Abstract
Background:
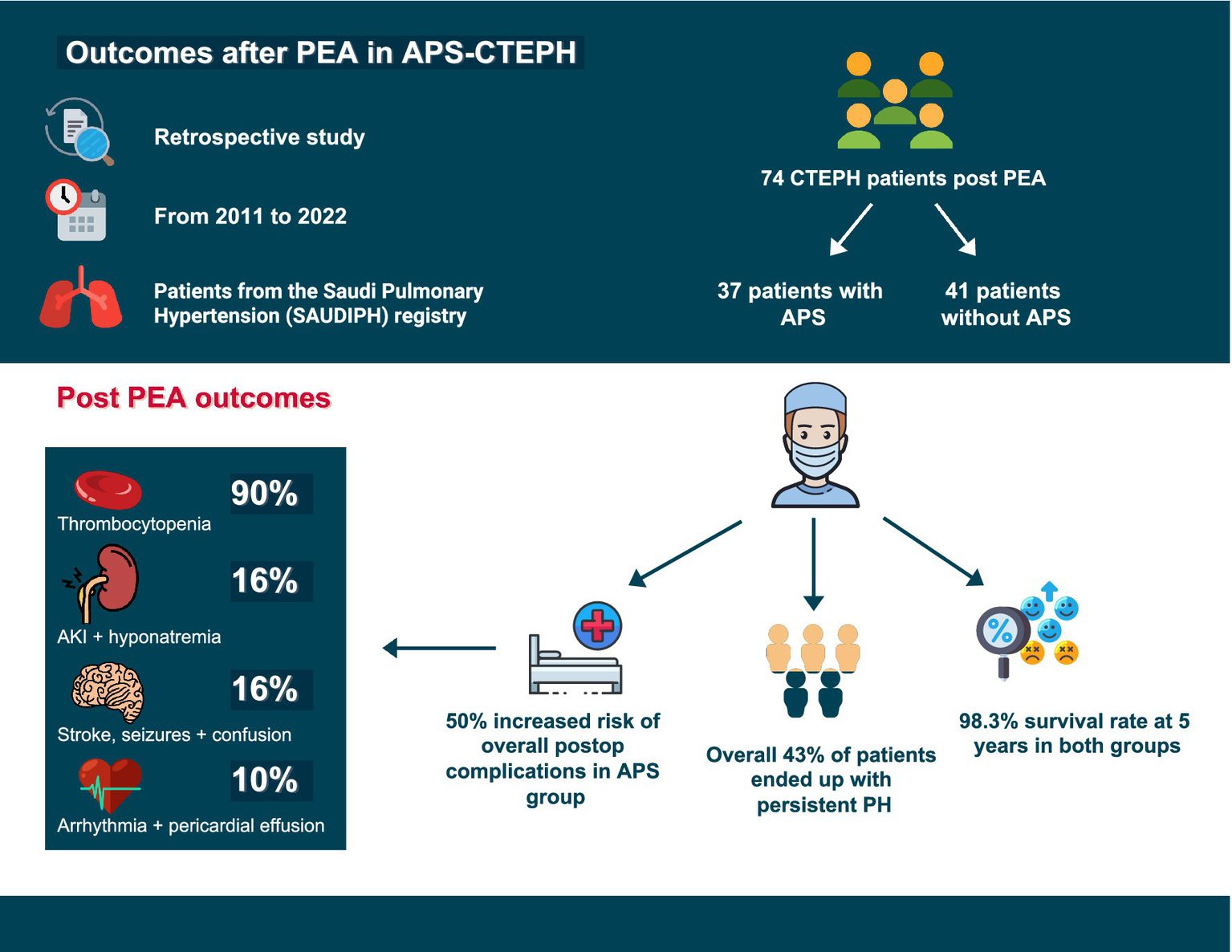
Antiphospholipid syndrome (APS) is associated with venous thromboembolism, which can lead to chronic thromboembolic pulmonary hypertension (CTEPH). Despite treatment with pulmonary endarterectomy (PEA), some patients continue to experience pulmonary hypertension (PH), which is potentially caused by APS-related distal vasculopathy. The aim of this study was to assess persistent PH after surgery and to investigate post PEA outcomes, including immediate postoperative complications, hospitalizations within 1 year of surgery, and mortality.
Methods:
We performed a retrospective analysis of adult patients with CTEPH who underwent PEA. We included patients with and without APS. Data were obtained from the Saudi Pulmonary Hypertension Registry (2011–2022). We assessed immediate postoperative complications, rehospitalizations within 1 year, and mortality. Additionally, we evaluated patients with right heart catheterization 1 year before and after PEA for persistent PH.
Results:
The study included 37 patients with APS-CTEPH and 41 patients without APS. Persistent PH was observed in 43% of patients, with no significant difference between the groups. Notably, patients in the APS-CTEPH group who received pulmonary vasodilator therapy before PEA had a reduced risk of developing persistent PH. Postoperative complications were significantly higher in the APS-CTEPH group (p = 0.002). Despite these risks, the 5-year survival rate was 98.3%, with no significant difference between the groups.
Conclusion:
APS is associated with a higher incidence of immediate postoperative complications and rehospitalizations within the 1st year after surgery. However, APS does not appear to increase the risk of persistent PH or affect long-term mortality in this cohort.
Graphical Abstract
Introduction
Antiphospholipid syndrome (APS) is a complex autoimmune disorder characterized by the persistent presence of antiphospholipid antibodies and a history of arterial or venous thrombotic events or specific pregnancy-related complications (1). APS often impacts the lungs in various ways, with pulmonary embolism (PE) being the most prevalent pulmonary manifestation (2). Throughout the disease course, 14.1% of APS patients experience PE (2, 3).
Pulmonary hypertension (PH) has emerged as the second most common pulmonary complication in patients with APS (4). The prevalence of PH in APS patients is 3.5% in those with primary APS and 1.8% in those with secondary APS (5). Chronic thromboembolic pulmonary hypertension (CTEPH) is notably prevalent among patients with APS because of their increased susceptibility to PE. Following PE, the incidence of developing CTEPH is estimated to be 3% (6, 7). The follow-up after acute PE trial reported a 2-year cumulative incidence of 2.3% (8). Additionally, APS is identified in 20% of CTEPH patients (9).
While various medical and interventional therapies are available, pulmonary endarterectomy (PEA) is the only curative treatment. PEA is the most effective treatment for patients with CTEPH who have operable disease (10). Patients who undergo PEA have significantly higher survival rates than those who do not undergo PEA (11, 12). Despite prior studies confirming the safety of PEA in patients with APS and describing immediate postoperative complications, there is a notable lack of data on long-term outcomes, specifically for the persistence or recurrence of PH after treatment with PEA (13–15).
In light of this, we hypothesized that patients diagnosed with APS and CTEPH (APS-CTEPH) may display distinct clinical characteristics and outcomes compared with patients diagnosed with CTEPH without APS (non-APS CTEPH) due to the underlying autoimmune conditions and chronic inflammation. This unique profile might result in more severe distal vasculopathy and vascular remodeling as well as World Health Organization Group I pulmonary arterial hypertension features, which could lead to a greater likelihood of persistent or recurrent PH following PEA, irrespective of the surgical technique employed. This scenario could result in a poorer long-term prognosis and increased mortality rate for patients with APS-CTEPH than for those with non-APS CTEPH.
Our study compared the baseline characteristics of the APS-CTEPH and non-APS CTEPH groups, investigated the short-term and long-term outcomes, specifically the risk of persistent disease, following PEA in each group, and identified predictors of adverse outcomes, particularly within the APS-CTEPH cohort.
Methods
Study design and population
We conducted a retrospective analysis of adult patients diagnosed with APS-CTEPH and non-APS CTEPH at our institution. Patients who had undergone PEA from 2011 to 2022 were identified from the Saudi Pulmonary Hypertension registry. The electronic health records were reviewed for potential inclusion in the final study population. The study was conducted in compliance with the Helsinki Declaration and was approved by the Institutional Review Board (RAC # 2231137).
We included adults over 18 years with APS-CTEPH or non-APS CTEPH who underwent PEA. APS was diagnosed per the American College of Rheumatology/European League Against Rheumatism criteria, and patients were seen at least once by a board-certified rheumatologist (16). The diagnosis of APS relies on clinical suspicion such as unexplained arterial or venous thrombosis or specific pregnancy morbidity followed by confirmatory laboratory testing. All patients must have at least one positive APS test (lupus anticoagulant, anticardiolipin antibodies [IgG and/or IgM, medium–high titer], or anti–β₂-glycoprotein I antibodies [IgG and/or IgM, medium–high titer]), and positivity must be persistent on two occasions at least 12 weeks apart (17). APS is confirmed when one clinical criterion and one persistent laboratory criterion are both present (17). CTEPH diagnosis required chronic clots on imaging (ventilation/perfusion scan and computed tomography chest angiogram) that was confirmed by a chest radiologist, and a PH diagnosis via right heart catheterization (RHC) per the 2022 ESC/ERS guidelines (12). Patients were excluded if they were in World Health Organization groups other than Group IV or had thrombophilia disorders except for APS. A total of 86 patients with CTEPH post-PEA were identified. Four were lost to follow-up, three had other hyperproliferative diseases (Factor V Leiden, protein C, and S deficiency), and one had combined CTEPH and congenital heart disease. The final number of patients included was 78.
Data collection
The following data were extracted from the electronic health records: Demographics; comorbidities; antiphospholipid status (primary vs. secondary); six-minute walk distance; computed tomography angiogram findings; echocardiography metrics; and hemodynamic parameters based on RHC. The clinical data collected included persistent PH, which was defined in our study as a mean pulmonary arterial pressure (mPAP) greater than 30 mmHg and pulmonary vascular resistance (PVR) over 2 Wood units. Given the lack of clearly established cutoffs for defining persistent pulmonary hypertension or guiding treatment initiation following pulmonary endarterectomy, we adopted a mPAP threshold of 30 mmHg, consistent with clinical practice and the level at which most pulmonary hypertension experts would consider initiating pulmonary vasodilator therapy (18, 19). These parameters were measured during the first postoperative RHC within the 1st year after surgery. Notably, prior studies, including a meta-analysis published in 2018, have highlighted the lack of a consistent or universally accepted definition of persistent disease (20).
Postoperative complications were categorized into hematological (thrombocytopenia), metabolic (hyponatremia and acute kidney injury), neurological (seizures, confusion, and strokes), and cardiac (arrhythmia and pericardial effusion/tamponade). This classification was based on existing literature that systematically details the spectrum of complications observed in patients with APS undergoing cardiac surgeries (21–24). Hematological and metabolic changes were considered surgery-related if they were observed within 5 days post-surgery. Thrombocytopenia was defined as a platelet count of less than 150 × 10 (9)/L, while severe thrombocytopenia was defined as a platelet count of less than 50 × 10 (9)/L. Hyponatremia was defined as a sodium level of less than 135 mEq/L. Complications were recorded as either absent or present, with the latter indicating the occurrence of one or more complications. We collected the number of hospitalizations/events after discharge from PEA admission during the 1st year following discharge. Additionally, we collected data on changes in hemodynamics before and after surgery via RHC data collected within 1 year before and after surgery.
Statistical analysis
We used R software for statistical analysis. Descriptive data were presented as means and standard deviations for continuous variables and as frequencies and percentages for categorical variables. Statistical significance was set at a p value of < 0.05. The Mantel–Haenszel method estimated risk or odds ratios. Kaplan–Meier curves were used for survival analysis from the surgery date until death.
We compared immediate postoperative complications, hospitalizations within 1 year after surgery, persistent PH, and mortality between the APS-CTEPH and non-APS CTEPH groups. Outcomes were adjusted for comorbidities, thromboembolic events, and pre-surgery pulmonary vasodilator therapy. The risk of hospitalization within 1-year post-discharge from PEA admission and the survival rate after surgery were analyzed. To more accurately evaluate persistent PH and hemodynamic changes before and after surgery, we included only the hemodynamic data from patients who underwent RHC within 1 year before and after surgery. This criterion was met by 40 out of 74 patients, and the others were excluded from this part of the analysis.
Results
Patient characteristics
Our study included 37 patients with APS-CTEPH and 41 patients with non-APS CTEPH who underwent PEA between 2011 and 2022 (Table 1). Our patients were predominantly female (73%). The mean age was 34.5 (± 10.9) years in the APS-CTEPH group and 33 (± 10.7) years in the non-APS CTEPH group. Most patients were classified as New York Heart Association functional class II-III. More than 50% of patients in both groups were receiving pulmonary vasodilator therapy before surgery. The history of venous thromboembolism episodes is detailed in Table 1. Among patients with APS-CTEPH, 86% demonstrated double or triple antiphospholipid antibody positivity, equally distributed between double (43%) and triple (43%) positivity. Interestingly, systemic lupus erythematosus was the only connective tissue disease associated with secondary APS in our cohort, consistent with its well-recognized association as the most common CTD linked to APS (1, 25). Approximately 65% of patients with APS-CTEPH were treated with immunosuppressive and/or immune-modulating therapy. Hydroxychloroquine was the most common type of therapy (Supplementary Tables 1, 2). The patients underwent surgery at various locations including 78% of patients at our center, 19% in the United States, and 3% in Europe.
Table 1
| Baseline characteristics | APS-CTEPH, n (% among n = 37) | Non-APS CTEPH, n (% among n = 41) |
|---|---|---|
| Age at CTEPH diagnosis | 34.5 ± 9.5 | 33 ± 10.61 |
| Sex | ||
| Female | 26 (70.0) | 31 (75.6) |
| Male | 11 (30.0) | 10 (24.4) |
| Comorbidities | ||
| DM | 3 (8.1) | 3 (7.3) |
| HTN | 2 (5.4) | 5 (12.2) |
| Heart failure | 4 (10.8) | 1 (2.4) |
| CKD | 4 (10.8) | 3 (7.3) |
| Seizures | 3 (8.1) | 1 (2.4) |
| CTD | 10 (27.0) | 0 (0) |
| NYHA FC at CTEPH diagnosis | ||
| FC I | 0 (0) | 1 (2.4) |
| FC II | 11 (30.0) | 13 (31.7) |
| FC III | 20 (54.0) | 21 (51.2) |
| FC IV | 6 (16.0) | 6 (14.6) |
| History of DVT only | ||
| Single | 0 (0) | 0 (0) |
| Multiple | 2 (5.4) | 2 (6.0) |
| History of PE only | ||
| Single | 9 (24.3) | 19 (54.0) |
| Multiple | 2 (5.4) | 7 (20.0) |
| History of DVT and PE | ||
| Single DVT and PE | 8 (21.6) | 4 (11.0) |
| Multiple DVTs and single PE | 4 (10.8) | 1 (3.0) |
| Multiple PEs with ≥ 1 DVT | 10 (27.0) | 2 (6.0) |
| ProBNP at PEA in pg./ml | 1,002 ± 1,014 | 810 ± 901 |
| Most recent 6MWT before PEA | 202 ± 151 | 219 ± 118 |
| Hemodynamics at CTEPH diagnosis | ||
| RA in mmHg | 14.47 ± 6.50 | 12.38 ± 5.95 |
| mPAP in mmHg | 51.00 ± 20.00 | 52.72 ± 11.28 |
| PAWP in mmHg | 13.77 ± 4.41 | 13.68 ± 6.13 |
| PVR in Wood Units | 12.05 ± 7.00 | 12.42 ± 7.52 |
| CO in L/min/CI | 3.29 ± 0.83 | 3.74 ± 1.26 |
| CI in L/min/m2 | 1.87 ± 0.35 | 1.97 ± 0.60 |
| SvO2% | 56.00 ± 10.00 | 57.58 ± 9.64 |
| Most recent echocardiography before PEA | ||
| RV size | ||
| Normal | 4 (10.8) | 5 (12.5) |
| Mild dilation | 6 (16.2) | 3 (7.5) |
| Moderate dilation | 10 (27.0) | 8 (20.0) |
| Severe dilation | 17 (46.0) | 24 (60.0) |
| RV function | ||
| Normal | 4 (11.0) | 9 (22.5) |
| Mild dysfunction | 11 (30.0) | 5 (12.5) |
| Moderate dysfunction | 10 (27.0) | 10 (25.0) |
| Severe dysfunction | 12 (32.0) | 16 (40.0) |
| CT chest findings before PEA | ||
| Acute on chronic PE | 3 (8.3) | 4 (10.5) |
| Mosaic attenuation | 28 (77.8) | 37 (97.4) |
| Pulmonary infarctions | 7 (19.4) | 7 (18.4) |
| Collaterals | 9 (25.0) | 0 (0) |
| Pulmonary vasodilator therapies | ||
| On therapy | 20 (54.0) | 26 (63.5) |
| Monotherapy | 9 (24.0) | 11 (27.0) |
| Combination | 11 (30.0) | 15 (36.5) |
| Type of pulmonary vasodilator therapy | ||
| Sildenafil | 14 (70.0) | 16 (61.5) |
| Bosentan | 6 (30.0) | 9 (34.6) |
| Macitentan | 5 (25.0) | 7 (27.0) |
| Riociguat | 3 (15.0) | 6 (23.0) |
| Iloprost | 5 (25.0) | 2 (7.6) |
| Type of AC | ||
| DOAC | 4 (11.0) | 23 (56.1) |
| Warfarin | 30 (81.0) | 16 (39.0) |
| LMWH | 3 (8.0) | 2 (4.9) |
| History of noncompliance with AC | 2 (5.4) | 1 (2.4) |
Baseline characteristics of patients diagnosed with chronic thromboembolic pulmonary hypertension with and without antiphospholipid syndrome before pulmonary endarterectomy.
6MWT, 6-min walk test; AC, Anticoagulation; APS, Antiphospholipid syndrome; CI, Cardiac index; CKD, Chronic kidney disease seizures; CO, Cardiac output; CT, Computed tomography; CTD, Connective tissue disease; CTEPH, Chronic thromboembolic pulmonary hypertension; DM, Diabetes mellitus; DOAC, Direct oral anticoagulants; DVT, Deep vein thrombosis; FC, Functional class; HTN, Hypertension heart failure; LMWH, Low molecular weight heparin; mPAP, Mean pulmonary artery pressure; NYHA, New York Heart Association; PAWP, Pulmonary artery wedge pressure; PE, Pulmonary embolism; PEA, Pulmonary endarterectomy; ProBNP, N-terminal pro b-type natriuretic peptide; PVR, Pulmonary vascular resistance; RA, Right atrium; RV, Right ventricle; SvO2, Mixed venous oxygen saturation.
To evaluate persistent PH after PEA, we included patients who underwent RHC within the 1st year, with a focus on persistent rather than recurrent PH. Approximately 43% of patients exhibited persistent disease, with no significant difference between the APS-CTEPH and non-APS CTEPH groups (p = 0.5) (Figure 1). Notably, the risk ratio for patients with APS-CTEPH receiving pulmonary vasodilator therapy before PEA was 0.52 [95% confidence interval (CI): 0.28–0.97] and was 2.65 (95%CI: 0.63–11.19) for those not receiving therapy. These values were significantly different from each other (p = 0.04). Approximately 32% of patients in both groups were on combination therapy after surgery.
Figure 1

Percentage of patients with persistent pulmonary hypertension (PH) according to antiphospholipid syndrome (APS) status.
Postoperative complications, hospitalizations, and mortality
Postoperative hematological, metabolic, neurological, and cardiac complications were analyzed. Patients with non-APS CTEPH had a significantly lower risk of post-PEA complications (60.0%) than patients with APS-CTEPH (93.6%), which corresponded to a risk ratio of 1.56 (95%CI: 1.15–2.12; p = 0.002). Thrombocytopenia was common in both groups after surgery (90% in the APS-CTEPH group vs. 45% in the non-APS CTEPH group) but was more severe in the APS-CTEPH group. Renal and neurological complications occurred in 16% of patients with APS-CTEPH, and cardiac complications occurred in 10% of patients with APS-CTEPH. Pulmonary vasodilator therapy before PEA did not significantly impact the occurrence of complications (p = 0.11). Additionally, hospitalization rates within the 1st year after surgery were higher in the APS-CTEPH group (p = 0.016). Mortality post-PEA was recorded at 3.0 years, 5.9 years, 6.5 years, and 10.0 years, with a 5-year survival rate of 98.3% and a lower confidence limit for true survival of 88.4%, with no statistically significant differences (p = 0.26 between the APS-CTEPH and non-APS CTEPH groups) (Figures 2, 3).
Figure 2
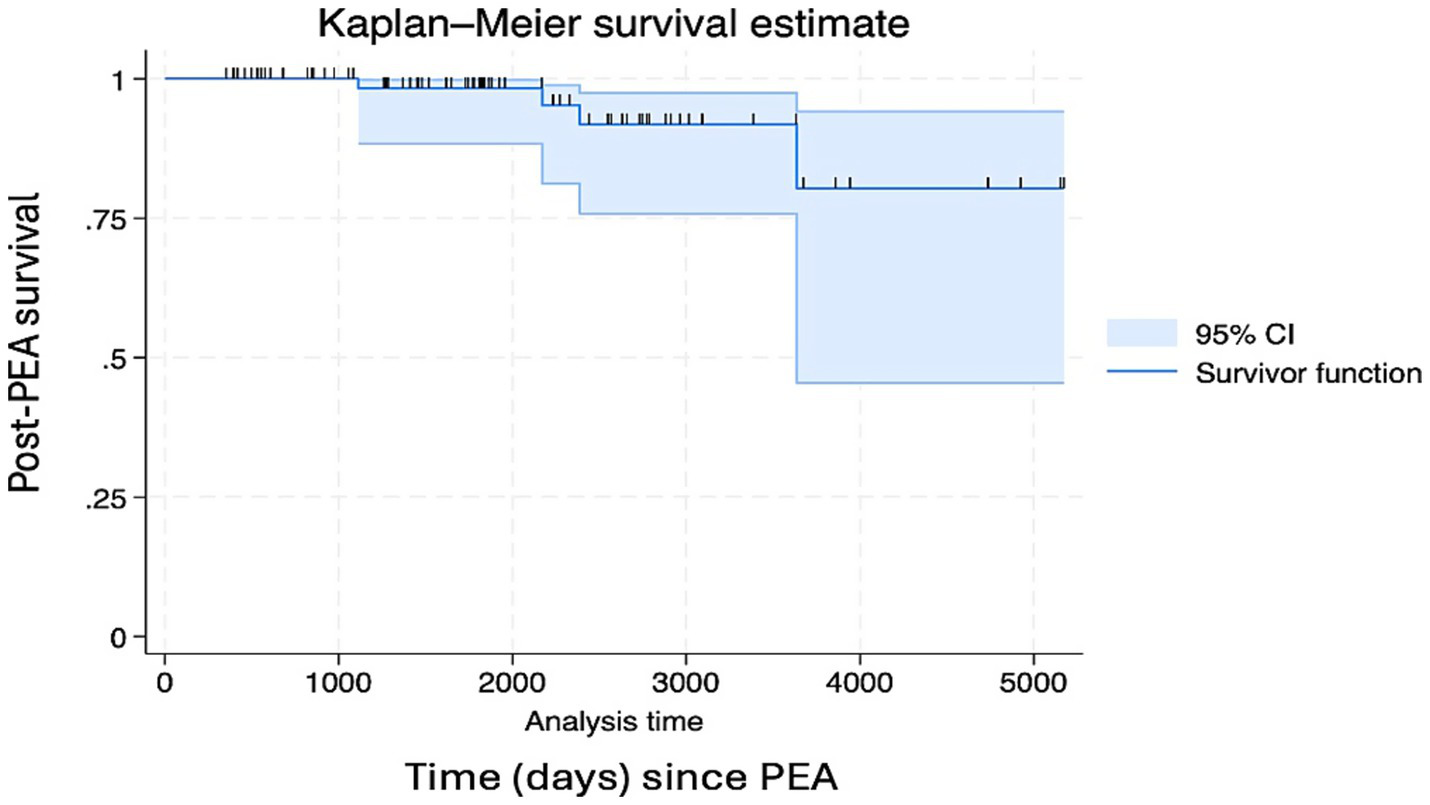
Post-surgery survival of the overall chronic thromboembolic pulmonary hypertension (CTEPH) group.
Figure 3
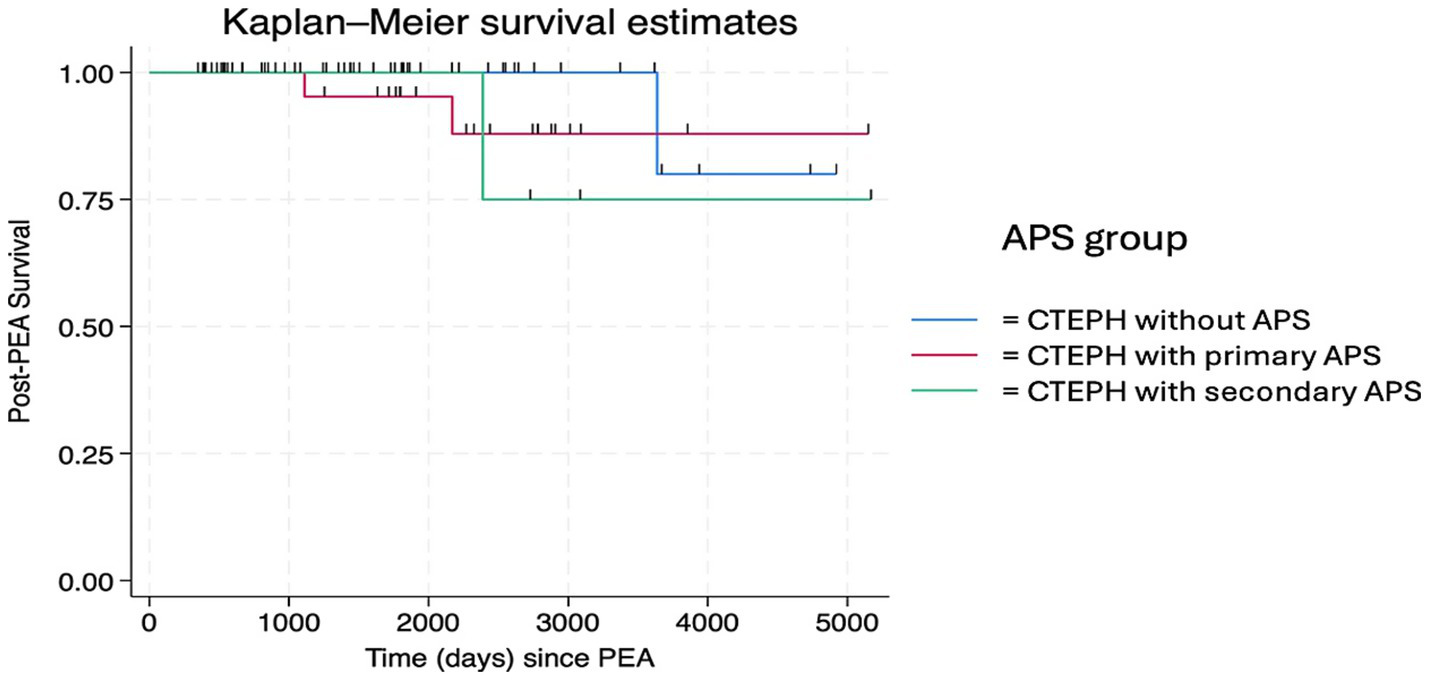
Post-surgery survival of chronic thromboembolic pulmonary hypertension (CTEPH) subgroups according to antiphospholipid syndrome (APS) status: non-, primary, and secondary.
First hemodynamic evaluation after PEA
Both groups exhibited statistically significant improvements in hemodynamics following surgery (p < 0.0001). Specifically, there was a 29% decrease in mPAP, a 54% decrease in PVR, a 19% increase in the cardiac index, and an 18% increase in mixed venous saturation (SvO2). No significant differences were observed between the two groups except for the change in SvO2 in the APS-CTEPH group (p = 0.02) (Table 2 and Supplementary Table 3).
Table 2
| Characteristics of post-PEA | APS-CTEPH, n (% among n = 37) | Non-APS CTEPH, n (% among n = 41) | |
|---|---|---|---|
| Primary (n = 27) | Secondary (n = 10) | ||
| Age in years at PEA surgery | 36.7 ± 10.0 | 35.0 ± 9.0 | 37.9 ± 11.0 |
| Days from diagnosis to PEA surgery | 257 ± 593 | 652 ± 1,147 | 349 ± 423 |
| Site of PEA surgery | |||
| KSA | 24 | 7 | 30 |
| USA | 2 | 2 | 11 |
| Europe | 1 | 1 | 0 |
| Hemodynamics at first follow-up RHC | |||
| RA in mmHg | 9.0 ± 4.0 | 11.0 ± 4.0 | 10.0 ± 4.4 |
| mPAP in mmHg | 32.0 ± 10.0 | 27.0 ± 6.5 | 34.0 ± 14.0 |
| PAWP in mmHg | 12.0 ± 2.6 | 14.0 ± 3.2 | 14.0 ± 5.0 |
| PVR in Wood units | 5.7 ± 3.6 | 3.4 ± 2.0 | 4.0 ± 1.1 |
| CO in L/min | 3.9 ± 1.1 | 4.0 ± 1.1 | 4.0 ± 1.1 |
| CI in L/min/m2 | 2.0 ± 0.4 | 2.2 ± 0.5 | 2.2 ± 0.5 |
| SvO2% | 64.0 ± 7.0 | 65.0 ± 6.0 | 65.5 ± 7.0 |
| Echocardiography at follow-up | |||
| RV size | |||
| Normal | 9 (33) | 5 (50) | 16 (39) |
| Mild dilation | 11 (41) | 3 (30) | 13 (32) |
| Moderate dilation | 5 (19) | 2 (20) | 7 (17) |
| Severe dilation | 2 (7) | 0 (0) | 5 (12) |
| RV function | |||
| Normal | 8 (30) | 4 (40) | 11 (27) |
| Mild dysfunction | 11 (41) | 2 (20) | 15 (37) |
| Moderate dysfunction | 6 (22) | 4 (40) | 10 (24) |
| Severe dysfunction | 2 (7) | 0 (0) | 5 (12) |
| Pulmonary vasodilator therapies | |||
| Monotherapy | 9 (33) | 3 (30) | 9 (22) |
| Combination | 6 (22) | 1 (10) | 13 (32) |
| Type of pulmonary vasodilator therapy | |||
| Riociguat | 9 (60) | 0 (0) | 17 (77) |
| Macitentan | 9 (60) | 4 (100) | 16 (73) |
| Sildenafil | 3 (20) | 1 (25) | 2 (9) |
| Selexipag | 0 (0) | 0 (0) | 2 (9) |
| Iloprost | 0 (0) | 0 (0) | 1 (5) |
| SC Treprostinil | 1 (10) | 0 (0) | 0 (0) |
| Type of AC | |||
| DOAC | 2 | 2 | 24 |
| Warfarin | 23 | 6 | 17 |
| Enoxaparin | 2 | 2 | 0 |
Characteristics of patients diagnosed with chronic thromboembolic pulmonary hypertension with and without antiphospholipid syndrome after pulmonary endarterectomy.
AC, Anticoagulant; APS, Antiphospholipid syndrome; CO/CI, Cardiac output/cardiac index; CTEPH, Chronic thromboembolic pulmonary hypertension; DOAC, Direct oral anticoagulant; KSA, Kingdom of Saudi Arabia; mPAP, Mean pulmonary artery pressure; PAWP, Pulmonary artery wedge pressure; PEA, Pulmonary endarterectomy; PVR, Pulmonary vascular resistance; RA, Right atrium; RHC, Right heart catheterization; RV, Right ventricle; SvO2, Mixed venous oxygen saturation; USA, United States of America.
Discussion
In this study, we assessed the immediate and long-term outcomes of patients diagnosed with CTEPH both with and without APS after treatment with PEA. The patients in the APS-CTEPH group in our study were young, which is consistent with the literature (13). However, the patients in the non-APS CTEPH group were significantly younger than those previously reported in Western countries (26). Our findings showed that treatment with PEA resulted in significant hemodynamic improvements in both groups. However, the APS-CTEPH group demonstrated a statistically significant improvement in SvO2 compared with the non-APS CTEPH group (p = 0.02), suggesting a greater impact on cardiac function and tissue oxygenation in patients with APS.
Patients in the APS-CTEPH group faced a significantly greater risk of immediate postoperative complications than patients in the non-APS CTEPH group. The risk ratio was 1.56 (95%CI: 1.15–2.12; p = 0.002). This represents an approximately 50% increased risk for the patients in the APS-CTEPH group. Postoperative thrombocytopenia was significantly more prevalent in the APS-CTEPH group, affecting 90% of patients. We observed that 22.5% of patients experienced a severe case where platelet counts fell below 50 × 10 (9)/L, and interventions such as corticosteroids and intravenous immunoglobulin were required. This complication, observed exclusively in the APS-CTEPH group, presented considerable challenges due to the need for continuous anticoagulation and the heightened risk of bleeding. Additionally, more serious complications in the APS-CTEPH group included neurological issues such as stroke or confusion. Hyponatremia was common but not severe, as indicated by a nadir postoperative sodium level of 130 mEq/L. Our findings aligned with the current literature (14, 15, 27). However, we found that an increased risk of postoperative complications led to a higher rate of hospitalization within the 1st year after surgery. In our cohort, 9% of patients required hospitalization within the 1st year after undergoing PEA. Hospitalization causes included APS flare, cerebellar hematoma, pericardial effusion/tamponade, and sepsis.
Previous studies have linked autoimmunity in APS with distal vasculopathy. It has been observed that pulmonary arterial hypertension has been thought to initially be CTEPH but was later found to be associated with primary APS (28–30). We hypothesized that patients in the APS-CTEPH group would have an increased risk of developing persistent PH after surgery. In our cohort of 37 patients with APS-CTEPH, nearly half had triple antiphospholipid antibody positivity, indicating a highly thrombogenic group (17). Although 43% of patients had persistent PH at their first postoperative follow-up RHC within the 1st year after PEA, there was no significant difference between the APS-CTEPH and non-APS CTEPH groups. Data from U. S. and European CTEPH registries show that persistent PH after PEA occurs in a proportion of patients, with reported prevalence ranging from approximately 17 to 51%, depending on the definition and timing of reassessment (18, 31). In the International CTEPH Registry, Hoeper et al. reported persistent PH in 16.7% of patients, defined as mPAP ≥25 mm Hg at the end of intensive care (31). Rates of persistent PH increase with later evaluation and stricter hemodynamic criteria, reaching 31% at 1 year post-PEA in the European cohort reported by Skoro-Sajer et al. (33) and 51% at 3–6 months in the UK National CTEPH Cohort (18). Similarly, Freed et al. reported elevated mPAP (≥30 mm Hg) at 3 months post-PEA in 31% of patients (32). Persistent PH was observed in 43% of our patients, which lies toward the higher end of rates reported in international registries. Potential reasons include a distinct patient population characterized by a high prevalence of APS, prolonged disease duration prior to referral, and a high operability rate, with approximately 75% of CTEPH patients undergoing PEA during a period when PEA was the primary therapeutic intervention at our center. Surgical specimen classification is not available for our patients, precluding further characterization of disease distribution or assessment of whether a substantial proportion had predominantly distal disease contributing to persistent pulmonary hypertension. This is clinically relevant given prior data from a Canadian cohort, which reported residual pulmonary hypertension in up to 38% of patients with CTEPH after PEA, particularly among those with more distal disease involvement (type 3 disease, originating at the segmental pulmonary artery branches) (33). Postoperatively, patients with persistent PH were treated with pulmonary vasodilator therapy, as balloon pulmonary angioplasty was not available during the study period and was only established in 2025.
Interestingly, patients in the APS-CTEPH group treated with pulmonary vasodilator therapy before surgery had a significantly lower risk of developing persistent PH than those who did not receive this treatment. We hypothesized that preoperative pulmonary vasodilator treatment could facilitate surgery by making the procedure technically easier for the surgeon and enabling the removal of more fibrotic clots, particularly in patients with lower pulmonary pressures. Our results accounted for potential confounders such as surgical timing (> 5 vs. 5 ≤ years), confirming that surgical technique did not influence outcomes (p = 0.85). Interestingly, the number of PE episodes did not affect the risk of persistent PH, suggesting that a history of multiple PEs does not necessarily lead to more distal vasculopathy than a single episode. Moreover, presurgery hemodynamics, such as elevated mPAP or PVR, did not predict the development of persistent PH in either group, which was contrary to what has been reported in the literature (34).
In experienced centers, the perioperative mortality risk following PEA is less than 2.5%, which is attributed to advancements in managing cardiac and pulmonary complications (28). Prior studies have documented the safety of PEA in patients with APS, highlighting a low risk of mortality that is comparable to patients without APS. Rosen et al. (14) reported significant functional and hemodynamic improvements after PEA with a survival rate of approximately 87%. Mortality in their cohort was related to advanced disease and surgical urgency. Long-term follow-up (median: 41 months) revealed that 38% of survivors required pulmonary vasodilators for persistent PH (14). Taş et al. (15) reported a 6.25% risk of late mortality primarily due to coronavirus disease 2019 pneumonia. They also observed persistent PH in 12.5% of their patients during follow-up (mean: 75 months). Camous et al. (27) reported a 30-day mortality rate of 5.9%, with no significant difference between patients with APS-CTEPH and controls.
Our cohort consisted of a moderately ill group of patients, with a mean mPAP of 50 mmHg and a mean PVR of 12 Wood units. According to the literature, these parameters are associated with an increased risk of mortality (35–37). Despite this, our patients achieved statistically significant hemodynamic improvements in both groups (p < 0.0001), with no significant difference in mortality between the APS-CTEPH and non-APS CTEPH groups. Post-PEA deaths were recorded at 3.0 years, 5.9 years, 6.5 years, and 10.0 years after surgery. The observed 5-year survival rate after PEA was 98.3%, with a lower limit for true survival of 88.4%, confirming previous findings in the literature (37–39).
Our study thoroughly addressed the outcomes, specifically persistent PH, between the APS-CTEPH and non-APS CTEPH groups. However, this study had several limitations, such as its retrospective nature and small cohort size. Additionally, we observed that there were missing data especially after converting patient records from charts to electronic formats. Patients missing postoperative data who were treated with PEA outside Saudi Arabia were eliminated from some parts of the analysis. Moreover, detailed surgical specimen classification was not available in this retrospective cohort, limiting our ability to accurately characterize disease distribution. Finally, the variability in the timing of follow-up studies, such as RHC and echocardiography before and after surgery, made it difficult to establish a unified timeline for assessing specific outcomes.
Conclusion
Patients in the APS-CTEPH experienced a greater incidence of immediate postoperative complications and consequently hospitalizations within the 1st year following treatment with PEA. However, the risk of persistent PH or mortality did not increase compared with the patients in the non-APS CTEPH group. Further research involving larger patient cohorts is necessary to validate these findings and to develop strategies for improving outcomes for these patients.
Statements
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Research Ethics Committee (RAC #2231137) at King Faisal Specialist Hospital and Research Centre, Riyadh, Saudi Arabia, and was also approved for publication. Verbal consent was obtained from all patients for inclusion in the Saudi PH registry and participation in research. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
NA: Writing – review & editing, Investigation, Writing – original draft, Project administration, Resources, Methodology, Visualization, Data curation, Conceptualization. FKA: Visualization, Resources, Methodology, Conceptualization, Writing – review & editing, Supervision. KM: Project administration, Resources, Investigation, Writing – original draft, Writing – review & editing, Methodology, Data curation, Conceptualization. FayA: Conceptualization, Writing – review & editing, Methodology, Data curation. NA: Writing – review & editing, Methodology, Data curation, Conceptualization. HZ: Data curation, Conceptualization, Writing – review & editing, Methodology. HA: Writing – review & editing, Conceptualization, Methodology, Data curation. FatA: Resources, Data curation, Methodology, Writing – review & editing, Investigation, Conceptualization. MH: Writing – review & editing, Methodology, Investigation, Conceptualization, Data curation. PH: Conceptualization, Data curation, Supervision, Writing – review & editing, Methodology, Investigation, Visualization. EV: Visualization, Formal analysis, Data curation, Conceptualization, Methodology, Writing – review & editing, Supervision, Investigation. AA: Data curation, Writing – review & editing, Conceptualization, Methodology.
Funding
The author(s) declared that financial support was not received for this work and/or its publication.
Conflict of interest
The author(s) declared that this work was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declared that Generative AI was not used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2026.1736115/full#supplementary-material
Abbreviations
APS, Antiphospholipid syndrome; CTEPH, Chronic thromboembolic pulmonary hypertension; PE, Pulmonary embolism; PEA, Pulmonary endarterectomy; PH, Pulmonary hypertension; RHC, Right heart catheterization; SvO2, Mixed venous oxygen saturation.
References
1.
Garcia D Erkan D . Diagnosis and management of the antiphospholipid syndrome. N Engl J Med. (2018) 378:2010–21. doi: 10.1056/NEJMra1705454,
2.
Espinosa G Cervera R Font J Asherson RA . The lung in the antiphospholipid syndrome. Ann Rheum Dis. (2002) 61:195–8. doi: 10.1136/ard.61.3.195,
3.
Shi M Gao W Jin Y Zhu J Liu Y Wang T et al . Antiphospholipid syndrome-related pulmonary embolism: clinical characteristics and early recognition. Front Cardiovasc Med. (2022) 9:872523. doi: 10.3389/fcvm.2022.872523,
4.
Maioli G Calabrese G Capsoni F Gerosa M Meroni PL Chighizola CB . Lung disease in antiphospholipid syndrome. Semin Respir Crit Care Med. (2019) 40:278–94. doi: 10.1055/s-0039-1683994,
5.
Stojanovich L . Pulmonary manifestations in antiphospholipid syndrome. Autoimmun Rev. (2006) 5:344–8. doi: 10.1016/j.autrev.2006.02.002,
6.
Yang J Madani MM Mahmud E Kim NH . Evaluation and management of chronic thromboembolic pulmonary hypertension. Chest. (2023) 164:490–502. doi: 10.1016/j.chest.2023.03.029,
7.
Pengo V Lensing AWA Prins MH Lensing AW Marchiori A Davidson BL et al . Incidence of chronic thromboembolic pulmonary hypertension after pulmonary embolism. N Engl J Med. (2004) 350:2257–64. doi: 10.1056/NEJMoa032274,
8.
Lang IM Artner T . FOCUS on sequelae of acute pulmonary embolism: does it pay off?Eur Heart J. (2022) 43:3399–401. doi: 10.1093/eurheartj/ehac170
9.
Wolf M Boyer-Neumann C Parent F Eschwege V Jaillet H Meyer D et al . Thrombotic risk factors in pulmonary hypertension. Eur Respir J. (2000) 15:395–9. doi: 10.1034/j.1399-3003.2000.15b28.x,
10.
Dartevelle P Fadel E Mussot S Chapelier A Hervé P de Perrot M et al . Chronic thromboembolic pulmonary hypertension. Eur Respir J. (2004) 23:637–48. doi: 10.1183/09031936.04.00079704,
11.
Delcroix M Lang I Pepke-Zaba J Jansa P D'Armini AM Snijder R et al . Long-term outcome of patients with chronic thromboembolic pulmonary hypertension: results from an international prospective registry. Circulation. (2016) 133:859–71. doi: 10.1161/CIRCULATIONAHA.115.016522,
12.
Humbert M Kovacs G Hoeper MM Badagliacca R Berger RMF Brida M et al . 2022 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Respir J. (2023) 61:2200879. doi: 10.1183/13993003.00879-2022
13.
Jiang X Du Y Cheng CY Denas G Zhou Y-P Wu T et al . Antiphospholipid syndrome in chronic thromboembolic pulmonary hypertension: a well-defined subgroup of patients. Thromb Haemost. (2019) 119:1403–8. doi: 10.1055/s-0039-1692428,
14.
Rosen K Raanani E Kogan A Kenet G Misgav M Lubetsky A et al . Chronic thromboembolic pulmonary hypertension in patients with antiphospholipid syndrome: risk factors and management. J Heart Lung Transplant. (2022) 41:208–16. doi: 10.1016/j.healun.2021.10.016,
15.
Taş S Antal A Durusoy AF Yanartaş M Yıldız K Olgun Yıldızeli Ş et al . Pulmonary endarterectomy in patients with antiphospholipid syndrome-associated chronic thromboembolic pulmonary hypertension. Anatol J Cardiol. (2021) 26:394–400. doi: 10.5152/AnatolJCardiol.2021.1138
16.
Barbhaiya M Zuily S Naden R Hendry A Manneville F Amigo M‐C et al . The 2023 ACR/EULAR antiphospholipid syndrome classification criteria. Arthritis Rheumatol. (2023) 75:1687–702. doi: 10.1002/art.42624,
17.
Negrini S Pappalardo F Murdaca G , Indiveri, F, and Puppo, F. The antiphospholipid syndrome: from pathophysiology to treatment. Clin Exp Med. (2016) 16:305–21. doi: 10.1007/s10238-016-0430-5
18.
Cannon JE Su L Kiely DG Page K Toshner M Swietlik E et al . Dynamic risk stratification of patient long-term outcome after pulmonary endarterectomy: results from the United Kingdom national cohort. Circulation. (2016) 133:1761–71. doi: 10.1161/CIRCULATIONAHA.115.019470,
19.
Freed DH Thomson BM Berman M Tsui SS Dunning J Sheares KK et al . Survival after pulmonary thromboendarterectomy: effect of residual pulmonary hypertension. J Thorac Cardiovasc Surg. (2011) 141:383–7. doi: 10.1016/j.jtcvs.2009.12.056,
20.
Hsieh WC Jansa P Huang WC Nižnanský M Omara M Lindner J . Residual pulmonary hypertension after pulmonary endarterectomy: a meta-analysis. J Thorac Cardiovasc Surg. (2018) 156:1275–87. doi: 10.1016/j.jtcvs.2018.04.110,
21.
Ciocca RG Choi J Graham AM . Antiphospholipid antibodies lead to increased risk in cardiovascular surgery. Am J Surg. (1995) 170:198–200. doi: 10.1016/s0002-9610(99)80285-2,
22.
Gorki H Malinovski V Stanbridge RD . The antiphospholipid syndrome and heart valve surgery. Eur J Cardiothorac Surg. (2008) 33:168–81. doi: 10.1016/j.ejcts.2007.11.004,
23.
Berkun Y Elami A Meir K Mevorach D Naparstek Y . Increased morbidity and mortality in patients with antiphospholipid syndrome undergoing valve replacement surgery. J Thorac Cardiovasc Surg. (2004) 127:414–20. doi: 10.1016/j.jtcvs.2003.07.016,
24.
Erkan D Leibowitz E Berman J Lockshin M . Perioperative medical management of antiphospholipid syndrome: Hospital for Special Surgery experience, review of literature, and recommendations. J Rheumatol. (2002) 29:843–9.
25.
Alturaif N Alduraibi FK . CTD-PAH: an updated practical approach to screening, diagnosis, and management. Ther Adv Respir Dis. (2025) 19:17534666251385674. doi: 10.1177/17534666251385674,
26.
Kerr KM Elliott C Chin K Elliott CG Benza RL Channick RN et al . Results from the United States chronic thromboembolic pulmonary hypertension registry. Chest. (2021) 160:1822–31. doi: 10.1016/j.chest.2021.05.052,
27.
Camous J Decrombecque T Louvain-Quintard V Doubine S Dartevelle P Stéphan F . Outcomes of patients with antiphospholipid syndrome after pulmonary endarterectomy. Eur J Cardiothorac Surg. (2013) 46:116–20. doi: 10.1093/ejcts/ezt572,
28.
Riboldi P Gerosa M Raschi E Testoni C Meroni PL . Endothelium as a target for antiphospholipid antibodies. Immunobiology. (2003) 207:29–36. doi: 10.1078/0171-2985-00211,
29.
Parthvi R Sikachi RR Agrawal A Adial A Vulisha A Khanijo S et al . Pulmonary hypertension associated with antiphospholipid antibody: call for a screening tool?Intractable Rare Dis Res. (2017) 6:163–71. doi: 10.5582/irdr.2017.01044,
30.
Yeo J Shin N Ahn KJ Seo M Jang AY Kim M et al . Pulmonary arterial hypertension due to antiphospholipid syndrome initially mimicking chronic thromboembolic pulmonary hypertension. Clin Hypertens. (2022) 28:10. doi: 10.1186/s40885-021-00191-1,
31.
Hoeper MM Madani MM Nakanishi N Meyer B Cebotari S Rubin LJ . Chronic thromboembolic pulmonary hypertension. Lancet Respir Med. (2014) 2:573–82. doi: 10.1016/S2213-2600(14)70089-X,
32.
Skoro-Sajer N Hack N Sadushi-Koliçi R Bonderman D Jakowitsch J Klepetko W et al . Pulmonary vascular reactivity and prognosis in patients with chronic thromboembolic pulmonary hypertension: a pilot study. Circulation. (2009) 119:298–305. doi: 10.1161/CIRCULATIONAHA.108.794610,
33.
Freed DH Thomson BM Berman M Tsui SS Dunning J Sheares KK et al . Survival after pulmonary thromboendarterectomy: effect of residual pulmonary hypertension. J Thorac Cardiovasc Surg. (2011) 141:383–7. doi: 10.1016/j.jtcvs.2009.12.056,
34.
Ishida K Masuda M Tanabe N Matsumiya G Tatsumi K Nakajima N . Long-term outcome after pulmonary endarterectomy for chronic thromboembolic pulmonary hypertension. J Thorac Cardiovasc Surg. (2012) 144:321–6. doi: 10.1016/j.jtcvs.2011.09.004,
35.
Condliffe R Kiely DG Gibbs JR Corris PA Peacock AJ Jenkins DP et al . Improved outcomes in medically and surgically treated chronic thromboembolic pulmonary hypertension. Am J Respir Crit Care Med. (2008) 177:1122–7. doi: 10.1164/rccm.200712-1841OC,
36.
Lankeit M Krieg V Hobohm L Kölmel S Liebetrau C Konstantinides S et al . Pulmonary endarterectomy in chronic thromboembolic pulmonary hypertension. J Heart Lung Transplant. (2018) 37:250–8. doi: 10.1016/j.healun.2017.06.011,
37.
Madani MM Auger WR Pretorius V Sakakibara N Kerr KM Kim NH et al . Pulmonary endarterectomy: recent changes in a single institution’s experience of more than 2,700 patients. Ann Thorac Surg. (2012) 94:97–103. doi: 10.1016/j.athoracsur.2012.04.004,
38.
Jamieson SW Kapelanski DP Sakakibara N Manecke GR Thistlethwaite PA Kerr KM et al . Pulmonary endarterectomy: experience and lessons learned in 1,500 cases. Ann Thorac Surg. (2003) 76:1457–64. doi: 10.1016/s0003-4975(03)00828-2
39.
Tromeur C Jaïs X Mercier O Couturaud F Montani D Savale L et al . Factors predicting outcome after pulmonary endarterectomy. PLoS One. (2018) 13:e0198198. doi: 10.1371/journal.pone.0198198,
Summary
Keywords
autoimmunity, chronic thromboembolic pulmonary hypertension, outcomes, persistent pulmonary hypertension, surgery
Citation
Alturaif N, Alduraibi FK, Marquez K, Alahmadi F, Alharbi N, Zaytoun H, Alhamoud H, Alzubi F, Hashim M, Hämmäinen P, De Vol E and Aldalaan AM (2026) Pulmonary endarterectomy in antiphospholipid syndrome: a retrospective analysis from the Saudi pulmonary hypertension registry. Front. Med. 13:1736115. doi: 10.3389/fmed.2026.1736115
Received
03 November 2025
Revised
24 December 2025
Accepted
02 January 2026
Published
14 January 2026
Volume
13 - 2026
Edited by
Roberto Giovanni Carbone, University of Genoa, Italy
Reviewed by
Giuseppe Murdaca, University of Genoa, Italy
Francesco Puppo, University of Genoa, Italy
Katsura Soma, The University of Tokyo, Japan
Updates
Copyright
© 2026 Alturaif, Alduraibi, Marquez, Alahmadi, Alharbi, Zaytoun, Alhamoud, Alzubi, Hashim, Hämmäinen, De Vol and Aldalaan.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Noura Alturaif, naalturaif@hotmail.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.