- 1Southwest National Primate Research Center, Texas Biomedical Research Institute, San Antonio, TX, United States
- 2Department of Molecular Virology and Microbiology, Baylor College of Medicine, Houston, TX, United States
The human-specific tropism of Human Immunodeficiency Virus Type 1 (HIV-1) has complicated the development of a macaque model of HIV-1 infection/AIDS that is suitable for preclinical evaluation of vaccines and novel treatment strategies. Several innate retroviral restriction factors, such as APOBEC3 family of proteins, TRIM5α, BST2, and SAMHD1, that prevent HIV-1 replication have been identified in macaque cells. Accessory proteins expressed by Simian Immunodeficiency virus (SIV) such as viral infectivity factor (Vif), viral protein X (Vpx), viral protein R (Vpr), and negative factor (Nef) have been shown to play key roles in overcoming these restriction factors in macaque cells. Thus, substituting HIV-1 accessory genes with those from SIV may enable HIV-1 replication in macaques. We and others have constructed macaque-tropic HIV-1 derivatives [also called simian-tropic HIV-1 (stHIV-1) or Human-Simian Immunodeficiency Virus (HSIV)] carrying SIV vif to overcome APOBEC3 family proteins. Additional modifications to HIV-1 gag in some of the macaque-tropic HIV-1 have also been done to overcome TRIM5α restriction in rhesus and cynomolgus macaques. Although these viruses replicate persistently in macaque species, they do not result in CD4 depletion. Thus, these studies suggest that additional blocks to HIV-1 replication exist in macaques that prevent high-level viral replication. Furthermore, serial animal-to-animal passaging of macaque-tropic HIV-1 in vivo has not resulted in pathogenic variants that cause AIDS in immunocompetent macaques. In this review, we discuss recent developments made toward developing macaque model of HIV-1 infection.
Introduction
The inefficient replication of HIV-1 in macaques has complicated the development of a true HIV-based animal model of AIDS. Alternative animal models such as infection of macaques with Simian Human Immunodeficiency Virus (SIV) or Simian-Human Immunodeficiency Virus (SHIV) containing HIV envelope (Env) or reverse transcriptase have been developed. These animal models have been extremely useful in understanding HIV pathogenesis and disease progression, as well as understanding the efficacy of vaccines and drugs. However, these models do have short comings. A major concern is the genetic difference between HIV-1 and SIV. These viruses are not likely to share immunodominant cytotoxic T-cell (CTL) epitopes, and the structural differences in Env protein may lead to qualitative differences in the antibody responses. Furthermore, although the SHIV-model allows for testing of HIV Env based vaccines, it is not possible to test vaccines or antiretroviral drugs targeting multiple HIV-1 proteins. For example, efficacy of vaccine approaches using HIV Gag and Nef as immunogens cannot be tested using SHIV as a challenge virus. Additionally, some of the vaccine candidates that showed protection against SHIV did not exhibit protective efficacy in human clinical trials. It is therefore important to rationally and minimally modify HIV-1 such that it can replicate and cause AIDS in macaque species. Such an animal model will be an extremely valuable tool for preclinical evaluation of vaccines and novel therapeutics. Therefore, there is a need for developing pathogenic HIV-1 variants that can cause AIDS in macaque species.
Retroviral Restriction Factors
The four major retroviral restriction factors are the apolipoprotein B mRNA editing enzyme catalytic polypeptide 3 (APOBEC3 or A3) family of proteins, tripartite motif containing (TRIM) family of proteins, BST2/CD317/Tetherin, and sterile alpha motif (SAM) and histidine/aspartic acid (HD) domain containing protein 1 (SAMHD1) [reviewed in Thippeshappa et al. (2012); Saito and Akari (2013)]. They inhibit retroviral replication at different stages of the life cycle. The fact that each of these retroviral restriction factors are upregulated by type 1 interferons (IFN-1) and each gene has been under strong positive selection in non-human primates and humans in response to lentiviral infections, suggests the importance of these restriction factors in controlling infection (Sawyer et al., 2004; Liu et al., 2005; Sawyer et al., 2005; McNatt et al., 2009; Laguette et al., 2012; Lim et al., 2012; Zhang et al., 2012). Both HIV-1 and SIV has counter measures to overcome these restriction in humans, but not in other species, suggesting the importance of overcoming these restriction factors for cross-species transmission (CST). Here, we briefly describe the importance of overcoming these restriction factors for generation of macaque-tropic HIV-1 and its derivatives.
The APOBEC3 family proteins are cytidine deaminases that render Vif deficient HIV-1 progeny virions non-infectious in non-permissive cells but not permissive cells (Sheehy et al., 2002; Aghokeng et al., 2010). In the absence of Vif, APOBEC3G (A3G) is efficiently packaged into HIV-1 progeny virions, while only small amount of A3G is packaged into wild-type HIV-1, which results in induction of G to A mutations in the viral genome (Sheehy et al., 2003). Interestingly, Vif counteraction of A3G occurs in a species-specific manner (Mariani et al., 2003; Bogerd et al., 2004; Mangeat et al., 2004; Schrofelbauer et al., 2004; Xu et al., 2004). HIV-1 Vif protein can antagonize human A3G (hA3G) but not rhesus macaque (RM, Macaca mulatta) A3G (Mariani et al., 2003). Interestingly, RM A3G is antagonized by both the SIVmac and SIVagm Vif proteins (Mariani et al., 2003), suggesting that Vif-mediated inhibition of macaque APOBEC3 family proteins could be important for CST of HIV-1 to macaques.
TRIM5α was identified by screening a rhesus macaque complementary DNA (cDNA) expression library for genes that would block HIV-1 infection in human cells (Stremlau et al., 2004). In New World monkey cells, such as Owl monkeys (OWM, Aotus trivirgatus), a novel TRIM5-cyclophilin A fusion protein (TRIMcyp) exhibits a post-entry barrier to HIV-1 infection (Nisole et al., 2004; Sayah et al., 2004). Prevalence of TRIMcyp has also been found in pigtailed macaques (PTM, Macaca nemestrina), cynomolgus macaques (CM, Macaca fascicularis) and Indian origin RMs (Brennan et al., 2007; Liao et al., 2007; Brennan et al., 2008; Newman et al., 2008; Wilson et al., 2008; Kuang et al., 2009; Dietrich et al., 2011). Both TRIM5α and TRIMcyp proteins exhibit species-specific restriction. Human TRIM5α does not restrict HIV-1; however, both RM and CM TRIM5α restrict HIV-1 but not SIVmac (Hatziioannou et al., 2004; Stremlau et al., 2004; Nakayama et al., 2005). TRIMcyp proteins also exhibit a diverse range of restrictions. OWM TRIMcyp interferes with HIV-1 but not SIVmac (Nisole et al., 2004; Sayah et al., 2004), whereas RM TRIMcyp restricts HIV-2 and SIVagm but does not inhibit HIV-1 and SIVmac (Virgen et al., 2008; Wilson et al., 2008). Interestingly, TRIMcyp protein expressed by PTM and CM do not block either HIV-1 or SIVmac239 infection (Brennan et al., 2008). However, PTM TRIMcyp can restrict FIV, HIV-2 and SIVagm infection (Virgen et al., 2008). These studies suggest that both the TRIM5α and TRIMcyp proteins can act as barriers for CST of lentiviruses.
BST2 or Tetherin is an interferon (IFN) inducible, Vpu sensitive factor that interferes with the release of HIV-1 progeny virions from the cell surface (Neil et al., 2008; Van Damme et al., 2008). HIV-1 Vpu can antagonize human and chimpanzee BST2, but cannot overcome the activity of BST2 from RM, AGM, and mustached monkeys (Cercopithecus cephus) (Goffinet et al., 2009; Gupta et al., 2009; Jia et al., 2009; Lim and Emerman, 2009; McNatt et al., 2009; Rong et al., 2009). However, Vpu may not be absolutely required for replication in humans. This is due to the fact that there are Vpu sequences (derived from primary isolates or directly from patients) in the HIV database that contain a mutation in the start codon (Li et al., 1991; Theodore et al., 1996; Schubert et al., 1999; Dejucq et al., 2000). Interestingly, SIVmac239 Nef can target RM, PTM, and AGM BST2 but cannot antagonize human BST2 (Jia et al., 2009; Zhang et al., 2009; Yang et al., 2010). Thus, although BST2 antagonism may not be absolutely required for HIV-1 infection in humans, counteraction of BST2 function may be required for CST of HIV-1 to macaques.
Sterile alpha motif (SAM) and histidine/aspartic acid (HD) domain containing protein 1 (SAMHD1) was identified as a novel HIV-1 restriction factor in myeloid cells by two independent groups. They showed that Vpx interacts with SAMHD1 and results in proteasome-mediated degradation in myeloid cells (Hrecka et al., 2011; Laguette et al., 2011), which was later found to be active in quiescent T cells as well (Baldauf et al., 2012; Descours et al., 2012). It is interesting that HIV-1 does not have a mechanism to overcome human SAMHD1 function. However, human and gibbon SAMHD1 can be degraded by Vpx proteins from HIV-2rod, SIVmac, and SIVsm but not by Vpx from SIVrcm and SIVmnd2. Interestingly, these Vpx proteins can induce degradation of rhesus macaque and mangabey SAMHD1 (Laguette et al., 2012). Thus, Vpx-mediated degradation of macaque SAMHD1 may be required for adaptation of HIV-1 to macaque species. In addition, importance of Vpx expression for SIV replication has also been noticed in CD4 T cells and activated PBMCs where SAMHD1 restriction is inactive (Guyader et al., 1989; Kappes et al., 1991; Yu et al., 1991; Akari et al., 1992; Belshan et al., 2012; Shingai et al., 2015). Interestingly, Vpx protein from SIVrcm and SIVmnd2 enhanced replication of HIV-1 in resting CD4 T cells in a SAMHD1-independent manner, suggesting that Vpx overcomes another restriction factor in CD4 T cells (Baldauf et al., 2017). Two recent studies identified the human silencing hub (HUSH) epigenetic repressor complex as a potential restriction factor that controls viral expression and is antagonized by Vpx (Chougui et al., 2018; Yurkovetskiy et al., 2018). Vpx associated with the HUSH complex and resulted in proteasome-mediated degradation (Chougui et al., 2018; Yurkovetskiy et al., 2018). Thus, Vpx-mediated antagonization of HUSH complex may also be required for efficient replication in macaque lymphocytes.
Additional Resistance Factors
There is growing evidence for the existence of additional IFN stimulated genes (ISGs) that control HIV-1 replication. In vitro, IFN treatment has been shown to potently inhibit HIV and SIV replication (Ho et al., 1985; Kornbluth et al., 1989; Shirazi and Pitha, 1992; Meylan et al., 1993; Cheney and McKnight, 2010; Goujon and Malim, 2010). Several resistance factors have been identified using in vitro cell culture models that potently inhibit retroviral replication. Interestingly, how HIV-1 evades the function of these resistance factors is not clear. (1) Myxovirus resistance 2 (MX2) was identified, using cDNA screens as a factor that inhibits viral cDNA accumulation and integration in IFN-treated cells (Goujon et al., 2013; Kane et al., 2013; Liu Z. et al., 2013). MX2 has been shown to interact with viral capsid protein (Goujon et al., 2013; Kane et al., 2013; Liu S.Y. et al., 2013; Fribourgh et al., 2014; Fricke et al., 2014) and may prevent viral cDNA from entering the nucleus by mechanisms that are not clear. (2) Interferon-inducible transmembrane proteins (IFITMs), particularly IFITM1, IFITM2, and IFITM3, are type II transmembrane proteins found in various cellular membranes (Bailey et al., 2013; Li et al., 2013; Jia et al., 2014; Li et al., 2015). IFITMs restrict a number of enveloped viruses including HIV-1 (Lu et al., 2011; Yu et al., 2015; Tartour et al., 2017). They have been shown to block virus entry by impairing the hemifusion process (Li et al., 2013). IFITM proteins protect target cells from incoming virus by affecting virus-cell fusion and targeting virions to endosomal or lysosomal compartments (Weidner et al., 2010; Desai et al., 2014; Spence et al., 2019). IFITM proteins also incorporate in to the nascent HIV particles during virus assembly and decrease the infectivity of the virions (Compton et al., 2014; Tartour et al., 2014). (3) Another ISG that inhibits HIV-1 infection is schlafen (SLFN11), which inhibits virion production by affecting protein synthesis (Li et al., 2012). (4) Cholesterol-25-hydoxylase (CH25H) is an enzyme that converts cholesterol to 25-hyroxycholesterol (25-HC). Treatment of cultured cells with 25-HC has been shown to inhibit replication of several enveloped viruses, including HIV, by impairing fusion of viral envelope with cell membrane (Liu S.Y. et al., 2013; Gomes et al., 2018). (5) Zinc-finger antiviral protein (ZAP) is another ISG that inhibits HIV-1 replication in overexpressed cells by translational repression and viral mRNA degradation through recruitment of cellular mRNA degradation machinery (Zhu et al., 2011; Zhu et al., 2012). (6) Guanylate-binding protein 5 is a member of the IFN-inducible guanosine triphosphatase (GTPases) superfamily that inhibits HIV-1 infectivity by interfering with the N-linked oligosaccharide glycosylation modifications of the HIV envelope glycoprotein (Krapp et al., 2016; Hotter et al., 2017). This increases the incorporation of unprocessed immature gp160 into progeny virions resulting in decrease in infectivity of the virions (Hotter et al., 2017). (7) Interferon-stimulated gene 15 (ISG15) is a 15 kDa protein belonging to the family of ubiquitin-like modifiers. The conjugation of ISG15 to target proteins is called ISGylation. HECT and RLD domain containing E3 ubiquitin protein ligase 5 (HERC5) mediated ISGylation results in the in the accumulation of Gag at the plasma membrane (Wong et al., 2006; Woods et al., 2011). Furthermore, ISGylation inhibits ubiquitination of Gag and Tsg101, which is a protein involved in endosomal sorting complexes required for transport (ESCRT) pathway. So, inhibition of this interaction prevents HIV-1 release (Okumura et al., 2006; Pincetic et al., 2010).
Non-IFN Induced Restriction Factors
Apart from IFN-inducible restriction factors, there are also constitutively expressed intrinsic restriction factors that inhibit HIV-1 replication. Serine Incorporator (SERINC) proteins are a class of proteins, comprising of five members (SERINC 1-5), that facilitate the incorporation of serines into membrane lipids (Inuzuka et al., 2005). Recently SERINC 3 and 5 were identified as inhibitors of HIV-1 infectivity that are counteracted by Nef (Rosa et al., 2015; Usami et al., 2015). In the absence of Nef expression, SERINC5 incorporates into budding virions and reduces the infectivity of virions through mechanisms that are not completely clear. HIV-1 Nef, as well as MLV GlycoGag and equine infectious anemia virus (EIAV) S2 proteins decrease the expression of SERINC5 at the plasma membrane and exclude them from virions, thus restoring the infectivity of virions (Pizzato et al., 2007; Usami et al., 2014; Rosa et al., 2015; Usami et al., 2015; Chande et al., 2016).
Another non-IFN induced restriction that inhibits HIV-1 release is The T cell Ig and mucin domain (TIM) protein (Li et al., 2019). Release of Nef-deficient HIV-1 is most potently inhibited by TIM1 compared to wild-type HIV-1. Interestingly, SERINC proteins enhance the ability of TIM-1 to block HIV-1 release likely by increasing TIM-1 expression at plasma membrane. Nef proteins of HIV-1 and other lentiviruses function as antagonists to overcome the TIM-mediated restriction in part by promoting TIM-1 internalization from the plasma membrane and sequestering TIM-1 within intracellular compartments (Li et al., 2019). Furthermore, MLV glycoGag and EIAV S2 proteins, which are known SERINC antagonists, can also relieve the ability of TIM-1 to block HIV-1 release, suggesting a role for SERINC proteins in TIM-mediated restriction (Li et al., 2019). This suggests that lentiviral Nef proteins counteract TIM-1 restriction in part through SERINC to facilitate HIV-1 release and replication.
Adaptation of HIV-1 to Macaques: Lessons From Cross-Species Transmission of Lentiviruses to Humans
SIVs are present in more than 40 species of non-human primates (Apetrei et al., 2004; Sharp and Hahn, 2011). The ones most closely related to HIV-1 and HIV-2 were detected in chimpanzees and sooty mangabeys, respectively (Hirsch et al., 1989; Gao et al., 1999). The ability of lentiviruses to infect new species vary. For example, SIVcol (from colobus monkeys) is evolutionarily isolated, whereas SIVagm (from African green monkeys) frequently moves between host subspecies (Bell and Bedford, 2017). So far, only chimpanzees, gorillas, and sooty mangabeys have transmitted their viruses to humans. Four independent transmission events of SIVcpz and SIVgor from chimpanzees and gorillas to humans gave rise to HIV-1 groups M, N, O, and P (Gao et al., 1999; Sharp and Hahn, 2011; D’Arc et al., 2015). HIV-2 groups A through I arose from nine zoonotic transmission events of SIVsmm from sooty mangabeys to humans (Hirsch et al., 1989; Gao et al., 1992; Chen et al., 1996; Ayouba et al., 2013). Studies over the years have demonstrated the key viral adaptations that led to successful CST of HIV-1 precursors from monkeys to chimpanzees, and then ultimately to humans [reviewed in Sauter and Kirchhoff (2019)]. Early report by Bailes et al. (2003) suggested that SIVcpz resulted from a recombination between an ancestor of SIVs found in greater spot-nosed, mona, and mustached monkeys (SIVgsn/mon/mus) and a SIV precursor found in redcapped mangabeys (SIVrcm). However, recent phylogenetic analysis studies from Bell and Bedford (2017) suggest cross-species transmission of SIV from redcapped mangabeys to mandrills (Bell and Bedford, 2017). Thus, it is not clear if part of the SIVcpz genome originated from SIVrcm or SIVmnd2. There are still large portions of the SIVcpz genome with unknown origins. Bell and Bedford (2017) also suggest that the genome of SIVcpz may have resulted from recombination of SIVrcm, SIVgsn/mon/mus, and an unknown SIV.
For CST to happen, lentiviruses have to adapt to utilize a number of cellular virus-dependency factors required for replication in the host. In addition, lentiviruses have to develop mechanisms to evade or counteract a variety of intrinsic restriction factors at every step of the virus life cycle. Recent studies have provided clues as to how this hybrid virus adapted to utilize some of the host-dependency factors as well as counteraction mechanisms required for spread in chimpanzees. The inability of chimpanzee TRIM5α to restrict many SIVs, including SIVgsn (Kratovac et al., 2008), probably presented an advantage for transmission of SIV from monkeys to chimpanzees. Interestingly, the recombination event that created SIVcpz resulted in the deletion of vpx coding sequences and generation of a unique vif that overlaps with vpr (Etienne et al., 2013). Unlike most SIV Vif proteins, this Vif protein from SIVcpz can antagonize chimpanzee A3G and A3D (Etienne et al., 2013). Additionally, chimpanzee A3F and A3H did not constitute a major barrier as SIVrcm Vif can antagonize these restriction factors (Etienne et al., 2013). However, the deletion of vpx may have cost the ability of these viruses to antagonize SAMHD1 and there by affecting the ability of SIVcpz and HIV-1, to infect myeloid cells and resting CD4+T cells. For adaptation to new species, lentiviruses also have to overcome additional restriction factors such as SERINC and BST2 at the late stage in virus life cycle. HIV-1 and SIV Nef can counteract SERINC5 in a species-independent manner (Heigele et al., 2016). Thus, it did not constitute a major barrier. However, SIVcpz needed to evolve mechanism to antagonize chimpanzee BST2. SIVcpz obtained its vpu gene from SIVgsn/mus/mon lineage, which can counteract monkey but not chimpanzee BST2 (Sauter et al., 2009). Although origin of the nef gene in SIVcpz is not clear, it is either derived from the SIVrcm lineage or from an unknown SIV (Bell and Bedford, 2017). Interestingly, during adaptation, SIVcpz evolved nef as a mechanism to antagonize BST2, and Vpu retained its other functions such as ability to degrade CD4. Apart from overcoming restriction factors, adaptation of SIVcpz to chimpanzees also coincided with changes in Gag that enabled interaction with host dependency factor RanBP2/Nup358 (Meyerson et al., 2018). This interaction of capsid with the nuclear pore protein RanBP2/Nup358 is required for efficient nuclear import of the viral genome (Ocwieja et al., 2011).
Transmission from chimpanzees to gorillas occurred probably because the virus was able to maintain interactions with host dependency factors as well mechanisms to counteract restriction factors in gorillas. Furthermore, SIVgor also acquired mutations in nef and vif to overcome gorilla BST2 and A3G mediated species-specific barriers, respectively (Sauter et al., 2009; Letko et al., 2013; D’Arc et al., 2015). These additional modifications probably helped SIVgor to replicate efficiently in gorillas. Adaptation to chimpanzees and gorillas probably made it easier for successful transmission of both SIVcpz and SIVgor to humans. Both SIVcpz and SIVgor Vif can effectively antagonize human APOBEC3G, F, and D proteins (Etienne et al., 2013; Zhang et al., 2017). SIVcpz and SIVgor Nef proteins cannot antagonize human BST2 function due to the deletions of the cytoplasmic domain (Jia et al., 2009; Sauter et al., 2009; Zhang et al., 2009). However, Vpu from pandemic HIV-1 M strains can counteract human BST2 (Sauter et al., 2009). Interestingly, only a few changes in the transmembrane domain of SIVcpz Vpu result in the ability to antagonize BST2 (Lim et al., 2010; Vigan and Neil, 2010; Kluge et al., 2013). Ability to overcome these restriction factors probably helped HIV-1 adapt to humans.
CST of SIVsmm from sooty mangabeys to humans occurred on nine independent occasions and gave rise to HIV-2 groups A-I (Hirsch et al., 1989; Gao et al., 1992; Chen et al., 1996; Ayouba et al., 2013). This jumping of SIV from monkeys to chimpanzees and then to humans has provided an excellent opportunity to understand the events and adaptations that are required for CST. SIVsmm adaptation to humans may have been easier as these viruses can replicate efficiently in human PBMCs (Gautam et al., 2007). SIVsmm Vif can counteract APOBEC3G from many species including human APOBEC3G (Letko et al., 2013). Interestingly, SIVsmm uses both Nef and Env to counteract BST2 in its natural hosts, and Env protein to antagonize human BST2 (Heusinger et al., 2018). This ability to antagonize human BST2 may have facilitated zoonotic transmission of SIVsmm to human. Another advantage for SIVsmm is that its Vpx can counteract human SAMHD1 and HUSH complex (Laguette et al., 2012; Chougui et al., 2018). Furthermore, SIVsmm Nef can antagonize human SERINC5 (Heigele et al., 2016). This ability of SIVsmm accessory proteins to overcome the function of human restriction factors may have facilitated the zoonotic transmission of SIVsmm to humans. However, HIV-2 strains may not have adapted very well for replication in human hosts. HIV-2 strains show higher A3G/F induced hyper mutations compared to HIV-1 (Bertine et al., 2015), suggesting inefficient degradation of these restriction factor by the HIV-2 Vif protein. Similarly, HIV-2 capsid is more susceptible to inhibition by human TRIM5α (Ylinen et al., 2005; Takeuchi et al., 2013). HIV-2 is also less pathogenic in humans compared to HIV-1. In most infected individuals, HIV-2 viral loads are controlled and results in slow disease progression (Martinez-Steele et al., 2007; Nyamweya et al., 2013).
Overall, these studies demonstrate that adaptation to the human host requires the ability of these viruses to counteract interferon-inducible restriction factors and the ability to exploit cellular dependency factors for virus replication.
Adaptation of Rationally Modified HIV-1 to Macaque Species
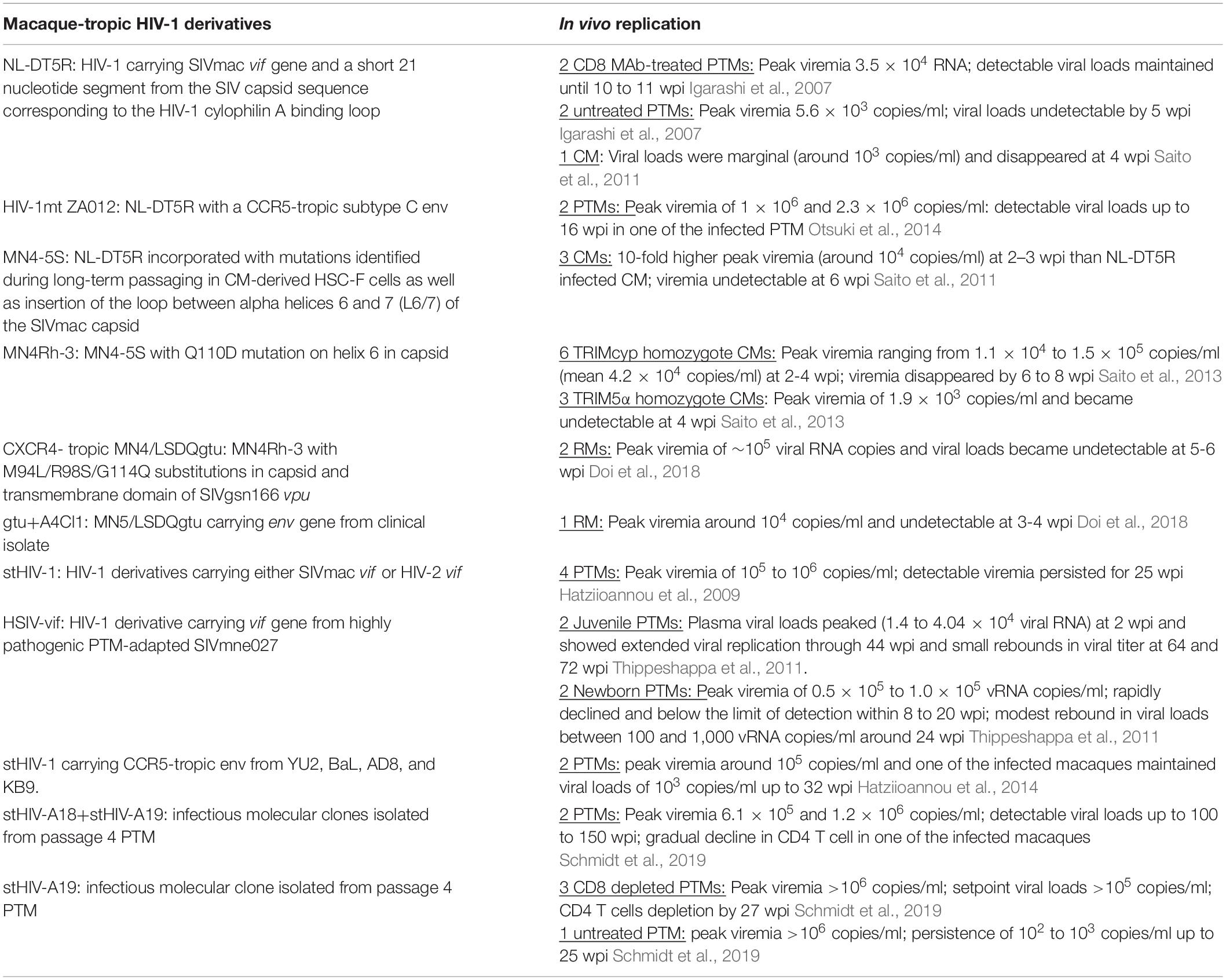
The counter measures used by primate lentiviruses have guided the rational modification of HIV-1 for replication in macaque species. These rationally modified HIV-1 with SIV gene substitutions are designated macaque-tropic HIV-1 (mtHIV-1) or simian-tropic HIV-1 (stHIV-1) or human-simian immunodeficiency virus HSIV (listed in Table 1). Since, HIV-1 cannot overcome RM TRIM5α and APOBEC3 family of restriction factors, a simian-tropic HIV-1 (stHIV-1) was initially developed by incorporating capsid and vif sequences from SIVmac239 (Hatziioannou et al., 2006). stHIV-1, whose genome is 88% HIV-1 derived, replicated robustly in a RM T-cell line and RM PBMCs after in vitro adaptation (Hatziioannou et al., 2006). This suggest that avoidance of capsid- and Vif-based restriction may be sufficient to allow cross-species transmission of HIV-1 to rhesus macaques. However, the replication efficiency of stHIV-1 in vivo is unknown.
To minimize the sequences from SIV, a variant HIV-1 which carries only the SIVmac vif gene and a short 21 nucleotide segment from the SIV capsid sequence corresponding to the HIV-1 cylophilin A binding loop has been constructed (Kamada et al., 2006). Long-term passaging of this clone in a CM lymphoid cell line resulted in an in vitro adapted HIV-1 derivative (NL-DT5R), which replicated well in the CM T-cell line (HSC-F) as well as CD8+ T-cells depleted T-cells from five of five PTMs and one of three RMs. To assess replicative and disease-inducing properties in vivo, 4 PTMs were inoculated intravenously with 1.9 × 106 TCID50 of NL-DT5R virus generated from CD8 + T-cell-depleted pig-tailed macaque PBMC. Two of the PTMs were treated with anti-human CD8 monoclonal antibody (MAb) cM-T807 subcutaneously on day 1 (10 mg/kg of body weight), and intravenously on days 4, and 7 (5 mg/kg of body weight) post-infection. HIV-1 NL-DT5R established productive infections in all four animals with no substantial difference in the levels of peak viremia (5.6 × 103 to 3.5 × 104 RNA copies/ml) in the untreated and anti-CD8 MAb-treated monkeys. However, plasma viremia became undetectable by week 5 post-infection in the two untreated macaques, whereas viremia was maintained until weeks 10 to 11 in the two treated animals. Although NL-DT5R established a productive infection and elicited humoral responses against all of the HIV-1 structural proteins in PTMs, it did not cause CD4+ T cells depletion or disease (Igarashi et al., 2007). To further adapt NL-DT5R to PTMs, an additional macaque was inoculated intravenously with virus inoculum containing lymph node cells collected from each of the 4 monkeys (7.5 × 107 cells) suspended in 20 ml of pooled whole blood. This animal was also transiently depleted of CD8 T cells by treating with the anti-CD8 MAb at the same doses and routes as two of the monkeys in the initial infection. The plasma viral loads in this PTM peaked (1.9 × 104 RNA copies/ml) at week 2.4 post-infection and then rapidly declined, becoming undetectable at week 6 post-infection (Igarashi et al., 2007). A new macaque-tropic HIV-1 (named HIV-1mt ZA012) carrying env from a CCR5 tropic subtype C HIV-1 clinical isolate (HIV-1 97ZA012) in the back bone of NL-DT5R was generated by intracellular homologous recombination (Otsuki et al., 2014). To improve the replication competence, HIV-1mt ZA012 was serially passaged in PTM PBMCs. Virus supernatant from passage 19 replicated better than NL-DT5R and HIV-1mt ZA012-P0 in CD8 T cell depleted PTM PBMCs. To study the in vivo replication capacity, two PTMs were inoculated intravenously with passage 19 virus grown in PTM PBMCs. PTM1 showed peak viremia of 1 × 106 copies/ml at week 2 post-infection and became undetectable by 8-week post-infection (wpi). PTM2 exhibited a peak viremia of 2.3 × 106 copies/ml at 1.5 wpi, maintained viral loads of 104 copies/ml, became undetectable at 16 wpi (Otsuki et al., 2014).
In vivo replication and disease-causing potential of NL-DT5R has also been studied in CMs. NL-DT5R established infection in CMs. However, viral loads were marginal and disappeared by week 4 post-infection (Saito et al., 2011). In order to improve the replication capability of NL-DT5R in CM, long-term passaging in CM-derived HSC-F cells were conducted. Additionally, NL-DT562 having CCR5-tropic env gene on a background of NL-DT5R was also passaged long-term in HSC-F cells. Long-term passaging improved the replication potential of both CXCR4 and CCR5 tropic NL-DT5R and resulted in a total of 14 mutations (10 in the NL-DT5R-derived clone and 4 in the NL-DT562-derived clone). These mutations were introduced into the parental NL-DT5R clone to generate a clone named MN4-5 (Saito et al., 2011). Previously, it was found that insertion of an SIVmac loop between alpha helices 6 and 7 (L6/7) of capsid into the corresponding region in HIV-1 significantly enhanced the NL-DT5R replication in HSC-F cells and PBMCs of CM by relieving the inhibitory effect of TRIM5α (Kuroishi et al., 2009). Therefore, A modified MN4-5 clone (named MN4-5S) was generated by inserting the loop between alpha helices 6 and 7 (L6/7) of the SIVmac capsid into the corresponding region in HIV-1 (Saito et al., 2011). MN4-5S showed enhanced replication compared to the parental NL-DT5R in CM-derived HSC-F cells and CD8+ T-cells depleted PBMCs from CMs. In intravenously (IV) inoculated CMs, MN4-5S resulted in 10-fold higher peak viremia at 2-3 wpi compared to NL-DT5R infected CMs. However, the viremia became undetectable at 6 wpi, partly due to control by CD8+ T-cells as in vivo depletion of CD8 + cells resulted in the reappearance of viremia (Saito et al., 2011).
MN4-5S has been further adapted in macaque cells by passaging and an adaptive mutation in capsid that enhances growth ability in the cells has been identified (Nomaguchi et al., 2013b). In silico structural modeling predicted that Q110D mutation on helix 6 in capsid (CA-Q110D) would promote viral replication in macaque cells. Therefore, a proviral clone carrying CA-Q110D, designated MN4Rh-3, was constructed. Indeed, MN4Rh-3 exhibited marked enhancement of growth potential in macaque cells relative to other mtHIV-1clones that have been constructed. Interestingly, the CA-Q110D mutation did not contribute to enhancement of further resistance to TRIMCyp or evasion from TRIM5α restriction (Nomaguchi et al., 2013b). To investigate whether TRIM5 genotypes could influence the growth of MN4Rh-3 in vivo, viral stocks propagated in CD8+ cell-depleted PBMCs were inoculated intravenously into TRIMCyp homozygotes (n = 6) or TRIM5α homozygotes (n = 3) (Saito et al., 2013). MN4Rh-3 replicated readily in all TRIMCyp homozygotes, with plasma viral loads reaching a peak at 2–4 weeks post-inoculation and ranging from 1.1 × 104 to 1.5 × 105 copies/ml (mean 4.2 × 104 copies/ml). In contrast, MN4Rh-3 replicated poorly in TRIM5α homozygotes (mean peak viremia 1.9 × 103 copies/ml) (Saito et al., 2013). As expected, HIV-1-specific antibodies were detected in the TRIMCyp homozygotes but minimally in TRIM5α homozygotes suggesting that the strength of antibody response reflected the level of virus replication (Saito et al., 2013). To adapt MN4Rh-3 to RMs, gag and vpu were altered to overcome TRIM5α and BST2 function (Nomaguchi et al., 2013a). Using sequence- and structure-guided mutagenesis, three amino acid substitutions in capsid (M94L/R98S/G114Q) were introduced to overcome TRIM5α susceptibility. Additionally, transmembrane domain of vpu was replaced with the corresponding region of simian immunodeficiency virus SIVgsn166 vpu. The resultant clone, designated MN4/LSDQgtu, antagonized macaque but not human BST2, and replicated efficiently in a macaque cell line. Notably, MN4/LSDQgtu grew comparably to SIVmac239 and much better than other mtHIV-1clones in RM PBMCs (Nomaguchi et al., 2013a). A CCR5-tropic version of MN4/LSDQgtu carrying HIV-1 SF162 env, designated MN5/LSDQgtu (or 5gtu) has also been constructed. However, MN5/LSDQgtu replicated poorly compared to MN4/LSDQgtu in RM cell line (Doi et al., 2013). Additional CCR5-tropic clones carrying pSHIVAD8–EH or env clones from clinical isolates have been generated in the backbone of MN5/LSDQgtu (Doi et al., 2017). Interestingly, two of the clones carrying env genes from clinical isolates, designated gtu + Cl1 and gtu + A4Cl1, grew better than the parental clone MN5/LSDQgtu (or 5gtu) in RM M1.3S cells. Furthermore, gtu+A4Cl1 grew comparably well with MN4/LSDQgtu in PBMCs isolated from two different donor RMs (Doi et al., 2017). To determine the replication potential in vivo, two RMs were challenged with CXCR4- tropic MN4/LSDQgtu and one RM with CCR5-tropic gtu+A4Cl1 (Doi et al., 2018). Although both viruses established infection in RMs, MN4/LSDQgtu replicated better with peak viremia of ∼105 viral RNA copies compared to 104 copies/ml for gtu+A4Cl1. However, virus replication was transient and became undetectable at 5–6 wpi (Doi et al., 2018).
Adaptation of Minimally Modified HIV-1 to Ptms
Among non-human primates, PTMs are known to be uniquely susceptible to HIV-1 infection (Agy et al., 1992; Frumkin et al., 1993; Gartner et al., 1994a, b; Agy et al., 1997; Bosch et al., 1997; Bosch et al., 2000). Agy et al. (1992) first showed that PTMs can be infected with HIV-1. All the eight infected animals experienced sustained seroconversion to a broad range of HIV-1 proteins. Furthermore, virus could be recovered from the infected macaque PBMCs by co-cultivation and proviral sequences could be detected in DNA isolated from PBMCs. However, cell free virus was detected in the plasma of only one infected macaque (Agy et al., 1992). To accelerate adaptation of HIV-1 to PTMs, blood from infected macaques was serially transfused into three groups of naive macaques. At three to 5 weeks after transfusion, plasma viral loads from several macaques in the first two groups exceeded those of the initially inoculated macaques. Unexpectedly, animals in the third group had diminished RNA levels, virus culture negative, and did not seroconvert. It was later found out that the blood used for transfusion was virus-culture negative (Agy et al., 1997).
In another study, four PTMs were inoculated with autologous cells expressing low amounts of HIV-1 (Gartner et al., 1994a). Infectious virus could be recovered from PBMCs and lymph nodes up to 10 wpi in 3 out of 4 infected macaques. Further, HIV-1 DNA was frequently detected in uncultured PBMCs from all three animals. In one of the infected animals, virus could be re-isolated at 38- and 61-weeks post-infection, suggesting that the animal was persistently infected with HIV-1. Interestingly, in vivo passaging of the virus at week 6 post-infection did not select for pathogenic variants. One PTM and one CM that received transfusion of virus-positive blood and lymph node cells failed to become detectably infected (Gartner et al., 1994b). Attempts have also been made to adapt HIV-1 to newborn PTMs. In the case of neonate PTMs, three out of five rectally exposed and two of two intravenously inoculated macaques became infected with HIV-1. However, none of the four orally exposed animals showed evidence of HIV-1 infection. Although HIV-1 replicated more vigorously in newborns, passaging of HIV-1 in newborn PTMs did not result in the emergence of pathogenic variants capable of causing CD4 depletion (Bosch et al., 1997; Bosch et al., 2000). However, the long-term presence of HIV-1-specific antibodies, proviral sequences, and the recovery of infectious virus in these studies indicate the unique susceptibility of PTMs to HIV-1 infection.
We have also observed that PTM PBMCs can be more easily transduced with VSVG pseudotyped HIV-1 than RM PBMCs, suggesting the absence of a post-entry block (Thippeshappa et al., 2011). Several groups have observed the absence of the retroviral restriction factor, TRIM5α, in this macaque species. Moreover, novel isoforms of TRIM5 [TRIM5θ, which lacks B30.2 (SPRY) domain and TRIM5η, which has a deletion of the entire exon 7] expressed by PTMs do not restrict HIV-1 infection (Brennan et al., 2007). Interestingly, PTMs express a TRIM5-cyclophilin A fusion protein (TRIMcyp) due to LINE-mediated retrotransposition of the cyclophilin A cDNA into the untranslated region of exon 8 of the TRIM5 locus (Liao et al., 2007; Brennan et al., 2008; Newman et al., 2008; Virgen et al., 2008). However, unlike OWM TRIMcyp, the PTM TRIMcyp does not restrict HIV-1 infection (Liao et al., 2007; Brennan et al., 2008; Newman et al., 2008; Virgen et al., 2008).
Absence of TRIM5α presents an advantage for the development of a minimally modified HIV-1 that can potentially infect and cause AIDS in PTMs. Since Vif expressed by SIVmac and HIV-2 can degrade RM APOBEC3G, Hatziioannou et al. (2009) constructed HIV-1 derivatives carrying either SIVmac vif or HIV-2 vif in place of HIV-1 vif. Intravenous (IV) Inoculation of PTMs with an admixture of these two viruses resulted in acute infection, and viremia persisted for 25 wpi. However, infection was controlled thereafter and it did not result in CD4+T-cell depletion. We also constructed an Human-Simian Immunodeficiency Virus, named HSIV-vifNL4–3 by substituting pNL4-3 vif with vif gene from highly pathogenic PTM-adapted SIVmne027 (Kimata et al., 1998; Kimata et al., 1999). IV inoculation of PTMs with HSIV-vifNL4–3 virus, generated from transfecting 293T cells, extended viral replication through 44 wpi and small rebounds in viral titer at 64 and 72 wpi in juvenile PTMs (Thippeshappa et al., 2011). Furthermore, viral DNA could be detected in PBMCs upto 92 wpi, suggesting that the animals were persistently infected for nearly 2 years (Thippeshappa et al., 2011). Hatziannou et al. conducted animal-to-animal transfer to generate pathogenic variants [discussed in Kimata (2014)]. Passage 1 PTMs were IV inoculated with an inoculum containing four clonal HIV-1NL4–3–derived viruses, each encoding a gp120 Env protein from a prototype HIV-1 strain that uses the CCR5 co-receptor (YU2, BaL, AD8, and KB9). Passage 2 to 4 PTMs were transiently depleted of their CD8 T-cells at the time of inoculation. The resulting virus from passage 4 only caused CD4 depletion in animals transiently depleted of CD8 T cells. However, immunocompetent macaques controlled the viral loads (Hatziioannou et al., 2014). Interestingly, HIV-1 Vpu acquired mutations during in vivo adaptation to antagonize PTM BST2. Furthermore, in vivo adaptation also led to changes in HIV Env that improved its ability to bind macaque CD4 (Hatziioannou et al., 2014). Recently, they also reported acquisition of amino acid changes in capsid that conferred partial resistance to PTM MX2 resistance factor (Schmidt et al., 2019). To recapitulate the phenotype observed with viral swarm from the blood of passage 4 animal, the group of Hatziioannou also generated several IMCs. One of the clones, named stHIV-A19, caused CD4 depletion only in macaques that were transiently depleted of CD8 T cells. However, it was controlled in immunocompetent PTMs (Schmidt et al., 2019). We also conducted animal-to-animal transfer of infected blood in 3 immunocompetent PTMs. Our initial inoculum contained a mixture of transfection supernatants of HSIV-vifNL4–3, HSIV-vifAD8, and HSIV-vifYU2, and virus recovered from co-culture of PBMCs isolated from previously infected macaque and naïve CD4 T cells. However, the viral loads remained controlled in all 3 macaques (unpublished data).
Possible Role of Interferon Response in Control of Macaque-Tropic HIV-1 Infection
The reasons for virologic control in the immunocompetent PTMs remain unclear. CD8+ T-cell depletion studies suggest that cellular immune responses may be limiting replication of the macaque-tropic HIV-1 clones (Hatziioannou et al., 2009). Additionally, the Type 1 IFN response induced during acute infection might restrict viral replication to a level that may prevent establishment of infection to achieve high peak viremia and set point viral loads. Indeed, IFNs are upregulated during HIV-1 and SIV infections (Bosinger et al., 2009; Jacquelin et al., 2009; Stacey et al., 2009; Sandler et al., 2014). Induction of IFNα results in the expression of many IFN-stimulated genes (ISGs) and the establishment of an antiviral state in the cell. Significantly, retroviral restriction factors (i.e. APOBEC3 family proteins, TRIM5α, BST2, and SAMHD1) are upregulated by IFN, linking restriction to the innate immune response [reviewed in Thippeshappa et al. (2012); Misra et al. (2013)]. Furthermore, IFN response also induces the expression of several resistance factors such as, myxovirus resistance 2 (MX2), IFN-induced transmembrane (IFITM) proteins, schlafen 11 (SLFN11), and other yet to be identified restriction factors that inhibit HIV-1 replication [reviewed in Doyle et al. (2015)]. Thus, it is possible that the IFN response during acute infection in PTMs restricts HIV-1 replication to a level that is not sufficient for adaptive mutations to occur. Therefore, Type 1 IFN response induced during acute infection suggests that these PTM-tropic HSIV-vif viruses should overcome the effect of restrictive ISGs in order to replicate to high levels and cause disease. We have previously demonstrated that the prototype PTM-tropic HSIV-vifNL4–3 is inhibited by IFNα in PTM cells. However, pathogenic SIVmne and SIVmac clones resist IFNα-induced inhibition (Bitzegeio et al., 2013; Thippeshappa et al., 2013). Interestingly, we have identified a HSIV-vif derivative with YU2 Env that resists IFNα treatment in PTM CD4+ T cells. Using chimeric viruses between HSIV-vifNL4–3 and HSIV-vifYU2, we demonstrated that YU2 Env is the determinant that contributes to IFN-resistance. We also demonstrated, using Vpr-beta lactamase fusion assay, that HSIV-vifYU2 overcomes IFN-induced restrictions at the entry step of the virus life cycle (Thippeshappa et al., 2013). However, further experiments need to be conducted to identify the IFN-induced restriction factors at the virion fusion step that restrict HSIV-vifNL4–3 but not HSIV-vifYU2.
Since many of the retroviral viral restriction factors are upregulated in the presence of IFN, it will be critical for the virus to overcome IFN responses to establish productive infection. Indeed, Transmitted/Founder (T/F) viruses have been shown to be IFN-resistant (Fenton-May et al., 2013; Iyer et al., 2017). Furthermore, adapting SHIVs to rhesus macaques (RMs) selects for Env-mediated IFNα-resistance (Boyd et al., 2016). Additionally, inhibition of the IFN-response by administration of a IFNα receptor antagonist has been shown to result in high viral loads during acute infection and faster progression to AIDS in a pathogenic SIV-RM model (Sandler et al., 2014). Thus, inoculating PTMs with IFN-resistant HSIV-vif may help to overcome the IFN response induced during acute infection leading to higher peak viremia. We have identified a variant PTM-tropic HSIV-vifYU2 that resists IFNα-treatment in both human PBMCs and PTM CD4 T cells. Additionally, Vpx is essential for replication of SIV in macaques (Belshan et al., 2012; Shingai et al., 2015) and it enables the replication of SIV in non-dividing cells by overcoming SAMHD1 function (Hrecka et al., 2011; Laguette et al., 2011). SIV Nef has also been shown to inhibit the effects of macaque BST2 (Jia et al., 2009; Zhang et al., 2009). Therefore, additional modifications to the HSIV-vifYU2 viral genome to overcome BST2-mediated and SAMHD1-mediated restriction may be required to establish persistent viremia in vivo. First generation SHIV constructs replicated poorly in macaques although long-term persistence was observed. Thus, serial in vivo passages were conducted to enhance the infectivity or replicative capacity of several SHIV strains (Luciw et al., 1995; Joag et al., 1996; Reimann et al., 1996; Igarashi et al., 1999; Chen et al., 2000; Song et al., 2006). We anticipate that serial in vivo passaging of IFNα-resistant HSIV-vifYU2 or its derivatives carrying SIV nef or vpx genes will generate pathogenic variants with enhanced infectivity. However, a consequence of adapation to restriction factors may be fitness cost. Interestingly, a molecular clone with adapted capsid that showed complete resistance to PTM MX2 exhibited impaired replication capacity (Schmidt et al., 2019). This suggests that complete resistance to certain restriction factors may incur fitness defect to the virus. Therefore, adaptation to a new species may require acquisition of mutations to overcome restriction factors without incurring replication fitness cost.
Conclusion
Inability of passaged viruses to cause AIDS in non-CD8 depleted macaques suggest that more work is required to develop a bon-a-fide macaque-model of HIV-1 infection. Overcoming initial IFN responses induced during acute infection may enable efficient replication of HSIV-vif in PTM host. Thus, we hypothesize that successful CST of HIV-1 to PTMs depends on inhibiting and evading IFN-induced restriction factors and that appropriate modifications to the genome will enable HIV-1 replication in the PTM host. We believe that infection of PTMs with IFN-resistant variants could provide insight into whether evasion of IFNα response is critical for viral replication in the host. Thus, IFN-resistant HSIV-vif viruses will be an excellent starting point for adaptation to PTMs and eventual development of macaque model of HIV-1 infection. Such an animal model would be extremely valuable for preclinical evaluation of novel vaccines and therapeutics, as these HSIV-vif clones have all the HIV immunologic and vaccine targets such as Gag, Env, Tat, Rev, and Nef. This is the drawback with SIV and SHIV models which are not ideal for testing vaccine approaches targeting HIV Gag and Nef antigens. Furthermore, establishment of HIV reservoirs in this model also provides an avenue for developing therapeutic vaccination approaches targeting HIV Gag and Env, apart from testing latency reversal agents. Once these models are established, they would also positively inform the process of refining models of HIV co-infections and co-morbidities, such as the Mtb/HIV co-infection model, which until now has relied on the use of SIV as a co-infecting agent in either rhesus (Mehra et al., 2011; Foreman et al., 2016; Bucsan et al., 2019) or cynomolgus macaques (Diedrich et al., 2010).
Author Contributions
RT wrote the manuscript, while JK and DK provided guidance, technical support, inputs, and edited the manuscript.
Funding
The authors acknowledge funding support from the NIH grants AI111943 and AI127043 to DK and AI116167 to JK as well as institutional grant OD011133.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
Aghokeng, A. F., Ayouba, A., Mpoudi-Ngole, E., Loul, S., Liegeois, F., Delaporte, E., et al. (2010). Extensive survey on the prevalence and genetic diversity of SIVs in primate bushmeat provides insights into risks for potential new cross-species transmissions. Infect. Genet. Evol. 10, 386–396. doi: 10.1016/j.meegid.2009.04.014
Agy, M. B., Frumkin, L. R., Corey, L., Coombs, R. W., Wolinsky, S. M., Koehler, J., et al. (1992). Infection of Macaca nemestrina by human immunodeficiency virus type-1. Science 257, 103–106. doi: 10.1006/viro.1993.1392
Agy, M. B., Schmidt, A., Florey, M. J., Kennedy, B. J., Schaefer, G., Katze, M. G., et al. (1997). Serial in vivo passage of HIV-1 infection in Macaca nemestrina. Virology 238, 336–343. doi: 10.1006/viro.1997.8832
Akari, H., Sakuragi, J., Takebe, Y., Tomonaga, K., Kawamura, M., Fukasawa, M., et al. (1992). Biological characterization of human immunodeficiency virus type 1 and type 2 mutants in human peripheral blood mononuclear cells. Arch. Virol. 123, 157–167. doi: 10.1007/bf01317146
Apetrei, C., Robertson, D. L., and Marx, P. A. (2004). The history of SIVS and AIDS: epidemiology, phylogeny and biology of isolates from naturally SIV infected non-human primates (NHP) in Africa. Front. Biosci. 9, 225–254. doi: 10.2741/1154
Ayouba, A., Akoua-Koffi, C., Calvignac-Spencer, S., Esteban, A., Locatelli, S., Li, H., et al. (2013). Evidence for continuing cross-species transmission of SIVsmm to humans: characterization of a new HIV-2 lineage in rural Cote d’Ivoire. AIDS 27, 2488–2491. doi: 10.1097/01.aids.0000432443.22684.50
Bailes, E., Gao, F., Bibollet-Ruche, F., Courgnaud, V., Peeters, M., Marx, P. A., et al. (2003). Hybrid origin of SIV in chimpanzees. Science 300:1713. doi: 10.1126/science.1080657
Bailey, C. C., Kondur, H. R., Huang, I. C., and Farzan, M. (2013). Interferon-induced transmembrane protein 3 is a type II transmembrane protein. J. Biol. Chem. 288, 32184–32193. doi: 10.1074/jbc.M113.514356
Baldauf, H. M., Pan, X., Erikson, E., Schmidt, S., Daddacha, W., Burggraf, M., et al. (2012). SAMHD1 restricts HIV-1 infection in resting CD4(+) T cells. Nat. Med. 18, 1682–1687. doi: 10.1038/nm.2964
Baldauf, H. M., Stegmann, L., Schwarz, S. M., Ambiel, I., Trotard, M., Martin, M., et al. (2017). Vpx overcomes a SAMHD1-independent block to HIV reverse transcription that is specific to resting CD4 T cells. Proc. Natl. Acad. Sci. U.S.A. 114, 2729–2734. doi: 10.1073/pnas.1613635114
Bell, S. M., and Bedford, T. (2017). Modern-day SIV viral diversity generated by extensive recombination and cross-species transmission. PLoS Pathog. 13:e1006466. doi: 10.1371/journal.ppat.1006466
Belshan, M., Kimata, J. T., Brown, C., Cheng, X., McCulley, A., Larsen, A., et al. (2012). Vpx is Critical for SIVmne infection of pigtail macaques. Retrovirology 9:32. doi: 10.1186/1742-4690-9-32
Bertine, M., Charpentier, C., Visseaux, B., Storto, A., Collin, G., Larrouy, L., et al. (2015). High level of APOBEC3F/3G editing in HIV-2 DNA vif and pol sequences from antiretroviral-naive patients. AIDS 29, 779–784. doi: 10.1097/QAD.0000000000000607
Bitzegeio, J., Sampias, M., Bieniasz, P. D., and Hatziioannou, T. (2013). Adaptation to the interferon-induced antiviral state by human and simian immunodeficiency viruses. J. Virol. 87, 3549–3560. doi: 10.1128/JVI.03219-12
Bogerd, H. P., Doehle, B. P., Wiegand, H. L., and Cullen, B. R. (2004). A single amino acid difference in the host APOBEC3G protein controls the primate species specificity of HIV type 1 virion infectivity factor. Proc. Natl. Acad. Sci. U.S.A. 101, 3770–3774. doi: 10.1073/pnas.0307713101
Bosch, M. L., Schmidt, A., Agy, M. B., Kimball, L. E., and Morton, W. R. (1997). Infection of Macaca nemestrina neonates with HIV-1 via different routes of inoculation. AIDS 11, 1555–1563. doi: 10.1097/00002030-199713000-00003
Bosch, M. L., Schmidt, A., Chen, J., Florey, M. J., Agy, M., and Morton, W. R. (2000). Enhanced replication of HIV-1 in vivo in pigtailed macaques (Macaca nemestrina). J. Med. Primatol. 29, 107–113. doi: 10.1034/j.1600-0684.2000.290303.x
Bosinger, S. E., Li, Q., Gordon, S. N., Klatt, N. R., Duan, L., Xu, L., et al. (2009). Global genomic analysis reveals rapid control of a robust innate response in SIV-infected sooty mangabeys. J. Clin. Invest. 119, 3556–3572. doi: 10.1172/JCI40115
Boyd, D. F., Sharma, A., Humes, D., Cheng-Mayer, C., and Overbaugh, J. (2016). Adapting SHIVs in vivo selects for envelope-mediated interferon-alpha resistance. PLoS Pathog. 12:e1005727. doi: 10.1371/journal.ppat.1005727
Brennan, G., Kozyrev, Y., and Hu, S. L. (2008). TRIMCyp expression in Old World primates Macaca nemestrina and Macaca fascicularis. Proc. Natl. Acad. Sci. U.S.A. 105, 3569–3574. doi: 10.1073/pnas.0709511105
Brennan, G., Kozyrev, Y., Kodama, T., and Hu, S. L. (2007). Novel TRIM5 isoforms expressed by Macaca nemestrina. J. Virol. 81, 12210–12217. doi: 10.1128/JVI.02499-06
Bucsan, A. N., Chatterjee, A., Singh, D. K., Foreman, T. W., Lee, T. H., Threeton, B., et al. (2019). Mechanisms of reactivation of latent tuberculosis infection due to SIV coinfection. J. Clin. Invest. 129, 5254–5260. doi: 10.1172/JCI125810
Chande, A., Cuccurullo, E. C., Rosa, A., Ziglio, S., Carpenter, S., and Pizzato, M. (2016). S2 from equine infectious anemia virus is an infectivity factor which counteracts the retroviral inhibitors SERINC5 and SERINC3. Proc. Natl. Acad. Sci. U.S.A. 113, 13197–13202. doi: 10.1073/pnas.1612044113
Chen, Z., Huang, Y., Zhao, X., Skulsky, E., Lin, D., Ip, J., et al. (2000). Enhanced infectivity of an R5-tropic simian/human immunodeficiency virus carrying human immunodeficiency virus type 1 subtype C envelope after serial passages in pig-tailed macaques (Macaca nemestrina). J. Virol. 74, 6501–6510. doi: 10.1128/jvi.74.14.6501-6510.2000
Chen, Z., Telfier, P., Gettie, A., Reed, P., Zhang, L., Ho, D. D., et al. (1996). Genetic characterization of new West African simian immunodeficiency virus SIVsm: geographic clustering of household-derived SIV strains with human immunodeficiency virus type 2 subtypes and genetically diverse viruses from a single feral sooty mangabey troop. J. Virol. 70, 3617–3627.
Cheney, K. M., and McKnight, A. (2010). Interferon-alpha mediates restriction of human immunodeficiency virus type-1 replication in primary human macrophages at an early stage of replication. PLoS One 5:e13521. doi: 10.1371/journal.pone.0013521
Chougui, G., Munir-Matloob, S., Matkovic, R., Martin, M. M., Morel, M., Lahouassa, H., et al. (2018). HIV-2/SIV viral protein X counteracts HUSH repressor complex. Nat. Microbiol. 3, 891–897. doi: 10.1038/s41564-018-0179-6
Compton, A. A., Bruel, T., Porrot, F., Mallet, A., Sachse, M., Euvrard, M., et al. (2014). IFITM proteins incorporated into HIV-1 virions impair viral fusion and spread. Cell Host Microbe 16, 736–747. doi: 10.1016/j.chom.2014.11.001
D’Arc, M., Ayouba, A., Esteban, A., Learn, G. H., Boue, V., Liegeois, F., et al. (2015). Origin of the HIV-1 group O epidemic in western lowland gorillas. Proc. Natl. Acad. Sci. U.S.A. 112, E1343–E1352. doi: 10.1073/pnas.1502022112
Dejucq, N., Simmons, G., and Clapham, P. R. (2000). T-cell line adaptation of human immunodeficiency virus type 1 strain SF162: effects on envelope, vpu and macrophage-tropism. J. Gen. Virol. 81(Pt 12), 2899–2904. doi: 10.1099/0022-1317-81-12-2899
Desai, T. M., Marin, M., Chin, C. R., Savidis, G., Brass, A. L., and Melikyan, G. B. (2014). IFITM3 restricts influenza A virus entry by blocking the formation of fusion pores following virus-endosome hemifusion. PLoS Pathog. 10:e1004048. doi: 10.1371/journal.ppat.1004048
Descours, B., Cribier, A., Chable-Bessia, C., Ayinde, D., Rice, G., Crow, Y., et al. (2012). SAMHD1 restricts HIV-1 reverse transcription in quiescent CD4(+) T-cells. Retrovirology 9:87. doi: 10.1186/1742-4690-9-87
Diedrich, C. R., Mattila, J. T., Klein, E., Janssen, C., Phuah, J., Sturgeon, T. J., et al. (2010). Reactivation of latent tuberculosis in cynomolgus macaques infected with SIV is associated with early peripheral T cell depletion and not virus load. PLoS One 5:e9611. doi: 10.1371/journal.pone.0009611
Dietrich, E. A., Brennan, G., Ferguson, B., Wiseman, R. W., O’Connor, D., and Hu, S. L. (2011). Variable prevalence and functional diversity of the antiretroviral restriction factor TRIMCyp in Macaca fascicularis. J. Virol. 85, 9956–9963. doi: 10.1128/JVI.00097-11
Doi, N., Miura, T., Mori, H., Sakawaki, H., Koma, T., Adachi, A., et al. (2018). CXCR4- and CCR5-tropic HIV-1 clones are both tractable to grow in Rhesus Macaques. Front. Microbiol. 9:2510. doi: 10.3389/fmicb.2018.02510
Doi, N., Okubo, A., Yamane, M., Sakai, Y., Adachi, A., and Nomaguchi, M. (2013). Growth potentials of CCR5-tropic/CXCR4-tropic HIV-1mt clones in macaque cells. Front. Microbiol. 4:218. doi: 10.3389/fmicb.2013.00218
Doi, N., Sakai, Y., Adachi, A., and Nomaguchi, M. (2017). Generation and characterization of new CCR5-tropic HIV-1rmt clones. J. Med. Invest. 64, 272–279. doi: 10.2152/jmi.64.272
Doyle, T., Goujon, C., and Malim, M. H. (2015). HIV-1 and interferons: who’s interfering with whom? Nat. Rev. Microbiol. 13, 403–413. doi: 10.1038/nrmicro3449
Etienne, L., Hahn, B. H., Sharp, P. M., Matsen, F. A., and Emerman, M. (2013). Gene loss and adaptation to hominids underlie the ancient origin of HIV-1. Cell Host Microbe 14, 85–92. doi: 10.1016/j.chom.2013.06.002
Fenton-May, A. E., Dibben, O., Emmerich, T., Ding, H., Pfafferott, K., Aasa-Chapman, M. M., et al. (2013). Relative resistance of HIV-1 founder viruses to control by interferon-alpha. Retrovirology 10:146. doi: 10.1186/1742-4690-10-146
Foreman, T. W., Mehra, S., LoBato, D. N., Malek, A., Alvarez, X., Golden, N. A., et al. (2016). CD4+ T-cell-independent mechanisms suppress reactivation of latent tuberculosis in a macaque model of HIV coinfection. Proc. Natl. Acad. Sci. U.S.A. 113, E5636–E5644. doi: 10.1073/pnas.1611987113
Fribourgh, J. L., Nguyen, H. C., Matreyek, K. A., Alvarez, F. J. D., Summers, B. J., Dewdney, T. G., et al. (2014). Structural insight into HIV-1 restriction by MxB. Cell Host Microbe 16, 627–638. doi: 10.1016/j.chom.2014.09.021
Fricke, T., White, T. E., Schulte, B., de Souza Aranha, Vieira, D. A., Dharan, A., et al. (2014). MxB binds to the HIV-1 core and prevents the uncoating process of HIV-1. Retrovirology 11:68. doi: 10.1186/s12977-014-0068-x
Frumkin, L. R., Agy, M. B., Coombs, R. W., Panther, L., Morton, W. R., Koehler, J., et al. (1993). Acute infection of Macaca nemestrina by human immunodeficiency virus type 1. Virology 195, 422–431. doi: 10.1126/science.1621083
Gao, F., Bailes, E., Robertson, D. L., Chen, Y., Rodenburg, C. M., Michael, S. F., et al. (1999). Origin of HIV-1 in the chimpanzee Pan troglodytes troglodytes. Nature 397, 436–441. doi: 10.1038/17130
Gao, F., Yue, L., White, A. T., Pappas, P. G., Barchue, J., Hanson, A. P., et al. (1992). Human infection by genetically diverse SIVSM-related HIV-2 in West Africa. Nature 358, 495–499. doi: 10.1038/358495a0
Gartner, S., Liu, Y., Lewis, M. G., Polonis, V., Elkins, W. R., Zack, P. M., et al. (1994a). HIV-1 infection in pigtailed macaques. AIDS Res. Hum. Retroviruses 10(Suppl. 2), S129–S133.
Gartner, S., Liu, Y., Polonis, V., Lewis, M. G., Elkins, W. R., Hunter, E. A., et al. (1994b). Adaptation of HIV-1 to pigtailed macaques. J. Med. Primatol. 23, 155–163.
Gautam, R., Carter, A. C., Katz, N., Butler, I. F., Barnes, M., Hasegawa, A., et al. (2007). In vitro characterization of primary SIVsmm isolates belonging to different lineages. In vitro growth on rhesus macaque cells is not predictive for in vivo replication in rhesus macaques. Virology 362, 257–270. doi: 10.1016/j.virol.2006.12.037
Goffinet, C., Allespach, I., Homann, S., Tervo, H. M., Habermann, A., Rupp, D., et al. (2009). HIV-1 antagonism of CD317 is species specific and involves Vpu-mediated proteasomal degradation of the restriction factor. Cell Host Microbe 5, 285–297. doi: 10.1016/j.chom.2009.01.009
Gomes, B., Goncalves, S., Disalvo, A., Hollmann, A., and Santos, N. C. (2018). Effect of 25-hydroxycholesterol in viral membrane fusion: insights on HIV inhibition. Biochim. Biophys. Acta Biomembr. 1860, 1171–1178. doi: 10.1016/j.bbamem.2018.02.001
Goujon, C., and Malim, M. H. (2010). Characterization of the alpha interferon-induced postentry block to HIV-1 infection in primary human macrophages and T cells. J. Virol. 84, 9254–9266. doi: 10.1128/JVI.00854-10
Goujon, C., Moncorge, O., Bauby, H., Doyle, T., Ward, C. C., Schaller, T., et al. (2013). Human MX2 is an interferon-induced post-entry inhibitor of HIV-1 infection. Nature 502, 559–562. doi: 10.1038/nature12542
Gupta, R. K., Hue, S., Schaller, T., Verschoor, E., Pillay, D., and Towers, G. J. (2009). Mutation of a single residue renders human tetherin resistant to HIV-1 Vpu-mediated depletion. PLoS Pathog. 5:e1000443. doi: 10.1371/journal.ppat.1000443
Guyader, M., Emerman, M., Montagnier, L., and Peden, K. (1989). VPX mutants of HIV-2 are infectious in established cell lines but display a severe defect in peripheral blood lymphocytes. EMBO J. 8, 1169–1175.
Hatziioannou, T., Ambrose, Z., Chung, N. P., Piatak, M. Jr., Yuan, F., Trubey, C. M., et al. (2009). A macaque model of HIV-1 infection. Proc. Natl. Acad. Sci. U.S.A. 106, 4425–4429. doi: 10.1073/pnas.0812587106
Hatziioannou, T., Del Prete, G. Q., Keele, B. F., Estes, J. D., McNatt, M. W., Bitzegeio, J., et al. (2014). HIV-1-induced AIDS in monkeys. Science 344, 1401–1405. doi: 10.1126/science.1250761
Hatziioannou, T., Perez-Caballero, D., Yang, A., Cowan, S., and Bieniasz, P. D. (2004). Retrovirus resistance factors Ref1 and Lv1 are species-specific variants of TRIM5alpha. Proc. Natl. Acad. Sci. U.S.A. 101, 10774–10779. doi: 10.1073/pnas.0402361101
Hatziioannou, T., Princiotta, M., Piatak, M. Jr., Yuan, F., Zhang, F., Lifson, J. D., et al. (2006). Generation of simian-tropic HIV-1 by restriction factor evasion. Science 314:95. doi: 10.1126/science.1130994
Heigele, A., Kmiec, D., Regensburger, K., Langer, S., Peiffer, L., Sturzel, C. M., et al. (2016). The potency of nef-mediated SERINC5 antagonism correlates with the prevalence of primate lentiviruses in the wild. Cell Host Microbe 20, 381–391. doi: 10.1016/j.chom.2016.08.004
Heusinger, E., Deppe, K., Sette, P., Krapp, C., Kmiec, D., Kluge, S. F., et al. (2018). Preadaptation of simian immunodeficiency virus SIVsmm facilitated Env-mediated counteraction of human Tetherin by human immunodeficiency virus type 2. J. Virol. 92:e00276-18. doi: 10.1128/JVI.00276-18
Hirsch, V. M., Olmsted, R. A., Murphey-Corb, M., Purcell, R. H., and Johnson, P. R. (1989). An African primate lentivirus (SIVsm) closely related to HIV-2. Nature 339, 389–392. doi: 10.1038/339389a0
Ho, D. D., Hartshorn, K. L., Rota, T. R., Andrews, C. A., Kaplan, J. C., Schooley, R. T., et al. (1985). Recombinant human interferon alfa-A suppresses HTLV-III replication in vitro. Lancet 1, 602–604. doi: 10.1016/s0140-6736(85)92144-0
Hotter, D., Sauter, D., and Kirchhoff, F. (2017). Guanylate binding protein 5: impairing virion infectivity by targeting retroviral envelope glycoproteins. Small GTPases 8, 31–37. doi: 10.1080/21541248.2016.1189990
Hrecka, K., Hao, C., Gierszewska, M., Swanson, S. K., Kesik-Brodacka, M., Srivastava, S., et al. (2011). Vpx relieves inhibition of HIV-1 infection of macrophages mediated by the SAMHD1 protein. Nature 474, 658–661. doi: 10.1038/nature10195
Igarashi, T., Endo, Y., Englund, G., Sadjadpour, R., Matano, T., Buckler, C., et al. (1999). Emergence of a highly pathogenic simian/human immunodeficiency virus in a rhesus macaque treated with anti-CD8 mAb during a primary infection with a nonpathogenic virus. Proc. Natl. Acad. Sci. U.S.A. 96, 14049–14054. doi: 10.1073/pnas.96.24.14049
Igarashi, T., Iyengar, R., Byrum, R. A., Buckler-White, A., Dewar, R. L., Buckler, C. E., et al. (2007). Human immunodeficiency virus type 1 derivative with 7% simian immunodeficiency virus genetic content is able to establish infections in pig-tailed macaques. J. Virol. 81, 11549–11552. doi: 10.1128/JVI.00960-07
Inuzuka, M., Hayakawa, M., and Ingi, T. (2005). Serinc, an activity-regulated protein family, incorporates serine into membrane lipid synthesis. J. Biol. Chem. 280, 35776–35783. doi: 10.1074/jbc.M505712200
Iyer, S. S., Bibollet-Ruche, F., Sherrill-Mix, S., Learn, G. H., Plenderleith, L., Smith, A. G., et al. (2017). Resistance to type 1 interferons is a major determinant of HIV-1 transmission fitness. Proc. Natl. Acad. Sci. U.S.A. 114, E590–E599. doi: 10.1073/pnas.1620144114
Jacquelin, B., Mayau, V., Targat, B., Liovat, A. S., Kunkel, D., Petitjean, G., et al. (2009). Nonpathogenic SIV infection of African green monkeys induces a strong but rapidly controlled type I IFN response. J. Clin. Invest. 119, 3544–3555. doi: 10.1172/JCI40093
Jia, B., Serra-Moreno, R., Neidermyer, W., Rahmberg, A., Mackey, J., Fofana, I. B., et al. (2009). Species-specific activity of SIV Nef and HIV-1 Vpu in overcoming restriction by tetherin/BST2. PLoS Pathog. 5:e1000429. doi: 10.1371/journal.ppat.1000429
Jia, R., Xu, F., Qian, J., Yao, Y., Miao, C., Zheng, Y. M., et al. (2014). Identification of an endocytic signal essential for the antiviral action of IFITM3. Cell. Microbiol. 16, 1080–1093. doi: 10.1111/cmi.12262
Joag, S. V., Li, Z., Foresman, L., Stephens, E. B., Zhao, L. J., Adany, I., et al. (1996). Chimeric simian/human immunodeficiency virus that causes progressive loss of CD4+ T cells and AIDS in pig-tailed macaques. J. Virol. 70, 3189–3197.
Kamada, K., Igarashi, T., Martin, M. A., Khamsri, B., Hatcho, K., Yamashita, T., et al. (2006). Generation of HIV-1 derivatives that productively infect macaque monkey lymphoid cells. Proc. Natl. Acad. Sci. U.S.A. 103, 16959–16964. doi: 10.1073/pnas.0608289103
Kane, M., Yadav, S. S., Bitzegeio, J., Kutluay, S. B., Zang, T., Wilson, S. J., et al. (2013). MX2 is an interferon-induced inhibitor of HIV-1 infection. Nature 502, 563–566. doi: 10.1038/nature12653
Kappes, J. C., Conway, J. A., Lee, S. W., Shaw, G. M., and Hahn, B. H. (1991). Human immunodeficiency virus type 2 vpx protein augments viral infectivity. Virology 184, 197–209. doi: 10.1016/0042-6822(91)90836-z
Kimata, J. T. (2014). Stepping toward a macaque model of HIV-1 induced AIDS. Viruses 6, 3643–3651. doi: 10.3390/v6093643
Kimata, J. T., Kuller, L., Anderson, D. B., Dailey, P., and Overbaugh, J. (1999). Emerging cytopathic and antigenic simian immunodeficiency virus variants influence AIDS progression. Nat. Med. 5, 535–541. doi: 10.1038/8414
Kimata, J. T., Mozaffarian, A., and Overbaugh, J. (1998). A lymph node-derived cytopathic simian immunodeficiency virus Mne variant replicates in nonstimulated peripheral blood mononuclear cells. J. Virol. 72, 245–256.
Kluge, S. F., Sauter, D., Vogl, M., Peeters, M., Li, Y., Bibollet-Ruche, F., et al. (2013). The transmembrane domain of HIV-1 Vpu is sufficient to confer anti-tetherin activity to SIVcpz and SIVgor Vpu proteins: cytoplasmic determinants of Vpu function. Retrovirology 10:32. doi: 10.1186/1742-4690-10-32
Kornbluth, R. S., Oh, P. S., Munis, J. R., Cleveland, P. H., and Richman, D. D. (1989). Interferons and bacterial lipopolysaccharide protect macrophages from productive infection by human immunodeficiency virus in vitro. J. Exp. Med. 169, 1137–1151. doi: 10.1084/jem.169.3.1137
Krapp, C., Hotter, D., Gawanbacht, A., McLaren, P. J., Kluge, S. F., Sturzel, C. M., et al. (2016). Guanylate Binding Protein (GBP) 5 Is an Interferon-Inducible Inhibitor of HIV-1 Infectivity. Cell Host Microbe 19, 504–514. doi: 10.1016/j.chom.2016.02.019
Kratovac, Z., Virgen, C. A., Bibollet-Ruche, F., Hahn, B. H., Bieniasz, P. D., and Hatziioannou, T. (2008). Primate lentivirus capsid sensitivity to TRIM5 proteins. J. Virol. 82, 6772–6777. doi: 10.1128/JVI.00410-08
Kuang, Y. Q., Tang, X., Liu, F. L., Jiang, X. L., Zhang, Y. P., Gao, G., et al. (2009). Genotyping of TRIM5 locus in northern pig-tailed macaques (Macaca leonina), a primate species susceptible to Human Immunodeficiency Virus type 1 infection. Retrovirology 6:58. doi: 10.1186/1742-4690-6-58
Kuroishi, A., Saito, A., Shingai, Y., Shioda, T., Nomaguchi, M., Adachi, A., et al. (2009). Modification of a loop sequence between alpha-helices 6 and 7 of virus capsid (CA) protein in a human immunodeficiency virus type 1 (HIV-1) derivative that has simian immunodeficiency virus (SIVmac239) vif and CA alpha-helices 4 and 5 loop improves replication in cynomolgus monkey cells. Retrovirology 6:70. doi: 10.1186/1742-4690-6-70
Laguette, N., Rahm, N., Sobhian, B., Chable-Bessia, C., Munch, J., Snoeck, J., et al. (2012). Evolutionary and functional analyses of the interaction between the myeloid restriction factor SAMHD1 and the lentiviral Vpx protein. Cell Host Microbe 11, 205–217. doi: 10.1016/j.chom.2012.01.007
Laguette, N., Sobhian, B., Casartelli, N., Ringeard, M., Chable-Bessia, C., Segeral, E., et al. (2011). SAMHD1 is the dendritic- and myeloid-cell-specific HIV-1 restriction factor counteracted by Vpx. Nature 474, 654–657. doi: 10.1038/nature10117
Letko, M., Silvestri, G., Hahn, B. H., Bibollet-Ruche, F., Gokcumen, O., Simon, V., et al. (2013). Vif proteins from diverse primate lentiviral lineages use the same binding site in APOBEC3G. J. Virol. 87, 11861–11871. doi: 10.1128/JVI.01944-13
Li, K., Jia, R., Li, M., Zheng, Y. M., Miao, C., Yao, Y., et al. (2015). A sorting signal suppresses IFITM1 restriction of viral entry. J. Biol. Chem. 290, 4248–4259. doi: 10.1074/jbc.M114.630780
Li, K., Markosyan, R. M., Zheng, Y. M., Golfetto, O., Bungart, B., Li, M., et al. (2013). IFITM proteins restrict viral membrane hemifusion. PLoS Pathog. 9:e1003124. doi: 10.1371/journal.ppat.1003124
Li, M., Kao, E., Gao, X., Sandig, H., Limmer, K., Pavon-Eternod, M., et al. (2012). Codon-usage-based inhibition of HIV protein synthesis by human schlafen 11. Nature 491, 125–128. doi: 10.1038/nature11433
Li, M., Waheed, A. A., Yu, J., Zeng, C., Chen, H. Y., Zheng, Y. M., et al. (2019). TIM-mediated inhibition of HIV-1 release is antagonized by Nef but potentiated by SERINC proteins. Proc. Natl. Acad. Sci. U.S.A. 116, 5705–5714. doi: 10.1073/pnas.1819475116
Li, Y., Kappes, J. C., Conway, J. A., Price, R. W., Shaw, G. M., and Hahn, B. H. (1991). Molecular characterization of human immunodeficiency virus type 1 cloned directly from uncultured human brain tissue: identification of replication-competent and -defective viral genomes. J. Virol. 65, 3973–3985.
Liao, C. H., Kuang, Y. Q., Liu, H. L., Zheng, Y. T., and Su, B. (2007). A novel fusion gene, TRIM5-Cyclophilin A in the pig-tailed macaque determines its susceptibility to HIV-1 infection. AIDS 21(Suppl. 8), S19–S26. doi: 10.1097/01.aids.0000304692.09143.1b
Lim, E. S., and Emerman, M. (2009). Simian immunodeficiency virus SIVagm from African green monkeys does not antagonize endogenous levels of African green monkey tetherin/BST-2. J. Virol. 83, 11673–11681. doi: 10.1128/JVI.00569-09
Lim, E. S., Fregoso, O. I., McCoy, C. O., Matsen, F. A., Malik, H. S., and Emerman, M. (2012). The ability of primate lentiviruses to degrade the monocyte restriction factor SAMHD1 preceded the birth of the viral accessory protein Vpx. Cell Host Microbe 11, 194–204. doi: 10.1016/j.chom.2012.01.004
Lim, E. S., Malik, H. S., and Emerman, M. (2010). Ancient adaptive evolution of tetherin shaped the functions of Vpu and Nef in human immunodeficiency virus and primate lentiviruses. J. Virol. 84, 7124–7134. doi: 10.1128/JVI.00468-10
Liu, H. L., Wang, Y. Q., Liao, C. H., Kuang, Y. Q., Zheng, Y. T., and Su, B. (2005). Adaptive evolution of primate TRIM5alpha, a gene restricting HIV-1 infection. Gene 362, 109–116. doi: 10.1016/j.gene.2005.06.045
Liu, S. Y., Aliyari, R., Chikere, K., Li, G., Marsden, M. D., Smith, J. K., et al. (2013). Interferon-inducible cholesterol-25-hydroxylase broadly inhibits viral entry by production of 25-hydroxycholesterol. Immunity 38, 92–105. doi: 10.1016/j.immuni.2012.11.005
Liu, Z., Pan, Q., Ding, S., Qian, J., Xu, F., Zhou, J., et al. (2013). The interferon-inducible MxB protein inhibits HIV-1 infection. Cell Host Microbe 14, 398–410. doi: 10.1016/j.chom.2013.08.015
Lu, J., Pan, Q., Rong, L., He, W., Liu, S. L., and Liang, C. (2011). The IFITM proteins inhibit HIV-1 infection. J. Virol. 85, 2126–2137. doi: 10.1128/JVI.01531-10
Luciw, P. A., Pratt-Lowe, E., Shaw, K. E., Levy, J. A., and Cheng-Mayer, C. (1995). Persistent infection of rhesus macaques with T-cell-line-tropic and macrophage-tropic clones of simian/human immunodeficiency viruses (SHIV). Proc. Natl. Acad. Sci. U.S.A. 92, 7490–7494. doi: 10.1073/pnas.92.16.7490
Mangeat, B., Turelli, P., Liao, S., and Trono, D. (2004). A single amino acid determinant governs the species-specific sensitivity of APOBEC3G to Vif action. J. Biol. Chem. 279, 14481–14483. doi: 10.1074/jbc.C400060200
Mariani, R., Chen, D., Schrofelbauer, B., Navarro, F., Konig, R., Bollman, B., et al. (2003). Species-specific exclusion of APOBEC3G from HIV-1 virions by Vif. Cell 114, 21–31. doi: 10.1016/s0092-8674(03)00515-4
Martinez-Steele, E., Awasana, A. A., Corrah, T., Sabally, S., van der Sande, M., Jaye, A., et al. (2007). Is HIV-2- induced AIDS different from HIV-1-associated AIDS? Data from a West African clinic. AIDS 21, 317–324. doi: 10.1097/QAD.0b013e328011d7ab
McNatt, M. W., Zang, T., Hatziioannou, T., Bartlett, M., Fofana, I. B., Johnson, W. E., et al. (2009). Species-specific activity of HIV-1 Vpu and positive selection of tetherin transmembrane domain variants. PLoS Pathog. 5:e1000300. doi: 10.1371/journal.ppat.1000300
Mehra, S., Golden, N. A., Dutta, N. K., Midkiff, C. C., Alvarez, X., Doyle, L. A., et al. (2011). Reactivation of latent tuberculosis in rhesus macaques by coinfection with simian immunodeficiency virus. J. Med. Primatol. 40, 233–243. doi: 10.1111/j.1600-0684.2011.00485.x
Meyerson, N. R., Warren, C. J., Vieira, D., Diaz-Griferro, F., and Sawyer, S. L. (2018). Species-specific vulnerability of RanBP2 shaped the evolution of SIV as it transmitted in African apes. PLoS Pathog. 14:e1006906. doi: 10.1371/journal.ppat.1006906
Meylan, P. R., Guatelli, J. C., Munis, J. R., Richman, D. D., and Kornbluth, R. S. (1993). Mechanisms for the inhibition of HIV replication by interferons-alpha, -beta, and -gamma in primary human macrophages. Virology 193, 138–148. doi: 10.1006/viro.1993.1110
Misra, A., Thippeshappa, R., and Kimata, J. T. (2013). Macaques as model hosts for studies of HIV-1 infection. Front. Microbiol. 4:176. doi: 10.3389/fmicb.2013.00176
Nakayama, E. E., Miyoshi, H., Nagai, Y., and Shioda, T. (2005). A specific region of 37 amino acid residues in the SPRY (B30.2) domain of African green monkey TRIM5alpha determines species-specific restriction of simian immunodeficiency virus SIVmac infection. J. Virol. 79, 8870–8877. doi: 10.1128/JVI.79.14.8870-8877.2005
Neil, S. J., Zang, T., and Bieniasz, P. D. (2008). Tetherin inhibits retrovirus release and is antagonized by HIV-1 Vpu. Nature 451, 425–430. doi: 10.1038/nature06553
Newman, R. M., Hall, L., Kirmaier, A., Pozzi, L. A., Pery, E., Farzan, M., et al. (2008). Evolution of a TRIM5-CypA splice isoform in old world monkeys. PLoS Pathog. 4:e1000003. doi: 10.1371/journal.ppat.1000003
Nisole, S., Lynch, C., Stoye, J. P., and Yap, M. W. (2004). A Trim5-cyclophilin A fusion protein found in owl monkey kidney cells can restrict HIV-1. Proc. Natl. Acad. Sci. U.S.A. 101, 13324–13328. doi: 10.1073/pnas.0404640101
Nomaguchi, M., Yokoyama, M., Kono, K., Nakayama, E. E., Shioda, T., Doi, N., et al. (2013a). Generation of rhesus macaque-tropic HIV-1 clones that are resistant to major anti-HIV-1 restriction factors. J. Virol. 87, 11447–11461. doi: 10.1128/JVI.01549-13
Nomaguchi, M., Yokoyama, M., Kono, K., Nakayama, E. E., Shioda, T., Saito, A., et al. (2013b). Gag-CA Q110D mutation elicits TRIM5-independent enhancement of HIV-1mt replication in macaque cells. Microbes Infect. 15, 56–65. doi: 10.1016/j.micinf.2012.10.013
Nyamweya, S., Hegedus, A., Jaye, A., Rowland-Jones, S., Flanagan, K. L., and Macallan, D. C. (2013). Comparing HIV-1 and HIV-2 infection: lessons for viral immunopathogenesis. Rev. Med. Virol. 23, 221–240. doi: 10.1002/rmv.1739
Ocwieja, K. E., Brady, T. L., Ronen, K., Huegel, A., Roth, S. L., Schaller, T., et al. (2011). HIV integration targeting: a pathway involving Transportin-3 and the nuclear pore protein RanBP2. PLoS Pathog. 7:e1001313. doi: 10.1371/journal.ppat.1001313
Okumura, A., Lu, G., Pitha-Rowe, I., and Pitha, P. M. (2006). Innate antiviral response targets HIV-1 release by the induction of ubiquitin-like protein ISG15. Proc. Natl. Acad. Sci. U.S.A. 103, 1440–1445. doi: 10.1073/pnas.0510518103
Otsuki, H., Yoneda, M., Igarashi, T., and Miura, T. (2014). Generation of a monkey-tropic human immunodeficiency virus type 1 carrying env from a CCR5-tropic subtype C clinical isolate. Virology 460-461, 1–10. doi: 10.1016/j.virol.2014.04.037
Pincetic, A., Kuang, Z., Seo, E. J., and Leis, J. (2010). The interferon-induced gene ISG15 blocks retrovirus release from cells late in the budding process. J. Virol. 84, 4725–4736. doi: 10.1128/JVI.02478-09
Pizzato, M., Helander, A., Popova, E., Calistri, A., Zamborlini, A., Palu, G., et al. (2007). Dynamin 2 is required for the enhancement of HIV-1 infectivity by Nef. Proc. Natl. Acad. Sci. U.S.A. 104, 6812–6817. doi: 10.1073/pnas.0607622104
Reimann, K. A., Li, J. T., Veazey, R., Halloran, M., Park, I. W., Karlsson, G. B., et al. (1996). A chimeric simian/human immunodeficiency virus expressing a primary patient human immunodeficiency virus type 1 isolate env causes an AIDS-like disease after in vivo passage in rhesus monkeys. J. Virol. 70, 6922–6928.
Rong, L., Zhang, J., Lu, J., Pan, Q., Lorgeoux, R. P., Aloysius, C., et al. (2009). The transmembrane domain of BST-2 determines its sensitivity to down-modulation by human immunodeficiency virus type 1 Vpu. J. Virol. 83, 7536–7546. doi: 10.1128/JVI.00620-09
Rosa, A., Chande, A., Ziglio, S., De Sanctis, V., Bertorelli, R., Goh, S. L., et al. (2015). HIV-1 Nef promotes infection by excluding SERINC5 from virion incorporation. Nature 526, 212–217. doi: 10.1038/nature15399
Saito, A., and Akari, H. (2013). Macaque-tropic human immunodeficiency virus type 1: breaking out of the host restriction factors. Front. Microbiol. 4:187. doi: 10.3389/fmicb.2013.00187
Saito, A., Nomaguchi, M., Iijima, S., Kuroishi, A., Yoshida, T., Lee, Y.-J., et al. (2011). Improved capacity of a monkey-tropic HIV-1 derivative to replicate in cynomolgus monkeys with minimal modifications. Microbes Infect. 13, 58–64. doi: 10.1016/j.micinf.2010.10.001
Saito, A., Nomaguchi, M., Kono, K., Iwatani, Y., Yokoyama, M., Yasutomi, Y., et al. (2013). TRIM5 genotypes in cynomolgus monkeys primarily influence inter-individual diversity in susceptibility to monkey-tropic human immunodeficiency virus type 1. J. Gen. Virol. 94(Pt 6), 1318–1324. doi: 10.1099/vir.0.050252-0
Sandler, N. G., Bosinger, S. E., Estes, J. D., Zhu, R. T., Tharp, G. K., Boritz, E., et al. (2014). Type I interferon responses in rhesus macaques prevent SIV infection and slow disease progression. Nature 511, 601–605. doi: 10.1038/nature13554
Sauter, D., and Kirchhoff, F. (2019). Key viral adaptations preceding the AIDS pandemic. Cell Host Microbe 25, 27–38. doi: 10.1016/j.chom.2018.12.002
Sauter, D., Schindler, M., Specht, A., Landford, W. N., Munch, J., Kim, K. A., et al. (2009). Tetherin-driven adaptation of Vpu and Nef function and the evolution of pandemic and nonpandemic HIV-1 strains. Cell Host Microbe 6, 409–421. doi: 10.1016/j.chom.2009.10.004
Sawyer, S. L., Emerman, M., and Malik, H. S. (2004). Ancient adaptive evolution of the primate antiviral DNA-editing enzyme APOBEC3G. PLoS Biol. 2:E275. doi: 10.1371/journal.pbio.0020275
Sawyer, S. L., Wu, L. I., Emerman, M., and Malik, H. S. (2005). Positive selection of primate TRIM5alpha identifies a critical species-specific retroviral restriction domain. Proc. Natl. Acad. Sci. U.S.A. 102, 2832–2837. doi: 10.1073/pnas.0409853102
Sayah, D. M., Sokolskaja, E., Berthoux, L., and Luban, J. (2004). Cyclophilin A retrotransposition into TRIM5 explains owl monkey resistance to HIV-1. Nature 430, 569–573. doi: 10.1038/nature02777
Schmidt, F., Keele, B. F., Del Prete, G. Q., Voronin, D., Fennessey, C. M., Soll, S., et al. (2019). Derivation of simian tropic HIV-1 infectious clone reveals virus adaptation to a new host. Proc. Natl. Acad. Sci. U.S.A. 116, 10504–10509. doi: 10.1073/pnas.1818059116
Schrofelbauer, B., Chen, D., and Landau, N. R. (2004). A single amino acid of APOBEC3G controls its species-specific interaction with virion infectivity factor (Vif). Proc. Natl. Acad. Sci. U.S.A. 101, 3927–3932. doi: 10.1073/pnas.0307132101
Schubert, U., Bour, S., Willey, R. L., and Strebel, K. (1999). Regulation of virus release by the macrophage-tropic human immunodeficiency virus type 1 AD8 isolate is redundant and can be controlled by either Vpu or Env. J. Virol. 73, 887–896.
Sharp, P. M., and Hahn, B. H. (2011). Origins of HIV and the AIDS pandemic. Cold Spring Harb. Perspect. Med. 1:a006841. doi: 10.1101/cshperspect.a006841
Sheehy, A. M., Gaddis, N. C., Choi, J. D., and Malim, M. H. (2002). Isolation of a human gene that inhibits HIV-1 infection and is suppressed by the viral Vif protein. Nature 418, 646–650. doi: 10.1038/nature00939
Sheehy, A. M., Gaddis, N. C., and Malim, M. H. (2003). The antiretroviral enzyme APOBEC3G is degraded by the proteasome in response to HIV-1 Vif. Nat. Med. 9, 1404–1407. doi: 10.1038/nm945
Shingai, M., Welbourn, S., Brenchley, J. M., Acharya, P., Miyagi, E., Plishka, R. J., et al. (2015). The Expression of Functional Vpx during Pathogenic SIVmac Infections of Rhesus Macaques Suppresses SAMHD1 in CD4+ Memory T Cells. PLoS Pathog. 11:e1004928. doi: 10.1371/journal.ppat.1004928
Shirazi, Y., and Pitha, P. M. (1992). Alpha interferon inhibits early stages of the human immunodeficiency virus type 1 replication cycle. J. Virol. 66, 1321–1328.
Song, R. J., Chenine, A. L., Rasmussen, R. A., Ruprecht, C. R., Mirshahidi, S., Grisson, R. D., et al. (2006). Molecularly cloned SHIV-1157ipd3N4: a highly replication- competent, mucosally transmissible R5 simian-human immunodeficiency virus encoding HIV clade C Env. J. Virol. 80, 8729–8738. doi: 10.1128/JVI.00558-06
Spence, J. S., He, R., Hoffmann, H. H., Das, T., Thinon, E., Rice, C. M., et al. (2019). IFITM3 directly engages and shuttles incoming virus particles to lysosomes. Nat. Chem. Biol. 15, 259–268. doi: 10.1038/s41589-018-0213-2
Stacey, A. R., Norris, P. J., Qin, L., Haygreen, E. A., Taylor, E., Heitman, J., et al. (2009). Induction of a striking systemic cytokine cascade prior to peak viremia in acute human immunodeficiency virus type 1 infection, in contrast to more modest and delayed responses in acute hepatitis B and C virus infections. J. Virol. 83, 3719–3733. doi: 10.1128/JVI.01844-08
Stremlau, M., Owens, C. M., Perron, M. J., Kiessling, M., Autissier, P., and Sodroski, J. (2004). The cytoplasmic body component TRIM5alpha restricts HIV-1 infection in Old World monkeys. Nature 427, 848–853. doi: 10.1038/nature02343
Takeuchi, J. S., Perche, B., Migraine, J., Mercier-Delarue, S., Ponscarme, D., Simon, F., et al. (2013). High level of susceptibility to human TRIM5alpha conferred by HIV-2 capsid sequences. Retrovirology 10:50. doi: 10.1186/1742-4690-10-50
Tartour, K., Appourchaux, R., Gaillard, J., Nguyen, X. N., Durand, S., Turpin, J., et al. (2014). IFITM proteins are incorporated onto HIV-1 virion particles and negatively imprint their infectivity. Retrovirology 11:103. doi: 10.1186/s12977-014-0103-y
Tartour, K., Nguyen, X. N., Appourchaux, R., Assil, S., Barateau, V., Bloyet, L. M., et al. (2017). Interference with the production of infectious viral particles and bimodal inhibition of replication are broadly conserved antiviral properties of IFITMs. PLoS Pathog. 13:e1006610. doi: 10.1371/journal.ppat.1006610
Theodore, T. S., Englund, G., Buckler-White, A., Buckler, C. E., Martin, M. A., and Peden, K. W. (1996). Construction and characterization of a stable full-length macrophage-tropic HIV type 1 molecular clone that directs the production of high titers of progeny virions. AIDS Res. Hum. Retroviruses 12, 191–194. doi: 10.1089/aid.1996.12.191
Thippeshappa, R., Polacino, P., Yu Kimata, M. T., Siwak, E. B., Anderson, D., Wang, W., et al. (2011). Vif substitution enables persistent infection of pig-tailed macaques by human immunodeficiency virus type 1. J. Virol. 85, 3767–3779. doi: 10.1128/JVI.02438-10
Thippeshappa, R., Ruan, H., and Kimata, J. T. (2012). Breaking barriers to an AIDS model with macaque-tropic HIV-1 derivatives. Biology 1, 134–164. doi: 10.3390/biology1020134
Thippeshappa, R., Ruan, H., Wang, W., Zhou, P., and Kimata, J. T. (2013). A variant macaque-tropic human immunodeficiency virus type 1 is resistant to alpha interferon-induced restriction in pig-tailed macaque CD4+ T cells. J. Virol. 87, 6678–6692. doi: 10.1128/JVI.00338-13
Usami, Y., Popov, S., and Gottlinger, H. G. (2014). The Nef-like effect of murine leukemia virus glycosylated gag on HIV-1 infectivity is mediated by its cytoplasmic domain and depends on the AP-2 adaptor complex. J. Virol. 88, 3443–3454. doi: 10.1128/JVI.01933-13
Usami, Y., Wu, Y., and Gottlinger, H. G. (2015). SERINC3 and SERINC5 restrict HIV-1 infectivity and are counteracted by Nef. Nature 526, 218–223. doi: 10.1038/nature15400
Van Damme, N., Goff, D., Katsura, C., Jorgenson, R. L., Mitchell, R., Johnson, M. C., et al. (2008). The interferon-induced protein BST-2 restricts HIV-1 release and is downregulated from the cell surface by the viral Vpu protein. Cell Host Microbe 3, 245–252. doi: 10.1016/j.chom.2008.03.001
Vigan, R., and Neil, S. J. (2010). Determinants of tetherin antagonism in the transmembrane domain of the human immunodeficiency virus type 1 Vpu protein. J. Virol. 84, 12958–12970. doi: 10.1128/JVI.01699-10
Virgen, C. A., Kratovac, Z., Bieniasz, P. D., and Hatziioannou, T. (2008). Independent genesis of chimeric TRIM5-cyclophilin proteins in two primate species. Proc. Natl. Acad. Sci. U.S.A. 105, 3563–3568. doi: 10.1073/pnas.0709258105
Weidner, J. M., Jiang, D., Pan, X. B., Chang, J., Block, T. M., and Guo, J. T. (2010). Interferon-induced cell membrane proteins, IFITM3 and tetherin, inhibit vesicular stomatitis virus infection via distinct mechanisms. J. Virol. 84, 12646–12657. doi: 10.1128/JVI.01328-10
Wilson, S. J., Webb, B. L., Ylinen, L. M., Verschoor, E., Heeney, J. L., and Towers, G. J. (2008). Independent evolution of an antiviral TRIMCyp in rhesus macaques. Proc. Natl. Acad. Sci. U.S.A. 105, 3557–3562. doi: 10.1073/pnas.0709003105
Wong, J. J., Pung, Y. F., Sze, N. S., and Chin, K. C. (2006). HERC5 is an IFN-induced HECT-type E3 protein ligase that mediates type I IFN-induced ISGylation of protein targets. Proc. Natl. Acad. Sci. U.S.A. 103, 10735–10740. doi: 10.1073/pnas.0600397103
Woods, M. W., Kelly, J. N., Hattlmann, C. J., Tong, J. G., Xu, L. S., Coleman, M. D., et al. (2011). Human HERC5 restricts an early stage of HIV-1 assembly by a mechanism correlating with the ISGylation of Gag. Retrovirology 8:95. doi: 10.1186/1742-4690-8-95
Xu, H., Svarovskaia, E. S., Barr, R., Zhang, Y., Khan, M. A., Strebel, K., et al. (2004). A single amino acid substitution in human APOBEC3G antiretroviral enzyme confers resistance to HIV-1 virion infectivity factor-induced depletion. Proc. Natl. Acad. Sci. U.S.A. 101, 5652–5657. doi: 10.1073/pnas.0400830101
Yang, S. J., Lopez, L. A., Hauser, H., Exline, C. M., Haworth, K. G., and Cannon, P. M. (2010). Anti-tetherin activities in Vpu-expressing primate lentiviruses. Retrovirology 7:13. doi: 10.1186/1742-4690-7-13
Ylinen, L. M., Keckesova, Z., Wilson, S. J., Ranasinghe, S., and Towers, G. J. (2005). Differential restriction of human immunodeficiency virus type 2 and simian immunodeficiency virus SIVmac by TRIM5alpha alleles. J. Virol. 79, 11580–11587. doi: 10.1128/JVI.79.18.11580-11587.2005
Yu, J., Li, M., Wilkins, J., Ding, S., Swartz, T. H., Esposito, A. M., et al. (2015). IFITM proteins restrict HIV-1 infection by antagonizing the envelope glycoprotein. Cell Rep. 13, 145–156. doi: 10.1016/j.celrep.2015.08.055
Yu, X. F., Yu, Q. C., Essex, M., and Lee, T. H. (1991). The vpx gene of simian immunodeficiency virus facilitates efficient viral replication in fresh lymphocytes and macrophage. J. Virol. 65, 5088–5091.
Yurkovetskiy, L., Guney, M. H., Kim, K., Goh, S. L., McCauley, S., Dauphin, A., et al. (2018). Primate immunodeficiency virus proteins Vpx and Vpr counteract transcriptional repression of proviruses by the HUSH complex. Nat. Microbiol. 3, 1354–1361. doi: 10.1038/s41564-018-0256-x
Zhang, C., de Silva, S., Wang, J. H., and Wu, L. (2012). Co-Evolution of Primate SAMHD1 and Lentivirus Vpx Leads to the Loss of the vpx Gene in HIV-1 Ancestor. PLoS One 7:e37477. doi: 10.1371/journal.pone.0037477
Zhang, F., Wilson, S. J., Landford, W. C., Virgen, B., Gregory, D., Johnson, M. C., et al. (2009). Nef proteins from simian immunodeficiency viruses are tetherin antagonists. Cell Host Microbe 6, 54–67. doi: 10.1016/j.chom.2009.05.008
Zhang, Z., Gu, Q., de Manuel Montero, M., Bravo, I. G., Marques-Bonet, T., Haussinger, D., et al. (2017). Stably expressed APOBEC3H forms a barrier for cross-species transmission of simian immunodeficiency virus of chimpanzee to humans. PLoS Pathog. 13:e1006746. doi: 10.1371/journal.ppat.1006746
Zhu, Y., Chen, G., Lv, F., Wang, X., Ji, X., Xu, Y., et al. (2011). Zinc-finger antiviral protein inhibits HIV-1 infection by selectively targeting multiply spliced viral mRNAs for degradation. Proc. Natl. Acad. Sci. U.S.A. 108, 15834–15839. doi: 10.1073/pnas.1101676108
Keywords: HIV-1, HSIV, stHIV, macaque model, pigtailed macaques, interferon, cross-species transmission, innate restriction
Citation: Thippeshappa R, Kimata JT and Kaushal D (2020) Toward a Macaque Model of HIV-1 Infection: Roadblocks, Progress, and Future Strategies. Front. Microbiol. 11:882. doi: 10.3389/fmicb.2020.00882
Received: 24 February 2020; Accepted: 16 April 2020;
Published: 13 May 2020.
Edited by:
Masako Nomaguchi, Tokushima University, JapanReviewed by:
Vanessa Hirsch, National Institutes of Health (NIH), United StatesHirofumi Akari, Kyoto University, Japan
Emi E. Nakayama, Osaka University, Japan
Copyright © 2020 Thippeshappa, Kimata and Kaushal. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rajesh Thippeshappa, rthippeshappa@txbiomed.org
 Rajesh Thippeshappa
Rajesh Thippeshappa Jason T. Kimata
Jason T. Kimata Deepak Kaushal
Deepak Kaushal