Abstract
Introduction:
Vulvar abscess as the primary and sole manifestation of Crohn’s disease (CD) is extremely rare, particularly in adolescents lacking typical gastrointestinal symptoms. This atypical presentation frequently leads to misdiagnosis and delayed treatment.
Case description:
We report the case of a 16-year-old female admitted for recurrent vulvar abscesses accompanied by high fever. Initial management involved local drainage and antibiotics, but efficacy was limited. Upon admission, targeted history taking revealed a change in bowel habits. Laboratory results indicated a significant inflammatory response and positive fecal calprotectin. Combined with imaging, endoscopy, and pathology, the patient was diagnosed with ileal CD. A multidisciplinary treatment strategy was adopted. This included standardized drainage, necessary antibiotic coverage, and exclusive enteral nutrition (EEN) combined with ustekinumab to achieve steroid-free induction. The patient achieved both clinical and mucosal remission.
Conclusion:
This case highlights that recurrent vulvar abscesses in adolescents warrant a high index of suspicion for CD. Clinicians must prioritize targeted history taking. Furthermore, fecal calprotectin testing and imaging should be combined to identify potential inflammatory bowel disease (IBD) early, thereby avoiding missed diagnoses and treatment delays.
1 Introduction
Crohn’s disease (CD) is a chronic inflammatory bowel disease (IBD) in which vulvar involvement represents a rare and clinically challenging extraintestinal manifestation. These lesions are generally classified into two categories: contiguous lesions extending directly from anorectal disease, and non-contiguous “metastatic” granulomatous lesions separated from the gastrointestinal tract (1). Because vulvar signs may precede gastrointestinal symptoms or overshadow mild intestinal manifestations, misdiagnosis is frequent. We report a case of adolescent CD initially presenting as recurrent vulvar abscesses accompanied by persistent high fever. Physical examination revealed local tenderness, a residual drainage opening, and purulent discharge. Laboratory investigations indicated a severe systemic inflammatory response, notably a white blood cell count of 21.3 × 109/L, C-reactive protein of 71.4 mg/L, and an erythrocyte sedimentation rate of 92 mm/h. This article highlights the importance of in-depth history taking, non-invasive screening, and clinical reasoning to achieve early diagnosis in the absence of typical digestive symptoms. Furthermore, it discusses the selection of appropriate biologic therapies for moderate-to-severe CD complicated by secondary infection.
2 Case presentation
2.1 General information and history
A 16-year-old female was admitted due to “intermittent high fever (maximum T 39.7 °C) accompanied by painful swelling of the left vulva for 28 days.” She was previously healthy. Prior to admission, she was diagnosed with a “vulvar abscess” at another hospital. Despite incision, drainage, and multiple courses of broad-spectrum antibiotics, symptoms recurred and progressively worsened. Initially, the patient did not volunteer any gastrointestinal complaints. However, during targeted history taking after admission, she reported a change in bowel habits over the past 6 months. This manifested as soft, unformed stools 1–2 times daily, with occasional watery stools. Although there was no obvious abdominal pain, hematochezia, or weight loss, this “occult symptom” became the diagnostic breakthrough.
2.2 Physical and auxiliary examinations
Physical examination revealed tenderness in the left vulva, with a residual drainage opening and a small amount of purulent discharge. Laboratory tests indicated a severe systemic inflammatory response: white blood cell count 21.3 × 109/L, C-reactive protein (CRP) 71.4 mg/L, and erythrocyte sedimentation rate (ESR) 92 mm/h. Despite prior broad-spectrum antibiotic treatment, inflammatory markers remained elevated (Figure 1).
Figure 1

Timeline of the case. GI, Gastrointestinal.
2.3 Diagnostic clues and confirmation process
Pathogen Detection and Analysis: Bacterial culture and tNGS (targeted next-generation sequencing) of the pus identified Klebsiella variicola and Veillonella parvula. However, even after escalating treatment to potent antibiotics like meropenem, the high fever and abscess remained uncontrolled. Given the poor response to conventional therapy, further screening for systemic inflammation was initiated.
Specific markers: The fecal calprotectin (FC) qualitative test was positive, suggesting active intestinal inflammation.
Imaging: Contrast-enhanced abdominal CT showed segmental thickening of the terminal ileum and adjacent bowel segments, accompanied by mesenteric lymphadenopathy (Figures 2A,B). Perineal ultrasound and pelvic MRI indicated a subcutaneous abscess cavity in the left vulva extending toward the anal canal and rectovaginal septum (Figures 2C,D). While the full fistula track was not clearly delineated, a potential fistula was suspected.
Figure 2
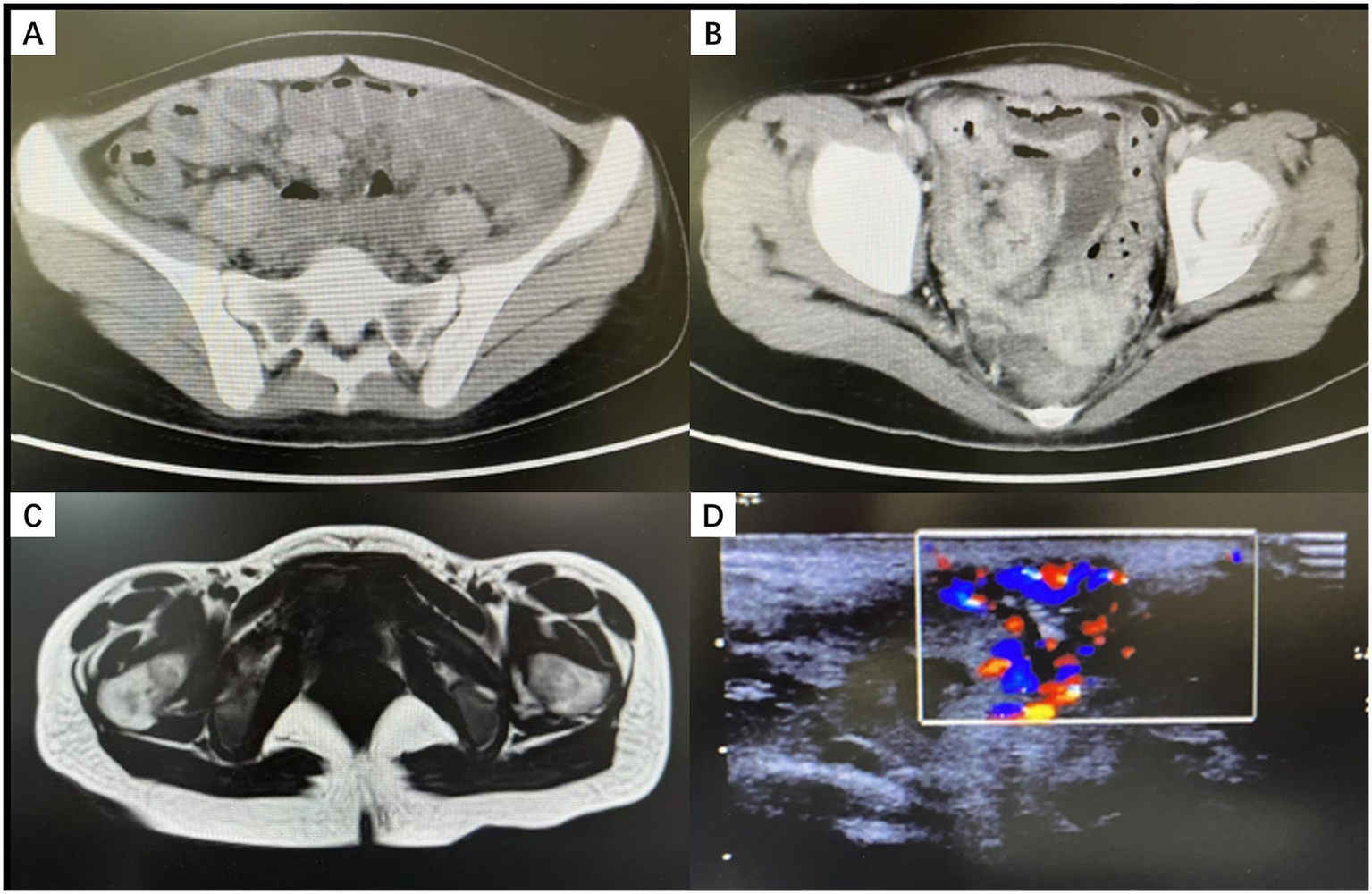
Imaging findings (A,B) Contrast-enhanced abdominal CT showing marked thickening and enhancement of the terminal ileum. (C) Contrast-enhanced pelvic MRI showing post–incision and drainage changes of a left vulvar abscess, with an abnormal signal posterior to the left vaginal introitus, suggesting a residual abscess. (D) Perineal ultrasonography revealing a left-sided perineal abscess with abundant blood flow.
Endoscopy and pathology: Colonoscopy revealed multiple longitudinal ulcers and typical “cobblestone” changes in the terminal ileum (Figure 3). Histopathology showed chronic active inflammation with non-caseating granuloma formation.
Figure 3

Colonoscopy showing longitudinal ulcers in the ileocecal region.
Based on these findings, the patient was diagnosed with CD (Montreal classification: A1 L1 B1p, moderate activity).
2.4 Treatment and clinical course
A multidisciplinary team (MDT) formulated the following plan: Anti-infection and Local Management: Local debridement and drainage were performed. Meropenem was continued based on susceptibility results to control secondary bacterial infection. Nutritional Support: Exclusive enteral nutrition (EEN) was initiated to improve nutritional status and assist in inducing remission. Biologic Induction: Given the local infection and the need for a favorable immune environment for vulvar healing, systemic corticosteroids were avoided. Ustekinumab (UST), which has a favorable safety profile, was selected. An initial intravenous induction dose of 260 mg was administered, followed by a second induction dose of the same quantity 2 weeks later, before transitioning to maintenance therapy. Following the initiation of UST, the patient’s temperature rapidly normalized, and inflammatory markers gradually returned to normal ranges. At the 3-month follow-up, abdominal CT showed significant resolution of small bowel inflammation, and the vulvar abscess had completely resolved. Repeat colonoscopy demonstrated mucosal healing in the ileum, with only scattered superficial erosions remaining. During the follow-up period, the patient reported formed stools and no recurrence of perineal discomfort, achieving both clinical and endoscopic remission.
3 Discussion
This case highlights the diagnostic pitfalls of adolescent CD presenting with recurrent vulvar abscesses. In previous literature, CD-related vulvar lesions typically present as edema, ulcers, and erythema; onset as an “abscess/sepsis-like presentation” is extremely rare (2). We identified six similar cases in the literature where vulvar abscess was the initial presentation of CD and compared them with the current case (Table 1).
Table 1
| Case | Age (year) | Country | Time to diagnosis | GI symptoms | Fever | Anal fistula | Diagnostic methods | Treatment |
|---|---|---|---|---|---|---|---|---|
| 1 (8) | 22 | UK | 3 years | Yes | No | Yes | Colonoscopy + pathology | Abscess ostomy (CD treatment unknown) |
| 2 (9) | 18 | Korea | 5 months | No | No | Yes | Imaging, colonoscopy + pathology | Antibiotics, incision and drainage (I&D); elemental diet + azathioprine + mesalazine; fistulectomy |
| 3 (10) | 12 | United States | 2 years | Yes | Transient, low-grade | No | Vulvar biopsy, colonoscopy + pathology | Prednisone |
| 4 (11) | 14 | United States | 16 months | Yes | No | Yes | Imaging, colonoscopy + pathology | Antibiotics, I&D; infliximab |
| 5 (12) | 10 | United States | 5 years | No | No | Yes | Colonoscopy + pathology | I&D; prednisone, colchicine, methotrexate, azathioprine, infliximab; fistulectomy |
| 6 (13) | 28 | Canada | 9 months | Yes | No | No | Vulvar biopsy, surgical bowel resection pathology | I&D; bowel resection |
| 7 (Current) | 16 | China | 1 month | No | High fever | Yes | FC, imaging, colonoscopy + pathology | Antibiotics, I&D, EEN, ustekinumab |
Clinical characteristics of reported cases of CD initially presenting with vulvar abscesses (all cases were female).
CD, Crohn’s disease; GI, gastrointestinal; I&D, incision and drainage; EEN, exclusive enteral nutrition.
Through literature review and analysis of this case, we summarize the following key clinical insights:
3.1 Diagnostic pitfalls and coping strategies: valuing “occult clues”
Vulvar abscesses are often viewed as local infections. However, when they recur, involve deep spaces, or respond poorly to drainage/antibiotics, CD should be included as a major differential diagnosis. A review of the six similar cases (Table 1) reveals a long average delay in diagnosis. The success in the current case is attributed to:
3.1.1 Targeted history taking
Even without spontaneous complaints, the physician actively inquired about symptoms, uncovering changes in bowel habits. This prompted a gastrointestinal assessment and shortened the time to diagnosis. In clinical practice, we recommend routine inquiry for patients with recurrent vulvar abscesses regarding: bowel habit changes, abdominal pain/distention, perianal symptoms (discharge, pain), oral ulcers, skin/joint symptoms, and growth development. It is important to note that in adolescents, distinct weight loss may not always be evident; instead, growth stagnation or inadequate weight gain can be a subtle but equivalent indicator of chronic disease.
3.1.2 The value of FC and imaging
Guidelines recommend FC to differentiate inflammatory from non-inflammatory bowel diseases (3). As a non-invasive, sensitive marker of intestinal inflammation, FC serves as an effective screening tool for vulvar abscesses unresponsive to antibiotic treatment to identify potential IBD. Regarding imaging, pelvic contrast-enhanced MRI is superior for assessing deep perineal spaces, rectovaginal septum involvement, and potential fistulas. Therefore, we recommend early pelvic MRI for recurrent or persistent vulvar abscesses to rule out deep undrained cavities. Abdominal contrast-enhanced CT can reveal small bowel lesions, such as those in the terminal ileum. In this case, a positive FC screen combined with imaging findings provided a critical chain of evidence, leading to colonoscopy and pathological confirmation.
3.1.3 Differential diagnosis and multidisciplinary strategy
Given the atypical presentation, differentiating vulvar CD from other etiologies is critical. Initially, this case required differentiation from Bartholin’s abscess, vulvar cellulitis, hidradenitis suppurativa, vulvar tuberculosis, sexually transmitted diseases, and Behçet’s disease. These were effectively excluded based on the lack of response to conventional anti-infective therapy, positive fecal calprotectin screening, and specific endoscopic findings. A multidisciplinary approach involving infectious disease specialists, gastroenterologists, gynecologists, surgeons, and dermatologists is essential for such complex cases. Regarding histopathological confirmation, although a vulvar biopsy is valuable for definitive diagnosis, it was deferred in this patient. The decision was made to avoid invasive procedures on the highly inflamed and edematous tissue, which could lead to iatrogenic fistulas or non-healing wounds. Instead, the diagnosis was successfully established through the combination of ileal pathology and the exclusion of other etiologies.
3.2 Literature review: clinical spectrum
Comparing this case with the six identified in the literature (Table 1), the mean age of onset was 17.3 years (range: 10–28 years), similar to our patient. This suggests a need for heightened vigilance in the adolescent population. Furthermore, previous cases mostly presented with a chronic, lingering course without fever (characteristic of “cold abscesses”). In contrast, our patient presented with high fever (39.7 °C) and a severe systemic inflammatory response. This indicates that the clinical spectrum of vulvar CD is broad; it can present not only as chronic granulomas but also as acute, sepsis-like changes with high inflammatory burden.
3.3 Treatment strategy: biologic selection in high-infection risk settings
Currently, guidelines strongly recommend anti-TNF-α monoclonal antibodies and interleukin inhibitors (e.g., UST) as first-line therapies for induction and maintenance in moderate-to-severe CD (3, 4). In pediatric and adolescent guidelines, anti-TNF drugs are often preferred due to stronger evidence (5). In the similar cases we reviewed that required biologic therapy, infliximab was the agent used. While infliximab is extensively documented, other anti-TNF agents such as adalimumab have also demonstrated efficacy in vulvar CD (6). However, the choice of biologic in this case was heavily influenced by the concurrent severe infection. In the acute phase accompanied by abscess and high fever, the use of anti-TNF agents, systemic steroids, or immunosuppressants carries a risk of exacerbating infection dissemination.
This case utilized a regimen of UST combined with EEN. UST precisely inhibits inflammation by blocking the IL-12/23 pathway and is associated with a relatively lower risk of serious opportunistic infections (7). When combined with the nutritional support, anti-inflammatory effects, and mucosal repair properties of EEN (5), this approach successfully achieved “steroid-free” induction of remission. This strategy not only avoided the infection risks associated with broad immunosuppression but also achieved dual healing of the vulvar lesion and intestinal mucosa, confirming its feasibility in complex adolescent CD cases.
4 Conclusion
When adolescent females present with recurrent vulvar abscesses—especially those accompanied by systemic inflammatory reactions disproportionate to local signs and poor response to conventional drainage/antibiotics—CD should be highly suspected. Clinicians must prioritize targeted history taking and combine fecal calprotectin screening with pelvic/abdominal imaging to facilitate early endoscopic and pathological confirmation. Regarding treatment, alongside standardized local management and necessary antibiotic coverage, timely initiation of induction therapy targeting CD activity (such as a steroid-free regimen of UST combined with EEN) contributes to the synchronous control and long-term remission of both vulvar lesions and intestinal inflammation.
5 Patient perspective
“I suffered from the painful swelling and high fever for a month, and the multiple surgeries and antibiotics did not help, which was terrifying. I never thought my mild stomach issues were related. I am grateful the doctors asked detailed questions about my digestion. After starting the new medication and the nutrition drink, my fever stopped quickly, and the pain finally disappeared. I am now back to school and living a normal life.”
Statements
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
Written informed consent was obtained from the minor(s)’ legal guardian/next of kin for the publication of any potentially identifiable images or data included in this article.
Author contributions
MH: Visualization, Methodology, Writing – original draft. HM: Methodology, Writing – original draft, Visualization. NH: Writing – review & editing, Supervision, Resources. JL: Resources, Supervision, Writing – review & editing. XL: Supervision, Writing – review & editing, Conceptualization, Project administration.
Funding
The author(s) declared that financial support was not received for this work and/or its publication.
Conflict of interest
The author(s) declared that this work was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declared that Generative AI was not used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
Barret M de Paras V Battistella M Sokol H Lemarchand N Marteau P . Crohn's disease of the vulva. J Crohns Colitis. (2014) 8:563–70. doi: 10.1016/j.crohns.2013.10.009,
2.
Andreani SM Ratnasingham K Dang HH Gravante G Giordano P . Crohn's disease of the vulva. Int J Surg. (2010) 8:2–5. doi: 10.1016/j.ijsu.2009.09.012,
3.
Lichtenstein GR Loftus EV Afzali A Long MD Barnes EL Isaacs KL et al . ACG clinical guideline: Management of Crohn's disease in adults. Am J Gastroenterol. (2025) 120:1225–64. doi: 10.14309/ajg.0000000000003465,
4.
Gordon H Minozzi S Kopylov U Verstockt B Chaparro M Buskens C et al . ECCO guidelines on therapeutics in Crohn's disease: medical treatment. J Crohns Colitis. (2024) 18:1531–55. doi: 10.1093/ecco-jcc/jjae091,
5.
van Rheenen PF Aloi M Assa A Bronsky J Escher JC Fagerberg UL et al . The medical Management of Paediatric Crohn's disease: an ECCO-ESPGHAN guideline update. J Crohns Colitis. (2021) 15:jjaa161. doi: 10.1093/ecco-jcc/jjaa161,
6.
Haghshenas H Darban B Bagherzadeh MA Karimi M Ataollahi M . Adalimumab as a potential therapeutic option for metastatic Crohn's disease with genital lesions and edema: a case report. Clin Case Rep. (2025) 13:e71424. doi: 10.1002/ccr3.71424,
7.
Cheng D Kochar BD Cai T Ananthakrishnan AN . Risk of infections with Ustekinumab and Tofacitinib compared to tumor necrosis factor α antagonists in inflammatory bowel diseases. Clin Gastroenterol Hepatol. (2022) 20:2366–2372.e6. doi: 10.1016/j.cgh.2022.01.013,
8.
Hudson CN Zeegen R . Crohn's disease, presenting as chronic Bartholin's abscesses. Proc R Soc Med. (1967) 60:338–9. doi: 10.1177/003591576706000409,
9.
Kim S Won YB Seo SK Cho S Choi YS Lee BS et al . Vulvar Crohn's disease in an adolescent diagnosed after unsuccessful surgical treatment. BMC Womens Health. (2021) 21:316. doi: 10.1186/s12905-021-01449-4,
10.
Ploysangam T Heubi JE Eisen D Balistreri WF Lucky AW . Cutaneous Crohn's disease in children. J Am Acad Dermatol. (1997) 36:697–704. doi: 10.1016/s0190-9622(97)80320-9,
11.
Bicette R Tenjarla G Kugathasan S Alazraki A Haddad L . A 14-year-old girl with recurrent vulvar abscess. J Pediatr Adolesc Gynecol. (2014) 27:e83–6. doi: 10.1016/j.jpag.2013.07.010,
12.
Ahad T Riley A Martindale E von Bremen B Owen C . Vulvar swelling as the first presentation of Crohn's disease in children-a report of three cases. Pediatr Dermatol. (2018) 35:e1–4. doi: 10.1111/pde.13272,
13.
Devroede G Schlaeder G Sanchez G Haddad H . Crohn’s disease of the vulva. Am J Clin Pathol. (1975) 63:348–58. doi: 10.1093/ajcp/63.3.348,
Summary
Keywords
adolescent, Crohn’s disease, fecal calprotectin, ustekinumab, vulvar abscess
Citation
He M, Ma H, Huo N, Li J and Li X (2026) Case Report: Recurrent vulvar abscess as the initial manifestation of Crohn’s disease in an adolescent. Front. Med. 13:1763956. doi: 10.3389/fmed.2026.1763956
Received
09 December 2025
Revised
08 January 2026
Accepted
15 January 2026
Published
29 January 2026
Volume
13 - 2026
Edited by
Yasin Sahin, Gaziantep Islam Science and Technology University, Türkiye
Reviewed by
Sabine Drossard, University Hospital Würzburg, Germany
Hend Alotaibi, King Saud University, Saudi Arabia
Updates
Copyright
© 2026 He, Ma, Huo, Li and Li.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiangyan Li, lixyan03598@pkufh.com
†These authors have contributed equally to this work and share first authorship
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.