Abstract
Acrodermatitis enteropathica (AE, OMIM 201100) is a rare autosomal recessive dermatosis characterized by periorificial dermatitis, diarrhea, alopecia, and hypozincaemia due to pathogenic variants of SLC39A4. Herein, we present a case series describing four unrelated patients with AE from Han, Yi, and Tibetan ethnicities in Sichuan region of southwestern China, speculate the hotspot variants of SLC39A4 causing AE in Sichuan region and highlight physicians should be alerted to unusual presentations of AE, such as the absence of hypozincaemia and the presence of acne-like lesions. Serum alkaline phosphatase and genetic testing should be considered to accurately evaluate the zinc deficiency in human body and help make the correct diagnosis.
1 Introduction
Acrodermatitis enteropathica (AE, OMIM 201100) is a rare autosomal recessive skin disease characterized by periorificial dermatitis, diarrhea, and alopecia. It is usually associated with hypozincaemia due to the defect in ZIP4 zinc transporter encoded by SLC39A4. Two Tibetan patients with AE from Sichuan region of southwestern China had been previously reported by our group (1, 2). Herein, we added another four patients from Han, Yi, and Tibetan families in Sichuan region and reported the unusual presentations in AE.
2 Case reports
2.1 Case 1
An 18-year-old man, born to non-consanguineous, healthy Han parents, presented with papules and pustules on the face and extremities since the age of 4 years. Physical examination revealed erythema, papules, pustules, crusts and scars on the face, trunk and periorificial region (Figures 1A,B). Diarrhea and hair loss were absent. He was repeatedly diagnosed with “acne” in local hospitals, but the anti-acne treatment with minocycline achieved no improvement. The serum zinc level was 103.8 μmol/L (normal 76.5–170.0 μmol/L), while the serum alkaline phosphatase level was only 41 IU/L (lower than the normal range of 45–125 IU/L). Sanger sequencing was performed using the genomic DNA of the patient and his parents. The patient was found to carry a 24-bp heterozygous deletion in exon 9 and intron 9 (c.1452_1474 + 1del TGAGCCCAGGAGACTGAGCCCAGG) and a heterozygous splicing variant in intron 7 (c.1288-1G > A) of SLC39A4 (RefSeq NM_130849.4). His father and mother were found to be heterozygous for c.1452_1474 + 1del TGAGCCCAGGAGACTGAGCCCAGG and c.1288-1G > A, respectively (Figure 1C). Thus, the diagnosis of AE was established. After 7 weeks of continuous treatment with a single oral zinc sulfate (50 mg three times daily), his skin lesions almost completely disappeared (Figures 1D,E) and the serum level of alkaline phosphatase increased to 90 IU/L.
Figure 1

Clinical manifestations and variants of SLC39A4 in patient 1 with AE. (A,B) Generalized pustules on the face and trunk prior to the treatment. (C) Heterozygous deletion of TGAGCCCAGGAGACTGAGCCCAGG in exon 9 and the adjoining intron 9 in patient 1 and his father. Heterozygous splicing variant c.1288-1G > A in intron 7 in patient 1 and his mother. (D,E) Marked relief of the lesions after 7 weeks of zinc supplementation.
2.2 Case 2
The patient was a girl aged 1 year and 10 months, the fourth child of second-degree consanguineous parents with Yi ethnicity (Figure 2A; IV: 4). Her parents reported erythema and crusts appeared on her periorificial areas accompanied with alopecia and chronic diarrhea since 4 months after birth. Her older brother had a history of similar lesions and alopecia, but had already died at the age of 3 years (Figure 2A; IV: 3). Physical examination revealed well-demarcated erythema and crusts on her hands, feet, extensor surface of the knees and in the perioral, periocular, perigenital, and perianal regions (Figures 2B–D). Her serum zinc level was 0.13 mg/L (normal 0.76–1.50 mg/L) and the serum alkaline phosphatase level was only 22 IU/L (normal 128–432 IU/L). Sanger sequencing analysis showed the patient carried a homozygous c.295G > A (p.Ala99Thr) in exon 2 of SLC39A4 (RefSeq NM_130849.4) (Figure 2E). Considering the diagnosis of AE, zinc supplementation at 3 mg per kg-body-weight was started, which led to complete remission after 2 weeks.
Figure 2
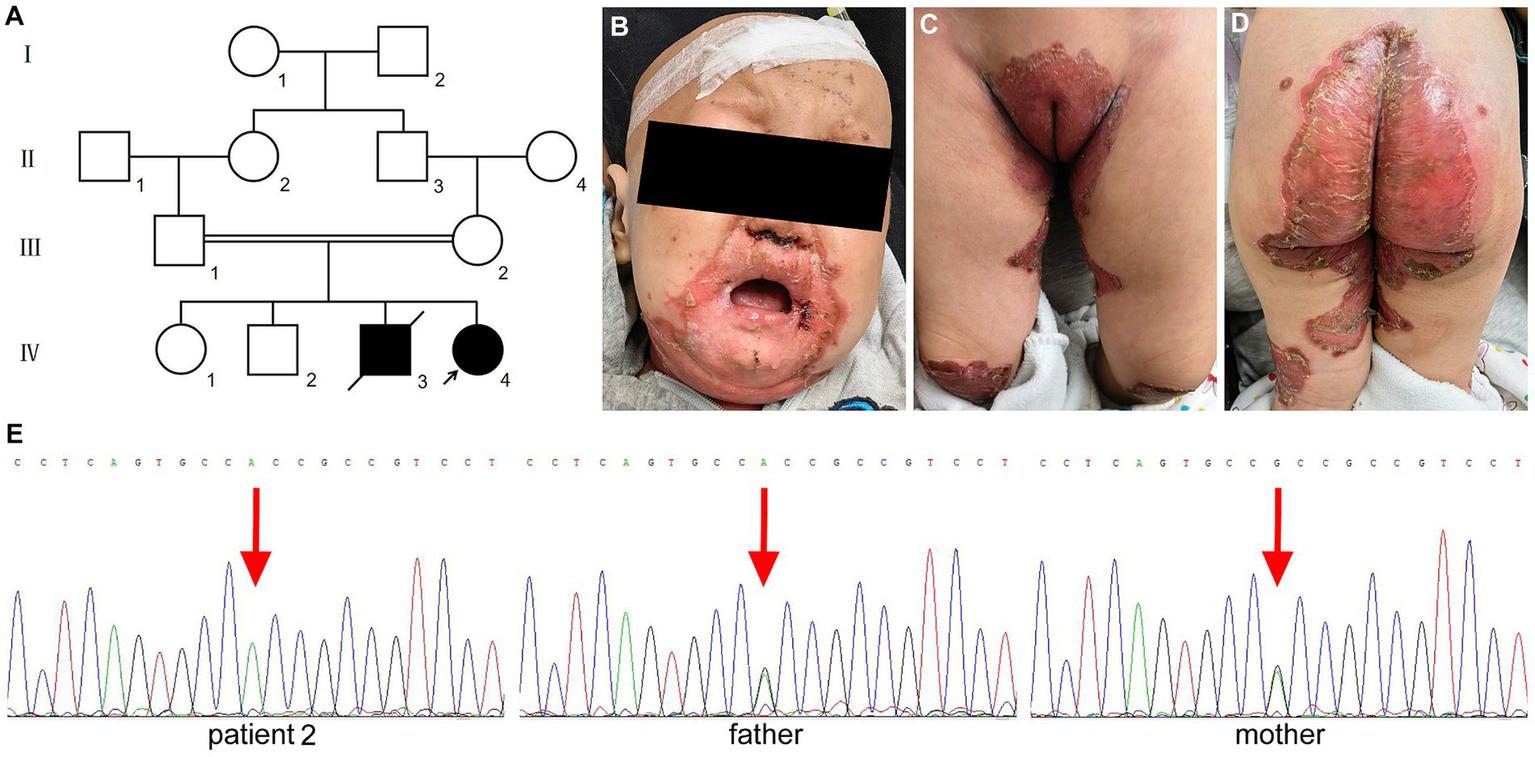
Clinical findings and the variant of SLC39A4 in patient 2 with AE. (A) Pedigree of the Chinese Yi family of patient 2. (B–D) Erythema and crusted lesions in the periorificial region and extensor surface of the knees. (E) Homozygous missense variant of c.295G > A in exon 2 of patient 2 and heterozygous variant for her parents.
2.3 Case 3
An 8-month-old Tibetan boy was referred to our department for evaluation of exanthema on the face and anogenital regions, which had developed approximately 4 months after birth. He had diarrhea, hair loss and irritability. There was no history of any consanguineous marriage in the family. Examination revealed well-demarcated erythema and crusts on the neck, flexor side of the lower extremities and in the perioral, periocular, perigenital, and perianal regions (Figures 3A,B). Laboratory data were within normal limits except for reduced serum zinc 28.44 μmol/L (normal 33.5–84.54 μmol/L). The detection of serum alkaline phosphatase was not performed. Sanger sequencing of SLC39A4 (RefSeq NM_130849.4) revealed that the patient was compound heterozygous for maternal c.1462_1474 + 1del AGACTGAGCCCAGG in exon 9 and intron 9 and paternal c.1110insG in exon 6 (Figure 3C). Both variants have been reported to be pathogenic (1, 3). The patient showed marked improvement after 2 weeks of oral zinc supplements.
Figure 3

(A,B) Clinical findings of patient 3 showed well-demarcated erythema and crusted lesions in the neck, feet, periorificial region, and flexor surface of the lower legs. (C) Heterozygous deletion of AGACTGAGCCCAGG in exon 9 and the adjoining intron 9 of SLC39A4 in patient 3 and his mother. Heterozygous frame-shift variant of c.1110insG in exon 6 of SLC39A4 in patient 3 and his father. (D) Homozygous frame-shift variant of c.1110insG in exon 6 of SLC39A4 in patient 4.
2.4 Case 4
A 10-year-old Tibetan girl presented with eczematous lesions in the perioral, perigenital, and perianal regions accompanied with diarrhea since 7 months after weaning. No alopecia was observed. She had been diagnosed with AE and the skin lesions had been almost disappeared with oral zinc supplements when she came to our department. The patient’s serum zinc level and serum alkaline phosphatase were not detected. No consanguinity was reported in the family. Sanger sequencing of all exons and their flanking intronic regions of SLC39A4 (RefSeq NM_130849.4) identified a homozygous c.1110insG variant in the patient (Figure 3D).
3 Discussion
SLC39A4 have been found to be responsible for the development of AE (1). Pathogenic variants of SLC39A4 would impair the zinc absorption of the ZIP4 transporter in the small intestine, leading to the zinc deficiency, further resulting in various clinical manifestations, such as skin dermatitis, alopecia, diarrhea, growth retardation, and neuropsychiatric symptoms (4). To date, 14 cases with SLC39A4 variants have been found in AE patients from China in the literature, including four cases described here (Table 1) (1–10). Among them, more than half (n = 8, 57.14%) were from Sichuan region of southwestern China, indicating it may be one of the high AE incidence areas. In addition, not all of them simultaneously have the classic triad of skin dermatitis, alopecia, and diarrhea. Growth retardation and neuropsychiatric symptoms were found in a few patients with AE.
Table 1
| Case | Year | Authors | Sex | Age of onset | Origin | History of consanguinity | Family members have similar symptoms | Clinical manifestations | Serum zinc level | Serum alkaline phosphatase level | SLC39A4 variants | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Skin lesions | Alopecia | Diarrhea | Other symptoms | |||||||||||
| 1 | 2008 | Wang et al. (1) | F | 3 months | Sichuan (Tibetan) | Yes | Older brother | Atypical (generalized pustules) | Yes | Yes | No | Low | Low | Homozygous for c.1462_1474 + 1del AGACTGAGCCCAGG (exon 9 and intron 9) |
| 2 | 2010 | Li et al. (5) | F | 5 months | Jiangsu | Yes | No | Typical | No | Yes | No | Low | Not detected | Homozygous for c.1115 T > G (exon 6) |
| 3 | 2014 | Gao et al. (6) | M | Infancy | Jiangsu | No | No | Typical | No | Yes | Growth retardation | Low | Low | Compound heterozygous for c.831G > A (exon 5) and c.1617delA (exon10) |
| 4 | 2016 | Zhou et al. (2) | F | Several months after birth | Sichuan (Tibetan) | Yes | Older brother and sister | Typical | Yes | Yes | No | Low | Not detected | Homozygous for c.1462_1474 + 1del AGACTGAGCCCAGG (exon 9 and intron 9) |
| 5 | 2017 | Mou et al. (3) | M | Several days after birth | Sichuan (Han) | Yes | No | Typical | Yes | Yes | Anorexia, apathia | Low | Not detected | Compound heterozygous for c.1110InsG (exon 6) and c.958C > T (exon 5) |
| 6 | 2019 | Wu et al. (7) | F | 2 months | Guangdong | Yes | Two brothers and two sisters | Typical | Yes | No | No | Normal | Low | Homozygous for c.106C > T (exon 1) |
| 7 | 2020 | Zhou et al. (8) | M | 3 days | Guangdong | No | No | Typical | No | Yes | No | Low | Not detected | Homozygous for c.948delC (exon 5) |
| 8 | 2020 | Zhong et al. (4) | M | 12 months | Guangdong | No | Twin brother | Typical | No | No | Apathia | Normal | Normal | Compound heterozygous for c.926G > T (exon 5) and c.976 + 2 T > A (intron 5) |
| 9 | 2022 | Li et al. (9) | F | 3 months | Hunan | No | Younger brother | Typical | Yes | No | No | Normal | Not detected | Homozygous for c.1456delG (exon9) |
| 10 | 2022 | Hua et al. (10) | F | 1 year | Sichuan (Han) | No | No | Typical | Yes | No | No | Low | Not detected | Compound heterozygous for c.1466dupT (exon 9) and c.295G > A (exon 2) |
| 11 | 2024 | Present patient 1 | M | 4 years | Sichuan (Han) | No | No | Atypical (acne-like pustules) | No | No | No | Normal | Low | Compound heterozygous for c.1452_1474 + 1del TGAGCCCAGGAGACTGAGCCCAGG (exon 9 and intron 9) and c.1288-1G > A (intron 7) |
| 12 | 2024 | Present patient 2 | F | 4 months | Sichuan (Yi) | Yes | Older brother | Typical | Yes | Yes | No | Low | Low | Homozygous for c.295G > A (exon 2) |
| 13 | 2024 | Present patient 3 | M | 4 months | Sichuan (Tibetan) | No | No | Typical | Yes | Yes | Irritability | Low | Not detected | Compound heterozygous for c.1462_1474 + 1delAGACTGAGCCCAGG (exon 9 and intron 9) and c.1110insG (exon 6) |
| 14 | 2024 | Present patient 4 | F | 7 months | Sichuan (Tibetan) | No | No | Typical | No | Yes | No | Not detected | Not detected | Homozygous for c.1110insG (exon 6) |
Summary of cases of AE with the SLC39A4 variant from China.
AE, Acrodermatitis enteropathica; F, Female; M, Male.
A total of 15 SLC39A4 variants have been reported in AE patients from China, almost half of which, seven variants, were found in Sichuan region (Table 1). Unlike other areas, some variants, including c.295G > A, c.1110insG and c.1462_1474 + 1del AGACTGAGCCCAGG, were repeatedly identified in Sichuan region. In particular, the c.1462_1474 + 1del AGACTGAGCCCAGG variant was exclusively identified in Tibetan ethnicity. Given the enclosed environment and prevalence of consanguineous marriage in this region, besides hotspot variants, we consider the founder effect is likely to exist.
Acrodermatitis enteropathica is typically manifested by periorificial dermatitis and usually associated with hypozincaemia. However, a few patients could exhibit some atypical lesions, such as generalized pustules and blisters mimicking infectious diseases, or plaques resembling psoriasis and palmoplantar keratoderma (1, 11, 12). Moreover, serum zinc level could be normal in a minority of patients with AE (7). As in this study, the skin lesions of patient 1 presented with erythema, papules, pustules, and scars on the face and trunk, which were so much like acne. In addition, his serum zinc level was normal but the serum alkaline phosphatase level was low. The acne-like lesions improved obviously and serum alkaline phosphatase level increased to the normal range after administration with a single regimen of zinc sulfate. Under this condition, patients with low serum alkaline phosphatase level presenting acne-like lesions should raise a high suspicious of atypical AE. Detection of zinc-dependent metalloenzyme serum alkaline phosphatase, a more sensitive and precise parameter for the assessment of zinc deficiency, is very essential to help make a correct diagnosis.
4 Conclusion
Overall, in this study, a total of five variants of SLC39A4, including two unreported before, was identified in four unrelated patients with AE from three different ethnicities in Sichuan region of southwestern China. The three recurrent variants, c.295G > A, c.1110insG, and c.1462_1474 + 1del AGACTGAGCCCAGG, seem to be hotspot variants of SLC39A4 in patients with AE from Sichuan region. Of note, the c.1462_1474 + 1del AGACTGAGCCCAGG variant was exclusively identified in Tibetan ethnicity, implying a founder effect is likely to exist. Sichuan region of southwestern China may be one of the high AE incidence areas. Unusual acne-like lesions developed in a Han patient with a normal serum zinc level, which highlights the diversity of clinical manifestations of AE. Serum alkaline phosphatase and genetic tests are necessary for evaluating the zinc deficiency in human body and helping make the correct diagnosis. In this study, some limitations should not be neglected, especially the small sample size. Therefore, more works are needed to verify our findings based on larger sample size in the future.
Statements
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the ethics committee of West China Hospital, Sichuan University. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin. Written informed consent was obtained from the individual(s), and minor(s)’ legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
Author contributions
ZL: Data curation, Formal Analysis, Methodology, Writing – original draft. SW: Conceptualization, Resources, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We acknowledge the patients and their families.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2024.1399511/full#supplementary-material
References
1.
Wang S Xue L Guo ZP Wang L Yang Y . A novel SLC39A4 gene mutation in the family of an acrodermatitis enteropathica patient with an unusual presentation. Br J Dermatol. (2008) 159:976–8. doi: 10.1111/j.1365-2133.2008.08777.x
2.
Zhou XY Chen XJ Wang S Xue J Liu W Wang Q et al . One recurrent homozygous mutation of SLC39A4 in a girl with acrodermatitis enteropathica from southwestern China. Int J Dermatol. (2016) 55:223–5. doi: 10.1111/ijd.12442
3.
Mu Y Zhang Z Yang P Yang H Liu Y Liu L et al . Analysis of SLC39A4 gene mutation in a patient with acrodermatitis enteropathica. Zhonghua Yi Xue Yi Chuan Xue Za Zhi. (2017) 34:387–9. doi: 10.3760/cma.j.issn.1003-9406.2017.03.016
4.
Zhong W Yang C Zhu L Huang YQ Chen YF . Analysis of the relationship between the mutation site of the SLC39A4 gene and acrodermatitis enteropathica by reporting a rare Chinese twin: a case report and review of the literature. BMC Pediatr. (2020) 20:34. doi: 10.1186/s12887-020-1942-4
5.
Li CR Yan SM Shen DB Li Q Shao JP Xue CY et al . One novel homozygous mutation of SLC39A4 gene in a Chinese patient with acrodermatitis enteropathica. Arch Dermatol Res. (2010) 302:315–7. doi: 10.1007/s00403-010-1047-2
6.
Gao Y Li X Huang S You SH Fan ZN . A study of SLC39A4 gene mutation responsible for acrodermatitis enteropathica. Acta Univ Med Nanjing. (2014) 34:660–3. doi: 10.7655/NYDXBNS20140525
7.
Wu F Zhang Y Shi X Lu P Yang C Man MQ et al . Novel nonsense mutation of the SLC39A4 gene in a family with atypical acrodermatitis enteropathica. Clin Exp Dermatol. (2019) 44:933–6. doi: 10.1111/ced.13964
8.
Zhou X Xue R Luo Q Zhang SQ . A study of SLC39A4 gene mutation in acrodermatitis enteropathica. Chin J Dermatovenereol. (2020) 34:739–42. doi: 10.13735/j.cjdv.1001-7089.201909054
9.
Li KY Tang JP Shu Y Qiu SZ Wang YW Wen R et al . Recurrent systemic sporadic rash for 10 years in a girl aged 11 years. Zhongguo Dang Dai Er Ke Za Zhi. (2022) 24:1047–52. doi: 10.7499/j.issn.1008-8830.2204123
10.
Hua W Zou J Zhuang Y Zhou T . Case report: Acrodermatitis enteropathica result from a novel SLC39A4 gene mutation. Front Pediatr. (2022) 10:972030. doi: 10.3389/fped.2022.972030
11.
Iyengar S Chambers C Sharon VR . Bullous acrodermatitis enteropathica: case report of a unique clinical presentation and review of the literature. Dermatol Online J. (2015) 21:13030. doi: 10.5070/D3214026272
12.
Behera B Mohapatra L Sahu B Patnaik M . A case of acrodermatitis enteropathica mimicking mutilating palmoplantar keratoderma. Indian J Dermatol. (2022) 67:314. doi: 10.4103/ijd.IJD_112_17
Summary
Keywords
acrodermatitis enteropathica, normal serum zinc, pustule, Tibetan, SLC39A4
Citation
Li Z and Wang S (2024) Variants of SLC39A4 cause acrodermatitis enteropathica in Tibetan, Yi, and Han families in Sichuan region of southwestern China: a case report series. Front. Med. 11:1399511. doi: 10.3389/fmed.2024.1399511
Received
12 March 2024
Accepted
01 May 2024
Published
20 May 2024
Volume
11 - 2024
Edited by
Devinder Mohan Thappa, Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), India
Reviewed by
Arti Nanda, As'ad Al-Hamad Dermatology Center, Kuwait
Leila Youssefian, University of California, Los Angeles, United States
Updates
Copyright
© 2024 Li and Wang.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sheng Wang, wangsheng1892@126.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.