Abstract
Objective:
This study aimed to evaluate the correlation between the consumption of red meat and processed meat and the incidence of colorectal cancer (CRC) in Asia and provide a scientific basis for reducing the incidence of CRC.
Methods:
PubMed, Embase, Cochrane Library, and other databases were searched electronically to collect studies on the correlation between the consumption of red meat and processed meat and the incidence of CRC in Asia. After the quality evaluation of the Newcastle–Ottawa scale, meta-analyses of the selected studies were performed using RevMan 5.4.1. The odds ratio (OR) and 95% confidence interval (95% CI) were combined, and the heterogeneity among the included studies was analyzed via sensitivity analysis. I2 was used to evaluate the heterogeneity among the included studies.
Results:
Twelve articles were included, which involved 13,292 and 12,544 cases in the case and control groups, respectively. The results of the meta-analysis revealed that in the study of the correlation between the consumption of red meat and the incidence of colon cancer, the combined OR was 2.14 (P < 0.00001); that for the consumption of red meat and the incidence of CRC, the OR was 1.77 (P = 0.006); that for the consumption of red meat and the incidence of rectal cancer, the OR was 2.42 (P = 0.0009); and that for the consumption of processed meat and the incidence of CRC, the combined OR was 1.51 (P > 0.05).
Conclusion:
The results suggest that red meat is a risk factor for the incidence of colon, colorectal, and rectal cancers. However, no significant correlation was found between the consumption of processed meat and the incidence of CRC.
1 Introduction
Consumption of red meat and processed meat has been identified to increase the risk of certain cancers, particularly colorectal cancer (CRC). CRC is a common malignancy of the digestive tract. It ranks third among global malignancies after lung cancer and female breast cancer and has the second-highest mortality rate worldwide (1). The International Agency for Research on Cancer classifies processed meat as a carcinogen and red meat as a probable carcinogen. The early symptoms of CRC are not typical and do not appear until the middle and late stages, when the treatment and prognosis are poor, seriously affecting the quality of life of the patients and imposing a huge financial burden on the patients and their families.
At present, although many local and foreign studies have examined the correlation between the consumption of red meat and processed meat and the incidence of CRC, the dietary habits of Asian population are significantly different from those of Western population. Asian diets tend to be high in vegetables, soy products, and fish, with relatively low consumption of red meat and processed meat. To further explore the correlation between the consumption of red meat and processed meat and the incidence of CRC in Asia, a meta-analysis of relevant literature was conducted to obtain new insights and provide a scientific basis for reducing the incidence of CRC in Asia.
2 Data and methods
2.1 Literature search
2.1.1 Search platform
PubMed, Embase, Cochrane Library, CNKI, Wan Fang database, and VIP Chinese database were searched electronically for relevant studies.
2.1.2 Search strategy
Using the combination of subject terms and free terms, the search strategy was determined according to different databases. In Chinese search, “red meat,” “processed meat,” and “colorectal cancer” were the main topics, and “colon cancer,” “colorectal cancer,” and “colorectal cancer” were the free words. In English retrieval, “processed meat,” “red meat,” and “colorectal neoplasms” were selected as the main words. “Neoplasm, Colorectal,” “Colorectal Tumors,” and “Colorectal Cancer” were the free words. After each keyword was retrieved, the search results of all keywords were combined for retrieval. The search period was up to April 11, 2024.
2.2 Literature inclusion and exclusion criteria
2.2.1 Inclusion criteria
The inclusion criteria were as follows: (1) all cases referred to patients with CRC diagnosed for the first time in medical institutions; (2) case-control studies; (4) participants were residing in Asia; (4) studies published locally or abroad before April 11, 2024; (5) research results can be extracted or converted into odds ratio (OR), 95% confidence interval (95% CI), and standard error, and (6) studies that examined the correlation between the consumption of red meat and processed meat and the incidence of CRC.
2.2.2 Exclusion criteria
The exclusion criteria were as follows: (1) the research types were review, animal experimental studies, review literature, etc.; (2) the full text is not retrievable; (3) complete or duplicated data cannot be provided; and (4) no control group was employed.
2.3 Literature screening, data extraction, and quality evaluation
Studies with obviously inconsistent research contents were excluded by browsing the abstract, studies meeting the inclusion and exclusion criteria were screened by reading the full text, and relevant data were recorded in Excel. Then, two researchers independently evaluated the quality of the studies using the Newcastle–Ottawa scale (NOS), cross-checked it, and negotiated with a third party to resolve any differences. The scale is composed of three parts: selection of exposure and control population, comparability, and evaluation of exposure or outcome, with 8 items. The score ranges from 0 to 9 points.
2.4 Statistical analyses
Meta-analysis was performed using Review Manager 5.4.1. The Cochrane Q test was used to analyze the heterogeneity among all studies, and I2 was used to evaluate the heterogeneity among the included studies. P > 0.1 and I2 < 50% indicated the lack of heterogeneity among the studies, and the fixed-effect model was used to summarize the data. On the contrary, random-effects model was used, and sensitivity analysis or subgroup analysis was performed to analyze the causes of heterogeneity. Funnel plot analysis was used to determine publication bias in the included studies. For studies lacking certain data, data conversion was performed first.
3 Results
3.1 Literature search results
A total of 278 studies were retrieved through preliminary database screening. Duplicate studies, reviews, and systematic reviews were excluded. After browsing the titles and abstracts, 189 studies that were obviously different from the subject were excluded, 89 were included in the preliminary screening, 77 were excluded after thorough reading of the full text, and 12 were finally included in the meta-analysis (Figure 1).
FIGURE 1

Literature screening flow chart.
3.2 Basic characteristics of the included studies
Among the 12 studies included, 11 were case-control studies and 1 was an analytical cross-sectional study. Published from 2010 to 2023, the included studies involved a total of 13,292 cases and 12,544 controls (Table 1).
TABLE 1
| Inclusion studies | Year | District | Research method | Sample size | Sex (male/female) | Outcome index | NOS score | ||
| Case group | control group | Case group | control group | ||||||
| Samarakoon et al. (2) | 2018 | Sri Lanka | Mismatched case-control study | 65 | 260 | 28/37 | 158/102 | ② | 8 |
| Saliba et al. (3) | 2019 | Israel | Prospective case-control study | 5,472 | 4,554 | 2,880/2,588 | 2,389/2,165 | ② ④ | 8 |
| Mahfouz et al. (4) | 2014 | Egypt | Case-control study | 150 | 300 | 72/78 | 144/156 | ② ④ | 8 |
| Ma et al. (5) | 2023 | China | Case-control study | 2,799 | 2,799 | 1,603/1,196 | 1,603/1,196 | ① ② ③ | 9 |
| Alsheridah and Akhtar (6) | 2018 | Kuwait | Matched case-control studies | 103 | 206 | 56/47 | 112/94 | ② | 8 |
| Pramual et al. (7) | 2018 | Thailand | Analytical cross-sectional study | 1,060 | 339/721 | ② ④ | 8 | ||
| Li et al. (8) | 2016 | China | 1:1 case-control study | 400 | 400 | 233/167 | 233/167 | ② ④ | 9 |
| Ghrouz and El Sharif (9) | 2022 | Palestine | Case-control study | 105 | 105 | 57/48 | 58/47 | ② ④ | 8 |
| Abu Mweis et al. (10) | 2015 | Jordan | Case-control study | 167 | 240 | 79/88 | 108/132 | ② | 9 |
| Song et al. (11) | 2019 | Korea | Case-control study | 703 | 1,406 | 480/223 | 960/446 | ② ④ | 9 |
| Promthet et al. (12) | 2010 | Thailand | Case-control study | 130 | 130 | 71/59 | 71/59 | ① | 9 |
| Luo et al. (13) | 2019 | China | Case-control study | 2,138 | 2,144 | 1,219/919 | 1,221/923 | ① ② ③ | 9 |
Basic characteristics of the included studies.
① Red meat is associated with the incidence of colon cancer. ② Correlation between the consumption of red meat and the incidence of colorectal cancer. ③ Correlation between the consumption of red meat and the incidence of rectal cancer. ④ Correlation between the consumption of processed meat and the incidence of colorectal cancer.
3.3 Biased risk assessment of the included studies
The NOS was used to evaluate the quality of the included studies. The NOS scale is suitable for evaluating cohort studies and case-control studies. It has three parts: selection of exposure and control population, comparability, and evaluation of exposure or outcome, with 8 items. The score ranges from 0 to 9 points. The NOS scale was used to evaluate the quality of the 12 studies included, all of which were of high quality (scoring > 7 points).
3.4 Results of the meta-analysis
In this study, a meta-analysis was performed on the correlation between the consumption of red meat and processed meat and the incidence of CRC in Asia, and the corresponding forest map was obtained after the heterogeneity test.
3.4.1 Correlation between the consumption of red meat and the incidence of colon cancer
The results of the meta-analysis on the correlation between the consumption of red meat and colon cancer incidence were as follows: P = 0.06 < 0.1, I2 = 65% > 50%, suggesting the heterogeneity of the results of the study. Therefore, a random-effect model was selected for the meta-analysis, which revealed that red meat was a risk factor for the incidence of colon cancer (P < 0.05). In summary, the risk of colon cancer was 2.14 times that of people who frequently ate red meat in Asia (Figure 2).
FIGURE 2

Forest map of correlation analysis between red meat consumption and colon cancer incidence.
3.4.2 Correlation between the consumption of red meat and the incidence of colorectal cancer
The results of the meta-analysis on the correlation between the consumption of red meat and the incidence of CRC were as follows: P < 0.00001, I2 = 93% 2 > 50%, suggesting heterogeneity in the results of the study. Therefore, a random-effects model was selected, which revealed that red meat was a risk factor for the incidence of CRC (P < 0.05). In summary, the risk of CRC was 1.77 times that of people who frequently ate red meat in Asia (Figure 3).
FIGURE 3

Forest map of correlation analysis between red meat consumption and colorectal cancer incidence.
3.4.3 Correlation between processed meat and incidence of colorectal cancer
The results of the meta-analysis on the correlation between the consumption of processed meat and the incidence of CRC were as follows: P < 0.1, I2 = 87% > 50%, suggesting heterogeneity in the results of the study. Therefore, a random-effects model was selected for meta-analysis, which did not find a significant correlation between the consumption of processed meat and the incidence of CRC in Asia (P > 0.05) (Figure 4).
FIGURE 4

Forest map of correlation analysis between processed meat consumption and colorectal cancer incidence.
3.4.4 Correlation between the consumption of red meat and the incidence of rectal cancer
The results of the meta-analysis on the correlation between the consumption of red meat and the incidence of rectal cancer were as follows: P = 0.01 < 0.1, I2 = 85% > 50%, suggesting heterogeneity in the results of the study. Therefore, a random-effects model was selected for meta-analysis, which revealed that red meat was a risk factor for the incidence of rectal cancer (P < 0.05). In summary, the risk of CRC was 2.42 times higher in people who frequently ate red meat in Asia than in those who did not eat red meat (Figure 5).
FIGURE 5
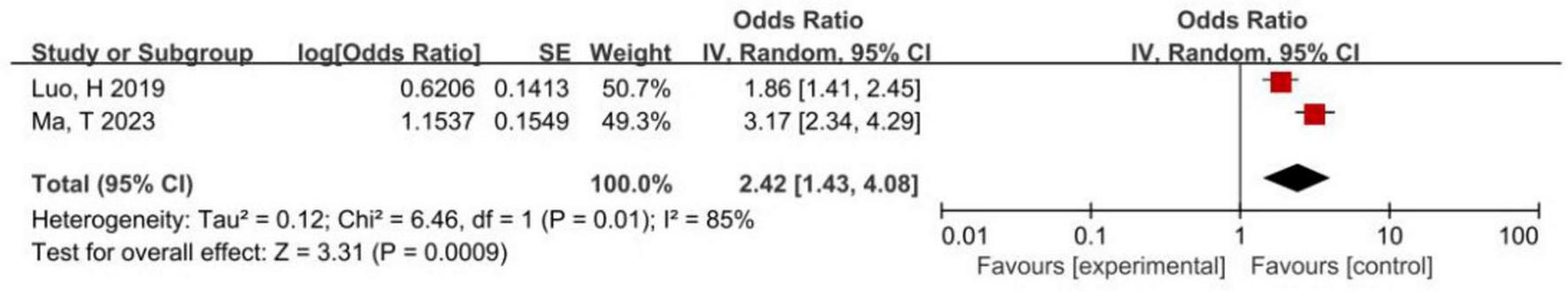
Forest map of correlation analysis between red meat consumption and rectal cancer incidence.
3.5 Publication bias
A publication bias analysis was conducted on the studies examining the correlation between the consumption of red meat and the incidence of CRC. The funnel plots were symmetric, suggesting no significant publication bias (Figure 6).
FIGURE 6
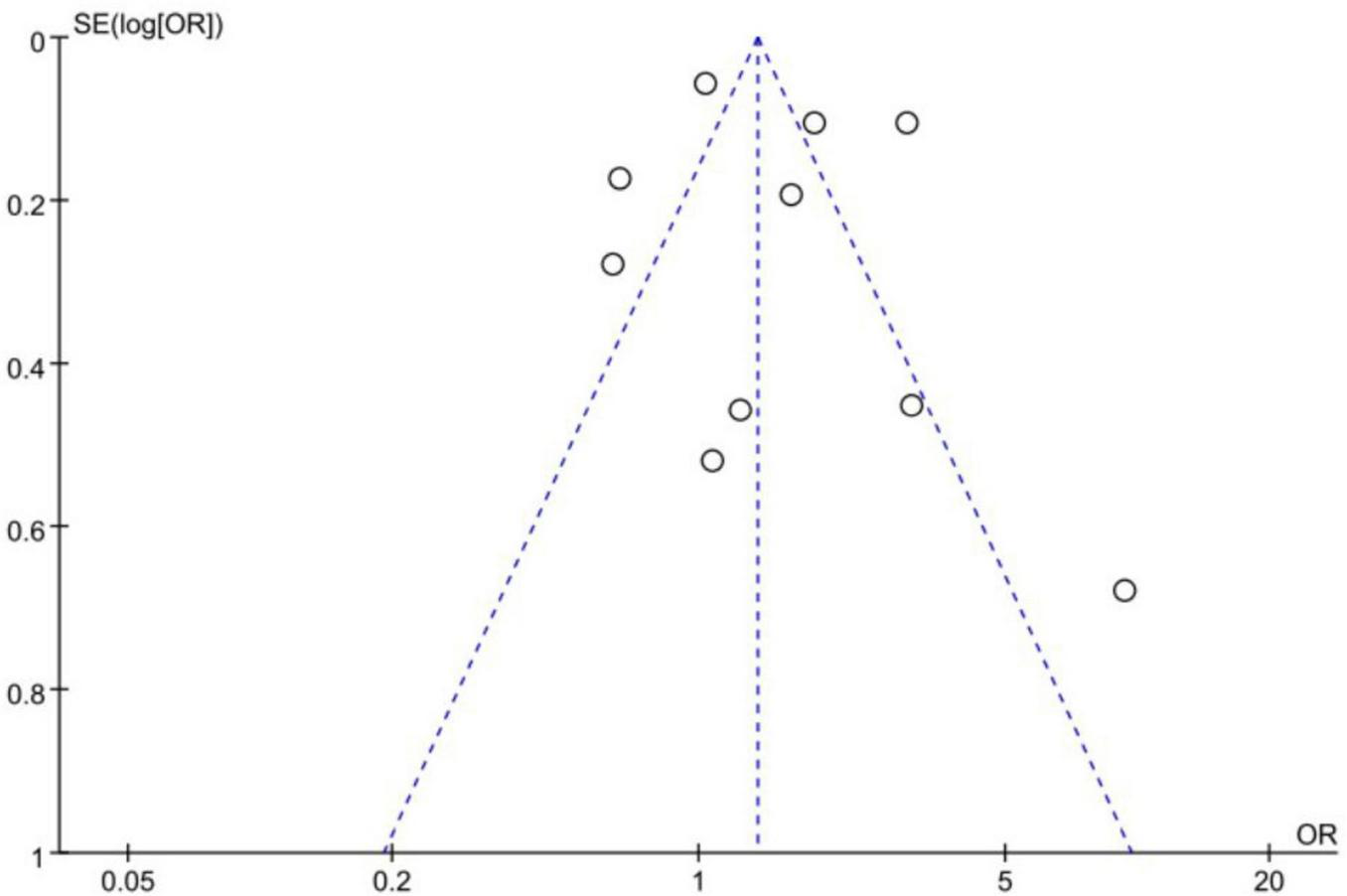
Funnel plot of correlation analysis between red meat consumption and colorectal cancer incidence.
3.6 Sensitivity analysis
For the correlation analysis between the consumption of red meat and the incidence of colon cancer, CRC, and rectal cancer, the fixed-effects and random-effects models were used to estimate the combined OR and 95% CI. The combined results of the two models were similar, and the combined results were statistically significant, indicating that the combined results were reliable (Table 2).
TABLE 2
| Analysis index | Fixed effect model | Random effects model | ||
| OR | 95% CI | OR | 95% CI | |
| Association between red meat consumption and colon cancer incidence | 2.22 | 1.89–2.60 | 2.14 | 1.56–2.93 |
| Correlation between red meat consumption and colorectal cancer incidence | 1.36 | 1.25–1.47 | 1.77 | 1.18–2.26 |
| Association between red meat consumption and rectal cancer incidence | 2.37 | 1.93–2.91 | 2.42 | 1.43–0.48 |
Sensitivity analysis of the association between the consumption of red meat and the incidence of colon cancer, colorectal cancer, and rectal cancer in the included studies.
The sensitivity analyses of the correlation between the consumption of red meat and the incidence of CRC and between the consumption of processed meat and the incidence of CRC were performed using the one-by-one elimination method. Studies on the correlation between the consumption of red meat and the incidence of CRC were eliminated one by one, and if the combined results of the remaining studies did not change direction, the study results were robust. Moreover, studies on the correlation between the consumption of processed meat and the incidence of CRC were excluded one after another; consequently, the combined results of the remaining studies were not statistically significant and the direction did not change, indicating that the results were robust, and no significant correlation was noted between the consumption of processed meat and the incidence of CRC (Table 3).
TABLE 3
| OR (95% CI) | P | I 2 (%) | |
| Correlation between red meat consumption and colorectal cancer incidence | 1.77 (1.18–2.26) | 0.006 | 93 |
| Excluding Abu Mweis et al. (10) | 1.98 (1.29–3.04) | 0.002 | 93 |
| Excluding Alsheridah and Akhtar (6) | 1.61 (1.07–2.42) | 0.02 | 93 |
| Excluding Ghrouz and El Sharif (9) | 1.84 (1.21–2.82) | 0.005 | 94 |
| Excluding Li et al. (8) | 1.81 (1.16–2.84) | 0.009 | 94 |
| Excluding Luo et al. (13) | 1.83 (1.13–2.96) | 0.01 | 93 |
| Excluding Ma et al. (5) | 1.58 (1.08–2.32) | 0.02 | 89 |
| Excluding Mahfouz et al. (4) | 1.50 (1.02–2.21) | 0.04 | 93 |
| Excluding Pramual et al. (7) | 1.83 (1.19–2.81) | 0.006 | 94 |
| Excluding Saliba et al. (3) | 1.96 (1.22–3.14) | 0.006 | 91 |
| Excluding Samarakoon et al. (2) | 1.69 (1.11–2.59) | 0.01 | 94 |
| Excluding et al. (11) | 2.01 (1.31–3.08) | 0.001 | 93 |
| Correlation between processed meat consumption and colorectal cancer incidence | 1.51 (0.78–2.94) | 0.23 | 87 |
| Excluding Ghrouz and El Sharif (9) | 1.71 (0.80–3.65) | 0.17 | 89 |
| Excluding Li et al. (8) | 1.22 (0.74–2.01) | 0.44 | 65 |
| Excluding Mahfouz et al. (4) | 1.27 (0.52–3.06) | 0.60 | 87 |
| Excluding Pramual et al. (7) | 1.73 (0.86–3.47) | 0.12 | 89 |
| Excluding Saliba et al. (3) | 1.54 (0.64–3.47) | 0.33 | 80 |
| Excluding Song et al. (11) | 1.62 (0.79–3.33) | 0.19 | 89 |
Correlation between red meat consumption and colorectal cancer incidence and between processed meat consumption and colorectal cancer incidence.
4 Discussion
CRC is a common malignant tumor of glandular epithelial origin, and its incidence increases with age. Many local and foreign studies and reports have examined the risk factors of CRC; however, their results are quite different. Among the 11 articles selected in the meta-analysis of the correlation between the consumption of red meat and the incidence of colon cancer, the combined OR was 2.14 (P < 0.00001). In the analysis of the correlation between the consumption of red meat and the incidence of CRC, the OR was 1.77 (P = 0.006). In the study of the correlation between the consumption of red meat and the incidence of rectal cancer, the OR was 2.42 (P = 0.0009). In the analysis of the correlation between the consumption of processed meat and the incidence of CRC, the combined OR was 1.51 (P > 0.05). This suggests that red meat is a risk factor for the incidence of colon, colorectal, and rectal cancers. However, no significant correlation was found between the consumption of processed meat and the incidence of CRC.
This review also revealed that processed meat may be associated with the incidence of colon and rectal cancers in Asia; however, a meta-analysis was not possible because of insufficient literature. Wada et al. (14) showed a positive correlation between the consumption of processed meat and colon cancer risk in men. Oba et al. (15) showed that high consumption of processed meat increased the risk of colon cancer in men.
This meta-analysis had certain limitations. The number of selected articles was small. Only Chinese and English studies with Asian populations as the study participants were selected, and data analysis of large numbers and articles in other languages cannot be performed. For the research results of the meta-analysis of influencing factors, some errors were possible because of the small number of existing studies, which need to be further analyzed. Second, some studies were not included because of the incompleteness of data, which may cause publication bias and affect the combined results. Thirdly, this study mainly relies on case-control studies, lacking cohort studies or RCTs, and fails to account for all potential confounding variables such as genetics, lifestyle, dietary patterns, and other factors, which may reduce the reliability of the research findings. Owing to the limitations of this study, more high-quality controlled studies, cohort studies, and randomized controlled trials (RCTs) are needed to further evaluate the association of red meat and processed meat with the incidence of CRC in Asia.
Statements
Data availability statement
The original contributions presented in this study are included in this article/supplementary material, further inquiries can be directed to the corresponding author/s.
Author contributions
ZL: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. WW: Conceptualization, Funding acquisition, Investigation, Resources, Writing – review & editing. SX: Investigation, Supervision, Writing – review & editing. LY: Investigation, Writing – review & editing. ZX: Investigation, Writing – review & editing. YL: Investigation, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was funded by the Clinical Key Specialty Construction fund of Futian District, Shenzhen. The funder was not involved in the design of the study, the collection, analysis and interpretation of the data, the writing of the report, and the decision to publish the manuscript.
Acknowledgments
We thank all patients and clinical investigators who were involved in the studies included in this meta-analysis.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
CI, confidence interval; CRC, colorectal cancer; OR, odds ratio.
References
1.
Bray F Ferlay J Soerjomataram I Siegel R Torre L Jemal A . Global cancer statistics 2018: Globocan estimates of incidence and mortality worldwide for 36 cancers in 185 countries.CA Cancer J Clin. (2018) 68:394–424. 10.3322/caac.21492
2.
Samarakoon Y Gunawardena N Pathirana A . Behavioral, familial and comorbid illness risk factors of colorectal cancer: A case control study.Ceylon Med J. (2018) 63:113–8. 10.4038/cmj.v63i3.8725
3.
Saliba W Rennert H Gronich N Gruber S Rennert G . Red meat and processed meat intake and risk of colorectal cancer: A population-based case-control study.Eur J Cancer Prev. (2019) 28:287–93. 10.1097/CEJ.0000000000000451
4.
Mahfouz E Sadek R Abdel-Latief W Mosallem F Hassan E . The role of dietary and lifestyle factors in the development of colorectal cancer: Case control study in Minia, Egypt.Cent Eur J Public Health. (2014) 22:215–22. 10.21101/cejph.a3919
5.
Ma T Tu K Ou Q Fang Y Zhang C . Comparing the associations of dietary patterns identified through principal component analysis and cluster analysis with colorectal cancer risk: A large case-control study in China.Nutrients. (2023) 16:147. 10.3390/nu16010147
6.
Alsheridah N Akhtar S . Diet, obesity and colorectal carcinoma risk: Results from a national cancer registry-based middle-eastern study.BMC Cancer. (2018) 18:1227. 10.1186/s12885-018-5132-9
7.
Pramual P Sarakarn P Kamsa-ard S Jirapornkul C Maneenin N Thavondunstid P et al Lack of association between red meat consumption and a positive fecal immunochemical colorectal cancer screening test in Khon Kaen, Thailand: A population- based randomized controlled trial. Asian Pac J Cancer Prev. (2018) 19:271–8. 10.22034/APJCP.2018.19.1.271
8.
Li Y Feng F Yan J Chen L Li X Liu W et al [Association between cured meat consumption and risk of colorectal cancer in people with different dietary habits and lifestyles]. Z Liu Xing Bing Xue Za Zhi. (2016) 37:1006–11. 10.3760/cma.j.issn.0254-6450.2016.07.020
9.
Ghrouz I El Sharif N . Diet and genetic risk factors of colorectal cancer in palestine: A case-control study.Nutr Cancer. (2022) 74:2460–9. 10.1080/01635581.2021.2013507
10.
Abu Mweis S Tayyem R Shehadah I Bawadi H Agraib L Bani-Hani K et al Food groups and the risk of colorectal cancer: Results from a Jordanian case-control study. Eur J Cancer Prev. (2015) 24:313–20. 10.1097/CEJ.0000000000000089
11.
Song N Lee J Cho S Kim J Oh J Shin A . Evaluation of gene-environment interactions for colorectal cancer susceptibility loci using case-only and case-control designs.BMC Cancer. (2019) 19:1231. 10.1186/s12885-019-6456-9
12.
Promthet S Pientong C Ekalaksananan T Wiangnon S Poomphakwaen K Songserm N et al Risk factors for colon cancer in Northeastern Thailand: Interaction of MTHFR codon 677 and 1298 genotypes with environmental factors. J Epidemiol. (2010) 20:329–38. 10.2188/jea.je20090140
13.
Luo H Zhang N Huang J Zhang X Feng X Pan Z et al Different forms and sources of iron in relation to colorectal cancer risk: A case-control study in China. Br J Nutr. (2019) 121:735–47. 10.1017/S0007114519000023
14.
Wada K Oba S Tsuji M Tamura T Konishi K Goto Y et al Meat consumption and colorectal cancer risk in Japan: The Takayama study. Cancer Sci. (2017) 108:1065–70. 10.1111/cas.13217
15.
Oba S Shimizu N Nagata C Shimizu H Kametani M Takeyama N et al The relationship between the consumption of meat, fat, and coffee and the risk of colon cancer: A prospective study in Japan. Cancer Lett. (2006) 244:260–7. 10.1016/j.canlet.2005.12.037
Summary
Keywords
colorectal cancer, colon cancer, rectal cancer, red meat, processed meat, meta-analysis
Citation
Liao Z, Wu W, Xia S, Yu L, Xu Z and Li Y (2025) Associations between the consumption of red meat and processed meat and the incidence of colorectal cancer in Asia: a meta-analysis. Front. Med. 12:1555717. doi: 10.3389/fmed.2025.1555717
Received
05 January 2025
Accepted
24 April 2025
Published
09 June 2025
Volume
12 - 2025
Edited by
José María Huerta, Carlos III Health Institute (ISCIII), Spain
Reviewed by
Shabnam Malik, The University of Texas Rio Grande Valley, United States
Nan Zhang, St. Jude Children’s Research Hospital, United States
Updates
Copyright
© 2025 Liao, Wu, Xia, Yu, Xu and Li.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shijun Xia, strasha@163.com
†These authors have contributed equally to this work and share first authorship
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.