- Medical Program, Faculty of Health Sciences and Medicine, Bond University, Gold Coast, QLD, Australia
Introduction: The selection process for medical schools plays a vital role in identifying candidates with the attributes and capabilities needed for success in medicine. Multiple Mini-Interviews (MMI) are widely used to assess non-cognitive attributes like communication, empathy, and ethical judgment. Ensuring their fairness and validity across diverse applicant groups is essential for equitable selection.
Aims: This study aimed to investigate: (1) is there evidence to support the factorial validity of MMI structure; (2) whether non-cognitive attributes assessed by MMIs are consistently interpreted across gender groups; and (3) whether gender-related disparities exist in MMI performance.
Methods: Data were drawn from applicants to an Australian Medical School across three selection cycles (2022–2024). Confirmatory Factor Analysis (CFA) was used to assess the dimensionality of MMI performance, with multiple competing models tested to identify the best-fitting structure. The selected model was then assessed for measurement invariance across gender using Multi-Group CFA. Once scalar invariance was established, latent mean comparisons were conducted to examine gender-related differences in MMI performance.
Results: CFA indicated a well-fitting structure for MMIs, with a higher-order model emerging as the most appropriate representation across cohorts. Measurement invariance testing confirmed scalar invariance across gender groups, indicating that MMI non-cognitive attributes were demonstrated equivalently by males and females. Significant latent mean differences were identified, with female applicants consistently outperforming male applicants across all 3 years.
Discussion: The results provided empirical support for the factorial validity and measurement fairness of the MMI across gender groups. However, the consistent gender-based performance differences highlight the need for continued research into potential sources of group disparities and how they may impact selections equity. The results are relevant for medical educators and policymakers committed to evidence-based and equitable selection processes.
1 Introduction
The selection process for medical schools plays a vital role in identifying candidates with the attributes and capabilities needed for success in medicine. In recent years, medical school selection processes have evolved significantly, transitioning from traditional academic selection models to multifaceted selection processes that evaluate non-cognitive attributes such as communication, empathy, and ethical judgment, that are considered essential for health professionals (1–6). With significantly more applicants than available places, medical schools have sought more robust processes that not only identify academically strong candidates but also include non-cognitive assessments (7, 8).
Given this reality, selection processes must be both rigorous and evidence-based to ensure that candidates admitted to medical schools possess the necessary attributes to succeed in medical training and practice. While academic performance remains a strong predictor of success in the early years of medical education (6, 47), additional qualities such as empathy, ethical reasoning, and interpersonal effectiveness, are equally vital in developing competent and compassionate healthcare professionals (9). The incorporation of Multiple Mini-Interviews (MMI) (2) into selection processes offers a well-supported approach to evaluating these attributes. MMIs have demonstrated reliability and predictive validity in ranking candidates based on non-cognitive attributes essential for clinical excellence (2, 3, 6, 10, 11).
Originating in Canada, MMIs are now widely used internationally as a standardized and reliable method for assessing medical school applicants’ non-cognitive attributes (2, 4, 11, 12). MMIs are designed to evaluate candidates beyond their academic credentials, focusing on interpersonal and intrapersonal skills that are essential for success in medicine (13). The format shares conceptual similarities with the Objective Structured Clinical Examination (OSCE), which is frequently used to assess the knowledge and practical competencies of medical students. While OSCEs test applied clinical skills, MMIs are designed to evaluate how applicants respond to structured tasks that reveal their non-cognitive attributes (2, 4, 13).
MMIs typically consist of a series of structured interview stations, each presenting candidates with a distinct scenario or task designed to assess specific non-cognitive attributes. Candidates rotate between stations, responding to prompts that may involve ethical dilemmas, role-playing exercises, or situational problem-solving tasks. Each interaction is timed, typically lasting between 6 and 10 minutes, and responses are evaluated against predetermined criteria to ensure consistency and fairness in assessment (1, 2). Unlike traditional panel interviews, which rely on the judgment of a single interviewer or panel evaluating one scenario (1, 2, 4, 47), MMIs engage multiple independent assessors across different stations to ensure more standardized evaluation reducing the impact of individual bias and improving interrater reliability (2, 11).
Importantly, MMIs do not aim to measure personality traits. Rather, they assess candidates’ behaviors and approach as they navigate structured tasks within a defined framework of professional expectations. In doing so, it is also hoped that selection processes including MMIs will identify suitable applicants without systematically advantaging or disadvantaging applicants of certain demographics. Research examining potential bias in MMI processes has produced mixed findings. Some studies suggest that female candidates tend to be evaluated more favorably by assessors in many (5, 14), but not all MMI processes (15). This may reflect broader gender-based expectations and stereotypes that portray women as warmer, more empathetic, and possessing stronger verbal communication skills than men (16, 17). If such stereotypes have some basis in actual skill differences, it is possible that female applicants are objectively stronger in non-cognitive attributes assessed in MMIs. However, there is also evidence that both male and female assessors tend to evaluate women as more positive than men outside of the context of selection (18). These evaluative biases, potentially shaped by stereotypes, may result in more favorable assessments of female candidates even when objective performance is equivalent. As such, it is important to establish whether there are gender differences in performance and if so, whether they reflect true differences in candidate ability or are instead because of biases introduced in the tool used to evaluate applicants.
Various approaches have been used to assess performance on MMI stations, including use of a single score (global rating), or an aggregate score based on station specific rubrics, or a general rubric/tool applied to all stations (19). Utilizing a consistent and well-defined framework to evaluate candidate’s performance is one strategy to mitigate assessor bias and ensure equitable assessment for all candidates. Fairness and transparency in medical school selection processes involve designing tools that assess candidate attributes in a consistent, unbiased manner regardless of gender, socioeconomic status, or ethnicity (1, 4, 5, 20).
Previous studies have consistently reported higher MMI scores for female applicants (7, 14, 48), raising important questions about whether these differences reflect true variation in attributes assessed or potential scoring biases. Previous studies on MMI dimensionality have reported mixed findings, with some supporting unidimensional models and others endorsing multi-group factor analysis (21, 22) (Leduc et al., 2017). To clarify these inconsistencies, researchers have applied generalizability theory (23) and multi-group confirmatory factor analysis (MG-CFA) to disentangle sources of reliable variance, revealing the MMIs inherently multidimensional structure (21, 22) (Leduc et al., 2017). To address this, we applied MG-CFA to test whether the Behaviorally Anchored Rating Scales (BARS) used in our MMIs function equivalently across gender. Establishing measurement invariance is essential, as noninvariance suggests that a construct may differ in structure or meaning across groups, rendering group comparisons invalid (24).
This study aimed to investigate: (1) is there evidence to support the factorial validity of the MMI structure at our medical school; (2) whether core attributes assessed in MMIs are consistently interpreted across gender groups; and (3) whether gender-related disparities exist in MMI performance. By exploring these aims, researchers can assess whether MMIs function as equitable selection tools or whether underlying biases affect their effectiveness. Addressing these concerns is essential in ensuring medical school selection processes continue to be fair, inclusive, and reflective of the diverse populations they serve.
2 Methods
2.1 Study design and setting
This retrospective, cross-sectional study used data from applicants to an Australian Medical School across three selection cycles (2022–2024). This time range was selected due to the relative stability of our selection processes during these years.
2.2 MMI process and scoring method
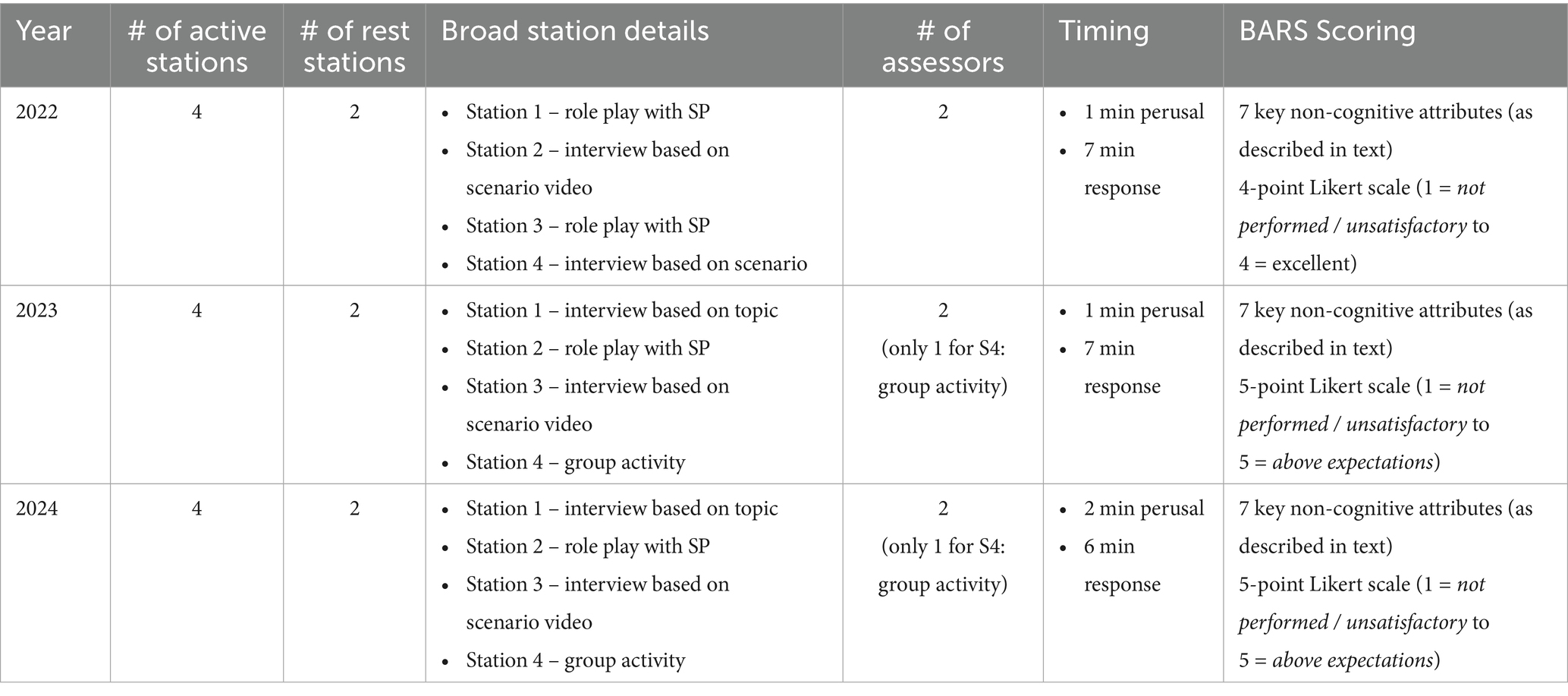
At our institution, applicants undertake MMIs as the final step in a staged selection process that includes four sequential and independent components: (1) eligibility checks (e.g., domestic student), (2) meeting a minimum academic threshold, (3) completion of proctored psychometric testing (ability-based emotional intelligence and self-report personality assessments), and (4) performance in MMI. Each stage is assessed independently, with no cumulative or weighted scoring across stages. Approximately 50% of applicants are excluded from the selection process at each stage. Importantly, it is MMI performance alone that determines whether an offer is made. See Figure 1 for an overview of the full selection process.
Consistent with previous literature, MMI stations at our institution are designed to evaluate non-cognitive attributes that are critical for future medical practice, including communication, ethical reasoning, empathy, and professionalism. MMIs comprise six stations (4 active and 2 rest), each lasting approximately 8 min, with a short transition period between stations (see Table 1 for further details). Each station presents candidates with a unique scenario or task aligned to specific non-cognitive attributes. These may involve ethical dilemmas, role-playing activities with a simulated participant, group activity tasks, or situational behavioral scenarios. Each MMI station is independently rated by two trained assessors (excluding the group station – see Table 1) using a Behaviorally Anchored Rating Scale (BARS) (25), which was developed specifically for our medical school through a three-round modified Delphi process (26, 27) of 13 experts.
BARS are a standardized scoring method to distinguish between a range of behaviors, as opposed to skills (25). In this type of scale, specific behaviors are identified that contribute to an overall rating of performance. BARS is typically developed by consensus methods to define the main dimensions of a particular role, clearly identifying the scale of performance (28). For example, Wright et al. (25) defined five dimensions that are a measure of teamwork, with explicit behaviors that demonstrate proficiency. In our case, we were looking to define the key behavioral attributes expected from prospective medical students at an Australian institution. Following a consensus seeking process, seven non-cognitive attributes were established with associated scales to measure non-cognitive attributes in prospective medical students.
The BARS provides assessors with clearly defined descriptors of performance for each score point, anchored in specific, observable behaviors across seven key non-cognitive attributes: (1) communication skills, (2) self-regulation, (3) effective team member, (4) adaptability, (5) analytical/critical thinking, (6) empathy, and (7) cultural capability. This allows interviewers to base ratings on observed candidate behavior rather than subjective impressions, thereby mitigating assessor bias (29). The use of the BARS across all MMI stations contributes to the fairness, transparency, and defensibility of the selection process (25, 28). It also ensures candidates are assessed against consistent criteria, regardless of which station or assessor they encounter.
Before participating in MMIs at our institution, assessors are provided with interviewer training resources and engage in interviewer training sessions to support standardization and reduce the potential for subjective bias. The aim is to familiarize interviewers with the structure of MMIs, how to deliver specific station scenarios, understand the BARS, and how to interpret the BARS for different scenarios. Interviewers are also provided with training on implicit biases that can influence evaluations of applicants (30).
In 2022, the BARS was scored on a 4-point Likert scale (1 = not performed / unsatisfactory to 4 = excellent). From 2023, a neutral anchor point was introduced, and the BARS was scored using a 5-point Likert scale (1 = not performed / unsatisfactory to 5 = above expectations). At each station, two interviewers independently evaluate candidates based on the seven non-cognitive attributes defined BARS framework. Scores for each station are aggregated into a total score. Where a score had been missed by an assessor or where there was only a single assessor, the average score for that station on that day the candidate attended was awarded and included in the aggregated total score.
MMIs at our institution do not employ a predefined threshold score to determine candidate success. Rather than adhering to a static benchmark, the annual cut score is established upon the performance distribution of candidates that had advanced to the next stage of the medical selection process. This data-driven approach allows the selection framework to accommodate year-to-year variability in candidate cohorts and maintain alignment with programmatic objectives and capacity constraints. While this method ensures contextual fairness, it also necessitates transparency in scoring procedures and rigorous post-hoc analysis to uphold reliability and equity in selection outcomes.
2.3 Study participants
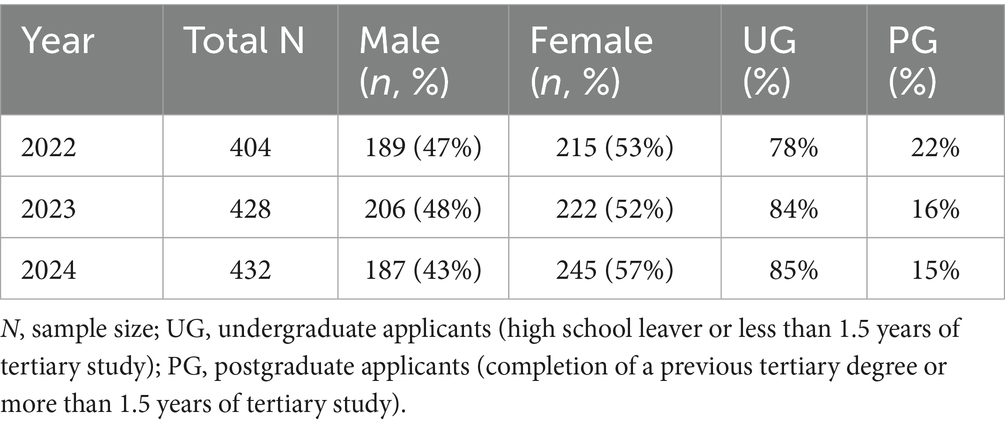
Participants were applicants to our medical school who completed MMIs in 2022 (N = 404), 2023 (N = 428), and 2024 (N = 432). One applicant from each of the 2023 and 2024 cohorts identified their gender as “Other” and was excluded from gender-based analyses due to the small subgroup size. Gender distribution was relatively balanced across years, with a slight female majority. The proportion of undergraduate (high school graduates with no tertiary experience) applicants increased steadily, from 78% in 2022 to 85% in 2024. Demographic distributions by gender and undergraduate/postgraduate status are summarized in Table 2.
As an Australian private institution, students can access government supported loans for only a portion of the total fees. There is no financial aid available only First Nations applicants are eligible for fee-waiver scholarships. This means that applicants are generally from families representing the highest levels of socioeconomic advantage.
2.4 Statistical data analysis
Data were analyzed in three phases using SPSS and JASP 0.19.3 (31). The following steps were followed after conducting initial data checks.
2.4.1 Dimensionality assessment
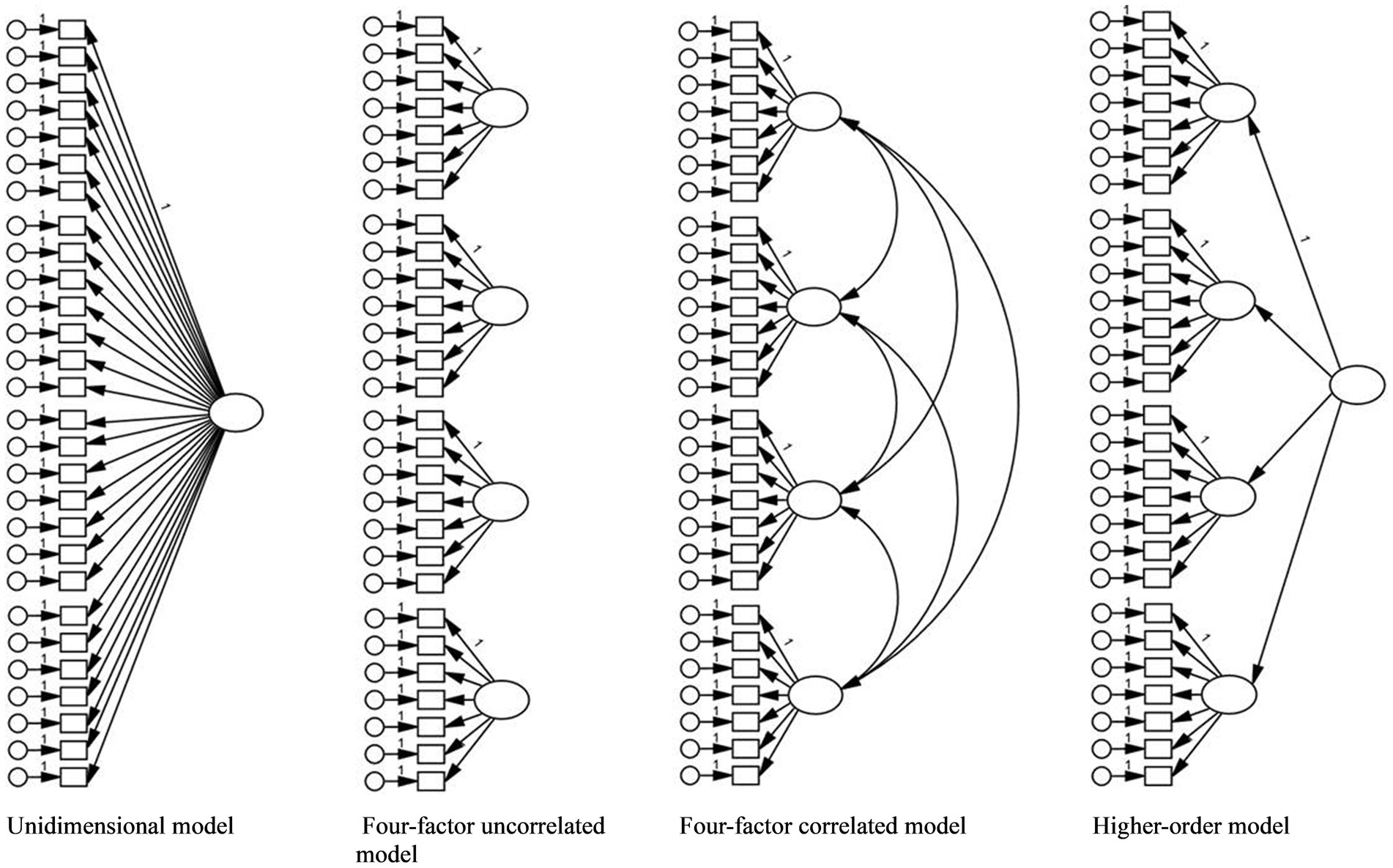
Confirmatory Factor Analysis (CFA) was conducted separately for each year to examine the factor structure of MMI scores. Four competing models (Figure 2) were tested using the robust maximum likelihood (MLR) estimator:
1. Unidimensional model - assumes all MMI items reflect a single general construct.
2. Four-factor uncorrelated model - assumes each station taps into a distinct unrelated attribute.
3. Four-factor correlated model - assumes non-cognitive attributes measured at each station are distinct but interrelated.
4. Higher-order model - assumes station performances reflect specific attributes, underpinned by a broader construct (e.g., general ability).
Model fit was evaluated using standard indices in Structural Equation Modeling (SEM), including the root mean square error of approximation (RMSEA), comparative fit index (CFI), Tucker–Lewis index (TLI), and standardized root mean square residual (SRMR). Following conventional criteria, values of RMSEA and SRMR < 0.05, and CFI and TLI > 0.95 were considered indicative of good fit (32, 33). Due to sample size sensitivity, χ2 was reported but not used as a primary evaluation criterion.
To further assess construct validity and reliability, we examined standardized factor loadings, average variance extracted (AVE), coefficient alpha (α), and McDonald’s omega (ω). Given the limitations of α (e.g., assuming tau-equivalence), ω was prioritized as a more robust reliability indicator (34, 35).
2.4.2 Measurement invariance (MI)
Multi-Group Confirmatory Factor Analysis (MG-CFA) was conducted to evaluate measurement invariance (whether the same underlying latent construct was measured equivalently) across applicant gender (Male vs. Female) within each year. A stepwise approach was applied:
1. Configural invariance - tests whether the same factor structure holds across groups, indicating that the constructs are conceptualized similarly across groups.
2. Metric invariance - tests whether factor loadings are equivalent, suggesting consistent interpretation of applicants’ demonstrated behaviors.
3. Scalar invariance - tests whether item intercepts are equivalent, allowing for valid comparisons of latent means across gender.
Model comparisons were based on changes in fit indices (ΔCFI and ΔRMSEA), following Chen (36). Changes of ≤ 0.010 in CFI and ≤ 0.015 in RMSEA were taken as evidence of invariance. Researchers generally agree that establishing scalar invariance is sufficient for supporting valid latent mean comparisons across groups (37–39). Without MI, any differences in scores could reflect measurement bias, not true differences in the underlying construct (40). In the context of medical school selection, testing measurement invariance is essential to ensure that assessment tools, such as MMIs, evaluate applicants consistently across demographic groups, thereby supporting fair and defensible selections decisions (38, 41, 42).
2.4.3 Latent mean comparisons
Where scalar invariance was established, latent mean differences across gender were estimated using MG-CFA, with males as the reference group.
2.5 Ethical considerations
This research was approved by the Human Research Ethics Committee (AB03432) at the authors’ institution.
3 Results
3.1 Descriptive statistics
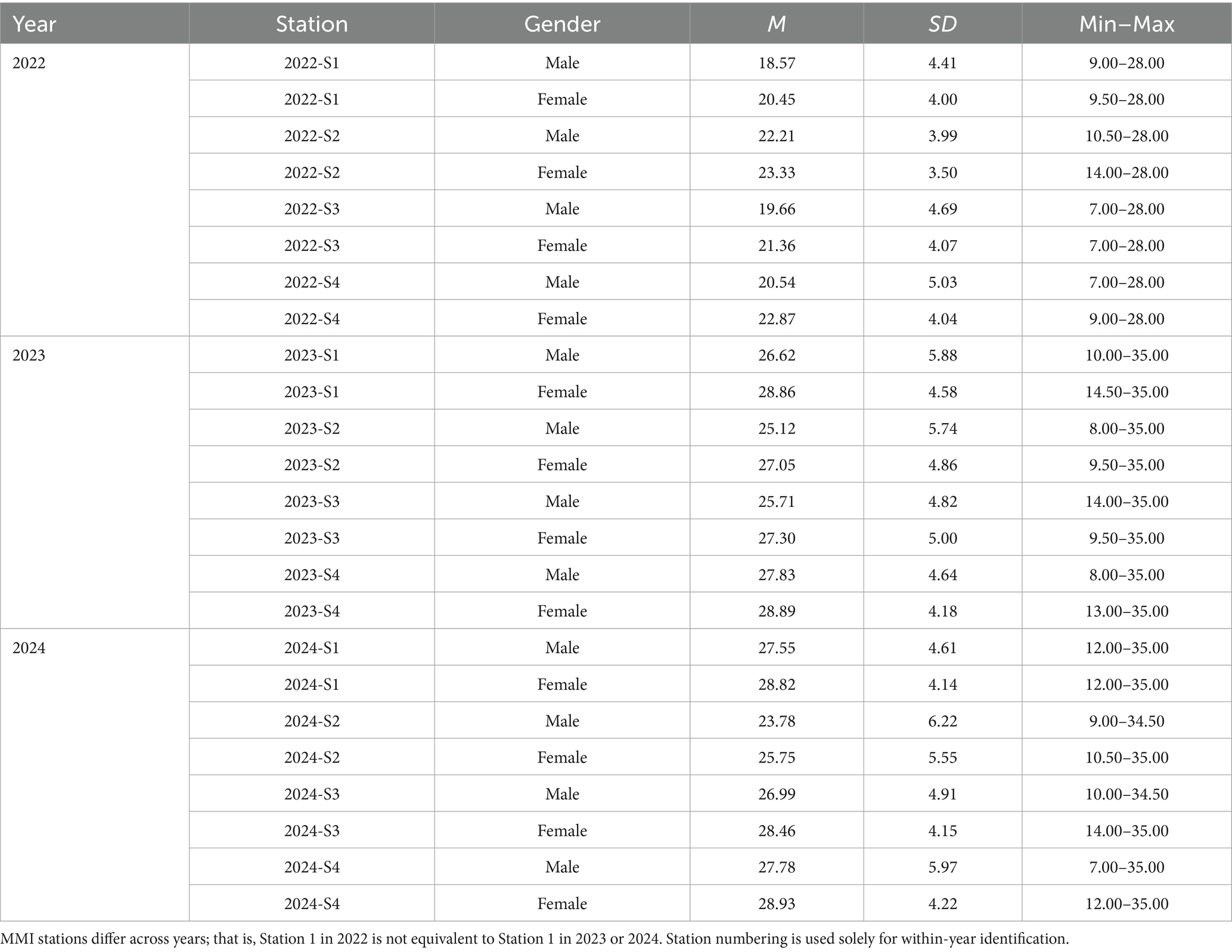
Assessor omissions for a non-cognitive attribute within the BARS framework occurred at a rate of 0.7% in 2022, 0.3% in 2023, and 0.0% in 2024. In cases where only a single assessor was present, 23.0% in 2022, and 0.0% in both 2023 and 2024, the station-specific average score, based on all candidates assessed on that day, was assigned for each of the seven non-cognitive attributes and incorporated into the aggregated total score. Table 3 presents descriptive statistics (means, standard deviations, ranges) for each MMI station by gender across all 3 years. Female applicants had consistently higher scores than males across all stations and years. Standard deviations were generally comparable between genders within each station and year, suggesting similar levels of score variability across groups.
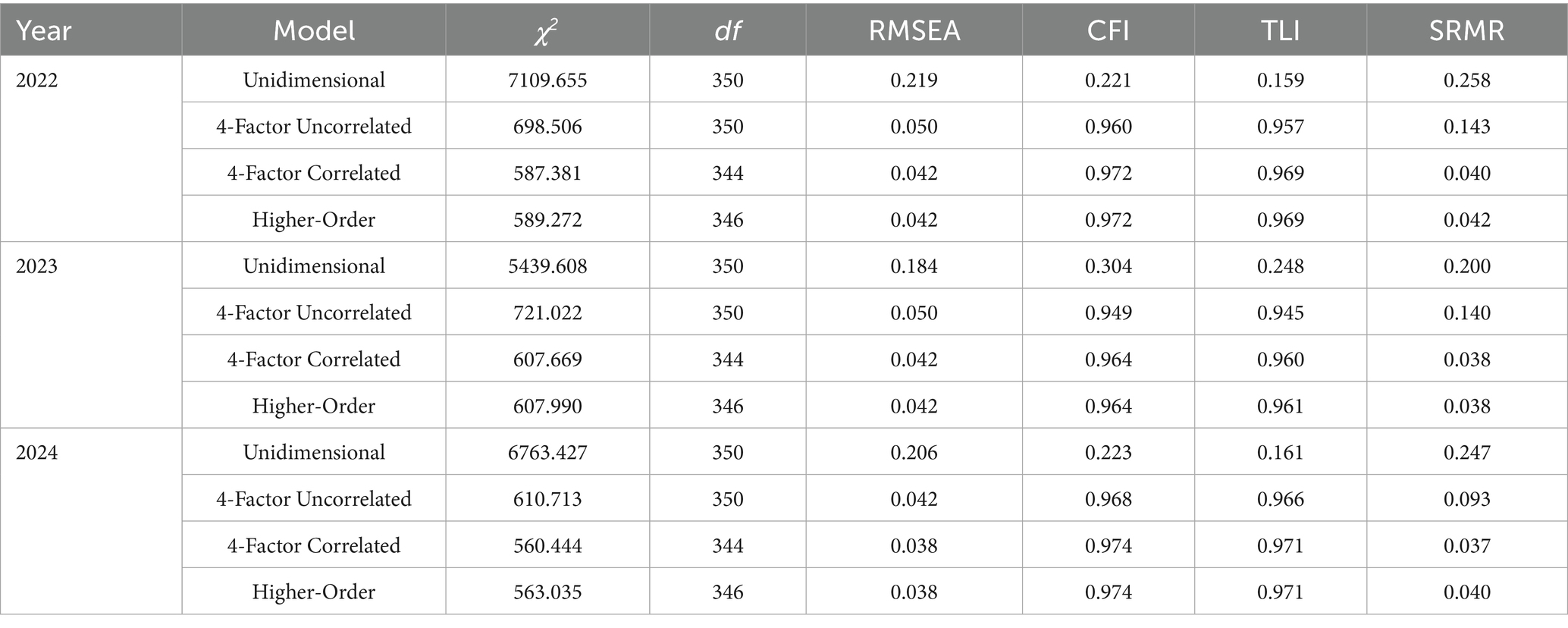
3.2 Confirmatory factor analysis (CFA)
Model fit indices for all tested models are presented in Table 4. The unidimensional model showed poor fit across all cohorts. The four-factor uncorrelated model improved fit considerably but underperformed relative to the four-factor correlated and higher-order models. Both the correlated and higher-order models demonstrated excellent and nearly equivalent fit. Chi-square difference tests between the correlated and higher-order models indicated no significant loss of fit when adopting the more parsimonious higher-order structure (2022: Δχ2 = 1.733, Δdf = 2, p = 0.420; 2023: Δχ2 = 0.075, Δdf = 2, p = 0.963; 2024: Δχ2 = 2.475, Δdf = 2, p = 0.290). Given these results and the theoretical appeal of modeling a general ability factor underlying MMI station performance, the higher-order model was retained for subsequent invariance testing. In the four-factor correlated CFA models, factor correlations ranged from 0.13 to 0.42 in 2022, 0.16 to 0.36 in 2023, and 0.03 to 0.23 in 2024, indicating generally low to moderate inter-factor relationships across years.
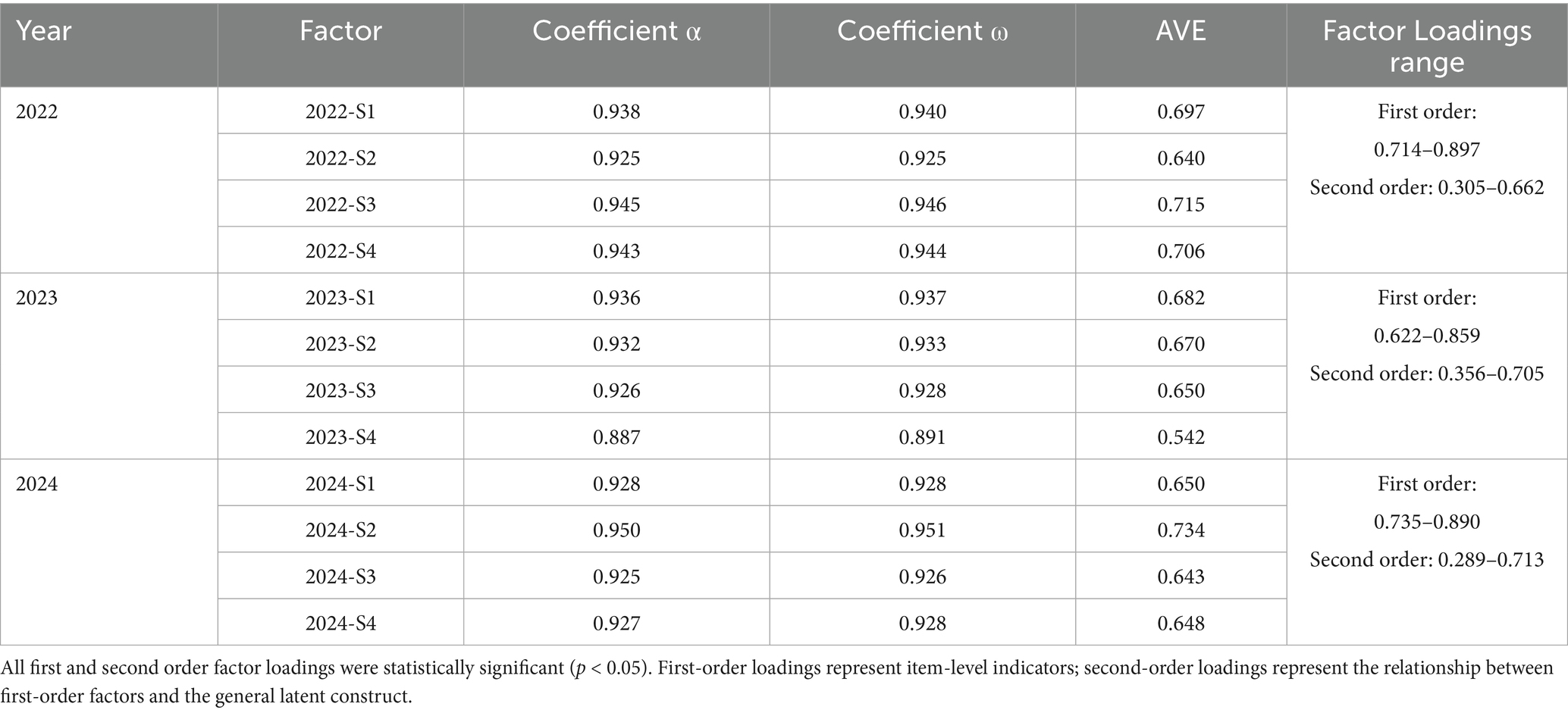
Table 5 reports internal consistency estimates, AVE, and range of factor loadings. Across all years, internal consistency was high for each station (α and ω > 0.88), and AVE values exceeded 0.50, indicating good reliability and convergent validity. All standardized factor loadings were statistically significant (p < 0.05).
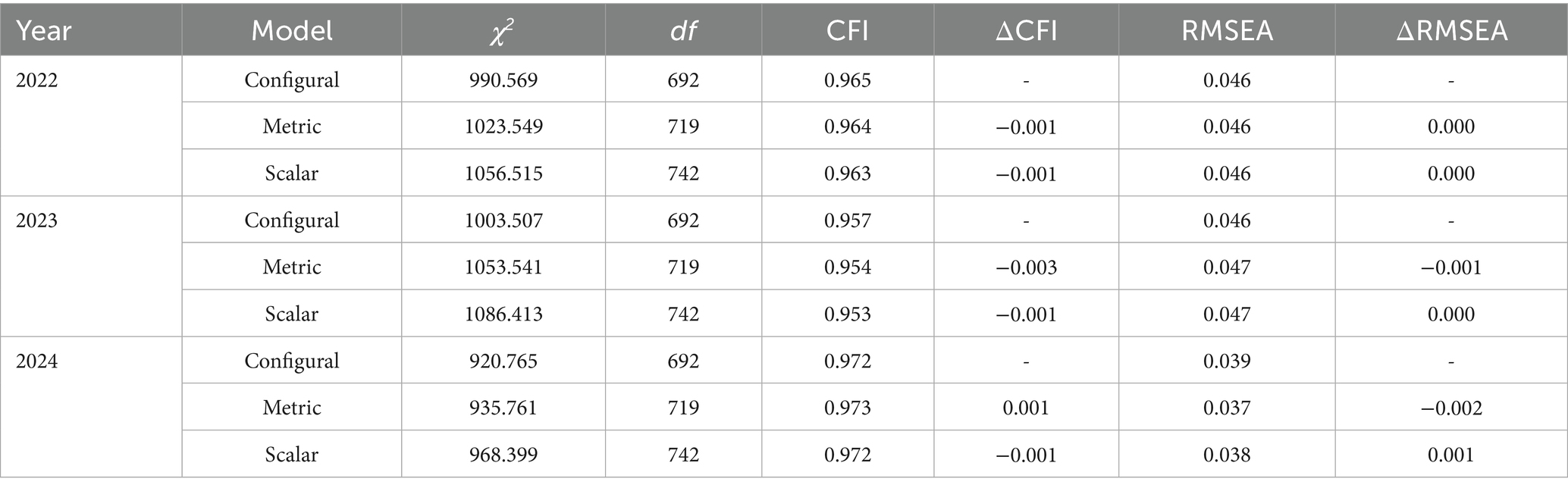
3.3 Measurement equivalence
As shown in Table 6, configural, metric, and scalar invariance were supported in all 3 years. ΔCFI and ΔRMSEA values fell within accepted thresholds, confirming that the MMI structure was interpreted equivalently across gender groups.
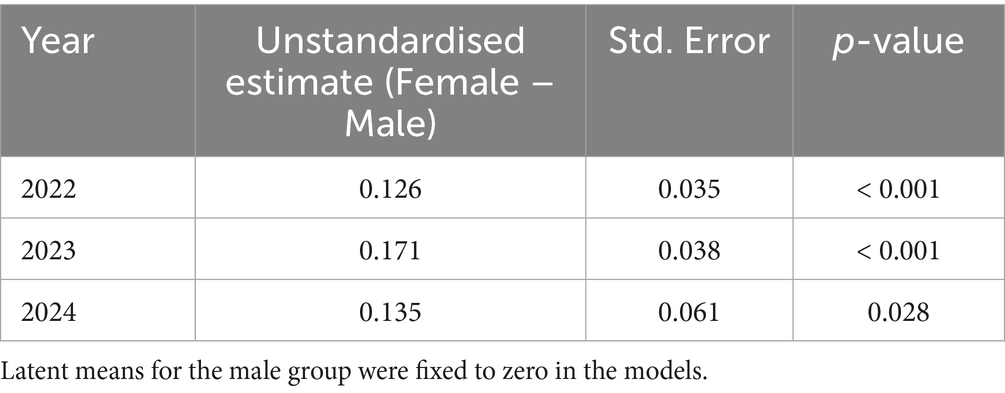
3.4 Gender differences
Table 7 presents latent mean differences by gender. In all 3 years, females had significantly higher latent mean scores compared to males. While measurement invariance confirmed that the MMI measured non-cognitive attributes equivalently across gender, persistent latent mean differences indicate a systematic gender-related performance trend.
4 Discussion
This study examined the dimensionality, reliability, and measurement equivalence of MMI scores across three consecutive selection cycles, with a particular focus on gender-based fairness. By applying a robust psychometric framework, we provide empirical evidence supporting the structural validity and reliability of MMIs, while also identifying consistent gender-based performance trends that warrant further attention.
Across all 3 years, a higher-order factor structure best represented MMI station performance, with each station loading onto specific non-cognitive attributes that were, in turn, underpinned by a broader latent non-cognitive ability construct. The findings align with prior literature conceptualizing MMIs as multidimensional tools that evaluate distinct, but related non-cognitive attributes that contribute to performance as a medical student and future clinician (2). The high internal consistency values, strong factor loadings and AVE estimates across cohorts further support the reliability and convergent validity of the BARS used in our selection process. Notably, the four-factor correlated model used also demonstrated excellent fit, indicating that station-level scores retain value as discrete measures of specific non-cognitive attributes. Thus, depending on the intended purpose, institutions may reasonably use either composite scores or station-specific results.
Crucially, measurement invariance analyses confirmed that male and female applicants interpreted and responded to the MMI tasks similarly, and that the observed scores reflected equivalent measurement of non-cognitive attributes across gender. These findings provide strong evidence that the BARS functioned equivalently across gender and may reflect the contribution of the associated interviewer training protocols to supporting equitable assessment practices. Establishing measurement invariance is a necessary precondition for making valid group comparisons and is an often overlooked, yet vital component of evaluating fairness in selection tools (38, 39).
Notably, females scored significantly higher than males on latent MMI performance across all 3 years, suggesting a consistent gender-related performance pattern that warrants further exploration. This pattern mirrors trends in other MMI-based studies (4, 5, 14, 20, 43–46) and may reflect genuine gender differences in the non-cognitive attributes assessed such as communication, empathy, and teamwork. Importantly, since scalar invariance was established, these differences likely reflect true variation in performance rather than measurement bias.
Nonetheless, persistent gender differences raise important questions for medical school leadership when considering their selection policies and procedures. While MMIs are designed to assess attributes essential to successful progression through medical school and future practice, selection processes must also ensure that such tools do not inadvertently favor certain groups. Future research might explore whether these gender differences persist in longitudinal academic, clinical outcomes or future career choices, or whether they reflect modifiable differences in socialization, experience, or preparation for the MMI format.
4.1 Strengths, limitations and future research
This study has several strengths, including its multi-year design, robust analytic approach, and use of a structured, theoretically grounded scoring system. Moreover, the consistency of findings across the 3 years enhances the generalizability of the results. However, some limitations should be acknowledged. First, our data reflects the context of a single private institution that is predominately a school leaver/undergraduate entry medical school. As such, the findings may not extend to other MMI designs or applicant populations. Second, while the sample sizes were sufficient for CFA and MG-CFA, the exclusion of non-binary participants due to small subgroup size limited the inclusivity of the analysis. Future research should explore intersectional factors (e.g., gender, culture, age, socioeconomic background) and use mixed methods to better understand why gender differences in performance persist despite structural equivalence. Replication across different settings/institutions would also be beneficial.
5 Conclusion
The results provide strong psychometric support for the use of MMIs in medical school selection processes, confirming their structural integrity and fairness in terms of measurement across gender. While the MMI assessed non-cognitive attributes equivalently for male and female applicants, consistent gender-based differences in performance were observed. These findings underscore the importance of ongoing monitoring of performance patterns and further investigation into the factors contributing to these disparities. As medical schools continue to refine their selection processes, integrating psychometric validation and fairness analyses into routine practice can support more defensible and equitable decision making.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, upon reasonable request.
Ethics statement
The studies involving humans were approved by Human Research Ethics Committee (AB03432) at the authors’ institution. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
JS: Conceptualization, Data curation, Formal analysis, Funding acquisition, Methodology, Project administration, Visualization, Writing – original draft, Writing – review & editing. AB: Conceptualization, Data curation, Formal analysis, Writing – original draft, Writing – review & editing, Project administration. MA: Conceptualization, Data curation, Formal analysis, Writing – original draft, Writing – review & editing, Methodology, Validation, Visualization. BC: Conceptualization, Writing – review & editing, Data curation, Formal analysis, Writing – original draft. JS-P: Writing – review & editing, Conceptualization, Project administration. JB: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We would like to offer special thank you to the professional and academic staff who generously dedicated their time in organizing and assessing MMIs and all the candidates that participated in the selection processes at our institution.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Banks, PW, Hagedorn, JC II, Soybel, A, Coleman, DM, Rivera, G, and Bhardwaj, N. Multiple mini interviews vs traditional interviews: investigating racial and socioeconomic differences in interview processes. Adv Med Educ Pract. (2025) 16:157–63. doi: 10.2147/AMEP.S480717
2. Eva, KW, Rosenfeld, J, Reiter, HI, and Norman, GR. An admissions OSCE: the multiple mini-interview. Med Educ. (2004) 38:314–26. doi: 10.1046/j.1365-2923.2004.01776.x
3. Hadad, A, Gafni, N, Moshinsky, A, Turvall, E, Ziv, A, and Israeli, A. The multiple mini-interviews as a predictor of peer evaluations during clinical training in medical school. Med Teach. (2016) 38:1172–9. doi: 10.1080/0142159X.2016.1181730
4. Jerant, A, Fancher, T, Fenton, JJ, Fiscella, K, Sousa, F, Franks, P, et al. How medical school applicant race, ethnicity, and socioeconomic status relate to multiple mini-interview-based admissions outcomes: findings from one medical school. Acad Med. (2015) 90:1667–74. doi: 10.1097/ACM.0000000000000766
5. Knorr, M, Meyer, H, Sehner, S, Hampe, W, and Zimmermann, S. Exploring sociodemographic subgroup differences in multiple mini-interview (MMI) performance based on MMI station type and the implications for the predictive fairness of the Hamburg MMI. BMC Med Educ. (2019) 19:243. doi: 10.1186/s12909-019-1674-z
6. Reiter, HI, Eva, KW, Rosenfeld, J, and Norman, GR. Multiple mini-interviews predict clerkship and licensing examination performance. Med Educ. (2007) 41:378–84. doi: 10.1111/j.1365-2929.2007.02709.x
7. Leduc, JM, Rioux, R, Gagnon, R, Bourdy, C, and Dennis, A. Impact of sociodemographic characteristics of applicants in multiple mini-interviews. Med Teach. (2017) 39:285–94. doi: 10.1080/0142159X.2017.1270431
8. Lemay, JF, Lockyer, JM, Collin, VT, and Brownell, AK. Assessment of non-cognitive traits through the admissions multiple mini-interview. Med Educ. (2007) 41:573–9. doi: 10.1111/j.1365-2923.2007.02767.x
9. Emanuel, EJ, and Gudbranson, E. Does medicine overemphasize IQ? JAMA. (2018) 319:651–2. doi: 10.1001/jama.2017.20141
10. Eva, KW, Reiter, HI, Rosenfeld, J, Trinh, K, Wood, TJ, and Norman, GR. Association between a medical school admission process using the multiple mini-interview and national licensing examination scores. JAMA. (2012) 308:2233–40. doi: 10.1001/jama.2012.36914
11. Jerant, A, Henderson, MC, Griffin, E, Rainwater, JA, Hall, TR, Kelly, CJ, et al. Reliability of multiple mini-interviews and traditional interviews within and between institutions: a study of five California medical schools. BMC Med Educ. (2017) 17:190. doi: 10.1186/s12909-017-1030-0
12. Pau, A, Jeevaratnam, K, Chen, YS, Fall, AA, Khoo, C, and Nadarajah, VD. The multiple mini-interview (MMI) for student selection in health professions training – a systematic review. Med Teach. (2013) 35:1027–41. doi: 10.3109/0142159X.2013.829912
13. Rees, EL, Hawarden, AW, Dent, G, Hays, R, Bates, J, and Hassell, AB. Evidence regarding the utility of multiple mini-interview (MMI) for selection to undergraduate health programs: a BEME systematic review: BEME guide no. 37. Med Teach. (2016) 38:443–55. doi: 10.3109/0142159X.2016.1158799
14. Ross, M, Walker, I, Cooke, L, Raman, M, Ravani, P, Coderre, S, et al. Are female applicants rated higher than males on the multiple mini-interview? Findings from the University of Calgary. Acad Med. (2017) 92:841–6. doi: 10.1097/ACM.0000000000001466
15. Hegmann, T. Effect of applicant gender on multiple mini-interview admissions score. J Physician Assist Educ. (2019) 30:54–6. doi: 10.1097/jpa.0000000000000234
16. Ellemers, N. Gender stereotypes. Annu Rev Psychol. (2018) 69:275–98. doi: 10.1146/annurev-psych-122216-011719
17. Löffler, CS, and Greitemeyer, T. Are women the more empathetic gender? The effects of gender role expectations. Curr Psychol. (2023) 42:220–31. doi: 10.1007/s12144-020-01260-8
18. Eagly, AH, Mladinic, A, and Otto, S. Are women evaluated more favorably than men? An analysis of attitudes, beliefs, and emotions. Psychol Women Q. (1991) 15:203–16. doi: 10.1111/j.1471-6402.1991.tb00792.x
19. Knorr, M, and Hissbach, J. Multiple mini-interviews: same concept, different approaches. Med Educ. (2014) 48:1157–75. doi: 10.1111/medu.12535
20. Parsons, W, McHugh, J, and Yi, Y. Traditional panel interview versus multiple mini-interview (MMI) in medical school admissions: does performance differ by age, gender, urban or rural, or socioeconomic status (findings from one medical school). Med Ed Publish. (2018) 7:272. doi: 10.15694/mep.2018.0000272.1
21. Breil, SM, Forthmann, B, Hertel-Waszak, A, Ahrens, H, Brouwer, B, Schönefeld, E, et al. Construct validity of multiple mini interviews: investigating the role of stations, skills, and raters using Bayesian G-theory. Med Teach. (2020) 42:164–71. doi: 10.1080/0142159X.2019.1670337
22. Callwood, A, Harris, J, Gillam, L, Roberts, S, Kubacki, A, Christidis, A, et al. Cross-sectional evaluation of an asynchronous multiple mini-interview (MMI) in selection to health professions training programmes with 10 principles for fairness built-in. BMJ Open. (2023) 13:e074440. doi: 10.1136/bmjopen-2023-074440
24. Putnick, DL, and Bornstein, MH. Measurement invariance conventions and reporting: the state of the art and future directions for psychological research. Dev Rev. (2016) 41:71–90. doi: 10.1016/j.dr.2016.06.004
25. Wright, MC, Phillips-bute, BG, Petrusa, ER, Griffin, KL, Hobbs, GW, and Taekman, JM. Assessing teamwork in medical education and practice: relating behavioural teamwork ratings and clinical performance. Med Teach. (2009) 31:30–8. doi: 10.1080/01421590802070853
26. Hasson, F, Keeney, S, and McKenna, H. Research guidelines for the Delphi survey technique. J Adv Nurs. (2000) 32:1008–15. doi: 10.1046/j.1365-2648.2000.t01-1-01567.x
27. Linstone, HA, Turoff, M, Linstone, HA, and Turoff, M. The Delphi method. Reading, MA: Addison-Wesley (1975).
28. Debnath, S, Lee, BB, and Tandon, S. Fifty years and going strong: what makes behaviorally anchored rating scales so perennial as an appraisal method? Int J Bus Social Sci Res. (2015) 6:16–25. Available at: https://ijbssnet.com/journals/Vol_6_No_2_February_2015/3.pdf
29. Murphy, KR, and Pardaffy, VA. Bias in behaviorally anchored rating scales: global or scale-specific? J Appl Psychol. (1989) 74:343–6. doi: 10.1037/0021-9010.74.2.343
30. Bergelson, I, Tracy, C, and Takacs, E. Best practices for reducing bias in the interview process. Curr Urol Rep. (2022) 23:319–25. doi: 10.1007/s11934-022-01116-7
32. Cudeck, R, and Browne, MW. Constructing a covariance matrix that yields a specified minimizer and a specified minimum discrepancy function value. Psychometrika. (1992) 57:357–69. doi: 10.1007/BF02295424
33. Hu, L, and Bentler, PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling. (1999) 6:1–55. doi: 10.1080/10705519909540118
34. Sijtsma, K. On the use, the misuse, and the very limited usefulness of Cronbach’s alpha. Psychometrika. (2009) 74:107–20. doi: 10.1007/s11336-008-9101-0
35. Teo, T, and Fan, X. Coefficient alpha and beyond: issues and alternatives for educational research. Asia Pac Educ Res. (2013) 22:209–13. doi: 10.1007/s40299-013-0075-z
36. Chen, FF. Sensitivity of goodness of fit indexes to lack of measurement invariance. Struct Equ Model. (2007) 14:464–504. doi: 10.1080/10705510701301834
37. Ercikan, K, and Lyons-Thomas, J. Adapting tests for use in other languages and cultures In: K Geisinger, editor. APA handbook of testing and assessment in psychology. Washington, DC: American Psychological Association (2013). 545–69.
38. Schmitt, N, and Kuljanin, G. Measurement invariance: review of practice and implications. Hum Resour Manag Rev. (2008) 18:210–22. doi: 10.1016/j.hrmr.2008.03.003
39. Vandenberg, RJ, and Lance, CE. A review and synthesis of the measurement invariance literature: suggestions, practices, and recommendations for organizational research. Organ Res Methods. (2000) 3:4–70. doi: 10.1177/109442810031002
40. Brown, GT, Harris, LR, O'Quin, C, and Lane, KE. Using multi-group confirmatory factor analysis to evaluate cross-cultural research: identifying and understanding non-invariance. Int J Res Method Educ. (2017) 40:66–90. doi: 10.1080/1743727X.2015.1070823
41. Han, K, Colarelli, SM, and Weed, NC. Methodological and statistical advances in the consideration of cultural diversity in assessment: a critical review of group classification and measurement invariance testing. Psychol Assess. (2019) 31:1481–96. doi: 10.1037/pas0000731
42. Roberts, C, Zoanetti, N, and Rothnie, I. Validating a multiple mini-interview question bank assessing entry-level reasoning skills in candidates for graduate-entry medicine and dentistry programmes. Med Educ. (2009) 43:350–9. doi: 10.1111/j.1365-2923.2009.03292.x
43. Barbour, ME, and Sandy, JR. Multiple mini interviews for selection of dental students: influence of gender and starting station. J Dent Educ. (2014) 78:589–96. doi: 10.1002/j.0022-0337.2014.78.4.tb05710.x
44. Jerant, A, Griffin, E, Rainwater, J, Henderson, M, Sousa, F, Bertakis, KD, et al. Does applicant personality influence multiple mini-interview performance and medical school acceptance offers? Acad Med. (2012) 87:1250–9. doi: 10.1097/ACM.0b013e31826102ad
45. Reiter, HI, Lockyer, J, Ziola, B, Courneya, CA, and Eva, K. Canadian multiple mini-interview research alliance (CaMMIRA). Should efforts in favor of medical student diversity be focused during admissions or farther upstream? Acad Med. (2012) 87:443–8. doi: 10.1097/ACM.0b013e318248f7f3
46. Says, FE, Ayuob, N, Fahmy, AR, Fayez, FE, Hasanian, M, and El Deek, B. Experience of establishment of multiple mini structure interview as part of student admission policy at faculty of medicine, king Abdulaziz university, 2011–2012. Med Teach. (2013) 35:S74–7. doi: 10.3109/0142159X.2013.765543
47. Jerant, A, Henderson, MC, Griffin, E, Hall, TR, Kelly, CJ, Peterson, EM, et al. Do admissions multiple mini-interview and traditional interview scores predict subsequent academic performance? A study of five California medical schools. Academic Medicine: Journal of the Association of American Medical Colleges. (2019) 94:388–395. doi: 10.1097/ACM.0000000000002440
Keywords: admission processes, selection processes, diversity and inclusion, gender, equity, medical education, medical school admission
Citation: Szkwara JM, Bannatyne AJ, Asil M, Craig B, Stokes-Parish J and Bishop J (2025) Leveling the playing field: evaluating measurement equivalence in MMIs between genders. Front. Med. 12:1639532. doi: 10.3389/fmed.2025.1639532
Edited by:
Julie Willems, Monash University, AustraliaReviewed by:
Jeff Bolles, Francis Marion University, United StatesDeborah Verran, Consultant, Sydney, NSW, Australia
Huiming Ding, University of Leeds, United Kingdom
Copyright © 2025 Szkwara, Bannatyne, Asil, Craig, Stokes-Parish and Bishop. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jaclyn Michele Szkwara, amFzemt3YXJAYm9uZC5lZHUuYXU=
†These authors have contributed equally to this work and share first authorship
 Jaclyn Michele Szkwara
Jaclyn Michele Szkwara Amy Jean Bannatyne
Amy Jean Bannatyne Mustafa Asil
Mustafa Asil Belinda Craig
Belinda Craig Jessica Stokes-Parish
Jessica Stokes-Parish Jo Bishop
Jo Bishop