Abstract
Objective:
To investigate the impact of preoperative grip strength on early postoperative recovery, functional outcomes, and prognosis in elderly patients with intertrochanteric fractures.
Methods:
A retrospective cohort study was conducted on 195 elderly patients who underwent closed reduction and intramedullary nailing for intertrochanteric fractures between January 2018 and December 2022. Based on EWGSOP2 cut-off values (men < 27 kg, women < 16 kg), patients were classified into a high grip strength group (n = 110) and a low grip strength group (n = 85). Data on baseline characteristics, perioperative indicators (postoperative hemoglobin, transfusion volume, time to ambulation, length of hospital stay), postoperative follow-up outcomes (Harris Hip Score, SF-36 quality of life score), as well as postoperative complications and 1-year all-cause mortality were collected and compared between the two groups.
Results:
The baseline characteristics were comparable between the two groups (P > 0.05). Compared to the high grip strength group, the low grip strength group had significantly lower postoperative hemoglobin levels (7.7 ± 3.4 vs. 9.2 ± 4.1 g/dL, P = 0.014), greater postoperative transfusion volume (78.9 ± 44.2 vs. 45.1 ± 26.8 ml, P = 0.025), longer time to ambulation (4.2 ± 2.5 vs. 2.5 ± 1.8 days, P = 0.034), and extended hospital stay (14.2 ± 3.5 vs. 10.4 ± 4.6 days, P = 0.041). At the 6- and 12-month follow-ups, the low grip strength group showed significantly worse Harris Hip Scores and SF-36 scores across all domains (all P < 0.05). Furthermore, the incidence of postoperative complications—including pneumonia (9 vs. 4, P = 0.033), deep vein thrombosis (6 vs. 4, P = 0.010), pressure ulcers (3 vs. 1, P = 0.018), urinary tract infections (4 vs. 2, P = 0.029), and internal fixation loosening (3 vs. 1, P = 0.005)—was significantly higher in the low grip strength group. The 1-year all-cause mortality was also significantly higher in the low grip strength group (4 vs. 2, P = 0.040).
Conclusion:
Preoperative grip strength is an effective predictor of postoperative prognosis in elderly patients with intertrochanteric fractures. Low grip strength is significantly associated with greater hidden blood loss, a higher incidence of complications, poorer functional recovery, and increased mortality. Incorporating grip strength assessment into the preoperative evaluation and developing targeted rehabilitation strategies may help improve patient outcomes.
Introduction
Intertrochanteric fractures are among the most common osteoporotic fractures in the elderly, with incidence increasing progressively with age, particularly in individuals aged 65 years and older (1–3). These fractures typically result from low-energy trauma such as falls and are associated with high rates of disability and mortality (4). They significantly impair patients’ quality of life and impose a substantial burden on healthcare resources (5, 6). With the global aging of the population, the incidence of intertrochanteric fractures is expected to rise further (7). Therefore, accurate prognostic assessment and individualized treatment and rehabilitation planning are crucial in clinical practice.
Surgical intervention remains the mainstay of treatment for intertrochanteric fractures. However, postoperative recovery is influenced by multiple factors, including age, sex, bone density, and comorbidities (8–10). The patient’s overall health status, functional capacity, and physiological reserves also play critical roles. Commonly used prognostic tools such as body mass index (BMI), bone mineral density (BMD), and the Charlson Comorbidity Index offer some reference value (11–13). Yet, these indicators do not fully capture the patient’s functional status, particularly in the postoperative period, and often fail to provide effective guidance. Thus, there is a pressing need for a simple, effective, and quantifiable tool for preoperative and postoperative prognostic assessment to aid clinicians in optimizing treatment and rehabilitation strategies.
Grip strength, an important indicator of muscle strength and overall health, has gained increasing attention in geriatric orthopedics (14–16). Declines in grip strength are significantly correlated with frailty, fall risk, hospitalization rates, and mortality (17). Studies have shown that grip strength is related not only to muscle strength, physical function, and balance, but also to metabolic and immune function (18, 19). As a simple, non-invasive, and highly reproducible measure, grip strength is increasingly recognized for its utility in postoperative monitoring and rehabilitation assessment in elderly fracture patients. Growing evidence suggests that grip strength reflects both muscle mass and overall physiological condition (20, 21). Thus, grip strength measurement can provide valuable information for preoperative and postoperative prognostic evaluation. Changes in grip strength are significantly associated with postoperative recovery, functional outcomes, and long-term quality of life (22–24). In elderly populations, early assessment of grip strength is essential for developing individualized rehabilitation plans, monitoring functional recovery, and preventing complications (25, 26).
This study aims to investigate the impact of grip strength on the prognosis of elderly patients with intertrochanteric fractures, specifically examining its relationship with postoperative recovery, functional outcomes, and long-term quality of life. We seek to provide evidence supporting the use of grip strength as a prognostic tool in clinical practice, thereby aiding in the optimization of postoperative management and ultimately improving patient outcomes and quality of life.
Materials and methods
This retrospective study included 210 elderly patients (aged ≥ 65 years) who underwent closed reduction and intramedullary nailing for intertrochanteric fractures between January 2018 and December 2022. The electronic medical records (EMR) of all identified patients were then individually and rigorously screened by two independent researchers against the pre-defined inclusion and exclusion criteria. The detailed screening process and reasons for exclusion are illustrated in the participant flow diagram (Figure 1). Inclusion criteria were: (1) diagnosis of unilateral intertrochanteric femoral fracture; (2) treatment with closed reduction and intramedullary nailing; (3) able to comprehend and cooperate with the grip strength measurement procedure, as determined by a Mini-Mental State Examination (MMSE) score of ≥ 18; and (4) injury resulting from a low-energy fall. Exclusion criteria were: Exclusion criteria were: (1) severe neuromuscular disease or limb dysfunction affecting grip strength measurement; (2) multiple fractures or other severe trauma; (3) high-energy trauma (e.g., motor vehicle accidents or falls from height); (4) severe cognitive impairment, defined as an MMSE score < 18, and 5) incomplete or missing follow-up data.
FIGURE 1

The participant flowchart and research process.
Grip strength was measured using a calibrated Jamar dynamometer (Carmy EH101). To control for pain variation and its potential impact on grip strength, measurements were taken only after the patient’s acute pain was adequately controlled with analgesic medications. Pain intensity was assessed using a 0–10 numerical rating scale (NRS), and measurements were performed only when the pain score was < 4. The type, dosage, and timing of analgesic administration (e.g., non-steroidal anti-inflammatory drugs or opioids) were systematically recorded to ensure consistency and to account for potential effects on muscle function. Additionally, upper limb edema was assessed, and cases with hand or wrist edema were excluded from the final analysis to avoid confounding factors. Patients were seated with the elbow flexed at 90°and forearm in a neutral position. The dominant hand was tested, beginning with one practice trial followed by three formal measurements, with rest intervals of at least 60 s between trials. The mean value of the three measurements was used for analysis. The assessment followed the standardized protocol recommended by the American Society of Hand Therapists. Based on EWGSOP2 guidelines (27), patients were classified into high or low grip strength groups using cutoffs of 16 kg for females and 27 kg for males. Baseline data collected included age, sex, and BMI. To assess participants’ baseline frailty and pre-injury physical function, the following parameters were evaluated: preoperative mobility level (categorized as unassisted outdoors, assist outdoors/unassisted indoors, indoor assistance, or unable to walk), the Barthel Index (as a measure of activities of daily living), and the Charlson Comorbidity Index (as a measure of comorbidity burden). Fracture type was classified according to the AO/OTA system. Surgical parameters recorded were time to surgery, preoperative hemoglobin level, preoperative albumin level, operative time, intraoperative blood loss, postoperative hemoglobin level, transfusion volume, time to ambulation, and length of stay. Postoperative outcomes included Harris Hip Score, quality of life (SF-36), postoperative complications (e.g., pneumonia, urinary tract infection, deep vein thrombosis, pressure sores), implant-related complications, and 1-year all-cause mortality.
Surgical procedure
Following successful spinal anesthesia, the patient was placed supine on a traction table. Under C-arm fluoroscopy, closed reduction with traction was performed to achieve satisfactory fracture alignment. After standard skin preparation and draping, a 4 cm longitudinal incision was made over the tip of the greater trochanter. The entry point was exposed, and a guidewire was inserted. After confirming correct placement fluoroscopically, the femoral canal was reamed. An appropriately sized intramedullary nail was inserted, and a guidewire was placed into the femoral neck using a targeting device under fluoroscopic guidance, ensuring central placement in the femoral head and neck with the tip reaching the subchondral bone. A spiral blade was inserted and locked, followed by percutaneous placement of a distal locking screw. Intraoperative fluoroscopy confirmed satisfactory fracture reduction, appropriate implant position and depth, and absence of joint penetration. Cases with favorable healing outcomes during follow-up are presented in Figures 2, 3.
FIGURE 2

Radiographic follow-up of a patient from the lowgrip strength group. (A) Preoperative radiograph showing a left intertrochanteric fracture. (B,C) Postoperative radiographs at 2 days. (D) Radiograph at 3 months showing callus formation and early union. (E) Radiograph at 12 months confirming complete fracture healing.
FIGURE 3

Radiographic follow-up of a patient from the high grip strength group. (A) Preoperative radiograph showing a left intertrochanteric fracture. (B,C) Postoperative radiographs at 2 days. (D,E) Radiographs at 6 months showing advanced fracture healing. (F,G) Radiographs at 12 months confirming complete fracture union.
Perioperative management
All patients received prophylactic antibiotics 30 min before surgery and for 48 h postoperatively. Postoperative pain was managed with short-term non-steroidal anti-inflammatory drugs (NSAIDs). Low molecular weight heparin was administered for deep vein thrombosis prophylaxis based on Autar scores. Patients were encouraged to mobilize early with walking aids, and both groups participated in early rehabilitation under the guidance of a physical therapist.
Postoperative complication diagnosis and verification
Pneumonia: Diagnosed per CDC criteria, requiring new pulmonary infiltrates on imaging plus at least two supporting clinical symptoms. Deep Vein Thrombosis (DVT): Confirmed by compression duplex ultrasonography performed by a certified radiologist. Pressure Injury: Assessed and staged daily by nursing staff using the Braden Scale and NPUAP staging system. Urinary Tract Infection (UTI): Diagnosed based on a positive urine culture, pyuria, and relevant clinical symptoms. Implant Loosening: Defined as a progressive radiolucent line > 2 mm around the implant or a clear change in position on serial radiographs, assessed by two independent orthopedic surgeons. (Typical cases of implant loosening are shown in Figures 4, 5.
FIGURE 4

Implant-related complication (screw cut-out) in a patient from the low grip strength group. (A,B) Preoperative radiographs showing a right intertrochanteric fracture. (C,D) Postoperative radiographs at 2 days. (E,F) Follow-up radiographs at 12 months demonstrating fracture healing with concomitant femoral neck shortening and partial screw cut-out (arrow).
FIGURE 5
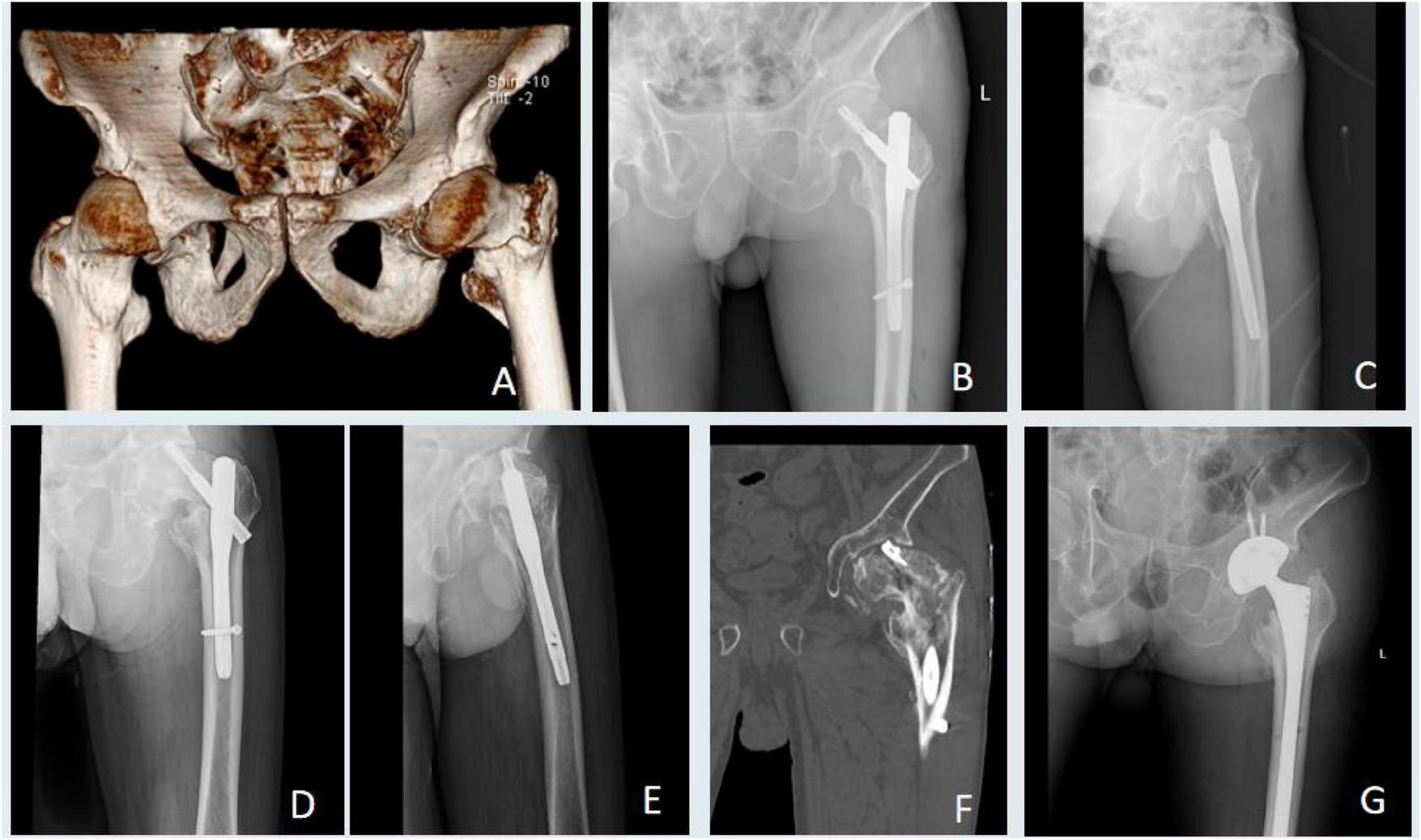
Management of a major implant failure in a patient from the low grip strength group. (A) Preoperative radiograph showing a left intertrochanteric fracture. (B,C) Postoperative radiographs at 2 days. (D–F) Radiographs at 6 months revealing implant cut-out and failure. (G) Radiograph after implant removal and subsequent total hiparthroplasty.
Functional outcome assessment
Functional outcomes, including the Harris Hip Score and the SF-36 quality of life survey, were assessed at 6 and 12 months postoperatively. All assessments were conducted by a dedicated research physical therapist who was blinded to the patients’ grip strength group allocation. A standardized protocol was followed for the administration of the HHS, which included a structured interview and a physical examination of hip function. The SF-36 was self-administered by patients in a quiet environment with assistance available if required for clarification.
Sample size and statistical analysis
A priori power analysis (G*Power; repeated-measures ANOVA, α = 0.05, power = 0.9) determined that 45 patients per group were required to detect differences in functional outcomes. The final sample size (High: n = 110; Low: n = 85) exceeded this requirement, ensuring adequate statistical power. Data were analyzed using SPSS version 23.0 (IBM Corp., Armonk, NY, United States). For the primary analysis of functional outcomes (Harris Hip Score and SF-36), a complete-case analysis was initially employed. A worst-case scenario sensitivity analysis was performed for patients who died or required revision surgery, assigning the worst possible scores (0 for HHS and SF-36) from the time of the event onward. A complete-case analysis was employed as the data missing rate for all variables was very low (< 2%) and judged to be missing completely at random (MCAR). Continuous variables were compared using Independent Samples t-test or Mann-Whitney U test, and categorical variables using Chi-square or Fisher’s exact test. To control for potential confounders, Harris Hip Score were further analyzed using multivariable logistic regression. Models were adjusted for age, sex, Charlson Comorbidity Index, and preoperative albumin level. A p < 0.05 was considered statistically significant.
Results
A total of 195 patients were included in the final analysis: 110 in the high grip strength group and 85 in the low grip strength group. Baseline characteristics did not differ significantly between groups (P > 0.05) (Table 1). Preoperative hemoglobin, Preoperative albumin level, operative time, and intraoperative blood loss were also comparable (P > 0.05). However, significant differences were observed in postoperative hemoglobin levels, transfusion volume, time to ambulation, and length of stay (P < 0.05) (Table 2). At 6 and 12 months postoperatively, both Harris Hip Scores and SF-36 scores showed statistically significant differences between groups in the complete-case analysis (Table 3). To address potential bias from missing data, a worst-case scenario sensitivity analysis was conducted. This analysis included imputing the worst possible outcomes for patients who died or developed major complications before assessment. The results of this sensitivity analysis corroborated the primary findings, with all functional outcomes remaining significantly better in the high grip strength group at 12 months (all p < 0.05). Several postoperative complications also differed significantly (P < 0.05), as did the 1-year all-cause mortality rate (P < 0.05) (Table 4). Multivariate regression identified that higher grip strength, a lower Charlson Comorbidity Index (CCI) score, and a higher pre-fracture Barthel Index were independent predictors of a higher Harris Hip Score at 12 months postoperatively (P < 0.05) (Table 5).
TABLE 1
| High grip strength (n = 110) | Low grip strength (n = 85) | P-value | |
|---|---|---|---|
| Age (years) | 76.1 ± 7.9 | 78.4 ± 10.2 | 0.670 |
| Gender (male/female) | 34/76 | 23/62 | 0.125 |
| BMI (kg/m2) | 23.0 ± 3.8 | 21.9 ± 5.7 | 0.516 |
| Barthel index (before injury) | 77.9 ± 25.3 | 75.5 ± 31.2 | 0.074 |
| CCI groups | |||
| No comorbidity/mild | 38 | 30 | 0.258 |
| Moderate | 66 | 51 | 0.680 |
| Severe | 6 | 4 | 0.097 |
| AO/OTA classification | |||
| 31A1 | 74 | 55 | 0.895 |
| 31A2 | 28 | 23 | 0.319 |
| 31A3 | 8 | 7 | 0.452 |
| Mobility level prior to fracture | |||
| Unassisted outdoors | 68 | 52 | 0.090 |
| Assist outdoors, unassisted indoors | 31 | 24 | 0.685 |
| Indoor assistance | 10 | 8 | 0.217 |
| Unable to walk | 1 | 1 | 0.087 |
Comparison of baseline characteristics of patients.
TABLE 2
| High grip strength (n = 110) | Low grip strength (n = 85) | P-value | |
|---|---|---|---|
| Surgery waiting time | |||
| 48–72 h | 53 | 40 | 0.771 |
| <24 h | 25 | 21 | 0.215 |
| >72 h | 32 | 24 | 0.931 |
| Preoperative indicators | |||
| Preoperative hemoglobin (g/dL) | 11.5 ± 3.8 | 11.1 ± 4.5 | 0.482 |
| Preoperative albumin (g/dL) | 3.8 ± 0.82 | 3.6 ± 0.69 | 0.102 |
| Operation time (min) | 34.5 ± 15.2 | 32.1 ± 12.7 | 0.142 |
| Intraoperative blood loss (mL) | 25.9 ± 21.2 | 23.2 ± 22.8 | 0.228 |
| Postoperative indicators | |||
| Postoperative hemoglobin (g/dL) | 9.2 ± 4.1 | 7.7 ± 3.4 | 0.014 |
| Postoperative blood transfusion volume (mL) | 45.1 ± 26.8 | 78.9 ± 44.2 | 0.025 |
| Time to ambulation (days). | 2.5 ± 1.8 | 4.2 ± 2.5 | 0.034 |
| Hospital stay (days). | 10.4 ± 4.6 | 14.2 ± 3.5 | 0.041 |
Comparison of perioperative indexes.
TABLE 3
| High grip strength (n = 110) | Low grip strength (n = 85) | P-value | |
|---|---|---|---|
| Harris Hip Score | |||
| 6 months postoperatively | 72.7 ± 8.6 | 65.2 ± 10.8 | 0.019 |
| 12 months postoperatively | 80.5 ± 5.9 | 72.8 ± 8.7 | 0.021 |
| SF-36 quality of life score | |||
| SF-36 physical health | |||
| 6 months postoperatively | 30.8 ± 3.6 | 28.5 ± 4.4 | 0.037 |
| 12 months postoperatively | 35.4 ± 2.7 | 31.8 ± 4.8 | 0.016 |
| SF-36 mental health | |||
| 6 months postoperatively | 32.5 ± 4.8 | 30.8 ± 5.3 | 0.023 |
| 12 months postoperatively | 35.9 ± 4.2 | 33.7 ± 4.1 | 0.008 |
Comparison of postoperative follow-up.
TABLE 4
| High grip strength (n = 110) | Low grip strength (n = 85) | P-value | |
|---|---|---|---|
| Postoperative complications | |||
| Pneumonia | 4 | 9 | 0.033 |
| Deep vein thrombosis | 4 | 6 | 0.040 |
| Pressure ulcers | 1 | 3 | 0.038 |
| Urinary tract infections | 2 | 4 | 0.029 |
| Implant loosening | 1 | 3 | 0.015 |
| All-cause rate within 1 year after surgery | 2 | 4 | 0.042 |
Comparison of postoperative complications and all-cause mortality.
TABLE 5
| Predictors | Univariate analysis | Multivariate analysis | ||
|---|---|---|---|---|
| β (95% CI) | p-value | β (95% CI) | p-value | |
| Age | −0.13(−4.25 to 2.44) | 0.106 | ||
| BMI | −0.12(−12.26 to 1.02) | 0.073 | ||
| CCI | −1.50 (−2.20 to 0.89) | <0.001 | −1.20 (−1.92 to 0.54) | 0.018 |
| Barthel index (before injury) | 0.32 (0.15 to 0.49) | < 0.001 | 0.25 (0.08, 0.42) | 0.030 |
| Fracture classification | 0.23(0.14 to 4.03) | 0.029 | 0.36(−0.22 to 3.48) | 0.503 |
| HGS | 0.25 (0.11 to 0.49) | <0.001 | 0.22 (0.07 to 0.37) | < 0.001 |
| Surgery waiting time | −0.23 (−0.70 to 0.24) | 0.073 | ||
| Preoperative hemoglobin | 0.63(−3.93 to 7.81) | 0.598 | ||
| Preoperative albumin level | −0.05(−1.78 to 0.77) | 0.326 | ||
| Operation time | 0.23(−1.83 to 3.49) | 0.073 | ||
| Time to ambulation | 0.06(−4.91 to 12.82) | 0.314 | ||
| Hospital stay | −0.15(−0.82 to 0.09) | 0.467 | ||
Univariate and multivariate analysis for variables significantly associated with 12 months postoperatively Harris Hip Score.
Discussion
Declines in muscle strength significantly impair the body’s ability to recover from injury, including surgical trauma. Sarcopenia has increasingly been recognized as a predictor of surgical outcomes and is associated with postoperative complications and mortality in geriatric orthopedic patients (28–30). Traditional methods for assessing sarcopenia are often complex and impractical for routine clinical use. This study employs grip strength as a simple, convenient, and clinically feasible surrogate for sarcopenia evaluation.
Covert blood loss is a common yet frequently overlooked issue after intertrochanteric fracture surgery, with important implications for recovery. We found that patients with low grip strength had greater covert blood loss and required more postoperative transfusions. While previous studies have identified factors such as BMI, operative time, fracture type, and medication use as influencers of covert blood loss (31, 32). However, our study identified a significant association between grip strength, and covert blood loss as well as postoperative transfusion requirements in elderly patients with intertrochanteric fractures. A study indicated that elderly patients with significantly lower preoperative grip strength in intertrochanteric fracture surgery had an average increase of 15–20% in covert blood loss, along with a marked increase in transfusion requirements. Further analysis revealed that these patients experienced a more significant decline in postoperative hemoglobin levels, with a notably longer recovery time to preoperative levels (33). This suggests that lower grip strength is not only directly related to postoperative blood loss but may also affect the speed of recovery in the blood system. Similar findings were reported in a study on hip arthroplasty, where patients with low grip strength had a significantly higher transfusion rate compared to those with normal grip strength (12.5% vs. 24.4%) (34). Another study on sarcopenia and femoral proximal fractures found that lower total body muscle density was associated with higher transfusion requirements, indicating a link between sarcopenia and the need for transfusions (35). The underlying mechanisms may involve the systemic physiological decline associated with low grip strength. A weakened metabolic and inflammatory profile could exacerbate the pathophysiological processes of covert blood loss, such as capillary leakage and impaired coagulation function, thereby increasing postoperative transfusion demands (36, 37). The reason for the increased transfusion demand in patients with low grip strength may be due to a weakened overall metabolic function and altered inflammatory status, which increase the risk of capillary leakage and blood loss.
One of the findings of this study is the association between postoperative DVT incidence and grip strength. A multicenter retrospective study indicated that patients with lower grip strength have a 40% increased risk of developing DVT, particularly in the early postoperative phase (38). An association between lower grip strength and an increased incidence of postoperative deep vein thrombosis (DVT) was another key finding. This can be interpreted as a clinical manifestation of underlying sarcopenia. The systemic muscle weakness it entails likely impairs the calf muscle pump, reducing venous return and creating stasis in the lower limbs (39). Another major factor is the inflammatory response and endothelial dysfunction. Low grip strength is a marker of sarcopenia and is closely associated with an enhanced systemic inflammatory state (40). Elevated levels of inflammatory markers have been shown to increase the risk of thrombus formation. Inflammatory factors can also induce endothelial dysfunction, disrupting normal blood flow and promoting thrombosis (41).
Postoperative functional recovery is a crucial goal for elderly patients with intertrochanteric fractures. Our data demonstrate a significant correlation between preoperative grip strength and functional outcomes, as measured by the Harris Hip Score and SF-36. This association can be explained by several factors. Patients with greater grip strength, indicative of overall robustness, likely possess better lower limb strength and balance, facilitating safer and earlier ambulation. Furthermore, they may exhibit greater resilience and adherence to postoperative rehabilitation protocols, thereby optimizing their functional recovery (42, 43). This may be related to better muscle coordination and psychological resilience in patients with higher grip strength. Conversely, patients with lower grip strength are more prone to functional impairments after surgery, especially gait abnormalities and balance deficits, which restrict their daily activities. Grip strength may also influence patients’ adherence to rehabilitation training. Patients with higher grip strength are generally more capable of completing postoperative physical therapy and exercise regimens, whereas those with lower grip strength may interrupt rehabilitation due to fatigue, pain, or lack of motivation (44). When interpreting the statistical significance of individual complications listed in Table 4, caution is warranted due to the low incidence rates of some events. For certain complications, such as pressure ulcers and implant loosening, the absolute differences between groups, although statistically significant (P < 0.05), are based on a small number of events (e.g., 1 vs. 3). In such cases, the p-value, while indicative of a potential association, should not be overinterpreted regarding its clinical impact without support from larger studies. Therefore, the findings for these specific low-incidence complications should be considered exploratory and hypothesis-generating. The principal conclusion from our analysis of postoperative complications is not reliant on any single outcome but rather on the consistent and robust trend observed across multiple domains, indicating a higher overall burden of complications in the low grip strength group. Studies have indicated that the interruption rate of postoperative rehabilitation is significantly higher in patients with low grip strength, which may further worsen their postoperative functional recovery outcomes (45). The lower incidence of postoperative complications in our cohort compared to some literature may reflect our stringent diagnostic criteria requiring objective confirmation, implementation of a standardized perioperative care protocol, and the exclusion of patients with severe cognitive impairment—potentially selecting a healthier patient population.
Grip strength, as a comprehensive indicator of overall health, is closely related to patients’ prognosis. This study demonstrates that patients with lower preoperative grip strength have a significantly higher 1-year all-cause mortality rate and a higher incidence of implant failure. Similar studies have reported that the 1-year mortality rate for patients with low grip strength is 20%, compared to only 10% for those with normal grip strength (46). This result is thought to be closely associated with malnutrition and an inflammatory state in patients with low grip strength. Furthermore, this study found that patients with lower grip strength are more prone to implant failure. Some studies suggest that grip strength is closely related to overall muscle strength, particularly the strength of the upper limbs and core muscles (20, 47). Muscle weakness can impair balance and coordination, increasing stress on the implant, and thereby increasing the probability of implant failure. Other studies indicate that a decline in grip strength is a common manifestation of sarcopenia, which is associated with delayed fracture healing and an increased risk of complications (48–50). Therefore, patients with lower grip strength may face a higher risk of implant failure.
Although the aforementioned studies have provided several new insights, this study has some limitations. First, the sample size in this study is relatively small, which may affect the generalizability of the results. Future research could involve larger sample sizes, multicenter, and prospective studies to further validate the causal relationship between grip strength and the outcomes of elderly patients with intertrochanteric fractures. A further limitation is potential bias from informative censoring. Future studies should use advanced methods like mixed-effects models to handle missing data. While multivariable models were used to control for potential confounders, residual confounding from unmeasured factors (e.g., specific medication details) inherent to observational studies cannot be completely excluded.
Conclusion
There were significant differences in postoperative hip function (Harris score) and quality of life (SF-36 score) between the high and low grip strength groups. The high grip strength group had a lower incidence of postoperative complications and a significantly lower all-cause mortality rate compared to the low grip strength group. A specially designed rehabilitation training program, implemented both preoperatively and postoperatively, may effectively improve patients’ grip strength, thereby enhancing the overall postoperative recovery of patients with intertrochanteric fractures.
Statements
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Jiujiang University Affiliated Hospital Ethics Committee. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
LZ: Investigation, Writing – original draft, Supervision, Writing – review & editing, Formal analysis. XS: Writing – original draft, Investigation, Data curation, Writing – review & editing, Formal analysis. HW: Writing – review & editing, Writing – original draft, Investigation, Formal analysis. BH: Writing – review & editing. KS: Project administration, Conceptualization, Supervision, Funding acquisition, Writing – review & editing, Writing – original draft.
Funding
The author(s) declared that financial support was received for this work and/or its publication. This work was supported by the Science and Technology Program of Health Commission of Jiangxi Province (No. 202311519) and Key Research and Development Plan of Jiujiang (No. S2022ZDYFN337).
Conflict of interest
The author(s) declared that this work was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declared that generative AI was not used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
Zhang Z Qiu Y Zhang Y Zhu Y Sun F Liu J et al Global trends in intertrochanteric hip fracture research from 2001 to 2020: a bibliometric and visualized study. Front Surg. (2021) 8:756614. 10.3389/fsurg.2021.756614
2.
Sing C Lin T Bartholomew S Bell J Bennett C Beyene K et al Global epidemiology of hip fractures: secular trends in incidence rate, post-fracture treatment, and all-cause mortality. J Bone Miner Res. (2023) 38:1064–75. 10.1002/jbmr.4821
3.
Lakstein D Oren N Haimovich Y Kharchenkov V . Evolving trends in hip fracture patterns among the elderly from 2001 to 2022.Injury. (2024) 55:111279. 10.1016/j.injury.2023.111279
4.
Babagoli M Ghaseminejad Raeini A Sheykhvatan M Baghdadi S Shafiei S . Influencing factors on morbidity and mortality in intertrochanteric fractures.Sci Rep. (2023) 13:12090. 10.1038/s41598-023-38667-9
5.
Behanova M Haschka J Zwerina J Wascher T Reichardt B Klaushofer K et al The doubled burden of diabetic bone disease: hip fracture and post-hip fracture mortality. Eur J Endocrinol. (2021) 184:627–36. 10.1530/EJE-20-1155
6.
Veronese N Maggi S . Epidemiology and social costs of hip fracture.Injury. (2018) 49:1458–60. 10.1016/j.injury.2018.04.015
7.
Ebeling P . Hip fractures and aging: a global problem requiring coordinated global solutions.J Bone Miner Res. (2023) 38:1062–3. 10.1002/jbmr.4881
8.
Takegami Y Osawa Y Funahashi H Asamoto T Ido H Otaka K et al One-year survival and postoperative complications in older patients with intertrochanteric fractures: association with polypharmacy-a multicenter retrospective cohort study. Drugs Aging. (2025) 42:435–44. 10.1007/s40266-025-01194-5
9.
He M Liu J Deng X Zhang X . The postoperative prognosis of older intertrochanteric fracture patients as evaluated by the Chang reduction quality criteria.BMC Geriatr. (2022) 22:928. 10.1186/s12877-022-03641-z
10.
Yu X Li Y Lu H Ao R Liu B . Analysis of factors affecting the surgical efficacy for elderly intertrochanteric fracture.Front Surg. (2025) 12:1589181. 10.3389/fsurg.2025.1589181
11.
Zhang D Cong Y Zhuang Y Xu X Zhang B . Age-adjusted Charlson comorbidity index predicts postoperative mortality in elderly patients with hip fracture: a prospective cohort.Front Med. (2023) 10:1066145. 10.3389/fmed.2023.1066145
12.
Lu Y Huang Q Xu Y Ren C Sun L Dong W et al Predictors of long-term mortality after intertrochanteric fractures surgery: a 3-year retrospective study. BMC Musculoskelet Disord. (2022) 23:472. 10.1186/s12891-022-05442-2
13.
Han X Han L Chu F Liu B Song F Jia D et al Predictors for 1-year mortality in geriatric patients following fragile intertrochanteric fracture surgery. J Orthop Surg Res. (2024) 19:701. 10.1186/s13018-024-05219-4
14.
Kemala Sari N Stepvia S Ilyas M Setiati S Harimurti K Fitriana I . Handgrip strength as a potential indicator of aging: insights from its association with aging-related laboratory parameters.Front Med. (2025) 12:1491584. 10.3389/fmed.2025.1491584
15.
Güner M Ceylan S Okyar Baş A Koca M Öztürk Y Doğu B et al A hand-in-hand phenomenon in older adults: increased risk of frailty in geriatric outpatients associated with handgrip strength asymmetry and weakness. Clin Nutr. (2024) 43:2381–7. 10.1016/j.clnu.2024.09.010
16.
Meng F Zhang Y Liu C Zhou C . Quantitative relationship between grip strength and quality of life in the older adult based on a restricted cubic spline model.Front Public Health. (2024) 12:1417660. 10.3389/fpubh.2024.1417660
17.
Szulc P Feyt C Chapurlat R . High risk of fall, poor physical function, and low grip strength in men with fracture-the STRAMBO study.J Cachexia Sarcopenia Muscle. (2016) 7:299–311. 10.1002/jcsm.12066
18.
Leong D Teo K Rangarajan S Lopez-Jaramillo P Avezum A Orlandini A et al Prognostic value of grip strength: findings from the prospective urban rural epidemiology (PURE) study. Lancet. (2015) 386:266–73. 10.1016/S0140-6736(14)62000-6
19.
Sayer A Kirkwood T . Grip strength and mortality: a biomarker of ageing?Lancet. (2015) 386:226–7. 10.1016/S0140-6736(14)62349-7
20.
Bohannon R . Grip strength: an indispensable biomarker for older adults.Clin Interv Aging. (2019) 14:1681–91. 10.2147/CIA.S194543
21.
Peng T Chen W Wu L Chang Y Kao T . Sarcopenia and cognitive impairment: a systematic review and meta-analysis.Clin Nutr. (2020) 39:2695–701. 10.1016/j.clnu.2019.12.014
22.
Sidiras G Patsaki I Karatzanos E Dakoutrou M Kouvarakos A Mitsiou G et al Long term follow-up of quality of life and functional ability in patients with ICU acquired Weakness - A post hoc analysis. J Crit Care. (2019) 53:223–30. 10.1016/j.jcrc.2019.06.022
23.
Savino E Martini E Lauretani F Pioli G Zagatti A Frondini C et al Handgrip strength predicts persistent walking recovery after hip fracture surgery. Am J Med. (2013) 126:1068–75.e1. 10.1016/j.amjmed.2013.04.017
24.
Pei D Zhou H Zhou Q . Grip strength can be used to evaluate postoperative residual neuromuscular block recovery in patients undergoing general anesthesia.Medicine. (2019) 98:e13940. 10.1097/MD.0000000000013940
25.
Guasti L Fumagalli S Afilalo J Geisler T Abreu A Ambrosetti M et al Cardiovascular diseases, prevention, and management of complications in older adults and frail patients treated for elective or post-traumatic hip orthopaedic interventions: a clinical consensus statement of the ESC Council for Cardiology Practice (CCP), the European Association of Preventive Cardiology (EAPC), the Association for Acute CardioVascular Care (ACVC), the Association of Cardiovascular Nursing & Allied Professions of the ESC (ACNAP), the ESC Working Group on Aorta and Peripheral Vascular Diseases (WG APVD), and the ESC Working Group on Thrombosis (WG T). Eur J Prev Cardiol. (2025): 10.1093/eurjpc/zwaf010Online ahead of print.
26.
Jia Q Pan Y Pan D Xia Y Wu J . Application of comprehensive geriatric assessment in assessment, management and prognosis of older adult patients with sarcopenia: a review of research progress and practice.Gerontology. (2025) 71:955–68. 10.1159/000546715
27.
Cruz-Jentoft A Bahat G Bauer J Boirie Y Bruyère O Cederholm T et al Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. (2019) 48:16–31. 10.1093/ageing/afy169
28.
Chang K Albright J Testa E Balboni A Daniels A Cohen E . Sarcopenia is associated with an increased risk of postoperative complications following total hip arthroplasty for osteoarthritis.Biology. (2023) 12:295. 10.3390/biology12020295
29.
Chiang M Kuo Y Chen Y . The association between sarcopenia and postoperative outcomes among older adults with hip fracture: a systematic review.J Appl Gerontol. (2021) 40:1903–13. 10.1177/07334648211006519
30.
Kim Y Yi S Lee Y Kwon J Jang S Park S . Effect of sarcopenia on postoperative mortality in osteoporotic hip fracture patients.J Bone Metab. (2018) 25:227–33. 10.11005/jbm.2018.25.4.227
31.
Cui H Chen K Lv S Yuan C Wang Y . An analysis of perioperative hidden blood loss in femoral intertrochanteric fractures: bone density is an important influencing factor.BMC Musculoskelet Disord. (2021) 22:6. 10.1186/s12891-020-03922-x
32.
Guo J Zhang Y Hou Z . Intramedullary fixation does not cause a large amount of hidden blood loss in elderly patients with intertrochanteric fractures.Clin Interv Aging. (2021) 16:475–86. 10.2147/CIA.S301737
33.
Ji H Han J Bae H Won Y . Combination of measures of handgrip strength and red cell distribution width can predict in-hospital complications better than the ASA grade after hip fracture surgery in the elderly.BMC Musculoskelet Disord. (2017) 18:375. 10.1186/s12891-017-1738-3
34.
Long G Chao C Ming-Sheng T Ping Y . Low grip strength associated with clinical outcomes after total hip arthroplasty - a prospective case-control study.Orthop Surg. (2021) 13:1488–95. 10.1111/os.13007
35.
Chang C Wu J Mhuircheartaigh J Hochman M Rodriguez E Appleton P et al Effect of sarcopenia on clinical and surgical outcome in elderly patients with proximal femur fractures. Skeletal Radiol. (2018) 47:771–7. 10.1007/s00256-017-2848-6
36.
Shah A Palmer A Klein A . Strategies to minimize intraoperative blood loss during major surgery.Br J Surg. (2020) 107:e26–38. 10.1002/bjs.11393
37.
Ghadimi K Levy J Welsby I . Perioperative management of the bleeding patient.Br J Anaesth. (2016) 117:iii18–30. 10.1093/bja/aew358
38.
Leknessund O Morelli V Strand B Hansen J Brækkan S . Hand grip strength and risk of incident venous thromboembolism: the Tromsø study.Res Pract Thromb Haemost. (2022) 6:e12833. 10.1002/rth2.12833
39.
Larsson L Degens H Li M Salviati L Lee Y Thompson W et al Sarcopenia: aging-related loss of muscle mass and function. Physiol Rev. (2019) 99:427–511. 10.1152/physrev.00061.2017
40.
Tuttle C Thang L Maier A . Markers of inflammation and their association with muscle strength and mass: a systematic review and meta-analysis.Ageing Res Rev. (2020) 64:101185. 10.1016/j.arr.2020.101185
41.
Jeon Y Shin M Saini S Custodero C Aggarwal M Anton S et al Vascular dysfunction as a potential culprit of sarcopenia. Exp Gerontol. (2021) 145:111220. 10.1016/j.exger.2020.111220
42.
Harris M Brovman E Urman R . Clinical predictors of postoperative delirium, functional status, and mortality in geriatric patients undergoing non-elective surgery for hip fracture.J Clin Anesth. (2019) 58:61–71. 10.1016/j.jclinane.2019.05.010
43.
Sayer A Syddall H Martin H Dennison E Roberts H Cooper C . Is grip strength associated with health-related quality of life? Findings from the hertfordshire cohort study.Age Ageing. (2006) 35:409–15. 10.1093/ageing/afl024
44.
Wouters R Tsehaie J Hovius S Dilek B Selles R . Postoperative rehabilitation following thumb base surgery: a systematic review of the literature.Arch Phys Med Rehabil. (2018) 99:1177–212.e2. 10.1016/j.apmr.2017.09.114
45.
McGrath R Kraemer W Snih S Peterson M . Handgrip strength and health in aging adults.Sports Med. (2018) 48:1993–2000. 10.1007/s40279-018-0952-y
46.
Kwak Y Kim Y . Quality of life and subjective health status according to handgrip strength in the elderly: a cross-sectional study.Aging Ment Health. (2019) 23:107–12. 10.1080/13607863.2017.1387766
47.
Granacher U Gollhofer A Hortobágyi T Kressig R Muehlbauer T . The importance of trunk muscle strength for balance, functional performance, and fall prevention in seniors: a systematic review.Sports Med. (2013) 43:627–41. 10.1007/s40279-013-0041-1
48.
Oliveira A Vaz C . The role of sarcopenia in the risk of osteoporotic hip fracture.Clin Rheumatol. (2015) 34:1673–80. 10.1007/s10067-015-2943-9
49.
Wong R Wong H Zhang N Chow S Chau W Wang J et al The relationship between sarcopenia and fragility fracture-a systematic review. Osteoporos Int. (2019) 30:541–53. 10.1007/s00198-018-04828-0
50.
Greco E Pietschmann P Migliaccio S . Osteoporosis and Sarcopenia increase frailty syndrome in the elderly.Front Endocrinol. (2019) 10:255. 10.3389/fendo.2019.00255
Summary
Keywords
grip strength, intertrochanteric fractures, elderly patients, clinical outcomes, predictor, impact
Citation
Zhang L, Sun X, Wan H, Huang B and Sun K (2026) Impact of handgrip strength on postoperative recovery and prognosis in elderly patients with intertrochanteric fractures. Front. Med. 12:1724799. doi: 10.3389/fmed.2025.1724799
Received
14 October 2025
Revised
24 November 2025
Accepted
19 December 2025
Published
12 January 2026
Volume
12 - 2025
Edited by
Marios Kyriazis, National Gerontology Centre, Cyprus
Reviewed by
Silvio Pires Gomes, University of São Paulo, Brazil
Vahid Rashedi, University of Social Welfare and Rehabilitation Sciences, Iran
Updates
Copyright
© 2026 Zhang, Sun, Wan, Huang and Sun.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kai Sun, jjsunkai2024@163.com
†These authors have contributed equally to this work
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.