Abstract
Bronchobiliary fistula (BBF) is an exceptionally rare and complex clinical entity that involves abnormal communication between the biliary system and the bronchial tree. This article presents the first reported case of BBF successfully occluded with percutaneous microwave ablation (PMWA). A 35-years-old female with primary colon cancer developed BBF after PMWA for liver metastasis and presented with bilioptysis that persisted despite conventional antibiotic therapy and drainage. Under computed tomography (CT) guidance, targeted PMWA with an ablation power of 40 w was applied to the fistula tract for 7 min, resulting in complete radiographic closure and resolution of symptoms. Compared with traditional surgical, endoscopic, or drainage-based approaches, PMWA represents a minimally invasive alternative. While this technique has significant advantages in terms of precision, quick recovery, and applicability to high-risk patients, its efficacy may be limited in patients with large or anatomically complex fistulas. Further clinical validation is needed to establish long-term outcomes and refine technical parameters. This case supports PMWA as a promising therapeutic option for BBF and highlights its potential in fistula management.
Introduction
Bronchobiliary fistula (BBF) is an extremely rare and challenging pathological condition, that mainly refers to the formation of an abnormal passage between the bronchial tree and the intrahepatic or extrahepatic bile ducts (1). Current therapeutic options for BBF are limited in several key aspects: conservative management and percutaneous transhepatic cholangial drainage (PTCD) rarely achieve definitive fistula closure (2, 3); endoscopic interventions can occlude the fistula via embolization or sealing but are associated with a risk of ectopic embolism (4); and although surgical repair allows direct fistula management, this approach is associated with significant trauma and risk of other complications (5). Therefore, a treatment that enables anatomical closure, offers precise intervention with minimal trauma is clearly needed.
Percutaneous microwave ablation (PMWA) is a commonly used minimally invasive treatment, but its application in the treatment of BBF has not been reported (6–8). This paper reports a case in which BBF was successfully treated with PMWA and aims to provide new ideas and methods for the clinical treatment of this disease.
Case presentation
A 35-years-old female patient with liver metastases from colon cancer underwent PMWA on August 5, 2022, targeting a lesion in the right hepatic lobe adjacent to the diaphragm (Figures 1a, b). She had no history of chronic obstructive pulmonary disease (COPD), subphrenic bullae, tuberculosis, or bronchiectasis. She developed fever with a maximum temperature of 39 °C on August 6, 2022, and blood cultures revealed Klebsiella oxytoca. Contrast-enhanced computed tomography (CT) on August 10, 2022, revealed the formation of a pyogenic liver abscess (PLA) (Figure 1c). Percutaneous drainage of the abscess was performed on August 16, 2022 (Figure 1d). Following antibiotic therapy and drainage, her fever subsided after September 21, 2022. However, she subsequently presented with typical bilioptysis, which was highly suggestive of BBF. To confirm the diagnosis, contrast agent was injected via the drainage tube followed immediately by CT and plain radiography on September 22, 2022. The imaging findings (Figures 2a–d), especially the coronal CT image (Figures 2b, d), clearly demonstrated extravasation of contrast agent from an intrahepatic bile duct branch, forming an abnormal fistula tract through the diaphragm and directly entering the right lower lobe bronchial tree. This imaging evidence was fully consistent with the patient’s clinical symptoms. According to the literature, direct visualization of the fistula tract on cholangiography is a reliable method for the diagnosis of BBF, and detection of bilirubin in sputum can also serve as supporting evidence (9). Therefore, this case was diagnosed as acquired BBF. Despite 13 days of adequate drainage and antibiotic therapy, the patient continued to cough up bile-like sputum. Therefore, on October 4, 2022, PMWA at an ablation watt of 40 w was performed on the fistula tract for 7 min to achieve closure (Figure 3a). A post-ablation CT scan confirmed closure of the fistula tract (Figures 3b, c). A follow-up CT scan on October 12, 2022, again demonstrated closure of the fistula (Figure 3d), and the patient no longer coughed up bile-like sputum.
FIGURE 1

Percutaneous microwave ablation (PMWA) of liver metastases and computed tomography (CT) images of pyogenic liver abscesses (PLA). (a) Coronal CT image showing the tumor adjacent to diaphragm (red arrow); (b) PMWA procedure for liver metastasis; (c) CT image of PLA; (d) percutaneous drainage procedure of PLA.
FIGURE 2
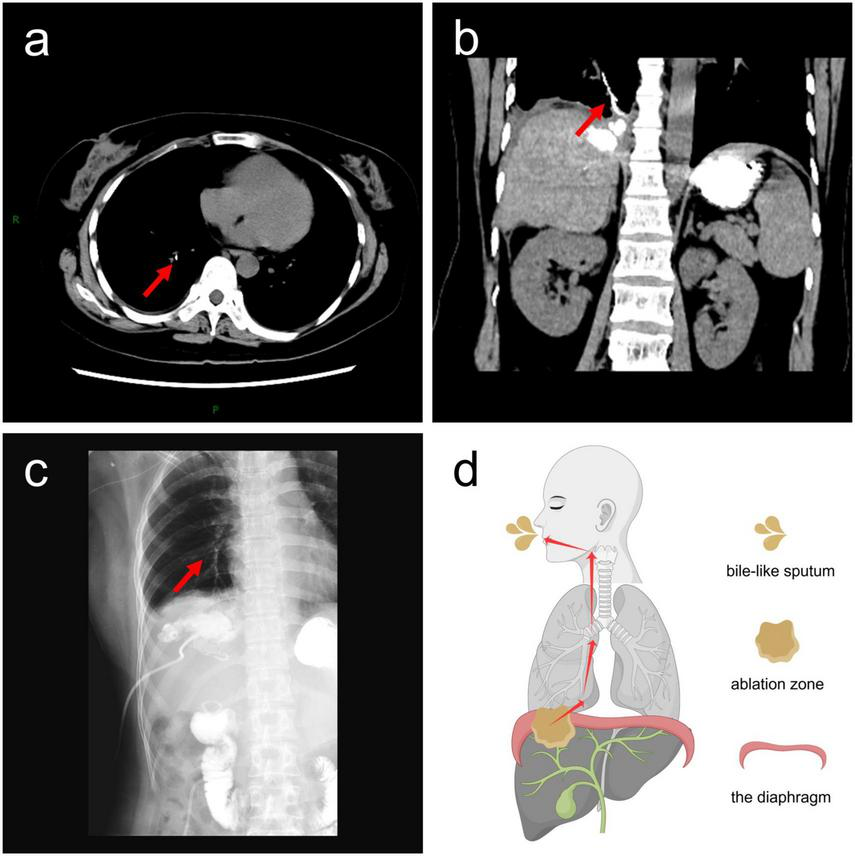
Imaging findings of bronchobiliary fistula (BBF). (a) Axial computed tomography (CT) image showing contrast agent within the fistula tract; (b) coronal CT image showing contrast agent within the fistula tract; (c) plain radiograph showing contrast agent within the fistula tract. The contrast agent within the fistula tract is indicated by red arrows; (d) the diagram illustrates the process by which bile passes through the diaphragm into the right segmental bronchus and is ultimately coughed out via the main bronchus and oral cavity. The red arrows indicate the direction of bile flow.
FIGURE 3

Computed tomography (CT) images of percutaneous microwave ablation (PMWA) for bronchobiliary fistula (BBF). (a) PMWA procedure on the fistula tract on October 4, 2022 (red arrow indicates the ablation needle adjacent to the contrast-filled fistula); (b) coronal CT image of the fistula after PMWA on October 4, 2022; (c) axial CT image of the fistula after PMWA on October 4, 2022; (d) repeated coronal CT image of the fistula on October 12, 2022.
Discussion
Bronchobiliary fistula usually results from biliary obstruction, infection, trauma and other pathological processes. Common etiologies include: choledocholithiasis leading to suppurative cholangitis, with subsequent upward spread of infection penetrating the diaphragm; rupture of a bacterial liver abscess through the diaphragm involving the lung and bronchi; and surgical injury to the diaphragm or secondary infection resulting in fistula formation (1). The BBF in the present case is characterized by a clear iatrogenic origin. Its direct cause was thermal injury from the ablation zone and secondary PLA following PMWA of a liver metastasis adjacent to the diaphragm. These factors collectively led to local disruption of diaphragmatic integrity and involvement of adjacent biliary branches, which ultimately led to an abnormal communication between the biliary tract and the bronchial tree. Therefore, this case represents an acquired, iatrogenic fistula, whose pathogenic mechanism distinctly differs from that of classic BBF caused by cholelithiasis or infection.
In this case, according to the biological principles of PMWA, we innovatively applied this treatment for the first time to occlude a BBF. The mechanism for achieving permanent BBF closure lies in a coherent pathophysiological process: first, PMWA targeting the fistula wall induces an instantaneous local temperature exceeding 60 °C through thermal effects, which leads to irreversible protein denaturation and coagulative necrosis of the tissue cells in the fistula wall (10). This is not merely a destructive event, and more importantly, necrotic tissue subsequently triggers the body’s intrinsic repair program, which elicits a strong localized inflammatory response (11, 12). The inflammatory environment promotes the proliferation and migration of fibroblasts toward the lesion site, along with the abundant synthesis and deposition of collagen. Ultimately, the original fistula is completely replaced and obliterated by newly formed, dense fibrous scar tissue, achieving permanent physical closure. This process is similar in principle to that of PMWA for the treatment of solid tumors, but the application goal shifts from the destruction of tumor tissue to sealing an abnormal channel. In terms of this mechanism, PMWA has its unique advantages in sealing a BBF: this technique requires only precise placement of the ablation antenna into the fistula tract to initiate the aforementioned healing cascade with minimal trauma, thereby achieving a minimally invasive, precise, and durable therapeutic effect (13–15).
Of course, the application of PMWA for BBF closure also presents several limitations. First, technical success may be limited for fistulas that are large in diameter or anatomically complex, particularly when they are adjacent to critical vascular or biliary structures, as complete and safe ablation may not be achievable in such cases. Second, to our knowledge, this represents the first reported use of PMWA for this specific condition, therefore, its long-term efficacy and safety profile require validation through larger clinical studies and longer follow-up. In conclusion, this case study demonstrates that PMWA is a novel, minimally invasive, and effective therapeutic alternative for the treatment of BBF. Future work should focus on refining puncture techniques, optimizing energy delivery parameters, and obtaining more robust clinical evidence to further validate the feasibility of this technique.
Statements
Data availability statement
The datasets presented in this article are not readily available because of ethical and privacy restrictions. Requests to access the datasets should be directed to the corresponding author/s.
Ethics statement
This study was performed in accordance with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of the Affiliated Hospital of Jining Medical University (reference number: 2021-10-C002) on October 2021. Written informed consent was obtained from the patient’s husband for the publication of any potentially identifiable images or data included in this article.
Author contributions
DY: Data curation, Formal analysis, Methodology, Writing – original draft. XZ: Data curation, Formal analysis, Methodology, Writing – original draft. GW: Data curation, Formal analysis, Methodology, Writing – original draft. GL: Data curation, Formal analysis, Writing – original draft. JY: Conceptualization, Writing – review & editing.
Funding
The author(s) declared that financial support was received for this work and/or its publication. This study was supported by the Jining Research and Development Program (2023YXNS046).
Conflict of interest
The author(s) declared that this work was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declared that generative AI was not used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
Edmunds C Hollingsworth J Kouri B Pawa R Pawa S . Bronchobiliary fistulas.Am J Med Sci. (2025) 370:83–9. 10.1016/j.amjms.2025.02.010
2.
Huang ZM Zuo MX Gu YK Lai CX Pan QX Yi XC et al Bronchobiliary fistula after ablation of hepatocellular carcinoma adjacent to the diaphragm: case report and literature review. Thorac Cancer. (2020) 11:1233–8. 10.1111/1759-7714.13380
3.
Schertz PJ Mao CA Derrick KD Galar F Ortiz CB Walker JA et al Biliary leaks: multidisciplinary approach to diagnosis and treatment. Radiographics. (2024) 44:e230155. 10.1148/rg.230155
4.
Li L Wang Y Zhu C Wei J Zhang W Sang H et al Endoscopic closure of refractory upper GI-tracheobronchial fistulas with a novel occluder: a prospective, single-arm, single-center study (with video). Gastrointest Endosc. (2023) 97:859–70.e5. 10.1016/j.gie.2022.12.017.
5.
Eryigit H Oztas S Urek S Olgac G Kurutepe M Kutlu CA . Management of acquired bronchobiliary fistula: 3 case reports and a literature review.J Cardiothoracic Surg. (2007) 2:52. 10.1186/1749-8090-2-52
6.
Castillo-Fortuño À Páez-Carpio A Matute-González M Odisio EG Vollmer I Baetens T et al Lung cryoablation: patient selection, techniques, and postablation imaging. Radiographics. (2025) 45:e240157. 10.1148/rg.240157
7.
Lanza C Angileri SA Biondetti P Coppola A Ricapito F Ascenti V et al Percutaneous microwave ablation of HCC: comparison between 100 and 150 W technology systems. Radiol Med. (2024) 129:1916–25. 10.1007/s11547-024-01927-3
8.
Rossebo AE Zlevor AM Knott EA Mao L Couillard AB Ziemlewicz TJ et al Percutaneous microwave ablation for treatment of retroperitoneal tumors. Radiol Imaging Cancer. (2024) 6:e230080. 10.1148/rycan.230080
9.
Zhou T Wu W Cheng C Wang H Hu X Jiang Z . Bronchobiliary fistula after traumatic liver rupture: a case report.J Med Case Rep. (2024) 18:289. 10.1186/s13256-024-04620-1
10.
Luo X Kandil E . Microwave ablation: a technical and clinical comparison to other thermal ablation modalities to treat benign and malignant thyroid nodules.Gland Surg. (2024) 13:1805–13. 10.21037/gs-24-221
11.
Akoum N Mekhael M Bisbal F Wazni O McGann C Lee H et al Lesion delivery and scar formation in catheter ablation for atrial fibrillation: the DECAAF II trial. Heart Rhythm. (2025) 22:1384–93. 10.1016/j.hrthm.2024.08.062
12.
Öcal O Dietrich O Lentini S Bour P Faller T Ozenne V et al Predicting liver ablation volumes with real-time MRI thermometry. JHEP Rep. (2024) 6:101199. 10.1016/j.jhepr.2024.101199
13.
Storman D Swierz MJ Mitus JW Pedziwiatr M Liang N Wolff R et al Microwave coagulation for liver metastases. Cochrane Database Syst Rev. (2024) 3:CD010163. 10.1002/14651858.CD010163.pub3
14.
Wei Z Chi J Cao P Jin Y Li X Ye X . Microwave ablation with a blunt-tip antenna for pulmonary ground-glass nodules: a retrospective, multicenter, case-control study.Radiol Med. (2023) 128:1061–9. 10.1007/s11547-023-01672-z
15.
Sugimoto K Imajo K Kuroda H Murohisa G Shiozawa K Sakamaki K et al Microwave ablation vs. single-needle radiofrequency ablation for the treatment of HCC up to 4 cm: a randomized-controlled trial. JHEP Rep. (2025) 7:101269. 10.1016/j.jhepr.2024.101269
Summary
Keywords
bilioptysis, bronchobiliary fistula (BBF), colon cancer, liver metastasis, percutaneous microwave ablation (PMWA)
Citation
Yang D, Zhang X, Wang G, Liu G and Yang J (2026) Successful occlusion of a bronchobiliary fistula using percutaneous microwave ablation: a case report. Front. Med. 13:1718950. doi: 10.3389/fmed.2026.1718950
Received
03 November 2025
Revised
13 January 2026
Accepted
14 January 2026
Published
02 February 2026
Volume
13 - 2026
Edited by
Francesco Lassandro, ASL Napoli 3 Sud, Italy
Reviewed by
Ying Chen, Kunming Medical University, China
Xianqiang Wang, PLA General Hospital, China
Updates
Copyright
© 2026 Yang, Zhang, Wang, Liu and Yang.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jundong Yang, 18653722620@163.comGuang Liu, maofeng14@126.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.