Abstract
Background:
Glaucoma is a major cause of vision loss. Preventing the development of glaucoma has become a focus of attention. Whether obesity or overweight is related to the glaucoma development still remains a matter of debate.
Objective:
The purpose of this study is to explore the impact of obesity or overweight on the risk of glaucoma.
Materials and methods:
A systematic search was conducted in the PubMed, Embase, and Web of Science databases for relevant studies published up to 24 March, 2025. Original studies reporting the relationship between obesity or overweight and glaucoma risk were selected. Clinical outcomes were evaluated based on odds ratios (OR) or hazard ratios (HR) with corresponding 95% confidence intervals (CI). The study quality was assessed using an eight-component rating scale.
Results:
Thirteen studies were included. Individuals with obesity or overweight had a 60% higher risk of glaucoma compared with the normal-weight population (OR: 1.60 [95% CI: 1.19–2.17], p = 0.002), while the association was not significant for HR values (HR: 1.14 [95% CI: 1.00–1.31], p = 0.058). Subgroup analysis revealed that individuals with obesity or overweight in developed countries had a 91% higher risk of glaucoma (OR: 1.91 [95% CI: 1.44–2.52], p < 0.001). In addition, obesity or overweight in men was associated with a higher risk of glaucoma (OR: 2.14 [95% CI: 1.24–3.69], p = 0.006).
Conclusion:
Obesity or overweight may increase the risk of glaucoma in term of OR values. Obese or overweight individuals in developed countries, especially obese men, appear to be associated with a higher risk of glaucoma. Maintaining weight within the normal range may be an effective measure to prevent glaucoma.
Introduction
Glaucoma is a disease that leads to irreversible vision loss and its main characteristic is the progressive degeneration of retinal ganglion cells, often accompanied by increased intraocular pressure (1–3). Glaucoma is primarily classified into open-angle glaucoma and angle-closure glaucoma, with approximately half of the glaucoma-related blindness attributable to angle-closure glaucoma (4). Other subtypes include congenital glaucoma and secondary glaucoma. Because glaucoma progresses slowly and neural mechanisms compensate for the areas of vision loss, patients often remain unaware of vision impairment until the late stages of the disease (5–7). At present, no effective treatment exists to restore vision loss caused by glaucoma. Therefore, effective case detection and preventive strategies are essential.
The prevalence of obesity has increased significantly over the past 30 years, mainly due to people’s dietary habits (8–10). Obesity or overweight negatively impact health. Obesity is well known to negatively impact both the cardiovascular and metabolic systems (11, 12). Meanwhile, obesity is also one of the main risk factors for diseases such as coronary heart disease, type 2 diabetes, hypertension, stroke, dyslipidemia, osteoarthritis, and sleep apnea (13, 14).
Currently, there are relatively few studies on the impact of obesity or overweight on the development of eye diseases. Whether obesity or overweight substantially increases the risk of glaucoma remains a focus of attention. A clinical study reported a harmful link between obesity and vision, although the specific mechanisms and consequences of this association are still unclear (15). Other studies have shown that obesity may be related to glaucoma development (16, 17). Liu et al. showed in a meta-analysis that obesity increases the risk of elevated intraocular pressure, but does not significantly affect the occurrence of open-angle glaucoma (18). In contrast, Jung et al. showed that obesity and metabolic health status are closely associated with an increased risk of open-angle glaucoma (16). Therefore, whether obesity or overweight is related to glaucoma risk remains debated, and further research is necessary.
This study conducted a meta-analysis on the relationship between obesity or overweight and the risk of glaucoma. The study also performed subgroup analyses for different countries, ages, and sexes to investigate the impact of various factors on the risk of glaucoma.
Materials and methods
Search strategy
This study was conducted in accordance with the preferred reporting items for systematic reviews and meta-analyses (PRISMA) (19). Two authors (PX and DHH) systematically and independently searched for relevant literature using the PubMed, Web of Science, and Embase databases up to 24 March, 2025. The search strategy included the following terms: “obesity” or “nutritional and metabolic diseases” or “nutrition disorders” or “overnutrition” OR “overweight” OR “obesity hypoventilation syndrome” OR “pediatric obesity” OR “pregnancy in obesity” OR “intra-abdominal fat” OR “body mass index” OR “BMI” AND “glaucoma” OR “intraocular pressure” OR “ocular hypertension” OR “open-angle glaucoma” OR “normal tension glaucoma” OR “high tension glaucoma.” In addition, the reference lists of the retrieved meta-analyses may be screened for additional eligible articles. No other restrictions were imposed.
Screening criteria
The inclusion criteria were as follows: (1) literature reported the relationship between obesity or overweight and the risk of glaucoma or elevated IOP; (2) cohort, case–control, or cross-sectional study design was adopted; (3) relevant risk outcomes, such as hazard ratio (HR), odds ratio (OR), or relative risk (RR), were further analyzed in this study; and (4) study was published in English.
The exclusion criteria were as follows: (1) conference abstracts, letters, or editorials; (2) published in a language other than English; (3) study subjects were non-human; and (4) studies involving the effects of relevant drug treatments or special situations (such as ophthalmic surgery).
Data extraction
The two authors (PX and DHH) independently extracted the data, and any discrepancies were resolved by consulting a third researcher. The data extracted from each included study comprised the first author, year, country, number of participants, proportion of women, age, study design, participant status, obesity assessment, and relevant outcomes (HR, OR, or RR, along with 95% confidence intervals (CI)). Obesity, overweight, and glaucoma are defined as shown in Table 1.
Table 1
| Author | Obesity or overweight definition | Glaucoma definition |
|---|---|---|
| Fujita (23) | Overweight or obese (BMI ≥ 25 kg/m2) | ICD-10 codes, H40.1-H40.9, H42.0, H42.8, Q15.0 |
| Ngo (24) | Overweight: BMI (25.0–29.9), Obese: BMI ≥ 30. | NR |
| Chen (25) | Obesity or morbid obesity (ICD-9-CM codes 278.0, 278.00, 278.01) | ICD-9-CM codes 365.1, 365.10, 365.11, 365.12 |
| Rosa (26) | BMI: low (<18.5), moderate (18.5–24.9), high (25.0–29.9), and very high (≥30). | NR |
| Lee (27) | BMI ≥ 25 kg/m2 | NR |
| Lin (28) | Lower BMI (<19 kg/m2) Normal BMI (19–24.9 kg/m2) |
NR |
| Zhao (29) | Obesity was defined as a BMI of 24.0 kg/m2 or higher. | Self-reports |
| Wise (30) | BMI ≥ 35 kg/m2 | Self-reports |
| Pasquale (31) | BMI ≥ 30 kg/m2 | Self-reports |
| Ko (32) | BMI ≥ 30 kg/m2 | Cup-to-disc ratio (CDR) |
| Cohen (33) | BMI ≥ 25 kg/m2 | NR |
| Jang (34) | BMI ≥ 25 kg/m2 | NR |
| Kyari (35) | Overweight or obese (BMI ≥ 25 kg/m2) | International Society for Geographical and Epidemiological Ophthalmology (ISGEO) criteria |
Definitions of obesity, overweight, and glaucoma included in this study.
NR, no report; BMI, body mass index.
Evaluation of study quality
This study used a modified eight-point assessment scale to evaluate the quality of the included studies (20). The scale consists of six parts: selection bias, study design (such as cross-sectional or cohort), confounding factors (such as age or sex control), data collection methods, and data extraction and analysis. Each component was graded as weak, moderate, or strong. The overall study quality was divided into weak quality (≥2 components rated as weak), moderate quality (<3 components rated as strong, and <2 components rated as weak), and strong quality (≥3 components rated as strong and ≤1 components rated as weak).
Statistical analysis
The HR, OR, and their corresponding 95% CI were used to assess the relationship between obesity or overweight and glaucoma. A random-effects model was used, and Stata version 15 (StataCorp LLC, College Station, TX, United States) was employed to conduct the meta-analysis of effect sizes (HR/OR) and their corresponding 95% CI.
Furthermore, the prediction intervals (21) for the relevant ORs was calculated using the following formula:
where SE = {ln(upper) − ln(lower)}/(2 × Z0.975) and Z0.975 ≈ 1.96.
In addition, stratified subgroup analyses were conducted based on sex, country (developed countries or developing countries), and age (≥40 years). The I2 statistic was used to assess the heterogeneity of the results. The Egger’s and Begg’s tests were employed to evaluate publication bias (22). Finally, apart from heterogeneity, a p-value of less than 0.05 was considered statistically significant.
Results
Initially, 7,719 relevant studies were identified, and seven additional studies were supplemented from reference lists. After excluding 3,976 duplicate studies, 3,699 irrelevant studies were excluded through abstract and title screening, leaving 51 studies for full-text assessment. Based on the inclusion and exclusion criteria, 38 studies were excluded, including reviews, meta-analyses, or case reports (n = 21); studies without relevant outcomes (n = 11); and studies without available full text (n = 6). Finally, a total of 13 studies were included in the meta-analysis (23–35) (Figure 1).
Figure 1
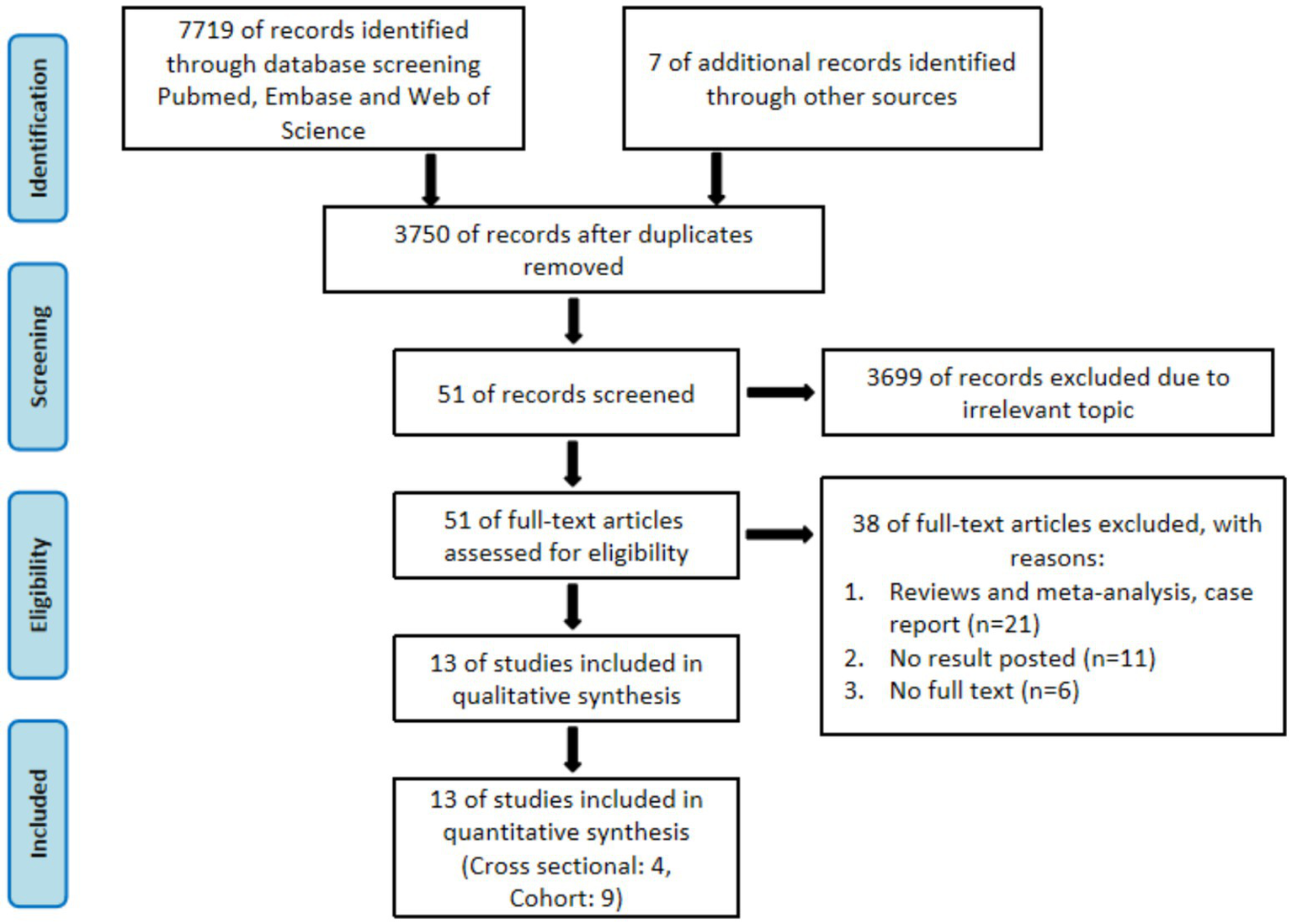
The flow chart of screening studies.
Study characteristics
Among the 13 studies included in this research, 4 were cross-sectional, 4 were prospective cohort, and 5 were retrospective cohort studies. After quality assessment of the literature, 84.6% of the studies were rated as medium quality, 7.7% as high quality, and 7.7% as weak quality. In terms of sample size, 12 studies exceeded 5,000 participants, while only one study had less than 5,000 participants (Table 2).
Table 2
| Author | Year | Country | Number of patients | Percentage of women (%) | Age | Study design | Patient’s condition | Outcomes | Quality assessment |
|---|---|---|---|---|---|---|---|---|---|
| Fujita (23) | 2023 | Japan | 3,110,743 | 38.3 | 44.4 | Retrospective | Excluding individuals aged <20 years, those with missing data and those with pre-existing glaucoma, defined as those who had diagnostic records of glaucoma (ICD-10 codes, H40.1–H40.9, H42.0, H42.8, and Q15.0) within a 1-year look-back period. | HR: 1.04 (1.02–1.07) | Moderate |
| Ngo (24) | 2013 | India | 115 | 60.86 | 65 | Prospective | Age of 30 years or older, OAG in the study eye as determined by a glaucoma specialist, best corrected by early treatment Diabetic Retinopathy Study visual acuity of 20/60 or better in the study eye, and acceptable reliability indexes in previous visual fields (VF) performed. | IOP decreased: Normal weight (−1.5, 95%CI -2.7–(−0.4)); Overweight (−1.9, 95%CI -3.4–(−0.4)); Obese (−2.5, 95%CI -3.9–(−1.2)) | Moderate |
| Chen (25) | 2021 | China | 11,939 | 66.7 | ≥18 | Retrospective | Individuals aged ≥18 years. | HR(95% CI): 1.54 (1.23–1.94) | Moderate |
| Rosa (26) | 2024 | African | 6,634 | NA | NA | Retrospective | The POAAGG study population consists of 10,255 subjects of African ancestry (Black, Afro-Caribbean, or African American) who were over the age of 35 and were recruited from greater Philadelphia. Each enrolled subject was classified by a glaucoma specialist or ophthalmologist as a POAG case, POAG suspect, or control based on previously determined criteria. | OR(95%CI) 1.02 (1.007–1.023), p = 0.0003 | Moderate |
| Lee (27) | 2019 | Korea | 287,553 | NA | >40 | Prospective | From the KNHIS-NSC 2002 to 2013 project, we included subjects who had undergone a general health examination at least once between 2002 and 2008 (n = 424,712). Subjects were identified as having POAG if they had at least two visits for POAG (International Classification of Diseases [ICD]-10 code H40.1) and received antiglaucoma medications during the study period. | HR: 1.35 (1.16–1.56) | Moderate |
| Lin (28) | 2018 | Korea | 10,978 | NA | >40 | Cross-sectional | All participants had measured intraocular pressure of <22 mmHg and open anterior chamber angles. OAG was defined using disc and visual field criteria established by the International Society for Geographical and Epidemiological Ophthalmology. | Lower vs. normal BMI OR: 2.28 (1.22–4.26) | Moderate |
| Zhao (29) | 2023 | Korea | 13,357 | NA | >45 | Retrospective | This study analyzed data from CHARLS, a nationally representative longitudinal survey of people in China aged 45 years or older and their spouses. In total, 150 county-level units from 28 provinces were randomly selected from a sampling framework that included all county-level units except Tibet. | HR: 0.90, 95% CI: 0.83–0.97 | Moderate |
| Wise (30) | 2011 | USA | 59,000 | 100 | 21–69 | Prospective | The BWHS is an ongoing U. S. prospective cohort study, established in 1995 when 59,000 African-American women aged 21–69 years were enrolled through mailed questionnaires. | Age: <50 HR: 3.96 (0.94–16.7); ≥ 50 1.38 (0.83–2.30) |
Moderate |
| Pasquale (31) | 2010 | USA | 120,129 | 65.6 | NA | Prospective | 78,777 women in the Nurses’ Health Study and 41,352 men in the Health Professionals Follow-up Study. | HR: 0.98 (0.76–1.26) | High |
| Ko (32) | 2016 | USA | 5,746 | NA | ≥ 40 | Cross-sectional | Data from the NHANES from 2005 to 2008, are presentative sample of the population in the United States. | OR: 1.63 (1.10–2.41) | Moderate |
| Cohen (33) | 2016 | USA | 18,575 | 32 | 46 ± 10 | Retrospective | The subjects attending the center include men and nonpregnant women within an age range of 20 to 80 years. | Men OR: 2.86 (2.09–3.91); Women OR: 2.73 (1.62–4.60) |
Moderate |
| Jang (34) | 2014 | Korea | 15,271 | 56.8 | >19 | Cross-sectional | A total of 15,271 subjects (6,600 men and 8,671 women) participated from 2008–2010 in the Korea National Health and Nutrition Examination Survey. | Men OR: 1.64 (1.31–2.05); Women OR: 1.40 (1.09–1.79) |
Moderate |
| Kyari (35) | 2016 | Nigeria | 13,200 | 54.3 | ≥ 40 | Cross-sectional | The Nigeria Blindness Survey gave a national representative sample of 15,375 persons aged 40 years and above in 310 clusters across the country. | Overweight OR: 0.82 (0.58–1.17); Obese OR: 1.18 (0.71–1.96) |
Weak |
Characteristics of the included studies.
BMI, body mass index; OR, odds ratio; HR, hazard ratio; CI, confidence intervals.
Obesity and risk of glaucoma
Pooling the existing evidence, we found that compared with individuals of normal weight, those with obesity or overweight had a 60% higher risk of glaucoma (OR: 1.60 [95% CI: 1.19–2.17], p = 0.002; prediction interval: 1.05–2.46), although significant heterogeneity was observed (I2 = 82.2%, p < 0.001) (Figure 2). In terms of the HR values, the risk of glaucoma in individuals with obesity or overweight was not significantly higher than in those of normal weight (HR: 1.14 [95% CI: 1.00–1.31], p = 0.058) (Figure 3). In addition, one study reported that in individuals with open-angle glaucoma of normal weight, changes in systolic blood pressure were positively correlated with changes in intraocular pressure (IOP), a relationship not observed overweight or obese individuals (Table 2).
Figure 2
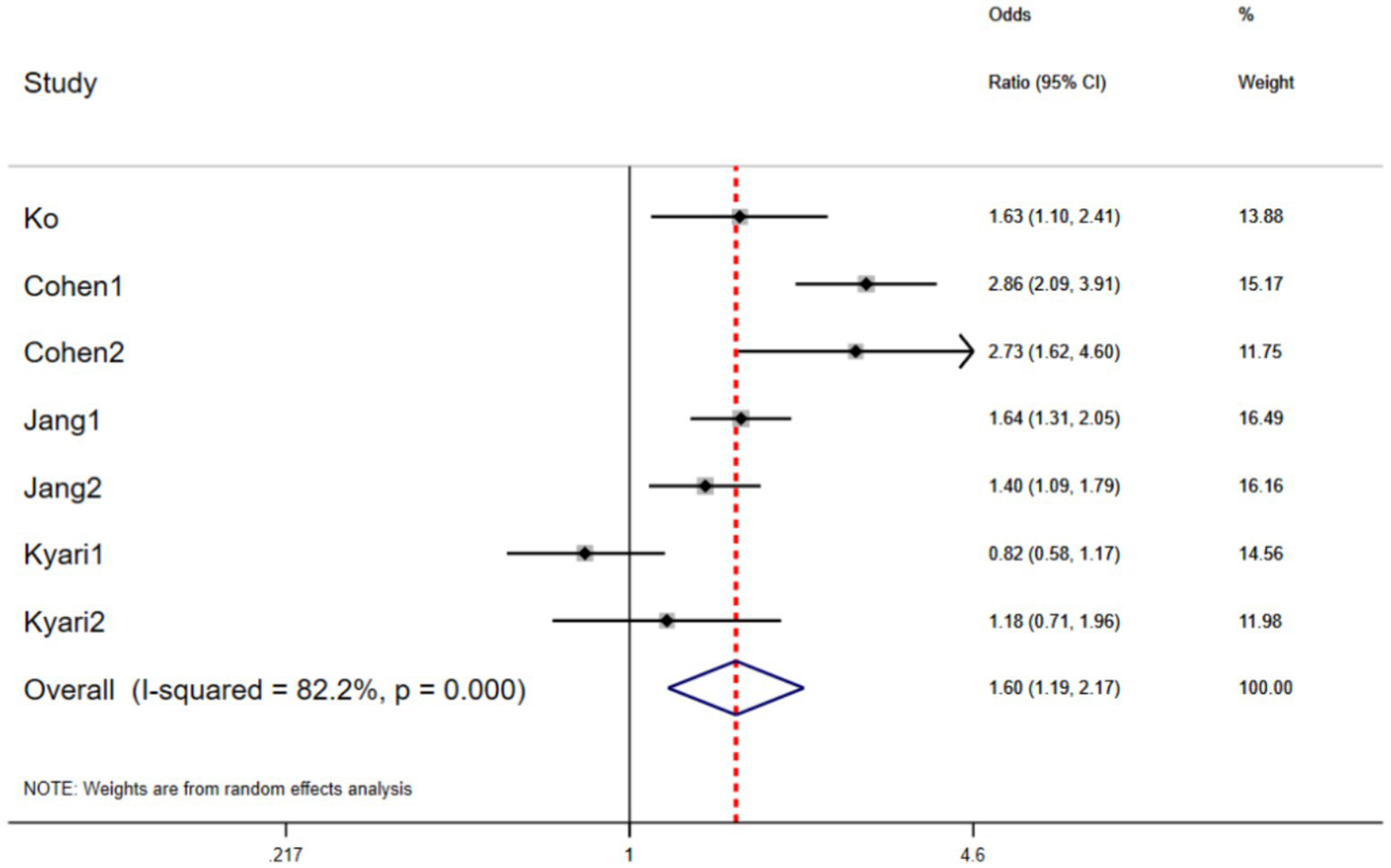
The forest plots of the odds ratio (OR) and 95% CIs for the relationship between obesity and glaucoma (p = 0.002).
Figure 3
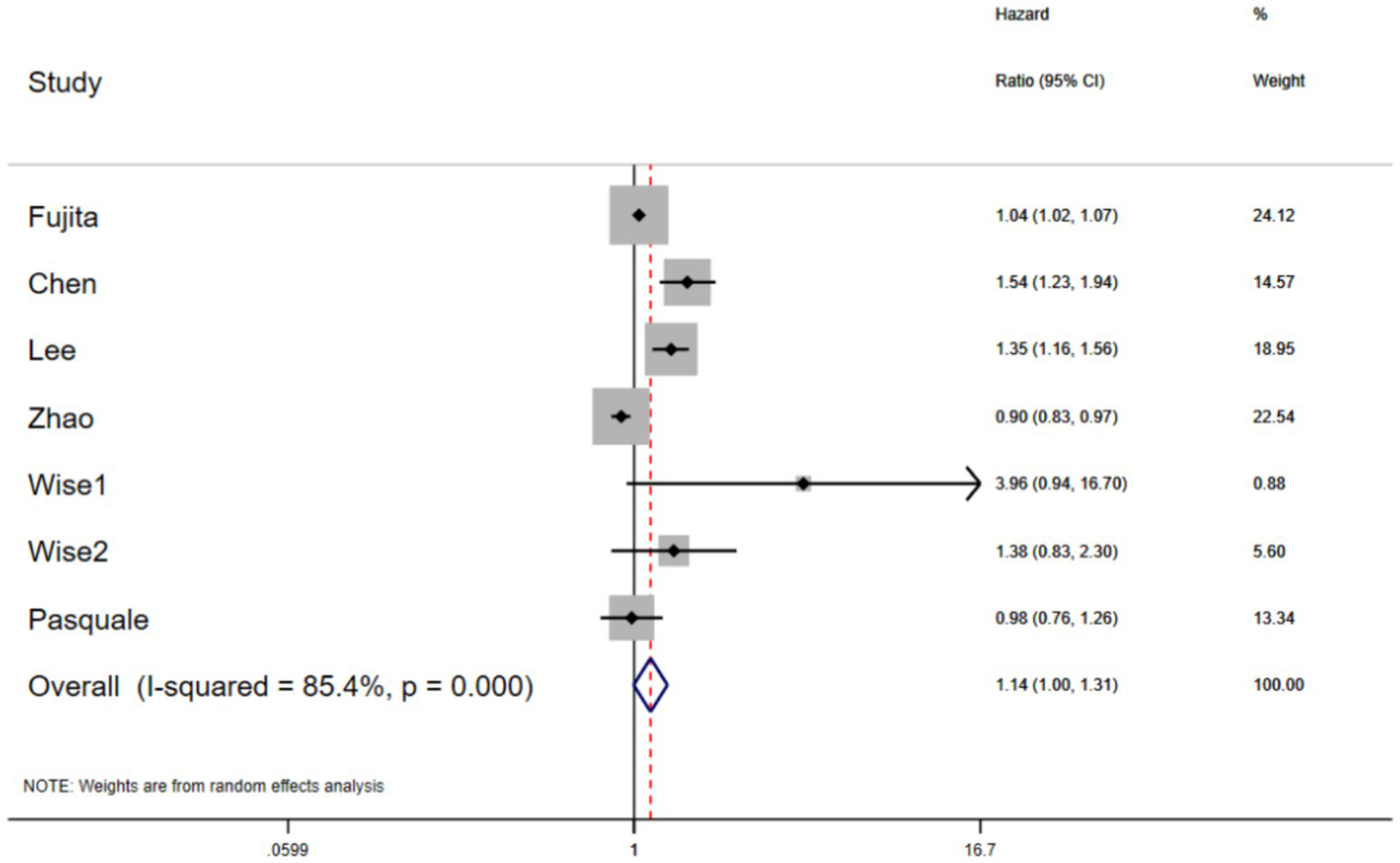
The forest plots of the hazard ratio (HR) and 95% CIs for the relationship between obesity and glaucoma (p = 0.05).
Subgroup analysis
To further explore sources of heterogeneity, subgroup analyses were conducted based on country, sex, and age. Compared with individuals of normal weight, those with obesity or overweight in developed countries had a 91% higher risk of glaucoma (OR: 1.91 [95% CI: 1.44–2.52], p < 0.001; prediction interval: 1.28–2.83), whereas in the developing countries the association was not significant (OR: 0.72 [95% CI: 0.40–1.30], p = 0.27) (Table 3). Individuals with obesity or overweight who are aged ≥ 40 did not show a higher risk of glaucoma than those of normal weight (OR: 1.65 [95% CI: 0.99–2.75], p = 0.06) (Table 3). In addition, compared with individuals of normal weight, obese or overweight men had a 114% higher risk of glaucoma (OR: 2.14 [95% CI: 1.24–3.69], p = 0.006; prediction interval: 0.99–4.63), while the association was not significant in women (OR: 1.88 [95% CI: 0.98–3.59], p = 0.06) (Table 3).
Table 3
| Subgroup | No. of studies | OR (95% CI) | P-value | Heterogeneity | Prediction interval | |
|---|---|---|---|---|---|---|
| I2 (%) | P-value | |||||
| Country | ||||||
| Developed | 5 | 1.91 (1.44–2.52) | <0.001 | 74.5 | 0.003 | 1.28–2.83 |
| Developing | 2 | 0.72 (0.40–1.30) | 0.27 | 81.0 | 0.005 | 0.31–1.66 |
| Age | ||||||
| ≥40 | 5 | 1.65 (0.99–2.75) | 0.06 | 87.6 | <0.001 | 0.80–3.40 |
| Sex | ||||||
| Men | 2 | 2.14 (1.24–3.69) | 0.006 | 87.5 | 0.005 | 0.99–4.63 |
| Women | 2 | 1.88 (0.98–3.59) | 0.06 | 80.5 | 0.02 | 0.75–4.70 |
The subgroup analysis of odds ratio for the relationship between obesity and glaucoma.
OR, odds ratio.
Furthermore, we also examined HR values for relationship between obesity and glaucoma. In both developed and developing countries, the HR values of glaucoma in individuals with obesity or overweight was not significantly higher than those of normal weight (developed HR: 1.07 [95% CI: 0.91–1.26], p = 0.43; developing HR: 1.22 [95% CI: 0.86–1.73], p = 0.27) (Table 4). In addition, individuals aged ≥ 40 or women with obesity or overweight did not exhibit significantly higher HR values (age ≥ 40 HR: 1.07 [95% CI: 0.94–1.21], p = 0.34; women HR: 1.87 [95% CI: 0.73–4.77], p = 0.19).
Table 4
| Subgroup | No. of studies | HR (95% CI) | P value | Heterogeneity | Prediction interval | |
|---|---|---|---|---|---|---|
| I2 (%) | P-value | |||||
| Country | ||||||
| Developed | 4 | 1.07 (0.91–1.26) | 0.43 | 36.3 | 0.19 | 0.85–1.35 |
| Developing | 3 | 1.22 (0.86–1.73) | 0.27 | 94.5 | <0.001 | 0.74–2.00 |
| Age | ||||||
| ≥ 40 | 5 | 1.07 (0.94–1.21) | 0.34 | 84.8 | <0.001 | 0.89–1.27 |
| Sex | ||||||
| Women | 2 | 1.87 (0.73–4.77) | 0.19 | 45.4 | 0.18 | 0.49–7.04 |
The subgroup analysis of the hazard ratio for the relationship between obesity and glaucoma.
HR, hazard ratio.
Publication bias
Egger’s and Begg’s tests were used to assess publication bias. The results showed no obvious publication bias (Egger: OR p = 0.94, HR p = 0.33; Begg: OR p = 0.88, HR p = 0.65) (Supplementary Figures 1–4).
Sensitivity analysis
Sensitivity analysis of the relationship between obesity and glaucoma showed that no study significantly affected the final pooled OR HR values (Supplementary Figures 5, 6).
Discussion
The most important contribution of this study is the finding that obesity or overweight substantially increases glaucoma risk. Subgroup analysis further suggest that the risk of glaucoma is higher among individuals with obesity or overweight in developed countries and among obese men.
Although the pathogenesis of glaucoma remains unclear, some studies have suggested that the mechanisms by which obesity increases the risk of glaucoma may include: (1) certain connection between glaucoma and high IOP, which may be related to the hypertension caused by high BMI (36, 37). Moreover, the increased red blood cell aggregation, hematocrit, and hemoglobin levels in obese individuals make their blood more viscous, thereby increases IOP by resistance to the outflow of aqueous humor from the eye (38, 39). (2) Vascular dysregulation and vasospasm can lead to reduced blood flow to the optic nerve and also cause increased IOP (40, 41). (3) The gut microbiome is considered a potential environmental factor, and obesity is often accompanied by gut microbiota dysbiosis (10). By pooling the existing evidence, this study demonstrates that obesity or overweight significantly increases glaucoma risk. Therefore, effective measures to prevent glaucoma include reasonably adjusting the diet and maintaining BMI within the normal level.
Compared with the study by Liu et al. (18), this study explores the relationship between obesity or overweight and glaucoma risk from two perspectives: OR values and prediction interval. The results indicate that obesity or overweight significantly increases glaucoma risk, consistent with some previous epidemiological findings (16, 25, 36). In addition, compared with the study by Khan et al. (42), this study provides detailed subgroup analyses based on country, age, and sex. The findings suggest that glaucoma risk is elevated among individuals with obesity or overweight in developed countries and among obese men. Furthermore, a study has shown that low BMI is also associated with increased glaucoma risk, potentially due to nutritional deficiencies and imbalances in fat-related factors (26, 28, 43).
Subgroup analysis further revealed that the risk of glaucoma in individuals with obesity or overweight in developed countries is higher than that in developing countries. This may be due to the combined effect of various interrelated pathophysiological mechanisms, such as gut microbiota dysbiosis and adipokine imbalance (10, 44). Gut microbiota dysbiosis increases intestinal permeability, leading to the accumulation of microbes and metabolites in the central nervous system, which promotes neurodegeneration and accelerates glaucoma progression (45, 46). Dysbiosis also disrupts the secondary bile acid pool, contributing to immune dysregulation, increased oxidative stress, and optic nerve damage. These mechanisms are closely related to lifestyle and dietary habits. In addition, the risk of glaucoma increased in men with obesity or overweight may be related to the differences in body composition between men and women. Estrogen in women may play an important neuroprotective role by regulating smooth muscle tone and vascular resistance to affect aqueous humor production and outflow (47). Moreover, relevant studies show that adipose tissue, as an endocrine organ, may affect retinal ganglion cell health by secreting other paracrine factors (44). Finally, the specific mechanisms by which obesity affects glaucoma require further investigation.
In addition to CI, this study also applied the prediction interval to evaluate the reliability of the results, thereby providing a more comprehensive and practical prediction outcome for related studies (21). Moreover, the heterogeneity in this study is more evident in the subgroup analysis. In the population stratified by age and sex, the I2 statistic fluctuates significantly. However, the sensitivity analysis did not show that any single study significantly affected the final pooled OR value. This may be related to the significant heterogeneity among populations in different regions.
Additionally, the pooled OR analysis in this study exhibited high heterogeneity. This study employed meta-regression analysis to investigate the heterogeneity. The results suggest that region (p = 0.015) and sex (p = 0.027) may be contributing factors to the high heterogeneity in the outcomes, associated with potential differences in genetic backgrounds and environmental exposures.
This study incorporated OR and HR values to evaluate the relationship between obesity or overweight and glaucoma risk. The OR value indicates that obesity or overweight is associated with a higher risk of glaucoma, while the HR value showed no significant correlation. The reasons for this discrepancy may be as follows: (1) glaucoma is a low-incidence event. Although many cohort studies included large sample sizes, the actual number of glaucoma cases was relatively small, which may have led to insufficient statistical power. This does not necessarily imply that obesity is unrelated to glaucoma risk. (2) Obesity influences glaucoma development through mechanisms such as IOP, vascular blood flow, and oxidative stress, which typically require a longer period to manifest. This may affect the outcomes of longitudinal studies, whereas cross-sectional studies might be less impacted.
This study has certain limitations. First, only cross-sectional, prospective and retrospective studies were included; well-designed and large-scale prospective cohort studies are necessary. Second, uncontrollable factors may influence the results. For example, differences in the obesity criteria or glaucoma diagnostic criteria across studies may have a certain impact on the final results. Third, high heterogeneity observed among studies, with varying definitions for obesity and glaucoma. Finally, despite assessment, the presence of publication bias remains incomplete.
Conclusion
We found that obesity or overweight increases glaucoma risk in term of OR values. Individuals with obesity or overweight in developed countries, as well as obese men, appear to be associated with higher risk. Therefore, maintaining weight within the normal range may be an effective measure to prevent glaucoma.
Statements
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
PX: Data curation, Methodology, Software, Writing – original draft. HQ: Data curation, Formal analysis, Writing – original draft. LZ: Data curation, Writing – review & editing. DH: Formal analysis, Methodology, Software, Writing – original draft. HT: Supervision, Writing – review & editing. RL: Validation, Writing – review & editing. HP: Writing – review & editing.
Funding
The author(s) declared that financial support was not received for this work and/or its publication.
Conflict of interest
The author(s) declared that this work was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declared that Generative AI was not used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2026.1756819/full#supplementary-material
Abbreviations
PRISMA, Preferred reporting items for systematic reviews and meta-analyses; HR, Hazard ratio; OR, Odds ratio; CI, Confidence interval; IOP, Intraocular pressure; BMI, Body mass index.
References
1.
Jayaram H Kolko M Friedman DS Gazzard G . Glaucoma: now and beyond. Lancet. (2023) 402:1788–801. doi: 10.1016/S0140-6736(23)01289-8,
2.
Quigley HA Broman AT . The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. (2006) 90:262–7. doi: 10.1136/bjo.2005.081224
3.
Quigley HA . Neuronal death in glaucoma. Prog Retin Eye Res. (1999) 18:39–57. doi: 10.1016/s1350-9462(98)00014-7,
4.
Weinreb RN Aung T Medeiros FA . The pathophysiology and treatment of glaucoma: a review. JAMA. (2014) 311:1901–11. doi: 10.1001/jama.2014.3192
5.
Ramulu PY Hochberg C Maul EA Chan ES Ferrucci L Friedman DS . Glaucomatous visual field loss associated with less travel from home. Optom Vis Sci. (2014) 91:187–93. doi: 10.1097/opx.0000000000000139,
6.
Ramulu PY Swenor BK Jefferys JL Friedman DS Rubin GS . Difficulty with out-loud and silent reading in glaucoma. Invest Ophthalmol Vis Sci. (2013) 54:666–72. doi: 10.1167/iovs.12-10618,
7.
Ramulu PY West SK Munoz B Jampel HD Friedman DS . Driving cessation and driving limitation in glaucoma: the Salisbury eye evaluation project. Ophthalmology. (2009) 116:1846–53. doi: 10.1016/j.ophtha.2009.03.033,
8.
Boutari C Mantzoros CS . A 2022 update on the epidemiology of obesity and a call to action: as its twin COVID-19 pandemic appears to be receding, the obesity and dysmetabolism pandemic continues to rage on. Metabolism. (2022) 133:155217. doi: 10.1016/j.metabol.2022.155217,
9.
Dinsa GD Goryakin Y Fumagalli E Suhrcke M . Obesity and socioeconomic status in developing countries: a systematic review. Obes Rev. (2012) 13:1067–79. doi: 10.1111/j.1467-789X.2012.01017.x,
10.
Pezzino S Sofia M Greco LP Litrico G Filippello G Sarvà I et al . Microbiome dysbiosis: a pathological mechanism at the intersection of obesity and glaucoma. Int J Mol Sci. (2023) 24:1166. doi: 10.3390/ijms24021166
11.
Head GA . Cardiovascular and metabolic consequences of obesity. Front Physiol. (2015) 6:32. doi: 10.3389/fphys.2015.00032,
12.
Fava MC Agius R Fava S . Obesity and cardio-metabolic health. Br J Hosp Med (Lond). (2019) 80:466–71. doi: 10.12968/hmed.2019.80.8.466
13.
Fruh SM . Obesity: risk factors, complications, and strategies for sustainable long-term weight management. J Am Assoc Nurse Pract. (2017) 29:S3–s14. doi: 10.1002/2327-6924.12510,
14.
Bray GA Kim KK Wilding JPH . Obesity: a chronic relapsing progressive disease process. A position statement of the world obesity federation. Obes Rev. (2017) 18:715–23. doi: 10.1111/obr.12551,
15.
Yang F Yang C Liu Y Peng S Liu B Gao X et al . Associations between body mass index and visual impairment of school students in Central China. Int J Environ Res Public Health. (2016) 13:1024. doi: 10.3390/ijerph13101024,
16.
Jung Y Han K Park HYL Lee SH Park CK . Metabolic health, obesity, and the risk of developing open-angle Glaucoma: metabolically healthy obese patients versus metabolically unhealthy but Normal weight patients. Diabetes Metab J. (2020) 44:414–25. doi: 10.4093/dmj.2019.0048,
17.
Marshall H Berry EC Torres SD Mullany S Schmidt J Thomson D et al . Association between body mass index and primary open angle Glaucoma in three cohorts. Am J Ophthalmol. (2023) 245:126–33. doi: 10.1016/j.ajo.2022.08.006,
18.
Liu W Ling J Chen Y Wu Y Lu P . The association between adiposity and the risk of glaucoma: a meta-analysis. J Ophthalmol. (2017) 2017:9787450. doi: 10.1155/2017/9787450
19.
Page MJ McKenzie JE Bossuyt PM Boutron I Hoffmann TC Mulrow CD et al . The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
20.
Armijo-Olivo S Stiles CR Hagen NA Biondo PD Cummings GG . Assessment of study quality for systematic reviews: a comparison of the Cochrane collaboration risk of Bias tool and the effective public health practice project quality assessment tool: methodological research. J Eval Clin Pract. (2012) 18:12–8. doi: 10.1111/j.1365-2753.2010.01516.x,
21.
IntHout J Ioannidis JP Rovers MM Goeman JJ . Plea for routinely presenting prediction intervals in meta-analysis. BMJ Open. (2016) 6:e010247. doi: 10.1136/bmjopen-2015-010247
22.
Egger M Davey Smith G Schneider M Minder C . Bias in meta-analysis detected by a simple, graphical test. BMJ. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629,
23.
Fujita A Hashimoto Y Matsui H Yasunaga H Aihara M . Association between lifestyle habits and glaucoma incidence: a retrospective cohort study. Eye Lond. (2023) 37:3470–6. doi: 10.1038/s41433-023-02535-7,
24.
Ngo S Harris A Siesky BA Schroeder A Eckert G Holland S . Blood pressure, ocular perfusion pressure, and body mass index in glaucoma patients. Eur J Ophthalmol. (2013) 23:664–9. doi: 10.5301/ejo.5000257,
25.
Chen WD Lai LJ Lee KL Chen TJ Liu CY Yang YH . Is obesity a risk or protective factor for open-angle glaucoma in adults? A two-database, Asian, matched-cohort study. J Clin Med. (2021) 10:4021. doi: 10.3390/jcm10174021
26.
Di Rosa I Halimitabrizi M Salowe R Augello P Zhu D Chen Y et al . Low body mass index poses greater risk of primary open-angle Glaucoma in African ancestry individuals. Am J Ophthalmol. (2025) 271:119–26. doi: 10.1016/j.ajo.2024.10.023,
27.
Lee JS Lee SH Oum BS Chung JS Cho BM Hong JW . Relationship between intraocular pressure and systemic health parameters in a Korean population. Clin Experiment Ophthalmol. (2002) 30:237–41. doi: 10.1046/j.1442-9071.2002.00527.x
28.
Lin SC Pasquale LR Singh K Lin SC . The association between body mass index and open-angle Glaucoma in a south Korean population-based sample. J Glaucoma. (2018) 27:239–45. doi: 10.1097/IJG.0000000000000867,
29.
Zhao X Bo Q Sun J Chen J Li T Huang X et al . The association between obesity and glaucoma in older adults: evidence from the China health and retirement longitudinal study. Epidemiol Health. (2023) 45:e2023034. doi: 10.4178/epih.e2023034,
30.
Wise LA Rosenberg L Radin RG Mattox C Yang EB Palmer JR et al . A prospective study of diabetes, lifestyle factors, and glaucoma among African-American women. Ann Epidemiol. (2011) 21:430–9. doi: 10.1016/j.annepidem.2011.03.006,
31.
Pasquale LR Willett WC Rosner BA Kang JH . Anthropometric measures and their relation to incident primary open-angle glaucoma. Ophthalmology. (2010) 117:1521–9. doi: 10.1016/j.ophtha.2009.12.017
32.
Ko F Boland MV Gupta P Gadkaree SK Vitale S Guallar E et al . Diabetes, triglyceride levels, and other risk factors for Glaucoma in the National Health and nutrition examination survey 2005-2008. Invest Ophthalmol Vis Sci. (2016) 57:2152–7. doi: 10.1167/iovs.15-18373,
33.
Cohen E Kramer M Shochat T Goldberg E Garty M Krause I . Relationship between body mass index and intraocular pressure in men and women: a population-based study. J Glaucoma. (2016) 25:e509–13. doi: 10.1097/IJG.0000000000000374,
34.
Jang HD Kim DH Han K Ha SG Kim YH Kim JW et al . Relationship between intraocular pressure and parameters of obesity in Korean adults: the 2008-2010 Korea National Health and nutrition examination survey. Curr Eye Res. (2015) 40:1008–17. doi: 10.3109/02713683.2014.975367,
35.
Kyari F Abdull MM Wormald R Evans JR Nolan W Murthy GV et al . Risk factors for open-angle glaucoma in Nigeria: results from the Nigeria National Blindness and visual impairment survey. BMC Ophthalmol. (2016) 16:78. doi: 10.1186/s12886-016-0264-7
36.
Garcia-Villanueva C Milla E Bolarin JM García-Medina JJ Cruz-Espinosa J Benítez-Del-Castillo J et al . Impact of systemic comorbidities on ocular hypertension and open-angle glaucoma, in a population from Spain and Portugal. J Clin Med. (2022) 11:5649. doi: 10.3390/jcm11195649
37.
Pileggi C Papadopoli R De Sarro C Nobile CGA Pavia M . Obesity, blood pressure, and intraocular pressure: a cross-sectional study in Italian children. Obes Facts. (2021) 14:169–77. doi: 10.1159/000514096,
38.
Guiraudou M Varlet-Marie E Raynaud de Mauverger E Brun JF . Obesity-related increase in whole blood viscosity includes different profiles according to fat localization. Clin Hemorheol Microcirc. (2013) 55:63–73. doi: 10.3233/CH-131690,
39.
Johnson M . What controls aqueous humour outflow resistance?Exp Eye Res. (2006) 82:545–57. doi: 10.1016/j.exer.2005.10.011,
40.
Orgül S . Blood flow in glaucoma. Br J Ophthalmol. (2007) 91:3–5. doi: 10.1136/bjo.2006.103010
41.
Moore D Harris A Wudunn D Kheradiya N Siesky B . Dysfunctional regulation of ocular blood flow: a risk factor for glaucoma?Clin Ophthalmol. (2008) 2:849–61. doi: 10.2147/opth.s2774,
42.
Khan S Kirubarajan A Lee M Pitha I Buckey JC Jr . The correlation between body weight and intraocular pressure. Aerosp Med Hum Perform. (2021) 92:886–97. doi: 10.3357/AMHP.5769.2021,
43.
Palanisamy K Raman R Sulochana KN Chidambaram S . Adiponectin: a potential candidate for treating fibrosis in posterior segment of the eye. Med Hypotheses. (2019) 123:9–12. doi: 10.1016/j.mehy.2018.12.005,
44.
Gimeno RE Klaman LD . Adipose tissue as an active endocrine organ: recent advances. Curr Opin Pharmacol. (2005) 5:122–8. doi: 10.1016/j.coph.2005.01.006,
45.
Di Benedetto G Burgaletto C Serapide MF Caltabiano R Munafò A Bellanca CM et al . TRAIL-R deficient mice are protected from neurotoxic effects of amyloid-β. Int J Mol Sci. (2022) 23:11625. doi: 10.3390/ijms231911625
46.
Di Benedetto G Burgaletto C Bellanca CM Munafò A Bernardini R Cantarella G . Role of microglia and astrocytes in Alzheimer's disease: from neuroinflammation to ca(2+) homeostasis dysregulation. Cells. (2022) 11:2728. doi: 10.3390/cells11172728,
47.
Vajaranant TS Pasquale LR . Estrogen deficiency accelerates aging of the optic nerve. Menopause. (2012) 19:942–7. doi: 10.1097/gme.0b013e3182443137,
Summary
Keywords
glaucoma, intraocular pressure, meta-analysis, obesity, overweight
Citation
Xie P, Qiu H, Zhao L, Hu D, Tang H, Lu R and Pan H (2026) The impact of obesity or overweight on the risk of glaucoma: a meta-analysis. Front. Med. 13:1756819. doi: 10.3389/fmed.2026.1756819
Received
29 November 2025
Revised
07 January 2026
Accepted
12 January 2026
Published
30 January 2026
Volume
13 - 2026
Edited by
Francesco Buonfiglio, Johannes Gutenberg University Mainz, Germany
Reviewed by
İrfan Uzun, Harran University, Türkiye
Parsa Panahi, Kepler Universitatsklinikum GmbH Universitatsklinik fur Augenheilkunde und Optometrie, Austria
Updates
Copyright
© 2026 Xie, Qiu, Zhao, Hu, Tang, Lu and Pan.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hui Tang, feifei_085@126.com; Rongzhao Lu, 190756225@qq.com; Hongwei Pan, pan_hongwei@163.com
†These authors have contributed equally to this work
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.