Abstract
Objectives:
This study aims to explore the value of integrating the Mini-Clinical Evaluation Exercise (Mini-CEX) and Check-list Scales in the training of emergency and critical care residents. The study evaluates the effectiveness of these tools in enhancing clinical diagnostic skills, improving teaching outcomes, and optimizing clinical processes.
Methods:
This study included 199 emergency and critical care residents who completed their training between January 2018 and April 2024. A paired study design was employed to evaluate the effectiveness of the combined use of the Mini-CEX and Check-list Scales. Initially, all participants used the Mini-CEX to assess their performance during clinical diagnosis and treatment (control group). After training with the Check-list Scales, the same participants underwent a second assessment using the Mini-CEX scale (experimental group). Data were analyzed using various statistical methods, including chi-square tests for categorical data, t-tests for normally distributed data, rank-sum tests for non-normally distributed data, and receiver operating characteristic (ROC) curve analysis to evaluate diagnostic performance.
Results:
The combination of Mini-CEX and Check-list significantly improved clinical competencies across several domains. In the control group, the overall failure rate was 2.513%, the pass rate was 70.352%, and the excellence rate was 27.136%. In contrast, the experimental group showed a reduction in the failure rate to 0%, with a pass rate of 19.598% and an excellence rate of 80.402%. The Mini-CEX scores in the experimental group were significantly higher than those in the control group (p < 0.001), with marked improvements in individual competencies, especially in clinical judgment and overall clinical competence. However, the experimental group had a longer diagnosis and treatment time compared to the control group (66.985 ± 9.126 min vs. 52.387 ± 7.635 min, p < 0.05). Correlation analysis revealed significant associations between various parameters before and after using Check-list tools, indicating improved diagnostic efficiency and clinical skills. The correlation between total score and components such as medical interviewing skills, physical examination skills, and overall clinical competence was notably stronger after the use of the Check-list (p < 0.05). ROC curve analysis demonstrated that all factors had good diagnostic performance, with the lowest being consultation/advice and communication skills [area under curve (AUC) 0.716, 95% CI: 0.680–0.752) and humanistic qualities/professionalism (AUC 0.733, 95% CI: 0.696–0.770), and the highest being clinical judgment (AUC 0.844, 95% CI: 0.813–0.875) and organizational skills/efficiency (AUC 0.815, 95% CI: 0.782–0.848).
Conclusion:
The integration of the Mini-CEX and Check-list significantly enhances the diagnostic and clinical skills of emergency medicine residents. This combined approach addresses the limitations of traditional training methods and provides an effective model for improving medical education and the quality of care for critically ill patients.
1 Background
As society advances and the economy grows, the global burden of disease continues to escalate, imposing greater demands on the diagnostic and therapeutic capabilities of healthcare professionals, particularly in China (1–3). In response, the cultivation of clinical skills has become a central focus in global medical education (4). However, traditional teaching methods are increasingly inadequate for the evolving needs of modern healthcare systems (5, 6), making the effective delivery of clinical education a critical challenge. This issue is especially acute in China, where the working environment in emergency and critical care units is notably more complex than in many developed countries (7, 8). Due to strained doctor–patient relationships and difficult clinical settings, highly skilled or experienced healthcare professionals are often reluctant to work in such departments (9, 10). As a result, junior residents—despite their limited clinical experience and decision-making capacity—are frequently placed in these high-stakes environments (11, 12).
To address the gap between training needs and clinical demands, competency-based evaluation tools such as the Mini-CEX and the Check-list have been widely introduced. Mini-CEX, recommended by the American Board of Internal Medicine, is commonly used to assess residents’ core clinical competencies and is integrated into routine educational practice (13). It provides a comprehensive assessment of communication skills, professional competence, and clinical reasoning. Its flexibility across diverse clinical contexts and capacity to deliver formative feedback make it well-suited for longitudinal competency tracking, although its effectiveness may vary depending on evaluator consistency and clinical setting (14–16). In contrast, Check-lists are structured evaluation tools developed from clinical guidelines and expert consensus. They promote diagnostic standardization and procedural adherence, thereby enhancing safety and clinical efficiency (17–19). Nevertheless, Check-lists often underemphasize non-technical competencies such as humanistic care, communication (20), and critical thinking, and they may lack formative feedback mechanisms (21). Furthermore, widespread medical disputes (22), cost-control reforms (23), and workforce burnout (24) have compounded the challenges of cultivating clinical and humanistic competencies in China’s emergency settings. These institutional constraints limit not only the effectiveness of clinical teaching but also residents’ capacity for communication, empathy, and timely decision-making.
Although both the Mini-CEX and Check-lists have demonstrated considerable educational value when applied independently (25, 26), their respective roles in this study are clearly defined: the Check-list functions as the structured instructional intervention, while the Mini-CEX serves as the evaluation tool to measure its impact. While each tool has been widely used in isolation, few studies have systematically compared the effectiveness of Mini-CEX when integrated with Check-list-based training versus when paired with conventional clinical instruction, particularly in emergency and critical care settings. Therefore, this study aims to investigate whether incorporating a standardized Check-list into resident training can achieve superior educational outcomes compared to traditional teaching methods, using the Mini-CEX as a formative and comprehensive assessment framework. By integrating the procedural standardization of the Check-list with the multidimensional evaluation strengths of the Mini-CEX, we aim to establish a balanced and effective training model suitable for high-acuity clinical environments.
2 Subjects and methods
2.1 Study objectives
2.1.1 Study population
The 199 residents were enrolled in the study on a rolling basis between January 2018 and April 2024. The cohort consisted of 113 male and 86 female residents, with an average age of 29.69 ± 5.775 years. Each participant entered the study individually upon starting their emergency or critical care rotation and completed the control-phase Mini-CEX evaluation, followed by checklist-based training and post-intervention assessment. Therefore, the phrase “completed their training” refers to the completion of the study-specific teaching and evaluation process, not necessarily the formal end of their standardized residency training.
2.1.2 Study methods
This study utilized the Mini-CEX as the primary outcome measure. The Mini-CEX assesses seven domains: medical interviewing skills, physical examination, humanistic qualities/professionalism, clinical judgment, consultation/advice/communication skills, organizational skills/efficiency, and overall clinical competence. Each domain was rated on a 9-point scale, where 1–3 indicated failure, 4–6 indicated pass, and 7–9 indicated excellence. The proportion of residents achieving each category was calculated based on the total sample (n = 199). In addition to the seven Mini-CEX domains, we also recorded each resident’s diagnosis and treatment time (hereafter referred to as “time”) as a quantitative measure of clinical efficiency. All evaluations were conducted by a fixed panel of three senior attending physicians, including the department’s teaching secretary and director of education. These assessors had completed formal training in competency-based assessment, in accordance with national residency evaluation protocols. Their fixed status throughout the study ensured inter-rater reliability and minimized subjective variability. The Check-list Scale, developed by the research team in accordance with contemporary emergency and critical care guidelines, expert consensus, and training standards, provided a structured framework to guide clinical performance during diagnostic and therapeutic processes. It included key domains such as history-taking, physical examination, diagnostic reasoning, treatment steps, and inter-professional communication. Residents in the control group first received traditional clinical training without the Check-list. Their performance was evaluated using the Mini-CEX following comparable clinical encounters. They then entered the intervention phase and received structured training based on the Check-list. Their performance was reassessed using the Mini-CEX on similarly matched clinical cases (Figure 1).
FIGURE 1

Flowchart of methods.
2.1.2.1 Inclusion and exclusion criteria for participants
Inclusion criteria: (1) Junior residents who had not participated in similar teaching or assessment interventions within the past year; (2) Residents who completed both the control and intervention phases and had complete data records available.
Exclusion criteria: (1) Prior exposure to checklist-based training within the past year; (2) Incomplete participation in either phase or missing Mini-CEX data; (3) Obvious logical inconsistencies or outlier scoring patterns.
2.1.2.2 Qualification criteria for assessors
(1) Held attending or senior academic titles; (2) Completed standardized rater training according to national guidelines; (3) Maintained fixed evaluator status throughout the study to ensure consistency; (4) Had no direct supervisory or mentoring relationship with the evaluated residents.
2.1.3 Data analysis
Categorical data were expressed as counts or percentages and analyzed using the chi-square test. Normally distributed data were presented as mean ± standard deviation (±s) and compared between groups using the t-test. Non-normally distributed data were analyzed using the rank-sum test. The correlation coefficient (ρ) between any two variables was calculated, and data analysis was performed using SPSS 20.0 software. The ROC curves were plotted and compared using MedCalc 22.0.3 software, with a significance level set at p < 0.05. Figures 2–4 were generated using R language.
FIGURE 2
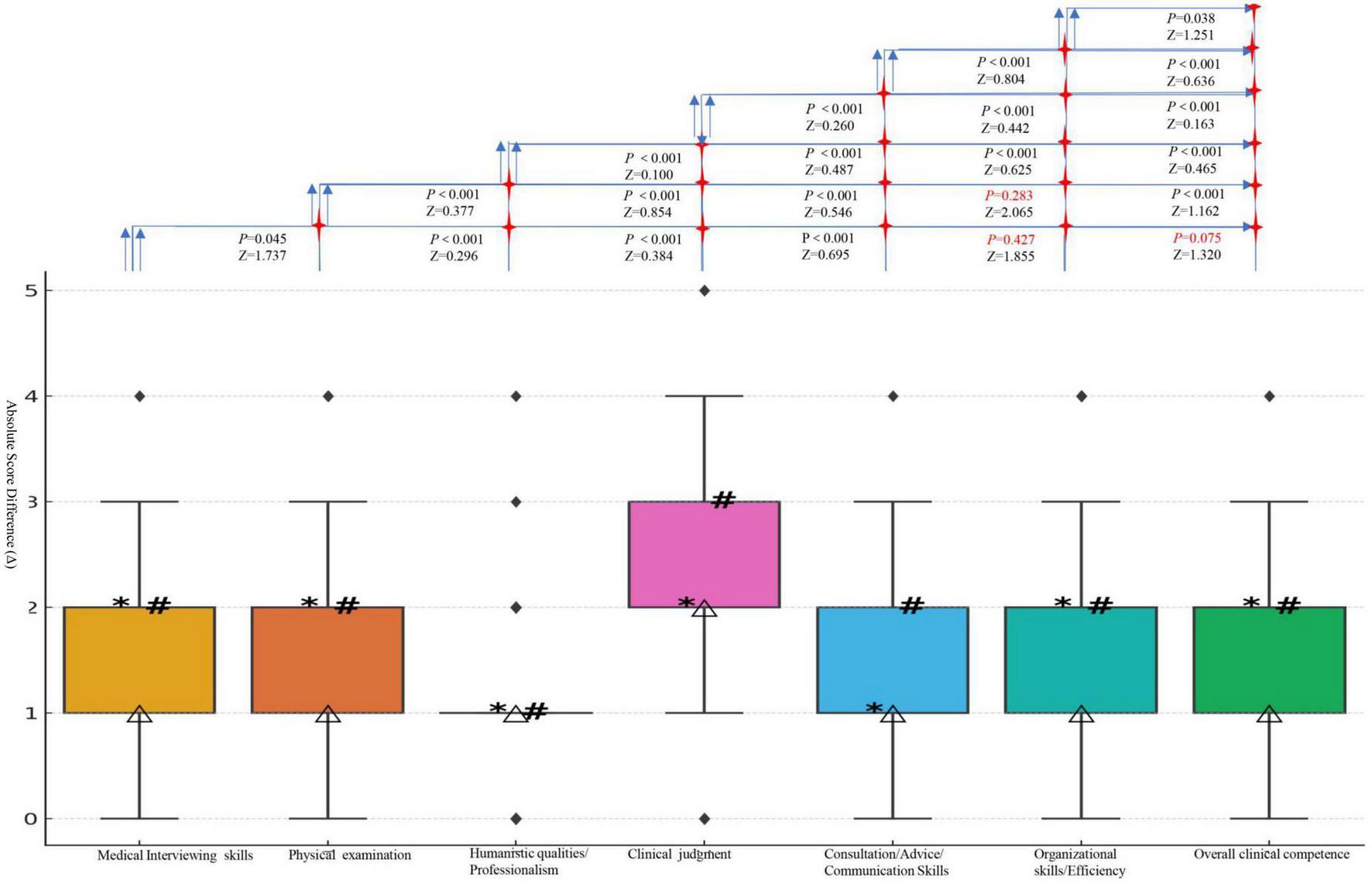
Boxplots of differences for each clinical skill; *, M50; △, M25; #, M75. The absolute score differences (Δ), ranked from highest to lowest, are as follows: clinical judgment: +2.417; physical examination: +2.407; organizational skills/Efficiency: +1.693; medical interviewing skills: +1.644; overall clinical competence: +1.543; consultation/advice/communication skills: +1.392; humanistic qualities/professionalism: +0.995. (All domains were confirmed to be non-normally distributed and were summarized using median and IQR. These raw score differences are for descriptive purposes only and should not be interpreted as statistically comparable across domains. Statistical significance should rely on p-values and Wilcoxon Z-statistics).
FIGURE 3
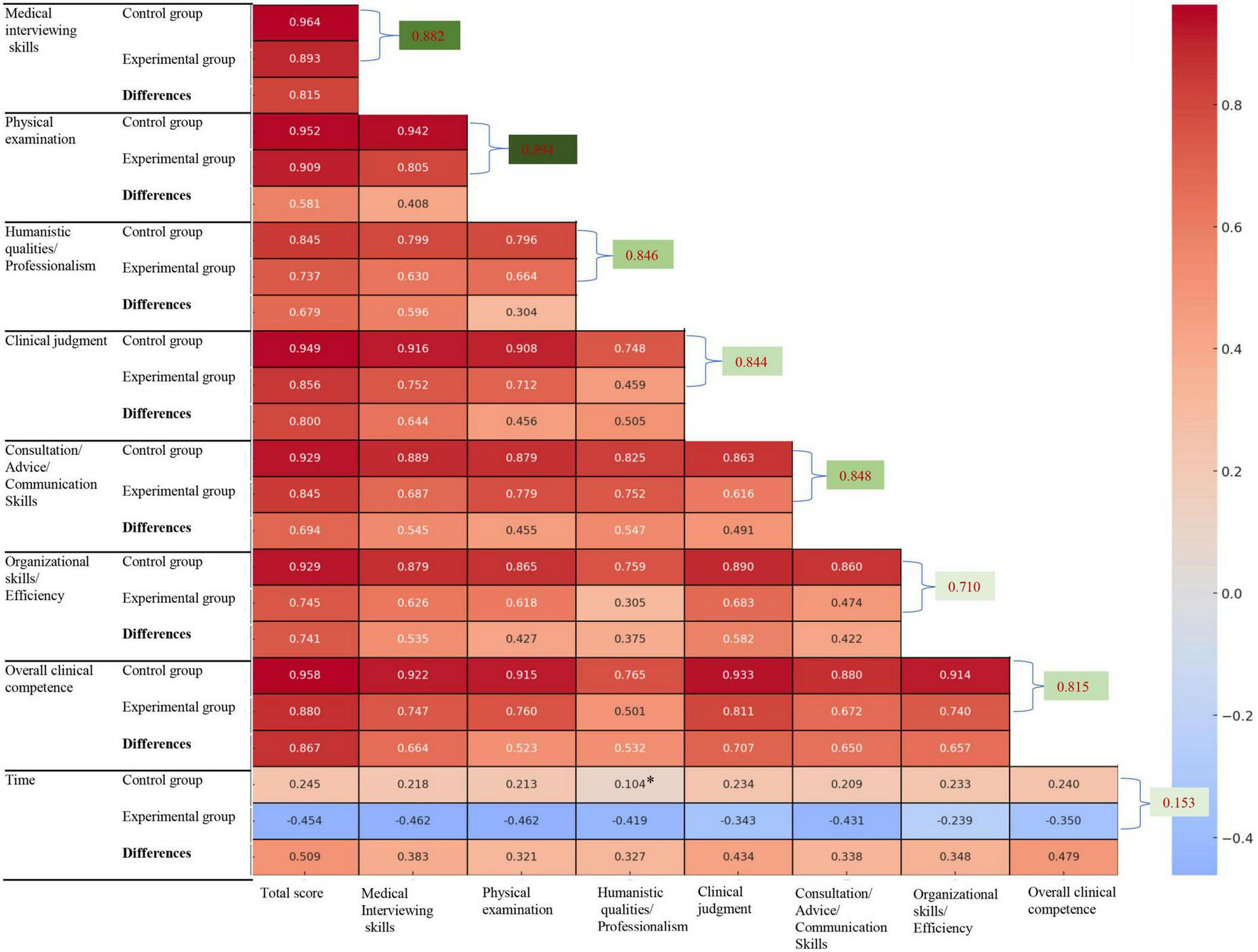
*Indicates p > 0.05. Correlation analysis of the same indicators before and after using Check-list is indicated in green.
FIGURE 4
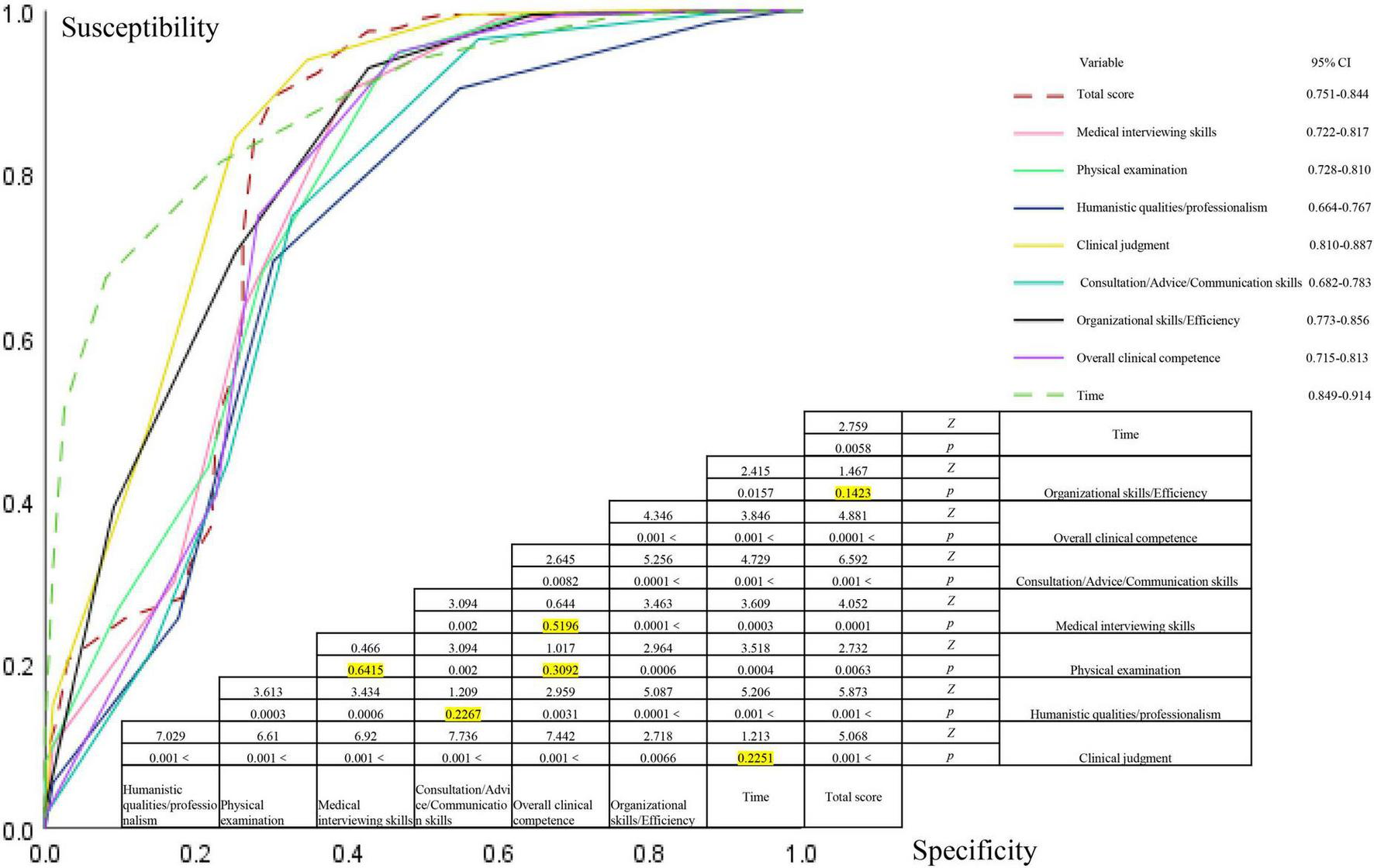
The receiver operating characteristic (ROC) curves of different indicators were compared pairwise, with yellow indicating a p-value greater than 0.05.
3 Results
3.1 Comparison of Mini-CEX scores and treatment times between control and experimental groups
In this study, the Mini-CEX scoring method was used to evaluate 199 cases before and after the implementation of the Check-list. The comparison of various competency scores and classifications between the control and experimental groups is shown in Figures 2, 3 and Table 1.
TABLE 1
| Variable | Control group | Experimental group | P-value | Z/t/χ2 |
| Total score | ||||
| Fail, n (%) | 5 (2.513) | 0 | < 0.001 | 27.332 |
| Pass, n (%) | 140 (70.352) | 39 (19.598) | – | – |
| Excellent, n (%) | 54 (27.136) | 160 (80.402) | – | – |
| Score | 34.000 (28.000, 46.000) | 48.146 ± 6.629 | < 0.001 | −12.212 |
| Medical interviewing skills | ||||
| Fail, n (%) | 28 (14.070) | 0 | < 0.001 | 68.572 |
| Pass, n (%) | 119 (59.799) | 73 (36.683) | – | – |
| Excellent, n (%) | 52 (26.131) | 126 (63.317) | – | – |
| Score | 5.281 ± 1.715 | 6.925 ± 1.150 | < 0.001 | −26.143 |
| Physical examination | ||||
| Fail, n (%) | 73 (36.683) | 1 (0.503) | < 0.001 | 107.771 |
| Pass, n (%) | 83 (41.709) | 110 (55.276) | – | – |
| Excellent, n (%) | 43 (21.608) | 88 (44.221) | – | – |
| Score | 4.000 (3.000, 6.000) | 6.407 ± 1.414 | < 0.001 | −12.131 |
| Humanistic qualities/professionalism | ||||
| Fail, n (%) | 3 (1.508) | 0 | < 0.001 | 38.719 |
| Pass, n (%) | 136 (68.342) | 61 (30.653) | – | – |
| Excellent, n (%) | 60 (30.151) | 138 (69.347) | – | – |
| Score | 5.899 ± 1.330 | 6.894 ± 1.042 | < 0.001 | −19.653 |
| Clinical judgment | ||||
| Fail, n (%) | 40 (20.101) | 0 | < 0.001 | 112.944 |
| Pass, n (%) | 109 (54.774) | 31 (15.578) | – | – |
| Excellent, n (%) | 50 (25.126) | 168 (84.422) | – | – |
| Score | 5.000 (4.000, 6.500) | 7.417 ± 1.065 | < 0.001 | −12.132 |
| Consultation/advice/communication skills | ||||
| Fail, n (%) | 16 (8.040) | 0 | < 0.001 | 83.521 |
| Pass, n (%) | 135 (67.839) | 110 (55.276) | – | – |
| Excellent, n (%) | 48 (24.121) | 89 (44.724) | – | – |
| Score | 5.000 (4.000, 6.000) | 6.392 ± 1.175 | < 0.001 | −11.329 |
| Organizational skills/efficiency | ||||
| Fail, n (%) | 12 (6.030) | 0 | < 0.001 | 32.727 |
| Pass, n (%) | 137 (68.844) | 59 (29.648) | – | – |
| Excellent, n (%) | 50 (25.126) | 140 (70.352) | – | – |
| Score | 5.352 ± 1.434 | 7.045 ± 1.001 | < 0.001 | −23.634 |
| Overall clinical competence | ||||
| Fail, n (%) | 16 (8.040) | 0 | < 0.001 | 59.244 |
| Pass, n (%) | 127 (63.819) | 50 (25.126) | – | – |
| Excellent, n (%) | 56 (28.141) | 149 (74.874) | – | – |
| Score | 5.573 ± 1.640 | 7.116 ± 0.933 | < 0.001 | −18.776 |
| Time | 52.387 ± 7.635 | 66.985 ± 9.126 | < 0.001 | −18.776 |
Comparison of Mini Clinical Evaluation Exercise (Mini-CEX) scores and time between control and experimental groups.
3.1.1 Score comparison between the two groups
Before the training, the overall failure rate was 2.513%, the pass rate was 70.352%, and the excellence rate was 27.136%. Among the various competencies, humanistic qualities/professionalism and overall clinical competence had the highest scores, while physical examination and clinical judgment had the lowest scores. After the training, the overall failure rate dropped to 0%, the pass rate decreased to 19.598%, and the excellence rate increased to 80.402%. At this stage, clinical judgment (5.899 ± 1.330) and overall clinical competence (52.387 ± 7.635) had the highest scores, while physical examination (median score: 4) and consultation/advice/communication skills (median score: 5) had the lowest scores (see Figure 2). The failure rates for all evaluation categories in the control group were significantly higher than those in the experimental group, while the rates of excellence in the experimental group were higher than those in the control group. The differences between the groups were statistically significant (p < 0.05). Specifically, in the experimental group, the pass rates for patient interview/medical communication skills, humanistic qualities/professionalism, clinical judgment, consultation/advice/communication skills, organizational skills/efficiency, and overall clinical competence were all lower than those in the control group, with statistically significant differences between the groups (p < 0.05) (Table 1).
3.1.2 Differences before and after using the Check-list
After using the Check-list, there was a significant improvement in all competency scores (Table 1). The increases in scores for various competencies, ranked from highest to lowest, were as follows: clinical judgment > physical examination > organizational skills/efficiency > medical interviewing skills > overall clinical competence > humanistic care/professionalism > consultation/advice/communication skills (Figure 2). Except for the comparisons between medical interviewing skills vs. organizational skills/efficiency, medical interviewing skills vs. overall clinical competence, and physical examination vs. organizational skills/efficiency, all other pairwise comparisons showed statistically significant differences (p < 0.05) (Figure 2).
3.1.3 Comparison of Mini-CEX scores and diagnosis/treatment times between the control and experimental groups
The control group had a median Mini-CEX score of 34.000 (IQR: 28.000, 46.000) and had an average time of 52.387 ± 7.635 min. In contrast, the experimental group had a significantly higher average Mini-CEX score of 48.15 ± 6.63 and had a longer time (66.985 ± 9.263 min). The differences between the two groups were statistically significant (p < 0.05), as detailed in Table 1.
3.2 Correlation analysis of different indicators
3.2.1 Correlation of variables prior to the use of the scale
Correlation analysis showed that before using the Check-list, there was a strong correlation among the seven indicators assessed by the Mini-CEX (p < 0.05). Specifically, the correlation coefficients between the total Mini-CEX score and the medical interviewing skills, physical examination, and overall clinical competence were 0.964, 0.952, and 0.958, respectively (p < 0.001). The correlation between various indicators was high (ρ ≥ 0.50) too, whereas the correlation between time and each of the indicators was weak (ρ < 0.50) (Figure 3).
3.2.2 Correlation among variables after the use of the scale
After using the Check-list, the correlations among the seven Mini-CEX indicators remained strong. The correlation coefficients between the total Mini-CEX score and medical interviewing skills, physical examination, and overall clinical competence were 0.893, 0.909, and 0.880, respectively (p < 0.001). However, the time showed a negative correlation with each of the indicators, though these correlations were weaker (p < 0.05, ρ < 0.50) (Figure 3).
3.2.3 Pairwise comparison and correlation analysis of the differences in each indicator before and after using the scale
In the differences observed among the indicators after using the Check-list, the correlation coefficients between the total Mini-CEX score and medical interviewing skills, clinical judgment, and overall clinical competence were 0.815, 0.800, and 0.867, respectively (p < 0.001). The time was positively correlated with each of the indicators, with a strong correlation only with the total Mini-CEX score (ρ < 0.509); the correlations with other indicators were relatively weak (p < 0.05, ρ < 0.50) (Figure 3).
3.2.4 Correlation analysis of the same indicators before and after using the scale
Except for the time indicator (p = 0.0313, ρ = 0.153), all other clinical competence-related indicators demonstrated a significant positive correlation before and after the use of the scale (p < 0.001). The correlations, ranked from highest to lowest, were as follows: total CEX score (0.945), physical examination (0.894), medical interviewing skills (0.882), advice/consultation/communication skill (0.848), humane qualities/professionalism (0.846), clinical judgment (0.844), overall clinical competence (0.815), and organizational skill and efficiency (0.710) (Figure 3).
3.3 ROC curve analysis
The ROC curve was used to perform sensitivity and specificity analysis based on the relationship between various indicators and scores before and after the use of the Check-list. The AUC for medical interviewing skills, physical examination, humanistic qualities/professionalism, clinical judgment, consultation/advice/communication skills, organizational skills/efficiency, overall clinical competence, Mini-CEX score, and time required were 0.770, 0.774, 0.716, 0.844, 0.733, 0.815, 0.764, 0.797, and 0.881, respectively, all indicating diagnostic efficacy (p < 0.05). These factors had a diagnostic efficacy on the total scores, as shown in Figure 4. Comparisons of the ROC curves for the seven indicators revealed that there was no statistically significant difference between overall clinical competence vs. clinical judgment, consultation/advice/communication skills, vs. humanistic qualities/professionalism, and physical examination vs. medical interviewing skills (p > 0.05). However, all other pairwise comparisons showed statistically significant differences (p < 0.05), as detailed in Figure 4.
4 Discussion
With soaring healthcare demand and increasingly stringent patient-safety standards (27), training competent emergency and critical-care physicians has become a worldwide challenge (28–30). In China, this problem is amplified because teaching is still dominated by lecture-based formats with little active or bedside learning (31–34). Our baseline evaluation quantifies this gap: only 27.136% of residents achieved an “excellent” rating, whereas > 20% failed key domains of clinical judgment and physical examination—skills indispensable for managing critically ill patients (35, 36). Several structural factors in China’s critical-care system further widen these deficits. First, critically ill patients often deteriorate rapidly (e.g., shock) and therefore require systematic diagnostic skills (37, 38), yet junior physicians struggle because of limited experience (39, 40). Second, compared with their Western counterparts, Chinese clinicians work under heavier pressures—from staffing shortages to complex workplace dynamics—leading to higher levels of anxiety, burnout, and other mental-health risks (41). Third, an over-emphasis on classroom teaching, an intensive research-productivity culture (42, 43), and rigid departmental management continually impede residents’ professional development (44, 45). Finally, although diagnostic technology has advanced, over-reliance on imaging and laboratory data is eroding foundational skills such as history-taking and physical examination (46–48); in complex critical illness this further elevates diagnostic-error risk (49). Collectively, these findings show that conventional instruction can no longer meet the demands of high-acuity care in China and underscore the need for a structured, competency-based intervention that combines check-list-guided standardization with Mini-CEX longitudinal assessment.
To address these challenges, educators have adopted tools such as the Mini-CEX to assess clinical competence (50). However, its standalone use remains insufficient to rapidly enhance junior physicians’ clinical judgment and therapeutic skills or reduce the high rate of medical errors in critically ill patients—estimated at 9 per 100 patients daily, with 10% deemed severe (51, 52)—largely due to limited experience, inadequate training, poor communication, and weak emergency responsiveness (53–55). Our results demonstrated that the checklist significantly improved scores across all assessed domain, standardizing clinical processes, and improving diagnostic efficiency (17–19). In this study, the introduction of checklists significantly improved performance across all assessed competencies, particularly in clinical judgment and physical examination (p < 0.05), further validating their value in clinical practice. This impact may stem from ICU physicians conducting structured assessments and treatment planning based on checklist steps, enabling even inexperienced doctors to follow protocols effectively under guideline-based supervision, thereby reducing the risk of misdiagnosis or oversight. Moreover, strong positive correlations were observed among various clinical competencies (p < 0.05), suggesting mutual reinforcement between them. ROC analysis further demonstrated that the checklist had the highest predictive accuracy for clinical judgment (AUC = 0.844) and organizational skills/efficiency (AUC = 0.815), likely reflecting its structured, guideline-driven design. Enhanced clinical judgment was also associated with improved performance in physical examination (AUC = 0.774) and medical interviewing skills (AUC = 0.770), which contributed to minimizing redundant procedures and diagnostic errors, ultimately improving overall clinical competence.
Although all competencies were improved through training, deficiencies remain in humanistic qualities/professionalism, as well as in consultation/advice/communication skills. These areas continue to pose significant challenges within the Chinese healthcare system. Our ROC curve analysis showed that improvements in humanistic qualities/professionalism and consultation/communication skills did not reach statistical significance (p > 0.05). This may reflect structural flaws in the current evaluation system: (many existing checklists use binary (“yes” or “no”) formats and lack graded criteria or practical guidance, a limitation noted in prior studies (51–59). Deeper systemic factors further exacerbate this problem. Frequent medical disputes (57) have led to the widespread adoption of defensive medical practices. Simultaneously, reforms such as the Diagnosis-Related Group (DRG) payment system (58) and healthcare cost-control policies (41) have significantly limited the time and energy available for clinicians to cultivate humanistic qualities. Moreover, persistent clinical and administrative burdens (54) have contributed to widespread occupational burnout, eroding professional identity and perpetuating a vicious cycle of reduced empathy and job dissatisfaction (60). This “institutional pressure–behavioral distortion–competency degradation” cascade not only hampers the development of humanistic values among medical trainees but also undermines the quality of clinical education. Given its deeply rooted institutional nature, this issue cannot be effectively resolved through technical interventions alone.
Some studies have shown that the use of checklists may lead to longer diagnostic and treatment times (17), which is consistent with the findings of this study. Our results indicate that the application of the checklist significantly increased the time (66.985 ± 9.126 vs. 52.387 ± 7.635 min). Although this may superficially suggest a decline in clinical efficiency, the overall comparison of overall clinical competence scores indicates an actual improvement in efficiency. This improvement may be attributed to the checklist’s ability to enhance the accuracy and standardization of physical examination, medical interviewing skills, and treatment procedures, thereby reducing omissions and errors (18). If feasible, future studies should further investigate the relationship between diagnostic/treatment duration, clinical efficiency, and competency outcomes through large-scale, multicenter clinical trials.
In conclusion, this study used the Mini-CEX as a validation tool to assess whether checklist-guided instruction is superior to traditional training in improving residents’ clinical competence. Our findings demonstrate that combining the procedural rigor of checklists with the formative, holistic evaluation of Mini-CEX offers a promising training model. This dual approach not only enhances key clinical skills—especially clinical judgment and efficiency—but also strengthens emergency response and bridges the gap between theoretical knowledge and practical application. However, ongoing adaptation is needed to address non-technical skill gaps and meet evolving healthcare demands.
5 Limitations
(1) The study may have focused only on the short-term effects of the training without tracking the long-term improvement and stability of clinical skills. (2) External factors such as hospital resources, the baseline competency levels of resident physicians, and the educational environment may have influenced the training outcomes but were not fully explored in this study. (3) The study was conducted in China, and cultural and regional differences might affect the generalizability of the results internationally. Different healthcare systems and educational approaches in other countries may require alternative evaluation tools or training methods. (4) Although the ROC curve analysis provided data on diagnostic efficacy, the direct impact on actual clinical outcomes (such as patient outcomes) was not assessed. (5) The COVID-19 pandemic (2020–2022) affected the availability of residents for enrollment due to changes in clinical rotations and staffing demands. This resulted in a slower recruitment rate and extended the overall study duration. However, the training design, assessment procedures, and quality standards were consistently maintained throughout the study period.
Statements
Data availability statement
The original contributions presented in this study are included in this article/supplementary material, further inquiries can be directed to the Corresponding authors.
Ethics statement
The studies involving humans were approved by the Ethics Committee of the First Affiliated Hospital of the University of Science and Technology of China (Anhui Provincial Hospital), ethics approval code 2024-ky-412. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent from the patients was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author contributions
X-gC: Writing – original draft, Writing – review and editing. H-cJ: Conceptualization, Data curation, Investigation, Software, Writing – review and editing. X-fZ: Conceptualization, Data curation, Investigation, Validation, Writing – review and editing. HM: Writing – original draft, Writing – review and editing. MS: Conceptualization, Investigation, Visualization, Writing – review and editing. J-xH: Data curation, Formal Analysis, Investigation, Supervision, Validation, Writing – review and editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
Xiong W Deng Y Yang Y Zhang Y Pan J . Assessment of medical service pricing in china’s healthcare system: Challenges, constraints and policy recommendations.Front Public Health. (2021) 9:787865. 10.3389/fpubh.2021.787865
2.
GBD 2021 Diseases and Injuries Collaborators. Global incidence, prevalence, YLDs, DALYs and HALE for 371 diseases and injuries, 1990-2021: A systematic analysis for the global burden of disease study 2021. Lancet. (2024) 403:2133–61. 10.1016/S0140-673600757-8
3.
GBD 2019 Human Resources for Health Collaborators. Measuring the availability of human resources for health and its relationship to universal health coverage, 1990-2019. Lancet. (2022) 399:2129–54. 10.1016/S0140-673600532-3
4.
Frenk J Chen L Bhutta Z Cohen J Crisp N Evans T . Health professionals for a new century: Transforming education to strengthen health systems in an interdependent world.Lancet. (2010) 376:1923–58. 10.1016/S0140-673661854-5
5.
Tyrrell E Knox R Saha R Berry K Taggar J . Comparison of the effectiveness of exclusively facilitated clinical teaching as an alternative to traditional practice-based primary care placements.Educ Prim Care. (2023) 34:152–60. 10.1080/14739879.2023.2217795
6.
Bansal A Singh D Thompson J Kumra A Jackson B . Developing medical students’ broad clinical diagnostic reasoning through GP-facilitated teaching in hospital placements.Adv Med Educ Pract. (2020) 11:379–88. 10.2147/AMEP.S243538
7.
Du B Xi X Chen D Peng J . Clinical review: Critical care medicine in mainland China.Crit Care. (2010) 14:206. 10.1186/cc8222
8.
Cong Y . Ethical challenges in critical care medicine: A Chinese perspective.J Med Philos. (1998) 23:581–600. 10.1076/jmep.23.6.581.2558
9.
Yu S Zou F Wang Q Zhou K Jian R Jin Y . Willingness to practice medicine and related influential factors among medical undergraduates during COVID-19: A cross-sectional study.BMC Med Educ. (2023) 23:427. 10.1186/s12909-023-04418-7
10.
Hu Y Zhang S Zhai J Wang D Gan X Wang F et al Relationship between workplace violence, job satisfaction and burnout among healthcare workers in mobile cabin hospitals in China. Prev Med Rep. (2024) 40:102667. 10.1016/j.pmedr.2024.102667
11.
Nilsson M Pilhammar E . Professional approaches in clinical judgements among senior and junior doctors: Implications for medical education.BMC Med Educ. (2009) 9:25. 10.1186/1472-6920-9-25
12.
Yon K Nettleton S Walters K Lamahewa K Buszewicz M . Junior doctor’ experiences of managing patients with medically unexplained symptoms: A qualitative study.BMJ Open. (2015) 5:e009593. 10.1136/bmjopen-2015-009593
13.
Norcini J Blank L Duffy F Fortna G . The mini-CEX: A method for assessing clinical skills.Ann Intern Med. (2003) 138:476–81. 10.7326/0003-4819-138-6-200303180-00012
14.
Martinsen S Espeland T Berg E Samstad E Lillebo B Slørdahl T . Examining the educational impact of the mini-CEX: A randomised controlled study.BMC Med Educ. (2021) 21:228. 10.1186/s12909-021-02670-3
15.
Mortaz Hejri S Jalili M Masoomi R Shirazi M Nedjat S Norcini J . The utility of mini-clinical evaluation exercise in undergraduate and postgraduate medical education: A BEME review.Med Teach. (2020) 42:125–42. 10.1080/0142159X.2019.1652732
16.
Humphrey-Murto S Côté M Pugh D Wood T . Assessing the validity of a multidisciplinary mini-clinical evaluation exercise.Teach Learn Med. (2018) 30:152–61. 10.1080/10401334.2017.1387553
17.
Ferorelli D Benevento M Vimercati L Spagnolo L De Maria L Caputi A . Improving healthcare workers’ adherence to surgical safety checklist: The impact of a short training.Front Public Health. (2022) 9:732707. 10.3389/fpubh.2021.732707
18.
Sotto K Burian B Brindle M . Impact of the WHO Surgical Safety Checklist relative to its design and intended use: A systematic review and meta-meta-analysis.J Am Coll Surg. (2021) 233:794–809.e8. 10.1016/j.jamcollsurg.2021.08.692
19.
Storesund A Haugen A Wæhle H Mahesparan R Boermeester M Nortvedt M . Validation of a Norwegian SURPASS in combination with the WHO surgical safety checklist.BMJ Open Qual. (2019) 8:e000488. 10.1136/bmjoq-2018-000488
20.
Fourcade A Blache J Grenier C Bourgain J Minvielle E . Barriers to staff adoption of a surgical safety checklist.BMJ Qual Saf. (2012) 21:191–7. 10.1136/bmjqs-2011-000094
21.
Dharampal N Cameron C Dixon E Ghali W Quan M . Attitudes and beliefs about the surgical safety checklist: Just another tick box?Can J Surg. (2016) 59:268–75. 10.1503/cjs.002016
22.
He Y Holroyd E Koziol-McLain J . Understanding workplace violence against medical staff in China: A retrospective review of publicly available reports.BMC Health Serv Res. (2023) 23:660. 10.1186/s12913-023-09577-3
23.
Zhang L Sun L . Impacts of diagnosis-related groups payment on healthcare providers’ behaviour in China: A cross-sectional study.Risk Manag Healthc Policy. (2021) 14:2263–76. 10.2147/RMHP.S308183
24.
Zakerkish M Shakurnia A Hafezi A Maniati M . Association between burnout and empathy in medical residents.PLoS One. (2024) 19:e0301636. 10.1371/journal.pone.0301636
25.
Soemantri D Dodds A Mccoll G . Examining the nature of feedback within the mini clinical evaluation exercise (Mini-CEX): An analysis of 1427 Mini-CEX assessment forms.GMS J Med Educ. (2018) 35:Doc47. 10.3205/zma001193
26.
Henrico K Makkink A . Use of global rating scales and checklists in simulation-based assessments: Protocol for a scoping review.BMJ Open. (2023) 13:e065981. 10.1136/bmjopen-2022-065981
27.
Astier-Peña M Martínez-Bianchi V Torijano-Casalengua M Ares-Blanco S Bueno-Ortiz J Férnandez-García M . The global patient safety action plan 2021-2030: Identifying actions for safer primary health care.Aten Prim. (2021) 53:102224. 10.1016/j.aprim.2021.102224
28.
Herron L Phillips G Brolan C Mitchell R O’Reilly G Sharma D . “When all else fails you have to come to the emergency department”: Lessons on emergency-care resilience in Pacific Island nations during COVID-19.Lancet Reg Health West Pac. (2022) 25:100519. 10.1016/j.lanwpc.2022.100519
29.
Mitchell R Bornstein S Piamnok D Sebby W Kingston C Tefatu R et al Multimodal learning for ED triage implementation: Experiences from Papua New Guinea during COVID-19. Lancet Reg Health West Pac. (2023) 33:100683. 10.1016/j.lanwpc.2023.100683
30.
Mitchell R White L Elton L Luke C Bornstein S Atua V . Triage implementation in resource-limited emergency departments: Tools and experience from the Pacific region.Int J Emerg Med. (2024) 17:21. 10.1186/s12245-024-00583-8
31.
Wang J Xu Y Liu X Xiong W Xie J Zhao J . Effectiveness of problem-based learning in physical diagnostics education in China: A meta-analysis.Sci Rep. (2016) 6:36279. 10.1038/srep36279
32.
Gao J Yang L Zhao J Wang L Zou J Wang C et al Problem-based vs traditional teaching in medical psychology education in China: A systematic review and meta-analysis. PLoS One. (2020) 15:e0243897. 10.1371/journal.pone.0243897
33.
Xu H Li Q Xie D Wang J Zhang M . Performance of PBL-based image teaching in clinical emergency teaching.Comput Math Methods Med. (2022) 2022:6096688. 10.1155/2022/6096688
34.
Zheng Q Li Y Yin Q Zhang N Wang Y Li G . Problem-based vs lecture-based learning in surgical education: A systematic review and meta-analysis.BMC Med Educ. (2023) 23:546. 10.1186/s12909-023-04531-7
35.
Windish D Paulman P Goroll A Bass E . Do clerkship directors think medical students are prepared for the clerkship years?Acad Med. (2004) 79:56–61. 10.1097/00001888-200401000-00013
36.
Du L Zhao L Xu T Wang Y Zu W Huang X et al Blended learning vs traditional teaching: A systematic review and meta-analysis in nursing education. Nurse Educ Pract. (2022) 63:103354. 10.1016/j.nepr.2022.103354
37.
Pandey S . Sepsis, management & advances in metabolomics.Nanotheranostics. (2024) 8:270–84. 10.7150/ntno.94071
38.
Shankar-Hari M Phillips G Levy M Seymour C Liu V Deutschman C et al Developing a new definition and assessing new clinical criteria for septic shock (Sepsis-3). JAMA. (2016) 315:775–87. 10.1001/jama.2016.0289
39.
Monrouxe L Grundy L Mann M John Z Panagoulas E Bullock A et al How prepared are UK medical graduates for practice? A rapid review (2009-2014). BMJ Open. (2017) 7:e013656. 10.1136/bmjopen-2016-013656
40.
Tallentire V Smith S Skinner J Cameron H . Preparedness of UK graduates in acute care: A systematic literature review.Postgrad Med J. (2012) 88:365–71. 10.1136/postgradmedj-2011-130232
41.
Sun L Zhang W Cao A . Associations between work-related variables and workplace violence among Chinese medical staff.Front Public Health. (2023) 10:1043023. 10.3389/fpubh.2022.1043023
42.
Liao D Long Y Yu T Kang X Liu S Yan J et al EMS personnel PTSD and psychological detachment: Mediating role of presenteeism. Front Public Health. (2023) 11:1030456. 10.3389/fpubh.2023.1030456
43.
Gqaleni T Bhengu B . Patient-safety incident reporting as an indicator of quality nursing in critical-care units in KwaZulu-Natal, South Africa.Health SA. (2020) 25:1263. 10.4102/hsag.v25i0.1263
44.
Schmidt M Lambert S Klasen M Sandmeyer B Lazarovici M Jahns F . Safety management in times of crisis: Lessons from German ICUs during COVID-19.Front Med (Lausanne). (2022) 9:988746. 10.3389/fmed.2022.988746
45.
Panagioti M Khan K Keers R Abuzour A Phipps D Kontopantelis E et al Prevalence, severity and nature of preventable patient harm: Systematic review and meta-analysis. BMJ. (2019) 366:l4185. 10.1136/bmj.l4185
46.
Huang C Barwise A Soleimani J Dong Y Svetlana H Khan S et al Clinicians’ perceptions of diagnostic errors in acutely ill patients. J Patient Saf. (2022) 18:e454–62. 10.1097/PTS.0000000000000840
47.
Likic R Maxwell S . Prevention of medication errors: Teaching and training.Br J Clin Pharmacol. (2009) 67:656–61. 10.1111/j.1365-2125.2009.03423.x
48.
Kogan J Holmboe E Hauer K . Tools for direct observation and assessment of clinical skills of medical trainees: A systematic review.JAMA. (2009) 302:1316–26. 10.1001/jama.2009.1365
49.
Graber M Franklin N Gordon R . Diagnostic error in internal medicine.Arch Intern Med. (2005) 165:1493–9. 10.1001/archinte.165.13.1493
50.
Sharma R Gupta T Haidery T Sinha S Kumar A . Current trends in mini-clinical evaluation exercise in medical education: A bibliometric analysis.Cureus. (2022) 14:e33121. 10.7759/cureus.33121
51.
Rothschild J Landrigan C Cronin J Kaushal R Lockley S Burdick E et al The critical care safety study: Incidence and nature of adverse events and serious medical errors in intensive care. Crit Care Med. (2005) 33:1694–700. 10.1097/01.ccm.0000171609.91035.bd
52.
Valentin A Capuzzo M Guidet B Moreno R Dolanski L Bauer P et al Patient safety in intensive care: Results from the sentinel events evaluation study. Intensive Care Med. (2006) 32:1591–8. 10.1007/s00134-006-0290-7
53.
Ellen M Wilson M Vélez M Shach R Lavis J Grimshaw J et al Addressing overuse of health services in health systems: A critical interpretive synthesis. Health Res Policy Syst. (2018) 16:48. 10.1186/s12961-018-0325-x
54.
Windover A Martinez K Mercer M Neuendorf K Boissy A Rothberg M . Correlates and outcomes of physician burnout within a large academic medical center.JAMA Intern Med. (2018) 178:856–8. 10.1001/jamainternmed.2018.0019
55.
Yu J Gao J Chen J Sun Y . Academic versus non-academic neurosurgeons in China: Workload, burnout and engagement.BMJ Open. (2019) 9:e028309. 10.1136/bmjopen-2018-028309
56.
Burian B Clebone A Dismukes K Ruskin K . More than a tick box: Medical checklist development, design and use.Anesth Analg. (2018) 126:223–32. 10.1213/ANE.0000000000002286
57.
Wu Y Fung H Shum H Zhao S Wong E Chong K et al DRG-based internal resource allocation in Hong Kong public hospitals: Outcomes analysis. JAMA Netw Open. (2022) 5:e2145685. 10.1001/jamanetworkopen.2021.45685
58.
Guo L Du X Wu H Xia S Du J Kong X et al Factors associated with healthcare-seeking behaviour under China’s hierarchical system. Front Public Health. (2024) 12:1326272. 10.3389/fpubh.2024.1326272
59.
Xiao Y Dong D Zhang H Chen P Li X Tian Z et al Burnout and well-being among medical professionals in China: A national cross-sectional study. Front Public Health. (2022) 9:761706. 10.3389/fpubh.2021.761706
60.
Quantrill S Tun J . Workplace-based assessment as an educational tool: Guide supplement 31.5.Med Teach. (2012) 34:417–8. 10.3109/0142159X.2012.668234
Summary
Keywords
Mini-CEX, Check-list, emergency and critical care, medical education, medical training
Citation
Cao X-g, Hu J-x, Jian H-c, Zhu X-f, Meng H and Shao M (2025) The combined application of Mini-CEX and Check-list Scales in enhancing clinical competence among emergency and critical care residents: a comparative study. Front. Med. 12:1492206. doi: 10.3389/fmed.2025.1492206
Received
06 September 2024
Accepted
19 June 2025
Published
11 July 2025
Volume
12 - 2025
Edited by
Ahsan Sethi, Qatar University, Qatar
Reviewed by
Weimin Wang, Peking University, China
Liesl Visser, Mohammed Bin Rashid University of Medicine and Health Sciences, United Arab Emirates
Yuejia Huang, Johns Hopkins University, United States
Updates
Copyright
© 2025 Cao, Hu, Jian, Zhu, Meng and Shao.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Huadong Meng, 471989325@qq.comMin Shao, 514507999@qq.com
†These authors share first authorship
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.