- Faculty of Medicine and Health, School of Rural Health (Orange/Dubbo), University of Sydney, Dubbo, NSW, Australia
Introduction: Workplace-based research training contributes to research capability and capacity in rural areas where access to university expertise is limited. Rural health complexities and the diverse approaches previously used to build research capacity have led to a lack of clarity about how to build research capacity within rural health services.
Methods: Using a critical realist foundation, we explored distributed workplace-based rural research training and synthesized five studies centered in rural New South Wales, Australia. Critical realism allowed the exploration of the structural supports and barriers for workplace-based research training activities and the ability of individuals to pursue research activities within rural health workplaces.
Results: The component studies showed that distributed rural research training programs improve individual research capability by developing research skill, increasing research experience and facilitating research networks across sectors. Rural research activities are characterized by individual agency and partnering or relationships to access support and expertise. Structural barriers including a lack of operational planning for research and few ongoing research opportunities limit translation of capability into research capacity.
Discussion: Individual workplace-based research training is effective, but not sufficient to build and maintain research capacity. Structural supports such as organizational commitment and careful training design can maximize cooperative partnerships with education partners. Addressing both structural and individual factors is needed to build rural health research capacity and generate real-world health research to drive meaningful improvements in rural health.
1 Introduction
People living in rural and remote locations experience significant health disadvantage when compared to their urban counterparts (1, 2). These disadvantages are linked to disparities in healthcare access (3, 4), fewer specialist doctors and allied health professionals, and specialist services clustered in cities (5). Other health service access challenges include large geographical distance between centers, low population densities (1) and disparities caused by social determinants of health (6, 7).
These challenges highlight the unique circumstances associated with rural and remote healthcare delivery. In Australian healthcare delivery, urban models of care are often applied to rural or remote areas, a “one size fits all” approach that may not translate into rural and remote areas (8, 9). The development of tailored rural solutions and bespoke models of care are required to better meet health needs of these unique populations with a goal of equal opportunity for good health “regardless of location” (10).
Addressing these particular circumstances and needs of rural and remote healthcare delivery in Australia indicates a need for rural-specific research (11, 12) including developing and implementing rural models of care (13) and translating relevant urban research into rural environments (14). Better rural healthcare relies upon a better understanding of the rural healthcare environment and rural health delivery.
One difficulty in understanding rural health issues is the limited number of rurally-based researchers (11, 15). Historically most researchers have been urban-based and if they conducted research in rural areas, this has not led to increased research activity driven by those rural communities (12). Research conducted with, within and by rural health services and rural clinicians has advantages in identifying the critical issues relevant to the rural or remote context and understanding of rural people’s mindset and characteristics (11, 16, 17). The unique circumstances surrounding rural healthcare delivery have led for a call for specific rural training for researchers in Australia (12).
Research training and capacity building within health services has taken many forms over the past two decades, including grant programs (18, 19), partnerships (20, 21), embedded researcher models (22–26) and training programs (27–31). The success of these initiatives is measured using different metrics, including self-rated research experience (28, 32, 33), completion rates (34), research activity (18, 35) and the ability to secure grant funding (21, 36). Other reported metrics include publications or presentations (37, 38), workforce development (29, 39), influence on policy and practice (18, 20) or research confidence (40). Provision of a formal qualification or articulation with research higher degrees was an important feature of some programs (26), but many programs led to no formal qualification. In Australia a range of health disciplines have been targeted for research capacity building, including Aboriginal health workers (39, 41, 42), allied health staff (22, 23, 43–47), medical staff (35, 48) and primary health care workers (20, 33, 49, 50).
The range of learner groups, approaches, contexts and metrics add complexity to understanding the relative merits of each approach. This highlights the need for studies such as this synthesis, where critical realism is used to create clarity from this complexity.
The setting for this synthesis is the public health system New South Wales (NSW), Australia. The NSW public health system is structured with a centralized governance and policy body overseeing 15 Local Health Districts (LHDs) and multiple specialty networks responsible for delivering clinical services (51). Nine of these LHDs cover rural and remote areas (51).
Within these rural LHDs, there has been an effort to build research capacity through the Rural Research Capacity Building Program (RRCBP), a distributed, workplace-based research training program (27–29, 34). This program was created in recognition of limited research expertise in rural health services and within rural health workers (29). The stated aims of the program are to build research knowledge and skill while contributing to the rural research evidence base (34). This aligns closely to the clinician-researcher model, producing rural clinicians with research capability and experience, whilst building research capacity.
The synthesis explores the constraints inherent in the rural health system and what rural research capacity building can achieve within this context. Five papers examining research capacity building within NSW and within the public health system (33, 52–55) were included in this synthesis. Collectively, the studies and a critical realism perspective allow development and testing of generative mechanisms that explain “why things are as they are” in research capacity building in rural health services, with the rural NSW experience as an exemplar. These underlying explanations may have applicability and relatability to other rural contexts outside NSW and outside Australia.
The aims of this synthesis were:
1. To describe and understand the contexts in which rural health research training occurs and the outcomes of research capacity building endeavors in the rural health workplace.
2. To use these outcomes in context to theorize what mechanisms exist in the education of research for the rural workforce which have led to the kinds of outcomes we see.
3. To develop key principles to guide the development of rural research capacity building programs.
2 Materials and methods
This paper brings together five papers centered on rural research capacity building (Table 1) in the form of a realist synthesis. Unlike a traditional systematic review which takes a broad view of the available literature, this realist synthesis uses purposively selected studies to form a unique data set that can be explored using realist principles to extract a new understanding. This approach is underpinned by the concept that the papers present theories about what works for who in what circumstance and that by synthesizing together these theories the underlying causative mechanisms can be unveiled in what is otherwise a complex area (56).
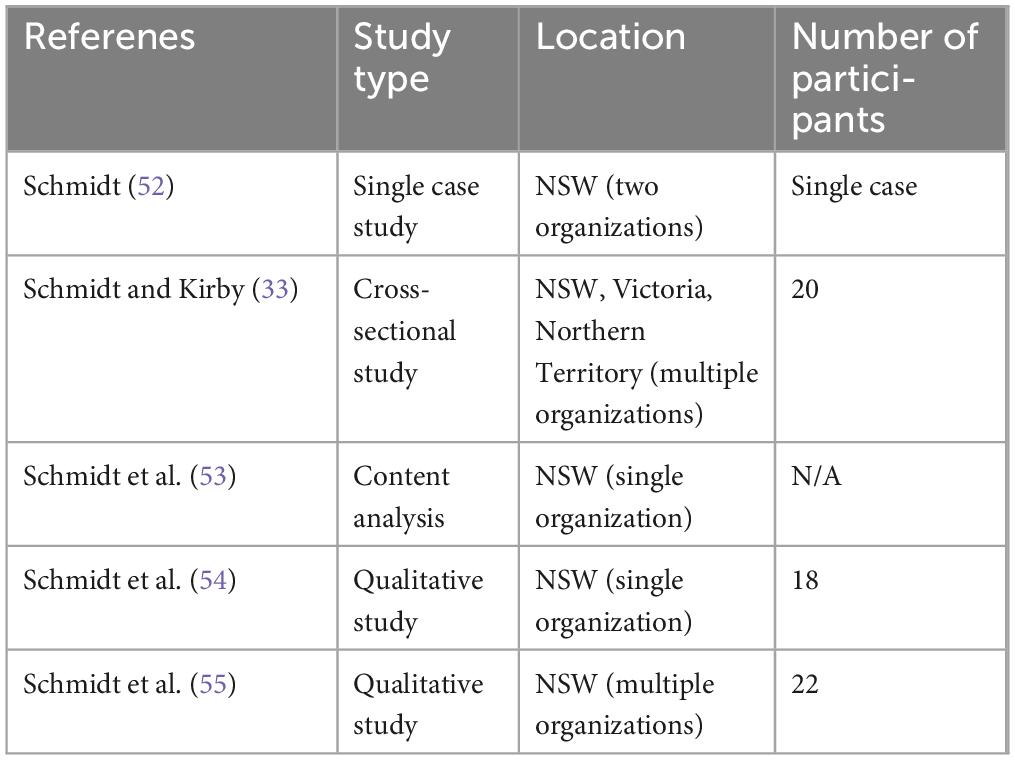
Table 1. Papers included in synthesis (103).
For this synthesis, the included papers report on the context of research training and the outcomes of the RRCBP and another similar program conducted in a more remote part of NSW and other states. These studies were selected for a number of reasons. Firstly, the RRCBP provides the longest-running example of rural research capacity building in Australia (29, 55) and as such provides opportunity for learnings that cannot be gleaned from shorter-term programs. Secondly, understanding the context in which these programs is an important part of realist synthesis (56) and the authors’ positions as “informed insiders” within these programs allows a nuanced perspective that an outsider may not achieve. Including papers that explore similar programs to the RRCBP or similar contexts to which the RRCBP is conducted provides a diversity of sources, paralleling the fact that rural communities are not homogenous (2). Bringing these studies together creates a necessary richness to the data.
The process of realist synthesis involves synthesizing the findings from the individual studies into new generative mechanisms and was led by the first author (DS). The process commenced with extracting elements known as Context, Mechanism and Outcome statements (CMO) of each of the included studies. These statements (also known as CMO chains) were broken down into their individual elements such as observations on the Context of the rural research capacity building endeavor or the proposed Mechanism that explains observed Outcomes within the study. The elements were considered separately, that is all Context statements were combined to create a collective understanding of Context, and so forth for Mechanisms and Outcomes. These collected components were then reviewed in light of existing literature, particularly through the structural levels of capacity building; individual, team, organizational and supra-organizational (57, 58). These elements were then combined via an iterative and intuitive process of retroduction and hypothesis building to form new CMO chains, using the “creative imagination” described by Bhaskar (59). Critical realism tenets of stratified reality, agency and structure were applied, along with external literature, as mechanisms were hypothesized, discussed between the authors and then explored for logic and coherence, leading to proposed mechanisms being refined, adopted or abandoned. These mechanisms were tested in two ways. Two external experienced health research educators checked the proposed mechanisms for coherence (60) and the consistency of proposed mechanisms with their knowledge and experience of rural research capacity building. Feedback was used to refine the mechanisms and the way they were expressed in CMO chains. Mechanisms were then compared to those highlighted by Cooke et al. (61), in their realist synthesis, a work that applies realist principles to the area of research capacity building but importantly does not consider the rural context. Bracketing and reflexive conversations with the second and third authors (EW and DL) added further rigor to the process (62–64).
Central to this process was the knowledge inherent in being an embedded insider with a deep understanding of the rural health context, the NSW public health system and the process of research capacity building. This insider perspective provided a credible foundation from which creative imagination could be employed. This process was repeated multiple times until a suite of proposed mechanisms were compiled. These CMO chains were then tested and consolidated into practical understandings of what works where and for whom, which could then be transferred into practical recommendations for health system, health service and education purposes.
3 Results
Context and outcomes for rural research training within rural NSW were explored at the individual, team and organizational structural levels at which research capacity building occurs (57, 58). While the supra-organizational context is acknowledged, none of the included papers focused on this structural level and it was therefore not a focus in this analysis.
3.1 Individual contexts and outcomes
Rural clinicians, with the challenges of rural health service delivery, see not only problems but also opportunities for research investigation (52). Rural individuals experience limited operational planning for research, which can act as an inhibitory structure for research (53). Rural clinicians want rural research to be immediately useful (55).
The individual rural clinician context and the way the individual interacts with that context is constantly evolving. Developing research experience and capability contributes to increased confidence in rural individuals (55), which can translate to changes in their individual agency, or ability to take action within their context. Distributed research training in the workplace can keep experienced health professionals in their roles whilst building research experience (55). It should be noted that not everyone who learns about research wants to continue to apply research skills in their work role (55).
Obtaining organizational support for research training and ongoing research activity where individuals can use their new skills is challenging (55). Without organizational support, a disconnect between workplace and individual can arise where research is seen as an individual pursuit unrelated to organizational goals (54).
The context for individual learning includes a low base of research activity and limited research expertise in rural areas (53). Research training generally needs to be introductory in nature, matched to the learner’s needs (65), and supported by expertise from experienced researchers where available (54). Many clinicians in rural NSW have existing research-relevant skills, so training may build on existing project management or quality improvement skills (52) and may require a multilevel training strategy (58).
Training programs have shown increased individual research experience (28, 33) and a range of research-specific and transferable skills such as project management experience, enhanced critical thinking, improved communication and improved confidence (55).
Close-to-practice research, such as that completed in experiential rural research programs (33, 55), is a key enabler of capacity building (29, 57, 58). This research activity, along with changes in individual research capability, skill and experience amount to real-world research capacity building (66) and continue to demonstrate that individual training can have capacity building outcomes (29).
3.2 Team contexts and outcomes
The papers synthesized focused on the organizational (53, 54) or individual level (33, 52, 55) and provide fewer insights into the team context. A supportive work team is an important facilitator of research (67), and the attitudes of work colleagues can be a powerful structure that influences rural clinicians undertaking workplace-based research. Research-emergent and novice clinician-researchers can make their own research networks to provide team level support that their workplace team may not (55).
Building a more capable, confident and skilled worker as a result of research experience and research training has team benefits including improved evaluation rigor, raised profile of research within a team, creating research activity and retaining a skilled workforce (55). Building team research capacity may be cumulative, with the collective individual capability outcomes contributing to team level capacity.
3.3 The organizational level
Research conducted within rural health organizations in NSW is often not conducted for or by these organizations (53), perpetuating the perception that research is not something that rural health organizations can do: a “too rural and too poor” view (54). The perception of limited capacity is both an outcome of the limited health research expertise within rural health organizations (12) and the difficulty accessing research funding (68), and is also a mechanism of limited research activity. This co-occurring role of both cause and outcome reflect a stratified reality: organizations that see themselves as incapable of undertaking their own research may engage with outside organizations in a passive way, thus limiting opportunities for research capacity building within the organization.
External partnerships are a potential solution to limited access to research expertise in rural areas (12, 54). These collaborative approaches across sectors, either formally or informally, can help provide access to research knowledge and support that is vital for research capacity development.
The organizational context for those wanting to learn about research includes the ability to access practical support, such as operational planning or positional responsibility for research (53), valuing and promoting research endeavors (54) and organizational commitment (55). Practical support may include creative solutions such as incorporating research activity into routine work to offset a lack of funding (52).
The value placed on research in rural health organizations may vary between strategic and operational levels (53) and a mismatch between organizational language and actions concerning the value of research activities (55) can create an inhibitory influence on rural health staff. A perception that research is a low-value individual activity inhibits the uptake of research opportunities and learning in research (54). Demonstrating that research is valued is a key facet of research capacity building (57, 58, 61).
An organizational perception that research is an individual, rather than an organizational, activity can lead to research activity being driven largely by the agency of individuals (53, 54). This reliance on individual agency is associated with a limited number of nursing and allied health research projects (53).
Maintaining research activity outside of the supportive structure of training programs also relies upon the individual agency of the worker (55), although there is a limit to how much individual agency can overcome structural limitations. A mismatch between research capability and research capacity can lead to discontent (55).
Organizational outcomes resulting from research training include increased local research activity, dissemination of research findings, demonstrable leadership and the establishment of partnerships (29, 33, 49, 54, 55).
Research training can be viewed as an organizational investment rather than a cost burden (52), if the organization acknowledges that retaining experienced staff whilst improving policy and practice (55) is a real return on that investment. Research-trained clinicians demonstrate capability as an outcome of a capacity building endeavor, whilst being an enabling mechanism of research activity by assuming the roles of researcher, resource person or mentor.
3.4 Synthesis and new generative mechanisms
This new understanding of outcomes in context reveals generative mechanisms that underlie research capacity building for the rural health workforce. A suite of proposed mechanisms were derived and are expressed as CMO chains in Table 2.
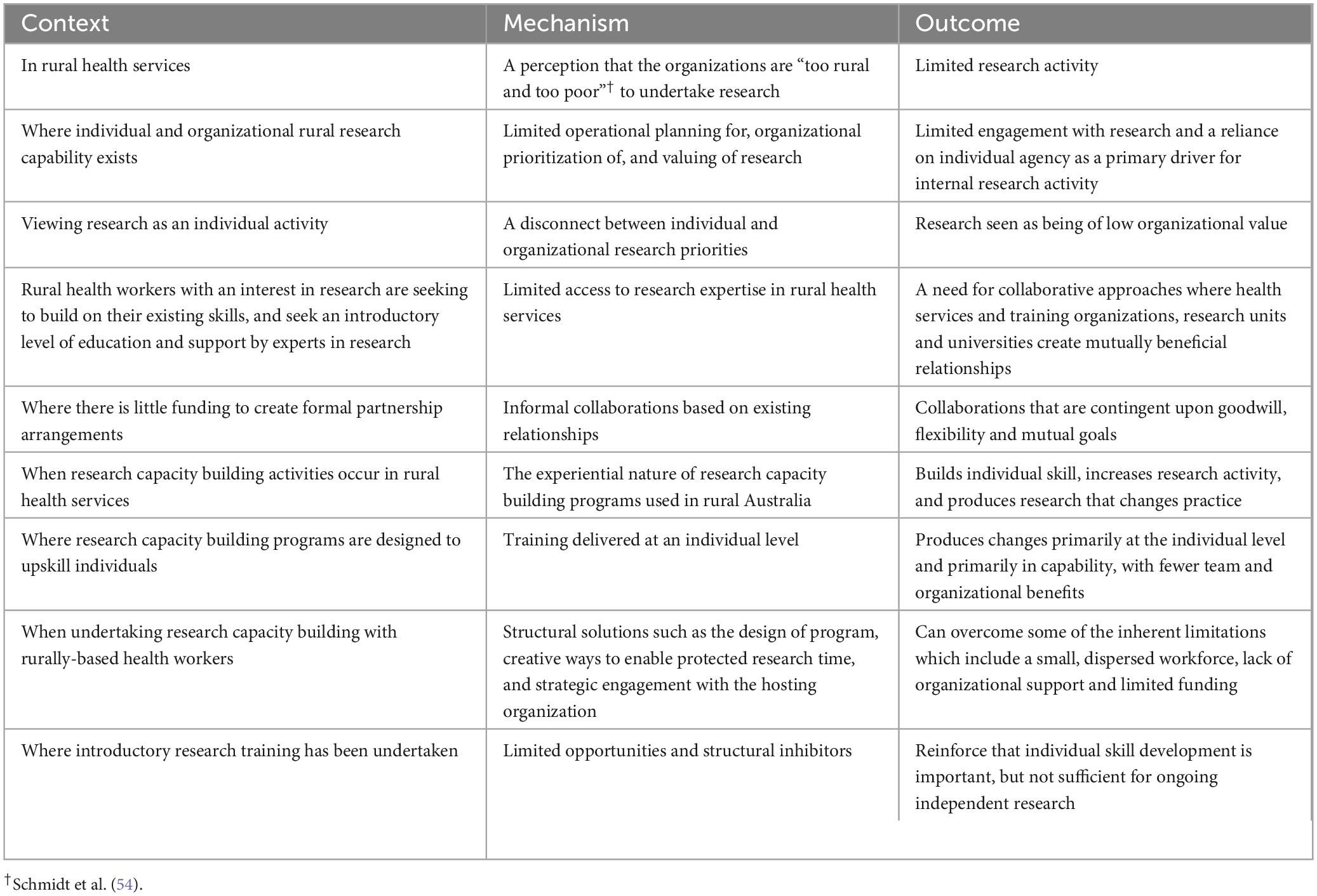
Table 2. Generative mechanisms of research capacity building in rural health workplaces expressed as context, mechanism outcome (CMO) chains (103).
Perceptions and beliefs can exert influence (69), and in a critical realist sense are therefore real. In rural health services a real underlying perception that the organizations are “too rural and too poor” to undertake research can lead to empirical limited research activity (54). Beliefs can, at an organizational level, stifle new approaches (70) and exert a real influence on rural health research. Beliefs and knowledge can intersect as explanations of the social world (71), and while there is evidence rural organizations are empirically disadvantaged in research grant funding (68), it is the real perception that rural health organizations are inherently incapable of undertaking research that is a key driver of low levels of research activity.
While research capability is an important part of research capacity within rural health services, limited operational planning for research, low organizational prioritization of research, and a perceived low organizational valuing of research directly are factors that impact on engagement with research. In rural NSW, Australia, a clear gap in organizational planning for research (53) has led to a reliance on individuals, and individual agency, to drive research activity. This resulted in research being seen as an individual activity disconnected from organizational research priorities and thus of low organizational value. The alignment between individual and organizational priorities for research is critical, given that a lack of organizational support leads to limited research activity (55) and is a cause of withdrawal from research training programs (34).
Limited research expertise in rural health organizations (54) is a mechanism leading to a need for collaborative approaches to provide both introductory research education and expert support for research. Collaborative approaches are essential for providing access to expertise, particularly when the rural context is considered (17, 23, 31).
Rural partnership arrangements are often relationship-based (33) and are contingent upon goodwill, flexibility and mutual goals. Mutual goal-setting is an important part of collaborative approaches to research partnerships (72) and in rural areas these relationships can be effective where the goals of the workplace and the learning institution align (54).
When training in research occurs in rural areas the experiential nature of training programs used in rural NSW builds individual skill, increases research activity, and produces research that changes practice (33, 55). Experiential learning aligns closely with adult learning principles (73, 74).
Training programs delivered at an individual level lead primarily to individual outcomes, with fewer team and organizational benefits. It must be noted that the tools used to empirically assess outcomes, such as the research spider (75) which is commonly used in assessing research experience (28, 76), are aimed at the individual level so could fail to identify co-occurring team and organizational outcomes. Team research capability and culture are less well developed in rural areas than individual or organizational capability (77) and thus an avenue for future research capacity building in rural areas should focus on team approaches as have been trialed elsewhere (19, 78–81).
Some of the inherent limitations of rural research education, such as a small, dispersed workforce, lack of organizational support and limited funding, can be accommodated by structural solutions such as the design of distributed training programs (33), creative ways to enable protected research time (17, 52) and strategic engagement with the hosting organization (17, 33).
While receiving training in research equips health workers for ongoing research activity (28, 29, 55) limited opportunities to use these skills and structural inhibitors such as a lack of time and resources reinforce that individual skill development is important, but not sufficient for ongoing independent research. This demonstrates the difference between research capability and research capacity; trained clinician-researchers could undertake independent research, but this does not mean that they can undertake independent research.
3.5 Testing research capacity building theory
The proposed mechanisms, after testing for coherence (60), were compared to the mechanisms of research capacity development proposed by Cooke et al. (61) in their realist synthesis (see Table 3). The mechanisms described by Cooke et al. represent a “best evidence available” model, one that is unencumbered by the constraints of the rural environment. This allows a comparison of “what is” in the rural environment of NSW, to “what could be” in Cooke et al.’s model. Demonstrating concordance between the two models confirms that these proposed mechanisms derived in this synthesis display coherence, whilst allowing an exploration of the rural and non-rural differences of the two models.

Table 3. Emerging mechanisms from this synthesis contrasted with mechanisms of research capacity development proposed by Cooke et al. (61, 103).
Notably, the mechanisms proposed in this synthesis contrast with those of Cooke et al. (61) in role modeling, signaling importance (where individuals see that engaging in research is a valued part of the organization’s business) and exceeding the sum of the parts. In the rural context, a shortage of rural researchers and organizational commitment lead to limited role modeling and limited visibility of research (53, 54). This contrast highlights that rural and metropolitan approaches to research capacity building differ due to important structural influences, such as geographical spread of the workforce, availability of research experts and ability to access to research funding. While the increasing the number of rural researchers is a long-term solution, rural health organizations can influence other elements such as increasing the visibility of research and signaling its importance within rural health organizations.
The final aim of this synthesis was to use these mechanisms to develop general principles to guide the development of rural research capacity building programs. These are found in Table 4. These principles extend the mechanisms into useful actions that can be applied in rural health contexts.
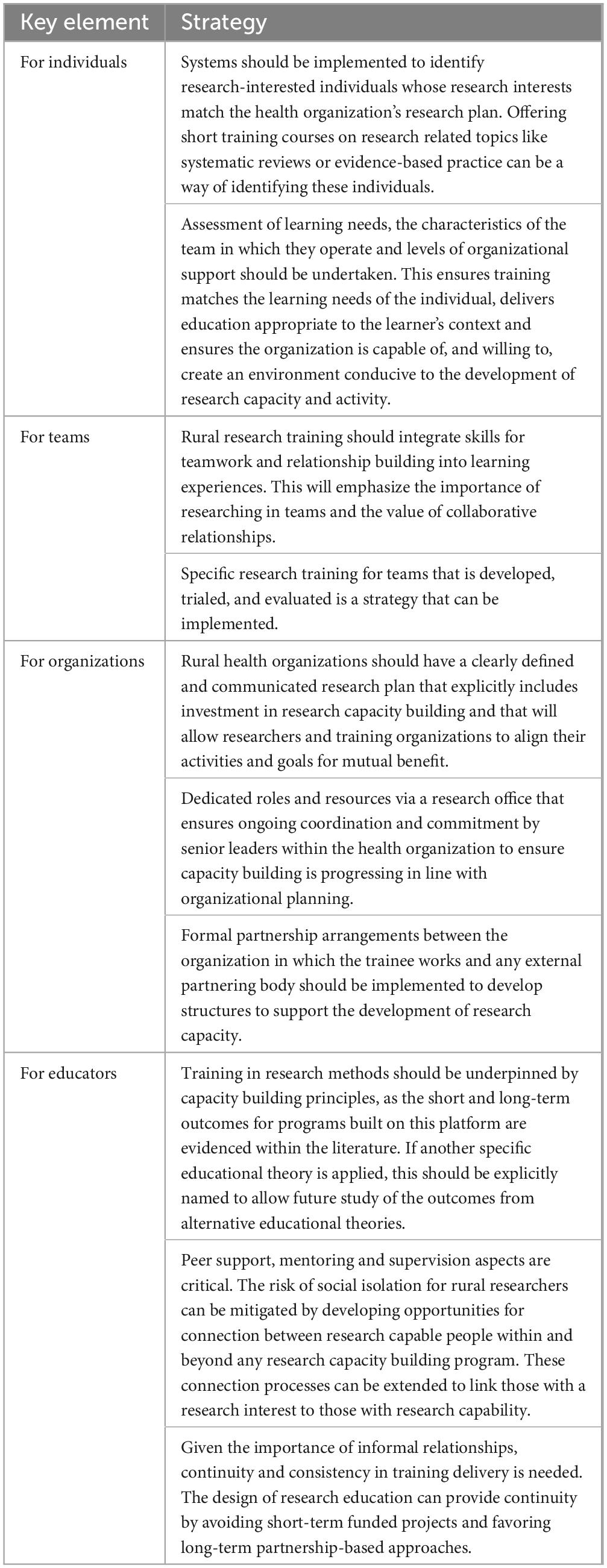
Table 4. Key elements and strategies to optimize rural research capacity building (103).
4 Discussion
Embedding academic researchers into rural health services provides a number of solutions to problems within rural organizations (82). Given the challenges associated with attracting and retaining rural academics (83), the idea of creating research-capable rural health workers that function as clinician-researchers is appealing. The “train them where you need them” philosophy has been shown to be instrumental for building and retaining rural workforce in health services such as medicine, nursing and allied health (84–87). Applying this principle to research, developing research experience and research capacity within rural health services will lead to rural-relevant research that leads to improved healthcare for rural communities.
There is no single model of research capacity building that can be applied across rural environments. While distributed programs built on a capacity building framework (28, 29, 55) are seen within the NSW context, programs built on other foundations also aim to build elements of research capability such as experience and research skill, or increase both research capability and research capacity in individuals (65, 76, 88–90). Educational philosophy is a component of research capacity building literature which did not emerge as a causative mechanism within this synthesis. Ensuring that educational foundations are described in future studies would allow exploration of alternate foundations and the outcomes of these educational approaches.
Educational and capacity building approaches are most effective when they incorporate experiential learning (61). Experiential elements extend the learning experience from building capability to building capacity, simply by the act of doing. From a learning point of view, “doing” or applying knowledge demonstrates a greater level of expertise than “learning about” (91).
Those building health research capacity must account for the unique characteristics and context of the rural environment; the organization’s goals, the individual’s position within the organization and the willingness of the organization to tangibly support the individual through funding or protected time for research. Models may need to be designed with a structure that assists learners in overcoming rural or remote challenges, including programs designed to reduce isolation for learners (33), as reduced isolation is associated with completion of researcher training in rural areas (34).
As there is limited research expertise within rural health services, capacity building approaches must include partnering for expertise. Partnering may be internal within the organization or with an external partner such as a university (92), but must be mutually beneficial and without the rural health organization ceding control of the direction of the research (54). Maximizing the value in existing relationships using a collaborative approach is a logical means of extending support. Rural universities have a role in researcher development through higher degree programs, and have undertaken a range of collaboration approaches with health services (92). The articulation between university-based and workplace-based training approaches is an area for further exploration.
Alongside this experiential component there is a need for targeted education. Given the limited critical mass of research expertise in rural areas this education is likely to be introductory research methods. However, “liberating the talents” (61) may mean that research education builds on existing skills rather than assuming all rural staff are commencing as novices. An assessment of learning needs should enable educational opportunities at the required level, rather than a generic approach.
Being an informed consumer of research that knows how to understand and apply research as part of evidence-based practice does not mean that all rural clinicians need to be capable of undertaking a research project. Selecting individuals for research capacity building opportunities should balance the passion of the individual and the needs of their organization. A committed and enthusiastic individual may become a valuable independent researcher given the right support.
Delivering training at the individual level will produce primarily individual level outcomes. Despite limited evidence of team approaches to research capacity building, a team approach does present as a structural solution to the risk of isolation for rural health workers undertaking research. Training in teams also maximizes the use of existing expertise with a rural team, again “liberating the talents” (61).
In addition to formal learning, research capacity can be enhanced through peer learning, with those who have research experience taking a role in building research activity and capacity with those around them (55). Learning about research by interacting with others who are undertaking research can be a form of cultural constructivism (33, 93), where a sense of belonging in the world of research is constructed through interaction and immersion, as well as activity and education. Connecting research capable and research interested individuals is a means of providing a supportive environment.
Extending capability into research capacity is more than an educational endeavor (94). As a health system the focus has often been on developing the motivated individual without the accompanying supportive environment (94). Structural supports (54) and meaningful opportunity to conduct research post-training (55) are essential to addresses the limited opportunities and structural inhibitors that prevent the transformation of research capability into research capacity. An organization committing to developing a rural health worker into a clinician-researcher should make a similar organizational commitment to creating conditions in which a clinician-researcher can function as both clinician and researcher. This combination of “smart and motivated people positioned in supportive environments that allow(ed) them to ask hard questions and pursue hard problems” is the key to success for clinician-researchers (95).
Delivery of research capacity building programs or approaches by those internal to the health system may influence the development of these supportive environments in a way that external education providers cannot. While informal relationships are a cornerstone of rural collaboration, training providers from outside the health system may need to partner with rural health organizations in formal agreements in addition to reciprocity and mutual respect (54). Continuity is important to building relationships, and consistent long-term offering of a research capacity building program (55) adds to this continuity.
Extending this concept of organizational commitment, there needs to be an operational responsibility for research (53). Aligning individual research effort to organizational direction is needed (54). The provision of a clear research direction for the rural health organization, one that is signaled as important (61), will allow clinicians to align their own research agenda to that of their organization. Specific research directions within an organization can allow external education partners to align teaching goals and processes to this direction. This allows effective partnering without the health organization ceding control of the direction of research activity and education (54).
Urban-centered research conducted in rural areas does little to enhance research capacity in the rural workforce, and ensuring urban-developed research has a rural individual as part of the project team is a practical capacity building step. This brings rural staff into contact with experienced researchers, thus maximizing the rural benefit of this research activity (53). Other models such as embedded researchers may also provide a more engaged organization (22, 26, 82). Similarly, a more egalitarian funding model that emphasizes partnerships may provide greater capacity building potential (18).
Lastly, organizations can address the “too rural and too poor” perception by adjusting the way in which they perceive and value research. Structures such as the hierarchy of evidence (96) and the way in which small-scale clinician-led research has been gradually subsumed by larger research driven by networks (97, 98) may lead rural organizations to view smaller, clinician-led projects to be of little or no value. Supporting, acknowledging, valuing and celebrating these smaller projects, “signaling importance” (61), can add to real-world research capacity. This small-scale research capacity can become a foundational building block for larger future research activity or for collaboration with a larger research organization.
In NSW the combination of individual LHDs with a centralized “system manager” (51) presents an opportunity for an educational body within the central system to interact with and influence the individual rural organizations. Australian states with a greater or lesser degree of centralization will have different challenges. Internationally the difference in health funding models and health system structures should also be acknowledged.
This synthesis has considered factors at three of the four structural levels of capacity building; individual, team and organizational (57, 58). Additional research considering the supra-organizational level, that is system-wide and policy factors, again from a critical realist perspective, would add another layer of depth in addition to the levels explored in this synthesis. This would be possible only in a program or programs that have been running for a sufficient length of time for outcomes of this type to be realistically achieved. Other future research directions include expanding team-level rural research capacity building approaches started in Queensland (19) and a nuanced economic evaluation of a capacity building program for rural areas which explores the longer-term value of investment in research capacity building from a business perspective. Research training, along with valuing and supporting research at multiple levels of an organization can lead toward a research-supportive culture (53). Research culture is often measured by self-report (45, 77, 99). An ethnographic study exploring the impact on research culture within a team as a result of training individuals in research would provide valuable insights and could be incorporated into a critical realist perspective (100).
4.1 Strengths and limitations of this synthesis
This synthesis draws from five papers containing small sample sizes, which may be considered a limitation. The size of these studies are consistent with similar studies in this field, and the studies themselves have samples representative of their trainees drawn from organizations typical of large rural health services within NSW. The focus on the NSW, and similar, contexts may limit generalizability however the nature of realist approaches is to explore what works for who in what circumstance (101). A broader approach which includes a wide range of contexts would in turn limit the ability to derive new understandings using realist approaches.
Drawing data from a single body of work may be seen as a potential limitation. The primary author’s position is as an insider who works in rural health research. This can be both a strength and limitation, with this insider perspective and inherent knowledge allowed for nuanced exploration and the expertise to apply retroductive processes and develop explanatory mechanisms of “why things are as they are” using critical realism (102). Offsetting these strengths is the limitation inherent with the personal biases brought by the researcher. Reflexive practices and consistent application of bracketing were used to enhance the rigor of this synthesis.
The diversity of source and approach enabled by different organizations, research types and data collection methods is a strength of this synthesis. Combining these as a single body of work in this synthesis is made possible by the use of critical realism, which embraces diversity in research methods.
5 Conclusion
This synthesis of studies focused on rural research capacity building has revealed a range of mechanisms including prevailing attitudes toward research, limited organizational valuing of research and a disconnect between individual and organizational research priorities, along with limited access to research expertise in rural health services. These inhibitory mechanisms are countered using existing relationships to build informal collaborations within teams and organizations to maximize the use of current expertise.
Distributed research education is important but not sufficient alone to develop rural clinicians into clinician-researchers. Structural supports are needed within rural health organizations, including organizational commitment to create environments in which rural health workers can learn about research, develop research experience and opportunities to undertake research. It is this combination of research training and supportive environments that will lead to optimized rural research capacity.
Capacity building endeavors should carefully consider the learner context and commit to long-term relationship-based approaches to rural research training programs. Further structural solutions such as the design of distributed education programs, creative ways to enable protected research time, and strategic engagement with the hosting organization are important aspects of research capacity building.
Individual level interventions have driven individual level outcomes. These are important but may miss opportunities to maximize the potential to move from individual capability to individual and organizational research capacity in rural health organizations. Considering and addressing structural supports will not only inform the next stage of organizational investment but will maximize the benefits of distributed training for rural research capacity building.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
DS: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Validation, Writing – original draft, Writing – review & editing. EW: Formal Analysis, Investigation, Methodology, Supervision, Validation, Writing – review & editing. DL: Investigation, Methodology, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
Then authors wish to acknowledge the contribution of Kerith Duncanson and Zoe Michaleff for their contributions in testing derived mechanisms from this synthesis.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
2. Pong R, Desmeules M, Lagacé C. Rural-urban disparities in health: How does Canada fare and how does Canada compare with Australia? Aust J Rural Health. (2009) 17:58–64. doi: 10.1111/j.1440-1584.2008.01039.x
3. Roots R, Li L. Recruitment and retention of occupational therapists and physiotherapists in rural regions: A meta-synthesis. BMC Health Serv Res. (2013) 13:59. doi: 10.1186/1472-6963-13-59
4. Smith K, Humphreys J, Wilson M. Addressing the health disadvantage of rural populations: How does epidemiological evidence inform rural health policies and research? Aust J Rural Health. (2008) 16:56–66. doi: 10.1111/j.1440-1584.2008.00953.x
5. Australian Institute of Health and Welfare. General practice, allied health and other primary care services. Canberra, ACT: AIHW (2022).
6. Dixon J, Welch N. Researching the rural-metropolitan health differential using the ‘social determinants of health’. Aust J Rural Health. (2000) 8:254–60. doi: 10.1046/j.1440-1584.2000.00327.x
7. McDonald E, Bailie R, Michel T. Development and trialling of a tool to support a systems approach to improve social determinants of health in rural and remote Australian communities: The healthy community assessment tool. Int J Eq Health. (2013) 12:15. doi: 10.1186/1475-9276-12-15
8. Australian Government. In: Care DoHaA editor. National strategic framework for rural and remote health. Canberra, ACT: Australian Government (2020).
9. Parliament of New South Wales. Report 57 – Health outcomes and access to health and hospital services in rural, regional and remote New South Wales. Sydney, NSW: Parliament of New South Wales (2022).
10. Hayes K, Coxon K, Bye R. Rural and remote health care: The case for spatial justice. Rural Remote Health. (2025) 25:8580. doi: 10.22605/RRH8580
11. Alston L, Field M, Brew F, Payne W, Aras D, Versace V. Addressing the lack of research in rural communities through building rural health service research: Establishment of a research unit in Colac, a medium rural town. Aust J Rural Health. (2022) 30:536–9. doi: 10.1111/ajr.12860
12. Taylor J, Hughes C, Petkov J, Williams M. Unique issues in research and evaluation in rural and remote locations: Is there a place for specific research training? Rural Remote Health. (2005) 5:351. doi: 10.22605/RRH351
13. Allan J, Ball P, Alston M. Developing sustainable models of rural health care: A community development approach. Rural Remote Health. (2007) 7:818. doi: 10.22605/RRH818
14. Bell E, Harpur S, Doherty K, Struber J, Davies L. What is translational research? Background, concepts, and a definition. Public Health Yearbook. (2011) 2011:141.
15. Brown L, Urquhart L, Squires K, Crowley E, Heaney S, Kocanda L, et al. Starting from scratch: Developing and sustaining a rural research team lessons from a nutrition and dietetics case study. Aust J Rural Health. (2021) 29:729–41. doi: 10.1111/ajr.12787
16. Alston L, Bourke L, Nichols M, Allender S. Responsibility for evidence-based policy in cardiovascular disease in rural communities: Implications for persistent rural health inequalities. Aust Health Rev. (2020) 44:527–34. doi: 10.1071/AH19189
17. Wong Shee A, Quilliam C, Corboy D, Glenister K, McKinstry C, Beauchamp A, et al. What shapes research and research capacity building in rural health services? Context matters. Aust J Rural Health. (2022) 30:410–21. doi: 10.1111/ajr.12852
18. Auld R, Loppacher T, Rose S, Milat A, Penna A. Translational research grants scheme (TRGS): A new approach to strengthening health system research capacity. Public Health Res Pract. (2018) 28:2831818. doi: 10.17061/phrp2831818
19. Flenady T, Dwyer T, Kahl J, Sobolewska A, Reid-Searl K, Signal T. research ready grant program (RRGP) protocol: A model for collaborative multidisciplinary practice-research partnerships. Health Res Policy Syst. (2022) 20:62. doi: 10.1186/s12961-022-00870-x
20. Hulcombe J, Sturgess J, Souvlis T, Fitzgerald C. An approach to building research capacity for health practitioners in a public health environment: An organisational perspective. Aust Health Rev. (2014) 38:252–8. doi: 10.1071/AH13066
21. Asghari S, Heeley T, Walsh A, Rourke J, Bethune C, Graham W. Rural 360: Incubating socially accountable research in the Canadian North. Int J Circumpolar Health. (2019) 78:1633191. doi: 10.1080/22423982.2019.1633191
22. Wenke R, Ward E, Hickman I, Hulcombe J, Phillips R, Mickan S. Allied health research positions: A qualitative evaluation of their impact. Health Res Policy Syst. (2017) 15:6. doi: 10.1186/s12961-016-0166-4
23. Wenke R, Tynan A, Scott A, Mickan S. Effects and mechanisms of an allied health research position in a Queensland regional and rural health service: A descriptive case study. Aust Health Rev. (2018) 42:667–75. doi: 10.1071/AH17086
24. Mickan S, Coates D. Embedded researchers in Australia: Survey of profile and experience across medical, nursing and midwifery and allied health disciplines. J Clin Nurs. (2020) 23:417–26. doi: 10.1111/jocn.15593
25. Ward V, Tooman T, Reid B, Davies H, Marshall M. Embedding researchers into organisations: A study of the features of embedded research initiatives. Evid Policy. (2021) 17:593–614. doi: 10.1332/174426421X16165177580453
26. Wolfenden L, Yoong S, Williams C, Grimshaw J, Durrheim D, Gillham K, et al. Embedding researchers in health service organizations improves research translation and health service performance: The Australian Hunter New England population health example. J Clin Epidemiol. (2017) 85:3–11. doi: 10.1016/j.jclinepi.2017.03.007
27. Duncanson K, Webster E, Schmidt D. Impact of a remotely delivered, writing for publication program on publication outcomes of novice researchers. Rural Remote Health. (2018) 18:4468. doi: 10.22605/RRH4468
28. Schmidt D, Webster E, Duncanson K. Building research experience: Impact of a novice researcher development program for rural health workers. Aust J Rural Health. (2019) 27:392–7. doi: 10.1111/ajr.12520
29. Webster E, Thomas M, Ong N, Cutler L. Rural research capacity building program: Capacity building outcomes. Aust J Prim Health. (2011) 17:107–13. doi: 10.1071/PY10060
30. McCarthy P, Bethune C, Fitzgerald S, Graham W, Asghari S, Heeley T, et al. Curriculum development of 6for6: Longitudinal research skills program for rural and remote family physicians. Can Fam Phys. (2016) 62:e89–95.
31. Walsh A, Heeley T, Furlong B, Bethune C, Graham W, Asghari S. Rural health research capacity building: An anchored solution. Rural Remote Health. (2021) 21:6162. doi: 10.22605/RRH6162
32. Pain T, Petersen M, Fernando M. Building allied health research capacity at a regional Australian hospital: A follow-up study. Internet J Allied Health Sci Pract. (2018) 16:8. doi: 10.46743/1540-580x/2018.1813
33. Schmidt D, Kirby SA. modular approach to rural and remote research education: A project report. Rural Remote Health. (2016) 16:3609. doi: 10.22605/RRH3609
34. Schmidt D, Robinson K, Webster E. Factors influencing attrition from a researcher training program. Int J Res Dev. (2014) 5:56–67. doi: 10.1108/ijrd-08-2013-0013
35. Ried K, Montgomery B, Stocks N, Farmer E. General practice research training: Impact of the Australian registrar research workshop on research skills, confidence, interest and involvement of participants, 2002-2006. Fam Pract. (2008) 25:119–26. doi: 10.1093/fampra/cmn010
36. Asghari S, Heeley T, Bethune C, Graham W, MacLellan C, Button C, et al. Evaluation plan of the 6for6 research skills program for rural and remote physicians. Eval Program Plann. (2021) 87:101933. doi: 10.1016/j.evalprogplan.2021.101933
37. Kuzhabekova A, Lee J. International faculty contribution to local research capacity building: A view from publication data. Higher Educ Policy. (2018) 31:423–46. doi: 10.1057/s41307-017-0067-3
38. Ramkalawan T, Dieppe P. Research capacity development and training. J Health Serv Res Policy. (2008) 13:6–11. doi: 10.1258/jhsrp.2008.008008
39. Ewen S, Ryan T, Platania-Phung C. Capacity building of the Australian aboriginal and torres strait islander health researcher workforce: A narrative review. Hum Resour Health. (2019) 17:10. doi: 10.1186/s12960-019-0344-x
40. Finch E, Cornwell P, Ward E, McPhail S. Factors influencing research engagement: Research interest, confidence and experience in an Australian speech-language pathology workforce. BMC Health Serv Res. (2013) 13:144. doi: 10.1186/1472-6963-13-144
41. Bailey J, Veitch C, Crossland L, Preston R. Developing research capacity building for Aboriginal & torres strait islander health workers in health service settings. Rural Remote Health. (2006) 6:556. doi: 10.22605/RRH556
42. Stajic J, Harfield S, Brown A, Dawson A, Davy C, Aromataris E, et al. Evaluating a research capacity strengthening program for Aboriginal community-controlled health organisations. Aust J Prim Health. (2019) 25:72–81. doi: 10.1071/PY18058
43. Golenko X, Pager S, Holden LA. thematic analysis of the role of the organisation in building allied health research capacity: A senior managers’ perspective. BMC Health Serv Res. (2012) 12:276. doi: 10.1186/1472-6963-12-276
44. Grimmer K, Lizarondo L, Kumar S, Bell E, Buist M, Weinstein P. An evidence-based framework to measure quality of allied health care. Health Res Policy Syst. (2014) 12:10. doi: 10.1186/1478-4505-12-10
45. Matus J, Wenke R, Hughes I, Mickan S. Evaluation of the research capacity and culture of allied health professionals in a large regional public health service. J Multidiscip Healthc. (2019) 12:83–96. doi: 10.2147/JMDH.S178696
46. McCurtin A, O’Connor A. Building a collaborative research community of practice and supporting research engagement in speech-language pathology: Identification of stakeholder priorities. JBI Evid Implement. (2020) 18:368–75. doi: 10.1097/XEB.0000000000000229
47. Nightingale J, Fowler-Davis S, Grafton K, Kelly S, Langham C, Lewis R, et al. The role of allied health professions and nursing research internships in developing a research culture: A mixed-methods exploration of stakeholder perspectives. Health Res Policy Syst. (2020) 18:122. doi: 10.1186/s12961-020-00638-1
48. Brett T, Sherrard R, Bower A. Research capacity building in general practice–a new opportunity in Fremantle, WA. Aust Fam Phys. (2006) 35:65–6.
49. McIntyre E, Brun L, Cameron H. Researcher development program of the primary health care research, evaluation and development strategy. Aust J Prim Health. (2011) 17:114–21. doi: 10.1071/PY10049
50. Meurer L, DeNomie M, Morzinski J, Nelson D, Meurer J, Chandler T, et al. Incorporating community engagement in primary care research training: Eleven-year outcomes. Prog Commun Health Partnersh. (2020) 14:63–74. doi: 10.1353/cpr.2020.0009
52. Schmidt D. What a great idea! Someone should evaluate that. Aust Health Rev. (2016) 40:270–2. doi: 10.1071/AH14215
53. Schmidt D, Reyment J, Kirby S, Webster E, Lyle D. The place of research in the rural health workplace structure: A content analysis of a rural health organisation’s strategic and operational documents. Rural Remote Health. (2020) 20:5493. doi: 10.22605/RRH5493
54. Schmidt D, Reyment J, Webster E, Kirby S, Lyle D. Workplace-based health research training: A qualitative study of perceived needs in a rural setting. Health Res Policy Syst. (2020) 18:67. doi: 10.1186/s12961-020-00580-2
55. Schmidt D, Duncanson K, Webster E, Saurman E, Lyle D. Critical realist exploration of long-term outcomes, impacts and skill development from an Australian rural research capacity building programme: A qualitative study. BMJ Open. (2022) 12:e065972. doi: 10.1136/bmjopen-2022-065972
56. Greenhalgh J, Edwards PK, O’Mahoney J, Vincent S. Realist synthesis. Studying organizations using critical realism: A practical guide. Oxford: Oxford University Press (2014). p. 264–81.
57. Cooke JA. framework to evaluate research capacity building in health care. BMC Fam Pract. (2005) 6:44. doi: 10.1186/1471-2296-6-44
58. Sarre G, Cooke J. Developing indicators for measuring Research Capacity Development in primary care organizations: A consensus approach using a nominal group technique. Health Soc Care Commun. (2009) 17:244–53. doi: 10.1111/j.1365-2524.2008.00821.x
60. Kempster S, Parry K. Critical realism and grounded theory. In: <snm>Edwards, O’Mahoney J</gnm>, <snm>Vincent S</gnm> editors. Studying organizations using critical realism: A practical guide. Oxford: Oxford University Press (2014). p. 86–108.
61. Cooke J, Gardois P, Booth A. Uncovering the mechanisms of research capacity development in health and social care: A realist synthesis. Health Res Policy Syst. (2018) 16:93. doi: 10.1186/s12961-018-0363-4
62. Dörfler V, Stierand M. Bracketing: A phenomenological theory applied through transpersonal reflexivity. J Organ Change Manag. (2020) 34:778–93. doi: 10.1108/JOCM-12-2019-0393
63. Tufford L, Newman P. Bracketing in qualitative research. Q Soc Work. (2012) 11:80–96. doi: 10.1177/1473325010368316
64. Fischer C. Bracketing in qualitative research: Conceptual and practical matters. Psychother Res. (2009) 19:583–90. doi: 10.1080/10503300902798375
65. Jones A, Burgess T, Farmer E, Fuller J, Stocks N, Taylor J, et al. Building research capacity. An exploratory model of GPs’ training needs and barriers to research involvement. Aust Fam Phys. (2003) 32:957–60.
66. Matus J, Walker A, Mickan S. Research capacity building frameworks for allied health professionals – a systematic review. BMC Health Serv Res. (2018) 18:716. doi: 10.1186/s12913-018-3518-7
67. Wenke R, Noble C, Weir K, Mickan S. What influences allied health clinician participation in research in the public hospital setting: A qualitative theory-informed approach. BMJ Open. (2020) 10:e036183. doi: 10.1136/bmjopen-2019-036183
68. Barclay L, Phillips A, Lyle D. Rural and remote health research: Does the investment match the need? Aust J Rural Health. (2018) 26:74–9. doi: 10.1111/ajr.12429
69. Cochran-Smith M, Ell F, Grudnoff L, Ludlow L, Haigh M, Hill M. When complexity theory meets critical realism: A platform for research on initial teacher education. Teach Educ Q. (2014) 41:105–22.
70. Lawani A. Critical realism: What you should know and how to apply it. Q Res J. (2021) 21:320–33. doi: 10.1108/QRJ-08-2020-0101
71. Vincent S, O’Mahoney J. Critical realism as an empirical project. Oxford: Oxford University Press (2014).
72. Nyström M, Karltun J, Keller C, Andersson Gäre B. Collaborative and partnership research for improvement of health and social services: Researcher’s experiences from 20 projects. Health Res Policy Syst. (2018) 16:46. doi: 10.1186/s12961-018-0322-0
73. Dernova M. Experiential learning theory as one of the foundations of adult learning practice worldwide. Comp Profess Pedag. (2015) 2:52–7. doi: 10.1515/rpp-2015-0040
74. Knowles M, Holton E, Swanson R. The adult learner: The definitive classic in adult education and human resource development. 6th ed. Boston, MA: Elsevier (2005).
75. Smith H, Wright D, Morgan S, Dunleavey J, Moore M. The ‘research spider’: A simple method of assessing research experience. Prim Health Care Res Dev. (2002) 3:139–40. doi: 10.1191/1463423602pc102xx
76. Harding K, Stephens D, Taylor N, Chu E, Wilby A. Development and evaluation of an allied health research training scheme. J Allied Health. (2010) 39:e143–8.
77. Raschke N, Bradbury J, Yoxall J. Perceptions of research capacity in public health organisations: Comparison of NSW metropolitan and non-metropolitan local health districts. Aust Health Rev. (2022) 46:746–55. doi: 10.1071/AH22100
78. Cooke J, Nancarrow S, Dyas J, Williams M. An evaluation of the ‘designated research team’ approach to building research capacity in primary care. BMC Fam Pract. (2008) 9:37. doi: 10.1186/1471-2296-9-37
79. Nelson L, Morrison-Beedy D. Research team training: Moving beyond job descriptions. Appl Nurs Res. (2008) 21:159–64. doi: 10.1016/j.apnr.2006.09.001
80. Priest H, Segrott J, Green B, Rout A. Harnessing collaboration to build nursing research capacity: A research team journey. Nurse Educ Today. (2007) 27:577–87. doi: 10.1016/j.nedt.2006.08.019
81. Whitworth A, Haining S, Stringer H. Enhancing research capacity across healthcare and higher education sectors: Development and evaluation of an integrated model. BMC Health Serv Res. (2012) 12:287. doi: 10.1186/1472-6963-12-287
82. Moran A, Haines H, Raschke N, Schmidt D, Koschel A, Stephens A, et al. Mind the gap: Is it time to invest in embedded researchers in regional, rural and remote health services to address health outcome discrepancies for those living in rural, remote and regional areas? Aust J Prim Health. (2019) 25:104–7. doi: 10.1071/PY18201
83. Ndebele C, Muhuro P, Nkonki V. Rurality and the professional development of university teachers. South Afr J High Educ. (2016) 30:127–45. doi: 10.20853/30-6-728
84. Laven G, Wilkinson D. Rural doctors and rural backgrounds: How strong is the evidence? A systematic review. Aust J Rural Health. (2003) 11:277–84. doi: 10.1111/j.1440-1584.2003.00534.x
85. Manahan C, Hardy C, MacLeod M. Personal characteristics and experiences of long-term allied health professionals in rural and northern British Columbia. Rural Remote Health. (2009) 9:1238.
86. McGrail M, O’Sullivan B, Russell D. Rural training pathways: The return rate of doctors to work in the same region as their basic medical training. Hum Resour Health. (2018) 16:56. doi: 10.1186/s12960-018-0323-7
87. Playford D, Wheatland B, Larson A. Does teaching an entire nursing degree rurally have more workforce impact than rural placements? Contemp Nurse. (2010) 35:68–76. doi: 10.5172/conu.2010.35.1.068
88. Aggarwal R, Gupte N, Kass N, Taylor H, Ali J, Bhan A, et al. A comparison of online versus on-site training in health research methodology: A randomized study. BMC Med Educ. (2011) 11:37. doi: 10.1186/1472-6920-11-37
89. Awaisu A, Kheir N, Alrowashdeh H, Allouch S, Jebara T, Zaidan M, et al. Impact of a pharmacy practice research capacity-building programme on improving the research abilities of pharmacists at two specialised tertiary care hospitals in Qatar: A preliminary study. J Pharm Health Serv Res. (2015) 6:155–64. doi: 10.1111/jphs.12101
90. Bäck-Pettersson S, Jensen K, Kylén S, Sernert N, Hermansson E. Nurses’ experiences of participation in a research and development programme. J Clin Nurs. (2013) 22:1103–11. doi: 10.1111/j.1365-2702.2012.04297.x
91. Williams B, Byrne P, Welindt D, Williams M. Miller’s pyramid and core competency assessment: A study in relationship construct validity. J Contin Educ Health Prof. (2016) 36:295–9. doi: 10.1097/CEH.0000000000000117
92. Nott M, Schmidt D, Thomas M, Reilly K, Saksena T, Kennedy J, et al. Collaborations between health services and educational institutions to develop research capacity in health services and health service staff: A systematic scoping review. BMC Health Serv Res. (2024) 24:1363. doi: 10.1186/s12913-024-11836-w
93. Stauffacher M, Walter A, Lang D, Wiek A, Scholz R. Learning to research environmental problems from a functional socio-cultural constructivism perspective. Int J Sustain High Educ. (2006) 7:252–75. doi: 10.1108/14676370610677838
94. Grundy J, Johnston F. Building research capacity in primary health care settings in the Northern Territory. Aust J Prim Health. (2003) 9:9–17. doi: 10.1071/PY03002
95. Jain M, Cheung V, Utz P, Kobilka B, Yamada T, Lefkowitz R. Saving the endangered physician-scientist –a plan for accelerating medical breakthroughs. N Engl J Med. (2019) 381:399–402. doi: 10.1056/NEJMp1904482
96. Evans D. Hierarchy of evidence: A framework for ranking evidence evaluating healthcare interventions. J Clin Nurs. (2003) 12:77–84. doi: 10.1046/j.1365-2702.2003.00662.x
97. Murdoch J. The end of practice-based research? Br J Gen Pract. (2009) 59:52. doi: 10.3399/bjgp09X394897
99. Holden L, Pager S, Golenko X, Ware R. Validation of the research capacity and culture (RCC) tool: Measuring RCC at individual, team and organisation levels. Aust J Prim Health. (2012) 18:62–7. doi: 10.1071/PY10081
101. Nielsen K, Miraglia M. What works for whom in which circumstances? On the need to move beyond the ‘what works?’ Question in organizational intervention research. Hum Relat. (2017) 70:40–62. doi: 10.1177/001872671667
102. Stutchbury K. Critical realism: An explanatory framework for small-scale qualitative studies or an ‘unhelpful edifice’? Int J Res Method Educ. (2022) 45:113–28. doi: 10.1080/1743727X.2021.1966623
Keywords: distributed training, research education, rural health, workplace-based education, realist synthesis
Citation: Schmidt D, Webster E and Lyle D (2025) Mechanisms to build research capacity in the rural health workplace: a realist synthesis. Front. Med. 12:1584904. doi: 10.3389/fmed.2025.1584904
Received: 27 February 2025; Accepted: 02 June 2025;
Published: 19 June 2025.
Edited by:
Roger Peter Strasser, Northern Ontario School of Medicine University, CanadaReviewed by:
Michael J. Wolyniak, Hampden–Sydney College, United StatesLigia Garcia-Bejar, Panamerican University, Mexico
Carol McKinstry, La Trobe University, Australia
Copyright © 2025 Schmidt, Webster and Lyle. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: David Schmidt, ZGF2aWQuc2NobWlkdEBzeWRuZXkuZWR1LmF1
†These authors share senior authorship
 David Schmidt
David Schmidt Emma Webster
Emma Webster David Lyle†
David Lyle†