Abstract
Background:
Current teaching models for clinical hematology laboratory interns often prioritize theoretical knowledge dissemination over the practical application of skills directly tied to analyzing and interpreting laboratory results. This approach potentially limits the development of critical clinical reasoning and problem-solving abilities within the framework of quality management systems like ISO 15189. To address these challenges, this study implemented and evaluated a novel laboratory-result-oriented modular teaching model, explicitly integrating ISO 15189 principles. The study assessed the design, implementation, effectiveness, advantages, and challenges of this model compared to traditional methods.
Methods:
A total of 60 medical laboratory interns were recruited. Thirty interns completed their internship from October 2022 to March 2023 (control group), following the traditional model involving theoretical lectures supplemented by limited laboratory demonstrations. The remaining 30 interns undertook their internship from October 2023 to March 2024 (experimental group), receiving the laboratory-result-oriented modular teaching. Teaching effectiveness was compared through theoretical examinations, operational skill assessments, and satisfaction surveys.
Results:
The experimental group scored significantly higher than the control group in both theoretical examinations and operational skill assessments (p < 0.05). Their overall teaching satisfaction was also significantly higher (p < 0.05).
Conclusion:
The laboratory-result-oriented modular teaching model improved teaching effectiveness and fostered greater learning initiative among interns. It enhanced interns’ ability to analyze and solve problems independently and developed clinical reasoning skills.
Introduction
Clinical laboratory medicine is a highly practical and interdisciplinary field (1–3), requiring rigorous quality management systems (QMS) to ensure reliable diagnostic results (4). ISO 15189:2012 (Medical Laboratories—Requirements for Quality and Competence, hereafter ISO 15189) represents the international standard for accrediting medical laboratory QMS (5–7). This standard emphasizes personnel competence as paramount for laboratory quality. Consequently, training programs for interns should evolve beyond traditional models focused solely on technical skills by explicitly integrating ISO 15189 core principles. This integration aims to cultivate professionals possessing not only technical proficiency and research potential but also robust quality management awareness.
Clinical hematology testing is pivotal for diagnosis and patient management (8–13). The accuracy and interpretation of blood test results directly impact clinical decisions (14, 15). However, conventional teaching models, often instructor-centered with passive knowledge delivery and summative assessment (16), frequently fail to adequately develop the analytical, interpretative, and quality management skills required within accredited laboratories, particularly under the ISO 15189 framework.
To address this gap, we propose, implement, and evaluate a novel “Laboratory-Result-Oriented Modular Teaching Model based on ISO 15189 principles” for clinical hematology interns. This model utilizes actual laboratory test results (e.g., complete blood counts [CBCs], coagulation profiles) as the anchor for learning, stimulating inquiry into their generation, reliability, and clinical meaning. The curriculum is structured into discrete, focused modules, each dedicated to a specific result-related aspect such as pre-analytical variables (17–19), analytical methods (including instrument operation and quality control aligned with ISO 15189), quality control, result interpretation, or clinical case integration. Crucially, the model systematically embeds core ISO 15189 requirements—including personnel roles, procedural documentation, quality control processes, equipment management, and the principles of continuous improvement and patient safety—throughout these modules.
By integrating internship management within the ISO 15189 QMS framework using this result-oriented modular approach, students directly engage with standardized practices. This framework aims to link theory and practice directly to result reliability, preparing interns for regulated practice and enhancing future result accuracy (20, 21). The pedagogical strategy leverages test results to drive inquiry within defined, ISO 15189-compliant modules, aiming to improve clinical reasoning, problem-solving, and intrinsic quality awareness. To empirically evaluate this model’s effectiveness and feasibility compared to traditional teaching, a controlled study was conducted with two intern cohorts.
Study subjects and methodology
Study participants
A total of 60 medical laboratory interns from a tertiary Grade-A hospital in Nanjing were recruited. Thirty interns completing their internship from October 2022 to March 2023 were assigned to the control group, and 30 interns undertaking their internship from October 2023 to March 2024 comprised the experimental group. Inclusion criteria required enrollment as interns within the medical laboratory department. Exclusion criteria were: (a) internship interruption, and (b) absence from one or more teaching sessions. To mitigate potential confounding effects from non-synchronized internship periods (2022–2023 vs. 2023–2024), we confirmed: (a) an identical instructional team composition and laboratory equipment; (b) unchanged ISO 15189 operational protocols; (c) no institutional reforms affecting training structure; and (d) no significant inter-group differences in pre-internship scores (Table 1, p > 0.05). (e) All instructors were certified Medical Laboratory Quality and Capability Accreditation Criteria Project Training (Certification No.: NJGLJYK-21-06-037). All participants provided written informed consent after being fully informed of the study’s objectives and methods. Ethical approval was obtained from the Ethics Committee of Nanjing Drum Tower Hospital (Approval No: 2022–238-02).
Table 1
| Item | Control group (n = 30) | Experimental group (n = 30) | p |
|---|---|---|---|
| Gender | 1.0 | ||
| Male | 15 (50%) | 15 (50%) | |
| Female | 15 (50%) | 15 (50%) | |
| Education level | 1.0 | ||
| Bachelor’s degree | 15 (50%) | 15 (50%) | |
| Associate’s degree | 15 (50%) | 15 (50%) | |
| Initial assessment at enrollment | 66.63 ± ±9.004 | 66.63 ± 9.042 | 0.275 |
| Preliminary assessment of basic knowledge (40%) | 32.57 ± 4.049 | 32.37 ± 4.760 | 0.861 |
| Preliminary assessment of practical skills (40%) | 24.13 ± 7.143 | 26.70 ± 7.212 | 0.171 |
| Preliminary assessment of report interpretation (20%) | 9.93 ± 2.815 | 10.13 ± 3.256 | 0.800 |
Demographic information.
Teaching strategy
Control group: traditional practical teaching model
The control group received traditional practical teaching. Instructors adhered strictly to the established curriculum, providing structured guidance. The model primarily combined theoretical instruction with laboratory demonstrations. Theoretical knowledge encompassing hematology testing principles, methods, and precautions was first delivered in the classroom, followed by standardized experimental demonstrations. Students then replicated procedures based on demonstrated steps under instructor supervision, with immediate correction of technical errors. Assessment focused primarily on the accuracy of experimental operations and theoretical knowledge grasp, with limited emphasis on clinical reasoning and laboratory result interpretation.
Experimental group: laboratory result-oriented modular teaching model
The experimental group’s curriculum integrated ISO 15189 principles. Training content was designed according to ISO 15189 requirements, departmental procedural documents, and the quality manual, incorporating key accreditation elements throughout. Implementation involved the following steps: (1) Preliminary preparation: A modular teaching team was established, comprising one team leader, one teaching secretary, and four instructors with >5 years of laboratory experience. The teaching secretary drafted the teaching plan, instructors implemented teaching activities and supervised plan execution, and the team leader oversaw plan design and process management. (2) Instructor training: Prior to teaching commencement, team members received training covering modular teaching concepts, instructional methods, and relevant content. (3) Teaching design: (i) Introduction: Three days before each weekly session, team members created training materials and introduced related cases aligned with teaching objectives to prepare students. (ii) Teaching objectives: Instructors prepared clinical cases, ISO 15189-related knowledge points, and teaching aids, clarifying expected knowledge and skill mastery. (iii) Pre-test: Instructors designed 2–3 content-related questions distributed with training materials 2 days in advance to assess preparation, identify weaknesses, and adjust teaching. (iv) Participatory learning: Methods such as simulations, case presentations, and skills workshops encouraged active participation. For instance, instrument training included ISO 15189-compliant calibration, maintenance, operation steps, and precautions, followed by supervised intern practice. Clinical case analysis followed ISO 15189 quality management processes to develop diagnostic reasoning skills. Interactive training enhanced conceptual understanding and engagement. (4) Post-test: One analytical question was provided post-session for interns to analyze and answer within a set timeframe, assessing comprehension and reinforcing learning. (5) Summary: Interns presented case reports using PowerPoint, reviewed and interpreted according to ISO 15189 standards. Instructor feedback addressed issues, further developing case analysis, clinical reasoning, and presentation skills (Figure 1).
Figure 1
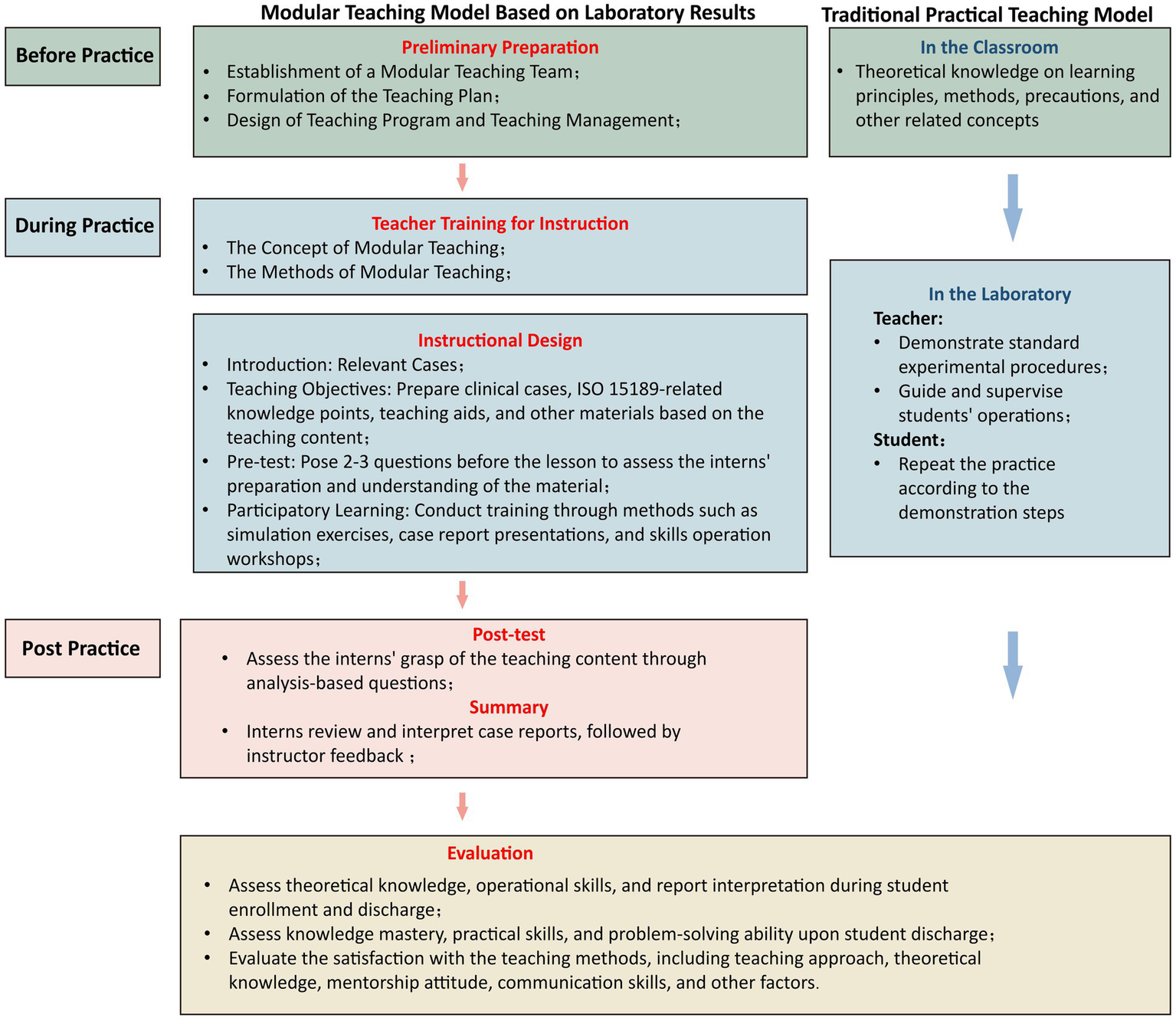
Schematic diagram of different teaching models for the experimental and control groups.
Evaluation criteria
Assessment was employed to evaluate teaching quality, guiding intern learning abilities, strategies, and overall instruction quality. Aligned with clinical hematology characteristics, assessment criteria were developed based on prior research: (i) Intern performance Evaluation: Upon entry, instructors assessed baseline performance and learning outcomes (100-point scale) covering knowledge acquisition, practical skills, and problem-solving abilities, enabling inter-group comparisons. (ii) Examination comparison: Performance in professional knowledge (100 points), operational skills (100 points), and clinical reasoning (100 points) was compared between groups. The clinical reasoning assessment evaluated case information retrieval, specialized knowledge, disease information integration, diagnostic/differential diagnostic skills, and medical logical thinking. (iii) Satisfaction survey: Both groups completed anonymous surveys rating satisfaction (100-point scale per item) with teaching methods, theoretical depth, instructor attitude, and communication skills. The overall satisfaction rate was calculated as a percentage (Figure 2).
Figure 2
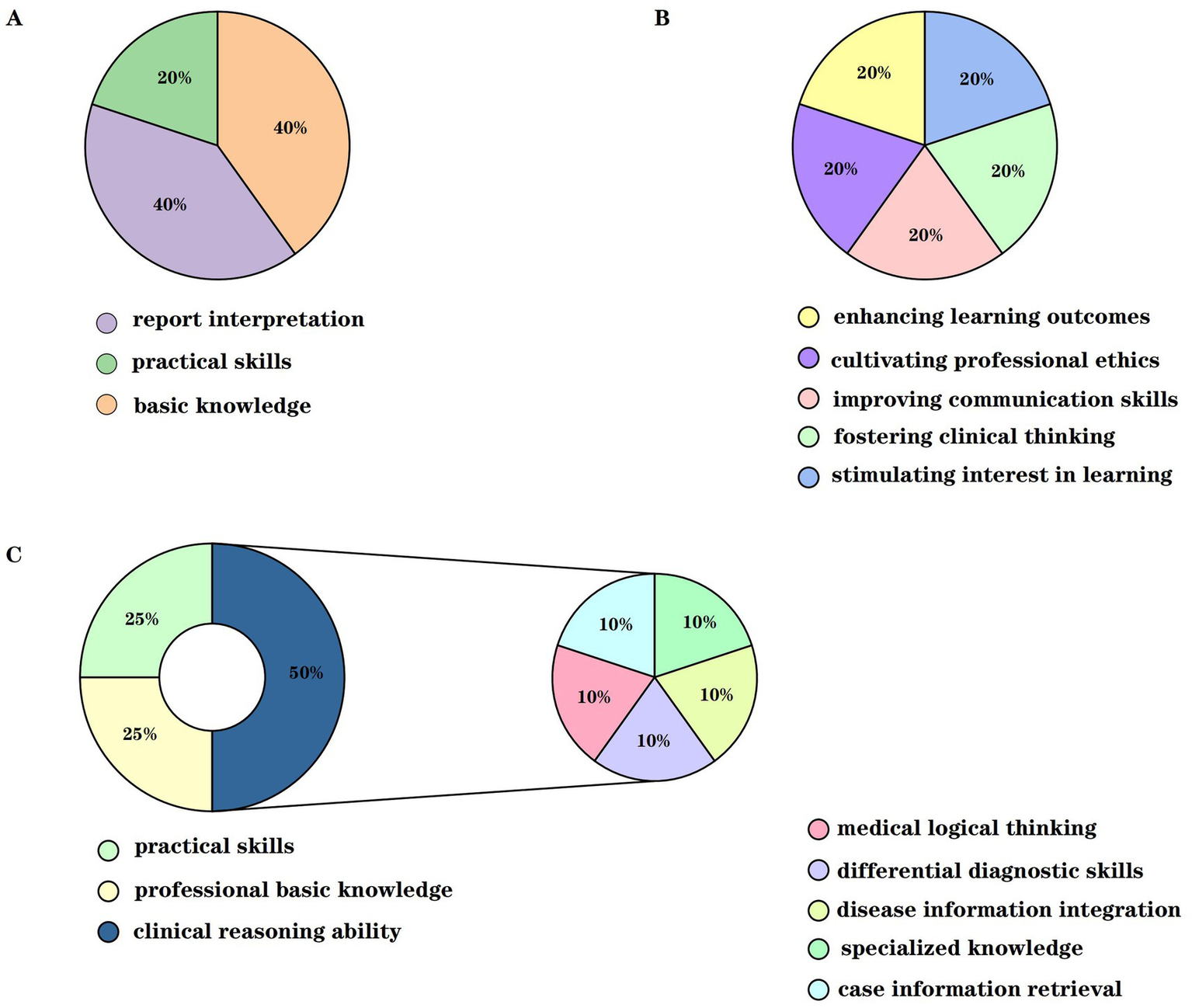
Schematic diagram of evaluation indicators for the experimental and control groups. (A) Represents the comprehensive evaluation scores prior to enrollment, which include the preliminary assessments of basic knowledge, practical skills, and report interpretation. (B) Represents the post-teaching evaluation of teaching effectiveness, which consists of five components: stimulating interest in learning, fostering clinical thinking, improving communication skills, cultivating professional ethics, and enhancing learning outcomes. (C) Represents the post-teaching assessment indicators for the experimental and control groups in three areas: professional basic knowledge, practical skills, and clinical reasoning ability.
Statistical methods and data processing
Statistical analyses were performed using SPSS version 25.0. Normally distributed data are presented as mean ± standard deviation. Inter-group comparisons utilized independent-sample t-tests. A significance level of p < 0.05 was applied.
Results
Demographic information
All 60 interns (30 experimental group, 30 control group) completed the study. Demographic characteristics and pre-enrollment comprehensive evaluation scores showed no significant differences between groups (p > 0.05), confirming comparability (Table 1).
Comparison of test results between the two groups of clinical laboratory interns after teaching
This study compared and analyzed the assessment results of clinical laboratory interns in the experimental and control groups across three dimensions: professional foundational knowledge, practical skills, and clinical reasoning ability. The results revealed that the teaching effectiveness was significantly superior in the experimental group compared to the control group. The evaluation scores across all dimensions were markedly higher in the experimental group, and these differences were statistically significant (p < 0.05) (see Table 2).
Table 2
| Item | Control group (n = 30) | Experimental group (n = 30) | p |
|---|---|---|---|
| Professional basic knowledge test | 87.00 ± 4.624 | 90.17 ± 4.356 | 0.008 |
| Practical skills test | 88.20 ± 4.604 | 92.87 ± 4.075 | <0.001 |
| Clinical thinking ability test | 64.43 ± 5.008 | 86.47 ± 4.191 | <0.001 |
| Case information retrieval ability | 13.43 ± 2.161 | 19.03 ± 0.999 | <0.001 |
| Specialized knowledge mastery ability | 13.17 ± 2.086 | 17.13 ± 2.047 | <0.001 |
| Disease information integration ability | 12.47 ± 1.756 | 16.23 ± 1.960 | <0.001 |
| Diagnostic and differential diagnosis ability | 12.70 ± 1.915 | 16.90 ± 1.900 | <0.001 |
| Medical logical thinking ability | 12.67 ± 1.845 | 17.17 ± 1.967 | <0.001 |
Comparison of comprehensive skills scores after teaching.
Based on the data in Table 2, a detailed comparative analysis of the clinical reasoning ability indicators was conducted. The results demonstrated that the experimental group scored significantly higher on all clinical reasoning ability evaluation criteria than the control group (p < 0.05), indicating comprehensive enhancement in the core elements of clinical reasoning. Specifically, the experimental group exhibited notably stronger case information integration skills, suggesting that these interns could rapidly identify key information and conduct more effective analyses when confronted with clinical problems. Furthermore, the experimental group demonstrated an advantage in medical logical thinking, enabling them to make sound judgments based on clinical data and knowledge. The experimental group also outperformed the control group in key indicators such as diagnostic and differential diagnostic abilities, as well as mastery of professional knowledge. Overall, the significantly higher clinical reasoning ability scores of the experimental group confirmed that the laboratory result-oriented modular teaching model had a substantial positive impact on the clinical reasoning abilities of medical laboratory students.
Comparison of teaching satisfaction between the two groups of interns
To comprehensively evaluate teaching satisfaction, the performance of the two intern groups was compared across five key dimensions: stimulating learning interest, fostering clinical thinking, improving communication skills, cultivating professional ethics, and enhancing learning outcomes (see Table 3). The results indicated that the experimental group expressed significantly higher satisfaction than the control group across all five dimensions (p < 0.05).
Table 3
| Item | Control group (n = 30) | Experimental group (n = 30) | p |
|---|---|---|---|
| Stimulate interest in learning | 13.10 ± 2.354 | 16.47 ± 2.315 | <0.001 |
| Fostering clinical thinking | 11.87 ± 1.592 | 17.27 ± 1.837 | <0.001 |
| Improving communication skills | 13.03 ± 1.752 | 17.43 ± 1.794 | <0.001 |
| Cultivating professional ethics | 14.23 ± 1.977 | 16.43 ± 2.542 | <0.001 |
| Enhancing learning outcomes | 13.33 ± 2.264 | 16.60 ± 2.527 | <0.001 |
| Total score | 65.57 ± 4.500 | 84.20 ± 5.242 | <0.001 |
Evaluation of the effect of teaching after the teaching session.
Regarding stimulating learning interest, interns in the experimental group generally found the teaching model novel and engaging, which significantly increased their learning motivation and intellectual curiosity. In terms of fostering clinical thinking, the experimental group reported a marked improvement in their clinical reasoning ability, which they attributed to the teaching approach integrating case analysis with practical exercises. Moreover, interns in the experimental group demonstrated greater initiative and efficiency when communicating with patients, instructors, and peers, indicating an improvement in their communication skills. In cultivating professional ethics, the experimental group exhibited a deeper understanding and better application of medical ethics principles. Finally, concerning the enhancement of learning outcomes, the experimental group surpassed the control group in both academic performance and clinical skills, reflecting the significant efficacy of the experimental teaching model.
Discussion
Experimental medicine demands strong practical applicability and high professional standards, necessitating training approaches that effectively integrate theoretical knowledge with clinical practice. Contemporary laboratory education requires multidisciplinary professionals capable of interpreting complex diagnostic data, participating in clinical decision-making, and providing evidence-based recommendations (22–24). To address this need, we revised the internship syllabus by embedding ISO 15189 quality management principles throughout the curriculum. Routine work in the laboratory is closely linked to laboratory equipment and quality control; however, traditional syllabi often emphasize scheduling and foundational knowledge while underemphasizing critical operational competencies such as equipment troubleshooting, quality control implementation, and diagnostic interpretation (25). Therefore, these aspects were also incorporated into the training plan for interns, aiming to better prepare interns to become qualified and modern laboratory management professionals.
During implementation, theoretical and practical training were delivered concurrently through a laboratory result-oriented modular framework. This approach aligns with innovative pedagogical models documented in recent literature, such as virtual-physical hybrid courses in microbiology education (26) and outcome-based teaching in clinical laboratories (27). Our study demonstrated that interns trained under this ISO 15189-integrated modular model scored significantly higher in hematology theory assessments (p < 0.05) than those in traditional training. This improvement reflects the model’s capacity to contextualize theoretical knowledge through authentic laboratory outcomes—enhancing comprehension and retention. The experimental group also demonstrated superior practical competencies, including: (1) increased technical proficiency in procedures such as coagulation testing with improved error recognition; (2) enhanced analytical efficiency; and (3) strengthened diagnostic interpretation through multidimensional integration of hematologic parameters with clinical presentation.
In terms of practical skills, the experimental group interns performed better in aspects such as the accuracy of instrument operation, the accuracy and efficiency of test results, and overall performance. For example, in the operation of coagulation function testing, the experimental group interns were able to operate the instruments more proficiently and provide more reasonable explanations and preliminary judgments for abnormal test results. In terms of result analysis, the experimental group interns demonstrated stronger capabilities in the comprehensive analysis of blood test results. They were able to propose more reasonable diagnostic suggestions by integrating results from multiple blood tests with the patient’s clinical symptoms.
This improvement is attributed to the systematic study of various blood testing modules and result-oriented thinking training within the modular teaching model. Specifically, throughout the overall teaching process, the instructors employed a combination of observation and explanation to integrate ISO 15189’s competency requirements for laboratory personnel into the curriculum. Three key strategies significantly enhanced the students’ learning outcomes: First, students were encouraged to explore clinical knowledge and diseases autonomously, selecting the most appropriate methods to obtain clinical data and learn about disease diagnosis and treatment. This self-directed learning process not only improved the students’ clinical reasoning abilities but also helped them master the medical laboratory knowledge system more comprehensively. Second, the teaching content and practical training were divided into specific modules, and repeated practice in short time intervals reinforced the students’ learning, enabling them to internalize detailed operational knowledge and understand the theoretical basis behind the procedures, thus making their learning more systematic. Each module was supported by specialized instructors to ensure consistency and quality in the content, reducing the students’ learning pressure and enhancing their ability to learn independently. Lastly, this teaching model centered on laboratory test results. Under the guidance of instructors, interns were able to combine theoretical knowledge with real clinical cases. This integrated approach established an iterative learning process where theoretical knowledge informed practical application, subsequently deepening conceptual understanding - particularly regarding quality management systems essential for diagnostic reliability.
However, this study also has some limitations. It was conducted at a single tertiary hospital in Nanjing, and the sample size was relatively small, which may introduce regional biases. Future studies could expand the sample size and validate the model across different regions and hospitals of varying levels to further refine this teaching model. During the teaching process, although the model was based on laboratory results, some rare cases might not have been sufficiently covered in the curriculum. Future iterations of the teaching model could incorporate more rare case studies to broaden the interns’ perspectives. A paramount limitation is that the absence of longitudinal data prevents assessment of competency retention in professional practice, while the model shows significant promise in developing foundational competencies within the training period, longitudinal studies are needed to evaluate its true impact on career development and the quality of laboratory professionals produced (28). Future refinements should incorporate digital learning tools for rare case exposure and establish longitudinal tracking systems to correlate training experiences with workplace performance metrics.
Conclusion
This study evaluated the implementation of a laboratory-result-oriented modular teaching model integrated with ISO 15189 principles for clinical hematology interns. Compared to traditional methods, the model demonstrated significantly enhanced teaching effectiveness, evidenced by statistically higher scores in theoretical examinations, operational skill assessments, and clinical reasoning evaluations (p < 0.05). Furthermore, interns reported significantly greater satisfaction with the teaching process. By utilizing actual laboratory test results as the learning anchor and embedding ISO 15189 requirements (covering personnel competence, procedural documentation, quality control, equipment management, and continuous improvement) within discrete modules, the model effectively bridges theoretical knowledge with the practical demands of standardized laboratory practice. Limitations include the single-center design and sample size, which necessitate further validation across diverse settings. Future research should also incorporate longitudinal studies to assess competency retention and explore the integration of digital tools for broader case exposure.
Statements
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
This study was approved by the Ethics Committee of Nanjing Drum Tower Hospital (Approval No: 2022-238-02). Informed consent was obtained from all individuals included in this study.
Author contributions
HX: Writing – review & editing, Writing – original draft, Conceptualization, Visualization. JL: Writing – review & editing, Validation. YZ: Writing – original draft, Investigation, Writing – review & editing. LC: Writing – original draft, Investigation, Methodology. AW: Data curation, Formal analysis, Writing – review & editing. LG: Data curation, Formal analysis, Writing – review & editing. TT: Supervision, Software, Writing – review & editing. XW: Writing – original draft, Resources, Project administration, Writing – review & editing. YC: Conceptualization, Supervision, Funding acquisition, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by National Natural Science Fund of China (92269118 to YC), the National key Research and Development program (2023YFC2309100).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2025.1612934/full#supplementary-material
References
1.
Phillips HL Jator EK Latchem SR Catalano TA . Clinical educators' teaching approaches and attributes in laboratory medicine. Lab Med. (2023) 54:e134–40. doi: 10.1093/labmed/lmad001
2.
Cook J . Laboratory integration and consolidation in a regional health system. Lab Med. (2017) 48:e43–52. doi: 10.1093/labmed/lmw069
3.
Sautter R Halstead D . The importance of medical laboratory scientists and the number of doctoral scientists that began their career by working on the front lines of laboratory medicine. Lab Med. (2023) 54:e121–3. doi: 10.1093/labmed/lmac143
4.
Weiss RL . Training in laboratory management and the MBA/MD in laboratory medicine. Clin Lab Med. (2007) 27:381–95; abstract viii. doi: 10.1016/j.cll.2007.03.009
5.
Guzel O Guner EI . ISO 15189 accreditation: requirements for quality and competence of medical laboratories, experience of a laboratory I. Clin Biochem. (2009) 42:274–8. doi: 10.1016/j.clinbiochem.2008.09.011
6.
Plebani M Sciacovelli L . ISO 15189 accreditation: navigation between quality management and patient safety. J Med Biochem. (2017) 36:225–30. doi: 10.1515/jomb-2017-0038
7.
Vanstapel FJLA Orth M Streichert T Capoluongo ED Oosterhuis WP Çubukçu HC et al . ISO 15189 is a sufficient instrument to guarantee high-quality manufacture of laboratory developed tests for in-house-use conform requirements of the European in-vitro-diagnostics regulation. Clin Chem Lab Med. (2023) 61:608–26. doi: 10.1515/cclm-2023-0045
8.
Knoll JS Rowell SL . Clinical hematology. In-clinic analysis, quality control, reference values, and system selection. Vet Clin North Am Small Anim Pract. (1996) 26:981–1002. doi: 10.1016/s0195-5616(96)50051-3
9.
World Health Organization . WHO guidelines on quality control in haematology. Geneva: World Health Organization (2022).
10.
Vroemen WHM van Beers JJBC Frissen J de Wit NCJ . Hypo-osmolality and its effect on erythrocyte parameters. Int J Lab Hematol. (2023) 45:1. doi: 10.1111/ijlh.14022
11.
Pozdnyakova O Brugnara C . Hematology laboratory in the digital and automation age. Clin Lab Med. (2024) 44:xiii–xiv. doi: 10.1016/j.cll.2024.06.001
12.
Weiser MG Vap LM Thrall MA . Perspectives and advances in in-clinic laboratory diagnostic capabilities: hematology and clinical chemistry. Vet Clin North Am Small Anim Pract. (2007) 37:221–36. doi: 10.1016/j.cvsm.2006.11.005
13.
Davis GM Lantis KL Finn WG . Laboratory hematology practice: present and future. Cancer Treat Res. (2004) 121:167–79.
14.
Sana N Moiz B Raheem A . Clinical significance of repeat testing of critical results in a hematology laboratory. Int J Lab Hematol. (2020) 42:e132–4. doi: 10.1111/ijlh.13166
15.
Vidali M Carobene A Apassiti Esposito S Napolitano G Caracciolo A Seghezzi M et al . Standardization and harmonization in hematology: instrument alignment, quality control materials, and commutability issue. Int J Lab Hematol. (2021) 43:364–71. doi: 10.1111/ijlh.13379
16.
Oderinu OH Adegbulugbe IC Orenuga OO Butali A . Comparison of students' perception of problem-based learning and traditional teaching method in a Nigerian dental school. Eur J Dent Educ. (2020) 24:207–12. doi: 10.1111/eje.12486
17.
Xin W Zou Y Ao Y Cai Y Huang Z Li M et al . Evaluation of integrated modular teaching in Chinese ophthalmology trainee courses. BMC Med Educ. (2020) 20:158. doi: 10.1186/s12909-020-02073-w
18.
Wright AF . Modular continuing medical education: our flexible friend?Br J Gen Pract. (1994) 44:146–7. PMID:
19.
Turan Gürhopur FD Işler Dalgiç A . The effect of a modular education program for children with epilepsy and their parents on disease management. Epilepsy Behav. (2018) 78:210–8. doi: 10.1016/j.yebeh.2017.07.048
20.
Vermeersch P Frans G von Meyer A Costelloe S Lippi G Simundic AM . How to meet ISO15189:2012 pre-analytical requirements in clinical laboratories? A consensus document by the EFLM WG-PRE. Clin Chem Lab Med. (2021) 59:1047–61. doi: 10.1515/cclm-2020-1859
21.
Lee GR Fitzgibbon MC O'Shea P . In control? IQC consensus and statutory regulation. Int J Health Care Qual Assur. (2016) 29:492–506. doi: 10.1108/IJHCQA-08-2015-0097
22.
Molinaro RJ Winkler AM Kraft CS Fantz CR Stowell SR Ritchie JC et al . Teaching laboratory medicine to medical students: implementation and evaluation. Arch Pathol Lab Med. (2012) 136:1423–9. doi: 10.5858/arpa.2011-0537-EP
23.
Lepiller Q Solis M Velay A Gantner P Sueur C Stoll-Keller F et al . Problem-based learning in laboratory medicine resident education: a satisfaction survey. Introduction de l’apprentissage par problèmes dans la formation théorique des internes du DES de biologie médicale: évaluation de la satisfaction des internes. Ann Biol Clin. (2017) 75:181–92. doi: 10.1684/abc.2017.1236
24.
Tong Y Chen H Wang Y Wu Z Gu J Wu Q et al . An innovative teaching approach for diabetes mellitus in laboratory medicine uses the clinical laboratory diagnostic pathway. J Med Educat Curri Develop. (2023) 10:23821205231219396. doi: 10.1177/23821205231219396
25.
Hopper MK . Assessment and comparison of student engagement in a variety of physiology courses. Adv Physiol Educ. (2016) 40:70–8. doi: 10.1152/advan.00129.2015
26.
Meng L Liu X Ni J Shen P Jiao F . An investigation for the efficacy of teaching model of combining virtual simulation and real experiment for clinical microbiology examination. Front Med. (2024) 11:1255088. doi: 10.3389/fmed.2024.1255088
27.
Liu SQ . Application of outcome-based education model in internship teaching of medical laboratory science. Chin J Lab Med. (2023) 46:193. doi: 10.3760/cma.j.cn114452-20231009-00193
28.
Agustian HY . Methodological rigor in laboratory education research. Laboratories. (2024) 1:74–86. doi: 10.3390/laboratories1010006
Summary
Keywords
medical laboratory education, laboratory results, modular teaching, interns, teaching effectiveness
Citation
Xie H, Li J, Zhu Y, Chen L, Wang A, Gong L, Tan T, Wang X and Chen Y (2025) Application of laboratory-result-oriented modular teaching model in the training of clinical hematology laboratory interns. Front. Med. 12:1612934. doi: 10.3389/fmed.2025.1612934
Received
06 May 2025
Accepted
29 July 2025
Published
18 August 2025
Volume
12 - 2025
Edited by
Goran Hauser, University of Rijeka, Croatia
Reviewed by
Predrag Jovanovic, University Clinical Center Tuzla, Bosnia and Herzegovina
Quekun Peng, Chengdu Medical College, China
Updates
Copyright
© 2025 Xie, Li, Zhu, Chen, Wang, Gong, Tan, Wang and Chen.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xian Wang, ctnicat@163.comYuxin Chen, yuxin.chen@nju.edu.cn
†These authors have contributed equally to this work
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.