Abstract
Background:
Consensus on the use of citrate vs.heparin for catheter locking remains elusive, with ongoing controversy. This meta-analysis investigates the efficacy and safety of citrate lock solutions compared to heparin lock solutions in preventing catheter-related complications.
Methods:
The review process was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Two independent reviewers conducted literature searches based on preferred reporting items from systematic reviews and meta-analyses. PubMed, EMBASE, Medline, and the Cochrane Library were searched for studies comparing citrate and heparin in patients with catheter. Catheter-related bloodstream infection (CRBSI), catheter-related infection (CRI), exit-site infection (ESI), and adverse events were analyzed.
Results:
The meta-analysis included 17 randomized controlled trials (RCTs), encompassing 247,431 catheter-days, with 128,904 in the citrate group, and 118,527 in the heparin group. Citrate lock solutions significantly reduced the incidence of CRBSI compared to heparin (RR: 0.48, 95% CI: 0.31–0.73), particularly when combined with antibiotics or used at low concentrations. No significant differences were observed between the groups for CRI, ESI, catheter dysfunction, or local bleeding. Subgroup and sensitivity analyses addressed heterogeneity, confirming the robustness of the primary findings.
Conclusions:
Citrate lock solutions effectively prevent CRBSI without increasing systemic coagulation dysfunction or bleeding risk. Citrate lock solutions are a safe and effective alternative to heparin, especially when combined with antibiotics.
Systematic review registration:
https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42024562511.
Introduction
Vascular catheter pathways are widely used in clinical settings, particularly in intensive care units, chemotherapy, hemodialysis, and long-term parenteral nutrition (1, 2). Currently, the most commonly used devices include central venous catheters (CVCs), non-tunneled-uncuffed catheters (NTCs), tunneled-cuffed catheters (TCCs), peripherally inserted central catheters (PICCs), and totally implantable venous access ports (TIVAPs) to address the needs of patients requiring long-term intravenous infusions or hemodialysis (3, 4).
Catheter-related bloodstream infection (CRBSI) is one of the most serious complications associated with vascular catheters. The incidence of CRBSI is influenced by factors such as catheter type (5), patient conditions (including advanced age, diabetes, hypoproteinemia, and prolonged steroid or immunosuppressive therapy) (6–8), operator experience (9), and the duration of catheter placement (10, 11). Among these, ICU patients with implanted CVCs and hemodialysis patients with NTC or TCC catheters are most commonly affected, with hemodialysis patients using NTCs being more susceptible to CRBSI compared to those using TCCs (12). The occurrence of CRBSI not only extends the patient's hospital stay but also increases medical costs and mortality rates.
Ensuring catheter patency through appropriate locking is crucial for the effective prevention of thrombosis and CRBSI during the use of central venous catheters. Therefore, exploring effective catheter locking methods to prevent CRBSI caused by intravascular catheters holds significant clinical importance. Citrate, as a local anticoagulant, chelates serum calcium ions without affecting systemic coagulation function and also possesses antibacterial properties. Its use in catheter locking is becoming increasingly widespread.
However, there is no consensus on the superiority of citrate vs. heparin locking solutions for catheter locking, and some controversy remains. Thus, this study aims to compare the efficacy of citrate and citrate lock solutions combined with antibiotics, vs. heparin locking solutions, in preventing catheter-related complications through a meta-analysis, providing a reference for clinical practice.
Methods
This meta-analysis was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and has been reported in line with the AMSTAR (Assessing the methodological quality of systematic reviews) Guideline (13, 14). The protocol for this meta-analysis was registered on PROSPERO (registration ID: CRD42024562511).
Inclusion criteria
-
(1) Clinical studies comparing citrate and heparin lock solutions in the prevention of catheter-related complications;
-
(2) Randomized controlled trials (RCT);
-
(3) Full text available;
-
(4) Participants older than 18 years.
Exclusion criteria
-
(1) Studies if they were letters, case reports, reviews, animal trials, or republished studies;
-
(2) Studies with incomplete or missing data relevant to the analysis will be excluded;
-
(3) Cohort studies, and case-control studies;
-
(4) CVCs used for chemotherapy.
Outcomes
The primary outcome was the CRBSI. The second outcome included Catheter-related infection (CRI), exit-site infection (ESI), and adverse events.
Search strategy
Two of the authors performed the search in PubMed, EMBASE, Medline, and the Cochrane Central Register of Controlled Trials from the inception dates to July 2024, using the keywords “citrate”, “heparin”, “locking solution”, and “infection”. No language restrictions were applied during the search.
Data collection process
Two investigators used a standard data extraction form to extract all related data from selected trials independently. Data extracted included the first author's name, year of publication, country, participants, CVC type, patients setting, locking solution, sample size, catheter-days, sex, age, and related outcomes. Disagreements were resolved by consensus.
Assessment of risk of bias and quality of evidence
Two researchers independently assessed the quality of RCTs using the Cochrane risk-of-bias criteria (15). When they consider their methods, researchers decide whether those assessing the risk of bias will be blinded to the authors' names, institutions, journals, and study results. Disagreements were resolved by consensus.
Data synthesis
The meta-analysis used Stata software (version 17; StataCorp, 2021). Heterogeneity was assessed via the Q-test and calculation of the I2 value. Our analysis employed the random effects model. Relative risk (RR) with corresponding 95% confidence intervals (CI) were used for count outcome assessment. Statistical significance was denoted by a P-value below 0.05. When dealing with multiple correlated comparisons in the same experiment, following the guidance provided by the Cochrane Handbook, which combine groups to create a single pair-wise comparison (16).
Sensitivity analyses
We performed a sensitivity analysis by excluding individually trials.
Results
Eligible studies
Initially, a total of 202 relevant articles were identified. After removing 70 duplicate articles, 132 articles remained. Screening the titles and abstracts of these articles led to the exclusion of 89 irrelevant articles. The full texts of the remaining 43 articles were reviewed, resulting in the exclusion of 29 studies. These exclusions included 6 conference abstracts, 6 studies with outcomes not relevant to our research, 3 studies with no results, 4 non-randomized controlled trials, 4 duplicate studies, 3 studies not comparing sodium citrate vs. heparin, 2 studies involving children, and 1 study involving patients with hematological malignancies undergoing intensive chemotherapy. Three studies from previous research were included, bringing a total of 17 trials included in our meta-analysis (17–33). The search detail was shown in Figure 1.
Figure 1

Flow diagram for search and selection of included studies.
Quality of trials
The quality of the included studies was assessed using the Cochrane risk-of-bias tool. Seven studies were of high quality, eight had moderate quality, and two had low quality. The primary sources of bias were the blinding of participants and personnel (Figure 2).
Figure 2

Risk of bias summary.
CRBSI
A total of 15 studies reported on CRBSI. The results indicated that the risk of CRBSI was significantly lower in the citrate lock solution group compared to the heparin lock solution group (RR: 0.48, 95% CI: 0.31–0.73, P = 0.001, I2 = 57.5%; Figure 3). Moderate heterogeneity was observed in the results. To address this, we considered whether the addition of antibiotics to citrate solutions could be a source of heterogeneity and conducted a subgroup analysis based on the presence of antibiotics in the citrate solution. The subgroup analysis revealed that citrate solutions without antibiotics did not significantly reduce the incidence of CRBSI (RR: 0.64, 95% CI: 0.35–1.16, P = 0.141, I2 = 68.3%; Figure 4A). In contrast, citrate solutions containing antibiotics significantly reduced the incidence of CRBSI (RR: 0.36, 95% CI: 0.24–0.54, P < 0.001, I2 = 0%; Figure 4A). Additionally, we conducted a subgroup analysis based on the concentration of citrate in the solution. For citrate combined with antibiotics, all solutions were of low concentration, and the results were consistent with those mentioned above. For citrate without antibiotics, the analysis was divided into low- and high-concentration groups. In the low-concentration subgroup, citrate demonstrated a significant reduction in CRBSI incidence compared to heparin (RR: 0.44, 95% CI: 0.27–0.73, P = 0.001, I2 = 0%; Figure 4B). However, in the high-concentration subgroup, no significant difference was observed between the two groups (RR: 0.82, 95% CI: 0.31–2.17, P = 0.682, I2 = 79.7%; Figure 4B). Notably, the high-concentration subgroup exhibited substantial heterogeneity, which resolved (I2 = 0%) upon excluding the study by Weijmer et al. (33), with the conclusion remaining unchanged.
Figure 3

Forest plot for catheter-related bloodstream infection.
Figure 4

Subgroup analysis for catheter-related bloodstream infection [Citrate solutions with and without antibiotics (A); Low-, low+antimicrobial, and high-concentration citrate solutions (B)].
CRI
Four studies reported on the incidence of CRI, with the citrate group comprising 9,099 catheter-days and the heparin group comprising 8,161 catheter-days. The aggregated results showed no difference in the incidence of CRI between the citrate and heparin lock solution groups (RR: 0.65, 95% CI: 0.30–1.40, P = 0.272, I2 = 52.6%; Figure 5). Substantial heterogeneity was observed in the studies. Upon analyzing the included literature, we found that four studies did not use antibiotic-containing citrate solutions, whereas the study by Dogra et al. (21) used an antibiotic-containing citrate solution. To further explore the impact of antibiotics, a subgroup analysis was performed based on the presence or absence of antibiotics. In the subgroup without antibiotics, no significant difference was observed between the two groups (RR: 0.77, 95% CI: 0.48–1.23, I2 = 0%; Figure 6). However, in the subgroup with antibiotics, citrate was found to significantly reduce the incidence of CRI (RR: 0.07, 95% CI: 0.01–0.57; Figure 6).
Figure 5

Forest plot for catheter-related infection.
Figure 6

Subgroup analysis for catheter-related infection.
ESI
Seven studies reported on the incidence of ESI, with the citrate group comprising 83,454 catheter-days and the heparin group comprising 74,440 catheter-days. The pooled analysis indicated no significant difference in ESI incidence between the two groups (RR: 0.61, 95% CI: 0.37–1.00, P = 0.052, I2 = 25.5%; Figure 7). A subgroup analysis was performed based on the use of antibiotics, and both subgroups showed no difference in ESI incidence between the two groups (Figure 8A). In the subgroup without antibiotics, high heterogeneity was observed (I2 = 70.6%). After excluding Weijmer et al.'s study (33), the heterogeneity decreased substantially (I2 = 38.9%; Figure 8B), with the conclusion remaining unchanged.
Figure 7

Forest plot for exit-site infection.
Figure 8

Subgroup analysis for exit-site infection [All trials (A); After excluding Weijmer et al.'s (33) trial (B)].
Catheter dysfunction
Six studies reported on catheter dysfunction, with the citrate group comprising 23,322 catheter-days and the heparin group comprising 22,567 catheter-days. The pooled results showed no significant difference in catheter dysfunction between the citrate and heparin lock solution groups (RR: 0.71, 95% CI: 0.48–1.03, P = 0.074, I2 = 54.6%; Figure 9).
Figure 9

Forest plot for catheter dysfunction.
Local bleeding
Four studies, encompassing a total of 31,817 catheter-days, reported on local bleeding. The combined results showed no significant difference in the incidence of local bleeding between the citrate and heparin lock solution groups (RR: 0.52, 95% CI: 0.22–1.22, P = 0.132, I2 = 11.7%; Figure 10).
Figure 10
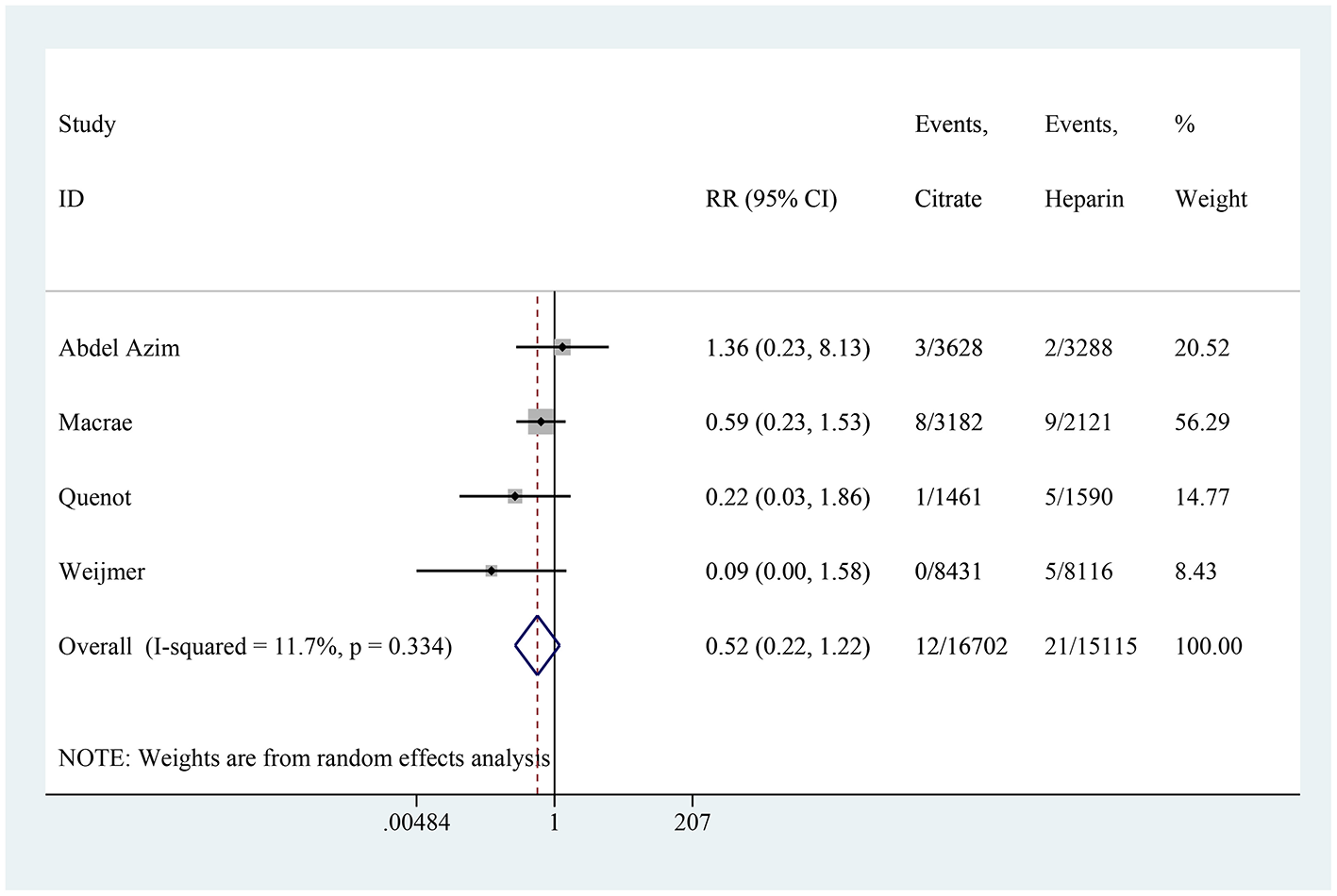
Forest plot for local bleeding.
Meta-regression
Considering that age differences could be a potential source of heterogeneity, we conducted a meta-regression with age as a covariate for CRBSI, CRI, and ESI. The results showed no statistically significant association between age and these outcomes (P > 0.05 for all) (Table 1).
Table 1
| Outcomes | Covariate | Coefficient | SE | Z | P | 95% CI |
|---|---|---|---|---|---|---|
| CRBSI | Age | −0.009 | 0.029 | −0.32 | 0.75 | −0.065, 0.047 |
| CRI | Age | 0.024 | 0.025 | 0.97 | 0.334 | −0.025, 0.073 |
| ESI | Age | 0.026 | 0.082 | 0.32 | 0.75 | −0.134, 0.186 |
Meta-regression analysis of age as a covariate on CRBSI, CRI, and ESI.
CRBSI, Catheter-related bloodstream infection; CRI, Catheter-related infection; ESI, exit-site infection.
Sensitivity analysis
The remaining studies were combined when any individual study was excluded. No particular study had a significant impact on the results.
Publication of bias
Figure 11 shows that small sample studies may be the leading cause of bias.
Figure 11

Funnel plot of the included studies in this meta-analysis for catheter-related bloodstream infection.
Discussion
This meta-analysis included 17 RCTs, comprising 128,904 catheter-days in the citrate group and 118,527 catheter-days in the heparin group. The combined results showed that the citrate group had a significantly lower incidence of CRBSI compared to the heparin group. Considering the substantial heterogeneity of the results, a subgroup analysis was conducted based on whether antibiotics were included in the citrate solution. The results indicated that citrate solutions with antibiotics significantly reduced the incidence of CRBSI, whereas, there was no difference between citrate without antibiotics and heparin lock solutions in CRBSI incidence. Additionally, subgroup analysis based on citrate concentration indicated that low-concentration citrate, with or without antibiotics, significantly reduced CRBSI incidence. In contrast, high-concentration citrate showed no difference between the two groups. There was no difference in the incidence of CRI between the two groups, primarily because the studies included used citrate lock solutions without antibiotics. In the study by Dogra et al., the use of antibiotic-containing citrate lock solution significantly reduced the incidence of CRI compared to heparin lock solution. Citrate showed no significant difference in reducing the incidence of ESI compared to heparin. Sensitivity analysis identified the study by Wenjmer et al. as the primary source of heterogeneity (33). After excluding this study, heterogeneity was significantly reduced, and the conclusion remained unchanged. A possible explanation for this finding is that the study exclusively included patients with newly inserted, well-positioned hemodialysis catheters expected to be used for more than 1 week. To further explore potential sources of heterogeneity, a meta-regression analysis was conducted using age as a covariate for CRBSI, CRI, and ESI. The results showed no statistically significant association between age and these outcomes. For CRBSI, the coefficient was −0.009 (95% CI: −0.065 to 0.047, P = 0.621), indicating a minimal and non-significant negative correlation with age. For CRI, the coefficient was 0.024 (95% CI: −0.025 to 0.073, P = 0.334), suggesting a slight, non-significant positive association. Similarly, for ESI, the coefficient was 0.026 (95% CI: −0.134 to 0.186, P = 0.750), reflecting a negligible and non-significant positive association. These findings suggest that age is unlikely to be a meaningful contributor to the observed heterogeneity, further supporting the robustness of the conclusions. There were no significant differences between the two groups in the incidence of catheter dysfunction and local bleeding. Besides, we attempted to explore potential factors influencing CRBSI, including patient characteristics such as age, comorbidities, and nutritional status. However, after reviewing the included studies, we found that none performed subgroup analyses based on these factors. Although patient conditions such as controlling blood glucose levels in diabetes and enhancing nutritional support may play a significant role in reducing infection risks, the available data did not allow for a detailed subgroup analysis in this context. Therefore, we emphasize the importance of optimizing the overall clinical condition of patients, particularly in terms of managing underlying health conditions, to reduce CRBSI incidence.
Biofilms are complex microbial communities that adhere to the surface of catheters and are a major cause of CRBSIs (34). Citrate can disrupt biofilm formation, thereby reducing the incidence of CRBSI, especially when combined with antibiotics (35, 36). However, in the absence of antimicrobial agents, citrate alone may be insufficient to disrupt established biofilms, resulting in no significant difference compared to heparin (37). CRBSIs are typically caused by contamination within the catheter or by skin microorganisms migrating along the catheter (34). The antimicrobial properties of citrate are more effective within the lumen where the solution is in direct contact with the biofilm (38). On the other hand, puncture occurs at the catheter exit site, where the skin barrier is breached. The chelating action of citrate may help reduce the microbial load at the exit site, thus lowering the incidence of ESI even without added antibiotics. Heparin sodium, commonly used as a locking solution, may cause systemic coagulation dysfunction and bleeding, including complications such as heparin-induced thrombocytopenia, which limits its clinical application to some extent (39, 40). Citrate binds to calcium ions in the blood and breaks down into carbon dioxide and other products, providing anticoagulation without causing systemic coagulation dysfunction or increasing bleeding risk, and it possesses inherent antibacterial activity (41). Our results indicate that citrate significantly reduces the incidence of CRBSI and that citrate without antibiotics is as effective as heparin in preventing ESI and CRI without increasing the occurrence of related complications.
Previous studies (42, 43) have shown that the combined use of citrate and antibiotics (such as gentamicin, taurolidine, EDTA, etc.) can reduce the incidence of sepsis and shorten treatment duration. This meta-analysis also suggests that using citrate locks can better prevent CRBSI. Subgroup analysis shows that the combination of citrate and antibiotic locks effectively prevents CRBI, while the use of citrate alone does not show a statistically significant difference compared to heparin, consistent with our previous research. Our study differs significantly from previous research by including all patients with indwelling catheters, rather than limiting the analysis to hemodialysis patients. This broader inclusion criterion allows for a more comprehensive evaluation of the effectiveness of citrate lock solutions across different patient populations. Previous studies have primarily focused on hemodialysis patients, often excluding other critical groups such as ICU patients, and those requiring long-term parenteral nutrition. By encompassing a wider range of patients, our study provides a more generalized understanding of the benefits of citrate lock solutions. This inclusive approach is particularly important because it reflects real-world clinical settings where various types of catheters are used for different medical purposes. Furthermore, the broader inclusion of various patient populations allows us to observe the safety profile of citrate lock solutions more accurately. Our results indicate that citrate does not cause systemic coagulation dysfunction or increase the risk of bleeding, making it a safer alternative to heparin, especially for patients who are already at a higher risk of bleeding complications.
Limitation
Although this study included only RCTs, several limitations should be noted. First, the follow-up periods varied among the studies, which may contribute to heterogeneity in the results. Second, the inclusion criteria differed, and variations in citrate concentration and the use of antibiotics also increased heterogeneity. Third, the definitions of catheter malfunction listed in Table 2 were not completely consistent, which may cause substantial heterogeneity. Forth, this study is the unable to conduct subgroup analyses based on patient characteristics. Despite these factors potentially influencing the outcomes, the included studies did not perform such subgroup analyses, and therefore, we were unable to assess their direct impact. This is an area for future research, where stratifying by patient condition could provide more tailored recommendations.
Table 2
| Study | Country | Participants | CVC type | Patients setting | Treatment group | Control group | No. of subjects | Catheter-days | Sex (female) | Age | Outcomes | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Citrate | Heparin | Citrate | Heparin | Citrate | Heparin | Citrate | Heparin | ||||||||
| Abdel Azim et al. (17) | Egypt | Hemodialysis patients | NS | Maintenance hemodialysis | 4% citrate | Heparin 5,000 U/mL | 105 | 105 | 3,628 | 3,288 | 47 | 40 | 51.33 ± 11.2 | 51.74 ± 13.1 | CRBSI, CRI, catheter dysfunction, thrombosis, bleeding |
| Barcellos et al. (18) | Brazil | Hemodialysis patients | NS | Maintenance hemodialysis | 30% trisodium citrate | Heparin 5,000 U/mL | 231 | 233 | 6,052 | 6,927 | 121 | 116 | 58.61 ± 17.14 | 57.44 ± 18.27 | CRBSI, catheter dysfunction, adverse event, death |
| Betjes et al. (19) | Netherlands | Hemodialysis patients | Non-tunneled | Maintenance hemodialysis | 4% citrate + 1.35% taurolidine | Heparin 5,000 U/mL | 37 | 39 | 1,519 | 1885 | 16 | 15 | 58.3 ± 16.3 | 50.3 ± 20.4 | CRBSI, catheter dysfunction, adverse event, ESI |
| Buturovic et al. (20) | USA | Hemodialysis patients | NS | Maintenance hemodialysis | 4% trisodium citrate | Heparin 5,000 U/mL | 10 | 10 | 510 | 230 | NA | NA | NA | NA | Catheter dysfunction |
| Filiopoulos et al. (22) | Greece | Hemodialysis patients | Uncuffed | Maintenance hemodialysis | 4% citrate + 1.35% taurolidine | Heparin 5,000 U/mL | 59 | 58 | 2,180 | 2,016 | 26 | 28 | 75 (36–95) | 70 (42–84) | CRBSI, thrombosis, adverse effects |
| Hendrickx et al. (23) | Belgium | Hemodialysis patients | Tunneled | Maintenance hemodialysis | 5% trisodium citrate | Heparin 5,000 U/mL | 10 | 9 | 730 | 640 | 6 | 5 | 74.6 | 71.4 | CRI |
| Joao Luiz et al. (24) | Brazil | Hemodialysis patients | NS | Maintenance hemodialysis | 30% trisodium citrate | Heparin 1,000 IU/mL | 25 | 25 | 2,000 | 1,956 | NA | NA | NA | NA | CRBSI, adverse events |
| Macrae et al. (25) | Canada | Hemodialysis patients | Cuffed | Maintenance hemodialysis | 4% citrate | Heparin 5,000 U/mL | 32 | 29 | 3,182 | 2,121 | 11 | 15 | 63 ± 16 | 69 ± 15 | CRBSI, catheter dysfunction, bleeding, ESI, cost |
| Maki et al. (26) | USA | Hemodialysis patients | Cuffed and tunneled | Maintenance hemodialysis | 7.0% citrate + 0.05% methylene blue + 0.15% methylparaben + 0.015% propylparaben | Heparin 5,000 U/mL | 201 | 206 | 25,274 | 24,395 | 103 | 100 | 62.2 ± 15.4 | 61.7 ± 15.2 | CRBSI, adverse events |
| Moran et al. (27) | USA | Hemodialysis patients | Cuffed and tunneled | Maintenance hemodialysis | 4% citrate + 20 g/mL of gentamicin | Heparin 1,000 U/mL | 155 | 148 | 39,827 | 32,933 | 79 | 67 | 63.4 ± 15.6 | 62.8 ± 16.8 | CRBSI, catheter clotting |
| Power et al. (30) | UK | Hemodialysis patients | Cuffed | Maintenance hemodialysis | 46.7% citrate | Heparin 5,000 U/mL | 132 | 100 | 19,086 | 17,100 | 59 | 41 | 63 ± 14 | 62 ± 13 | CRBSI, adverse events |
| Quenot et al. (31) | France | Critically ill patients | Tunneled | Critically ill patients | 4% trisodium citrate | Heparin 5,000 U/mL | 199 | 197 | 1,461 | 1,590 | 72 | 74 | 69.4 ± 13.4 | 69.5 ± 12.9 | CRBSI, bleeding, thrombosis, death |
| Solomon et al. (32) | England | Hemodialysis patients | Tunneled cuffed | Maintenance hemodialysis | 4% citrate + 1.35% taurolidine | Heparin 5,000 U/mL | 53 | 54 | 8,129 | 9,642 | 27 | 13 | 59.8 ± 14.7 | 56.7 ± 17.4 | CRBSI, ESI, adverse events |
| Weijmer et al. (33) | Belgium | Hemodialysis Patients | Tunneled cuffed and untunneled uncuffed | Maintenance hemodialysis | 30% trisodium citrate | Heparin 5,000 U/mL | 148 | 143 | 8,431 | 8,116 | 87 | 87 | 61.6 ± 14.8 | 61.3 ± 16 | CRBSI, bleeding, adverse events |
| Dogra et al. (21) | Australia. | Hemodialysis patients | Tunneled cuffed | Maintenance hemodialysis | 1.04% citrate + 26.7 mg/mL gentamicin | Heparin 5,000 U/mL | 42 | 37 | 3,280 | 2,643 | 18 | 11 | 55.7 ± 2.5 | 59.3 ± 2.1 | CRBSI, ESI, CRI |
| Pervez et al. (29) | USA | Tunnel catheter placement patients | Tunneled cuffed | Maintenance hemodialysis | 4.6% citrate + 18.2 mg/mL gentamicin | Heparin 1,000 U/mL | 14 | 22 | 1,613 | 1,311 | 4 | 12 | 53.7 ± 4.0 | 47.6 ± 3.3 | CRBSI, thrombosis |
| Nori et al. (28) | USA | Hemodialysis patients | NS | Maintenance hemodialysis | 3.13% citrate + 4 mg/mL gentamicin | Heparin 5,000 U/mL | 20 | 20 | 2,002 | 1,734 | NA | NA | 58 ± 3 | 59 ± 4 | CRBSI |
Characteristics of included studies.
CRBSI, Catheter-related bloodstream infection; CRI, catheter-related infection; ESI, exit-site infection; NA, not applicable; NS, not specified.
Conclusions
Citrate lock solutions offer a dual advantage of anticoagulant and antimicrobial properties, effectively minimizing the risk of systemic coagulation dysfunction and bleeding. When combined with antibiotics, they emerge as a safe and highly effective alternative to heparin, demonstrating significant potential in reducing catheter-related complications. This makes citrate lock solutions a compelling choice for enhancing patient safety and optimizing clinical outcomes in catheter management.
Statements
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
HL: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. BL: Conceptualization, Data curation, Investigation, Methodology, Project administration, Software, Validation, Writing – original draft. WH: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Writing – original draft. HY: Conceptualization, Investigation, Methodology, Project administration, Visualization, Writing – original draft. TC: Methodology, Project administration, Writing – original draft. YG: Methodology, Writing – original draft. WW: Conceptualization, Data curation, Investigation, Methodology, Software, Supervision, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Zhejiang Medicine and Health Scientific Research Project (No. 2024KY531). The funders had no role in the study design, data collection and analysis, decision to publish, or manuscript preparation.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
Huang H Chang Q Zhou Y Liao L . Risk factors of central catheter bloodstream infections in intensive care units: a systematic review and meta-analysis. PLoS ONE. (2024) 19:e0296723. 10.1371/journal.pone.0296723
2.
Takeshita J Tachibana K Nakajima Y Shime N . Incidence of catheter-related bloodstream infections following ultrasound-guided central venous catheterization: a systematic review and meta-analysis. BMC Infect Dis. (2022) 22:772. 10.1186/s12879-022-07760-1
3.
Lai NM Chaiyakunapruk N Lai NA O'Riordan E Pau WS Saint S . Catheter impregnation, coating or bonding for reducing central venous catheter-related infections in adults. Cochrane Database Syst Rev. (2016) 3:Cd007878. 10.1002/14651858.CD010140.pub2
4.
Gadodia G . Central venous access. In:ChandREltoraiAEMHealeyTAhnS, editors. Essential Interventional Radiology Review: A Question and Answer Guide. Cham: Springer International Publishing. (2022). p. 215–43.
5.
Zanoni F Pavone L Binda V Tripepi G D'Arrigo G Scalamogna A et al . Catheter-related bloodstream infections in a nephrology unit: analysis of patient- and catheter-associated risk factors. J Vasc Access. (2021) 22:337–43. 10.1177/1129729820939762
6.
Kumbar L Yee J . Current concepts in hemodialysis vascular access infections. Adv Chronic Kidney Dis. (2019) 26:16–22. 10.1053/j.ackd.2018.10.005
7.
Taylor G Gravel D Johnston L Embil J Holton D Paton S . Incidence of bloodstream infection in multicenter inception cohorts of hemodialysis patients. Am J Infect Control. (2004) 32:155–60. 10.1016/j.ajic.2003.05.007
8.
Allon M . Dialysis catheter-related bacteremia: treatment and prophylaxis. Am J Kidney Dis. (2004) 44:779–91. 10.1016/S0272-6386(04)01078-9
9.
Boulet N Pensier J Occean B-V Peray PF Mimoz O Rickard CM et al . Central venous catheter-related infections: a systematic review, meta-analysis, trial sequential analysis and meta-regression comparing ultrasound guidance and landmark technique for insertion. Crit Care. (2024) 28:378. 10.1186/s13054-024-05162-0
10.
Timsit J-F Baleine J Bernard L Calvino-Gunther S Darmon M Dellamonica J et al . Expert consensus-based clinical practice guidelines management of intravascular catheters in the intensive care unit. Ann Intens Care. (2020) 10:118. 10.1186/s13613-020-00713-4
11.
Fletcher S . Catheter-related bloodstream infection. Continu Educ Anaesth Crit Care Pain. (2005) 5:49–51. 10.1093/bjaceaccp/mki011
12.
Deliberato RO Marra AR Corrêa TD Martino MD Correa L Dos Santos OF et al . Catheter related bloodstream infection (CR-BSI) in ICU patients: making the decision to remove or not to remove the central venous catheter. PLoS ONE. (2012) 7:e32687. 10.1371/journal.pone.0032687
13.
Shea BJ Reeves BC Wells G Thuku M Hamel C Moran J et al . AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. (2017) 358:j4008. 10.1136/bmj.j4008
14.
Page MJ McKenzie JE Bossuyt PM Boutron I Hoffmann TC Mulrow CD et al . The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. 10.1136/bmj.n71
15.
Cumpston M Li T Page MJ Chandler J Welch VA Higgins JP et al . Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev. (2019) 10:Ed000142. 10.1002/14651858.ED000142
16.
Julian Higgins JT Jacqueline C Miranda C Tianjing L Matthew P Vivian W . Cochrane Handbook for Systematic Reviews of Interventions version 6.4 (updated August 2023). Cochrane. (2023). Available at: http://www.training.cochrane.org/handbook (accessed August 08, 2024).
17.
Abdel Azim ABE ElSaid TW El Said HW Hemida W Zaghlool S Ramadan A et al . A randomized controlled clinical trial of 4% sodium citrate versus heparin as locking solution for temporary dialysis catheters among hemodialysis patients Clin Nephrol. (2018) 90:341–9. 10.5414/CN109162
18.
Barcellos FC Nunes BP Valle LJ Lopes T Orlando B Scherer C et al . Comparative effectiveness of 30 % trisodium citrate and heparin lock solution in preventing infection and dysfunction of hemodialysis catheters: a randomized controlled trial (CITRIM trial). Infection. (2017) 45:139–45. 10.1007/s15010-016-0929-4
19.
Betjes MG van Agteren M . Prevention of dialysis catheter-related sepsis with a citrate-taurolidine-containing lock solution. Nephrol Dial Transplant. (2004) 19:1546–51. 10.1093/ndt/gfh014
20.
Buturovic J Ponikvar R Kandus A Boh M Klinkmann J Ivanovich P . Filling hemodialysis catheters in the interdialytic period: heparin versus citrate versus polygeline: a prospective randomized study [Editorial Material]. Artif Organs. (1998) 22:945–7. 10.1046/j.1525-1594.1998.06268.x
21.
Dogra GK Herson H Hutchison B Irish AB Heath CH Golledge C et al . Prevention of tunneled hemodialysis catheter-related infections using catheter-restricted filling with gentamicin and citrate: a randomized controlled study. J Am Soc Nephrol. (2002) 13:2133–9. 10.1097/01.ASN.0000022890.29656.22
22.
Filiopoulos V Hadjiyannakos D Koutis I Trompouki S Micha T Lazarou D et al . Approaches to prolong the use of uncuffed hemodialysis catheters: results of a randomized trial. Am J Nephrol. (2011) 33:260–8. 10.1159/000324685
23.
Hendrickx L Kuypers D Evenepoel P Maes B Messiaen T Vanrenterghem Y . A comparative prospective study on the use of low concentrate citrate lock versus heparin lock in permanent dialysis catheters. Int J Artif Organs. (2001) 24:208–11. 10.1177/039139880102400407
24.
Joao Luiz MVS Scavone C Tzanno C . The CLOCK trial, a double-blinded randomized controlled trial: trisodium citrate 30% and minocycline 3 mg/mL plus EDTA 30 mg/mL are effective and safe for catheter patency maintenance among CKD 5D patients on hemodialysis. Hemodialy Int. (2017) 21:294–304. 10.1111/hdi.12492
25.
Macrae JM Dojcinovic I Djurdjev O Jung B Shalansky S Levin A et al . Citrate 4% versus heparin and the reduction of thrombosis study (CHARTS). Clin J Am Soc Nephrol. (2008) 3:369–74. 10.2215/CJN.01760407
26.
Maki DG Ash SR Winger RK Lavin P Investigators AT . A novel antimicrobial and antithrombotic lock solution for hemodialysis catheters: a multi-center, controlled, randomized trial. Crit Care Med. (2011) 39:613–20. 10.1097/CCM.0b013e318206b5a2
27.
Moran J Sun S Khababa I Pedan A Doss S Schiller B . A randomized trial comparing gentamicin/citrate and heparin locks for central venous catheters in maintenance hemodialysis patients. Am J Kidney Dis. (2012) 59:102–7. 10.1053/j.ajkd.2011.08.031
28.
Nori US Manoharan A Yee J Besarab A . Comparison of low-dose gentamicin with minocycline as catheter lock solutions in the prevention of catheter-related bacteremia. Am J Kidney Dis. (2006) 48:596–605. 10.1053/j.ajkd.2006.06.012
29.
Pervez A Ahmed M Ram S Torres C Work J Zaman F et al . Antibiotic lock technique for prevention of cuffed tunnel catheter associated bacteremia. J Vasc Access. (2002) 3:108–13. 10.1177/112972980200300305
30.
Power A Duncan N Singh SK Brown W Dalby E Edwards C et al . Sodium citrate versus heparin catheter locks for cuffed central venous catheters: a single-center randomized controlled trial. Am J Kid Dis. (2009) 53:1034–41. 10.1053/j.ajkd.2009.01.259
31.
Quenot J-P Helms J Bourredjem A Dargent A Meziani F Badie J et al . Trisodium citrate 4% versus heparin as a catheter lock for non-tunneled hemodialysis catheters in critically ill patients: a multicenter, randomized clinical trial. Ann Intens Care. (2019) 9:75. 10.1186/s13613-019-0553-4
32.
Solomon LR Cheesbrough JS Ebah L Al-Sayed T Heap M Millband N et al . A randomized double-blind controlled trial of taurolidine-citrate catheter locks for the prevention of bacteremia in patients treated with hemodialysis. Am J Kidney Dis. (2010) 55:1060–8. 10.1053/j.ajkd.2009.11.025
33.
Weijmer MC van den Dorpel MA Van de Ven PJ ter Wee PM van Geelen JA Groeneveld JO et al . Randomized, clinical trial comparison of trisodium citrate 30% and heparin as catheter-locking solution in hemodialysis patients. J Am Soc Nephrol. (2005) 16:2769–77. 10.1681/ASN.2004100870
34.
Lal S Chadwick P Gompelman M Wanten G . Prevention, diagnosis and management of catheter-related blood stream infections. In:NightingaleJMD, editor. Intestinal Failure. Cham: Springer International Publishing. (2023). p. 849–56.
35.
Donlan RM . Biofilm elimination on intravascular catheters: important considerations for the infectious disease practitioner. Clin Infect Dis. (2011) 52:1038–45. 10.1093/cid/cir077
36.
Chung PY Toh YS . Anti-biofilm agents: recent breakthrough against multi-drug resistant Staphylococcus aureus. Pathogens Dis. (2014) 70:231–9. 10.1111/2049-632X.12141
37.
Stucker F Ponte B Tataw J Martin P-Y Wozniak H Pugin J et al . Efficacy and safety of citrate-based anticoagulation compared to heparin in patients with acute kidney injury requiring continuous renal replacement therapy: a randomized controlled trial. Crit Care. (2015) 19:91. 10.1186/s13054-015-0822-z
38.
Bosma JW Siegert CEH Peerbooms PGH Weijmer MC . Reduction of biofilm formation with trisodium citrate in haemodialysis catheters: a randomized controlled trial. Nephrol Dial Transplant. (2009) 25:1213–7. 10.1093/ndt/gfp651
39.
Yevzlin AS Sanchez RJ Hiatt JG Washington MH Wakeen M Hofmann RM et al . Concentrated heparin lock is associated with major bleeding complications after tunneled hemodialysis catheter placement. Semin Dial. (2007) 20:351–4. 10.1111/j.1525-139X.2007.00294.x
40.
Salter Benjamin S Weiner Menachem M Trinh Muoi A Heller J Evans Adam S Adams David H et al . Heparin-induced thrombocytopenia. J Am Coll Cardiol. (2016) 67:2519–32. 10.1016/j.jacc.2016.02.073
41.
Boer W Fivez T Vander Laenen M Bruckers L Grön HJ Schetz M et al . Citrate dose for continuous hemofiltration: effect on calcium and magnesium balance, parathormone and vitamin D status, a randomized controlled trial. BMC Nephrol. (2021) 22:409. 10.1186/s12882-021-02598-2
42.
Zhao Y Li Z Zhang L Yang J Yang Y Tang Y et al . Citrate versus heparin lock for hemodialysis catheters: a systematic review and meta-analysis of randomized controlled trials. Am J Kidney Dis. (2014) 63:479-90. 10.1053/j.ajkd.2013.08.016
43.
Liu J Wang C Zhao H Zhang J Ma J Hou Y et al . Anticoagulant therapies versus heparin for the prevention of hemodialysis catheter-related complications: systematic review and meta-analysis of prospective randomized controlled trials. Int J Clin Exp Med. (2015) 8:11985–95.
Summary
Keywords
heparin, citrate, locking solution, catheter-related bloodstream infection, adverse event
Citation
Lai B, Huang W, Yu H, Chen T, Gao Y, Wang W and Luo H (2025) Citrate as a safe and effective alternative to heparin for catheter locking: a systematic review and meta-analysis of randomized controlled trials. Front. Med. 12:1530619. doi: 10.3389/fmed.2025.1530619
Received
19 November 2024
Accepted
27 January 2025
Published
26 February 2025
Volume
12 - 2025
Edited by
Giuseppe Regolisti, University of Parma, Italy
Reviewed by
Valentina Pistolesi, Sapienza University of Rome, Italy
Evelien Snauwaert, Ghent University Hospital, Belgium
Updates
Copyright
© 2025 Lai, Huang, Yu, Chen, Gao, Wang and Luo.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wei Wang wangw2005@zju.edu.cnHua Luo 18732196660@163.com
†These authors have contributed equally to this work
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.