Abstract
Background:
Preeclampsia is the leading cause of maternal and fetal morbidity and mortality. Calcium supplementation has been considered a potential intervention to reduce the risk of preeclampsia. This umbrella review aims to summarize the effects of calcium supplementation in the prevention of preeclampsia based on existing systematic reviews and meta-analyses studies.
Methods:
A systematic search of electronic databases, such as MEDLINE, Web of Science, SCOPUS, and the Cochrane Library, was conducted from inception to 30 December 2023. The methodological quality of the included studies was assessed using the revised version of the Assessing the Methodological Quality of Systematic Reviews (AMSTAR 2) tool. A random-effects model was used to estimate the effect of calcium supplementation on preeclampsia. Heterogeneity among included studies and publication bias were assessed using the I2 statistic and the Egger’s test, respectively.
Results:
Calcium supplementation reduced the risk of preeclampsia by 47% (RR: 0.53, 95% CI: 0.42, 0.68) with a considerable level of heterogeneity (I2 = 84.39%). Our subgroup analyses revealed that the risk of preeclampsia was significantly lower in high-risk pregnancies that received calcium supplementation (RR: 0.35, 95% CI: 0.26, 0.47), indicating a 65% risk reduction. In comparison, low-risk pregnant women who received calcium supplementation experienced a 33% risk reduction (RR: 0.67, 95% CI: 0.59, 0.77). Furthermore, the effects of calcium supplementation were more pronounced in women from developing countries compared to those from developed countries.
Conclusion:
This umbrella review provides a summary of the evidence supporting the use of calcium supplementation to reduce preeclampsia. Incorporating calcium supplementation into antenatal care interventions may help to reduce the burden of preeclampsia and improve maternal and fetal outcomes. Further studies are needed to explore the impact of baseline calcium levels, optimal dosage, timing, and routes of supplementation to effectively decrease the incidence of preeclampsia.
Background
Preeclampsia is a pregnancy-specific multisystem complication characterized by high blood pressure, proteinuria, and organ damage that poses a significant risk to both the mother and the fetus. Its incidence varies across regions, affecting 2–5% of pregnancies worldwide (1). Evidence suggests that the burden of preeclampsia is greater in developing countries, with a reported rate of 2.8% of live births, which is seven times higher than the rate in developed countries (0.4%) (2). Preeclampsia is one of the leading causes of maternal and perinatal morbidity and mortality worldwide, accounting for up to 29,000 maternal deaths annually (3). Calcium supplementation has emerged as a topic of interest and investigation for the prevention of preeclampsia (4, 5).
Calcium plays a crucial role in muscle contraction, maintaining water balance, and regulating blood pressure. Insufficient calcium levels trigger the release of parathyroid hormone, resulting in elevated intracellular calcium concentrations in vascular smooth muscle cells. This leads to vasoconstriction and high blood pressure (6). Consequently, maintaining adequate calcium levels ensures vascular stability, thereby reducing the risk of hypertension (6). Moreover, dietary calcium supplementation has been observed to decrease renin levels in the blood, although it does not completely eliminate them. In addition, the renin-angiotensin-aldosterone system, which plays a pivotal role in regulating blood pressure, is influenced by the acute activation of calcium-sensing receptors in juxtaglomerular cells due to high extracellular calcium concentrations. Taken together, these factors contribute to the preventive effect of calcium against hypertension (7, 8).
During pregnancy, adequate blood calcium levels are associated with positive maternal–fetal health outcomes and a reduced risk of maternal and fetal cardiovascular disease (9). However, the demand increases due to a combination of physiological, metabolic, and hormonal factors in a period of pregnancy (10, 11). Calcitonin hormone, which is responsible for calcium deposition in the bones, is also elevated during pregnancy (12). Furthermore, vitamin D, which plays a crucial role in calcium metabolism and bone health, can also be affected during pregnancy (13). These conditions indicate the need for a relatively high calcium intake during pregnancy. However, insufficient dietary calcium intake can impair the body’s ability to maintain calcium balance, potentially causing maternal calcium deficiency and complications, such as disrupted vascular tone regulation, preterm birth, and fetal growth restriction (13, 14). This is particularly concerning in mothers who have a low dietary calcium intake (5). In 2015, the World Health Organization (WHO) recommended calcium supplementation for pregnant women (15) and has subsequently updated its guidelines to emphasize the potential benefits of calcium in the prevention of preeclampsia (15–17). However, a review of low- and middle-income countries revealed that the average calcium intake was less than 900 mg/day (18). Subsequent reviews in 2004 and 2018 indicated that dietary calcium intake remained at approximately 600 mg/day in these regions, with no significant improvement, compared to over 1,000 mg/day in high-income countries, resulting in a difference of approximately 300 mg/day mean calcium intake (19, 20).
There is limited and inconsistent evidence regarding the effectiveness of calcium supplementation in preventing preeclampsia. A systematic review and meta-analysis of four randomized trials that included 7,272 women reported that calcium supplementation led to an 11% reduction in the incidence of preeclampsia (10). Another review conducted by Christina Oh et al. (21) indicated a 70% reduction in the risk of preeclampsia (21).
Therefore, this umbrella review aims to summarize and address the inconsistencies found in systematic reviews and meta-analyses on the effectiveness of calcium supplementation in preventing preeclampsia. Furthermore, this review aims to consolidate current knowledge, identify potential sources of heterogeneity, and provide valuable insights into the effectiveness of calcium supplementation in reducing the burden of preeclampsia, ultimately guiding clinical practice and informing future research endeavors.
Methods
Design
This umbrella review was conducted to evaluate the effects of calcium supplementation on the prevention of preeclampsia using existing systematic reviews and meta-analyses studies. The review process adhered to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines (22). The target population (P) comprised pregnant women at risk of developing preeclampsia, the intervention (I) was calcium supplementation, the comparator (C) was pregnant women who did not receive calcium supplementation, and the outcome (O) was preeclampsia, defined as a pregnancy-specific illness characterized by the onset of hypertension after 20 weeks of gestation, with or without proteinuria (23). This review was registered with PROSPERO (CRD42024547701).
Search strategy
Using a combination of Medical Subject Headings (MeSH) and keywords, we systematically searched MEDLINE via PubMed, Embase, Web of Science, Scopus, the Cochrane Database of Systematic Reviews, the PROSPERO register, and the Google Scholar web search engine. MeSH terms and keywords included ‘preeclampsia,’ ‘hypertensive disorders during pregnancy,’ ‘pregnancy-induced hypertension,’ ‘calcium,’ ‘Ca++,’ ‘supplementation,’ ‘systematic review,’ and ‘meta-analysis.’ The search period was from inception to 30 December 2023. Additionally, citations of the eligible studies were manually searched. The detailed search strategy is included in the Supplementary Table S1.
Study inclusion criteria
Types of studies
This umbrella review included all systematic reviews and meta-analyses studies that assessed the effects of calcium supplementation in the prevention of preeclampsia.
Types of participants
The participants included in this review were women who received calcium supplementation during their pregnancy, regardless of whether the pregnancy was a singleton or multiple gestation. A pregnant woman considered to have an unknown status was defined as one who received calcium supplementation despite her risk for preeclampsia, her country of residence and her baseline status. In contrast, pregnant women participating in the study were categorized into two subgroups based on their risk profile. The high-risk group consisted of pregnant women who exhibited calcium deficiency, a history of gestational hypertension or preeclampsia, a positive roll-over test, a positive angiotensin-sensitivity test, or other high-risk factors as defined in the original study. The low-risk group included healthy pregnant women with a lower risk of developing these conditions (5). Additionally, baseline calcium intake levels were categorized as low if they were below 900 mg/day and adequate if they were 900 mg/day or above (5). Moreover, for the analysis, a high dose was defined as ≥1 g of elemental calcium per day, a medium dose was defined as 0.6–1.5 g, and a low dose was defined as <1 g of elemental calcium per day.
Types of interventions
Studies were eligible if they compared calcium supplementation during pregnancy with a placebo group, no treatment. The included studies considered different risk factors for preeclampsia, dietary intake, dosage variations, and the economic status of the countries involved.
Outcomes of interest
The primary outcome of interest was the incidence of preeclampsia.
Setting
This umbrella review included studies conducted globally without any geographical limitations.
Publication condition
This review included only published articles in English that had full texts and reported the effect of the outcome of interest.
Selection and data extraction
The retrieved systematic review and meta-analysis studies were exported into EndNote software to eliminate any duplicate studies. Two independent reviewers (HK and NBY) retrieved records from the databases and then screened the articles based on their titles and abstracts. The records retained during this screening phase underwent full-text assessment by the two reviewers. Disagreements between the two reviewers were resolved through consensus and the involvement of a third reviewer. A data extraction form was used to extract information from the included studies. The form includes author, year of publication, sample size (number of primary studies), intervention and control group sample sizes, effect estimates with confidence intervals, dose levels, the economic status of the countries, calcium dietary status, and risk status of women. Furthermore, the data extraction process in Microsoft Excel involved transforming each factor’s relative risk (RR) to its logarithmic form.
Additionally, the upper and lower confidence intervals were also log-transformed. The standard error (SE) of these confidence intervals was then calculated using the formula SE = (logUCL—logLCL) / 3.92, where logUCL and logLCL represent the logarithmic upper and lower confidence limits. The log-transformed RR and the SE of their corresponding confidence intervals were utilized in the pooled RR estimation to estimate effect sizes.
Quality assessment
The methodological quality of the included studies was assessed using the revised version of the Assessing the Methodological Quality of Systematic Reviews (AMSTAR 2) tool (24). AMSTAR 2 has 16 method-related questions that serve as a critical appraisal tool for systematic reviews and meta-analyses that include randomized or non-randomized studies. Two independent reviewers, EM and MW, critically appraised the included studies using the checklists. As suggested in AMSTAR 2, we rated the confidence in the results of the included reviews as follows: high (no or one non-critical weakness), moderate (more than one critical weakness but no critical flaws), low (one critical flaw with or without non-critical weaknesses), and critically low (more than one critical flaw with or without non-critical weaknesses). The Supplementary Material includes the quality assessment of the studies included in this umbrella review (Supplementary Table S2). The quality of the primary studies included in each of the research syntheses was rigorously evaluated to ensure their robustness and reliability. The list of primary studies in the meta-analyses is in the Supplementary Table S3.
Data synthesis and statistical analysis
After extracting the data using Microsoft Excel, we imported them into STATA version 17.0 for further analysis. This allowed us to perform statistical tests and sensitivity analyses and to apply meta-analytic techniques to ensure robust and reliable results. The findings of the included studies were presented quantitatively and qualitatively to provide comprehensive evidence about the current use of calcium supplementation and its potential effects on the reduction of preeclampsia. A random-effects model meta-analysis was conducted to summarize the effects of calcium supplementation on the reduction of preeclampsia. The estimates were reported as relative risks with corresponding 95% confidence intervals.
Heterogeneity between studies was assessed using the I2 statistic. The I2 statistic describes the percentage of variation across different studies due to heterogeneity (25). We used the Q test to estimate I2, and heterogeneity was classified by I2. The findings of the I2 test were classified as low (25% and below), moderate (26–50%), high (51–75%), and very high (above 75%) (25). If there was evidence of heterogeneity, we used a subgroup analysis using different characteristics of the included studies, such as preeclampsia risk status, baseline dietary status, and dosage of calcium supplement. Publication bias was assessed using a funnel plot and an Egger’s regression test. An asymmetric funnel plot and an Egger’s test with results lower than 0.05 were considered indicative of publication bias. Sensitivity analyses were performed to evaluate the influence of individual studies on the overall pooled effect estimate. This involved systematically removing one study at a time from the meta-analysis and recalculating the overall effect size to observe any significant changes.
Results
This umbrella review of systematic reviews and meta-analyses includes published studies on calcium supplementation for the prevention of preeclampsia. The included studies were systematic reviews and meta-analyses published from 1996 to 2022. A total of 1,157 records were retrieved through electronic searches, and 12 studies were included to estimate the effects of calcium supplementation in the prevention of preeclampsia (Figure 1).
Figure 1

Flow chart of study selection for an umbrella review of systematic reviews and meta-analyses of the effect of calcium supplementation on prevention of preeclampsia in calcium supplemented group compared to placebo.
Characteristics of included studies
In the systematic reviews and meta-analyses, the number of primary studies included ranged from a minimum of 3 to a maximum of 29. The minimum and maximum sample sizes in these included studies were 1,324 participants (660 in the experimental group and 664 in the control group) and 27,765 participants (13,896 in the experimental group and 13,869 in the control group), respectively. With the exception of the review by Christina Oh et al. (21) which included quasi-experimental studies, the remaining reviews included only randomized controlled trials in their meta-analyses. Eight systematic reviews and meta-analyses reported the effects of calcium supplementation on the reduction of preeclampsia, regardless of dose, duration, baseline dietary intake, and risk status for preeclampsia. Additionally, systematic reviews and meta-analyses classified calcium-supplemented women based on their risk status for preeclampsia, baseline calcium diet status, dosage, and the economic status of the countries in which the studies were conducted (Table 1).
Table 1
| Author | Year of publication | No primary article | Experimental | Control | Sample size | Status of women |
|---|---|---|---|---|---|---|
| Calcium supplementation despite the risk status of the pregnant women | ||||||
| Imdad and Bhutta (40) | 2012 | 15 | 8,231 | 8,259 | 16,490 | Unknown status |
| Tang et al. (28) | 2014 | 10 | 12,399 | 12,388 | 24,787 | Unknown status |
| Li-bin An et al. (10) | 2015 | 4 | 7,252 | 7,272 | 14,524 | Unknown status |
| Win Khaing et al. (30) | 2017 | 16 | 12,876 | 13,060 | 25,936 | Unknown status |
| G. J. Hofmeyr et al. (5) | 2018 | 13 | 7,851 | 7,879 | 15,730 | Unknown status |
| Xiaotong Sun et al. (27) | 2019 | 25 | 13,896 | 13,869 | 27,765 | Unknown status |
| Christina Oh et al. (21) | 2020 | 3 | 660 | 664 | 1,324 | Unknown status |
| Mai-Lei Woo et al. (29) | 2022 | 31 | NR | NR | 17,915 | Unknown status |
| Risk status for preeclampsia | ||||||
| Tito Silvio P. et al. (26) | 2012 | 3 | 162 | 184 | 346 | High risk |
| Tang et al. (28) | 2014 | 4 | 4,320 | 4,345 | 8,665 | High risk |
| G. J. Hofmeyr et al. (5) | 2018 | 5 | 281 | 306 | 587 | High risk |
| Win Khaing et al. (30) | 2017 | 8 | 1,140 | 1,160 | 2,300 | High risk |
| Xiaotong Sun et al. (27) | 2019 | 12 | 797 | 820 | 1,617 | High risk |
| Tippawan L. et al. (31) | 2022 | 13 | NR | NR | 26,021 | High risk |
| Dexin Chen et al. (32) | 2022 | 3 | 99 | 100 | 199 | High risk |
| Mai-Lei Woo et al. (29) | 2022 | 17 | 1,540 | 2,121 | 3,661 | High risk |
| José Villar et al. (9) | 2000 | 6 | 3,146 | 3,161 | 6,307 | Low risk |
| Tito Silvio P. et al. (26) | 2012 | 7 | 5,535 | 5,524 | 11,059 | Low risk |
| Tang et al. (28) | 2014 | 6 | 8,049 | 8,043 | 16,092 | Low risk |
| Win Khaing et al. (30) | 2017 | 8 | 12,876 | 13,060 | 25,936 | Low risk |
| G. J. Hofmeyr et al. (5) | 2018 | 8 | 7,570 | 7,573 | 15,143 | Low risk |
| Xiaotong Sun et al. (27) | 2019 | 13 | 13,119 | 1,305 | 14,424 | Low risk |
| Mai-Lei Woo et al. (29) | 2022 | 13 | 8,423 | 8,361 | 16,784 | Low risk |
| Baseline calcium dietary level status | ||||||
| José Villar et al. (9) | 2000 | 6 | 907 | 935 | 1842 | Low baseline |
| Tito Silvio P. et al. (26) | 2012 | 6 | 5,958 | 5,096 | 11,054 | Low baseline |
| Imdad and Bhutta (40) | 2012 | 10 | 5,711 | 5,727 | 11,438 | Low baseline |
| Tang et al. (28) | 2014 | 6 | 5,272 | 5,262 | 10,534 | Low baseline |
| G. J. Hofmeyr et al. (5) | 2018 | 8 | 5,331 | 5,347 | 10,678 | Low baseline |
| Mai-Lei Woo et al. (29) | 2022 | 24 | 7,266 | 7,784 | 15,050 | Low baseline |
| Tito Silvio P. et al. (26) | 2012 | 6 | 4,815 | 4,826 | 9,641 | Adequate baseline |
| G. J. Hofmeyr et al. (5) | 2018 | 4 | 2,505 | 2,517 | 5,022 | Adequate baseline |
| Mai-Lei Woo et al. (29) | 2022 | 6 | 2,697 | 2,698 | 5,395 | Adequate baseline |
| Tang et al. (28) | 2014 | 2 | 4,605 | 4,602 | 9,207 | Unknown |
| G. J. Hofmeyr et al. (5) | 2018 | 1 | 15 | 15 | 30 | Unknown |
| Level of calcium supplementation dose | ||||||
| Xiaotong Sun et al. (27) | 2019 | 16 | 404 | 445 | 849 | High |
| Mai-Lei Woo et al. (29) | 2022 | 19 | 8,249 | 8,447 | 16,696 | High |
| Dexin Chen et al. (31) | 2022 | 13 | 12,942 | 12,839 | 25,781 | High |
| Xiaotong Sun et al. (27) | 2019 | 5 | 137 | 137 | 274 | Moderate |
| Dexin Chen et al. (31) | 2022 | 3 | 678 | 695 | 1,373 | Moderate |
| Xiaotong Sun et al. (27) | 2019 | 4 | 236 | 235 | 471 | Low |
| Mai-Lei Woo et al. (29) | 2022 | 12 | 2035 | 1714 | 3,749 | Low |
| Dexin Chen et al. (31) | 2022 | 13 | 1,498 | 1,498 | 1,498 | Low |
| Economic status of the countries | ||||||
| Win Khaing et al. (30) | 2017 | 12 | 10,253 | 10,415 | 20,668 | Developed |
| Xiaotong Sun et al. (27) | 2019 | 4 | 4,508 | 4,526 | 10,034 | Developed |
| Aamer Imdad et al. (33) | 2011 | 10 | 5,697 | 5,708 | 11,405 | Developing |
| Win Khaing et al. (30) | 2017 | 4 | 2,641 | 2,645 | 5,286 | Developing |
| Xiaotong Sun et al. (27) | 2019 | 21 | 11,278 | 11,252 | 22,530 | Developing |
Characteristics of the included systematic reviews and meta-analyses, 2023.
Effects of calcium supplementation on preeclampsia
Using eight systematic review and meta-analysis studies, the effects of calcium supplementation on the reduction of preeclampsia incidence were reported, regardless of the risk for preeclampsia, baseline calcium diet status, and dose. The results revealed a significant reduction in the risk of preeclampsia in women receiving calcium supplementation [0.53 (95% CI: 0.42, 0.68)] (Figure 2). The level of heterogeneity was high, as evidenced by an I2 value of = 83.74%. Due to publication bias (p value less than 0.0001), a trim-and-fill analysis was conducted. However, differences in the results were not seen. The Galbraith and funnel plots are also available in Supplementary Figures S1, S2.
Figure 2
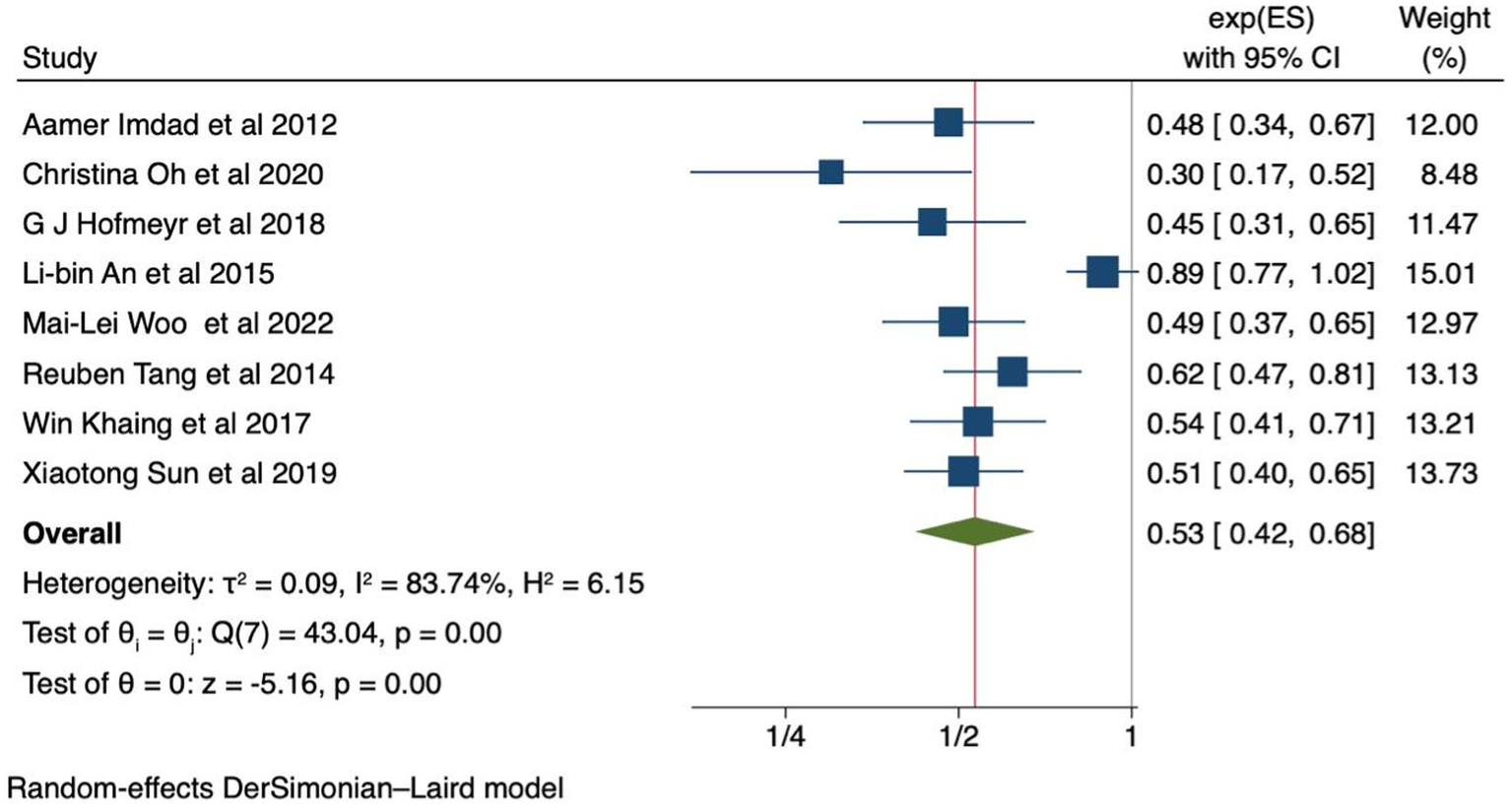
Forest plot of calcium supplementation and preeclampsia.
Effects of calcium supplementation based on risk status for preeclampsia
Calcium supplementation in high-risk pregnancies was evaluated in eight studies (5, 26–32). The pooled relative risk showed a 65% reduction in the incidence of preeclampsia [RR 0.35 (95% CI: 0.26, 0.47)] (Figure 3). On the other hand, in seven studies, calcium supplementation in low-risk pregnancies showed 33% of reduction of preeclampsia [RR 0.67 (95% CI: 0.59, 0.77)] (Figure 3). We conducted an Egger’s test to evaluate the presence of publication bias, and the obtained p-value of 1 indicates that there is no evidence of publication bias. The Galbraith and funnel plots are available in Supplementary Figures S3, S4.
Figure 3
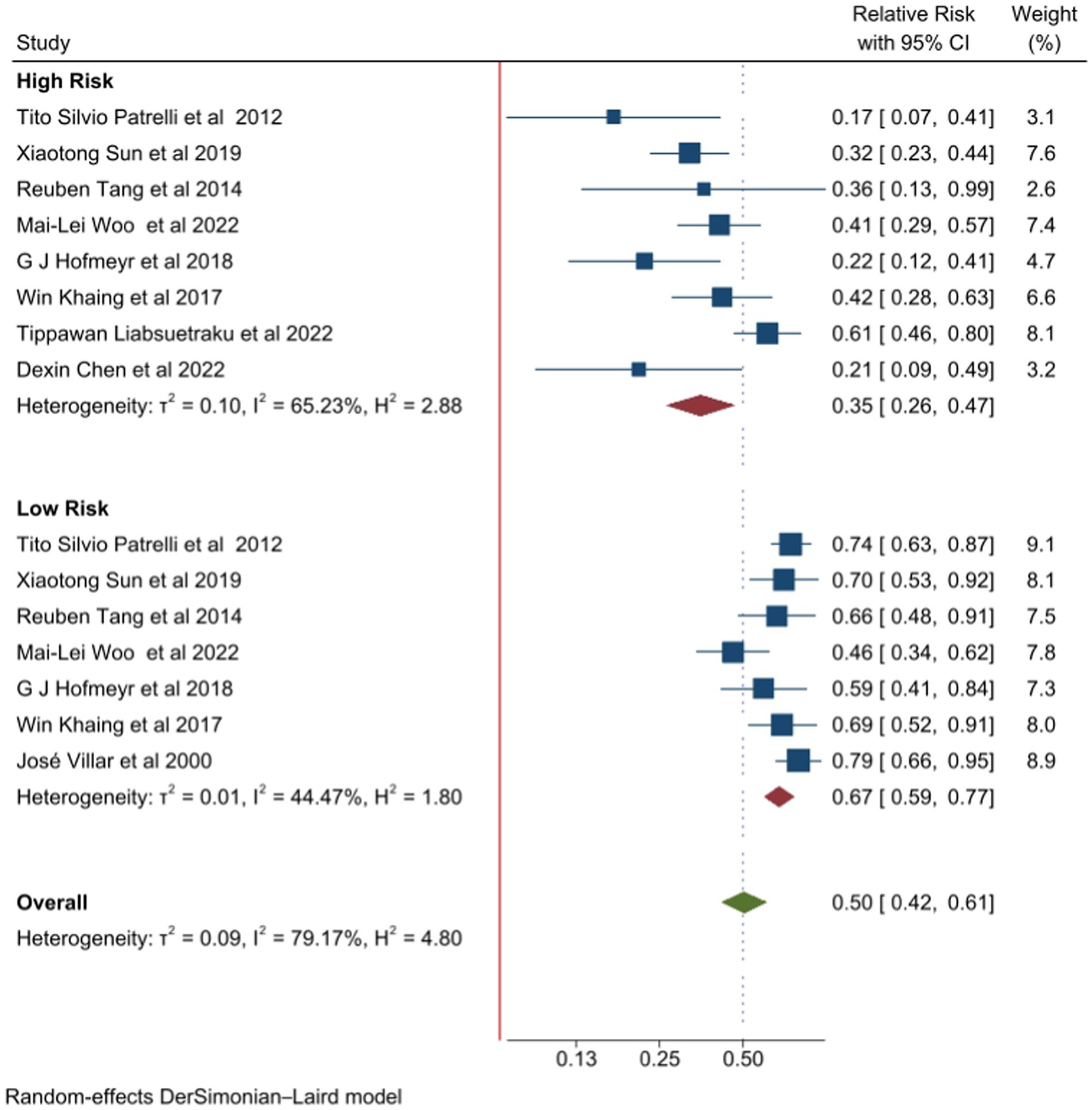
Forest plot of calcium supplementation and preeclampsia based on risk status.
Effects of calcium supplementation based on baseline dietary status
A pooled analysis of six studies found that women with a low baseline diet experienced a 59% reduction in the risk of developing preeclampsia with calcium supplementation [RR 0.41 (95% CI: 0.35–0.48)] compared to those who received a placebo, without heterogeneity between the studies (I2 = 0.0%). Similarly, calcium supplementation in women with an adequate baseline calcium level, as reported by three studies, was found to be associated with a 33% reduction in the risk of preeclampsia [RR 0.67 (95% CI: 0.56, 0.80)] without moderate heterogeneity (I2 = 0.0%), compared to placebo (Figure 4). Additionally, the Egger’s test yielded a p-value of 1, indicating no publication bias. The Galbraith and funnel plots are available in Supplementary Figures S5, S6, respectively.
Figure 4
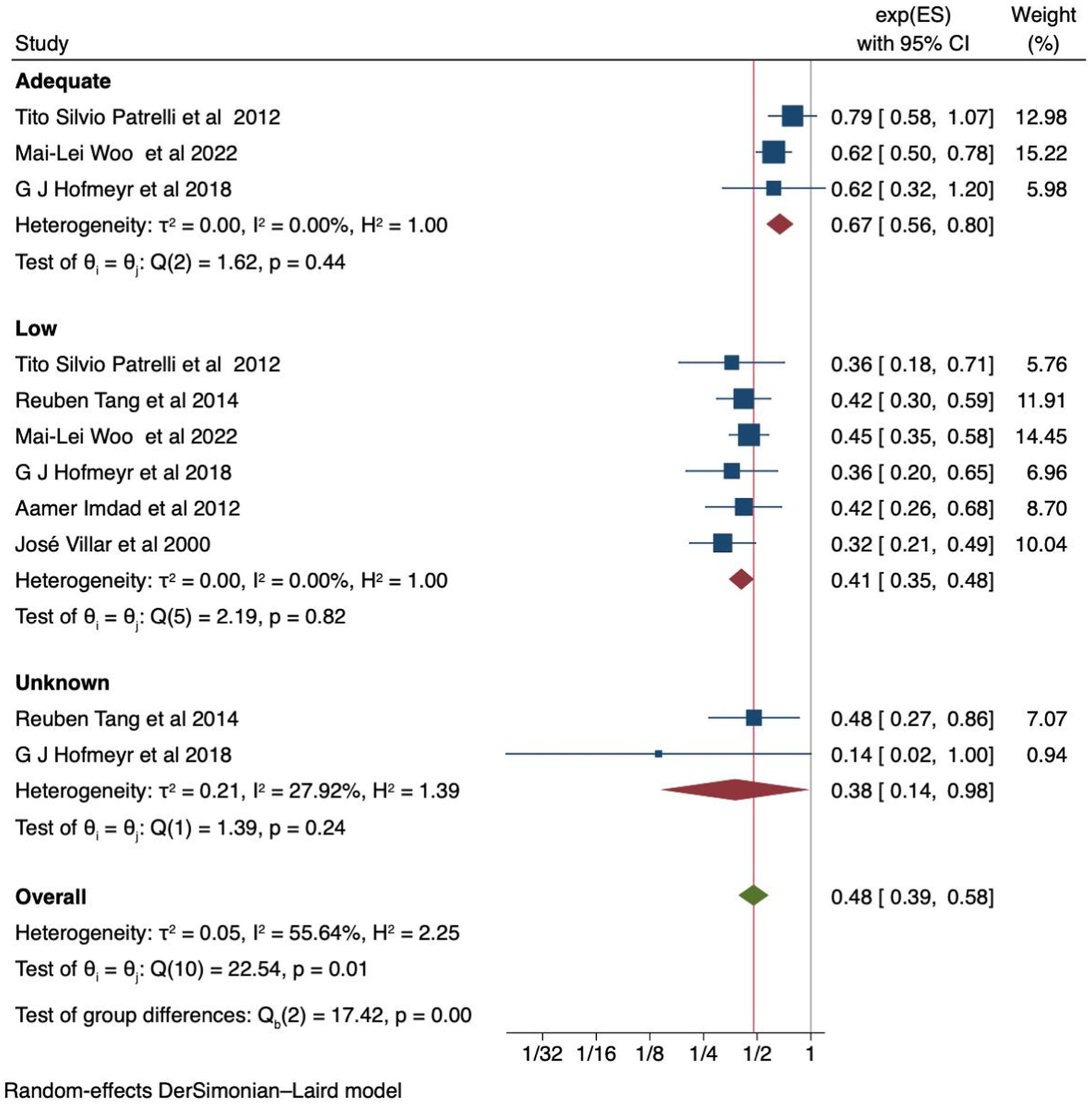
Forest plot of calcium supplementation and preeclampsia based on baseline calcium dietary status.
Effects of calcium supplementation based on dose
Sun et al. (27) and Chen et al. (32) classified calcium supplementation into three categories: high, moderate, and low doses, while Mai-Lei et al. (29) classified it into high and low. The pooled analysis of high-dose supplementation showed a steadily decreasing incidence of preeclampsia [RR 0.59 (95% CI: 0.51–0.69)]. The level of heterogeneity was low (I2 value of 19.05%). The forest plot is available in Figure 5. Furthermore, the Egger’s test yielded a p-value of 1. The Galbraith and funnel plots are available in Supplementary Figures S7, S8, respectively.
Figure 5
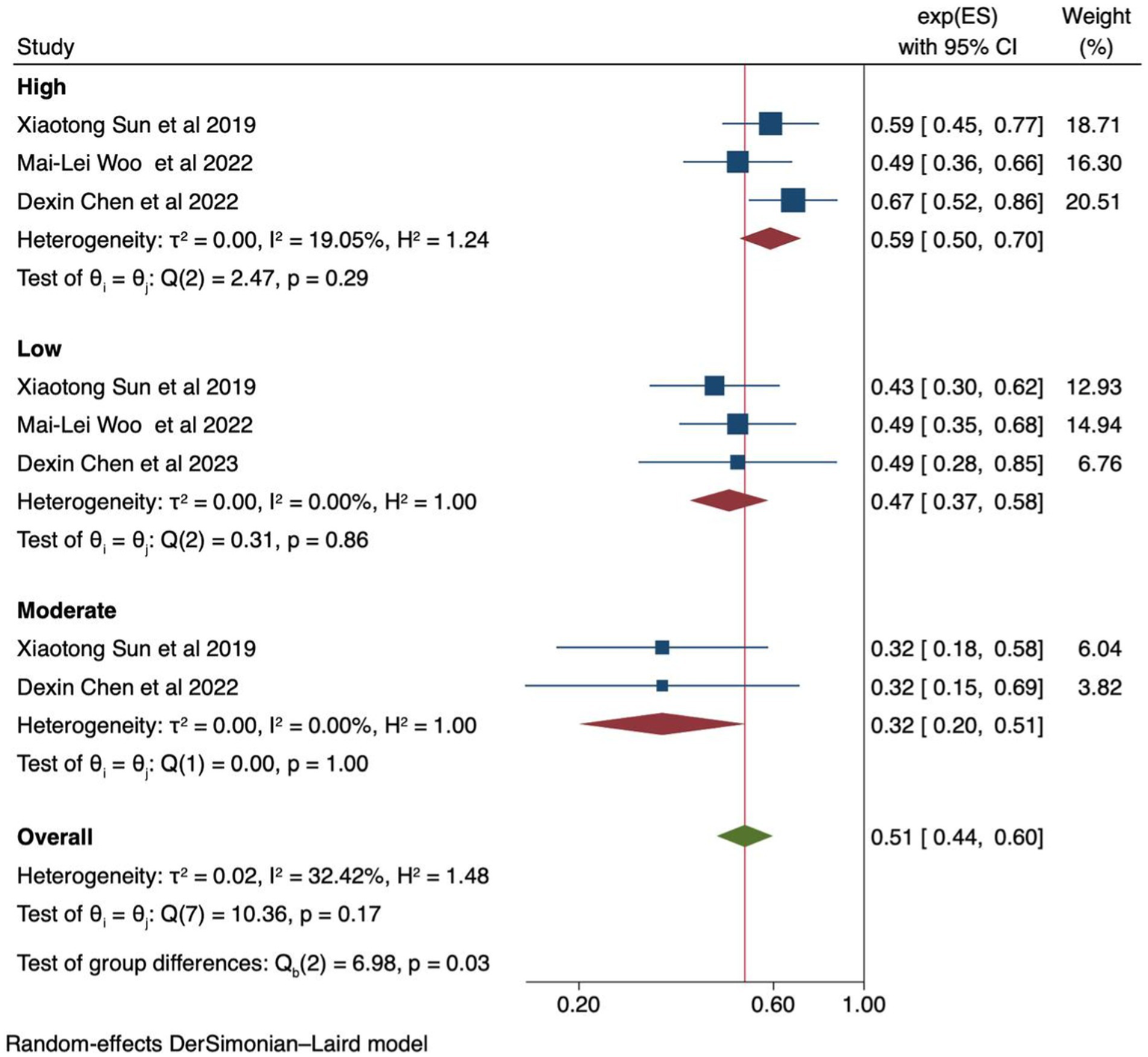
Forest plot of calcium supplementation and preeclampsia based on supplemented calcium dose level.
Effects of calcium supplementation based on the economic status of the countries
We conducted a subgroup analysis based on the economic status of the countries using five studies (27, 30, 33). In developed countries, calcium supplementation reduced the risk of preeclampsia by 38% [RR 0.62 (95% CI: 0.41, 0.95)]. In developing countries, a 56% reduction was noted [RR 0.44 (95% CI: 0.36, 0.56)] without heterogeneity (I2 = 00%) (Figure 6). Additionally, the Egger’s test yielded a p-value of 1, and funnel plots are also available in the Supplementary Figure S9.
Figure 6
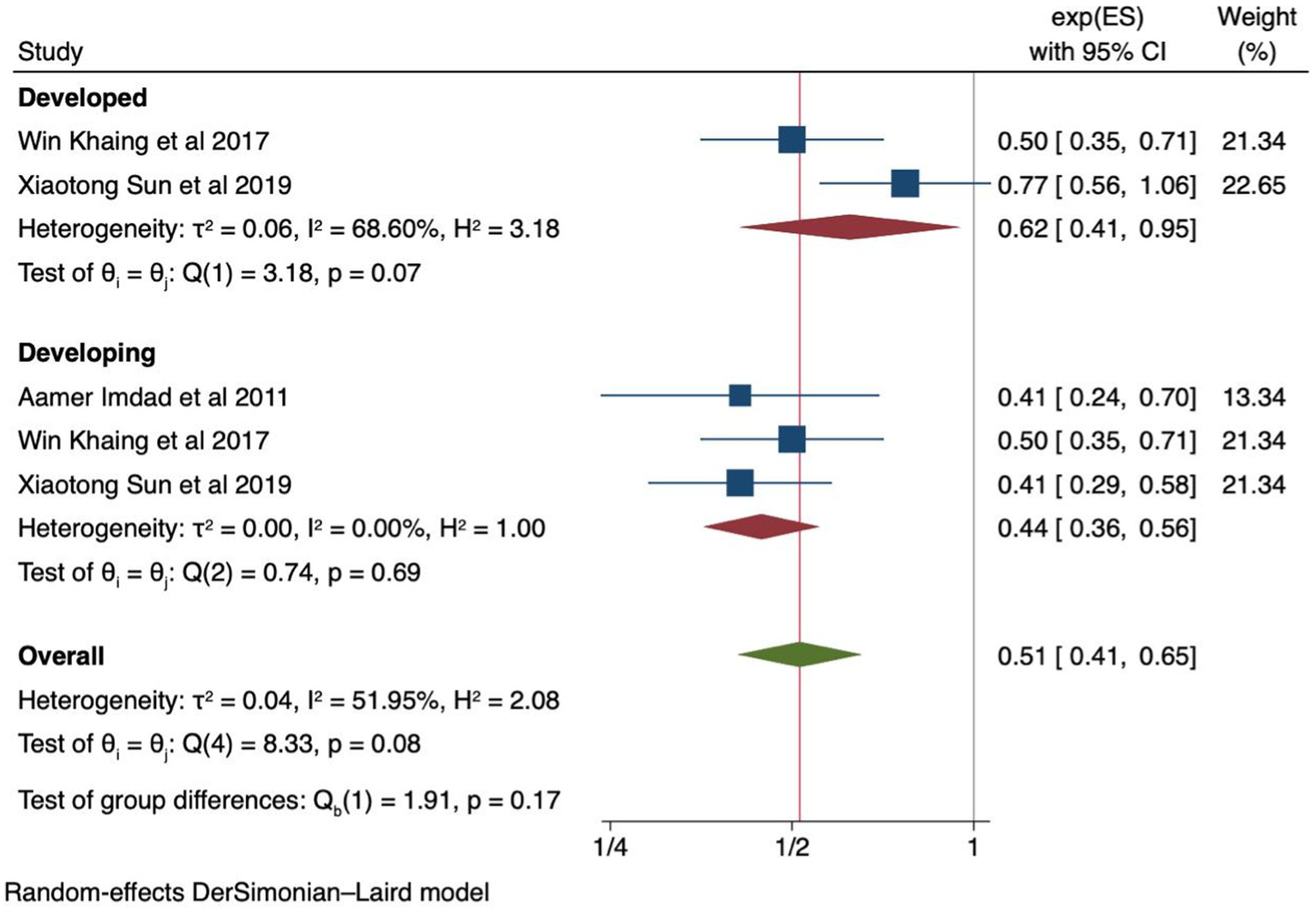
Forest plot of calcium supplementation and preeclampsia based on economic status economic status of the countries.
Sensitivity analysis
A leave-one-out sensitivity analysis was performed to identify the impact of each individual study on the overall pooled effect. The results of this sensitivity analysis showed that the pooled finding was not dependent on a single study (Supplementary Tables S4–S6).
Discussion
Calcium supplementation to prevent preeclampsia is recommended by different guidelines (16, 34). However, there has been no prior umbrella review on using calcium supplementation to prevent preeclampsia. An umbrella review of eight systematic reviews and meta-analyses showed a significant reduction (47%) in the incidence of preeclampsia with the use of calcium supplements compared to control groups. Furthermore, it was observed that calcium supplementation significantly reduced the risk of preeclampsia in both high-risk women (65%) and low-risk women (33%) compared to placebo group.
In this umbrella review, calcium supplementation was associated with a 47% reduction in the incidence of preeclampsia among pregnant women. With the exception of one meta-analysis of multicenter randomized controlled trials, which reported an 11% reduction (10), the remaining seven meta-analyses included in this review consistently demonstrated a significant reduction in preeclampsia incidence in the calcium supplementation group compared to the control or placebo groups (5, 35). The discrepancy in findings may be due to the majority of the included primary studies being from developed or middle-upper income countries (10). Additionally, out of the four studies used for the meta-analysis, only one indicated that pregnant women had a low-calcium diet (10). However, the baseline calcium level is a crucial factor in reducing the incidence of preeclampsia with calcium supplementation.
In the current review, the pooled relative risk of preeclampsia in high-risk women with calcium supplementation compared to placebo reduced the risk of preeclampsia by 65% [0.35 (95% CI: 0.26, 0.47)] and I2 = 65.23. Although the effect was less pronounced in low-risk women, calcium supplementation still demonstrated a significant reduction in the incidence of preeclampsia (RR 0.67 95% CI: 0.59, 0.77). All the meta-analyses used in this umbrella review, both for high- and low-risk subgroup analyses, agreed on the reduction of preeclampsia incidence with calcium supplementation compared to placebo. However, the high level of heterogeneity observed among high-risk women for preeclampsia might be due to differences in risk definitions, variations in calcium dosage, and discrepancies in the timing of supplementation initiation among the primary studies included in the meta-analysis. Incorporating calcium supplementation into the guidelines for antenatal care, with special attention to high-risk pregnancies, may help to reduce maternal morbidity and mortality.
Recommended calcium intake for pregnant women varies between 900 and 1,200 mg/day, depending on the country (36, 37). However, actual intake among pregnant women often falls short of these recommendations, particularly in developing countries and even in developed countries where calcium-rich foods are readily available and affordable (19, 38). Furthermore, inconsistent results have been observed in systematic reviews and meta-analyses, with no effects in the prevention of preeclampsia on women with adequate calcium serum levels. However, a study conducted by Mai-Lei et al. showed a reduced incidence of preeclampsia. This umbrella review supports their finding that calcium supplementation in women with adequate baseline calcium levels has an effect on the prevention of preeclampsia. This finding suggests a potential need for increased calcium intake during pregnancy or that preeclampsia may involve multiple systems despite normal serum calcium levels. This can be explained by the significant physiological, metabolic, and hormonal changes that occur during pregnancy, which increase calcium demand (10, 11). One key factor is the heightened calcium demand of the developing fetus and growing placenta. This leads to increased calcium transfer from the mother to the fetus, depleting maternal calcium levels and heightening the risk of preeclampsia (11).
We found that calcium supplementation in women with low baseline calcium levels significantly reduced the risk of preeclampsia compared to placebo. Inadequate calcium intake, defined as consuming less than 600 mg daily, is associated with an increased incidence of hypertensive disorders during pregnancy (39). Moreover, the incidence of preeclampsia decreased significantly in the supplemented group in developing countries (56%) compared to developed countries (38%). This may explain the association between low calcium levels and hypertension (7, 8). Therefore, in regions where the diet is traditionally low in calcium and in developing countries, the recommendation of calcium supplementation during pregnancy is a safe approach. The authors also support the WHO recommendation of calcium supplementation as part of antenatal care in populations with low calcium intake (15).
We also found that high-dose and low-dose calcium supplementation have different effects on decreasing the incidence of preeclampsia. However, no strong signals indicated which group of women was more likely to benefit or be harmed, or which type of administration maximized the effect. Our findings do not suggest any superiority of high-dose over low-dose calcium supplementation. It should be noted that the study conducted by Chen et al. (22) used high-dose calcium supplementation only in high-risk pregnant women and low-dose in low-risk women, which may have influenced the results. High-dose calcium poses challenges in terms of cost, transportation, and storage. Low-dose calcium is equally effective as high-dose supplementation when initiated before 20 weeks of gestation (21). Lower dosages are recommended by the WHO (1.5–2.0 g/day) (16), and the fortification of staple foods with calcium could be considered for populations with low-calcium diets (21).
We categorized the outcomes based on various factors to provide a comprehensive perspective on calcium supplementation. This thorough inclusion of studies enhances the breadth of our review and offers a more detailed understanding of the efficacy of calcium supplementation in preventing preeclampsia.
Our findings should be considered in light of the limitations present in the included studies. The optimal timing of calcium supplementation for the prevention of preeclampsia may not be fully elucidated in the included studies. Variations in the timing and dosage of calcium supplementation across studies could introduce additional heterogeneity and affect the effect estimates. Furthermore, variations in the definition of preeclampsia across studies can lead to inconsistencies in pooled analyses, especially when combining data from trials with different control groups, such as placebo, no treatment controls, and alternative agents used. Additionally, the definition of risk varied between the individual studies and the pooled analysis, leading to potential inconsistencies in the findings. A few primary studies in the meta-analysis included co-supplementation of Vitamin D, which could be a potential source of heterogeneity.
Conclusion
In conclusion, our findings indicate that daily calcium supplementation during pregnancy may be an effective strategy to prevent preeclampsia. The beneficial effect is more pronounced in women with low baseline calcium intake, those at high risk for preeclampsia, and those in developing nations. Considering the guidelines provided by the WHO, calcium supplementation can help reduce the incidence of preeclampsia and its associated complications. Furthermore, fortifying staple foods with calcium will be vital for populations with low-calcium diets.
Statements
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
HK: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. EM: Conceptualization, Data curation, Project administration, Resources, Writing – review & editing. MA: Data curation, Investigation, Resources, Validation, Writing – review & editing. BA: Data curation, Investigation, Methodology, Visualization, Writing – review & editing. MB: Formal analysis, Investigation, Methodology, Writing – review & editing. MR: Formal analysis, Writing − original draft, Writing − review & editing. NY: Conceptualization, Formal analysis, Methodology, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2025.1434416/full#supplementary-material
References
1.
Poon LC Shennan A Hyett JA Kapur A Hadar E Divakar H et al . Erratum to" the International Federation of Gynecology and Obstetrics (FIGO) initiative on pre-eclampsia: a pragmatic guide for first-trimester screening and prevention"[int J gynecol obstet 145 suppl. 1 (2019) 1-33]. Int J Gynaecol Obstet. (2019) 146:390–1. doi: 10.1002/ijgo.12892
2.
Say L Chou D Gemmill A Tunçalp Ö Moller A-B Daniels J et al . Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health. (2014) 2:e323–33. doi: 10.1016/S2214-109X(14)70227-X
3.
Hug L You D Blencowe H Mishra A Wang Z Fix MJ et al . Global, regional, and national estimates and trends in stillbirths from 2000 to 2019: a systematic assessment. Lancet. (2021) 398:772–85. doi: 10.1016/S0140-6736(21)01112-0
4.
Gomes F Ashorn P Askari S Belizan JM Boy E Cormick G et al . Calcium supplementation for the prevention of hypertensive disorders of pregnancy: current evidence and programmatic considerations. Ann N Y Acad Sci. (2022) 1510:52–67. doi: 10.1111/nyas.14733
5.
Hofmeyr GJ Lawrie TA Atallah ÁN Torloni MR . Calcium supplementation during pregnancy for preventing hypertensive disorders and related problems. Cochrane Database Syst Rev. (2018) 2018. doi: 10.1002/14651858.CD001059.pub5
6.
Villa-Etchegoyen C Lombarte M Matamoros N Belizán JM Cormick G . Mechanisms involved in the relationship between low calcium intake and high blood pressure. Nutrients. (2019) 11:1112. doi: 10.3390/nu11051112
7.
Ortiz-Capisano MC Ortiz PA Garvin JL Harding P Beierwaltes WH . Expression and function of the calcium-sensing receptor in juxtaglomerular cells. Hypertension. (2007) 50:737–43. doi: 10.1161/HYPERTENSIONAHA.107.095158
8.
Atchison DK Harding P Beierwaltes WH . Hypercalcemia reduces plasma renin via parathyroid hormone, renal interstitial calcium, and the calcium-sensing receptor. Hypertension. (2011) 58:604–10. doi: 10.1161/HYPERTENSIONAHA.111.172890
9.
Villar J Belizán JM . Same nutrient, different hypotheses: disparities in trials of calcium supplementation during pregnancy. Am J Clin Nutr. (2000) 71:1375S–9S. doi: 10.1093/ajcn/71.5.1375s
10.
An L-b Li W-t Xie T-n Peng X Li B Xie S-h et al . Calcium supplementation reducing the risk of hypertensive disorders of pregnancy and related problems: a meta-analysis of multicentre randomized controlled trials. Int J Nurs Pract. (2015) 21:19–31. doi: 10.1111/ijn.12171
11.
King JC . Physiology of pregnancy and nutrient metabolism. Am J Clin Nutr. (2000) 71:1218S–25S. doi: 10.1093/ajcn/71.5.1218s
12.
Felsenfeld AJ Levine BS . Calcitonin, the forgotten hormone: does it deserve to be forgotten?Clin Kidney J. (2015) 8:180–7. doi: 10.1093/ckj/sfv011
13.
Karras SN Wagner CL Castracane VD . Understanding vitamin D metabolism in pregnancy: from physiology to pathophysiology and clinical outcomes. Metabolism. (2018) 86:112–23. doi: 10.1016/j.metabol.2017.10.001
14.
Gehlert J Morton A . Hypercalcaemia during pregnancy: review of maternal and fetal complications, investigations, and management. Obstetric Med. (2019) 12:175–9. doi: 10.1177/1753495X18799569
15.
Organization WH . Guideline: calcium supplementation in pregnant womenWorld Health Organization (2013).
16.
Organization WH . WHO recommendation: Calcium supplementation during pregnancy for the prevention of pre-eclampsia and its complicationsWorld Health Organization (2018).
17.
World Health Organization . WHO recommendation on calcium supplementation before pregnancy for the prevention of pre-eclampsia and its complications. (2020).
18.
Lee SE Talegawkar SA Merialdi M Caulfield LE . Dietary intakes of women during pregnancy in low-and middle-income countries. Public Health Nutr. (2013) 16:1340–53. doi: 10.1017/S1368980012004417
19.
Merialdi M Mathai M Ngoc N Purwar M Campodonico L Abdel-Aleem H et al . World Health Organization systematic review of the literature and multinational nutritional survey of calcium intake during pregnancy. Fetal Mat Med Rev. (2005) 16:97–121. doi: 10.1017/S0965539505001506
20.
Cormick G Betrán A Romero I Lombardo C Gülmezoglu A Ciapponi A et al . Global inequities in dietary calcium intake during pregnancy: a systematic review and meta-analysis. BJOG Int J Obstet Gynaecol. (2019) 126:444–56. doi: 10.1111/1471-0528.15512
21.
Oh C Keats EC Bhutta ZA . Vitamin and mineral supplementation during pregnancy on maternal, birth, child health and development outcomes in low-and middle-income countries: a systematic review and meta-analysis. Nutrients. (2020) 12:491. doi: 10.3390/nu12020491
22.
Page MJ McKenzie JE Bossuyt PM Boutron I Hoffmann TC Mulrow CD et al . The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. (2021) 88:105906. doi: 10.1016/j.ijsu.2021.105906
23.
Mol BW Roberts CT Thangaratinam S Magee LA De Groot CJ Hofmeyr GJ . Pre-eclampsia. Lancet. (2016) 387:999–1011. doi: 10.1016/S0140-6736(15)00070-7
24.
Shea BJ Reeves BC Wells G Thuku M Hamel C Moran J et al . AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. (2017):j4008. doi: 10.1136/bmj.j4008
25.
Higgins JP Thompson SG Deeks JJ Altman DG . Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
26.
Patrelli TS Dall’Asta A Gizzo S Pedrazzi G Piantelli G Jasonni VM et al . Calcium supplementation and prevention of preeclampsia: a meta-analysis. J Matern Fetal Neonatal Med. (2012) 25:2570–4. doi: 10.3109/14767058.2012.715220
27.
Sun X Li H He X Li M Yan P Xun Y et al . The association between calcium supplement and preeclampsia and gestational hypertension: a systematic review and meta-analysis of randomized trials. Hypertens Pregnancy. (2019) 38:129–39. doi: 10.1080/10641955.2019.1593445
28.
Tang R Tang IC Henry A Welsh A . Limited evidence for calcium supplementation in preeclampsia prevention: a meta-analysis and systematic review. Hypertens Pregnancy. (2015) 34:181–203. doi: 10.3109/10641955.2014.988353
29.
Woo Kinshella M-L Sarr C Sandhu A Bone JN Vidler M Moore SE et al . Calcium for pre-eclampsia prevention: a systematic review and network meta-analysis to guide personalised antenatal care. BJOG Int J Obstet Gynaecol. (2022) 129:1833–43. doi: 10.1111/1471-0528.17222
30.
Khaing W Vallibhakara SA Tantrakul V Vallibhakara O Rattanasiri S McEvoy M et al . Calcium and vitamin D supplementation for prevention of preeclampsia: a systematic review and network Meta-analysis. Nutrients. (2017) 9. doi: 10.3390/nu9101141
31.
Liabsuetrakul T Yamamoto Y Kongkamol C Ota E Mori R Noma H . Medications for preventing hypertensive disorders in high-risk pregnant women: a systematic review and network meta-analysis. Syst Rev. (2022) 11:1–17. doi: 10.1186/s13643-022-01978-5
32.
Chen D Wang H Xin X Zhang L Yu A Li S et al . Different doses of calcium supplementation to prevent gestational hypertension and pre-eclampsia: a systematic review and network meta-analysis. Front Nutr. (2022) 8:795667. doi: 10.3389/fnut.2021.795667
33.
Imdad A Jabeen A Bhutta ZA . Role of calcium supplementation during pregnancy in reducing risk of developing gestational hypertensive disorders: a meta-analysis of studies from developing countries. BMC Public Health. (2011) 11:1–13. doi: 10.1186/1471-2458-11-S3-S1
34.
Poon LC Shennan A Hyett JA Kapur A Hadar E Divakar H et al . The International Federation of Gynecology and Obstetrics (FIGO) initiative on preeclampsia (PE): a pragmatic guide for first trimester screening and prevention. Int J Gynaecol Obstet. (2019) 145:1–33. doi: 10.1002/ijgo.12802
35.
Hofmeyr GJ Roodt A Atallah A Duley L . Calcium supplementation to prevent pre-eclampsia-a systematic review. S Afr Med J. (2003) 93:224–8. PMID:
36.
NDA ESP . Scientific opinion on dietary reference values for calcium. EFSA J. (2015) 13:4101.
37.
Del Valle HB Yaktine AL Taylor CL Ross AC . Dietary reference intakes for calcium and vitamin D. (2011).
38.
Molag ML Vries JH Duif N Ocke MC Dagnelie PC Goldbohm RA . Selecting informative food items for compiling food-frequencyquestionnaires: comparison of procedures. Br J Nutr. (2010) 104:446–56. doi: 10.1017/S0007114510000401
39.
Atallah A Hofmeyr G Duley L . Calcium supplementation during pregnancy for preventing hypertensive disorders and related problems (Cochrane review)Cochrane Library (2000). 1.
40.
Imdad A Bhutta ZA . Effects of calcium supplementation during pregnancy on maternal, fetal and birth outcomes. Paediatr Perinat Epidemiol. (2012) 1:138–52. doi: 10.1111/j.1365-3016.2012.01274.x
Summary
Keywords
preeclampsia, calcium supplementation, umbrella review, systematic review, meta-analysis
Citation
Kumsa H, Mislu E, Arage MW, Abate BB, Beriye M, Mehari Reda M and Yimer NB (2025) Effects of calcium supplementation on the prevention of preeclampsia: an umbrella review of systematic reviews and meta-analyses. Front. Med. 12:1434416. doi: 10.3389/fmed.2025.1434416
Received
17 May 2024
Accepted
28 January 2025
Published
05 March 2025
Volume
12 - 2025
Edited by
Ravindra Veeranna, Xavier University School of Medicine, Netherlands
Reviewed by
Mozammel Hoque, Indian Veterinary Research Institute (IVRI), India
Henri Korkes, Pontifical Catholic University of São Paulo, Brazil
Updates
Copyright
© 2025 Kumsa, Mislu, Arage, Abate, Beriye, Mehari Reda and Yimer.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Henok Kumsa, henokkumsa@gmail.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.