or 3 (12). Therefore, we hypothesized that early sodium bicarbonate infusion may be able to correct acidosis and halt its progression, thereby mitigating the risk of additional renal damage and resulting in lower mortality in patients with AKI.
Materials and methods
Source of data
This study was conducted by collecting data from a real-world and publicly available clinical database named the Multiparameter Intelligent Monitoring in Intensive Care Database IV (MIMIC IV), which included more than 60,000 ICU patients treated at Beth Israel Deaconess Medical Center (Boston, MA) from 2008 to 2019, as previously described (13). One author, (Yunting Wang), had access to the database and was responsible for data extraction (certification ID: 41733658). Because the database here had already been approved by the institutional review board (IRB) of the Massachusetts Institute of Technology (MIT), exemption from additional institutional IRB approval was allowed (14).
Participants and variables
The inclusion criteria were patients (1) diagnosed with AKI; (2) with metabolic acidosis with pH < 7.3 and bicarbonate <20 mmoL/L; and (3) who did not have respiratory acidosis (PaCO2 < 50 mmHg) (12). The minimum values were used for BC and pH, and the maximum value was used for PaCO2 within 48 h after ICU entry. In this study, all adult patients met the criteria for AKI within 48 h after ICU admission according to the Kidney Disease Improving Global Outcomes (KDIGO) clinical practice guidelines (15), and both urine output and creatinine were used to define AKI stages. If patients were admitted multiple times, only the first stay was analysed. Patients aged <18 years old and those who were discharged or died within 48 h after ICU admission were excluded.
We extracted clinical data within 24 h after admission to the ICU, including age, sex, mechanical ventilation, and sequential organ failure assessment (SOFA) score. In addition, laboratory data, including chloride, potassium, sodium, lactate, creatinine, and blood urea nitrogen (BUN), were included. If a variable was measured more than once in the first 24 h, the value associated with the greatest severity of illness was used. Because missing data may create bias, variables with >70% missing values were excluded from further analysis. Other variables with a lesser degree of missing values were analysed using the multiple imputation method (16).
The primary outcome was patient mortality in the hospital and ICU. Both were identified as the outcomes of patient survival on discharge from the hospital and ICU.
Statistical analysis
According to whether patients were infused with SB 48 h after ICU entry, we divided the investigated cohort into two groups: the intervention (SB) group and the control (non-SB) group. Continuous variables are expressed as the mean and standard deviation (SD) and interquartile ranges (IQR). The chi-square test or Fisher’s exact test was used to test comparisons between the groups for categorical variables, whereas the t test or Mann–Whitney U test was used for comparisons of continuous variables, as appropriate. Categorical variables are presented as numbers and proportions (%). All statistical analyses were performed by the R package (version 3.6.3). p values <0.05 were considered statistically significant for all analyses.
We used propensity score analysis (PSA) to account for the baseline differences in the probability of receiving SB or not within 48 h after ICU entry so that covariate imbalance between the SB and no SB groups was minimized (17). The standardized mean difference (SMD) was calculated and was significantly smaller after group matching. A Cox regression model was used to adjust for residual imbalance by including parameters with statistically significant p value and based on clinical expertise advice of any potential confounders.
Marginal structural Cox models (MSCM) provide the time-dependent relation between a time-varying variable (SB treatment) and a survival outcome during hospitalization after ICU admission. Age, sex, mechanical ventilation, total fluid input, vasopressor, BUN, creatinine, urine output, SOFA score, anion gap (AG), and sodium and potassium levels were obtained in the first 24 h after ICU admission as potential baseline variables. BC, PaCO2, lactate and PH were used as time-varying variables in the entire ICU period. Inverse probability weighting estimation in R and the “ipw” package. Were performed on MSCM parameters to correct confounding and selection bias formed by informative censoring.
Results
We identified AKI adult patients according to the KDIGO criteria, and after including only adult patients’ first ICU admissions, 1853 AKI patients with metabolic acidosis 48 h after ICU admission from the MIMIC-IV database were included in our study. Among the study cohort, 614 patients received SB treatment, and 1,239 patients did not receive SB treatment in the first 48 h after entering the ICU department (Figure 1).
Figure 1
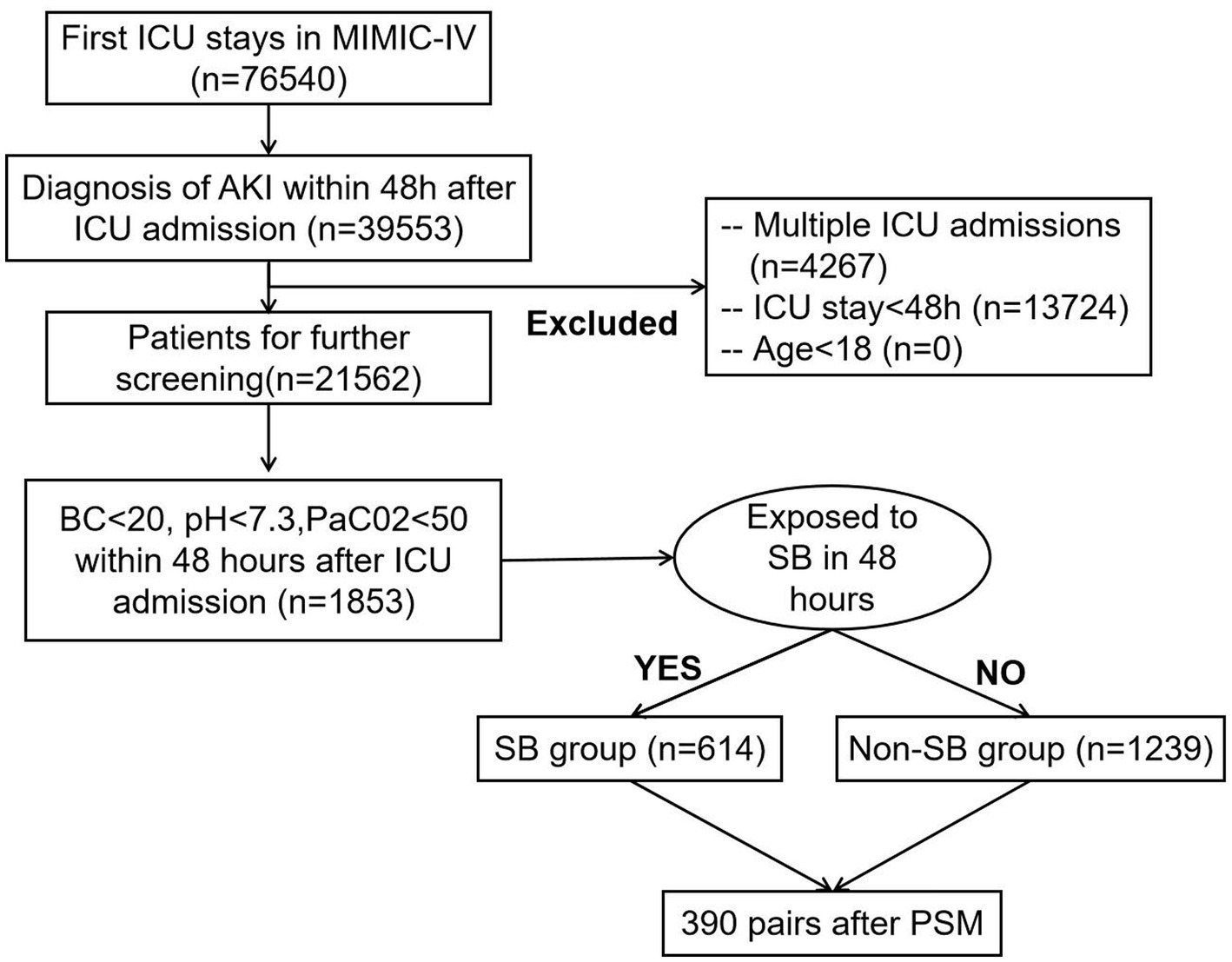
Study cohort selection based on the inclusion and exclusion criteria.
The baseline characteristics of the SB treatment group and non-SB treatment group before and after PSA matching are shown in Table 1. The SB treatment group had a more serious situation than the non-SB group. The SB treatment group had significantly higher severity scores on admission [SOFA 9.0 (7.0, 11.0) vs. 7.0 (5.0, 9.0)]. A larger proportion of the SB patients received vasopressors (36.5% vs. 17.1%) during the first 24 h of their ICU stay, but there were few differences in mechanical ventilation. In the first 24 h of admission, PH [7.19 (0.11) vs. 7.26 (0.07)], BC [12.36 (4.26) vs. 15.96 (3.25) mmol/L] and urine output [684.00 (264.25, 1399.25) vs. 1000.00 (561.00, 1667.00) mL] were significantly lower in the SB group. On the first day, fluid input [3825.00 (2081.25, 6257.50) vs. 2300.00 (1100.50, 3922.50) mL] and anion gap [24.23 (7.79) vs. 19.89 (5.82)] was significantly higher in the SB treatment group. Renal function, including creatinine [2.60 (1.60, 4.10) vs. 1.60 (1.10, 2.70) mg/dL] and BUN [42.00 (26.00, 67.00) vs. 32.00 (20.00, 51.50) mmol/L], was more serious in the SB treatment group.
Table 1
| Original cohort | Matched cohort | |||||||
|---|---|---|---|---|---|---|---|---|
| Non-SB | SB | SMD | p | Non-SB | SB | SMD | p | |
| n | 1,239 | 614 | 390 | 390 | ||||
| Age | 66.66 (15.91) | 64.62 (15.61) | 0.130 | 0.009 | 66.55 (15.52) | 65.51 (15.77) | 0.067 | 0.351 |
| Gender (Female) | 559 (45.1) | 299 (48.7) | 0.072 | 0.151 | 191 (49.0) | 185 (47.4) | 0.031 | 0.72 |
| SOFA score | 7.0 (5.0,9.0) | 9.0 (7.0,11.0) | 0.636 | <0.001 | 8.00 [6.00, 10.00] | 8.00 [6.00, 10.00] | 0.032 | 0.596 |
| Mechanical ventilation | 1,014 (81.8) | 482 (78.5) | 0.084 | 0.091 | 81 (20.8) | 81 (20.8) | <0.001 | 1 |
| Vasopressor | 212 (17.1) | 224 (36.5) | 0.448 | <0.001 | 96 (24.6) | 96 (24.6) | <0.001 | 1 |
| Urine output | 1000.00 (561.00, 1667.00) | 684.00 (264.25, 1399.25) | 0.134 | <0.001 | 850.50 [420.00, 1436.75] | 819.50 [335.00, 1543.75] | 0.03 | 0.796 |
| AKI stage, n (%) | 0.466 | <0.001 | 0.061 | 0.707 | ||||
| 1 | 243 (19.6) | 72 (11.7) | 50 (12.8) | 54 (13.8) | ||||
| 2 | 514 (41.5) | 164 (26.7) | 139 (35.6) | 128 (32.8) | ||||
| 3 | 482 (38.9) | 378 (61.6) | 201 (51.5) | 208 (53.3) | ||||
| Fluid input | 2300.00 (1100.50, 3922.50) | 3825.00 (2081.25, 6257.50) | 0.59 | <0.001 | 2829.00 [1484.25, 4748.25] | 2999.50 [1735.75, 5037.50] | 0.015 | 0.363 |
| Lactate | 3.86 (2.78) | 5.93 (4.72) | 0.535 | <0.001 | 4.53 (3.34) | 4.63 (3.74) | 0.027 | 0.708 |
| PH | 7.26 (0.07) | 7.19 (0.11) | 0.717 | <0.001 | 7.23 (0.09) | 7.23 (0.09) | 0.02 | 0.781 |
| PCO2 | 41.56 (5.78) | 38.98 (7.69) | 0.378 | <0.001 | 39.97 (6.63) | 40.25 (6.88) | 0.04 | 0.574 |
| Bicarbonate | 15.96 (3.25) | 12.36 (4.26) | 0.949 | <0.001 | 14.11 (3.64) | 14.12 (3.81) | 0.004 | 0.951 |
| BUN | 32.00 (20.00,51.50) | 42.00 (26.00,67.00) | 0.382 | <0.001 | 38.00 [24.25, 64.00] | 39.00 [25.00, 63.00] | 0.01 | 0.743 |
| Creatinine | 1.60 (1.10,2.70) | 2.60 (1.60,4.10) | 0.284 | <0.001 | 2.00 [1.40, 3.30] | 2.40 [1.50, 3.80] | 0.018 | 0.014 |
| Anion gap | 19.89 (5.82) | 24.23 (7.79) | 0.631 | <0.001 | 21.76 (6.54) | 22.28 (6.92) | 0.077 | 0.283 |
Comparison of the basic covariates between the original cohort and the adjusted cohort.
After propensity score analysis, we matched 390 pairs of SB treatment and non-SB treatment patients in subsequent studies. The imbalance of variables was reduced, and all variables had an SMD value <0.1. In our study, SB infusion was not associated with improved mortality in all AKI patients after PSA matching (p = 0.056). However, SB infusion is associated with beneficial mortality in AKI patients with high AG metabolic acidosis (p = 0.012), as shown in Table 2. Our further study found that the use of SB was an important factor correlating with the mortality outcome in AKI patients with high AG acidosis (p = 0.021), as shown in Table 3.
Table 2
| Groups | HR | Lower.95 | Upper.95 | p |
|---|---|---|---|---|
| Overall population | 0.85 | 0.71 | 1.00 | 0.056 |
| AKI stage 1 (n = 104) | 0.71 | 0.44 | 1.14 | 0.159 |
| AKI stage 2 (n = 267) | 1.05 | 0.80 | 1.39 | 0.725 |
| AKI stage 3 (n = 409) | 0.79 | 0.61 | 1.02 | 0.065 |
| AG>18 (n = 529) | 0.76 | 0.61 | 0.94 | 0.012 |
Relation of SB use and hospital mortality in the overall and subgroups using Cox proportional hazard model analysis.
Table 3
| Variables | HR | Lower.95 | Upper.95 | p |
|---|---|---|---|---|
| Use of SB | 0.77 | 0.62 | 0.96 | 0.021 |
| Age | 1.01 | 1.00 | 1.02 | 0.021 |
| PH minimum | 0.48 | 0.14 | 1.61 | 0.236 |
| PaCO2 max | 0.99 | 0.98 | 1.01 | 0.522 |
| BC min | 0.96 | 0.93 | 1.00 | 0.074 |
| Ventilation | 1.07 | 0.81 | 1.40 | 0.649 |
| Urine output | 1.00 | 1.00 | 1.00 | 0.372 |
| BUN | 1.00 | 1.00 | 1.00 | 0.439 |
| Creatinine | 1.01 | 0.99 | 1.03 | 0.580 |
| Lactate max | 0.95 | 0.92 | 0.98 | 0.002 |
| Total fluid input | 1.00 | 1.00 | 1.00 | 0.766 |
Cox regression model after propensity score matching in AKI patients with AG>18.
In our study, variables could be estimated using inverse probability weighting (IPW) to correct both for confounding and for forms of selection bias (Figure 2). PH, BC and lactate were the most important predicting variables of SB use; among them, pH ((for each 0.1) increase, p < 0.001), BC (for each 5 mmoL/L increase, p < 0.001) and lactate (for each 1 increase, p = 0.002), as time-varying variables, all have significance (Table 4). Our results revealed that SB treatment was not associated with improving hospital mortality in the overall cohort of patients (p = 0.179). MSCM showed that AKI stage 1 to 3 patients had a less significant relationship between SB use and mortality (AKI phase 1, p = 0.126; AKI phase 2, p = 0.131; AKI phase 3, p = 0.106). SB use still closely correlated with the improving outcome of the AKI patients with high AG metabolic acidosis (HR:0.88, p = 0.045) as shown in Table 5.
Figure 2
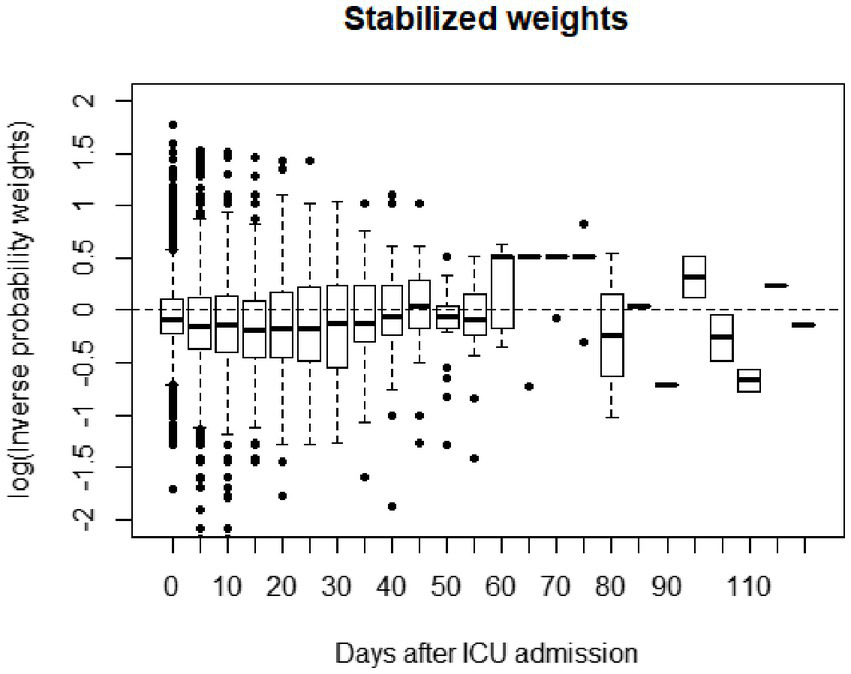
Weight distribution plot for the inverse probability weights that were used to adjust for confounding.
Table 4
| Odds ratio | Lower 95% CI | Upper 95% CI | p value | |
|---|---|---|---|---|
| Gender (male as reference) | 0.90 | 0.75 | 1.08 | 0.244 |
| Age with 10 years increase | 0.99 | 0.93 | 1.05 | 0.721 |
| Mechanical ventilation | 1.04 | 0.84 | 1.30 | 0.699 |
| Fluid input with 1,000 increase | 1.03 | 0.99 | 1.06 | 0.122 |
| Urine output with 1,000 increase | 1.05 | 0.96 | 1.14 | 0.294 |
| pH with 0.1 increase | 0.53 | 0.45 | 0.61 | <0.001 |
| Vasopressor | 0.74 | 0.60 | 0.92 | 0.006 |
| Anion gap with 5 increase | 0.91 | 0.84 | 0.99 | 0.022 |
| Lactate with 1 increase | 1.05 | 1.02 | 1.08 | 0.002 |
| BC (mmol/l) with 5 increase | 0.39 | 0.34 | 0.44 | <0.001 |
| PaCO2 (mmHg) with 10 increase | 1.08 | 0.96 | 1.22 | 0.208 |
| Bun with 5 increase | 1.01 | 0.99 | 1.03 | 0.298 |
| Cre with 0.1 increase | 1.00 | 0.99 | 1.00 | 0.225 |
Predictors of the use of sodium bicarbonate infusion at each time point.
Table 5
| Groups | HR | Lower.95 | Upper.95 | p |
|---|---|---|---|---|
| Overall population | 0.92 | 0.82 | 1.04 | 0.179 |
| AKI stage 1 | 0.77 | 0.55 | 1.08 | 0.126 |
| AKI stage 2 | 1.10 | 0.97 | 1.24 | 0.131 |
| AKI stage 3 | 0.88 | 0.74 | 1.03 | 0.106 |
| AG>18 | 0.86 | 0.74 | 1.00 | 0.045 |
Results of marginal structural Cox model in overall population and subgroups.
By considering 48 h SB volumes, the results showed that receiving 800–1,600 mL was associated with reduced risk of mortality as compared with the non-SB group (HR 0.56; 95% CI 0.31–0.99; p = 0.045). Beneficial effect was not observed in the small (dose <400 mL) and large volume (dose >1,600 mL) groups (Table 6).
Table 6
| HR | Lower.95 | Upper.95 | p | |
|---|---|---|---|---|
| 48 h SB volume (Non-SB group as reference)* | ||||
| SB < 400 mL | 1.28 | 0.97 | 1.69 | 0.079 |
| 400–800 mL | 0.93 | 0.68 | 1.27 | 0.656 |
| 800 to 1,600 mL | 0.56 | 0.31 | 0.99 | 0.045 |
| >1,600 mL | 0.52 | 0.13 | 2.11 | 0.363 |
Dose–response relationship between SB volume and survival benefits in AKI patients with metabolic acidosis.
Discussion
The present study focused on the effect of SB infusion on hospital mortality in AKI patients with metabolic acidosis. In our study, SB infusion was verified to not benefit all-stage AKI patients. But the improving hospital mortality of the AKI patients with high AG metabolic acidosis was associated with SB infusion; Previous studies have confirmed that high AG is an important predictor of all-cause death (18, 19), and the rate of patients with elevated AG requiring admission to the ICU and the mortality rate were significantly higher (20). Another study suggested that the risk of death of AKI patients within 28 days during hospitalization in the ICU was increased when AG ≥14 mmol/L (21).
The metabolic acidoses are readily subdivided into those with a large AG (HAGMA) and those with a normal AG (by definition the hyperchloremic metabolic acidoses). When HAGMA exists, the reciprocal relationship between the amount of increase of [AG] and decrease in [HCO3−] (designated as the Δ [AG]/Δ[HCO3−] can be a very helpful indicator of certain forms of mixed acid–base disorders (22)).
When HAGMA occurs, the ratio of Δ[AG] to Δ[HCO3-] is disrupted and the acid–base balance of the body is impaired. Infusion of SB provided a weak base and was able to correct the acidosis by adding bicarbonate base. The results of this study further confirm that SB infusion improves hospital mortality in AKI patients with high AG metabolic acidosis.
This study used PSM and MSCM and considered the effect of baseline and time-varying confounders. PH, PaCO2, lactate and BC were examined as time-varying factors. SB infusion and pH, PaCO2, lactate and BC are an interacting and dynamically changing relationship throughout the course of medical care, and the use of MSCM, can effectively minimize the effects of these confounding factors. Previous studies have confirmed that the MSCM model can be used for the observation and analysis of time variables and outcomes (23, 24).
In our study, SB infusion was verified to not benefit all-stage AKI patients. But the improving hospital mortality of the AKI patients with high AG metabolic acidosis was associated with SB infusion. This study also has some limitations, as an observational single-center study that retrospectively reviewed electronic health record (EHR) data, the potential for residual confounding by uncaptured variables in the EHR and the generalizability of the findings to other institutions require further investigation. Second, we used PSM and MSCM to balance important confounders, but residual confounders could not be completely excluded. Finally, we hope to explore this in some prospective trials and conduct further randomized controlled trials to confirm the results of this study.
Conclusion
In conclusion, we found that the use of SB infusion in AKI patients complicated with metabolic acidosis has little association on hospital mortality. At the same time, we also found that timely use of SB for AKI patients with high AG acidosis significantly correlated with improving hospital mortality. Further larger randomized controlled trials are needed to confirm these results.
Statements
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Massachusetts Institute of Technology (Cambridge, MA) and Beth Israel Deaconess Medical Center (Boston, MA). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants' legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
YW: Data curation, Methodology, Writing – original draft, Writing – review & editing. LC: Data curation, Writing – review & editing. GG: Data curation, Writing – review & editing. YG: Methodology, Writing – review & editing. HG: Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. Funding from the Innovation project for doctoral students of the First Affiliated Hospital of Chongqing Medical University (CYYY-BSYJSCXXM-202229).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
Al-Jaghbeer M Dealmeida D Bilderback A Ambrosino R Kellum JA . Clinical decision support for in-hospital AKI. J Am Soc Nephrol. (2017) 29:654–60. doi: 10.1681/ASN.2017070765
2.
Hoste EA Bagshaw SM Bellomo R Cely CM Colman R Cruz DN et al . Epidemiology of acute kidney injury in critically ill patients: the multinational AKI-EPI study. Intensive Care Med. (2015) 41:1411–23. doi: 10.1007/s00134-015-3934-7
3.
Marco F Tohme FA Shu W Raghavan M Angus DC Kellum JA et al . Long-term survival in patients with septic acute kidney injury is strongly influenced by renal recovery. PLoS One. (2018) 13:e198269. doi: 10.1371/journal.pone.0198269
4.
Singbartl K Kellum J . AKI in the ICU: definition, epidemiology, risk stratification, and outcomes. Kidney Int. (2012) 81:819–25. doi: 10.1038/ki.2011.339
5.
Zhang C . From AKI to CKD: maladaptive repair and the underlying mechanisms. Int J Mol Sci. (2022) 23:10880. doi: 10.3390/ijms231810880
6.
Cecconi M Hofer C Teboul JL Pettila V Wilkman E Molnar Z et al . Fluid challenges in intensive care: the FENICE study: a global inception cohort study. Intensive Care Med. (2015) 41:1529–37. doi: 10.1007/s00134-015-3850-x
7.
Grams M Estrella MM Coresh J Brower RG Liu KD National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome Network . Fluid balance, diuretic use, and mortality in acute kidney injury. Clin J Am Soc Nephrol. (2011) 6:966–73. doi: 10.2215/CJN.08781010
8.
Silva Júnior G Daher EDF Mota RMS Menezes FA . Risk factors for death among critically ill patients with acute renal failure. Rev Paul Med. (2006) 124:257–63. doi: 10.1590/S1516-31802006000500004
9.
Hu J Wang Y Geng X Chen R Xu X Zhang X et al . Metabolic acidosis as a risk factor for the development of acute kidney injury and hospital mortality. Exp Ther Med. (2017) 13:2362–74. doi: 10.3892/etm.2017.4292
10.
Parker M Parshuram C . Sodium bicarbonate use in shock and cardiac arrest: attitudes of pediatric acute care physicians. Crit Care Med. (2013) 41:2188–95. doi: 10.1097/CCM.0b013e31828a6669
11.
Fujii T Udy AA Nichol A Bellomo R Deane AM El-Khawas K et al . Incidence and management of metabolic acidosis with sodium bicarbonate in the ICU: an international observational study. Crit Care. (2021) 25:45.
12.
Zhang Z Zhu C Mo L Hong Y . Effectiveness of sodium bicarbonate infusion on mortality in septic patients with metabolic acidosis. Intensive Care Med. (2018) 44:1888–95. doi: 10.1007/s00134-018-5379-2
13.
Yang R Huang T Shen L Feng A Li L Li S et al . The use of antibiotics for ventilator-associated pneumonia in the MIMIC-IV database. Front Pharmacol. (2022) 13:869499. doi: 10.3389/fphar.2022.869499
14.
Nicholls SG Quach P von Elm E Guttmann A Moher D Petersen I et al . The REporting of studies conducted using observational routinely-collected health data (RECORD) statement: methods for arriving at consensus and developing Reporting guidelines. PLoS One. (2015) 10:e0125620. doi: 10.1371/journal.pone.0125620
15.
Kellum JA Lameire N Aspelin P Barsoum RS Burdmann EA Goldstein SL et al . Kidney disease: improving global outcomes (KDIGO) acute kidney injury work group. KDIGO clinical practice guideline for acute kidney Injury. Kidney Int Suppl. (2012) 1:1–138. doi: 10.1038/kisup.2012.1
16.
Zhang Z . Multiple imputation with multivariate imputation by chained equation (MICE) package. Ann Transl Med. (2016) 4:30. doi: 10.3978/j.issn.2305-5839.2015.12.63
17.
Zhang Z . Propensity score method: a non-parametric technique to reduce model dependence. Ann Transl Med. (2016) 5:7. doi: 10.21037/atm.2016.08.57
18.
Cheng B Li D Gong Y Ying B Wang B . Serum anion gap predicts all-cause mortality in critically ill patients with acute kidney injury: analysis of the MIMIC-III database. Dis Markers. (2020) 2020:6501272. doi: 10.1155/2020/6501272
19.
Zhong L Xie B Ji XW Yang XH . The association between albumin corrected anion gap and ICU mortality in acute kidney injury patients requiring continuous renal replacement therapy. Intern Emerg Med. (2022) 17:2315–22. doi: 10.1007/s11739-022-03093-8
20.
Mitra B Roman C Charters KE O'Reilly G Gantner D Cameron PA . Lactate, bicarbonate and anion gap for evaluation of patients presenting with sepsis to the emergency department: a prospective cohort study. Emerg Med Australas. (2020) 32:20–4. doi: 10.1111/1742-6723.13324
21.
Jiang L Wang Z Wang L Liu Y Chen D Zhang D et al . Predictive value of the serum anion gap for 28-day in-hospital all-cause mortality in sepsis patients with acute kidney injury: a retrospective analysis of the MIMIC-IV database. Ann Transl Med. (2022) 10:1373. doi: 10.21037/atm-22-5916
22.
Fenves A Emmett M . Approach to patients with high anion gap metabolic acidosis: Core curriculum 2021. Am J Kidney Dis. (2021) 78:590–600. doi: 10.1053/j.ajkd.2021.02.341
23.
Karim ME Gustafson P Petkau J Zhao Y Shirani A Kingwell E et al . Marginal structural cox models for estimating the association between β-interferon exposure and disease progression in a multiple sclerosis cohort. Am J Epidemiol. (2014) 180:160–71. doi: 10.1093/aje/kwu125
24.
Dupuis C Garrouste-Orgeas M Bailly S Adrie C Goldgran-Toledano D Azoulay E et al . Effect of transfusion on mortality and other adverse events among critically ill septic patients: an observational study using a marginal structural cox model. Crit Care Med. (2017) 45:1972–80. doi: 10.1097/CCM.0000000000002688
Summary
Keywords
AKI, metabolism acidosis, sodium bicarbonate, hospital mortality, MIMIC
Citation
Wang Y, Chen L, Guo G, Gao Y and Gan H (2023) Effect of sodium bicarbonate infusion on hospital mortality in acute kidney injury patients with metabolic acidosis. Front. Med. 10:1268252. doi: 10.3389/fmed.2023.1268252
Received
27 July 2023
Accepted
25 September 2023
Published
12 October 2023
Volume
10 - 2023
Edited by
Zhongheng Zhang, Sir Run Run Shaw Hospital, China
Reviewed by
Khushleen Jaggi, San Mateo Medical Center, United States; Marco Fiorentino, University of Bari Aldo Moro, Italy
Updates
Copyright
© 2023 Wang, Chen, Guo, Gao and Gan.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hua Gan, ghzxgcqckd@163.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.