Abstract
Objective:
To compare high-flow nasal cannula (HFNC) oxygen therapy and non-invasive ventilation (NIV) for patients after liberation from invasive mechanical ventilation, to assess whether HFNC is better than NIV at improving blood gases [PaO2, PaCO2, and oxygenation index (OI)], reducing re-intubation rates, pulmonary infections, mortality, and shortening the length of stay in intensive care unit (ICU), and to evaluate if HFNC is a feasible alternative to NIV for respiratory support.
Methods:
This meta-analysis included randomized controlled trials (RCTs) and non-RCTs (NRCTs) from PubMed, Web of Science, CNKI, and Wanfang for further assessment. Evaluation indexes included PaO2, PaCO2, OI, re-intubation rate, pulmonary infection rate, length of stay in ICU, and mortality rate.
Results:
HFNC showed higher PaO2 [MD = 2.95, 95%CI (2.23, 3.67), p < 0.00001], lower PaCO2 [MD = −3.04, 95%CI (−3.56, −2.52), p < 0.00001], higher OI [MD = 10.98, 95%CI (6.52, 15.45), p < 0.00001], lower re-intubation rate [OR = 0.45, 95%CI (0.33, 0.63), p < 0.00001], and shorter length of stay in ICU [MD = −6.15, 95%CI (−6.86, −5.44), p < 0.00001] compared to NIV. Additionally, no significant differences in pulmonary infection rate [OR = 0.57, 95%CI (0.29, 1.11), p = 0.10] or mortality [OR = 1.29, 95%CI (0.96, 1.72), p = 0.09] were observed between HFNC and NIV.
Conclusion:
HFNC can improve PaO2 and OI, reduce PaCO2, re-intubation rate, and length of stay in ICU, with no difference in pulmonary infection or mortality compared to NIV, supporting it as a viable clinical alternative for post-extubation respiratory support.
1 Introduction
Invasive mechanical ventilation has been recognized to be an important supportive measure for acute respiratory failure. However, complications such as asphyxia, dyspnea and hypoxemia during tracheal extubation after condition stabilization, when patients are ready for extubation, will increase the risk of pulmonary infection and prolong the length of stay in the hospital (1). It highlights the significance and requirement for one mode of non-invasive ventilation after invasive ventilation. As clinical practice advances, a series of research hotspots and controversial issues have emerged in the application of oxygen therapy. Currently, there are three non-invasive modalities to increase post-extubation oxygenation, including conventional oxygen therapy, high-flow nasal cannula (HFNC) oxygen therapy, and non-invasive ventilation (NIV) (2). Clinically, NIV is a relatively common therapeutic option for managing patients with respiratory failure, which can facilitate an effective relief of dyspnea, reduce arterial partial pressure of carbon dioxide (PaCO2) and increase arterial partial pressure of oxygen (PaO2) in patients. However, its therapeutic effect may be compromised by factors such as relatively high complication rate and poor tolerance in some patients (3).
It promotes the introduction of novel therapeutic approaches in the clinical setting. Among these, HFNC has been gradually concerned due to its significant effects (4). HFNC, with the functions of providing heating and humidification, was initially used for neonates or infants with respiratory distress (5). It can deliver oxygen at a gas flow rate of 0–60 L/min, an oxygen concentration of 21–100%, and a temperature of 37 °C. It can meet patients’ requirements for humidity and temperature simultaneously, thus alleviating the damage to the tracheal mucosa caused by humidity and temperature during conventional oxygen therapy (6).
HFNC offers better comfort than NIV, which can improve patients’ compliance to cooperate with treatment (7, 8), consequently holding significant potential for broader clinical application. However, it is still inconclusive regarding the clinical efficacy of HFNC revealed by current evidence. Therefore, based on the retrieval of literature comparing HFNC with NIV in post-extubation patients, this study employed a systematic review and meta-analysis. Existing meta-analyses, despite investigation on the efficacy differences between HFNC and NIV (9, 10), possess significant limitations, such as primarily focusing on adult COPD patients. In contrast, this study included populations with multiple conditions and of diverse age groups (premature infants, lung transplant recipients, and post-cardiac surgery patients), covering a wider range of underlying diseases and patients. Significantly, this design in our study may address clinical scenarios not covered by prior research, which can benefit a better interpretation of heterogeneity encountered in real-world clinical practice, and enhance the robustness of conclusions through sensitivity analysis and based on a larger sample size. This study intended to evaluate whether HFNC is an effective and safe therapeutic modality, whether it offers advantages over NIV, and whether it can serve as an alternative strategy to NIV, thereby providing evidence-based support for the clinical application of HFNC.
2 Data and methods
2.1 Study selection
This study focused on the inclusion of randomized controlled trials (RCTs) or non-RCTs (NRCTs) investigating sequential therapy with HFNC or NIV in patients following liberation from invasive mechanical ventilation. These trials enrolled patients with: chronic obstructive pulmonary disease (COPD) complicated by type II respiratory failure, acute exacerbation of COPD, post-lung transplantation, acute respiratory failure, postoperative hypoxemia, and post-extubation preterm infants. Eligible studies compared HFNC with NIV reporting at least one of the following outcomes were included: ① PaO2, ② PaCO2, ③ oxygenation index (OI), ④ re-intubation rate, ⑤ pulmonary infection rate, ⑥ length of stay in intensive care unit (ICU), and ⑦ mortality rate. In addition to the inclusion criteria, this study also collected patients’ characteristics, such as age, gender, sample size, and features of the intervention and control groups. We excluded studies involving: (1) patients without a history of intubation therapy, (2) literature with incomplete raw data, (3) duplicate publications, and (4) literature in languages other than Chinese or English. Ethical approval was not required for this systematic review as it did not utilize patient-level data.
2.2 Electronic search strategy
We searched for studies comparing the sequential efficacy of HFNC and NIV in patients following invasive mechanical ventilation from PubMed, Web of Science, CNKI, and Wanfang, from database inception to February 2025. Search terms included: (“Non-Positive Pressure Ventilation” OR “NPPV” OR “Non-Invasive Positive Pressure Ventilation” OR “NIPPV” OR “Non-invasive ventilation” OR “NIV” AND “High-flow oxygen therapy” OR “High-flow nasal cannula” OR “HFNC”).
2.3 Data collection and analysis
Through management using EndNote X9, the retrieved literature was independently screened by reviewing corresponding titles and abstracts by two authors. With the exclusion of literature that was obviously not relevant to our research, the remaining articles underwent full-text review based on the predefined inclusion and exclusion criteria. The methodological quality and extracted data were assessed by two researchers independently; and discrepancies were resolved through discussion or by a third reviewer. Corresponding authors were contacted for complete raw data if necessary.
2.4 Literature quality assessment
The quality of the included eligible studies was independently assessed by two researchers using the Cochrane Handbook for Systematic Reviews of Interventions and Review Manager (RevMan) software version 5.3. Evaluation criteria encompassed: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other potential sources of bias. Based on the risk of bias scores, literature quality was categorized as low risk (≥5 points), moderate risk (3–4 points), or high risk (1–2 points) (11).
2.5 Statistical analysis
Meta-analysis was conducted using RevMan 5.3, with mean difference (MD) and odds ratio (OR) for continuous variables and dichotomous variables, respectively, both reported with 95% confidence intervals (CI). According to the assessment of heterogeneity using I2 and p-values, fixed-effects model and random-effects model were, respectively, adopted when there was low (p > 0.1 and I2 < 50%) and high heterogeneity (p ≤ 0.1 and I2 ≥ 50%) (12), with sensitivity analysis employed to identify heterogeneity sources. Sensitivity analysis was performed by removing individual studies to assess their impact on the overall results. Finally, forest and fennel plots were generated to indicate the meta-analysis results, and assess publication bias, respectively. Statistical significance was set at p < 0.05.
3 Results
3.1 Literature search results and flow chart of literature screening flow
Initially, 959 articles were retrieved from PubMed, Web of Science, CNKI, and Wanfang databases. Finally, 20 (13–32) studies [18 RCTs (13–30) and 2 NRCTs (31, 32)] were included for meta-analysis after removing 389 duplicates, 272 irrelevant articles, 195 non-compliant studies, 65 reviews, and 18 articles with incomplete data. These studies involved 3,159 patients, including 1,447 in the HFNC group and 1,712 in the NIV group. The screening process is detailed in Figure 1, and the baseline characteristics of the included studies are summarized in Table 1.
Figure 1

Literature screening flow chart.
Table 1
| Author | Country of publication | Type of study | Sample size (cases) | Sex (M/F) | Age | Primary disease | Outcome indicator | |||
|---|---|---|---|---|---|---|---|---|---|---|
| HNFC Group | NIV Group | HNFC group | NIV group | HNFC group | NIV group | |||||
| Li (13) | China | RCT | 36 | 36 | 21/15 | 19/17 | (65.32 ± 10.88) | (65.28 ± 11.91) | COPD combined with type II respiratory failure | ①②③④⑥ |
| Gao et al. (14) | China | RCT | 206 | 276 | 37/69 | 188/88 | (62.34 ± 5.54) | (62.57 ± 4.10) | Post-operative cardiac hypoxemia | ①②④⑤⑥ |
| Huang et al. (15) | China | RCT | 28 | 32 | 22/6 | 23/9 | (64.50 ± 3.21) | (65.28 ± 4.87) | Acute exacerbation of COPD | ②③④⑥ |
| Yuan (16) | China | RCT | 56 | 44 | 31/25 | 25/19 | (49.01 ± 9.00) | (52.00 ± 8.02) | Post Lung Transplantation | ④⑥ |
| Huang et al. (17) | China | RCT | 150 | 151 | 97/53 | 91/60 | (72.87 ± 6.97) | (72.92 ± 7.11) | Acute respiratory failure | ①②⑥⑦ |
| Yu et al. (18) | China | RCT | 18 | 17 | 13/5 | 11/6 | (75.00 ± 5.10) | (71.00 ± 6.50) | Acute exacerbation of COPD | ①②④⑥ |
| Han et al. (19) | China | RCT | 55 | 55 | 36/19 | 35/20 | (65.70 ± 7.30) | (66.20 ± 6.80) | Acute exacerbation of COPD | ①②④⑥⑦ |
| Xu et al. (20) | China | RCT | 43 | 43 | 26/17 | 28/15 | (65.80 ± 4.60) | (65.20 ± 5.30) | COPD | ①②④⑥ |
| Yue (21) | China | RCT | 30 | 30 | 20/10 | 21/9 | (78.34 ± 2.16) | (78.27 ± 2.33) | COPD | ①②③④⑥ |
| Zhang (22) | China | RCT | 40 | 40 | 27/13 | 25/15 | (67.41 ± 18.92) | (68.15 ± 16.22) | Acute exacerbation of COPD | ①②③④⑥ |
| Li et al. (23) | China | RCT | 24 | 21 | 17/7 | 16/5 | (52.30 ± 18.50) | (48.91 ± 22.40) | Post-operative hypoxemia | ②③④⑥⑦ |
| Wang et al. (24) | China | RCT | 24 | 24 | 15/9 | 13/11 | (51.30 ± 11.60) | (53.80 ± 9.30) | Post Lung Transplantation | ③④⑤⑥⑦ |
| Chen et al. (25) | China | RCT | 48 | 46 | 30/18 | 29/17 | (27.20 ± 2.80) | (27.50 ± 3.200) | Preterm infants after extubation | ④ |
| Uchiyama et al. (26) | Japan | RCT | 176 | 196 | 91/85 | 97/99 | (28.40 ± 3.00) | (28.20 ± 3.00) | Preterm infants after extubation | ②④ |
| Liu et al. (27) | USA | RCT | 82 | 96 | 52/29 | 32/64 | 48~74 | 47~72 | Sequential therapy after mechanical ventilation | ④⑥⑦ |
| Shi and Qiu (28) | China | RCT | 60 | 60 | 32/28 | 36/24 | 64.64 ± 10.34 | (64.64 ± 10.34) | AE-COPD combined with type II respiratory failure | ①②③ |
| Zheng and Wang (29) | China | RCT | 47 | 47 | 27/20 | 25/22 | 60.57 ± 6.09 | 61.42 ± 6.17 | Acute respiratory failure | ②③④ |
| Lu et al. (30) | China | RCT | 49 | 48 | 28/21 | 30/18 | 67.88 ± 10.36 | 68.31 ± 9.62 | AE-COPD combined with type II respiratory failure | ①②⑦ |
| Koga et al. (31) | Japan | NRCT | 200 | 378 | 127/73 | 231/147 | 66–82 | 69–84 | Acute respiratory failure | ⑦ |
| Chen et al. (32) | China | NRCT | 75 | 72 | 43/32 | 38/34 | 70 ± 14 | 69 ± 16 | Respiratory failure | ①②④⑦ |
Baseline characteristics of the included studies.
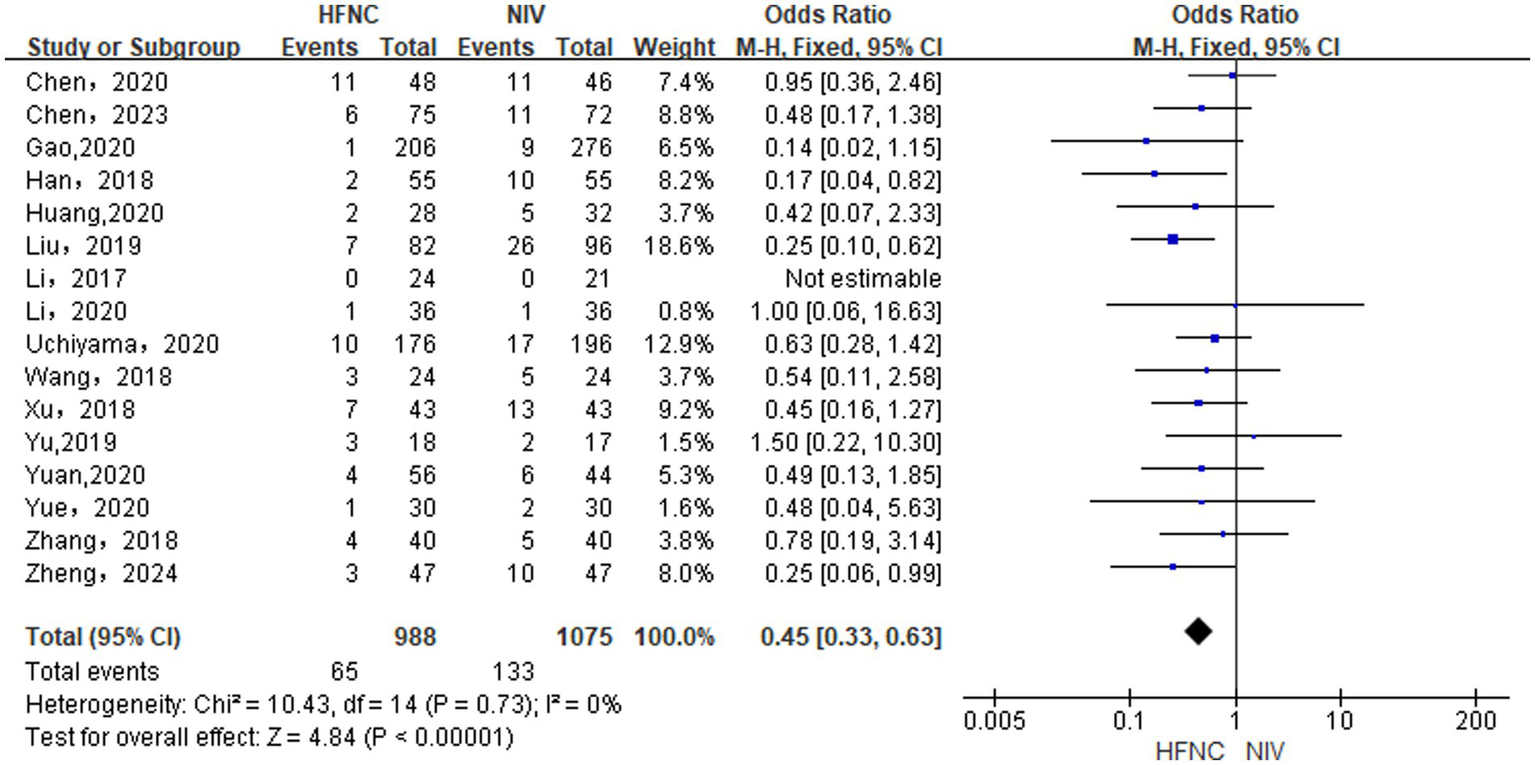
3.2 Results of literature quality evaluation
The quality of the 18 (13–30) RCTs included in our study was assessed using RevMan 5.3, showing high overall quality (Tables 2, 3). Meanwhile, the other 2 (31, 32) retrospective cohort studies were evaluated using the Newcastle-Ottawa Scale (NOS), both (13–32) of which revealed high quality and were suitable for Meta-analysis, as shown in Table 4.
Table 2
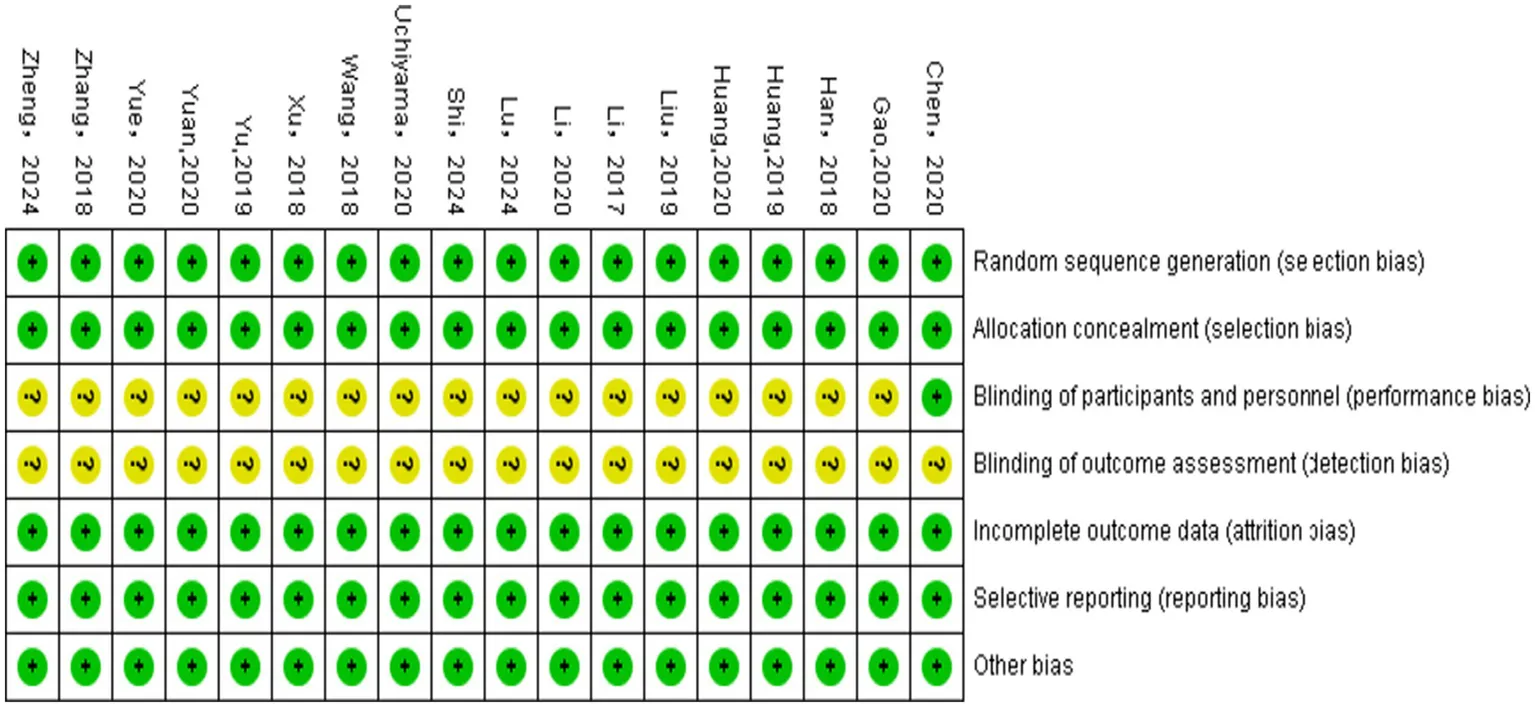
|
Evaluation on the methodological quality of the included studies.
Table 3
|
Percentage of risk of bias.
Table 4
| First author/year of publication | Selection of study populations | Comparability of groups | Outcome measures | Total score | Quality ratings |
|---|---|---|---|---|---|
| Koga et al. (31), 2020 | 3 | 2 | 2 | 7 | High quality |
| Chen et al. (32), 2023 | 3 | 2 | 2 | 7 | High quality |
Literature quality assessment.
The full score of the NOS is 9 points, with high-, moderate- and low-quality determined based on the score of ≥7, 5–6, and <5 points, respectively.
3.3 Outcomes of the meta-analysis
The comparative efficacy of HFNC versus NIV across the primary and secondary outcomes was rigorously evaluated. We now present the detailed meta-analytic results for each specific outcome measure.
3.3.1 Differences in PaO2 levels between groups
Inter-group comparison of the difference in PaO2 levels incorporated 10 RCTs (13, 14, 17–22, 28, 30) and 1 NRCT (32). With the use of a random-effects model (p < 0.00001, I2 = 95%), HFNC significantly improved PaO2 over NIV [MD = 2.95, 95% CI (2.23, 3.67), p < 0.00001], as shown in Figure 2.
Figure 2

Forest plot of meta-analysis comparing PaO2 between HFNC group and NIV group.
3.3.2 Differences in PaCO2 levels between groups
With the inclusion of 14 RCTs (13–15, 17–23, 26, 28–30) and 1 NRCT (32), a random-effects model (p < 0.00001, I2 = 95%) was used for analysis. Consequently, HFNC was superior to NIV in reducing PaCO2 [MD = −3.04, 95% CI (−3.56, −2.52), p < 0.00001], as shown in Figure 3.
Figure 3

Forest plot of meta-analysis comparing PaCO2 between HFNC group and NIV group.
3.3.3 Differences in OI levels between groups
A random-effects model (p = 0.01, I2 = 62%) was used for comparing differences in OI levels between groups based on the inclusion of 8 RCTs (13, 15, 21–24, 28, 29). HFNC was superior to NIV in improving OI levels [MD = 10.98, 95%CI (6.52, 15.45), p < 0.00001], Figure 4.
Figure 4

Forest plot of meta-analysis comparing OI between HFNC group and NIV group.
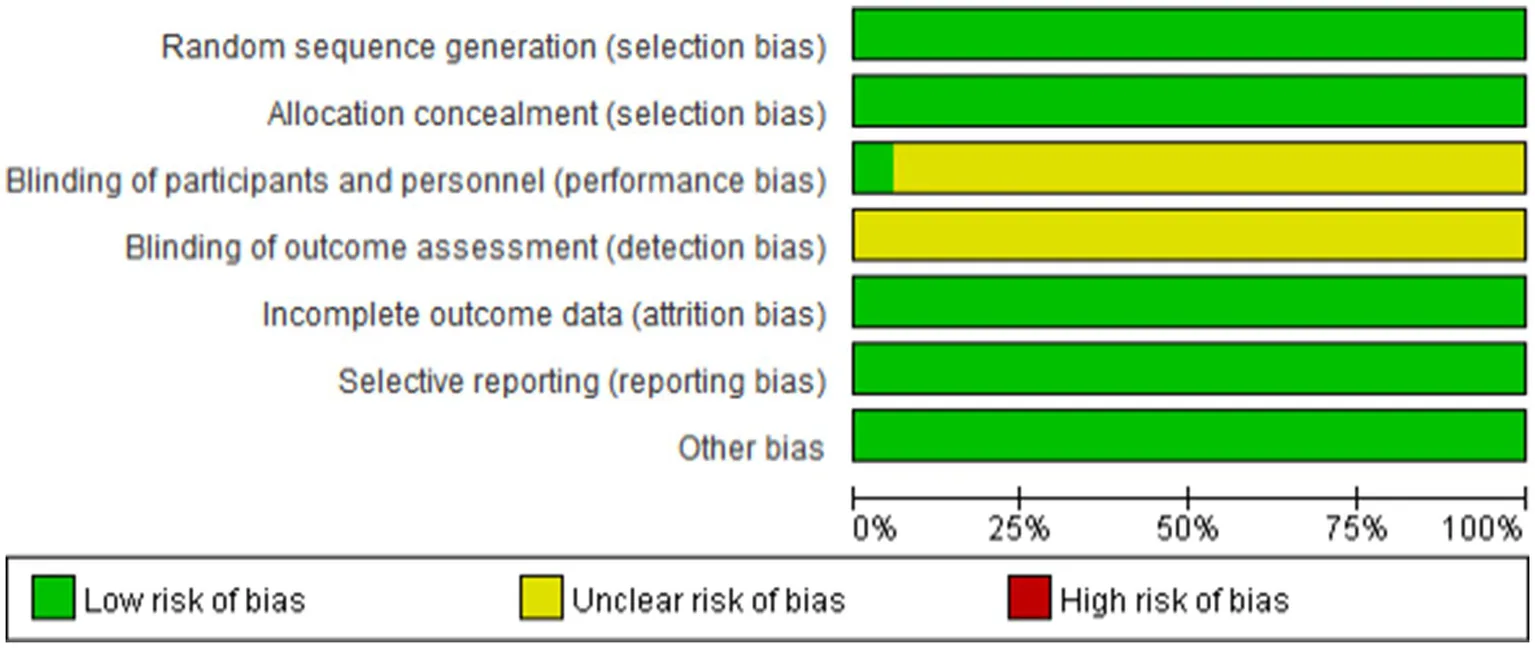
3.3.4 Difference in re-intubation rate between groups
Based on the inclusion of 15 RCTs (13–16, 18–27, 29) and 1 NRCT (32), analysis in a fixed-effects model (p = 0.73, I2 = 0%) showed that HFNC was superior to NIV in reducing re-intubation rate, [OR = 0.45, 95% CI (0.33, 0.63), p < 0.00001], as depicted in Figure 5.
Figure 5
Forest plot of meta-analysis comparing re-intubation rate between HFNC group and NIV group.
3.3.5 Differences in the pulmonary infection rate between groups
As revealed by the analysis in 2 RCTs (14, 24) using a fixed-effects model (p = 0.88, I2 = 0%), HFNC did not differ from NIV in reducing pulmonary infection rate [OR = 0.57, 95% CI (0.29, 1.11), p = 0.10], as shown in Figure 6.
Figure 6
![Forest plot comparing HFNC and NIV therapies for two studies. Odds ratio with 95% confidence intervals shows combined effect at 0.57 [0.29, 1.11], indicating no significant difference. Heterogeneity is zero, and the overall test effect indicates Z = 1.65 with P = 0.10.](https://www.frontiersin.org/files/Articles/1594145/xml-images/fmed-12-1594145-g006.webp)
Forest plot of meta-analysis comparing the pulmonary infection rate between HFNC group and NIV group.
3.3.6 Differences in duration of stay in the ICU between groups
With 13 RCTs (13–24, 27) included, analysis in a random-effects model (p < 0.00001, I2 = 98%) suggested that HFNC was superior to NIV in reducing length of stay in ICU (day) [MD = −6.15, 95% CI (−6.86, −5.44), p < 0.00001, Figure 7].
Figure 7
![Forest plot displaying mean differences between HFNC and NIV across various studies. Each study is listed with mean, standard deviation, total, and weight. The plot shows effect sizes as green squares, with confidence intervals as horizontal lines. The overall mean difference is −6.15, with a 95% confidence interval of [−6.86, −5.44]. Heterogeneity is indicated by Chi-squared 696.43, degrees of freedom 11, and I-squared 98%. The overall effect Z-score is 16.97 with a p-value < 0.00001.](https://www.frontiersin.org/files/Articles/1594145/xml-images/fmed-12-1594145-g007.webp)
Forest plot of meta-analysis comparing the length of stay in ICU between HFNC group and NIV group.
3.3.7 Differences in the mortality rate between groups
With the inclusion of 6 RCTs (17, 19, 23, 24, 27, 30) RCT and 2 NRCTs (31, 32), our analysis using a fixed-effects model (p = 0.88, I2 = 0%) observed that HFNC did not differ from NIV in reducing mortality [OR = 1.29, 95% CI (0.96, 1.72), p = 0.09, Figure 8].
Figure 8

Forest plot of meta-analysis comparing the mortality rate between HFNC group and NIV group.
3.3.8 Results of sensitivity analysis
Meta-analysis of PaO2, PaCO2, OI levels, and length of stay in ICU showed high heterogeneity, while the source remained unclear as sequential exclusion of studies did not significantly reduce heterogeneity. Sensitivity analyses using a random-effects model confirmed the robustness of the results.
3.3.9 Publication bias analysis
Funnel plots generated using RevMan indicated potential publication bias for PaO2 levels (Figure 9A) and length of stay in ICU time (Figure 9D), possible bias for PaCO2 levels (Figure 9B), and minimal bias for the re-intubation rate (Figure 9C). These findings highlighted the need for cautious interpretation and a more comprehensive literature search in future studies.
Figure 9

Funnel plots of outcome indicators (A–D).
4 Discussion
Respiratory failure is a serious clinical syndrome caused by various diseases, which may induce significant respiratory dysfunction, and serve as a major cause of ICU morbidity and mortality (33). Patients often require invasive mechanical ventilation initially (34), with NIV occupying an important position in post-extubation recovery (35). However, NIV can cause facial pressure ulcers and discomfort (36), and it may impair ciliary function and airway defense owing to its limited warming and humidifying capabilities, restricting its clinical application (37).
HFNC, as a novel oxygen delivery device, demonstrates multiple clinical advantages. It can generate positive end-expiratory pressure (PEEP) by delivering temperature- and humidity-regulated high-flow gas. This can promote alveolar recruitment and gas exchange, effectively improving hypoxemia, particularly effective in patients at risk of alveolar collapse, such as those with respiratory failure. The PEEP effect may benefit the maintenance of alveolar patency, mitigating ventilator-induced lung injury from atelectasis and thereby enhancing oxygenation. Additionally, through flushing the upper airway dead space, HFNC can facilitate the improvement of CO₂ clearance efficiency, holding significant importance for patients prone to CO2 retention, as it can reduce PaCO2 and alleviate respiratory acidosis. Concurrently, HFNC preserves mucociliary function, decreases airway resistance, and reduces respiratory effort. By diminishing the burden on respiratory muscles, it may enhance the function of breathing for patients with compromised respiratory function, alleviating dyspnea and respiratory muscle fatigue as well (38).
The nasal cannula interface can avoid skin contact, thus eliminating facial pressure injuries and discomfort associated with traditional masks. It can also preserve patients’ ability to eat, speak, and perform daily activities—a critical advantage for those requiring long-term oxygen therapy, such as COPD patients during stable rehabilitation. Maintaining normal nutrition and communication can enhance patients’ quality of life and treatment adherence, while significantly improving comfort and reducing complications such as skin breakdown and infection caused by fixed interfaces (39–41). In addition, its integrated gas warming and humidification system can further improve patient tolerance and comfort, especially for those in dry/cold environments or with sensitive airway mucosa (42). HFNC has thus emerged as a viable alternative to NIV for managing severe hypoxemia (43).
With the inclusion of 20 articles (13–32) (n = 3, 159), this study evaluated the effectiveness of HFNC (n = 1,447) and NIV (n = 1,712) in post-extubation respiratory failure. The primary outcomes included PaO2, PaCO2, OI, re-intubation rate, pulmonary infection rate, length of stay in ICU time, and mortality, with a purpose to offer stronger evidence for clinical decision-making.
Consequently, HFNC outperformed NIV in improving PaO2 and OI, reducing PaCO2 and re-intubation rate, as well as shortening the length of stay in ICU, without difference in pulmonary infection or mortality. Similarly, Yue (21) noted that HFNC could deliver high-concentration, humidified oxygen, enhancing oxygenation and maintaining stable PaCO2, while avoiding complications such as abdominal distension and aspiration occurred in NIV; and it could also reduce the requirement for re-intubation and shorten the length of stay in ICU. Lin et al. (44) also highlighted the ability of HFNC to improve respiratory mucosal function, promote alveolar opening, and stabilize oxygen levels.
Wang et al. (24) documented that HFNC could improve oxygenation, comfort, and reduce invasive ventilation use compared to NIV, with better tolerance and lower risks of complications such as ventilator-induced lung injury and pneumonia. However, HFNC has limitations, including inconsistent airway pressure and challenges in patients with poor expectoration, such as post-lung transplant recipients, who may require bronchoscopy for sputum drainage. HFNC is safe and effective only if expectoration improves. Therefore, non-invasive ventilatory support should be tailored to individual needs, and combination therapies may enhance the therapeutic outcome for respiratory failure.
Our results indicate high heterogeneity between HFNC and NIV in PaO2, PaCO2, OI, and length of stay in ICU. Sensitivity and meta-regression analyses identified no influencing factors. Possible reasons may include differences in baseline characteristics; variability in treatment plans; treatment tolerance; study design and sample size limitations; patient compliance and nursing intervention frequency; as well as treatment timing and duration.
This study has certain limitations. Firstly, it investigated the short-term efficacy, with an absence of long-term follow-up. Future multi-center and large-sample studies should be conducted to verify the clinical efficacy of HFNC in sequential mechanical ventilation and explore long-term outcomes such as quality of life and survival rates. Secondly, funnel plot asymmetry for PaO2, PaCO2, length of stay in ICU, and re-intubation rates may suggest potential publication bias, which may compromise result reliability and clinical decisions. Future studies should emphasize pre-registration and transparency to minimize bias.
5 Conclusion
In summary, HFNC demonstrates superior efficacy over NIV across diverse patient populations and clinical conditions. HFNC can significantly improve key respiratory parameters—including PaO2, OI, and PaCO2 reduction—while also lowering re-intubation rates and shortening length of stay in ICU. Collectively, findings in the present study support the clinical adoption of HFNC as a valuable respiratory support alternative.
Statements
Author contributions
MaM: Writing – original draft. TY: Data curation, Writing – review & editing. MuM: Writing – review & editing. MeM: Data curation, Writing – review & editing. AA: Methodology, Writing – original draft. ZC: Writing – review & editing. YN: Data curation, Writing – review & editing. MN: Supervision, Writing – original draft.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by the Project: Intramural Project of Xinjiang Uygur Autonomous Region People’s Hospital (20220129).
Acknowledgments
We thank all authors for contributions to all aspects of the work.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Correction note
A correction has been made to this article. Details can be found at: 10.3389/fmed.2025.1712847.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
HFNC, high-flow nasal cannula oxygen therapy; NIV, non-invasive ventilation; RCT, randomized controlled study; MD, mean difference; OR, odds ratio.
References
1.
Miskovic A Lumb AB . Postoperative pulmonary complications. Br J Anaesth. (2017) 118:317–34. doi: 10.1093/bja/aex002
2.
Girardis M Busani S Damiani E Donati A Rinaldi L Marudi A et al . Effect of conservative vs conventional oxygen therapy on mortality among patients in an intensive care unit: the oxygen-ICU randomized clinical trial. JAMA. (2016) 316:1583–9. doi: 10.1001/jama.2016.11993
3.
Ding H Karunanithi M Kanagasingam Y Vignarajan J Moodley Y . A pilot study of a mobile-phone-based home monitoring system to assist in remote interventions in cases of acute exacerbation of COPD. J Telemed Telecare. (2014) 20:128–34. doi: 10.1177/1357633X14527715
4.
Frat JP Thille AW Mercat A Girault C Ragot S Perbet S et al . High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N Engl J Med. (2015) 372:2185–96. doi: 10.1056/NEJMoa1503326
5.
Abdel-Latif ME Tan O Fiander M Osborn DA . Non-invasive high-frequency ventilation in newborn infants with respiratory distress. Cochrane Database Syst Rev. (2024) 5:Cd012712. doi: 10.1002/14651858.CD012712.pub2
6.
Ricard JD Roca O Lemiale V Corley A Braunlich J Jones P et al . Use of nasal high flow oxygen during acute respiratory failure. Intensive Care Med. (2020) 46:2238–47. doi: 10.1007/s00134-020-06228-7
7.
Papazian L Corley A Hess D Fraser JF Frat JP Guitton C et al . Use of high-flow nasal cannula oxygenation in ICU adults: a narrative review. Intensive Care Med. (2016) 42:1336–49. doi: 10.1007/s00134-016-4277-8
8.
Patel BK Wolfe KS Pohlman AS Hall JB Kress JP . Effect of noninvasive ventilation delivered by helmet vs face mask on the rate of endotracheal intubation in patients with acute respiratory distress syndrome: a randomized clinical trial. JAMA. (2016) 315:2435–41. doi: 10.1001/jama.2016.6338
9.
Feng Z Zhang L Yu H Su X Shuai T Zhu L et al . High-flow nasal cannula oxygen therapy versus non-invasive ventilation for AECOPD patients after extubation: a systematic review and meta-analysis of randomized controlled trials. Int J Chron Obstruct Pulmon Dis. (2022) 17:1987–99. doi: 10.2147/COPD.S375107
10.
Ovtcharenko N Ho E Alhazzani W Cortegiani A Ergan B Scala R et al . High-flow nasal cannula versus non-invasive ventilation for acute hypercapnic respiratory failure in adults: a systematic review and meta-analysis of randomized trials. Crit Care. (2022) 26:348. doi: 10.1186/s13054-022-04218-3
11.
Higgins JP Higgins JPT Altman DG Gotzsche PC Juni P Moher D et al . The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ. (2011) 343:d5928. doi: 10.1136/bmj.d5928
12.
Higgins JP Thompson SG Deeks JJ Altman DG . Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
13.
Li Y-c . Analysis of the application value of high –flow humidified oxygen therapy through the nose in COPD patients with type 2 respiratory failure after tracheal intubation and extubation. Syst Med. (2020) 5:35–7. doi: 10.19368/j.cnki.2096-1782.2020.18.035
14.
Gao Z Fan D Yang K . Observation of the therapeutic effect of HFNC on post-cardiovascular surgery hypoxemia in cardiac surgery patients. Chin J Integr Med. (2020) 18:3079–82. doi: 10.12102/j.issn.1672-1349.2020.18.037
15.
Huang J Liang Z Huang L . Effect of sequential treatment of HFNC and NIPPV in patients with AECOPD after extubation. Chin Evid Nurs. (2020) 6:565–9. doi: 10.12102/j.issn.2095-8668.2020.06.015
16.
Yuan CC . Clinical effects of alternating application of high–flow nasal oxygen therapy and non–invasive ventilation in patients with lung transplants after removal of artificial airways. Med Equip. (2020) 33:177–9.
17.
Huang J Cai J Cai Y Tu Q Liang J Lin Z . Application effect of nasal high-flow oxygen therapy in patients with acute respiratory failure after extubation. China Mod Med. (2019) 26:42–8.
18.
Yu J Zheng R Zhu J Lin H Chen Q Shao J . Clinical efficacy of sequential therapy from invasive ventilator to high–flow nasal cannula oxygen therapy of patients with acute exacerbations of chronic obstructive pulmonary disease. Chin J Crit Care. (2019) 5:213–8. doi: 10.3877/cma.j.issn.2096-1537.2019.03.002
19.
Han X Liu S Liu Y Xu M . The effect of nasal high–flow oxygen therapy on weaning outcomes in patients with AECOPD. J Hunan Norm Univ. (2018) 15:145–8.
20.
Xu X Wang J Yao H . Effect of humidified high flow nasal cannula on reintubation and respiratory failure after extubation in COPD patients. J Qilu Nurs. (2018) 24:1–3. doi: 10.3969/j.issn.1006-7256.2018.05.001
21.
Ai Jun Y . The effectiveness and safety of nasal high–flow oxygen therapy sequential treatment in mechanically ventilated patients with chronic obstructive pulmonary disease. Med Equip. (2020) 33:3–4.
22.
Zhang C . Study on the curative effect of three kinds of oxygen therapy for AECOPD patients after extubation. Qingdao: Qingdao University (2018).
23.
Li Z Li C Dong Q Ma J Wang L Li Y et al . Comparison between nasal high flow oxygen therapy and non–invasive Ventilation Care for Post-extubation hypoxemia after abdominal surgery in ICU. J Kunming Med Univ. (2017) 38:65–9.
24.
Wang D Nie X Pan H Xu H Chen J . A clinical study on humidified high flow nasal cannula therapy for patients with primary graft dysfunction after lung transplantation. Prog Mod Biomed. (2017) 17:6709–12. doi: 10.13241/j.cnki.pmb.2017.34.023
25.
Chen J Lin Y Du L Kang M Chi X Wang Z et al . The comparison of HHHFNC and NCPAP in extremely low–birth–weight preterm infants after extubation: a single–center randomized controlled trial. Front Pediatr. (2020) 8:250. doi: 10.3389/fped.2020.00250
26.
Uchiyama A Okazaki K Kondo M Oka S Motojima Y Namba F et al . Randomized controlled trial of high–flow nasal cannula in preterm infants after extubation. Pediatrics. (2020) 146:e20201101. doi: 10.1542/peds.2020-1101
27.
Liu F Shao Q Jiang R Zeng Z Liu Y Li Y et al . High–flow oxygen therapy to speed weaning from mechanical ventilation: a prospective randomized study. Am J Crit Care. (2019) 28:370–6. doi: 10.4037/ajcc2019130
28.
Shi SS Qiu LL . The effect of invasive ventilation sequential non-invasive high-flow nasal cannula oxygen therapy on AECOPD combined with type II respiratory failure. Med Equip. (2024) 37:140–3. doi: 10.3969/j.issn.1002-2376.2024.05.041
29.
Zheng QQ Wang LH . The application effect of non–invasive mechanical ventilation and high–flow nasal cannula oxygen therapy in the sequential treatment of patients with acute respiratory failure after weaning. Med Equip. (2024) 37:91–3. doi: 10.3969/j.issn.1002-2376.2024.03.028
30.
Lu S Wei S Sun R . Effect of high flow nasal cannula and non–invasive ventilation in the treatment of acute exacerbation of chronic obstructive pulmonary disease complicated with type II respiratory failure. Chin Med Innov. (2024) 21:24–7. doi: 10.3969/j.issn.1674-4985.2024.05.006
31.
Koga Y Kaneda K Fujii N Tanaka R Miyauchi T Fujita M et al . Comparison of high–flow nasal cannula oxygen therapy and non–invasive ventilation as first–line therapy in respiratory failure: a multicenter retrospective study. Acute Med Surg. (2020) 7:e461. doi: 10.1002/ams2.461
32.
Chen X Tan C Jiang H . High–flow nasal cannula oxygen therapy is superior to conventional oxygen therapy in intensive care unit patients after extubation. Am J Transl Res. (2023) 15:1239–46.
33.
Lamba TS Sharara RS Singh AC Balaan M . Pathophysiology and classification of respiratory failure. Crit Care Nurs Q. (2016) 39:85–93. doi: 10.1097/CNQ.0000000000000102
34.
Guilhermino MC Inder KJ Sundin D . Education on invasive mechanical ventilation involving intensive care nurses: a systematic review. Nurs Crit Care. (2018) 23:245–55. doi: 10.1111/nicc.12346
35.
Ketan PS Kumar R Ish P Chakrabarti S Gupta NK Gupta N . Post-extubation high-flow nasal cannula oxygen therapy versus non-invasive ventilation in chronic obstructive pulmonary disease with hypercapnic respiratory failure. Monaldi Arch Chest Dis. (2023) 94:88. doi: 10.4081/monaldi.2023.2576
36.
Yang H Huang D Luo J Liang Z Li J . The use of high-flow nasal cannula in patients with chronic obstructive pulmonary disease under exacerbation and stable phases: a systematic review and meta-analysis. Heart Lung. (2023) 60:116–26. doi: 10.1016/j.hrtlng.2023.02.016
37.
Hernández G Roca O Colinas L . High-flow nasal cannula support therapy: new insights and improving performance. Crit Care. (2017) 21:62. doi: 10.1186/s13054-017-1640-2
38.
Nagata K Horie T Chohnabayashi N Jinta T Tsugitomi R Shiraki A et al . Home high-flow nasal cannula oxygen therapy for stable hypercapnic COPD: a randomized clinical trial. Am J Respir Crit Care Med. (2022) 206:1326–35. doi: 10.1164/rccm.202201-0199OC
39.
Lee CC Mankodi D Shaharyar S Ravindranathan S Danckers M Herscovici P et al . High flow nasal cannula versus conventional oxygen therapy and non-invasive ventilation in adults with acute hypoxemic respiratory failure: a systematic review. Respir Med. (2016) 121:100–8. doi: 10.1016/j.rmed.2016.11.004
40.
Wang SY Liang H-W Lu G-S Jiang Z-J Zhang B-Z Deng Q-X et al . Effect of sequential high-flow nasal cannula oxygen therapy and non-invasive positive-pressure ventilation in patients with difficult weaning from mechanical ventilation after extubation on respiratory mechanics. Ann Transl Med. (2021) 9:1251. doi: 10.21037/atm-21-3408
41.
Schwabbauer N Berg B Blumenstock G Haap M Hetzel J Riessen R . Nasal high-flow oxygen therapy in patients with hypoxic respiratory failure: effect on functional and subjective respiratory parameters compared to conventional oxygen therapy and non-invasive ventilation (NIV). BMC Anesthesiol. (2014) 14:66. doi: 10.1186/1471-2253-14-66
42.
Tan D Walline JH Ling B Xu Y Sun J Wang B et al . High-flow nasal cannula oxygen therapy versus non-invasive ventilation for chronic obstructive pulmonary disease patients after extubation: a multicenter, randomized controlled trial. Crit Care. (2020) 24:489. doi: 10.1186/s13054-020-03214-9
43.
Nishimura M . High-flow nasal cannula oxygen therapy in adults: physiological benefits, indication, clinical benefits, and adverse effects. Respir Care. (2016) 61:529–41. doi: 10.4187/respcare.04577
44.
Lin H Fu H Zhao Z Guo A Sun T . Effect of sequential nasal high flow oxygen therapy after extubation in patients with chronic obstructive pulmonary disease. Lab Med Clin. (2019) 16:1646–9. doi: 10.3969/j.issn.1672-9455.2019.12.005
Summary
Keywords
HFNC, NIV, invasive mechanical ventilation, meta-analysis, respiratory failure
Citation
Maimaitiniyazi M, Yisimitila T, Maimaitiniyazi M, Maisuti M, Aihaiti A, Chenfei Z, Nijiati Y and Nijiati M (2025) Meta-analysis of high-flow nasal cannula oxygen therapy versus non-invasive ventilation after invasive mechanical ventilation. Front. Med. 12:1594145. doi: 10.3389/fmed.2025.1594145
Received
15 March 2025
Accepted
26 August 2025
Published
25 September 2025
Corrected
15 October 2025
Volume
12 - 2025
Edited by
Cátia Caneiras, University of Lisbon, Portugal
Reviewed by
Aslıhan Gürün Kaya, Ankara University, Türkiye
Yang Wu, University of Nebraska Medical Center, United States
Updates
Copyright
© 2025 Maimaitiniyazi, Yisimitila, Maimaitiniyazi, Maisuti, Aihaiti, Chenfei, Nijiati and Nijiati.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Muyesai Nijiati, muyassar11@aliyun.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.