1 Introduction
In the ever-evolving healthcare landscape, Artificial Intelligence (AI) can revolutionize the patient distribution process among hospitalists. AI-driven patient redistribution (often called Automated Patient Assignment) is a rapidly growing field in hospital medicine. Historically, hospitalist “rounding lists” were created manually by a lead physician or administrator using a whiteboard or spreadsheet—a process that often took 2–3 h every morning. Today, AI systems accomplish this by directly integrating with Electronic Health Records (EHRs) to balance workloads in real-time. It has emerged as a transformative force in an otherwise manual, time-consuming process, bringing new efficiency and precision to healthcare delivery systems.
Hospitalists are physicians who specialize in the comprehensive care of hospitalized patients, managing everything from admission through discharge. They serve as the central coordinators of inpatient care, collaborating with specialists, nurses, and other healthcare professionals to ensure seamless treatment and optimal outcomes. Available around the clock within the hospital setting, hospitalists provide continuity and immediate responsiveness that traditional outpatient physicians cannot offer. Their expertise in managing acute medical conditions, navigating complex hospital systems, and facilitating efficient care transitions makes them indispensable to modern healthcare. By focusing exclusively on inpatient medicine, hospitalists have become the backbone of hospital operations, improving patient safety, reducing length of stay, and enhancing the overall quality of care delivery in an increasingly complex healthcare environment.
2 Present-day challenges
Daily patient distribution among hospitalists presents several complex operational hurdles. The process must balance competing factors, including individual physician workload caps, continuity of care preferences, geographic unit-based assignments, and varying patient acuity levels (1, 2). Hospitalists often have different experience levels and clinical interests that need to be considered, while some may have additional administrative or teaching responsibilities that affect their optimal patient load. The dynamic nature of admissions and discharges creates challenges in maintaining even distribution, potentially overwhelming some hospitalists while underutilizing others (3). The task is further complicated by the need to account for cross-coverage during off-hours, ensure appropriate hand-offs for patients requiring specialty consultation, and manage bounce-backs to avoid patient dissatisfaction (4). Weekend coverage and holiday scheduling add another layer of complexity, as does the need to factor in systemic issues such as language barriers between patients and providers or the geographic spread of patients across different hospital units (5).
3 How it works: understanding AI tools and methodology
The foundation of effective patient distribution lies in accurate workload assessment, where AI excels by processing multiple variables simultaneously [Figure 1].
Figure 1
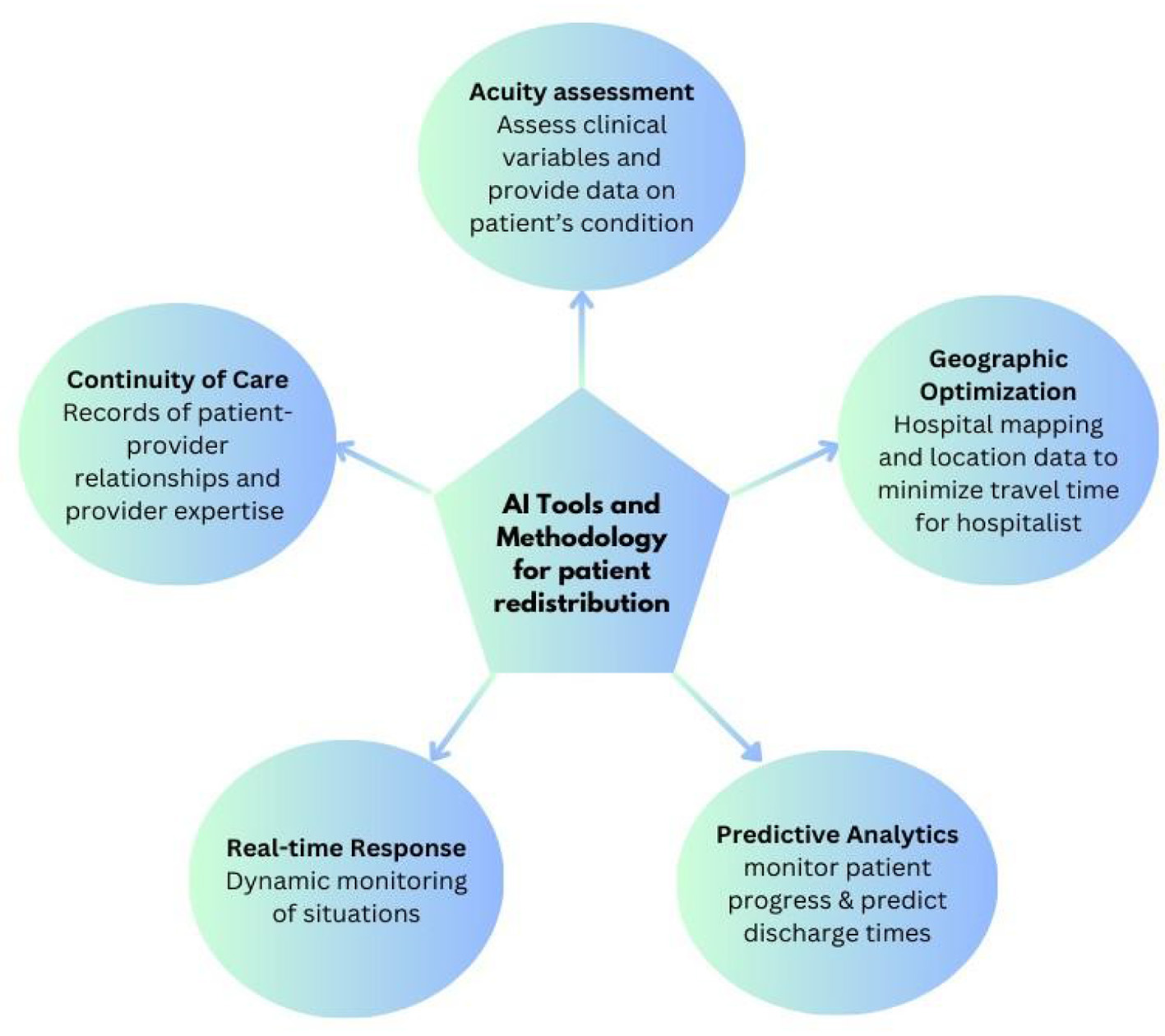
AI tools for patient redistribution.
3.1 Assessing patient acuity
Modern AI systems can analyze patient acuity levels with remarkable precision, accounting for basic metrics and the full complexity of care required for each case (6). These sophisticated systems continuously analyze several clinical variables in real-time, providing healthcare providers with crucial insights into patient conditions by processing vast amounts of data, including vital signs, laboratory results, medication responses, and nursing assessments (7).
3.2 Facility management
AI systems consider the geographic layout of hospital facilities, calculating optimal patient placement to minimize travel time for healthcare providers while maintaining high standards of care. These systems track real-time locations of patients and staff to determine optimal placement and provider assignments, while some focus on predictive bed management using pattern analysis (8). Advanced systems integrate with Real-Time Location Systems to accurately track resources and personnel, enabling workforce distribution across geographic zones. It can incorporate with the Hospital building management infrastructure to monitor occupancy, predict demand, and calculate optimal paths for healthcare providers across different units (9, 10).
3.3 Predictive analytics
By analyzing historical data patterns and current patient conditions, AI systems can accurately forecast likely discharge times (11). The system continuously monitors patient progress and updates predictions, providing a dynamic view of future hospital capacity and staffing needs. These predictive capabilities extend to anticipating potential transfers between units and estimating patient length of stay. By understanding these patterns, hospitals can better allocate resources and maintain optimal staffing levels across different departments. This proactive approach helps prevent bottlenecks in patient flow and ensures smoother transitions across care levels (12).
3.4 Real-time adaptation
Healthcare environments are inherently dynamic, with situations changing rapidly due to emergency admissions, unexpected discharges, or sudden changes in patient conditions (13). AI systems continuously monitor these changes and can recalculate optimal distribution patterns in real time, ensuring the workload remains balanced as conditions evolve (6). The system's ability to process multiple variables simultaneously allows it to suggest redistributions that account for both immediate needs and longer-term implications. When a change occurs, such as an emergency admission or an unexpected staff absence, the AI can quickly propose adjustments that maintain workload balance while minimizing disruption to existing care patterns (9).
3.5 Prioritizing care continuity
AI systems can strengthen patient-provider relationships by tracking interactions and matching patients with familiar providers when appropriate (10). The technology factors in language capabilities, cultural considerations, specialty expertise, and specific treatment requirements to ensure that patients receive care from the most appropriately qualified providers (14). Additionally, AI maintains detailed profiles of healthcare providers' specializations, past experiences, and strengths, enabling nuanced assignment decisions for complex cases and effective workload management for new hospitalists (15).
4 Implementation in current hospital systems & impact
Several major hospital systems have already moved past the pilot phase and fully integrated automated patient assignment and redistribution systems. Here are the specific systems, the technology they use, and the data-backed results they have reported [Table 1]:
Table 1
| System | Primary focus | Notable features |
|---|---|---|
| Medaptus (assign) | Workload balancing | Uses “configurable logic” to automate morning lists. It factors in census, acuity, and “continuity” rules. |
| Qventus | Capacity & flow | An AI “command center” that predicts discharge barriers and redistributes resources to prevent “boarding” in the ER. |
| Lightning bolt | Scheduling & equity | Uses “combinatorial optimization” to ensure shifts, night calls, and patient loads are equalized over months, not just days. |
| Ingenious med | Workflow & census | Features a “census manager” that allows for bulk drag-and-drop reassignment and real-time visibility of patient spikes. |
| Carealign | Task management | While not a pure “redistribution” engine, it acts as a digital “paper sheet” that syncs tasks across teams to prevent redundant work. |
Examples of specific AI platforms currently leading the market.
4.1 Northwell health (New York)
Northwell Health is one of the most prominent examples of success in this area. They implemented Medaptus's “Assign” software to replace manual spreadsheets and whiteboards. This reduced the lead hospitalists' morning assignment process time by 80% from 2.5 h down to about 30 min, saving roughly 2 h of administrative work per day for every lead physician, allowing them to start patient rounds significantly earlier and reducing the “morning bottleneck” of discharges (16).
4.2 HCA healthcare (National)
HCA, the largest for-profit hospital chain in the U.S., developed an internal AI-driven operational solution called Timpani. Although not used among physicians, this tool manages nursing shifts and patient loads and has shown its impact. The system monitors real-time needs on each nursing unit. If the AI detects a nurse is overloaded, or a patient is behind on scheduled care, it alerts clinical coordinators to rebalance patient loads mid-shift. HCA also uses AI for nurse handoffs, which they estimated previously took 40 min per shift. Early data from their pilot sites showed an 86% factuality rate in AI-generated reports, which significantly lightened the cognitive load on staff during redistribution (17).
4.3 Banner health (arizona/multistate)
Banner Health partnered with Qventus, a leading AI platform for hospital operations, to manage inpatient capacity and surgical scheduling. Across its facilities, Banner reported that the AI solution released 369 h of block time (operating room capacity) every month by predicting cancellations and reallocating time automatically. Qventus reported that its hospital clients (including Banner and Ardent Health) typically see a 15% to 30% reduction in “excess days” (days patients stay beyond what is medically necessary) and a 10% to 20% reduction in Emergency Department boarding times (18).
4.4 Pacific northwest health system
In a broader implementation across 12 hospitals, this system integrated AI-driven staff scheduling and patient load balancing. Within 6 months, the system reported about 32% reduction in nurse overtime, about 27% increase in staff satisfaction scores, and about 28% decrease in agency staffing costs (19).
5 Impact of AI on patient distribution
Using AI to distribute patients among hospitalists represents a transformative advancement in healthcare operations management. It has a positive impact on the daily workflow in many ways [Figure 2].
Figure 2
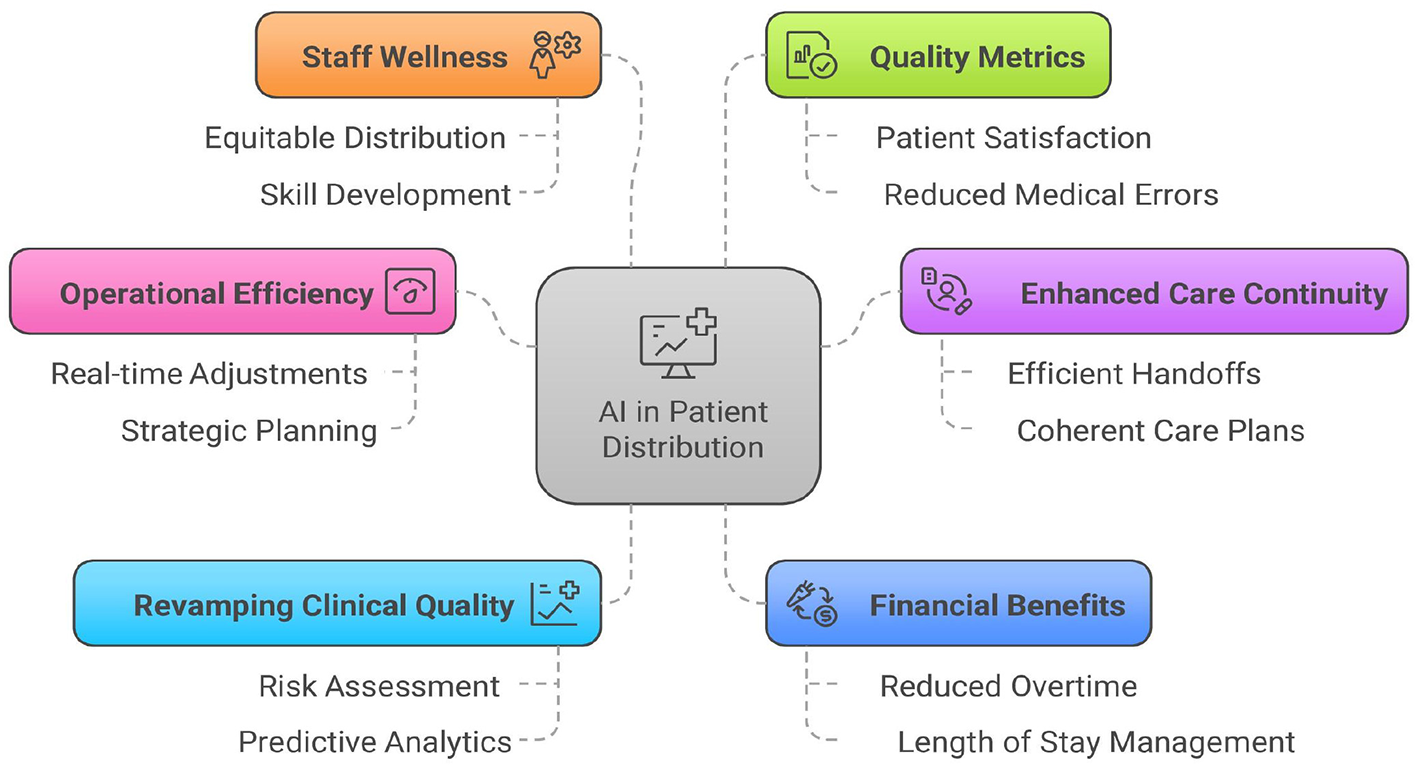
Impact of AI-driven patient redistribution.
5.1 Operational efficiency
Modern AI algorithms automate the previously manual process, freeing up significant time for hospitalist leaders and allowing them to focus on direct patient care and strategic planning. The system's ability to make real-time adjustments ensures dynamic redistribution when new admissions arrive or patient conditions change (20).
5.2 Enhanced care continuity
AI systems excel at maintaining consistent patient-physician relationships by tracking previous assignments and preferences. This systematic approach minimizes the number of different hospitalists seeing each patient, resulting in more efficient handoff management and more coherent care plans. The technology ensures that complex cases receive appropriate follow-up and consistent care throughout the patient's hospital stay (14).
5.3 Revamping clinical quality
AI's risk assessment capabilities enable precise matching of patient needs with hospitalist expertise. The system evaluates patient complexity and acuity to ensure equitable distribution of high-risk cases, while accounting for hospitalist subspecialty training and experience levels. Hospitals can anticipate patient flow patterns through merged predictive analytics and prepare proactively for admission surges or discharge patterns (15).
5.4 Financial benefits
There is a potential for substantial financial advantages through optimized resource utilization. Hospitals experience reduced overtime costs due to better workload balancing and decreased reliance on locum coverage. The system's efficient care coordination leads to appropriate length-of-stay management and reduced delays in care delivery, resulting in significant cost savings (21).
5.5 Staff wellness
AI-driven distribution systems promote staff wellbeing by ensuring equitable distribution of complex cases and patient load. The technology considers individual hospitalist preferences and scheduling constraints while providing opportunities for skill development through appropriate case mix assignments. This balanced approach significantly reduces the risk of burnout while enhancing professional growth opportunities (6).
5.6 Quality metrics
Patient satisfaction has markedly improved through enhanced continuity of care and reduced wait times. Consistent hospitalist assignments lead to better communication and patient experience. Clinical outcomes benefit from advanced management of complex cases and a reduced risk of medical errors, due to balanced workloads and consistent provider coverage (9).
6 Considerations and challenges
Successfully implementing AI-driven patient distribution requires careful planning and consideration of various factors. The technical infrastructure must be well-consolidated with existing hospital management systems. This merger should enable seamless data flow while maintaining high-security standards for patient and provider information.
6.1 Technical considerations
Blending existing Electronic Health Record systems must enable real-time access to patient data, including acuity scores, admission/discharge timing, and special care requirements. The AI system requires reliable interfaces with scheduling software and hospitalist management platforms (13).
6.2 Operational impact
Daily redistribution affects hospitalist workflows, handoffs, and continuity of care. Geographic clustering of patients' needs to be balanced against workload equity. The system must accommodate varying levels of hospitalist experience and specialties while maintaining appropriate patient-to-provider ratios (13).
6.3 Clinical safety
Patient safety depends on accurate handoff documentation and clear communication protocols during redistributions. The AI system must be robust enough to recognize complex cases that require continuity with specific providers and to account for hospitalists' familiarity with particular conditions or units (22).
6.4 Data requirements
The system needs comprehensive historical data on patient outcomes, hospitalist performance metrics, and workload patterns. Real-time inputs include fluctuations in census, admission patterns, and provider availability. Data quality and standardization across different hospital units are essential (20).
6.5 Implementation strategy
A phased rollout allows for system refinement and staff adaptation. Initial implementation should focus on essential load balancing before incorporating more complex factors. Regular evaluation of redistribution outcomes helps refine algorithms and identify needful adjustments (10).
6.6 Employee training
Success requires hospitalist buy-in through clear communication of benefits and addressing concerns about disrupted patient relationships. Training programs must prepare staff for new workflows and system interactions. Regular feedback channels help identify and resolve operational issues (23).
6.7 Cost implications
Implementation costs include software development, consolidation with existing systems, staff training, and ongoing maintenance. The Return On Investment (ROI) assessment should consider improved efficiency against potential increases in technical support needs (13).
6.8 Ethical/Legal considerations
Systems must be transparently designed, allowing healthcare administrators to understand the basis for distribution recommendations. Privacy protection and data security must be prioritized, and accountability structures should be established for system outcomes (24). The system must comply with privacy regulations and maintain audit trails of redistribution decisions. Clear policies should address liability concerns and establish override protocols when human judgment conflicts with AI recommendations (15). The goal is to support, not replace, human judgment in decisions, maintaining the critical role of experienced healthcare professionals in the distribution process.
7 Future outlook
As advanced analytics and machine learning capabilities continue to evolve, they will leverage increasingly larger datasets to improve prediction accuracy, employ sophisticated pattern recognition to optimize staffing models and resource allocation, and better integrate with telemedicine and cross-facility coordination (10). Future developments will include enhanced integration with hospital systems, improved team coordination tools, and advanced performance-monitoring capabilities. These technologies promise to significantly improve efficiency, provider satisfaction, and patient outcomes as healthcare organizations continue to refine their patient distribution processes.
Statements
Author contributions
DS: Conceptualization, Data curation, Formal analysis, Investigation, Project administration, Resources, Supervision, Validation, Writing – original draft, Writing – review & editing. NT: Data curation, Formal analysis, Methodology, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declared that financial support was not received for this work and/or its publication.
Conflict of interest
The author(s) declared that this work was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declared that generative AI was used in the creation of this manuscript. Figure 2 was created using Napkin AI (https://www.napkin.ai/).
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
Elliott DJ Young RS Brice J Aguiar R Kolm P . Effect of hospitalist workload on the quality and efficiency of care. JAMA Intern Med. (2014) 174:786. doi: 10.1001/jamainternmed.2014.300
2.
Wachter RM Goldman L . Zero to 50,000 - the 20th anniversary of the hospitalist. N Engl J Med. (2016) 375:1009–11. doi: 10.1056/NEJMp1607958
3.
Arora VM Reed DA Fletcher KE . Building continuity in handovers with shorter residency duty hours. BMC Med Educ. (2014) 14:S16. doi: 10.1186/1472-6920-14-S1-S16
4.
Rattray NA Flanagan ME Militello LG Barach P Franks Z Ebright P et al . “Do you know what I know?”: how communication norms and recipient design shape the content and effectiveness of patient handoffs. J Gen Intern Med. (2019) 34:264–71. doi: 10.1007/s11606-018-4755-5
5.
Sinsky CA Trockel MT Dyrbye LN Wang H Carlasare LE West CP et al . Vacation days taken, work during vacation, and burnout among US physicians. JAMA Netw Open. (2024) 7:e2351635. doi: 10.1001/jamanetworkopen.2023.51635
6.
Topol EJ . High-performance medicine: the convergence of human and artificial intelligence. Nat Med. (2019) 25:44–56. doi: 10.1038/s41591-018-0300-7
7.
Edelson DP Churpek MM Carey KA Lin Z Huang C Siner JM et al . Early warning scores with and without artificial intelligence. JAMA Netw Open. (2024) 7:e2438986. doi: 10.1001/jamanetworkopen.2024.38986
8.
Al Harbi S Aljohani B Elmasry L Baldovino FL Raviz KB Altowairqi L et al . Streamlining patient flow and enhancing operational efficiency through case management implementation. BMJ Open Qual. (2024) 13:e002484. doi: 10.1136/bmjoq-2023-002484
9.
Blanchard JC Rudin RS . Improving hospital efficiency through data-driven management: a case study of health first, Florida. Rand Health Q. (2016) 5:2. https://pmc.ncbi.nlm.nih.gov/articles/PMC5158217/
10.
Maleki Varnosfaderani S Forouzanfar M . The role of AI in hospitals and clinics: transforming healthcare in the 21st century. Bioengineering. (2024) 11:337. doi: 10.3390/bioengineering11040337
11.
Sharma BK . AI-managed hospital workforce. In:ChatterjeeJMSujathaRSaxenaSK, editors. Medical Virology: From Pathogenesis to Disease Control. Singapore: Springer Nature (2024). 221–51.
12.
Bertsimas D Pauphilet J Stevens J Tandon M . Predicting inpatient flow at a major hospital using interpretable analytics. Manuf Serv Oper Manag. (2022) 24:2809–24. doi: 10.1287/msom.2021.0971
13.
Li Y-H Li Y-L Wei M-Y Li G-Y . Innovation and challenges of artificial intelligence technology in personalized healthcare. Sci Rep. (2024) 14:18994. doi: 10.1038/s41598-024-70073-7
14.
Shaban M Mohammed HH Gomaa Mohamed Amer F Shaban MM Abdel-Aziz HR Ibrahim AM . Exploring the nurse-patient relationship in caring for the health priorities of older adults: qualitative study. BMC Nurs. (2024) 23:480. doi: 10.1186/s12912-024-02099-1
15.
Daneshvar N Pandita D Erickson S Snyder Sulmasy L DeCamp M ACP Medical Informatics Committee and the Ethics Professionalism and Human Rights Committee. Artificial intelligence in the provision of health care: an American College of Physicians policy position paper. Ann Intern Med. (2024) 177:964–7. doi: 10.7326/M24-0146
16.
17.
18.
19.
20.
Knight DRT Aakre CA Anstine CV Munipalli B Biazar P Mitri G et al . Artificial intelligence for patient scheduling in the real-world health care setting: a metanarrative review. Health Policy Technol. (2023) 12:100824. doi: 10.1016/j.hlpt.2023.100824
21.
Beam AL Kohane IS . Big data and machine learning in health care. JAMA. (2018) 319:1317–8. doi: 10.1001/jama.2017.18391
22.
Shaik T Tao X Higgins N Li L Gururajan R Zhou X et al . Remote patient monitoring using artificial intelligence: current state, applications, and challenges. Wiley Interdiscip Rev Data Min Knowl Discov. (2023) 13:10–18. doi: 10.1002/widm.1485
23.
Gianfrancesco MA Tamang S Yazdany J Schmajuk G . Potential biases in machine learning algorithms using electronic health record data. JAMA Intern Med. (2018) 178:1544–7. doi: 10.1001/jamainternmed.2018.3763
24.
Char DS Shah NH Magnus D . Implementing machine learning in health care - addressing ethical challenges. N Engl J Med. (2018) 378:981–3. doi: 10.1056/NEJMp1714229
Summary
Keywords
artificial intelligence, hospital operations, hospitalists, patient assignment, patient redistribution
Citation
Save D and Tillu N (2026) Artificial Intelligence (AI) driven patient assignment: optimizing daily redistribution among hospitalists. Front. Med. 13:1767258. doi: 10.3389/fmed.2026.1767258
Received
14 December 2025
Revised
31 December 2025
Accepted
06 January 2026
Published
05 February 2026
Volume
13 - 2026
Edited by
Cheng Kai Kao, The University of Chicago, United States
Reviewed by
Aydin Teymourifar, Istanbul Sabahattin Zaim University, Türkiye
Kiran Veernapu, Intermountain Healthcare, United States
Updates
Copyright
© 2026 Save and Tillu.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dhaval Save, dhavalsave@gmail.com
ORCID: Dhaval Save orcid.org/0000-0003-3166-9594
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.