Abstract
Objective:
To systematically evaluate the efficacy of transcutaneous electrical acupoint stimulation (TEAS) in preventing postoperative delirium (POD) in elderly patients undergoing various surgical procedures.
Methods:
A comprehensive literature search was conducted across multiple electronic databases to identify randomized controlled trials (RCTs) comparing TEAS with control interventions (sham or no stimulation) in patients aged >60 years undergoing surgery. The primary outcome was the incidence of POD within the first seven postoperative days. Meta-analysis was performed using RevMan software, calculating risk ratios (RR), mean differences (MD), or standard MD with 95% confidence intervals (CIs). The quality of evidence was assessed based on the Grading of Recommendations Assessment, Development, and Evaluation approach.
Results:
Twenty RCTs involving 2,290 patients (aged >60 years) were included. The overall incidence of POD was 5.6% in the TEAS group compared to 17.0% in the control group (RR 0.34, 95% CI 0.26–0.45). TEAS also significantly reduced CAM score (MD −1.01, 95% CI −1.98 to −0.04), propofol consumption (MD −35.59 mg, 95% CI −65.75 to −5.42), postoperative pain score (MD −0.60, 95% CI −1.02 to −0.18), and improved recovery quality (QoR-15 score: MD 23.76, 95% CI 21.72–25.80). The intervention appeared safe with no serious adverse events reported.
Conclusion:
Perioperative TEAS application significantly reduces the risk of POD in elderly surgical patients. Its protective effects are potentially mediated through anti-inflammatory effects. TEAS represents a promising non-pharmacological intervention for POD prevention within enhanced recovery protocols.
Systematic review registration:
CRD420251128976.
Introduction
Postoperative delirium (POD) constitutes a prevalent and serious complication in elderly surgical patients, characterized by acute fluctuations in attention, awareness, and cognition (1, 2). Its incidence varies considerably, ranging from 15 to 50% depending on the type of surgery and patient vulnerability, and it is associated with devastating consequences, including prolonged hospitalization, increased healthcare costs, accelerated cognitive decline, higher morbidity and mortality rates, and elevated caregiver burden (3, 4). The aging global population has led to a rising number of elderly patients undergoing surgical interventions, making POD a critical public health concern that imperatively demands effective preventive strategies.
The pathophysiology of POD is multifactorial and not entirely elucidated, but it is widely recognized as a manifestation of cerebral vulnerability precipitated by the stress response to surgery and anesthesia (5). Key mechanistic contributors include neuroinflammation (6), increased permeability of the blood–brain barrier (7), oxidative stress (8), and neuronal injury (9). Current preventive approaches are primarily pharmacological, often involving antipsychotics or other psychoactive medications; however, their efficacy remains limited and their use is frequently associated with significant adverse effects, including sedation, and cardiovascular events (10, 11). This limited risk–benefit profile underscores the urgent need for safe, effective, and non-pharmacological adjunctive interventions.
Transcutaneous electrical acupoint stimulation (TEAS), a non-invasive modality derived from traditional acupuncture principles, applies electrical stimulation to specific acupoints through surface electrodes (12). It has gained increasing attention in perioperative medicine for its potential to modulate physiological functions, including analgesia, anti-emesis, attenuation of the surgical stress response, and organ protection (13–16). Emerging evidence from randomized controlled trials (RCTs) suggests that TEAS may confer protective effects against POD by modulating inflammatory cytokines (17), reducing markers of neuronal injury (18), improving sleep quality (19), and decreasing analgesic requirements (20). However, the findings across individual studies have been inconsistent, and the overall efficacy of TEAS for POD prevention has not been conclusively established due to variations in study design, patient populations, and TEAS protocols.
Therefore, we conducted this systematic review and meta-analysis of RCTs to synthesize the existing evidence and quantitatively evaluate the efficacy of TEAS in preventing POD in elderly patients undergoing surgery. We aimed to evaluate its effect on POD incidence and explore its impact on secondary outcomes including cognitive scores, pain, recovery quality, and key pathophysiological biomarkers.
Methods
This systematic review and meta-analysis was conducted and reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. The study protocol was registered prospectively on the International Prospective Register of Systematic Reviews (PROSPERO) (Registration number: CRD420251128976).
Search strategy and data sources
A comprehensive and systematic literature search was performed from inception until July 31, 2025 to identify all relevant published RCTs. The following electronic databases were searched: PubMed, Embase, Cochrane Central Register of Controlled Trials (CENTRAL), Web of Science, China National Knowledge Infrastructure (CNKI), Wanfang Data, and VIP Database. The full detailed search strategy, including all MeSH terms and free-text keywords used for each database, is provided in Supplementary material. In brief, the search concepts included terms related to the intervention (“transcutaneous electrical acupoint stimulation,” “TEAS,” “acupoint”) and the outcome (“postoperative delirium,” “POD,” “delirium”) combined with filters for RCTs and aged population. No language restrictions were applied. The reference lists of all included studies and relevant review articles were also manually screened to identify any additional eligible records.
Eligibility criteria
Studies were selected based on the following PICOS criteria: Population (P): Patients aged ≥60 years undergoing any elective surgical procedure. Intervention (I): Perioperative TEAS applied alone or as an adjunct to standard anesthesia care. Studies using any acupoint selection [e.g., Shenmen (HT7), Neiguan (PC6), Hegu (LI4)] and stimulation parameters were included. Comparison (C): Sham TEAS (electrodes placed at the same acupoints without electrical stimulation) or standard care/placebo. Outcomes (O): The primary outcome was the incidence of POD within the first seven postoperative days, diagnosed using validated tools such as the Confusion Assessment Method (CAM) or its variants. Secondary outcomes included CAM score, intraoperative propofol and remifentanil consumption, postoperative pain score, quality of recovery (QoR-15 score), levels of neuronal injury markers (TNF-α and NSE), and other adverse events (e.g., postoperative nausea and vomiting, PONV). Study Design (S): Only RCTs were included.
Study selection and data extraction
Two reviewers independently screened titles, abstracts, and subsequently full-text articles according to the eligibility criteria. Any discrepancies were resolved through discussion or by consultation with a third reviewer. A standardized pre-piloted data extraction form was used to collect information on: first author, publication year, sample size, patient characteristics, surgical type, TEAS protocol (acupoints, parameters, timing), control intervention, and outcomes of interest.
Risk of bias and quality assessment
The methodological quality of the included studies was assessed using the Cochrane Risk of Bias tool by two independent reviewers. The assessment covered domains of random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other potential biases. The overall certainty of evidence for each outcome was evaluated using the Grading of Recommendations, Assessment, Development, and Evaluations (GRADE) approach.
Data synthesis and statistical analysis
Statistical analysis was performed using Review Manager (RevMan) software (Version 5.4, The Cochrane Collaboration) and Stata software (Version 17.0). For dichotomous outcomes (e.g., POD incidence), the treatment effect was expressed as risk ratios (RR) with 95% confidence intervals (CIs). For continuous outcomes (e.g., pain score, biomarker levels), mean difference (MD) or standardized MD (SMD) were calculated with 95% CIs. Heterogeneity among studies was assessed using the I2 statistic and Chi-squared test. An I2 value > 50% indicated substantial heterogeneity. Considering multiple factors that contributed to the high clinical heterogeneity in this study, a random-effect model was utilized for the studies with low I2 values. Pre- specified subgroup analyses were conducted based on surgical type to explore potential sources of heterogeneity. Sensitivity analyses were performed to test the robustness of the results. Publication bias was assessed visually using funnel plots.
Results
Study selection
The initial systematic literature search identified a total of 391 records from all electronic databases and other sources. After removing duplicates, 178 unique records remained for title and abstract screening. Following this initial screening, 22 articles were selected for full-text review to assess their eligibility against the pre-defined PICOS criteria. After a detailed evaluation, 20 RCTs met all inclusion criteria and were included in the quantitative synthesis (meta-analysis) (17–36). The detailed process of study selection, with reasons for exclusion at the full-text stage, is presented in the PRISMA flow diagram (Figure 1).
Figure 1

PRISMA flow diagram.
Study characteristics
The 20 included studies enrolled a total of 2,290 patients, with sample sizes ranging from 57 to 547 participants. All studies involved elderly patients (age >60 years) undergoing various surgical procedures, including but not limited to hip fracture repair, laparoscopic cholecystectomy, radical thyroidectomy, and spinal open surgery. The baseline characteristics of included studies is shown in Table 1. The TEAS interventions utilized common acupoints, predominantly Shenmen (HT7), Neiguan (PC6), Hegu (LI4), and Zusanli (ST36). Stimulation parameters varied across studies, with frequencies often set at 2/100 Hz (dense-disperse mode) and intensity adjusted to patient tolerance (typically 6–15 mA). The control groups received either sham TEAS (placebo stimulation) or standard care. The primary outcome (POD incidence) was assessed using the CAM or its variants in all studies. A detailed summary of the characteristics of the included studies is provided in Table 2.
Table 1
| Study | Age (years) | Sample size | Gender (M/F) | ASA grade | Type of surgery | Duration of surgery | Type of anesthesia |
|---|---|---|---|---|---|---|---|
| Cao et al. (21) | >60 | TEAS: 60 Control: 60 |
TEAS: 29/31 Control: 32/28 |
I-II | Total hip replacement arthroplasty | TEAS: 52.8 ± 8.5 min Control: 52.6 ± 8.0 min |
Spinal anesthesia |
| Chang et al. (27) | 65–80 | TEAS: 44 Control: 41 |
TEAS: 24/20 Control: 26/15 |
II-III | Total hip arthroplasty | TEAS: 1.4 ± 0.5 h Control: 1.4 ± 0.4 h |
Spinal anesthesia |
| Ding et al. (18) | >60 | TEAS: 28 Control: 29 |
TEAS: 14/14 Control: 17/12 |
I-III | Pedicle internal fixation and bone-graft fusion | TEAS: 151 ± 32 min Control: 141 ± 25 min |
General anesthesia |
| Du et al. (29) | 66–80 | TEAS: 70 Control: 70 |
TEAS: 36/34 Control: 37/33 |
I-III | Radical resection of pulmonary carcinoma | TEAS: 162.43 ± 18.82 min Control: 165.65 ± 17.12 min |
General anesthesia |
| Gao et al. (17) | ≥65 | TEAS: 32 Control: 32 |
TEAS: 15/17 Control: 18/14 |
I-II | Spine surgery | TEAS: 136 ± 8 min Control: 134 ± 9 min |
General anesthesia |
| Ge et al. (20) | 60–80 | TEAS: 37 Control: 39 |
TEAS: 17/20 Control: 20/19 |
I-II | Total hip arthroplasty | TEAS: 60.0 ± 10.9 min Control: 57.2 ± 11.2 min |
Not mentioned |
| Liu (31) | 65–78 | TEAS: 60 Control: 60 |
TEAS: 42/18 Control: 40/20 |
II-III | Lobectomy for lung cancer | TEAS: 162.97 ± 18.73 min Control: 165.67 ± 16.82 min |
General anesthesia |
| Lu et al. (14) | ≥65 | TEAS: 39 Control: 39 |
TEAS: 8/31 Control: 9/30 |
II-III | Proximal femoral nail internal fixation | TEAS: 86.0 ± 24.1 min Control: 88.2 ± 30.9 min |
Intraspinal anesthesia |
| Qian et al. (36) | ≥65 | TEAS: 49 Control: 48 |
TEAS: 13/36 Control: 15/33 |
Not mentioned | Hip or knee joint replacement surgery | Not mentioned | General anesthesia or Intraspinal anesthesia |
| Shi et al. (28) | 65–78 | TEAS: 32 Control: 34 |
TEAS: 11/21 Control: 10/24 |
I-II | Spinal surgery | TEAS: 190.75 ± 37.47 min Control: 181.35 ± 31.36 min |
General anesthesia |
| Wang et al. (22) | >60 | TEAS: 88 Control: 86 |
TEAS: 31/57 Control: 41/45 |
I-III | Pedicle screw internal fixation |
TEAS: 1218.10 ± 45.69 min Control: 214.20 ± 34.10 min |
General anesthesia |
| Wei et al. (35) | ≥60 | TEAS: 41 Control: 42 |
TEAS: 6/35 Control: 4/38 |
I-III | Total knee replacement surgery | Not mentioned | General anesthesia |
| Wei et al. (24) | 65–80 | TEAS: 50 Control: 52 |
TEAS: 17/33 Control: 22/30 |
II-III | Hip replacement surgery | TEAS: 124 ± 32 min Control: 133 ± 37 min |
Combined spinal-epidural anesthesia or general anesthesia |
| Wen and Liang (32) | ≥60 | TEAS: 31 Control: 31 |
TEAS: 5/26 Control: 3/28 |
I-III | Radical thyroidectomy | Not mentioned | General anesthesia |
| Wu et al. (26) | 65–80 | TEAS: 30 Control: 30 |
TEAS: 18/12 Control: 17/13 |
II-III | Radical resection of gastrointestinal tumor | TEAS: 146 ± 20 min Control: 149 ± 21 min |
General anesthesia |
| Xu et al. (30) | >60 | TEAS: 35 Control: 35 |
TEAS: 20/15 Control: 13/22 |
I-III | Single-segment lumbar vertebral surgery | Not mentioned | General anesthesia |
| Yang et al. (25) | 61–85 | TEAS: 60 Control: 60 |
TEAS: 40/20 Control: 39/21 |
Not mentioned | Hip replacement surgery | Not mentioned | General anesthesia |
| Yu et al. (33) | 65–90 | TEAS: 32 Control: 32 |
TEAS: 12/20 Control: 11/21 |
I-II | Spinal open surgery | TEAS: 119.2 ± 9.2 min Control: 116.5 ± 6.5 min |
General anesthesia |
| Zhang et al. (19) | 65–79 | TEAS: 52 Control: 52 |
TEAS: 27/25 Control: 28/24 |
Not mentioned | Lower limb surgery | Not mentioned | Subarachnoid block |
| Zhang et al. (23) | >65 | TEAS: 273 Control: 274 |
TEAS: 107/166 Control: 110/164 |
I-III | Laparoscopic cholecystectomy | Not mentioned | General anesthesia |
Baseline characteristics of included studies.
Transcutaneous electrical acupoint stimulation, TEAS; American Society of Anesthetists, ASA.
Table 2
| Study | TEAS group | Control group | Blinding method | POD assessment | Postoperative analgesia protocol |
|---|---|---|---|---|---|
| Cao et al. (21) | Position: PC6, LI4 Timing: from 30 min before the commencement of surgery until 30 min before the end of surgery Parameter: 10 Hz, 7–15 mA |
Sham TEAS: electrodes at PC6, LI4, no electrical stimulation | Blinding of Participants: unclear Blinding of Personnel: unclear Blinding of Outcome Assessors: unclear |
CAM | PCIA: sufentanil 100 μg |
| Chang et al. (27) | Position: EX-HN3, PC6, LI4 Timing: 30 min before anesthesia induction until the end of the surgery Parameter: 2/100 Hz, 6–10 mA |
Sham TEAS: electrodes at EX-HN3, PC6, LI4, no electrical stimulation | Blinding of Participants: unclear Blinding of Personnel: unclear Blinding of Outcome Assessors: unclear |
CAM | PCIA: sufentanil 2.0 μg/kg |
| Ding et al. (18) | Position: GV20, GV24, PC6, LI4 Timing: 30 min before anesthesia induction until the end of the surgery Parameter: 2/6 Hz, 6–12 mA |
Sham TEAS: electrodes at GV20, GV24, PC6, LI4, no electrical stimulation | Blinding of Participants: yes Blinding of Personnel: yes Blinding of Outcome Assessors: yes |
CAM | Not mentioned |
| Du et al. (29) | Position: SP10, ST36, PC6, LI4 Timing: Not mentioned Parameter: 2/100 Hz, 6–10 mA |
Sham TEAS: electrodes at SP10, ST36, PC6, LI4, no electrical stimulation | Blinding of Participants: unclear Blinding of Personnel: unclear Blinding of Outcome Assessors: unclear |
Not mentioned | Not mentioned |
| Gao et al. (17) | Position: PC6, LI4 Timing: 30 min before anesthesia induction until the end of the surgery Parameter: 2/100 Hz |
Sham TEAS: electrodes at PC6, LI4, no electrical stimulation | Blinding of Participants: unclear Blinding of Personnel: unclear Blinding of Outcome Assessors: yes |
CAM-ICU | PCIA: sufentanil 1.5 μg/kg |
| Ge et al. (20) | Position: SP10, ST36, PC6, LI4 et al. Timing: 30 min before surgery, 2 h, 4 h after surgery, and on the first and second day after surgery, twice a day. Each session lasting for 30 min Parameter: 2/100 Hz |
No TEAS: standard care | Blinding of Participants: unclear Blinding of Personnel: yes Blinding of Outcome Assessors: yes |
Nursing Delirium Screening Scale | Not mentioned |
| Liu (31) | Position: LI4, PC6 Timing: from the completion of anesthesia induction until the end of surgery Parameter: 2/100 Hz; 6–10 mA |
Sham TEAS: electrodes at LI4, PC6, no electrical stimulation | Blinding of Participants: unclear Blinding of Personnel: unclear Blinding of Outcome Assessors: unclear |
CAM–ICU | PCIA: sufentanil 3.0 μg/kg |
| Lu et al. (14) | Position: PC6, LI4, HT7 Timing: 30 min before anesthesia induction and then once daily on postoperative days 1 to 3, each session lasting for 30 min Parameter: 2/100 Hz, 6–15 mA |
Sham TEAS: electrodes at PC6, LI4, HT7, no electrical stimulation | Blinding of Participants: yes Blinding of Personnel: yes Blinding of Outcome Assessors: unclear |
Not mentioned | PCIA: sufentanil 10 μg/kg |
| Qian et al. (36) | Position: LI4, HT7, LR3, SP6 Timing: on the day before the surgery date (AM and PM), intervention on the day of surgery day, and the week after the surgery day, each session lasting for 30 min Parameter: 2/100 Hz |
No TEAS: standard care | Blinding of Participants: unclear Blinding of Personnel: unclear Blinding of Outcome Assessors: unclear |
CAM | Not mentioned |
| Shi et al. (28) | Position: GV20, Ex-HN18, HT7, SP6 Timing: 1 day before surgery, 30 min before anesthesia, and 1 day after surgery Parameter: 2/10 Hz; 6–15 mA |
Sham TEAS: electrodes at GV20, Ex-HN18, HT7, SP6, no electrical stimulation | Blinding of Participants: unclear Blinding of Personnel: unclear Blinding of Outcome Assessors: unclear |
CAM | PCIA: sufentanil 1.0 μg/kg |
| Wang et al. (22) | Position: LI4, PC6, HT7, GV20 Timing: before anesthesia induction and maintained for 30 min Parameter: 10 Hz |
Sham TEAS: electrodes at LI4, PC6, HT7, GV20, no electrical stimulation | Blinding of Participants: yes Blinding of Personnel: yes Blinding of Outcome Assessors: yes |
CAM | Not mentioned |
| Wei et al. (35) | Position: EX-HN3, PC6, LI11, P8, P7, GV20 Timing: 30 min before anesthesia induction until the end of the surgery Parameter: 2/6 Hz, 6–12 mA |
Sham TEAS: electrodes at EX-HN3, PC6, LI11, P8, P7, GV20, no electrical stimulation | Blinding of Participants: unclear Blinding of Personnel: unclear Blinding of Outcome Assessors: unclear |
CAM | PCIA: dezocine 0.5 mg/kg |
| Wei et al. (24) | Position: PC6, HT7 Timing: 30 min/session/day, from preoperative day 1 to postoperative day Parameter: 10 Hz |
Sham TEAS: electrodes at PC6, HT7, no electrical stimulation | Blinding of Participants: unclear Blinding of Personnel: unclear Blinding of Outcome Assessors: unclear |
CAM | PCIA: sufentanil 2.0 μg/kg |
| Wen and Liang (32) | Position: PC6, LI4, LU7, LU5 Timing: 30 min before anesthesia induction until the end of surgery Parameter: 2/100 Hz |
Sham TEAS: electrodes at PC6, LI4, LU7, LU5, no electrical stimulation | Blinding of Participants: unclear Blinding of Personnel: unclear Blinding of Outcome Assessors: unclear |
CAM | Not mentioned |
| Wu et al. (26) | Position: HT7, PC6, ST36 Timing: 30 min before anesthesia induction until the end of the surgery; 30 min at postoperative 24, 48, 72 h Parameter: 2/100 Hz; 1–30 mA |
Sham TEAS: electrodes at HT7, PC6, ST36, no electrical stimulation | Blinding of Participants: unclear Blinding of Personnel: unclear Blinding of Outcome Assessors: unclear |
CAM | PCIA: sufentanil 1.5–2.0 μg/kg |
| Xu et al. (30) | Position: LI4, PC6, ST36 Timing: 30 min before anesthesia induction until the end of the surgery Parameter: 30/2 Hz; 6–10 mA |
Sham TEAS: electrodes at LI4, PC6, ST36, no electrical stimulation | Blinding of Participants: unclear Blinding of Personnel: unclear Blinding of Outcome Assessors: unclear |
Rapid Diagnostic Protocol for Delirium | PCIA: sufentanil 1.8 μg/kg |
| Yang et al. (25) | Position: LI4, PC6 Timing: 30 min before anesthesia induction Parameter: not mentioned |
No TEAS: standard care | Blinding of Participants: unclear Blinding of Personnel: unclear Blinding of Outcome Assessors: unclear |
CAM | Not mentioned |
| Yu et al. (33) | Position: LI4, PC6 Timing: 30 min before anesthesia induction until the end of the surgery Parameter: 2/100 Hz |
Sham TEAS: electrodes at LI4, PC6, no electrical stimulation | Blinding of Participants: unclear Blinding of Personnel: unclear Blinding of Outcome Assessors: unclear |
CAM | Not mentioned |
| Zhang et al. (19) | Position: PC6, HT7 Timing: 30 min before surgery and then once daily on postoperative days 1 to 3, each session lasting for 30 min Parameter: 2/100 Hz, 6–15 mA |
No TEAS: standard care | Blinding of Participants: unclear Blinding of Personnel: unclear Blinding of Outcome Assessors: unclear |
CAM | PCIA: sufentanil 2.0 μg/kg |
| Zhang et al. (23) | Position: BL32, SP6, CV3, CV4 Timing: 30 min before anesthesia induction and lasted 45 min after surgery Parameter: 4/20 Hz |
Sham TEAS: electrodes at BL32, SP6, CV3, CV4, no electrical stimulation | Blinding of Participants: yes Blinding of Personnel: yes Blinding of Outcome Assessors: yes |
CAM–ICU | PCIA with sufentanil |
A detailed summary of the characteristics of the included studies.
Transcutaneous electrical acupoint stimulation, TEAS; Postoperative delirium, POD; Confusion assessment method, CAM; Intensive care unit, ICU; Patient-controlled intravenous analgesia, PCIA; Neiguan, PC6; Hegu, LI4; Yintang, EX-HN3; Zusanli, ST36; Xuehai, SP10; Shenmen, HT7; Tai Chong, LR 3; Baihui, GV20; Lieque, LU7, Chizhe, LU5.
Risk of bias assessment
The methodological quality of the included studies was assessed using the Cochrane Risk of Bias tool. Allocation concealment was clearly reported in only three trials. Blinding of participants and personnel was implemented in four trials. Five trials reported blinding of outcome assessment. Two studies had the risk of selective reporting. A visual summary of the risk of bias across all domains is presented in Figure 2.
Figure 2

The risk bias assessment of all included studies.
Results of meta-analysis
Primary outcome: incidence of POD
Nineteen studies reported data on the incidence of POD. The pooled meta-analysis using a random-effects model demonstrated that TEAS significantly reduced the risk of developing POD compared to the control group. The overall effect was highly statistically significant (RR = 0.34, 95% CI: 0.26–0.45; p < 0.001, I2 = 0%). The forest plot for the primary outcome is shown in Figure 3.
Figure 3

Forest plot of the incidence of POD between TEAS and control group (POD, postoperative delirium; TEAS, transcutaneous electrical acupoint stimulation).
Secondary outcomes
CAM Score: Pooled analysis from four studies that reported CAM score showed that patients in the TEAS group had significantly lower score than those in the control group (MD = −1.01, 95% CI: −1.98 to −0.04; p < 0.05, I2 = 80%) (Figure 4), indicating less severe delirium symptoms.
Figure 4

Forest plot of the CAM score between TEAS and control group (CAM, Confusion Assessment Method; TEAS, transcutaneous electrical acupoint stimulation).
Postoperative Pain Score: Meta-analysis of five studies assessing pain intensity revealed that TEAS was associated with a statistically significant reduction in postoperative pain score compared to control (MD = −0.60, 95% CI: −1.02 to −0.18; p < 0.05, I2 = 86%) (Figure 5).
Figure 5
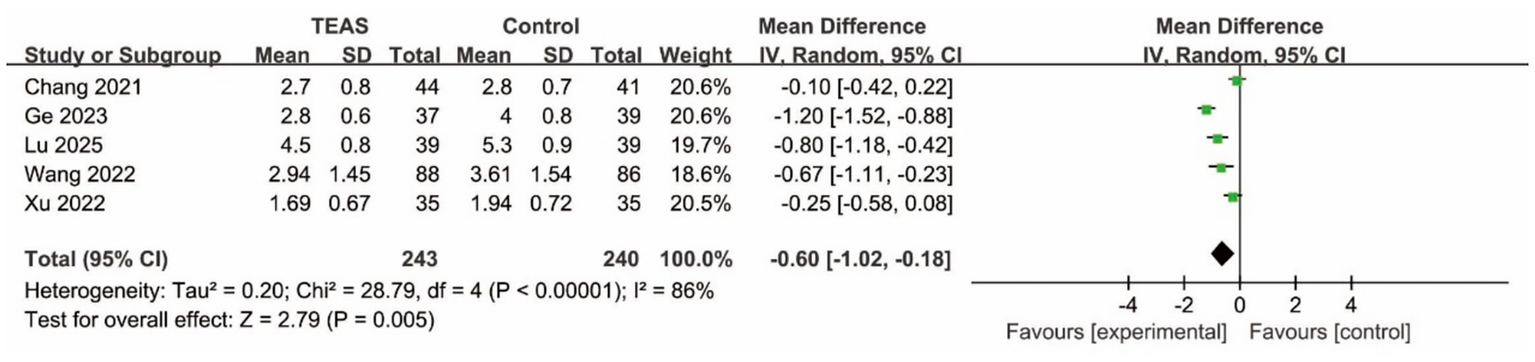
Forest plot of the postoperative pain score between TEAS and control group (TEAS, transcutaneous electrical acupoint stimulation).
Quality of Recovery: Data from two studies using the QoR-15 indicated that the TEAS group experienced a significantly better quality of recovery in the postoperative period (MD = 23.76, 95% CI: 21.72–25.80; p < 0.05, I2 = 0%) (Figure 6).
Figure 6
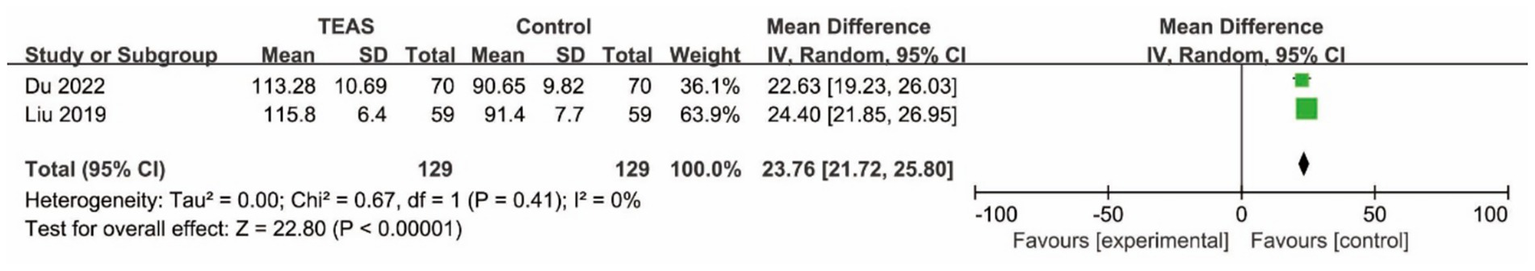
Forest plot of the QoR-15 score between TEAS and control group (TEAS, transcutaneous electrical acupoint stimulation).
Inflammatory and Neuronal Injury Biomarkers: Qualitative synthesis suggested a consistent trend across studies where TEAS was associated with lower postoperative levels of neuronal injury markers (TNF-α and NSE) (Supplementary Figures 1, 2) compared to control groups.
Intraoperative propofol and remifentanil consumption: The pooled analysis showed a significant reduction in propofol consumption the TEAS group compared to control (MD −35.59 mg, 95% CI −65.75 to −5.42, p < 0.05) (Figure 7), while no significant difference in remifentanil consumption (SMD −0.66, 95% CI −1.60–0.27, p > 0.05) (Figure 8).
Figure 7
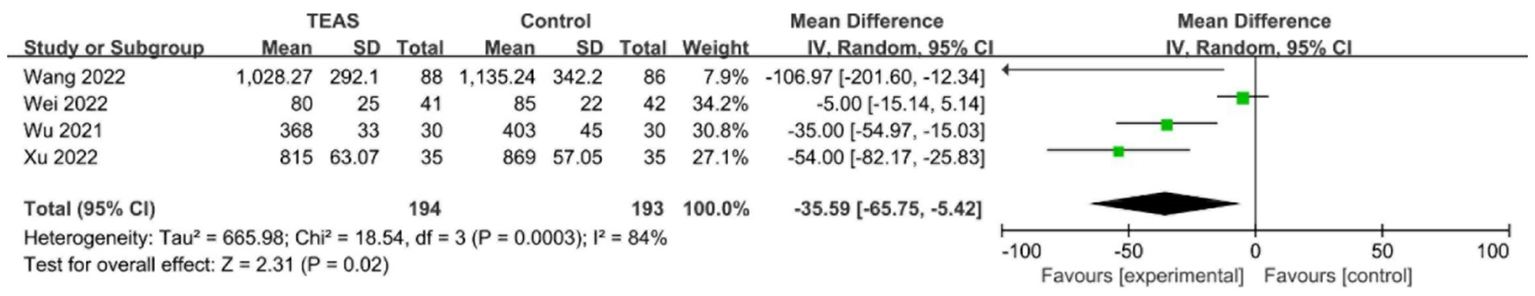
Forest plot of propofol consumption between TEAS and control group (TEAS, transcutaneous electrical acupoint stimulation).
Figure 8

Forest plot of remifentanil consumption between TEAS and control group (TEAS, transcutaneous electrical acupoint stimulation).
Adverse Events: Meta-analysis revealed that no statistically significant difference in incidence of PONV, hypotension and bradycardia between two groups (Supplementary Figures 3–5).
Subgroup and sensitivity analyses
Pre-specified subgroup analyses based on surgical type (orthopedic surgeries vs. non-orthopedic surgeries) (Supplementary Figure 6) did not identify significant subgroup differences, suggesting a consistent benefit of TEAS across these categories. Sensitivity analyses, performed by excluding each study, did not materially alter the overall pooled estimate for the primary outcome, confirming the robustness of the results.
Publication bias
Publication bias was assessed for the primary outcome (incidence of POD) through visual inspection of the funnel plot. The funnel plot displayed an approximately symmetrical distribution of effect estimates around the pooled result (Figure 9). Based on this visual assessment, there was no obvious evidence of significant publication bias among the included studies for this outcome.
Figure 9
![Funnel plot displaying several circles representing studies, distributed around a vertical dashed line. The x-axis is labeled "RR" ranging from 0.01 to 100, and the y-axis is labeled "SE(log[RR])" ranging from 0 to 2.](https://www.frontiersin.org/files/Articles/1717702/xml-images/fmed-13-1717702-g009.webp)
Funnel plot for the primary outcome.
Certainty of evidence (GRADE)
According to the GRADE approach, the certainty of evidence for the primary outcome (POD incidence) was assessed as moderate. The rating “Other considerations” was downgraded “serious.” The certainty of evidence for other outcomes was ranged from low to moderate. Table 3 showed the summary of GRADE.
Table 3
| Outcome | Included studies (n) | Patients (n) | RR/MD/SMD | 95% CI | I2 | Quality of evidence | Reasons |
|---|---|---|---|---|---|---|---|
| Incidence of POD | 19 | 2,205 | 0.34 | (0.26, 0.45) | 0% | ⨁⨁⨁◯ MODERATE |
“Other considerations” was downgraded “serious.” |
| CAM score | 4 | 374 | −1.01 | (−1.98, −0.04) | 80% | ⨁⨁◯◯ LOW |
“Imprecision” and “Other considerations” were downgraded to “serious” |
| Postoperative pain score | 5 | 483 | −0.06 | (−1.02, −0.18) | 86% | ⨁⨁◯◯ LOW |
“Imprecision” and “Other considerations” were downgraded to “serious” |
| Quality of recovery | 2 | 258 | 23.76 | (21.72, 25.80) | 0% | ⨁⨁⨁◯ MODERATE |
“Other considerations” was downgraded “serious.” |
| Propofol consumption | 4 | 387 | −35.59 | (−65.75, −5.42) | 84% | ⨁⨁◯◯ LOW |
“Imprecision” and “Other considerations” were downgraded to “serious” |
| Remifentanil consumption | 4 | 387 | −0.66 | (−1.60, 0.27) | 94% | ⨁⨁◯◯ LOW |
“Imprecision” and “Other considerations” were downgraded to “serious” |
| TNF-α level | 4 | 418 | −14.07 | (−25.00, −3.14) | 96% | ⨁⨁◯◯ LOW |
“Imprecision” and “Other considerations” were downgraded to “serious” |
| NES level | 5 | 592 | −3.32 | (−4.06, −2.59) | 79% | ⨁⨁◯◯ LOW |
“Imprecision” and “Other considerations” were downgraded to “serious” |
| Incidence of PONV | 4 | 805 | 0.36 | (0.10, 1.24) | 70% | ⨁⨁◯◯ LOW |
“Imprecision” and “Other considerations” were downgraded to “serious” |
| Incidence of bradycardia | 2 | 258 | 0.94 | (0.61, 1.45) | 0% | ⨁⨁⨁◯ MODERATE |
“Other considerations” was downgraded “serious.” |
| Incidence of hypotension | 2 | 258 | 1.13 | (0.68, 1.87) | 0% | ⨁⨁⨁◯ MODERATE |
“Other considerations” was downgraded “serious.” |
Summary for GRADE assessment.
POD, postoperative delirium; CAM, Confusion Assessment Method; PONV, postoperative nausea and vomiting; RR, risk ratio; MD, mean difference; SMD, standard mean difference; CI, confidence interval.
Discussion
This systematic review and meta-analysis of 20 randomized controlled trials, encompassing 2,290 elderly surgical patients, provides evidence that perioperative TEAS is associated with a significantly reduced risk of POD. Furthermore, our analysis demonstrates that TEAS confers additional benefits, including amelioration of delirium severity, reduction in postoperative pain, and improvement in the overall quality of recovery. The intervention was found to be safe, with no serious adverse events reported.
The magnitude of the protective effect observed in our study is substantial and underscores the potential of TEAS as a pivotal non-pharmacological strategy within enhanced recovery after surgery (ERAS) protocols (37). The consistency of the beneficial effect across diverse surgical populations, as confirmed by our subgroup analysis showing no significant difference between orthopedic and non-orthopedic surgeries, enhances the generalizability of our findings. This suggests that the neuroprotective mechanism of TEAS may target fundamental pathways common to the pathogenesis of delirium following various surgical insults.
The positive effects of TEAS on secondary outcomes offer critical insights into its potential mechanisms of action. The significant reduction in CAM scores indicates that TEAS not only prevents the onset of delirium but also mitigates its severity. The observed analgesic effect is particularly salient. Postoperative pain is a well- established risk factor for POD; it induces stress, disrupts sleep, and often necessitates increased opioid consumption, which itself can contribute to neuroinflammation and cognitive dysfunction (38, 39). By effectively reducing pain, TEAS may break this vicious cycle, thereby reducing the delirium burden. This is further supported by the marked improvement in the QoR-15 score, indicating a holistic enhancement of the patient’s postoperative experience.
While the exact mechanisms remain to be fully elucidated, our results, combined with the findings of the included studies, point toward multi-modal actions. The qualitative synthesis suggesting a reduction in inflammatory (TNF-α) and neuronal injury (NSE) biomarkers aligns with the prevailing neuroinflammatory hypothesis of POD. Surgery triggers a systemic inflammatory response, leading to the release of cytokines that can breach the blood–brain barrier, activate microglia, and disrupt neuronal function and neurotransmission. TEAS has been shown in preclinical and clinical studies to modulate this response, potentially through vagal nerve stimulation and cholinergic anti-inflammatory pathways, leading to a attenuated neuroinflammatory state (40, 41). The underlying pathway may involve the modulation of the cholinergic anti-inflammatory pathway via vagal nerve activation, which suppresses the release of pro-inflammatory cytokines such as TNF-α (42). This anti-inflammatory effect, coupled with improved analgesia and sleep quality, likely creates a synergistic effect that protects the vulnerable aging brain from the precipitating factors of delirium.
Our analysis further indicated that TEAS reduced intraoperative propofol requirement while exerting no significant effect on remifentanil consumption. The propofol-sparing effect is clinically meaningful, as propofol may contribute to neuroinflammation in the aging brain (43). TEAS likely provides intrinsic sedation through GABAergic modulation (44), thereby lowering propofol demand and its potential neurotoxic burden.
Several limitations of this analysis must be acknowledged. First, the overall certainty of evidence was graded as moderate for the primary outcome, primarily due to the methodological limitations present in many of the included studies. Common issues included unclear allocation concealment and challenges in blinding personnel administering the intervention, which are inherent difficulties in trials of physical interventions like TEAS. While sham TEAS was employed as control in most studies, the inability to blind personnel may have introduced performance bias. Second, while the funnel plot appeared symmetrical, the possibility of unpublished negative studies (publication bias) can never be completely excluded. Third, we observed substantial statistical heterogeneity (I2 > 80%) in the meta-analyses for CAM scores and postoperative pain score. This heterogeneity likely stems from clinical diversity, including variations in the specific TEAS protocols (acupoint combinations, stimulation parameters, treatment duration), the types and intensities of surgical procedures, and the different tools used to assess pain. While the random-effects model accounts for this, the findings should be interpreted with awareness of this underlying variability. Fourth, an important clinical dimension of POD, its psychomotor subtype (hyperactive, hypoactive, mixed), could not be analyzed. None of the included studies reported such data. Finally, the majority of included trials were conducted in China, which may limit the generalizability of our findings to other healthcare settings and ethnic populations. Future international multi-center studies are warranted.
Conclusion
In conclusion, this meta-analysis provides evidence that perioperative TEAS is an effective and safe intervention for preventing postoperative delirium in elderly patients. Its benefits extend beyond mere risk reduction to encompass less severe delirium, improved pain control, and a better overall recovery experience. TEAS might be considered a promising component of multimodal, non-pharmacological strategies aimed at optimizing neurological outcomes and enhancing recovery in the growing population of elderly surgical patients.
Statements
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
Y-jC: Conceptualization, Writing – original draft, Writing – review & editing. Q-hS: Conceptualization, Data curation, Writing – review & editing. YY: Investigation, Methodology, Writing – review & editing. RS: Investigation, Methodology, Writing – original draft. H-fL: Conceptualization, Software, Writing – original draft, Writing – review & editing.
Funding
The author(s) declared that financial support was not received for this work and/or its publication.
Conflict of interest
The author(s) declared that this work was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declared that Generative AI was not used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2026.1717702/full#supplementary-material
References
1.
Li T Li J Yuan L Wu J Jiang C Daniels J et al . Effect of regional vs. general anesthesia on incidence of postoperative delirium in older patients undergoing hip fracture surgery: the RAGA randomized trial. JAMA. (2022) 327:50–8. doi: 10.1001/jama.2021.22647,
2.
Aldecoa C Bettelli G Bilotta F Sanders RD Aceto P Audisio R et al . Update of the european society of anaesthesiology and intensive care medicine evidence-based and consensus-based guideline on postoperative delirium in adult patients. Eur J Anaesthesiol. (2024) 41:81–108. doi: 10.1097/EJA.000000000000187
3.
Jin Z Hu J Ma D . Postoperative delirium: perioperative assessment, risk reduction, and management. Br J Anaesth. (2020) 125:492–504. doi: 10.1016/j.bja.2020.06.063,
4.
Li J Fan Y Luo R Yin N Wang Y Jing J et al . The impact of non-pharmacological sleep interventions on delirium prevention and sleep improvement in postoperative ICU patients: a systematic review and network meta-analysis. Intensive Crit Care Nurs. (2025) 87:103925. doi: 10.1016/j.iccn.2024.103925,
5.
Tong RJ Lv YZ Shi YF Lai L Shen QH . Remimazolam versus propofol for postoperative delirium prevention in geriatric surgery: a systematic review and meta-analysis of randomized controlled trials. Aging Clin Exp Res. (2025) 37:253. doi: 10.1007/s40520-025-03166-6,
6.
Feng H Liu Y Wang X Wang C Wang T . Cerebrospinal fluid biomarkers of neuroinflammation and postoperative neurocognitive disorders in patients undergoing orthopedic surgery: a systematic review and meta-analysis. Int J Surg. (2025) 111:3573–88. doi: 10.1097/JS9.0000000000002344,
7.
Taylor J Parker M Casey CP Tanabe S Kunkel D Rivera C et al . Postoperative delirium and changes in the blood-brain barrier, neuroinflammation, and cerebrospinal fluid lactate: a prospective cohort study. Br J Anaesth. (2022) 129:219–30. doi: 10.1016/j.bja.2022.01.005,
8.
Lopez MG Shotwell MS Hennessy C Pretorius M McIlroy D Kimlinger MJ et al . Intraoperative oxygen treatment, oxidative stress, and organ injury following cardiac surgery: a randomized clinical trial. JAMA Surg. (2024) 159:1106–16. doi: 10.1001/jamasurg.2024.2906,
9.
Skelly DT Griffin ÉW Murray CL Harney S O'Boyle C Hennessy E et al . Acute transient cognitive dysfunction and acute brain injury induced by systemic inflammation occur by dissociable IL-1-dependent mechanisms. Mol Psychiatry. (2019) 24:1533–48. doi: 10.1038/s41380-018-0075-8,
10.
Queiroz I Barbosa LM Gallo Ruelas M Araújo B Defante MLR Tavares AH et al . Effect of peri-operative pharmacological interventions on postoperative delirium in patients having cardiac surgery: a systematic review and Bayesian network meta-analysis. Anaesthesia. (2025). [Epub ahead of print]. doi: 10.1111/anae.16757
11.
Caetano da Silva L Tapioca V Viana P Pereira EM Gibicoski T Amaral S . Dexmedetomidine for delirium prevention after cardiac surgery: an updated systematic review and meta-analysis with trial sequential analysis. Anaesth Crit Care Pain Med. (2025) 44:101578. doi: 10.1016/j.accpm.2025.101578,
12.
Wang B Tang J White PF Naruse R Sloninsky A Kariger R et al . Effect of the intensity of transcutaneous acupoint electrical stimulation on the postoperative analgesic requirement. Anesth Analg. (1997) 85:406–13. doi: 10.1213/00000539-199708000-00029,
13.
Wu C Deng Z Zhu Y Li Y Chen Y Wang L et al . Transcutaneous electrical acupoint stimulation accelerates gastrointestinal function recovery after abdominal surgery: a systemic review and meta-analysis of randomized controlled trials. Int J Surg. (2025) 111. doi: 10.1097/JS9.0000000000002946,
14.
Lu Z Wang Q Sun X Zhang W Min S Zhang J et al . Transcutaneous electrical acupoint stimulation before surgery reduces chronic pain after mastectomy: a randomized clinical trial. J Clin Anesth. (2021) 74:110453. doi: 10.1016/j.jclinane.2021.110453,
15.
Chen J Tu Q Miao S Zhou Z Hu S . Transcutaneous electrical acupoint stimulation for preventing postoperative nausea and vomiting after general anesthesia: a meta-analysis of randomized controlled trials. Int J Surg. (2020) 73:57–64. doi: 10.1016/j.ijsu.2019.10.036,
16.
Liu Y Fan J Zhang X Xu W Shi Z Cai J et al . Transcutaneous electrical acupoint stimulation reduces postoperative patients' length of stay and hospitalization costs: a systematic review and meta-analysis. Int J Surg. (2024) 110:5124–35. doi: 10.1097/JS9.0000000000001598,
17.
Gao F Zhang Q Li Y Tai Y Xin X Wang X et al . Transcutaneous electrical acupoint stimulation for prevention of postoperative delirium in geriatric patients with silent lacunar infarction: a preliminary study. Clin Interv Aging. (2018) 13:2127–34. doi: 10.2147/CIA.S183698,
18.
Ding L Ning J Guo Y Wang Q Kou S Ke H et al . The preventive effect of transcutaneous electrical Acupoint stimulation on postoperative delirium in elderly patients with time factors: a randomized trial. J Integ Complement Med. (2022) 28:689–96. doi: 10.1089/jicm.2021.0141,
19.
Zhang L Qiu Q Zhou L . The influence of transcutaneous electrical acupoint stimulation on fatigue and delirium in elderly patients with sleep disorders after lower extremity surgery. Guide Chin Med. (2025) 23:139–41.
20.
Ge Y Zheng J Yu Y . Effect of transcutaneous electrical acupoint stimulation on postoperative rehabilitation in elderly patients with kidney deficiency and blood stasis type undergoing hip replacement. Nurs Rehabil J. (2023) 22:50–52+55.
21.
Cao L Chen Z Yang J Ding Z Meng Z . Clinical study on preoperative transcutaneous electrical acupoint stimulation for postoperative delirium in elderly patients undergoing total hip replacement. Chin J Integ Med. (2022) 20:348–52.
22.
Wang Q Zhou R Ding L Ning J Kou S Li W . Effect of electroacupuncture and transcutaneous electrical acupoint stimulation on postoperative delirium in elderly patients. Chin J Surg Integ Trad West Med. (2022) 28:485–90.
23.
Zhang Y Gong L Zhang Y Dong S Shi J Li X et al . Effect of transcutaneous Acupoint electrical stimulation on urinary retention and urinary ATP in elderly patients after laparoscopic cholecystectomy: a prospective, randomized, controlled clinical trial. Clin Interv Aging. (2022) 17:1751–60. doi: 10.2147/CIA.S382912,
24.
Wei L Luo W Huang J Tai S Su Y Tang Y et al . The effect of transcutaneous electrical acupoint stimulation of Shenmen and Neiguan points on sleep quality and postoperative delirium in elderly patients undergoing hip replacement. Int J Anesth Resuscit. (2021) 42:1056–60.
25.
Yang S Zhong B Zhong W . Effect of transcutaneous electrical acupoint stimulation on postoperative delirium and its biomarkers in elderly patients with hip fracture. Mod Diagn Treat. (2023) 34:2272–4.
26.
Wu H Gao H Mi Z Lin S Gao J . Effect of transcutaneous electrical acupoint stimulation on postoperative delirium in frail elderly patients. Chin J Anesthesiol. (2021) 41:723–6.
27.
Chang M Long Q Lin S et al . Effect of transcutaneous electrical acupoint stimulation on postoperative fatigue and delirium in elderly patients with sleep disorder undergoing total hip arthroplasty. J Clin Anesthesiol. (2021) 37:1013–7.
28.
Shi H Li W Zhang Y Wang Y . Effect of transcutaneous electrical acupoint stimulation on sleep after spinal surgery in elderly. Orthop J China. (2022) 30:2045–9.
29.
Du W Zheng J Huang M He H . Effect of transcutaneous electrical acupoint stimulation on the incidence of postoperative delirium in elderly patients undergoing radical lung cancer surgery. J Anhui Med Coll. (2022) 21:30–31+34.
30.
Xu X Huang X Yu Y Wang W Xia P . Effects of percutaneous acupoint electrical stimulation assisted anesthesia on stress response and delirium after lumbar surgery in the elderly. Med Innov China. (2022) 19:53–7.
31.
Liu W . Effects of transcutaneous acupoint electrical stimulation on postoperative delirium and early rehabilitation of elderly patients undergoing radical mastectomy. J Basic Clin Oncol. (2019) 32:400–4.
32.
Wen M Liang W . Effects of transcutaneous electric acupoint stimulation on postoperative stress response and delirium in elderly patients undergoing radical thyroidectomy. China Mod Doctor. (2025) 63:1–4.
33.
Yu Y Qian X Li G Tang W Li C Liu G . The effects of transcutaneous electrical acupoint stimulation on perioperative neurocognitive disorders and clinical outcomes in elderly patients undergoing open spinal surgery. J Wenzhou Med Univ. (2024) 54:1–6.
34.
Lu F Li Y Liu T et al . Effects of transcutaneous electrical acupoint stimulation on postoperative sleep quality in elderly patients undergoing proximal femoral bionic nail fixation surgery. J Clin Anesthesiol. (2025) 41:19–24.
35.
Wei C Hao N Liu J Li j . Observation on the effect of electrical stimulation at ghost points combined with an endotracheal general anesthesia on delirium in elderly patients after a total knee arthroplasty. Jilin J Chin Med. (2022) 42:362–5.
36.
Qian J He M Zhan X Ren L Sun Q . Transcutaneous electrical acupoint stimulation combined with an integrated perioperative nursing program prevents subsyndromal delirium in older patients after joint replacement. Geriatr Nurs (NY). (2023) 49:199–206. doi: 10.1016/j.gerinurse.2022.12.010,
37.
Li Y Ma Y Guo W Ge W Cheng Y Jin C et al . Effect of transcutaneous electrical acupoint stimulation on postoperative pain in pediatric orthopedic surgery with the enhanced recovery after surgery protocol: a prospective, randomized controlled trial. Anaesth Crit Care Pain Med. (2023) 42:101273. doi: 10.1016/j.accpm.2023.101273,
38.
Ma JH Liu YF Hong H Li CJ Cui F Mu DL et al . Effect of acute pain on the association between preoperative cognitive impairment and postoperative delirium: a secondary analysis of three trials. Br J Anaesth. (2023) 130:e272–80. doi: 10.1016/j.bja.2022.06.033,
39.
Vaurio LE Sands LP Wang Y Mullen EA Leung JM . Postoperative delirium: the importance of pain and pain management. Anesth Analg. (2006) 102:1267–73. doi: 10.1213/01.ane.0000199156.59226.af,
40.
Tan Z Dong F Wu L Xu G Zhang F . Transcutaneous electrical acupoint stimulation attenuated neuroinflammation and oxidative stress by activating SIRT1-induced signaling pathway in MCAO/R rat models. Exp Neurol. (2024) 373:114658. doi: 10.1016/j.expneurol.2023.114658
41.
Chi YL Zhang WL Yang F Su F Zhou YK . Transcutaneous electrical Acupoint stimulation for improving postoperative recovery, reducing stress and inflammatory responses in elderly patient undergoing knee surgery. Am J Chin Med. (2019) 47:1445–58. doi: 10.1142/S0192415X19500745,
42.
Xiong S Wang Q Chen Y Du H Zhao Y . Leptin limits hepatic lipid accumulation and inflammation via vagal activation of the JAK2-STAT3/AMPK pathway. J Nutr Biochem. (2024) 134:109748. doi: 10.1016/j.jnutbio.2024.109748,
43.
Xue H Zhang X Chou C Jia Y Hao C Duan X . Advances in research on propofol-induced postoperative cognitive dysfunction via piezo channels. Front Mol Neurosci. (2025) 18:1668523. doi: 10.3389/fnmol.2025.1668523,
44.
Lu Z Huo T Deng J Guo F Liu K Liu P et al . Transcutaneous electrical acupoint stimulation induced sedative effects in healthy volunteers: a resting-state fMRI study. Front Hum Neurosci. (2022) 16:843186. doi: 10.3389/fnhum.2022.843186
Summary
Keywords
elderly, meta-analysis, perioperative, postoperative delirium, transcutaneous electrical acupoint stimulation
Citation
Chen Y-j, Shen Q-h, Yang Y, Shen R and Li H-f (2026) Transcutaneous electrical acupoint stimulation for preventing postoperative delirium in elderly patients: a systematic review and meta-analysis. Front. Med. 13:1717702. doi: 10.3389/fmed.2026.1717702
Received
02 October 2025
Revised
18 December 2025
Accepted
02 January 2026
Published
15 January 2026
Volume
13 - 2026
Edited by
Lei Zhao, Capital Medical University, China
Reviewed by
Xuli Ren, Jilin University, China
Li-Xin An, Capital Medical University, China
Updates
Copyright
© 2026 Chen, Shen, Yang, Shen and Li.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hui-fang Li, lihuifang213@126.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.